Abstract
Retrospective analysis of the spino-pelvic alignment in a population of 85 patients with a lumbar degenerative disease. Several previous publications reported the analysis of spino-pelvic alignment in the normal and low back pain population. Data suggested that patients with lumbar diseases have variations of sagittal alignment such as less distal lordosis, more proximal lumbar lordosis and a more vertical sacrum. Nevertheless most of these variations have been reported without reference to the pelvis shape which is well-known to strongly influence spino-pelvic alignment. The objective of this study was to analyse spino-pelvic parameters, including pelvis shape, in a population of 85 patients with a lumbar degenerative disease and compare these patients with a control group of normal volunteers. We analysed three different lumbar degenerative diseases: disc herniation (DH), n = 25; degenerative disc disease (DDD), n = 32; degenerative spondylolisthesis (DSPL), n = 28. Spino-pelvic alignment was analysed pre-operatively on full spine radiographs. Spino-pelvic parameters were measured as following: pelvic incidence, sacral slope, pelvic tilt, lumbar lordosis, thoracic kyphosis, spino-sacral angle and positioning of C7 plumb line. For each group of patients the sagittal profile was compared with a control population of 154 asymptomatic adults that was the subject of a previous study. In order to understand variations of spino-pelvic parameters in the patients’ population a stratification (matching) according to the pelvic incidence was done between the control group and each group of patients. Concerning first the pelvis shape, patients with DH and those with DDD demonstrated to have a mean pelvic incidence equal to 49.8° and 51.6°, respectively, versus 52° for the control group (no significant difference). Only young patients, less than 45 years old, with a disc disease (DH or DDD) demonstrated to have a pelvic incidence significantly lower (48.3°) than the control group, P < 0.05. On the contrary, in the DSPL group the pelvic incidence was significantly greater (60°) than the control group (52°), P < 0.0005. Secondly the three groups of patients were characterized by significant variations in spino-pelvic alignment: anterior translation of the C7 plumb line (P < 0.005 for DH, P < 0.05 for DDD and P < 0.05 for DSPL); loss of lumbar lordosis after matching according to pelvic incidence (P < 0.0005 for DH, DDD and DSPL); decrease of sacral slope after matching according to pelvic incidence (P = 0.001 for DH, P < 0.0005 for DDD and P < 0.0005 for DSPL). Measurement of the pelvic incidence and matching according to this parameter between each group of patients and the control group permitted to understand variations of spino-pelvic parameters in a population of patients.
Keywords: Sagittal balance, Pelvis shape, Pelvic incidence, Spinal alignment, Lumbar lordosis, Lumbar herniation, Spondylolisthesis
Introduction
The analysis of the sagittal balance recently appeared to be essential in the management of lumbar degenerative pathologies, especially when a spinal fusion is achieved [3, 8, 13, 14, 15, 16, 18, 19, 27]. The problem refers to the great variability of spinal alignment in the normal population, with a wide range of normal values in adults [7, 12, 25].
The sagittal balance is characterized by both pelvic and spinal parameters. Several studies have been carried out in the normal [5–7, 23, 26] and low back pain populations [9, 10, 13, 22].
In the normal population, correlations between the pelvic incidence, the sacral slope and sagittal curves (especially lumbar lordosis) have been well documented [4, 17, 26]. It is now well established that the shape and the spatial orientation of the pelvis determines the organization of the lumbo-thoracic spine. The shape is determinated by a fundamental parameter, the pelvic incidence, described by During [4] and more recently by Duval-Beaupère [5]. The pelvic incidence is a morphological parameter, not affected by the posture or the pelvis position and considered as invariable for a subject after the end of growth. Additionally being unaffected by lumbar degenerative changes the pelvic incidence represents a constant guide value to understand variations in the patients population. The orientation of pelvis is defined by two positional parameters: the pelvic tilt and the sacral slope.
The highest correlation (r = 0.85) in the normal population was found between lumbar lordosis (global lordotic curvature) and the sacral slope (angle defined by the horizontal axis and the superior endplate of S1). Regarding this data, Roussouly [23] proposed a classification of lumbar lordosis into four types based on the orientation of the sacral slope. However this classification described in a normal population may be difficult to apply in a population of patients considering that sacral slope is reported to be often affected by lumbar degenerative changes.
Correlation between lumbar lordosis and pelvic incidence is weaker, about 0.7, but seeing that pelvis incidence is a morphological parameter, not affected by degenerative lumbar lesions, this correlation is extremely useful and permits especially to understand variations in a population of patients affected by degenerative lumbar changes.
Several studies are reported concerning the analysis of sagittal balance in definite population of patients [4, 9, 10, 13]. However these studies were mainly performed in low back pain or isthmic spondylolisthesis populations, very few concerned disc herniations [22] or degenerative spondylolisthesis [21]. Low back pain subjects were characterized by less distal lordosis, more proximal lumbar lordosis and a more vertical sacrum. Nevertheless most of these variations have been reported without reference to the pelvis shape which is well-known to strongly influence spinal alignment, as discussed above.
Regarding these data, it appeared essential to undertake a comparative study with analysis of the sagittal balance, including analysis of pelvis shape, in a population of patients. In a first step, our institute established a data set for healthy asymptomatic volunteers that was the subject of a previously published paper [23]. We then proceeded with a roentgenographic analysis of spino-pelvic sagittal parameters in 85 patients with lumbar degenerative diseases: disc herniation (DH), degenerative disc disease (DDD) and degenerative spondylolisthesis (DSPL). The patients have been strictly evaluated with the same methodology of the asymptomatic control group.
Materials and methods
Materials
A total of 85 adult patients were included in this study. The average age of the subjects was 49 ± 12 years; there were 36 males and 49 females. Anthropometric characteristics of patients are summarised in Table 1.
Table 1.
Patient’s anthropomorphic characteristics
| Asymtomatic population | DH | DDD | DSPL | ||
|---|---|---|---|---|---|
| n | 154 | 25 | 32 | 28 | |
| Age | 27 ± 8 | 43.7 ± 11.6 | 46.2 ± 7.6 | 59.2 ± 12.2 | |
| Sex (%) | male | 46.3 | 68 | 48.4 | 14.3 |
| female | 53.7 | 32 | 51.6 | 85.7 | |
| Weight (kg) | – | 74.4 ± 14.6 | 68.9 ± 10.6 | 67.5 ± 13 | |
| Height (m) | – | 1.74 ± 0.1 | 1.69 ± 0.1 | 1.62 ± 0.1 | |
| BMI (kg/m²) | – | 24.3 ± 3.4 | 24.2 ± 3 | 25.7 ± 4.2 | |
BMI body mass index
For each parameter mean and SD are mentioned
All these patients have underwent a surgical procedure for a lumbar degenerative disease in the Centre des Massues between 1994 and 2004. Three pathologies were included in the study: disc herniation (DH), degenerative disc disease (DDD) involved one or two levels and degenerative spondylolisthesis (DSPL).
Levels concerned for DH: L5–S1, n = 11/25; L4–L5, n = 14/25;
Levels concerned for DDD: L5–S1, n = 8/32; L4–L5, n = 2/32; L5–S1 and L4–L5, n = 22/32;
Levels concerned for DSPL: L4–L5, n = 21/28; L3–L4, n = 3/28; L4–L5 and L3–L4, n = 4/28. The slipping was evaluated according to Morgan and King method index and was equal to 19.8 ± 8% with a range from 5 to 35%.
The surgery was a lumbo-sacral or lumbar fusion for DSPL and DDD and was a simple discectomy for DH.
Patients were excluded from the study if they had one or more of the following criteria (according to clinical and/or radiological data):
background of any spinal surgery (included simple lumbar discectomy)
spinal disease (trauma or tumor)
scoliosis
coxo-femoral pathology
isthmic lysis with or without spondylolisthesis.
Methods
Spino-pelvic parameters were measured on preoperative full spine radiographs in a standing position (Fig. 1). The patient was asked to stand in a standardized erect posture with the hands placed on supports and the knees held in extension. Two 30 × 90 cm exposures from the skull base to the proximal femora in both antero-posterior and lateral views were made. The distance from the radiographic source to the film was maintained at 230 cm for all exposures. The edges of the radiographic film were squared with respect to the horizontal and vertical axes. All radiological parameters were measured by a single author (CB).
Fig. 1.
AP and lateral radiographs of the spine and pelvis were made with the subject in a controlled standing position. The hands were placed on the rest and the patient was asked to stand in a comfortable but erect posture
Pelvic parameters
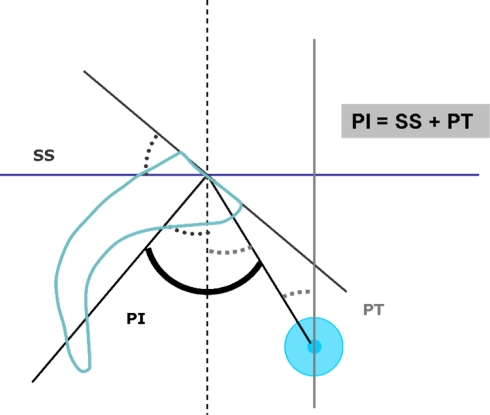
Pelvic parameters included in this analysis were the pelvic incidence, the sacral slope and the pelvic tilt (Fig. 2).
Fig. 2.
Pelvic parameters included in this analysis were the pelvic incidence (PI), the sacral slope (SS) and the pelvic tilt (PT)
The pelvic incidence (PI) was defined as the angle between the perpendicular to the sacral plate and the line connecting the midpoint of the sacral plate to the bi-coxo-femoral axis. The PI is a morphological parameter, considered as a constant, independent of the spatial orientation of the pelvis.
The sacral slope (SS) corresponds to the angle between the sacral plate and the horizontal plane. The SS is a positional parameter, varying according to the pelvis positioning.
The pelvic tilt (PT) corresponds to the angle between the line connecting the midpoint of the sacral plate to the bi-coxo-femoral axis and the vertical plane. As said for the SS, the PT is also a positional parameter.
The PI represents the algebraic sum of the SS and the PT: PI = SS + PT
Thus if we consider the incidence of one subject when the sacral slope increases the pelvic tilt decreases, and vice versa.
The sacro-femoral distance (SFD) is the horizontal distance between the bi-coxo-femoral axis and the vertical line passing through the posterior corner of the sacrum. This distance was used to analyse the positioning of the C7 plumb line and especially to measure the C7/SFD ratio.
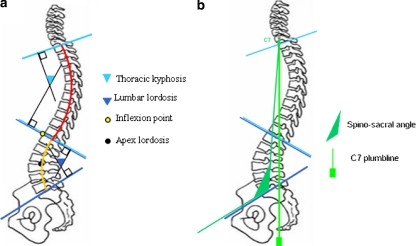
Spinal parameters
Spinal parameters included in this analysis were the lumbar lordosis (LL), the thoracic kyphosis (TK) and the spino-sacral angle (SSA) (Fig. 3).
Fig. 3.
a, b Spinal parameters included in this analysis were the lumbar lordosis (LL), the thoracic kyphosis (TK) and the spino-sacral angle (SSA)
The LL was defined as the extension spinal segment above the sacral plate. Thus it was measured using Cobb’s method from the sacral plate to the upper endplate of the most incline vertebrae into the thoraco-lumbar junction zone (corresponding to the inflection point where the spine transitions from lordosis to kyphosis).
The TK was measured from the upper endplate of the most incline vertebrae into the thoraco-lumbar junction zone to the superior plate of C7.
The SSA was defined as the angle between the sacral plate and the line connecting the centroid of C7 vertebral body and the midpoint of the sacral plate [24].
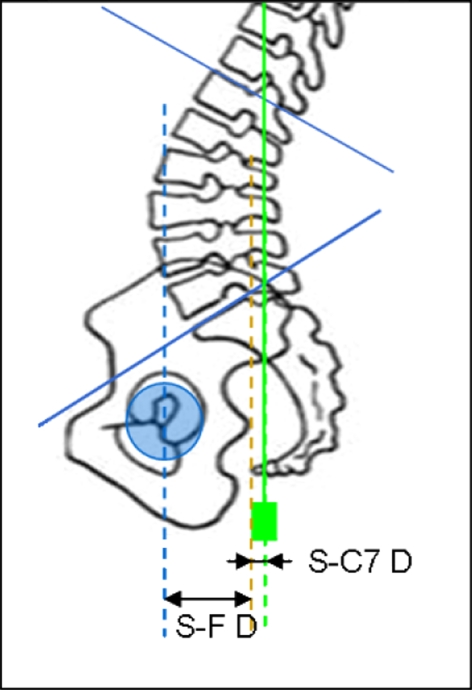
C7/SFD ratio
The horizontal distance between the posterior corner of the sacrum and the C7 plumb line was measured. The distance was noted positive when C7 plumb line projection was anterior to the posterior corner of the sacral endplate and negative when the projection of that line lied behind the posterior corner of the sacrum.
Then we calculated the C7/SFD ratio between this distance and the distance between the bi-coxo-femoral axis and the vertical line passing through the posterior corner of the sacral endplate [1] (Fig. 4). This ratio was equal to zero, when C7 plumb line projection was exactly on the posterior corner of the sacrum, and one, when C7 plumb line projection was exactly on the bi-coxo-femoral axis. It was negative when C7 plumb line projection lies behind the sacrum and more than one when C7 plumb line projects from anterior to the femoral heads. In the normal population the value of this ratio is −0.9 ± 1 [24].
Fig. 4.
Measurement of the C7/SFD ratio. SFD is the horizontal distance between the vertical bi-coxo-femoral axis and the vertical line passing through the posterior corner of the sacrum. The horizontal distance between C7 PL and the posterior corner of the sacrum (that is SC7 D) was also measured. Then we calculated the C7/SFD ratio corresponding to the ratio between SC7 Distance and SF Distance [1 ]
The spino-sacral angle and the C7/SFD ratio permitted to evaluate the global sagittal balance of the spine above the pelvis.
Statistical analysis
For the comparison with the normal population, we used data from a previous work recently published and realized in our institution [23]. In this work, we analysed the spino-pelvic parameters of a cohort of 154 normal volunteers without symptoms of back pain or radiographic abnormalities. The standardized radiographic examination was exactly the same than in our study.
So, Student’s t-tests could be performed to compare the mean value of spinal and pelvic parameters between two groups (a group of patients versus the control group). Correlations between two quantitative values were determinated using the Pearson correlation coefficient (Spearman coefficient when the size of the sample was less than 30). All P-values were two-sided and were considered statistically significant for a P value less than 0.05.
To statistically analyse and also understand the variations of positional parameters such as SS, PT, LL and TK in the patients’ population a stratification (matching) according to the pelvic incidence was carried out between the normal control group and each group of patients [1]. Thus we defined six different classes of pelvic incidence in the normal control group from I to VI corresponding to a progressively increase of the PI value (28–37.9°, 38–47.9°, 48–57.9°, 58–67.9°, 68–77.9°, 78–87.9°). Values of positional parameters for each class of PI are summarised in Table 2.
Table 2.
The six classes of pelvic incidence used for the stratification between the control group (n = 154) and each group of patients
| n | PI | PT | SS | LL | TK | |
|---|---|---|---|---|---|---|
| I 28° < PI < 37.9° | 12 | 35.4 ± 1.3 [33.7–37.9] | 3.9 ± 4.5 [−1.5 to 13.3] | 31.5 ± 5.2 [21.2–38.5] | 53.3 ± 6.6 [41.2–62] | 43.8 ± 9.1 [22.5–51.5] |
| II 38° < PI < 47.9° | 44 | 42.7 ± 2.8 [37.9–47.6] | 8.9 ± 4.8 [−5.1 to 18.2] | 33.8 ± 4.8 [23.1–48.4] | 55.5 ± 8 [41.5–76.5] | 48 ± 8.8 [24–64.7] |
| III 48° < PI < 57.9° | 59 | 52.6 ± 2.8 [48.2–57.4] | 12.5 ± 5.6 [−1.2 to 23.2] | 40.1 ± 5.5 [28.2–52.9] | 61.5 ± 8.4 [43.1–81.9] | 47.4 ± 10.7 [24–70.3] |
| IV 58° < PI < 67.9° | 26 | 62.6 ± 2.8 [58.2–67.6] | 15.8 ± 4.3 [7.1–26.8] | 46.8 ± 4.2 [37.9–58.5] | 68.3 ± 5.1 [60.9–76.3] | 47.6 ± 7.8 [34.7–64.7] |
| V 68° < PI < 77.9° | 11 | 72.6 ± 2.8 [69.6–77.4] | 19.7 ± 5.5 [12.6–27.9] | 52.9 ± 5.2 [46.2–59.6] | 74.9 ± 6.8 [62.2–81.6] | 46 ± 10.2 [29.7–62] |
| VI 78° < PI < 87.9° | 2 | 81.4 ± 3.3 [79.1–81.4] | 21.9 ± 12.3 [13.2–30.6] | 59.5 ± 9 [53.1–65.9] | 76 ± 8.3 [70.1–81.9] | 44.6 ± 12.2 [36–53.3] |
For each parameter mean, SD (±) and [min–max] are mentioned
Data derive from a previous already published study about spinal alignment of a cohort of 154 normal asymptomatic adults [23]. In order to understand variations of the SS, the PT, the LL and the TK in the patient’s population a stratification according to the PI was done between the normal control group and each group of patients [1]. Thus we define six different classes of pelvic incidence in the normal control group from I to VI
Results
Pelvic parameters
The pelvic incidence was 49.8° ± 11.4 for DH group and 51.6° ± 12.4 for the DDD group. No significant difference was found for the two groups after comparison with the control group (PI = 52° ± 10.7) (Tables 3, 4).
Table 3.
Pelvic parameters
| Control group | Control group class III | DH | DDD | Control group class IV | DSPL | |
|---|---|---|---|---|---|---|
| n | 154 | 59 | 25 | 32 | 26 | 28 |
| Pelvic incidence | 52° ± 10.7 | 52.6° ± 2.8 | 49.8° ± 11.4 NS | 51.6° ± 12.4 NS | 62.6° ± 2.8 | 60° ± 11.3 NS |
| Sacral slope | 40° ± 8.2 | 40.1° ± 5.5 | 35.4° ± 10.1 P = 0.001 | 35.6° ± 9.8 P < 0.0005 | 46.8° ± 4.2 | 40.1° ± 8.8 P < 0.0005 |
| Pelvic tilt | 12° ± 6.5 | 12.5° ± 5.6 | 14.4° ± 5.9 P = 0.017 | 16° ± 7.4 P < 0.0005 | 15.8° ± 4.3 | 19.9° ± 7 P < 0.0005 |
NS non significant
For each parameter mean and SD (±) are mentioned
Concerning mean value of the SS and the PT the significance of the statistical analysis results from the comparison with values of the normal population after stratification according to the PI
Table 4.
Pelvic incidence in population with disc diseases according to the age
| Asymtomatic population | DH + DDD < 45 ans | DH + DDD > 45 ans | |
|---|---|---|---|
| n | 154 | 27 | 30 |
| Pelvic incidence | 52° ± 10.7 | 48.3° ± 9.6 P < 0.05 | 53.2° ± 13.2 NS |
Population with disc diseases include patients with DH and patients with DDD
NS non significant
Only young patients, less than 45 years old, with disc disease (DH or DDD) demonstrated to have a pelvic incidence significantly lower than the control group (48.3° ± 9.6 versus 52°, respectively, P < 0.05).
After stratification according to the PI between the patients groups and the control group, we found that the sacral slope was significantly diminished for DH (P = 0.001) and for DDD (P < 0.0005). On the contrary, the pelvic tilt was significantly increased for DH (P < 0.05) and for DDD (P < 0.0005).
Concerning the patients with DSPL, the PI was significantly greater than the normal population (P < 0.0005). After stratification according to the PI between the patients groups and the control group, the SS appeared to be decreased (P < 0.0005) and the PT appeared to be increased (P < 0.0005).
Spinal parameters
After stratification according to the PI between the patients groups and the control group, the three groups of patients demonstrated significant less global lumbar lordosis, P < 0.0005 for each patients group (Table 5).
Table 5.
Spinal parameters
| Control group | Control Group Class III | DH | DDD | Control Group Class IV | DSPL | |
|---|---|---|---|---|---|---|
| n | 154 | 59 | 25 | 32 | 26 | 28 |
| Lumbar lordosis | 61° ± 9.7 | 61.5 ± 8.4 | 48.8° ± 11.9 P < 0.0005 | 48.8° ± 12.5 P < 0.0005 | 68.3 ± 5.1 | 59° ± 11.9 P < 0.0005 |
| Thoracic kyphosis | 47° ± 10.2 | 47.4 ± 10.7 | 40.2° ± 11.3 P < 0.002 | 39° ± 10.4 P < 0.0005 | 47.6 ± 7.8 | 43.8° ± 9.8 NS |
| C7/SFD ratio | − 0.9 ± 1 | – | 0.87 ± 0.62 P < 0.005 | 0.59 ± 0.77 P < 0.05 | – | 0.57 ± 0.66 P < 0.05 |
| SSA | 135° ± 7.8 | – | 123.5° ± 9.8 P < 0.005 | 127° ± 11.3 P < 0.05 | – | 127.5° ± 10 P < 0.05 |
NS non significant
For each parameter mean and SD (±) are mentioned
Concerning mean value of LL and TK the significance of the statistical analysis results from the comparison with values of the normal population after stratification according to the PI
SSA Spino-sacral angle
Concerning the thoracic kyphosis, after stratification, DH and DDD were the only two groups with significant less thoracic kyphosis (P < 0.002 for DH; P < 0.0005 for DDD).
Finally, the three lumbar diseases demonstrated a constant anterior translation of C7 plumb line as shown by a significant increase of the C7/SFD ratio, P < 0.05 for DH and DSPL and P < 0.005 for DH. This tendency to sagittal anterior unbalance was confirmed by the diminution of the sacro-spinal angle with a mean loss of 10°, P < 0.05 for DH and DSPL and P < 0.005 for DH.
Discussion
Into the normal population a standard sagittal balance does not exist [12, 25]. We can observe a great variability of spinal alignment, with a wide range of normal values in adults, and it is unreasonable to speak of normal kyphotic or lordotic curves. The most important thing to have is optimal congruence between pelvic and spinal parameters in order to achieve an economic posture placing the axis of gravity in a physiologic position [11, 16, 17]. To analyse sagittal balance of a subject it is fundamental now to include not only the spatial position of the pelvis but also its shape, reflected by pelvic incidence. Several studies demonstrated chain of correlations between spino-pelvic parameters with the main role of the pelvic incidence, determining the organization of the lumbo-thoracic spine [3, 7, 26].
Values and correlations of spino-pelvic parameters are now well established in the asymptomatic population. Concerning population of patients, we hypothesized first that lumbar degenerative lesions could affect all the positional spino-pelvic parameters, and secondly, that the shape of the pelvis, and thus the type of spino-pelvic alignment, could determine the type of lumbar degenerative disease.
Disc pathologies
Patients with DH and patients with DDD demonstrated to have a very similar sagittal profile characterized by a normal or low pelvic incidence. Values of the sacral slope, the pelvis tilt, the lumbar lordosis and the thoracic kyphosis were very close in the two groups. Thus these patients are characterized by flat spine with significant reduction of both lumbar lordosis and thoracic kyphosis. This profile was more marked for patients with disc diseases below 45 years old with a PI significantly lower than the asymptomatic population.
Loss of lordosis is not only structural, secondary to the segmental discopathy and loss of disc height, but also postural secondary to the analgesic posture of the patient to avoid posterior discal hyperpression. Unfortunately it is difficult to precisely determine the respective part of structural and/or postural loss of lordosis.
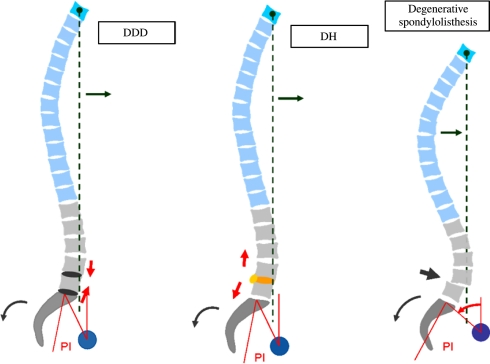
Loss of lordosis necessarily leads to a significant anterior displacement of the C7 plumbline (Fig. 5), as observed in our study. This sagittal unbalance is partially corrected by the pelvis backtilt.
Fig. 5.
Variations of spino-pelvic alignment in patient’s population. Variations of sagittal balance were in the same ways for patients with disc diseases (DDD and DH) and for patients with DSPL: anterior displacement of C7 plumb line, loss of lordosis and pelvis backtilt. Difference between disc diseases (DH and DDD) and DSPL concerned the shape of the pelvis: the PI was normal or decreased for DH and DDD and was increased for DSPL population
Our findings were concordant with those of Rajnic showing that patients with disc herniation had a relatively straight spine in the sagittal plane with a significant decrease of both the lumbar lordosis and the sacral slope [22].
Although the surgical procedure is clearly different for patients with degenerative discopathy (fusion) and patients with disc herniation (discectomy), it was some kind of relief to find a similar profile for these two pathologies taking in account that the same anatomical structure is concerned in them, i.e. the intervertebral disc.
Degenerative spondylolisthesis
In this study patients with degenerative spondylolisthesis demonstrated a significant greater pelvic incidence (60°) than the normal population suggesting that the shape of the pelvis is a main predisposing factor for DSPL. In the normal population great pelvis incidence is usually associated with pronounced sacral slope and more lumbar lordosis [23]. The great lordosis of these patients generates amount of forces on posterior articular joints and probably excessive mechanical stresses on posterior facets accelerating arthrosis changes. We may hypothesize that posterior arthritis associated with a marked inclination of the vertebral endplate of L5 (consequently of the sagittal profile of the subject) represent a significant predisposing factor for slippage [2, 20].
As for disc diseases, we also observed in the DSPL population loss of lordosis, tendancy to anterior sagittal unbalance and less sacral slope reflecting the pelvis backtilt of these patients (Fig. 5). It was interesting to find that these variations were in the same ways that those usually described for major sagittal unbalance [27].
As for disc diseases, we can assess that these variations are consequences of both postural and structural changes. Discopathy and slippage result in a structural loss of lordosis. On the other side analgesic flexion posture, limiting spinal canal stenosis, leads to a postural decrease of LL. Even if it is difficult to determine the part of structural loss of lordosis and the postural part, we observe that this loss of lordosis induces into a significant anterior displacement of C7 plumbline and center of gravity, resulting in an increased flexion moment applied to the spine. To compensate this, patients generate a decrease of SS associated with an increase of PT (that is pelvis backtilt). This mechanism can be easily achieved for these patients characterized by a great PI and seeing that the value of PI determines the capacity of pelvis retroversion (considering that PI = SS + PT and that SS cannot be a negative number). You can tilt more with a high PI than a low PI since there is a much wider range through which adaptation can occur. Thus in DSPL population the sagittal unbalance is usually moderate and compensated (Fig. 5).
Our findings were concordant with those mentioned by Morel in a series of 53 DSPL [21]. The group of DSPL demonstrated a significant higher PI, a loss of LL and a decrease in SS. This study suggested the impact of the sagittal profile in pathogenesis of the degenerative spondylolisthesis.
Conclusions
The three groups of patients demonstrated three fundamental and significant variations into spino-pelvic alignment as followed: anterior translation of the C7 plumb line, loss of lumbar lordosis and less sacral slope, that is pelvis backtilt.
Additionally the shape of the pelvis appeared well influence the type of degenerative disease observed seeing that patients with disc lesions were characterized by a normal or low PI with straight spine whereas degenerative spondylolisthesis population demonstrated pronounced spinal curves with great PI.
Finally this study suggests the high interest of a spinal alignment’s classification based on the PI into normal and pathologic conditions.
Acknowledgments
We express our gratitude to Dr. Mark Weidenbaum, department of orthopaedic surgery, New York, and Dr Jérôme Paquet, Hôpital Neurologique P. Wertheimer, Lyon, France, for their assistance in paper’s translation.
References
- 1.Barrey C (2004) Equilibre sagittal pelvi-rachidien et pathologies lombaires dégénératives. Etude comparative à propos de 100 cas (in French). Thèse de Médecine. Université Claude Bernard, Lyon
- 2.Berlemann U, Jeszenszky, Buhler D, Harms J. Facet joint remodelling in degenerative spondylolisthesis: an investigation of joint orientation and tropism. Eur Spine J. 1998;7:376–380. doi: 10.1007/s005860050093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal spine and pelvis using shape and orientation parameters. J Spinal Disord Tech. 2005;18:40–47. doi: 10.1097/01.bsd.0000117542.88865.77. [DOI] [PubMed] [Google Scholar]
- 4.During J, Goudfrooij H, Keessen W, Beeker TW, Crowe A. Towards standards for posture. Postural characteristics of the lower back system in normal and pathologic conditions. Spine. 1985;10:83–87. doi: 10.1097/00007632-198501000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Duval-Beaupère G, Legaye J. Composante sagittale de la statique rachidienne (in French) Rev Rhum. 2004;71:105–119. doi: 10.1016/j.rhum.2003.09.018. [DOI] [Google Scholar]
- 6.Gelb DE, Lenke LG, Bridwell KH, Blanke K, MacEnery KW. An analysis of sagittal spinal aligment in 100 asymptomatic middle and older aged volunteers. Spine. 1995;20:1351–1358. doi: 10.1097/00007632-199506000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Guigui P, Levassor N, Rillardon L, Wodecki P, Cardinne L. Valeur physiologique des paramètres pelviens et rachidiens de l’équilibre sagittal du rachis. Analyse d’une série de 250 volontaires (in French) Rev Chir Orthop. 2003;89:496–506. [PubMed] [Google Scholar]
- 8.Izumi Y, Kumano K. Analysis of sagittal lumbar alignment before and after posterior instrumentation: risk factor for adjacent unfused segment. Eur J Orthop Surg Traum. 2001;1:9–13. doi: 10.1007/BF01706654. [DOI] [Google Scholar]
- 9.Jackson RP, MacManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex and size. Spine. 1994;19:1611–1618. doi: 10.1097/00007632-199407001-00010. [DOI] [PubMed] [Google Scholar]
- 10.Jackson RP, Kanemura T, Kawakami N, Hales C. Lumbopelvic lordosis and pelvic balance on repeated standing lateral radiographs of adult volunteers and untreated patients with constant low back pain. Spine. 2000;25:575–586. doi: 10.1097/00007632-200003010-00008. [DOI] [PubMed] [Google Scholar]
- 11.Kobayashi T, Atsuta Y, Matsuno T, Takeda N. A longitudinal study of congruent sagittal spinal alignment in an adult cohort. Spine. 2004;29:671–676. doi: 10.1097/01.BRS.0000115127.51758.A2. [DOI] [PubMed] [Google Scholar]
- 12.Korovessis PG, Stamatakis MV, Baikousis AG. Reciprocal angulation of vertebral bodies in the sagittal plane in a asymptomatic greek population. Spine. 1998;23:700–704. doi: 10.1097/00007632-199803150-00010. [DOI] [PubMed] [Google Scholar]
- 13.Korovessis PG, Dimas A, Iliopoulos P, Lambiris E. Correlative analysis of lateral vertebral radiographic variables and medical outcomes study short-form health survey: a comparative study in asymptomatic volunteers versus patients with low back pain. J Spinal Disord Tech. 2002;15:384–390. doi: 10.1097/00024720-200210000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Kumar MN, Baklanov A, Chopin D. Correlation between sagittal plane changes and adjacent segment degeneration following lumbar spine fusion. Eur Spine J. 2001;10:314–319. doi: 10.1007/s005860000239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lazennec JY, Ramare S, Arafati N, Laudet CG, Gorin M, Roger B, Hansen S, Saillant G, Maurs L, Trabelsi R. Sagittal alignment in lumbosacral fusion: relations between radiological parameters and pain. Eur Spine J. 2000;9:47–55. doi: 10.1007/s005860050008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Legaye J, Hecquet J, Marty C, Duval-Beaupère G. Equilibre sagittal du rachis. Relations entre bassin et courbures rachidiennes sagittales en position debout. Rachis. 1993;5:215–226. [Google Scholar]
- 17.Legaye J, Duval-Beaupère G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7:99–103. doi: 10.1007/s005860050038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mangione P, Senegas J. L’équilibre rachidien dans le plan sagittal (in French) Rev Chir Orthop. 1997;83:22–32. [PubMed] [Google Scholar]
- 19.Marnay T (1988) Equilibre du rachis et du bassin. Cahiers d’enseignement de la SOFCOT. Elsevier, Paris, pp 281–313
- 20.Matsunaga S, Sakou T, Morizono Y, Masuda A, Demirtas AM. Natural history of degenerative spondylolisthesis. Pathogenesis and natural course of the slippage. Spine. 1990;15:1204–1210. doi: 10.1097/00007632-199011010-00021. [DOI] [PubMed] [Google Scholar]
- 21.Morel E, Vialle R, Rillardon L, Guigui P (2004) Analyse de l’équilibre sagittal du rachis dans les spondylolisthésis dégénératifs. Deuxièmes Journées du Rachis de Paris. In: Sauramps medical, Paris, pp 107–118
- 22.Rajnics P, Templier A, Skalli W, Lavaste F, Illes T. The importance of spinopelvic parameters in patients with lumbar disc lesions. Int Orthop. 2002;26:104–108. doi: 10.1007/s00264-001-0317-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine. 2005;30:346–353. doi: 10.1097/01.brs.0000152379.54463.65. [DOI] [PubMed] [Google Scholar]
- 24.Roussouly P, Gollogly S, Noseda O, Berthonnaud E, Dimnet J. The vertical projection of the sum of the ground reactive forces of a standing patient is not the same as the C7 plumbline: a radiographic study of the sagiital alignment of 153 asymptomatic volunteers. Spine. 2006;31:E320–E325. doi: 10.1097/01.brs.0000218263.58642.ff. [DOI] [PubMed] [Google Scholar]
- 25.Stagnara P, Mauroy JC, Dran G, Gonon G, Costanzo G, Dimnet J, Pasquet A. Reciprocal angulation of vertebral bodies in a sagittal plane: approach to references for the evaluation of kyphosis and lordosis. Spine. 1982;7:335–342. doi: 10.1097/00007632-198207000-00003. [DOI] [PubMed] [Google Scholar]
- 26.Vaz G, Roussouly P, Berthonnaud E, Dimnet J. Sagittal morphology and equilibrium of pelvis and spine. Eur Spine J. 2002;11:80–87. doi: 10.1007/s005860000224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vital JM, Gille O, Gangnet N. Equilibre sagittal et applications cliniques (in French) Rev Rhum. 2004;71:120–128. doi: 10.1016/j.rhum.2003.09.020. [DOI] [Google Scholar]