Abstract
With the advent of segmental pedicle screw fixation that enables more powerful corrective forces, it is postulated that an additional anterior procedure may be unnecessary even in severe deformities. The purpose of this paper is to evaluate the results of a posterior procedure alone using segmental pedicle screw fixation in severe scoliotic curves over 70°. Thirty-five scoliosis patients treated by pedicle screw fixation and rod derotation were retrospectively analyzed after a minimum follow-up of 2 years (range 2–10.4). The mean age of patients was 15.3 years (range 9.8–34.2). Diagnoses were idiopathic scoliosis in 29, neuromuscular scoliosis in 3 and scoliosis associated with Marfan syndrome in 3. Scoliosis consisted of single thoracic curve in 18, double thoracic in 5 and double major in 12. Twenty-five patients showed a major thoracic curve greater than 70° (range 70–100), and different ten patients showed a major lumbar curve greater than 70° (range 70–105), pre-operatively. The deformity angle, lowest instrumented vertebral tilt (LIVT) and spinal balance were measured. Pre-operatively there were nine patients with coronal decompensation. The pre-operative thoracic curve of 80 ± 9° with the flexibility of 45 ± 11% (45 ± 11° in side-bending film) was corrected to 27 ± 10° at the most recent follow-up, showing a correction of 66% (53°) and loss of correction of 3.0% (3.7°). The pre-operative lumbar curve of 79 ± 12° with the flexibility of 62 ± 14% (30 ± 11° in side-bending film) was corrected to 33 ± 14° at the most recent follow-up [59% (46°) curve correction, 3.5% (3.0°) loss of curve correction]. The pre-operative LIVT of 30 ± 8° was corrected to 11 ± 6°, showing a correction of 62% (19°). Residual coronal decompensation was observed in three patients postoperatively. Pre-operative thoracic kyphosis of 27° (range 0–82) improved postoperatively to 31° (range 14–53). In conclusion, posterior segmental pedicle screw fixation without anterior release in severe scoliosis had satisfactory deformity correction without significant loss of curve correction. In this series a posterior procedure alone obviated the need for the anterior release and avoided complications related anterior surgery.
Keywords: Severe scoliosis, Posterior correction, Pedicle screw, Segmental fixation
Introduction
The surgical correction of scoliosis has improved with the development of spinal instrument. With the introduction of Harrington instrumentation, and subsequently Luque and Cotrel–Dubousset instrumentation, posterior approaches have been commonly used for the treatment of scoliosis. However scoliosis correction in severe curves frequently necessitates combined anterior release and posterior instrumentation to achieve a satisfactory result. Anterior procedures in patients with severe curves are not ideal as these patients often have the cardiopulmonary limitations.
Spinal pedicle screws, first introduced by Boucher [1] in the 1950s and popularized by Roy-Camillle et al. [15, 16] in the 1960s, are a penetrating type of anchor that makes use of the pedicle, the hardest part of the vertebrae. From a position within the pedicle, this strong anchor resists all directions of force and offers improved three-dimensional correction of deformity and rigid fixation [17, 18]. Segmental pedicle screw fixation, dispersing the stress by allowing multiple anchors per spinal level and thus, dispersal of the stress on each implant, provides spine surgeons with more powerful correction forces.
Since the first author applied thoracic pedicle screws for the scoliosis treatment in late 1980s, the application is gradually increased among spine surgeons and it is postulated that an additional anterior release may be unnecessary even in severe scoliosis. The results of a posterior procedure alone with segmental pedicle screw fixation in severe scoliosis over 70° were evaluated to test this hypothesis and suggest the severity and flexibility of scoliosis able to be treated by this procedure.
Materials and methods
Thirty-five scoliosis patients with major curves ≥70° who had been surgically treated by segmental pedicle screw fixation and rod derotation through a posterior alone approach were retrospectively analyzed after a minimum of 2 years (range 2–10.4) postoperative follow-up. The average age of patients at surgery was 15.3 years (range 9.8–34.2) and the female/male ratio was 27:8. Etiologic diagnoses were idiopathic scoliosis in 29, neuromuscular scoliosis in 3 and scoliosis associated with Marfan syndrome in 3. The curve types consisted of a single thoracic curve in 18, double thoracic in 5 and double major in 12. According to the King–Moe classification [7], the number of patients in the idiopathic scoliosis was as follows: 8 for Type I, 7 for Type II, 8 for Type III, 1 for Type IV, and 5 for Type V. Using the Lenke et al. classification [9], the number of patients in the idiopathic scoliosis was as follows: 16 for Type 1, 5 for Type 2, and 8 for Type 6. Twenty-five patients had the major curve ≥70° in thoracic area (range 70–100°) and different ten patients had the major curve ≥70° in lumbar area (range 70–105°). The posteroanterior (PA) and lateral standing radiographs were used to check for deformity correction, lowest instrumented vertebral tilting (LIVT), coronal and sagittal balance, and pseudarthrosis. These parameters were measured on the pre-operative, immediate postoperative (within 1 month) and the latest postoperative radiographs. The coronal balance was measured as the distance between the C7 plumb line and a perpendicular line drawn from the center of the S1 (center sacral vertical line). A measurement of more than 2 cm was considered as coronal decompensation. The sagittal balance was measured as the shortest distance between the C7 plumb line and the posterior superior corner of S1 body. Curve flexibility, determined on the pre-operative supine side-bending films, was expressed as the percentages of correction compared with the pre-operative standing film. The diagnosis of pseudarthrosis was made if the patient had more than two of the following clinical or radiographic criteria more than 6 months after surgery. (1) Breakage or dislodgement of rods or screws; (2) Back-out or halo sign of screws; (3) Progression of deformity clinically or radiologically; (4) increasing angulation ≥5° of a disc space; (5) Any motion on side-bending or flexion/extension radiographs.
Surgical techniques
All surgeries were carried out by the first author using the techniques described below. The pre-operative end vertebrae of curves were determined by the Cobb method. A single thoracic curve in idiopathic (n = 16) and Marfan (n = 2) scoliosis was treated with single thoracic fusion, extending usually from one vertebra above the upper end vertebra to one vertebra below the lower end vertebra. Double thoracic curve (n = 5) was treated with both thoracic fusion, extending from T1 (n = 3) or T2 (n = 2) to one vertebra below the lower end vertebra of lower thoracic curve. Distal fusion levels in single and double thoracic curve were T11 (n = 1), T12 (n = 6), L1 (n=8), L2 (n = 7), and L3 (n = 1). Double major curve in idiopathic (n = 8), Marfan (n = 1), and neuromuscular scoliosis (n = 3) was treated with fusion of both thoracic and lumbar curve, extending from one vertebra above the upper end vertebra of thoracic curve to L3 (n = 8), L4 (n = 1) or S1 (n = 3). Fusion level was extended if there was the kyphosis at thoracolumbar junction. The surgical incision spanned from the upper end of the spinous process two levels above the uppermost instrumented vertebra to the lower end of the lamina of the lowest instrumented vertebra. The proximal incision was large enough to allow the pedicle screw of the uppermost instrumented vertebra to be inserted with convergence. After the posterior exposure, facets were destroyed to promote intra-articular fusion. Then guide pins were inserted shallowly at the presumed pedicle entry point. The presumed pedicle entry point of the lower thoracic and lumbar spine is at the junction of the bisected transverse process and lateral margin of the facet joint and that of the upper thoracic spine is at the junction of superior margin of the transverse process and lateral aspect to mid-portion of facet joint. With intraoperative PA and lateral radiographs, the ideal entry point (IEP) and the direction of screws were determined. The IEP in a neutrally rotated vertebra is at the junction of the transverse line and the lateral margin of pedicle ring shadow and the ideal direction is parallel to the vertebral endplates. In a rotated vertebra, the IEP of the concave side (where the pedicle is disappearing or has disappeared) moves more laterally while that of opposite side moves medially with increasing amounts of vertebral rotation. PA radiograph usually gives information about the IEP and convergence/diversion of screw and lateral radiograph determines the direction of screws and vice versa in severe rotated vertebra. If concave pedicles in vertebra with severe rotation could not be seen on any radiographs, the position of them should be inferred from other anatomical landmarks, such as rib, transverse process, margin of vertebral body, and convex pedicle by making use of pre-operative bending radiograph, CT or MRI. Calculating the distance between the guide pin at the presumed entry point and the IEP on the radiograph, the IEP in the surgical field could be found. At this IEP, the pedicle was entered with an awl or a small-diameter drill, checked with a blunt-ended probe, and then pedicle screws were inserted. Pedicle screws were inserted segmentally on the correction side (concave side of the thoracic curve and convex side of the lumbar curve) and every other or every third vertebra on the supporting side (convex side of the thoracic curve and concave of the lumbar curve). Following screw insertion, a rigid rod, contoured to a more exaggerated curve than the normal sagittal contour, was inserted on the correction side. Correction of the curve was then performed by rod derotation. If the rod was severely bent out during rod derotation, it was extracted. Then, the removed rod or another new rod was recontoured, inserted, and derotated. This procedure could be required several times for the better deformity correction. In the double thoracic and double major curves treated with double curve fusion, it could be difficult to put one rod into the correction side. In that time, two rods were separately inserted on the correction side of each curve. They were connected by a longitudinal connector after curve correction. After locking the rod(s) of the correction side in a corrected position, the other rod, contoured to the corrected alignment of the spine, was placed on the supporting side and locked in situ. Neither compression nor distraction was used for correction. Two rods were connected by transverse connectors at both ends of the construct. Subsequently, the posterior fusion was performed. All patients ambulated on the third postoperative day and were protected by a custom made throacolumbosacral orthosis for 3 months.
Results
Deformity correction
In 25 patients (18 single thoracic, five double thoracic, and two double major curves) with the major thoracic curve ≥70°, the pre-operative thoracic curve was 79.6° ± 9.3° with a flexibility of 44.5 ± 10.5% (44.5 ± 11.3° in side-bending film). The thoracic deformity was corrected to 24.1 ± 9.8° resulting in 70.0% (56.6°) immediate postoperative correction compared with the pre-operative values and 26.8 ± 9.5° or 66.4% (52.8°) correction at the most recent follow-up. There was 3.0% (3.7°) loss of curve correction during postoperative follow-up. The immediate postoperative Cobb angle of the major thoracic curve had a negative correlation with flexibility (Spearman’s rank correlation; ρ = −0.40, P < 0.05). The pre-operative lumbar curve was 42.9 ± 11.5° with a flexibility of 87.1 ± 19.5% (6.7 ± 8.8° in side-bending film). The lumbar deformity was corrected to 13.9 ± 10.6° demonstrating 69.5% (29.5°) immediate postoperative correction and 16.0 ± 11.3° or 65.2% (26.9°) correction at the most recent follow-up. There was 3.3% (2.6°) loss of curve correction during postoperative follow-up (Table 1). In five patients treated with double thoracic fusion, the pre-operative upper thoracic curve was 50.2 ± 9.7° with a flexibility of 31.9 ± 8.5% (34.6 ± 10.3° in side-bending film). The deformity was corrected to 23.8 ± 2.8° demonstrating 51.2% (26.4°) immediate postoperative correction and 25.2 ± 3.5° [48.5% (25.0°) correction, 2.7% (1.4°) loss of curve correction] at the most recent follow-up (Fig. 1).
Table 1.
Coronal deformity of patients with major thoracic curve (n = 25)
| Thoracic curve | Lumbar curve | |
|---|---|---|
| Pre-operative | ||
| Cobb angle in standing (°) | 79.6 ± 9.3 (70–100) | 42.7 ± 11.5 (24–90) |
| Cobb angle in bending (°) | 44.5 ± 11.3 (24–69) | 6.7 ± 8.8 (−9 to 22) |
| Flexibility (%) | 44.5 ± 10.5 (24.0–65.7) | 87.1 ± 19.5 (54.3–137.5) |
| IMPO (°) | 24.1 ± 9.8 (10–62) | 13.9 ± 10.6 (1–48) |
| IM correction | 70.0% (56.5°) | 69.5% (29.5°) |
| Final follow-up (°) | 26.8 ± 9.5 (13–64) | 16.0 ± 11.3 (0–51) |
| Final correction | 66.4% (52.8°) | 65.2% (26.9°) |
| LOC | 3.0% (3.7°) | 3.3% (2.6°) |
IMPO immediate postoperative, IM correction immediate postoperative correction rate, Final correction correction rate at the final follow-up, LOC loss of correction during the follow-up after operation
Fig. 1.
A 12.4-year-old girl with double thoracic curve. a Pre-operative anteroposterior radiograph showed 45° proximal thoracic, 92° main thoracic, and 50° lumbar scoliosis. b Pre-operative lateral radiograph. c Anteroposterior radiograph taken 1 month after surgery with segmental pedicle screw fixation from T1 to L3. The proximal thoracic curve was corrected to 23°, main thoracic curve to 20°, and lumbar curve to 6°. d Lateral radiograph taken 1 month after surgery. e, f Anteroposterior and lateral radiographs taken 3.9 years after surgery. Coronal and Sagittal alignments were well-maintained during the follow-up
In ten patients (ten double major) with the major lumbar curve ≥70°, the pre-operative lumbar curve was 78.6 ± 11.5° with a flexibility of 62.0 ± 14.1% (29.7 ± 10.9° in side-bending film). The deformity was corrected to 29.7 ± 11.5° demonstrating 61.9% (48.9°) immediate postoperative correction and 32.7 ± 13.9° or 58.5% (45.9°) correction at the most recent follow-up. There was 3.5% (3.0°) loss of curve correction during postoperative follow-up. The immediate postoperative Cobb angle of the major lumbar curve had a negative correlation with flexibility (Spearman’s rank correlation; ρ = −0.81, P < 0.05). The pre-operative thoracic curve was 65.8 ± 12.8° with a flexibility of 50.3 ± 18.8% (34.3 ± 17.8° in side-bending film). The thoracic deformity was corrected to 24.8 ± 16.6° demonstrating 64.4% (41.0°) immediate postoperative correction and 25.9 ± 17.7° or 62.7% (39.9°) correction at the most recent follow-up. There was 1.7% (1.1°) loss of curve correction during postoperative follow-up (Table 2, Fig. 2).
Table 2.
Coronal deformity of patients with major lumbar curve (n = 10)
| Thoracic curve | Lumbar curve | |
|---|---|---|
| Pre-operative | ||
| Cobb angle in standing (°) | 65.8 ± 12.8 (50–95) | 78.6 ± 11.5 (70–105) |
| Cobb angle in bending (°) | 34.3 ± 17.8 (2–72) | 29.7 ± 10.9 (14–47) |
| Flexibility (%) | 50.3 ± 18.8 (24.2–96.0) | 62.0 ± 14.1 (37.3–80.6) |
| IMPO (°) | 24.8 ± 16.6 (8–63) | 29.7 ± 11.5 (6–40) |
| IM correction | 64.4% (41.0°) | 61.9% (48.9°) |
| Final follow-up (°) | 25.9 ± 17.7 (9–70) | 32.7 ± 13.9 (7–57) |
| Final correction | 62.7% (39.9°) | 58.5% (45.9°) |
| LOC | 1.7% (1.1°) | 3.5% (3.0°) |
IMPO immediate postoperative, IM correction immediate postoperative correction rate, Final correction correction rate at the final follow-up, LOC loss of correction during the follow-up after operation
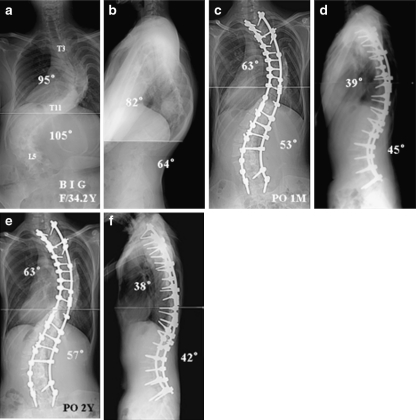
Fig. 2.
A 34.2-year-old girl with double major curve related to Marfan syndrome. a Pre-operative anteroposterior radiograph showed 95° thoracic and 105° lumbar scoliosis. b Pre-operative lateral radiograph. c Anteroposterior radiograph taken 1 month after surgery with segmental pedicle screw fixation from T2 to S1. The thoracic curve was corrected to 63° and lumbar curve to 53°. d Lateral radiograph taken 1 month after surgery. e, f Anteroposterior and lateral radiographs taken 2 years after surgery. Coronal and Sagittal alignments were well-maintained during the follow-up
In a separate analysis of 35 major curves, the pre-operative major curve was 79.3 ± 9.8° (70–105°) with a flexibility of 49.7 ± 14.0% (24.0–80.6%). The deformity was corrected to 25.7 ± 10.5° demonstrating 67.6% (54.3°) immediate postoperative correction and 28.5 ± 11.0° or 64.2% (50.8°) correction at the most recent follow-up. There was 3.1% (3.5°) loss of curve correction during postoperative follow-up.
The pre-operative thoracic kyphosis (T5–T12) and lumbar lordosis (T12–S1) of 27.1 ± 16.2° and 45.9 ± 13.8°, respectively, measured 29.2 ± 11.6° and 42.9 ± 11.7° at immediate postoperative follow-up and 31.0 ± 10.3° and 46.1 ± 10.0° at the most recent follow-up (Table 3). In 30 patients with the pre-operative thoracic kyphosis <40°, thoracic kyphosis was corrected from 22.3 ± 10.3° to 29.2 ± 9.6° at the most recent follow-up with statistically significant difference (P = 0.0001). In five patients with the pre-operative thoracic kyphosis >40°, thoracic kyphosis was changed from 55.6 ± 16.3° to 42.0 ± 7.6° at the most recent follow-up without significant difference (P > 0.05).
Table 3.
Other curve characteristics
| Pre-operative | Final follow-up | Final corr | |
|---|---|---|---|
| T-kyphosis (°) | 27.1 ± 16.2 (0–82) | 31.0 ± 10.3 (14–53) | |
| L-lordosis (°) | 45.9 ± 13.8 (13–72) | 46.1 ± 10.0 (25–70) | |
| Balance (mm) | |||
| Coronal | 14.6 ± 12.8 (2–61) | 8.1 ± 6.8 (0–24) | |
| Sagittal | 20.0 ± 16.5 (0–62) | 16.1 ± 12.8 (0–49) | |
| IVT (°) | |||
| Uppermost IVT | 23.0 ± 7.9 (4–40) | 12.0 ± 6.3 (2–26) | 46.8% |
| Lowest IVT | 30.1 ± 8.2 (8–51) | 10.7 ± 5.8 (0–27) | 61.6% |
Final corr correction rate of the final follow-up, IVT instrumented vertebral tilting
There was no significant difference between the pre-operative and postoperative lumbar lordosis (P > 0.05).
Spinal balance
Before surgery, the coronal balance was 14.6 ± 12.8 mm with nine patients demonstrating coronal decompension. At the most recent follow-up, the coronal balance was 8.1 ± 6.8 mm with residual coronal decompensation observed in three patients. The pre-operative sagittal balance of 20.0 ± 16.5 mm was improved to 16.1 ± 12.8 mm at the most recent follow-up (Table 3).
Other measurements and complications
The pre-operative uppermost IVT (UIVT) of 23.0 ± 7.9° was corrected to 12.0 ± 6.3° at the most recent follow-up, demonstrating 46.8% correction. The pre-operative LIVT of 30.1 ± 8.2 was corrected to 10.7 ± 5.8 at the most recent follow-up, demonstrating 61.6% correction (Table 3).
The average fusion length was 10.9 ± 2.4 segments (7–17 segments) and the average operation time was 246 ± 54 min (130–400 min). The average number of pedicle screws utilized was 17.3 ± 3.8 (12–26). There was no screw-related complication except in one patient who had a leakage of cerebrospinal fluid (CSF) detected postoperatively. This patient developed a deep wound infection in 2 weeks after surgery and managed with debridement and delayed repair. However her instrumentation was removed at 15 months after surgery because of recurrent infection. This patient was considered to have a pseudarthrosis.
As no anterior surgery was performed, there was no complication related anterior surgery, such as respiratory, cardiac, vascular, and visceral complication.
Discussion
Severe scoliosis results in a complex three-dimensional spinal deformity that often requires correction in multiple planes. Posterior instrumentation techniques using Harrington, Luque or Cotrel–Dubousset instrumentation are suboptimal for a three-dimentional deformity correction. Pedicle screws, using the strongest part as an anchor, provide the spine surgeon with an enhanced three-dimensional deformity correction and preservation of motion segments. Several reports [4, 6, 10, 11, 17, 18] have demonstrated the superiority of pedicle screws over other posterior instrument systems. Posterior correction with pedicle screws is widely used for the treatment of the scoliosis. However, an additional anterior release and fusion followed by posterior instrumentation has been utilized for the treatment of the severe scoliosis [2, 3, 8, 12, 14]. Anterior release is usually used to improve curve flexibility by removing intervertebral discs around the apex. Lenke [8] reported that anterior endoscopic release and fusion procedures followed by a posterior instrumentation in the treatment of AIS had an average pre-operative curve of 82° (range 41–125°) with postoperative correction of 70% to 28° (range 5–60°). Newton et al. [13] reported 112 pediatric spinal deformity cases of thoracic anterior release combined with posterior instrumentation. The average pre-operative scoliosis of 80° was improved to 31° with 67% correction in idiopathic scoliosis and 52% correction in neuromuscular scoliosis. However 14% of patients had perioperative respiratory complications related to anterior surgery. Neither Lenke’s nor Newton’s study noted the type of posterior instrument used. In our series of 35 severe scoliosis treated with posterior segmental pedicle screw fixation without anterior release, the average pre-operative scoliosis of 79° was corrected to 28° (65%) at latest follow-up. In the absence of an anterior procedure, there were no complications related to anterior surgery, and respiratory, cardiac, and vascular complications were avoided. The radiographic results were comparable to other studies using anterior release combined with posterior instrumentation.
The LIVT correction of 62% with pedicle screw in this study was superior to that of about 50% with hook instrumentation reported by other authors [5, 10]. Pedicle screw offers a better horizontalization of the LIV for two reasons; first, the more lateral position of the pedicle screw compared to a hook provides a better leverage; second, the tangential fixation strength of a pedicle screw is greater than that of a hook.
In our study, there was no crankshaft phenomenon during the follow-up. Segmental pedicle screw fixation can control three column of the spine because screw reaches vertebral body through pedicle. It has been suggested that this control prevent crankshaft phenomenon.
Pedicle screws placed in the vertebral body have a 30% greater moment arm for applying corrective forces than posterior hooks. Posterior segmental instrumentation with a powerful pedicle screw anchor offers satisfactory correction without significant loss of curve correction even in severe deformity. In our study, the patients had the average pre-operative Cobb major angle of 79° (range 70–105°) with the flexibility ranging from 24 to 81%. There was no case with the flexibility ≤20%. It is concluded that severe curves of 70–105° Cobb angle with the flexibility ≥25% can be treated by posterior segmental pedicle screw fixation and correction without anterior release. However, more rigid and severer curves than these criteria, i.e., curves ≥110° with the flexibility ≤20%, can require additional anterior release/arthrodesis or other posterior techniques, such as decancellation and vertebral resection, for the satisfactory correction of deformity. This indication will be extended with improved posterior spinal instrumentation and new surgical techniques in the future.
Conclusion
Posterior segmental pedicle screw fixation without anterior release in severe scoliosis had satisfactory deformity correction without a significant correction loss. This technique can eliminate the need for the anterior release, with the associated complications related anterior surgery, in the treatment of severe scoliosis.
References
- 1.Boucher HH (1559) A method of spinal fusion. J Bone Joint Surg 41-B:248–259 [DOI] [PubMed]
- 2.Bridwell KH. Surgical treatment of idiopathic adolescent scoliosis. Spine. 1999;24:2607–2616. doi: 10.1097/00007632-199912150-00008. [DOI] [PubMed] [Google Scholar]
- 3.Gorgi G, Stella G, Becchetti S, Martucci G, Miscoscia D. Cotrel-Dubousset instrumentation for the treatment of severe scoliosis. Eur Spine J. 1999;8:8–15. doi: 10.1007/s005860050120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delorme S, Labelle H, Aubin C, et al. Intraoperative comparision of two instrumentation techniques for the correction of adolescent idiopathic scoliosis. Spine. 1999;24:2011–2018. doi: 10.1097/00007632-199910010-00009. [DOI] [PubMed] [Google Scholar]
- 5.Hamil CL, Lenke LG, Bridwell KH, Chapman MP, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis. Spine. 1996;21:1241–1249. doi: 10.1097/00007632-199605150-00020. [DOI] [PubMed] [Google Scholar]
- 6.Kim YJ, Lenke LG, Cho SK, Bridwell KL, Sides B, Blanke K. Comparative analysis of pedicle screw versus hook instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine. 2004;29:2040–2048. doi: 10.1097/01.brs.0000138268.12324.1a. [DOI] [PubMed] [Google Scholar]
- 7.King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg. 1983;65-A:1302–1313. [PubMed] [Google Scholar]
- 8.Lenke LG. Anterior endoscopic discectomy and fusion for adolescent idiopathic scoliosis. Spine. 2003;28:S36–S43. doi: 10.1097/00007632-200308011-00007. [DOI] [PubMed] [Google Scholar]
- 9.Lenke LG, Betz RR, Harms J, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg. 2001;83-A:1169–1181. [PubMed] [Google Scholar]
- 10.Liljenqvist U, Lepsien U, Hackenberg L, Niemeyer T, Halm H. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336–343. doi: 10.1007/s00586-002-0415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 12.Luhmann S, Lenke LG, Kim YJ, Bridwell KH, Schootman M (2004) Thoracic adolescent idiopathic scoliosis curves between 70 and 100 degree: is anterior release necessary? Presented at 39th Annual Meeting of Scoliosis Research Society, Buenos aires, Argentina [DOI] [PubMed]
- 13.Newton PO, White KK, Faro F, Gayor TG. The success of throacoscopic anterior fusion in a consecutive series of 112 pediatric spinal deformity cases. Spine. 2005;30:392–398. doi: 10.1097/01.brs.0000153404.62017.75. [DOI] [PubMed] [Google Scholar]
- 14.Niemeyer T, Freeman BJC, Grevitt MP, Webb JK. Anterior thoracoscopic surgery followed by posterior instrumentation and fusion in spinal deformity. Eur Spine J. 2000;9:499–504. doi: 10.1007/s005860000181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roy-Camille R, Sailant G, Mazel C. Internal fixation of the lumbar spine woth pedicle screw plating. Clin Orthop. 1986;203:7–17. [PubMed] [Google Scholar]
- 16.Roy-Camille R, Sailant G, Mazel C. Plating of thoracic, thoracolumbar and lumbar injuries with pedicle screw plates. Orthop Clin North Am. 1986;17:147–159. [PubMed] [Google Scholar]
- 17.Suk SI, Kim WJ, Kim JH, Lee SM. Restoration of thoracic kyphosis in the hypokyphotic spine: a comparison between multiple-hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord. 1999;12:489–495. doi: 10.1097/00002517-199912000-00008. [DOI] [PubMed] [Google Scholar]
- 18.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. doi: 10.1097/00007632-199506000-00012. [DOI] [PubMed] [Google Scholar]