Abstract
The insufficient exploration of intervertebral translation during flexion and extension prevents the further understanding of the cervical biomechanics and treating the cervical related dysfunction. The objective of this study was to quantitatively measure the continuous intervertebral translation of healthy cervical spine during flexion and extension by videofluoroscopic technique. A total of 1,120 image sequences were analyzed for 56 healthy adult subjects by a precise image protocol during cervical flexion and extension. our results showed there were no statistical angular differences among five spinal levels in either flexion or extension, except for the comparison between C2/3 (13.5°) and C4/5 (22.6°) angles. During cervical flexion, the smallest anterior translations were 0.7 mm at C2/3 level, followed by 0.9 mm at C6/7, 1.0 mm at C3/4, 1.1 mm at C5/6, and the largest 1.2 mm at C4/5 levels. The significantly greater translations were measured in the posterior direction at C3/4 (1.1 mm, P = 0.037), C4/5 (1.3 mm, P = 0.039), and C5/6 (1.2 mm, P = 0.005) levels than in the anterior one. The relatively fluctuant and small average posterior translation fashion at C6/7 level (0.4 mm) possibly originated from the variations in the direction of translation during cervical extension among subjects. Normalization with respect to the widths of individual vertebrae showed the total translation percentages relative to the adjacent vertebrae were 9.5, 13.7, 16.6, 15.0, and 8.6% for C2/3 to C6/7 levels, respectively, and appeared to be within the clinical-accepted ranges of translation in cervical spine. The intervertebral translations of cervical spine during flexion and extension movements were first described in quality and quantity based on the validated radiographic protocol. This analysis of the continuous intervertebral translations may be further employed to diagnose translation abnormalities like hypomobility or hypermobility and to monitor the treatment effect on cervical spines.
Keywords: Cervical spine, Intervertebral translation, Videofluoroscopy, Biomechanics
Introduction
The cervical spine supports the skull and allows for a wide range of physiological motion of neck in order to integrate the head with the rest of the body and environments. Abnormal intervertebral movements of spine have been reported to be associated with trauma and pathological conditions [1, 4, 12, 25, 33, 38]. The evaluation of cervical intervertebral movements is essential for providing the diagnostic information in cervical related dysfunction.
Several methods of determining the cervical motion (such as tape measure, goniometer, and inclinometer) are available to the medical practitioners [19, 36, 41]. The application of these methods is relatively easy and inexpensive, but the absence of accurate identification of the skeletal movements leads to controversy. Recently, the experimental instruments like electromagnetic tracking device, video-based motion analysis, and ultrasonography-based system have been applied to investigate the movement of spine [6, 13, 15, 20, 34, 37, 39]. However, without resorting to invasive techniques, the precise assessment of clinically relevant variables, such as intervertebral movements, is difficult to obtain. The radiographic evaluation has long been considered as a gold standard for studying the cervical intervertebral motions. Several studies explored the intervertebral angles or spinal curvature by lateral plain radiographs [3, 5, 7, 8, 17, 21, 28], but the translation movements between spinal segments attracted limited attentions. The abnormal or excessive translations between vertebrae in the sagittal plane are clinically important clues to dysfunction or instability. Roche et al. [33] reported the different distance indexes to detect the anterior atlanto-axial subluxation in patients with rheumatoid arthritis. Tsai et al. [38] explored the abnormal lumbar segmental angulation and translation in patients with the spinal spondylolisthetic change. Frobin et al. [8] proposed a new protocol to precisely measure the sagittal plane intervertebral motion of the cervical spine by radiographs. Though these radiographic researches provided a highly reliable tool for measuring the segmental spinal curvatures, the use of the X-ray photographic method is restricted to static imaging and excessive radiation exposure.
Because of the real-time visualization and reduced radiation exposure, the videofluoroscopy technology is more appreciated when the examination of skeletal movements is necessary for clinical diagnosis and research purposes [2, 28]. A few researchers have applied the videofluoroscopy to evaluate the continuous spinal movement and the different time lags and motion sequences were detected between normal and pathological spines [12, 25]. The dynamic intervertebral movements in lumbar flexion and extension were recently investigated [10, 20, 42], however, these studies revealed the divergent results on motion sequences in flexion and extension from upper to lower vertebrae and the variations on anatomical identification. Penning further suggested that the segmental motion of cervical spine was not simply a rocking movement but accompanied by a displacement between vertebrae [28]. Those previous studies which have included only the rotational movements between vertebral segments, the translation movements were usually disregarded. Despite the fact that translational data could be assessed at the end range of movement [8, 30, 32], the drawback of those results was the absence of information regarding the dynamic motion that occurred throughout the ROM. Therefore the objective of this study was to quantitatively analyze the continuous intervertebral translation of healthy cervical spine during flexion–extension movements by a standard radiographic image protocol in order to provide additional insights to the cervical biomechanics.
Methods
A total of 56 healthy adult subjects (28 males and 28 females) without neck symptoms within recent 4 weeks participated in this study. Their ages ranged from 20 to 30 years with a mean age of 25.8 ± 2.7 years. The subjects were excluded if she/he had (1) history of cervical trauma or surgery, (2) bone pathology, (3) arthritic or other inflammatory disorders, (4) pregnancy, and (5) restrictive muscle spasm.
The videofluoroscopy system (Diagnost 97, Philips Corporation, USA) was applied to evaluate the continuous segmental movement of the cervical spine at a rate of 30 frames per second. The image intensifier was used in videofluoroscopy instead of intensifying screens and film as an image receptor, and this permited imaging at very low radiation exposure to the patient. This study was approved by the ethics committee for human research of a medical center. The experimental procedures and risks of the radiation exposure were fully explained to each subject, and signed informed consent was obtained. During screening, the images were displayed on a high-resolution monitor and recorded by a super VHS video recorder. The subjects were instructed to stand upright between the image intensifier and the examination table. The subjects placed their forearms on the armrests aside the examination table to reduce excessive trunk movement. The radiographic beam field of the videofluoroscopy unit was collimated to obtain optimal sharpness of the image. The size of the imaging field was also adjusted to view the whole cervical spine motion.
The measurement of the kinematics in the sagittal plane in this study involved two assumptions. First, the voluntary flexion–extension has been reported to be accompanied by limited lateral bending or axial rotation [36]. Second, the intact vertebral body was assumed to be a rigid body for the kinematic analysis. Before actual screening, the subjects were allowed to practice the flexion–extension of the cervical spine a few times with correction to reduce the trunk and out-of-plane motions. Though the fluoroscopic image sequence could provide an objective and precise quantification of intervertebral movement, the out-of-plane motion and errors in reference point placement should be considered [11]. To increase accuracy of intervertebral translation measurement in 2-D representation of the videofluoroscopy system, it was important to align the projection direction of the radiographic beam perpendicular to the plane of movement. Two portable laser alignment devices were used to assure the perpendicularity between the plane of cervical motion and the projection direction of the radiographic beam. A semicircular guide was also positioned in the mid-sagittal plane in front of the subjects during cervical motion. The subjects were instructed to move at a modest, constant rate to avoid the motion blur or excessive radiation exposure. The motion of cervical flexion, extension, and then return to the neutral position was performed in five seconds.
The recorded video images of the cervical motion were captured at 30 frames per second using the Matrox RT 2000 (Matrox Electronic Systems Ltd., Quebec, Canada) and Adobe Premiere 6.5 computer software (Adobe Systems Inc., USA) and then transformed into sequences of bitmap pictures. Ten pictures in evenly divided intervals of the cervical ROM in flexion and extension were selected for digitizing, respectively. During the image analysis, the positions of the 22 bony landmarks were digitized utilizing SigmaScan 5.0 (SPSS Inc., Chicago, IL, USA) on a high-resolution monitor. The anatomical identifications of the bony landmarks were based on the well-accepted radiographic method of Frobin et al. [8, 22, 29]. There were two inferior corners of the second vertebra (C2), and anterior- posterior corners of the superior and inferior endplates from the third to seventh cervical vertebrae (C3–C7). This method of skeletal identification has been proved valid, accurate, and reliable for detecting the intervertebral movements [22, 29]. The methods for identifying vertebral landmarks were blinded between examiners and totally 2 sets of 1,120 image sequences were digitized by 2 trained individuals. These vertebral landmarks were digitized three times each, and the mean values of the three measurements were used for subsequent analysis.
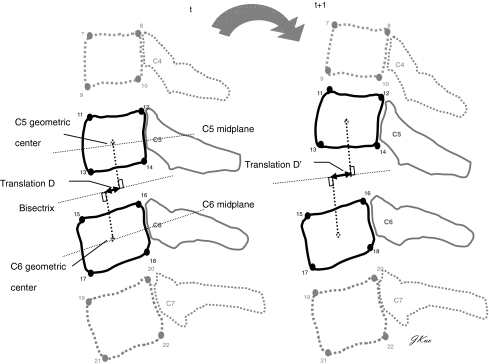
A custom computer program was used to construct the midplanes of vertebrae defined as a line running through the midpoints between anterior two corners and posterior two corners, bisectrix between two midplanes, and the perpendiculars from centers of the adjacent vertebrae in order to calculate the relative translation of cervical spine [8, 29] (Fig. 1). An X-ray ruler was used to obtain the actual vertebral dimensions and the width of next upper vertebral endplate was used to normalize the measurement of intervertebral anterior or posterior translation. The reliabilities of the digitizing procedures within raters at a 2-week interval and between raters were assessed with the intraclass correlation coefficient (ICC) and mean absolute difference (MAD) methods in six different randomly selected subjects [18, 35, 43]. Comparisons among intervertebral angulation or translation movements throughout ROM were performed with one-way analysis of variance (ANOVA) with a probability level of P < 0.05 selected as the criterion for noting significant difference. For any statistically significant findings obtained in the ANOVA, the Tukey’s studentized range (HSD) test was performed to identify the differences among 5 vertebral levels in both flexion and extension. For the comparison at the same spinal level, a Student t test with a probability level of P < 0.05 was selected as the criterion for noting significant difference between flexion and extension movements. Analyses were performed using the Scientific Package for Social Sciences (version 12; SPSS, Chicago, IL, USA).
Fig. 1.
Definition of the intervertebral angulations and translations between C5/6 from sequential images during cervical extension. The intervertebral angulation was determined by the angle of midplanes, and the perpendiculars from centers of the adjacent vertebrae were applied to calculate the translation at specific spinal level
Results
The mean ages of the 56 asymptomatic participants were 25.8 ± 2.7 years (female: 25.1 ± 2.5 years; male: 26.5 ± 1.8 years). The body heights and weights were 160.7 ± 3.8 cm and 51.3 ± 4.7 kg for the female subjects, and 172.8 ± 5.7 cm and 70.7 ± 6.2 kg for the male subjects.
Evaluation of errors and repeatability
Two assessments were conducted to measure the errors on identifying the positions of vertebral landmarks and calculating the derived sequential translation movements throughout the flexion and extension. The ICCs averaged 0.993 and 0.999 for the first and second raters on identifying the positions of vertebral landmarks in sequential images, respectively. The MADs of identifying the positions of vertebral landmarks were 0.7 ± 0.1 mm for both raters. For the inter-rater reliability, the ICC values averaged 0.974 with a MAD of 0.7 ± 0.2 mm on identifying the positions of different vertebral landmarks in sequential images.
The ICCs for the calculated sequential translation movements throughout the flexion and extension ranged from 0.710 to 0.918 (average = 0.802) and the corresponding MAD averaged 0.2 ± 0.1 mm and 0.3 ± 0.1 mm within the first rater and second rater, respectively. Considering the inter-rater reliability, the ICC values for the calculated sequential translation movements ranged from 0.662 to 0.882 (average = 0.723) and the MAD averaged 0.2 ± 0.2 mm between raters.
Intervertebral angulation
In order to understand better the intervertebral movement, the spinal angulation between two vertebrae defined by the angle of vertebral midplanes was also presented (Fig. 1). The range of intervertebral angles that accounted 95% of our subjects studied during flexion and extension movements were summarized in Table 1. In general, there were no statistical angular differences among 5 spinal levels in different motion, whereas only the comparison between C2/3 angle and C4/5 angle revealed the significances at extension (P = 0.044) and at total ROM (P = 0.007). For the comparison between flexion and extension at the individual spinal levels, no significant angular differences were detected (P = 0.066–0.931).
Table 1.
The mean values of the intervertebral angulations with 95% confidence intervals at each spinal level during cervical flexion and extension
| Level | Mean (degree) | Standard deviation | Individual 95% confidence interval | Comparison between flexion and extension P value | ||
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| C2/3 Angle (1) | Flexion | 5.8 | 2.8 | 4.4 | 7.1 | 0.066 |
| Extension | 7.7 | 3.7 | 6.0 | 9.5 | ||
| Total ROM | 13.5 | 4.8 | 11.2 | 15.8 | ||
| C3/4 Angle (2) | Flexion | 7.3 | 3.8 | 5.5 | 9.2 | 0.079 |
| Extension | 10.0 | 5.6 | 7.2 | 12.7 | ||
| Total ROM | 17.3 | 7.4 | 13.7 | 20.8 | ||
| C4/5 Angle (3) | Flexion | 10.0 | 6.4 | 6.7 | 13.4 | 0.268 |
| Extension | 12.6 | 5.2 | 10.0 | 15.1 | ||
| Total ROM | 22.6 | 7.9 | 18.8 | 26.4 | ||
| C5/6 Angle (4) | Flexion | 9.6 | 6.1 | 6.7 | 12.6 | 0.931 |
| Extension | 9.4 | 6.7 | 6.2 | 12.7 | ||
| Total ROM | 19.0 | 6.6 | 15.9 | 22.2 | ||
| C6/7 Angle (5) | Flexion | 10.0 | 6.6 | 6.4 | 13.7 | 0.204 |
| Extension | 7.9 | 7.7 | 3.6 | 12.2 | ||
| Total ROM | 17.9 | 9.1 | 13.6 | 22.3 | ||
| Comparison among 5 spinal levels P Value |
Flexion | 0.083 | ||||
| Extension | 0.044* (1,3) | |||||
| Total ROM | 0.007* (1,3) | |||||
No significant difference was found between flexion and extension within each level
* P < 0.05 compared among spinal levels; no significant difference was found among spinal level in flexion. There were significant differences between C2/3 and C4/5 (1,3) angles in extension and total ROM
Intervertebral translation
The intervertebral translations accounting 95% of our subjects studied during flexion and extension movements were summarized in Table 2. There were statistical differences among five spinal levels in anterior, posterior, and total translations (P < 0.001; P < 0.001; P < 0.001). The Tukey HSD tests showed the least anterior translation at C2/3 level, followed by C6/7, and C4/5 as well as C5/6 levels had the greatest translations during cervical flexion. The C6/7 level revealed the least posterior translation, followed by C2/3 level, while C4/5 level again had the greatest translations during cervical extension.
Table 2.
The mean values of the intervertebral translations with 95% confidence intervals at each spinal level during cervical flexion and extension
| Level | Mean (mm) | Standard deviation | Individual 95% confidence interval | Comparison between flexion and extension P value | ||
|---|---|---|---|---|---|---|
| Lower bound | Upper bound | |||||
| C2/3 Translation (1) | Anterior | 0.7 | 0.2 | 0.6 | 0.8 | 0.543 |
| Posterior | 0.7 | 0.2 | 0.6 | 0.8 | ||
| Total translation | 1.4 | 0.3 | 1.3 | 1.6 | ||
| C3/4 Translation (2) | Anterior | 1.0 | 0.3 | 0.9 | 1.1 | 0.037† |
| Posterior | 1.1 | 0.3 | 1.0 | 1.2 | ||
| Total translation | 2.1 | 0.5 | 1.8 | 2.3 | ||
| C4/5 Translation (3) | Anterior | 1.2 | 0.3 | 1.1 | 1.4 | 0.039† |
| Posterior | 1.3 | 0.4 | 1.1 | 1.4 | ||
| Total translation | 2.5 | 0.6 | 2.2 | 2.8 | ||
| C5/6 Translation (4) | Anterior | 1.1 | 0.3 | 1.0 | 1.2 | 0.005† |
| Posterior | 1.1 | 0.4 | 1.0 | 1.3 | ||
| Total translation | 2.2 | 0.6 | 2.0 | 2.5 | ||
| C6/7 Translation (5) | Anterior | 0.9 | 0.4 | 0.7 | 1.1 | 0.001† |
| Posterior | 0.4 | 0.7 | 0.1 | 0.7 | ||
| Total translation | 1.3 | 1.0 | 0.8 | 1.7 | ||
| Comparison among 5 spinal levels P value |
Anterior translation | <0.001* (1,2)(1,3)(1,4)(3,5) | ||||
| Posterior translation | <0.001* (1,3)(1,4)(2,5)(3,5)(4,5) | |||||
| Total translation | <0.001* (1,2)(1,3)(1,4)(2,5)(3,5)(4,5) | |||||
* P < 0.05 compared among spinal levels; There were significant differences between C2/3 & C3/4 (1,2), C2/3 & C4/5 (1,3), C2/3 & C5/6 (1,4), C3/4 & C6/7 (2,5), C4/5 & C6/7 (3,5), and C5/6 & C6/7 (4,5) in total translation during cervical motion
†P < 0.05 compared between flexion and extension within each level; There were significant differences between anterior and posterior translation within C3/4, C4/5, C5/6 and C6/7 levels during cervical flexion and extension
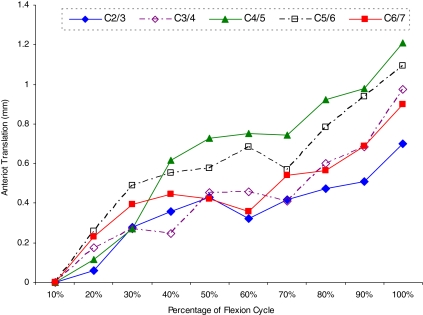
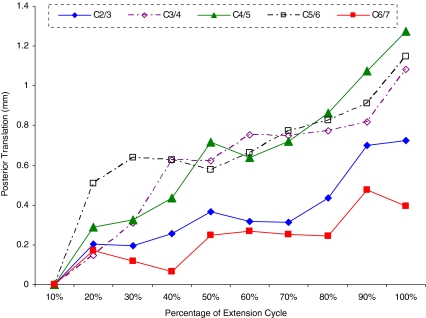
The significantly greater translations in the posterior direction during extension were detected for C3/4, C4/5, and C5/6 spinal levels in comparison with those during flexion. A significantly lesser range of posterior translation at C6/7 level was noted when compared to the anterior one. The stepwise linear patterns of the intervertebral translations at different points of cervical flexion and extension ROM are shown in Figs. 2 and 3.
Fig. 2.
The intervertebral translation showed the ascending patterns at each spinal level throughout the different percentages of cervical flexion range. The relative anterior translation was adjusted by the difference between two different points of cervical flexion
Fig. 3.
The intervertebral translation showed the ascending patterns at each spinal level throughout the different percentages of cervical extension range. The relative posterior translation was adjusted by the difference between two different points of cervical extension
Discussion
The cervical spine motion was commonly evaluated by means of plain radiographic methods. Since the number of radiographs obtained is limited by the radiation exposure, the assessment of dynamic intervertebral motion, especially for translation movements were usually ignored. This study utilized the videofluoroscopic technique to quantify the translation movements between intervertebral segments throughout the cervical flexion–extension movements and demonstrated the good reliabilities within and between raters.
Evaluation of errors and repeatability
Considering the reliability tests within raters in the present study, the high ICCs on identifying the vertebral landmarks in sequential videofluoroscopic images were in accordance with the thumb and finger results which averaged 0.967 and 0.940 [18, 35]. The average ICC values in marking videofluoroscopic images were reported to reach 0.880 and 0.920 in the lumbar and cervical spinal researches [20, 43]. The error of locating vertebral landmarks within raters was comparable to the findings of Harada et al. [10]. The standard deviation of digitizing was documented as 0.5 mm in the X and Y directions in their study while our corresponsive standard deviation valued only 0.3 mm. The small error for derived translations was also supported by the early publications [8, 32]. Forbin et al. summarized an approximately 0.7 mm standard deviation within rater in intervertebral translation corresponded to a vertebrae of 15 mm width on a radiographic method.
For the reliability tests between raters, though the mean ICC was slightly decreased with a larger MAD compared to the within rater ones, our results were still in agreement with the above-mentioned researches. In a recent videofluoroscopic study [32], a 16% error (2.4 mm) of the vertebral width (15 mm) in measuring the vertebral shear movement between raters appeared to be much greater than our results of 0.2 mm. One possible explanation for the discrepancies may be resulted from the selection of different vertebral landmarks in digitizing procedure. The anatomic symmetry in adopting the midpoints of vertebral bodies as reference points in present study may provide a better vertebral identification than using a single vertebral corner. Reitman et al. [32] have suggested that the measured displacements between vertebrae could be more reproducible by selecting the anterior- and posterior- midpoints of the vertebral bodies (as our experimental procedure) than by selecting only the anterior or posterior inferior corner between adjacent vertebrae.
Intervertebral angulation
In general, the angular ROM was least for C2/3 spinal level, whereas the greatest for C4/5 and C5/6 levels in flexion or extension. Our mean values and standard deviations of each intervertebral angulation and the trend of motion contribution among segments in cervical movement were consistent with previously published studies [Table 3]. The measurement errors of intervertebral angles were 1.6° and 1.9° within and between raters. The atypical orientation of the C2/3 facet joint which faced not only upwards and backwards but also medially by about 40° may be attributed to the significantly smaller angular motion in sagittal plane when compared to the relatively horizontal facets at other lower spinal levels [4]. On the other hand, one probable reason for the larger ROM in C4/5 and C5/6 levels may be associated to the larger disc height of these two spinal levels [9]. The disc heights had a proportionally linear relationship with the sagittal plane angle, and the anterior disc height increased with the increasing cervical extension angle [9]. Moreover, the loss of disc height was regarded as one sign of clinical vertebral degeneration and the restoration of disc height was documented to have a positive effect on ROM [14, 16, 30].
Table 3.
Historical comparison of reported mean values (standard deviation) of the intervertebral angulations and translations for cervical flexion and extension at each spinal level
| Intervertebral movement | C2/3 Level | C3/4 Level | C4/5 Level | C5/6 Level | C6/7 Level |
|---|---|---|---|---|---|
| Angulation (degrees) | |||||
| Bhalla and Simmons [3] | 9 (1) | 15 (2) | 23 (1) | 19 (1) | 18 (3) |
| Penning [28] | 12 | 18 | 20 | 20 | 15 |
| Dvorak et al. [7] | 12.0(3.0) | 17.2 (3.9) | 21.1 (3.5) | 22.6 (4.2) | 21.4 (3.7) |
| Panjabi et al. [27] | 6.2 (2.3) | 7.7 (5.0) | 10.1 (4.9) | 9.9 (4.8) | 7.1 (4.0) |
| Frobin et al. [8] | 8.4 (3.4) | 15.2 (4.7) | 17.0 (5.5) | 17.9 (6.6) | 11.4 (6.8) |
| Reitman et al. [32] | 9.9 (4) | 15.2 (3) | 16.9 (4) | 15.8 (4) | 13.5 (5) |
| Present study | 13.5 (4.8) | 17.3 (7.4) | 22.6 (7.9) | 19.1 (6.6) | 18.0 (9.1) |
| Translation (mm) | |||||
| Frobin et al. [8] | 1.00 | 1.72 | 1.89 | 1.21 | 0.30 |
| Reitman et al. [32] | 1.73 | 2.26 | 2.41 | 1.86 | 0.99 |
| Pickett et al. [30] | 1.56 | 2.16 | 2.45 | 2.05 | 1.14 |
| Present study | 1.4 (0.3) | 2.1 (0.5) | 2.5 (0.6) | 2.2 (0.6) | 1.3 (1.0) |
Intervertebral translation
The intervertebral motion was usually assessed either at the end range of movement [3, 7, 8, 28, 30–32] or with the fixed time frames of the spinal movements [10, 12, 25]. The drawbacks in previous studies were the absence of information regarding the dynamic motion sequences occurred throughout the ROM and the hardship in comparison between subjects due to the time dependent parameter. Since the definition of vertebral landmarks varied in individual studies, comparison with proposed findings would be more complicated. On the other hand, the spinal alignment was suggested to be determined by the George’s line in some occasion [4, 33, 40], yet the judgment on smoothness of this line measured from the posterior vertebral alignment throughout ROM was reported to be not precise for clinical interpretation of vertebral instability [22]. Therefore, the translation movements presented in the present study were the translations between adjacent vertebrae at the normalized 10 evenly-divided points of ROM. This method has been validated and would simultaneously illustrate the intervertebral motions in quality and quantity throughout ROM as presented in Figs. 2 and 3. In general, the stepwise linear patterns might help to explore the dynamic motion contribution between cervical segments at different points of ROM, though they were variable between subjects. Onan et al. [26] have proposed that the intact cervical segment permitted a maximum of 3.5 mm translation before the removal of surrounding ligaments and facet joints. The translation movement between vertebrae greater than 3.5 mm or 20% of the vertebral width was suggested to be an indicator of spinal instability or pathologies [27, 40]. The average measured total translation in the present study ranging from 1.3 mm to 2.5 mm appeared to be within the reasonable range of translation in cervical spine, however the intervertebral translation based on the single observation of a range of motion must be interpreted carefully. After adjusted for the normalized width of individual vertebrae, our results of translation percentages relative to the next adjacent vertebrae were 9.5, 13.7, 16.6, 15.0, and 8.6% from C2/3 to C6/7 levels, respectively. These findings were in agreement with the vertebral shear results of Reitman et al. [32]. Their average shear percentages relative to the adjacent vertebrae were 11.7, 15.1, 16.2, 11.7, and 6.2% from C2/3 to C6/7 levels, respectively. The segmental contributions of the translation movements in present study were also encouraged by the radiographic observations [8, 30] (Table 3).
Our results indicating the lesser translations occurred at C2/3 level during flexion and extension could be associated with the medically inclined and socket-like facets which nestled the inferior articular processes of the C2 [4]. The unique orientation and anatomic congruence of C2/3 articular surfaces may restrict the translation movement at C2/3 level. The C4/5 and C5/6 levels demonstrated the greater translations in either flexion or extension could be partially related to the higher discs as mentioned in the previous discussion. The reduced spinal stability resulted from the increased disc annulus and cortical stresses after spinal disruption or degeneration was also reported to be concentrated on C4/5 and C5/6 motion segments [23, 27]. Interestingly, there were significantly smaller amounts of posterior translation and consequent total translation at C6/7 level compared to those of other segments. White and Panjabi [40] identified that the cervical alignment affected the spinal motions, with the motion at one level sometimes occurring in a direction opposite to that at the adjacent level. The anterior translation movement at C6/7 level during cervical extension was occasionally observed in 18 subjects (18/56) in the present study. Bogduk and Mercer [4] proposed that the maximum ROM of a given cervical segment was not necessarily reflected by the full flexion or extension. The reverse motion may occur especially before reaching its final position. Similarly, the posterior translations at C6/7 spinal level displayed a relatively inconsistent trend on movement direction throughout ROM in Fig. 3. This scenario could be the reason accounting for the small average posterior translation at C6/7 level observed in the present study. The cervical spine motion was reported to be stepwise from the upper to lower levels with motion lags from maximum extension to maximum flexion in the study of Hino et al. [12]. However, the current results did not agree with this finding because the intervertebral translations took place at all cervical levels at the beginning of flexion or extension from the neutral position (Figs. 2, 3). Though the segmental translation was unevenly contributed by each spinal level, every segment did move with a different extent of translation at the first ten percentage of cervical motion which accounted 0.2–0.3 s from neutral position. The different starting positions of cervical movements and variations in habitual control of cervical motion could possibly attribute to the divergence in motion fashion.
The total amount of spinal translation was rarely investigated in the literature, and consequently the anterior and posterior translations during flexion and extension at each spinal level have never well explored. The anterior-posterior displacement described by the posterior aspects of adjacent vertebrae [32] or the anterior-posterior distraction calculated by disc height displacement [30] made the definition of vertebral translation equivocal and laborious for contrast. Generally, the linear descending and ascending patterns of the intervertebral translation at different spinal levels were observed in flexion and extension before the adjustment for initial offset. However, the relatively fluctuant translation fashions at different levels in cervical extension compared to flexion may imply a larger variation in cervical extension pattern among subjects. One possible reason could be that the extension movement facilitated the intervertebral joints into close-packed conditions allowing relative irregular articular glide among segments before reaching the end range of extension. Our results suggested that the significantly greater translations occurred in the posterior direction than the anterior one at C3/4, C4/5, and C5/6 levels. The segmental motions of cervical spine have been reported to be the angular rotation accompanied by the horizontal translation. The ratio between translation and rotation was suggested to be relatively stable across spinal segments [8]. The greater posterior translation and extension angle in present study were endorsed by the larger segmental angulation in cervical extension relative to flexion movement [24, 39]. The only exception was that a smaller average posterior translation at C6/7 level could possibly originate from the previously discussed variations in the direction of translation during cervical extension. To summarize, the intervertebral translations of cervical spine during flexion and extension were first described in quality and quantity based on the validated radiographic protocol. With the advantages of low radiation and real-time visualization of vertebral segments, the highly reliable videofluoroscopic technique is considered feasible in clinical and research applications. The quantitative analysis of the continuous intervertebral translations may be employed to diagnose translation abnormalities like hypomobility or hypermobility and to monitor the treatment effect on the cervical spines; however, our study focuses on a group of similar age asymptomatic male and female subjects.
Future researches expand the subject groups across different spinal problems and ages may reveal more complicated or even compensatory movements for the spinal impairment.
References
- 1.Axelsson P, Karlsson BS. Intervertebral mobility in the progressive degenerative process. A radiostereometric analysis. Eur Spine J. 2004;13:567–572. doi: 10.1007/s00586-004-0713-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bell GD. Skeletal applications of videofluoroscopy. J Manip Physiol Ther. 1991;14:390–392. [PubMed] [Google Scholar]
- 3.Bhalla SK, Simmons EH. Normal ranges of intervertebral joint motion of the cervical spine. Can J Surg. 1969;12:181–187. [PubMed] [Google Scholar]
- 4.Bogduk N, Mercer M. Biomechanics of the cervical spine I: normal kinematics. Clin Biomech. 2000;15:633–648. doi: 10.1016/S0268-0033(00)00034-6. [DOI] [PubMed] [Google Scholar]
- 5.Boyle JJW, Milne N, Singer KP. Influence of age on cervicothoracic spinal curvature: An ex vivo radiographic survey. Clin Biomech. 2002;17:361–367. doi: 10.1016/S0268-0033(02)00030-X. [DOI] [PubMed] [Google Scholar]
- 6.Descarreaux M, Blouin JS, Teasdale N. A non-invasive technique for measurement of cervical vertebral angle: report of a preliminary study. Eur Spine J. 2003;12:314–319. doi: 10.1007/s00586-002-0511-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dvorak J, Froehlich D, Penning L, Baumgartner H, Panjabi MM. Functional radiographic diagnosis of the cervical spine: flexion/extension. Spine. 1998;13:748–755. doi: 10.1097/00007632-198807000-00007. [DOI] [PubMed] [Google Scholar]
- 8.Frobin W, Leivseth G, Biggemann M, Brinckmann P. Sagittal plane segmental motion of the cervical spine: a new precision measurement protocol and normal motion data of healthy adults. Clin Biomech. 2002;17:21–31. doi: 10.1016/S0268-0033(01)00105-X. [DOI] [PubMed] [Google Scholar]
- 9.Frobin W, Leivseth G, Biggemann M, Brinckmann P. Vertebral height, disc height, posteroanterior displacement and dens-atlas gap in the cervical spine: precision measurement protocol and normal data. Clin Biomech. 2002;17:423–431. doi: 10.1016/S0268-0033(02)00044-X. [DOI] [PubMed] [Google Scholar]
- 10.Harada M, Abumi K, Ito M, Kaneda K. Cineradiographic motion analysis of normal lumbar spine during forward and backward flexion. Spine. 2000;25:1932–1937. doi: 10.1097/00007632-200008010-00011. [DOI] [PubMed] [Google Scholar]
- 11.Harvey SB, Hukins DWL. Measurement of lumbar spinal flexion–extension kinematics from lateral radiographs: simulation of the effects of out-of-plane movement and errors in reference point placement. Med Eng Phys. 1998;20:403–409. doi: 10.1016/S1350-4533(98)00052-6. [DOI] [PubMed] [Google Scholar]
- 12.Hino H, Abumi K, Kanayama M, Kaneda K. Dynamic motion analysis of normal and unstable cervical spines using cineradiography: an in vivo study. Spine. 1999;24:163–168. doi: 10.1097/00007632-199901150-00018. [DOI] [PubMed] [Google Scholar]
- 13.Houck J, Yack HJ, Mulhausen P. Neck mobility: the influence of age and a history of neck pain. Gait Posture. 1997;5:184. doi: 10.1016/S0966-6362(97)83433-9. [DOI] [Google Scholar]
- 14.Huang RC, Tropiano P, Marnay T, Girardi FP, Lim MR, Cammisa FP. Range of motion and adjacent level degeneration after lumbar total disc replacement. Spine J. 2006;6:242–247. doi: 10.1016/j.spinee.2005.04.013. [DOI] [PubMed] [Google Scholar]
- 15.Koerhuis CL, Winters JC, Helm FCT, Hof AL. Neck mobility measurement by means of the ‘Flock of Birds’ electromagnetic tracking system. Clin Biomech. 2003;18:14–18. doi: 10.1016/S0268-0033(02)00146-8. [DOI] [PubMed] [Google Scholar]
- 16.Kolstad F, Myhr G, Kvistad KA, Nygaard OP, Leivseth G. Degeneration and height of cervical discs classified from MRI compared with precise height measurements from radiographs. Eur J Radiol. 2005;55:415–420. doi: 10.1016/j.ejrad.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 17.Kristjansson E, Jonsson H. Is the sagittal configuration of the cervical spine changed in women with chronic whiplash syndrome? A comparative computer-assisted radiographic assessment. J Manip Physiol Ther. 2002;25:550–555. doi: 10.1067/mmt.2002.128371. [DOI] [PubMed] [Google Scholar]
- 18.Kuo LC, Su FC, Chiu HY, Yu CY. Feasibility of using a video-based motion analysis system for measuring thumb kinematics. J Biomech. 2002;35:1499–1506. doi: 10.1016/S0021-9290(02)00083-0. [DOI] [PubMed] [Google Scholar]
- 19.Lantz CA, Chen J, Buch D. Clinical validity and stability of active and passive cervical range of motion with regard to total and unilateral uniplanar motion. Spine. 1999;24:1082–1089. doi: 10.1097/00007632-199906010-00007. [DOI] [PubMed] [Google Scholar]
- 20.Lee SW, Wong KWN, Chan MK, Yeung HM, Chiu JLF, Leong JCY. Development and validation of a new technique for assessing lumbar spine motion. Spine. 2002;27:E215–E220. doi: 10.1097/00007632-200204150-00022. [DOI] [PubMed] [Google Scholar]
- 21.McAviney J, Schulz D, Bock R, Harrison DE, Holland B. Determining the relationship between cervical lordosis and neck complaints. J Manip Physiol Ther. 2005;28:187–193. doi: 10.1016/j.jmpt.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 22.Muggleton JM, Allen R. Insights into the measurement of vertebral translation in the sagittal plane. Med Eng Phys. 1998;20:21–32. doi: 10.1016/S1350-4533(97)00045-3. [DOI] [PubMed] [Google Scholar]
- 23.Ng HW, Teo EC, Zhang QH. Biomechanical effects of C2–C7 intersegmental stability due to laminectomy with unilateral and bilateral facetectomy. Spine. 2004;29:1737–1745. doi: 10.1097/01.BRS.0000134574.36487.EB. [DOI] [PubMed] [Google Scholar]
- 24.Nyland J, Johnson D. Collegiate foot ball palters display more active servical spine mobility than high school football players. J Athl Training. 2004;39:146–150. [PMC free article] [PubMed] [Google Scholar]
- 25.Okawa A, Shinomiya K, Komori H, Muneta T, Arai Y, Nakai O. Dynamic motion study of the whole lumbar spine by videofluoroscopy. Spine. 1998;23:1743–1749. doi: 10.1097/00007632-199808150-00007. [DOI] [PubMed] [Google Scholar]
- 26.Onan OA, Heggeness MH, Hipp JA. A motion analysis of the cervical facet joint. Spine. 1998;23:430–439. doi: 10.1097/00007632-199802150-00005. [DOI] [PubMed] [Google Scholar]
- 27.Panjabi MM, White AA, John RM. Cervical spine mechanics as function of transaction of components. J Biomech. 1975;8:327–336. doi: 10.1016/0021-9290(75)90085-8. [DOI] [PubMed] [Google Scholar]
- 28.Penning L. Normal movements of the cervical spine. Am J Roentgenol. 1978;130:317–326. doi: 10.2214/ajr.130.2.317. [DOI] [PubMed] [Google Scholar]
- 29.Pfeiffer M, Geisel T. Analysis of a computer-assisted technique for measuring the lumbar spine on radiographs: Correlation of two methods. Acad Radiol. 2003;10:275–282. doi: 10.1016/S1076-6332(03)80101-0. [DOI] [PubMed] [Google Scholar]
- 30.Pickett GE, Rouleau JP, Duggal N. Kinematic analysis of the cervical spine following implantation of an artificial cervical disc. Spine. 2005;30:1949–1954. doi: 10.1097/01.brs.0000176320.82079.ce. [DOI] [PubMed] [Google Scholar]
- 31.Reitman CA, Hipp JA, Nguyen L, Esses SI. Change in segmental intervertebral motion adjacent to cervical arthrodesis: A prospective study. Spine. 2004;29:E221–E226. doi: 10.1097/00007632-200406010-00022. [DOI] [PubMed] [Google Scholar]
- 32.Reitman CA, Mauro KM, Nguyen L, Ziegler JM, Hipp JA. Intervertebral motion between flexion and extension in asymptomatic individuals. Spine. 2004;29:2832–2843. doi: 10.1097/01.brs.0000147740.69525.58. [DOI] [PubMed] [Google Scholar]
- 33.Roche CJ, Eyes BE, Whitehouse GH. The rheumatoid cervical spine: signs of instability on plain cervical radiographs. Clin Radiol. 2002;57:241–249. doi: 10.1053/crad.2001.0745. [DOI] [PubMed] [Google Scholar]
- 34.Sforza C, Grassi G, Fragnito N, Turci M, Ferrario VF. Three-dimensional analysis of active head and cervical spine range of motion: effect of age in healthy male subjects. Clin Biomech. 2002;17:611–614. doi: 10.1016/S0268-0033(02)00071-2. [DOI] [PubMed] [Google Scholar]
- 35.Su FC, Kuo LC, Chiu HY, Hsu HY. The validity of using a video-based motion analysis system measuring maximal area of fingertip motion and angular variation. Proc Instn Mech Eng [H] 2002;216:257–263. doi: 10.1243/09544110260138745. [DOI] [PubMed] [Google Scholar]
- 36.Tousignant M, Boucher N, Bourbonnais J, Gravelle T, Quesnel M, Brosseau L. Intratester and intertester reliability of the Cybex electronic digital inclinometer (EDI-320) for measurement of active neck flexion and extension in healthy subjects. Manual Ther. 2001;6:235–241. doi: 10.1054/math.2001.0419. [DOI] [PubMed] [Google Scholar]
- 37.Trott PH, Pearcy MJ, Ruston SA, Fulton I, Brien C. Three-dimensional analysis of active cervical motion: the effect of age and gender. Clin Biomech. 1996;11:201–206. doi: 10.1016/0268-0033(95)00072-0. [DOI] [PubMed] [Google Scholar]
- 38.Tsai KH, Chang GL, Lin HT, Kuo DC, Chang LT, Lin RM. Differences of lumbosacral kinematics between degenerative and induced spondylolisthetic spine. Clin Biomech. 2003;18:S10–S16. doi: 10.1016/S0268-0033(03)00079-2. [DOI] [PubMed] [Google Scholar]
- 39.Wang SF, Teng CC, Lin KH. Measurement of cervical range of motion pattern during cyclic neck movement by an ultrasound-based motion system. Manual Ther. 2005;10:68–72. doi: 10.1016/j.math.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 40.Whit AA, Panjabi MM. Clinical biomechanics of the spine. 2nd. Philadelphia: Lippincott; 1990. [Google Scholar]
- 41.Wolfenberger VA, Batenchuk GB. A comparison of methods of evaluating cervical range of motion. J Manip Physiol Ther. 2002;25:154–160. doi: 10.1067/mmt.2002.122327. [DOI] [PubMed] [Google Scholar]
- 42.Wong KWN, Leong JCY, Chan MK, Luk KDK, Lu WW. The flexion–extension Profile of lumbar spine in 100 healthy volunteers. Spine. 2004;29:1636–1641. doi: 10.1097/01.BRS.0000132320.39297.6C. [DOI] [PubMed] [Google Scholar]
- 43.Wu SK, Lan HC, Kuo LC, Tsai SW, Chen CL, Su FC (2006) The feasibility of a video-based motion analysis system in measuring the segmental movements between upper and lower cervical spine. Gait Posture (in press) [DOI] [PubMed]