Abstract
The balance function of children is known to be affected by carriage of a school backpack. Children with adolescent idiopathic scoliosis (AIS) tend to show poorer balance performance, and are typically treated by bracing, which further affects balance. The objective of this study is to examine the combined effects of school backpack carriage and bracing on girls with AIS. A force platform was used to record center of pressure (COP) motion in 20 schoolgirls undergoing thoraco-lumbar-sacral orthosis (TLSO brace) treatment for AIS. COP data were recorded with and without brace while carrying a backpack loaded at 0, 7.5, 10, 12.5 and 15% of the participant’s bodyweight (BW). Ten participants stood on a solid base and ten stood on a foam base, while all participants kept their eyes closed throughout. Sway parameters were analyzed by repeated measures ANOVA. No effect of bracing was found for the participants standing on the solid base, but wearing the brace significantly increased the sway area, displacement and medio-lateral amplitude in the participants standing on the foam base. The medio-lateral sway amplitude of participants standing on the solid base significantly increased with backpack load, whereas significant increases in antero-posterior sway amplitude, sway path length, sway area per second and short term diffusion coefficient were found in participants standing on the foam base. The poorer balance performance exhibited by participants with AIS when visual and somatosensory input is challenged appears to be exacerbated by wearing a TLSO brace, but no interactive effect between bracing and backpack loading was found.
Keywords: Scoliosis, Balance, Load carriage, Bracing, Center of pressure
Introduction
Individual balance performance and stability of upright stance may be affected by different clinical conditions, including scoliosis, a lateral curvature of the spine [2]. Upright stance is an inherently unstable condition, and can be characterized by the motion of the center of pressure (COP) of the ground reaction force, which follows the motion of the center of gravity of the body and has been modeled as a fractal Brownian motion, analogous to the random motion or diffusion of particles suspended in a fluid [8, 20, 21]. Stability and balance in upright stance is maintained by keeping the COP above the base of support, which is achieved by a feedback mechanism integrating information from the visual, proprioceptive and vestibular systems [9]. Idiopathic scoliosis is associated with disorders of postural control parameters [9] and patients with adolescent idiopathic scoliosis (AIS) generally show poorer balance control than age-matched normals, particularly when the visual and somatosensory systems are simultaneously challenged [3, 22, 23, 30]. Studies have indicated that the lateral stability of patients with AIS is significantly poorer than that found in normal subjects [5, 7].
External factors can also add to the burden on the balance mechanism and have adverse effects on control of balance. An obvious example of this is load carriage, which has been shown to result in greater COP motion than when no load is carried [7]. The effects of load carriage have become an area of concern in schoolchildren, as the loads carried daily in schoolbags are relatively high with respect to the child’s bodyweight (BW), and have generally been found to exceed the recommended 10% BW limit. Cavallo et al. [4] found that over a quarter of the female students in a fourth grade group carried a backpack of greater than 15% BW, while Negrini and Carabalona [18] reported a mean backpack load of over 20% BW, similar to the reported mean schoolbag weight carried by children in Hong Kong [11]. The daily loads applied by schoolbags are of concern because of the association with back pain [25], and are of particular concern in patients with AIS as abnormal external loading has been suggested as one of the possible factors that may affect the growth of the spine and exacerbate the scoliotic deformity [19]. The immediate ergonomic effects of backpack carriage are also a concern in patients with AIS, as both of these factors challenge the balance function and will therefore increase the risk of loss of balance and fall, which account for most of the hospital accident and emergency department cases involving backpacks [27].
Bracing is generally recommended for AIS patients with a Cobb angle of between 25° and 45° [2], primarily in order to prevent curve progression but also with the aim of achieving some curve correction. The custom molded thoraco-lumbo-sacral orthosis (TLSO) or “underarm” brace is typically prescribed for non-operative treatment of progressive AIS. Bracing has also been demonstrated to have an immediate effect on sitting balance [26], with a better balance of weight on each ischial tuberosity and increased sitting stability. However, Sales De Gauzy et al. [24] reported that a group of patients with AIS showed significantly poorer static balance performance when wearing their brace than without it, although no details were given and it is not clear what balance parameters where being compared in this case. As experimental evidence suggests that both backpack carriage and bracing individually cause poorer balance performance, it is therefore hypothesized that the effect of backpack carriage on stance balance will be more severe when the subject is wearing a brace. The combined effect of bracing and backpack carriage may not be a simple superposition of the individual effects if there is any interaction between backpack carriage and bracing.
Overall, backpack carriage is known to adversely affect the control of balance in patients with AIS, and experimental evidence suggests that this effect may be more pronounced while wearing a brace. However, to the authors’ knowledge, no experimental data reflecting these conditions have been reported. The aim of this study is therefore to examine the balance of patients with AIS when carrying different backpack loads both with and without using a brace under different somatosensory conditions.
Methods
Twenty skeletally immature schoolgirls (Risser’s sign from 0 to II) between the ages of 10 and 16 (mean age 13) undergoing TLSO brace treatment for AIS were recruited for this study (Table 1). Inclusion criteria were a Cobb angle of between 25° and 35°, no history of operative treatment and no other known musculoskeletal problems. The experimental procedures were clearly explained in each case and written informed consent was obtained from participants and their parents/guardians prior to the participants taking part in the experiment. Participants were asked to stand barefoot on a force platform (Kistler 9281CA, Winterthur, Switzerland), adopting a natural and comfortable stance, with the arms relaxed at the sides [17, 29] and the feet separated at approximately at shoulder width, making an angle of 14° between the long axis of the feet [16]. Ten participants (S01 to S10, Table 1) stood on the solid base of the force platform, while ten participants (F01 to F10) stood on a 10 cm thick foam base. The position of the feet was marked to ensure reproducible foot placements for subsequent tests [10]. The participants were asked to close their eyes and the two-dimensional horizontal coordinates of the center of pressure (COP) were recorded for 30 s. The data were recorded at a frequency of 50 Hz and low-pass filtered with a cut-off frequency of 2.5 Hz [28] using Matlab software (The MathWorks Inc, Natick, MA) and stored on a PC. COP data were recorded at various backpack loads for participants without a brace, and while wearing their prescribed thoraco-lumbo-sacral orthosis (TLSO). A specially designed backpack [6] was used loaded at 7.5, 10, 12.5 and 15% of the participants’ bodyweight (BW), and data were also recorded without backpack, giving a total of ten different testing conditions of bracing and backpack load. The order in which the testing conditions were carried out was randomized to minimize possible effects of fatigue or hysteresis, and three repeat trials were conducted for each condition, with 1-min rest between trials [12].
Table 1.
Details of the anthropometry and scoliotic curvature of the schoolgirls pariticipating in this study
| No. | Age (years) | Weight (kg) | Height (m) | Risser’s sign | AIS curve pattern | Cobb angle (degrees) | Apex level |
|---|---|---|---|---|---|---|---|
| S01 | 11 | 38.6 | 1.51 | 0 | R thoracic/L lumbar | 27/31 | T8/L2 |
| S02 | 12 | 41.8 | 1.53 | II | L lumbar | 25 | L2 |
| S03 | 14 | 36.4 | 1.52 | I | L thoracolumbar | 28 | T12 |
| S04 | 15 | 52.9 | 1.67 | II | R thoracic/L lumbar | 35/33 | T8/L1 |
| S05 | 12 | 40.8 | 1.5 | I | R thoracic | 23 | T8 |
| S06 | 15 | 38.6 | 1.56 | II | R thoracic/L lumbar | 35/26 | T9/L2 |
| S07 | 16 | 40.8 | 1.55 | II | L thoracolumbar | 34 | T12 |
| S08 | 15 | 40.8 | 1.56 | I | L thoracic/R lumbar | 20/25 | T11/L3 |
| S09 | 10 | 38.1 | 1.51 | 0 | L lumbar | 25 | L1 |
| S10 | 12 | 33 | 1.47 | 0 | Double thoracic | 25/28 | T4/T10 |
| F01 | 13 | 47.9 | 1.52 | I | R thoracic/L lumbar | 35/35 | T8/L2 |
| F02 | 15 | 48.8 | 1.52 | II | R thoracic | 35 | T8 |
| F03 | 14 | 45.3 | 1.57 | I | R lumbar | 30 | L3 |
| F04 | 12 | 29.8 | 1.38 | 0 | R thoracolumbar | 32 | T12-L1 |
| F05 | 11 | 45.8 | 1.55 | 0 | R thoracic/L lumbar | 20/28 | T8/L1 |
| F06 | 11 | 35.4 | 1.54 | 0 | Double thoracic | 35/35 | T3/T9 |
| F07 | 12 | 50.1 | 1.61 | I | R thoracic/L lumbar | 35/31 | T8/L2 |
| F08 | 14 | 45.5 | 1.6 | II | Double thoracic | 29/16 | T4/T12 |
| F09 | 12 | 32.3 | 1.47 | II | Double thoracic | 24/29 | T4/T12 |
| F10 | 14 | 39 | 1.64 | 0 | R thoracic/L lumbar | 19/25 | T8/L1 |
Relevant and stable measures of postural sway identified by Wolff et al. [29] were calculated and subject to statistical analysis. The parameters used were:
Antero-posterior (AP) sway amplitude: The maximum range of anterior–posterior sway motion over the data collection interval.
Medio-lateral (ML) sway amplitude: The maximum range of medio-lateral sway motion over the data collection interval.
- Average sway path length (P): The average distance per second traced out by the COP path (the average speed of the COP motion) over the data collection interval is given by
where f is the sampling rate, N is the number of sample points, and xi, yi, xi+m and yi+m are the medio-lateral and antero-posterior coordinates respectively of the COP at sample indices i and i+m, respectively.
- Average radial displacement (Rd): The average distance from the instantaneous radial COP position (ri) to the mean radial centroid of the COP position over the data collection interval (rc), given by
where the mean medio-lateral and antero-posterior COP positions xc and yc are defined as
and the radial centroid rc is given as
- Sway area per second (A): The average area per second swept out by the line between the instantaneous COP position and the mean COP position over the data collection interval, given by
- Mean frequency (MF): The average frequency at which the instantaneous COP position circles the mean COP position, given by
- Short-term diffusion coefficient: The average rate at which the center of pressure is likely to change over the short term. This models COP motion on the basis of Brownian motion [8] and the value of the short-term diffusion coefficient reflects the stochastic activity of the COP motion. This value is determined as half of the gradient of the diffusion plot given by (drdt)2 versus dt for small dt where
such that m is the data interval, and dt = m/f.
Diffusion scaling exponent: The likelihood that the COP position will continue to change along the same direction, given by the gradient of the base-10 logarithm of the diffusion plot. If the diffusion scaling exponent is less than 0.5, the COP tends to reverse its direction in the next dt, whereas if the diffusion scaling exponent is greater than 0.5, the COP tends to continue moving in the same direction [8].
Shapiro–Wilk test was used to confirm the normality of the data and the mean value of each of these parameters were analyzed by three-way repeated measures ANOVA (SPSS 14.0, SPSS Inc., Chicago, IL, USA), with within-subject factors of bracing and backpack load and between-subject factor of base. The level of statistical significance was set at 0.05, and post-hoc comparisons were made using Bonferroni criteria [13].
Results
Significant effects of load, brace and base were found on all of the static balance parameters with the exception of the mean sway frequency (Table 2). However, significant interactions between brace and base and load and base were also found, and therefore the results were analyzed for the foam and the solid bases independently.
Table 2.
A summary of the results of the statistical analysis conducted
| Antero-posterior amplitude | Medio-lateral amplitude | Path length | Average radial displacement | Sway area/second | Mean sway frequency | Short term diffusion coefficient | Scaling exponent | |
|---|---|---|---|---|---|---|---|---|
| Load | P = 0.003 | P = 0.008 | P < 0.001 | P = 0.024 | P = 0.002 | NS | P < 0.001 | NS |
| Base | P < 0.001 | P = 0.000 | P < 0.001 | P < 0.001 | P < 0.001 | NS | P < 0.001 | P = 0.007 |
| Brace | NS | NS | P = 0.037 | P = 0.041 | NS | NS | P = 0.046 | NS |
| Load × base | NS | NS | P = 0.001 | NS | P = 0.019 | NS | P = 0.002 | NS |
| Base × brace | NS | P = 0.013 | P = 0.044 | P = 0.033 | P = 0.035 | NS | NS | NS |
| Load × brace | NS | NS | NS | NS | NS | NS | NS | NS |
| Load × base × brace | NS | NS | NS | NS | NS | NS | NS | NS |
| Solid base results (no bonferroni correction) | ||||||||
| load | NS | P = 0.030 | NS | NS | NS | NS | NS | NS |
| brace | NS | NS | NS | NS | NS | NS | NS | NS |
| Load × brace | NS | NS | NS | NS | NS | NS | NS | NS |
| Foam base results (no bonferroni correction) | ||||||||
| Load | P = 0.022 | NS | P < 0.001 | NS | P = 0.008 | NS | P < 0.001 | NS |
| Brace | NS | P = 0.022 | P = 0.036 | P = 0.045 | NS | NS | NS | NS |
| Load × brace | NS | NS | NS | NS | NS | NS | NS | NS |
P values are shown for significant main effects of and interactions between load, base and brace as appropriate, and are marked
NS where not significant
The results for the participants standing on the solid base showed that increase in backpack loading had no significant effects on any of the recorded static balance parameters apart from a slight but significant increase in ML COP sway amplitude (Table 3; Fig. 1). No significant effect of bracing was found on any of the recorded parameters for the participants standing on the solid base, nor where any interactions between bracing and backpack loading found.
Table 3.
Results of the separate statistical analyses for a) the solid base and b) the foam base
| Antero-posterior amplitude | Medio-lateral amplitude | Path length | Average radial displacement | Sway area/second | Mean sway frequency | Short term diffusion coefficient | Scaling exponent | |
|---|---|---|---|---|---|---|---|---|
| a—solid base results | ||||||||
| Load | NS | P = 0.030 | NS | NS | NS | NS | NS | NS |
| Brace | NS | NS | NS | NS | NS | NS | NS | NS |
| Load × brace | NS | NS | NS | NS | NS | NS | NS | NS |
| b—foam base results | ||||||||
| Load | P = 0.022 | NS | P < 0.001 | NS | P = 0.008 | NS | P < 0.001 | NS |
| Brace | NS | P = 0.022 | P = 0.036 | P = 0.045 | NS | NS | NS | NS |
| Load × brace | NS | NS | NS | NS | NS | NS | NS | NS |
P values are shown for significant main effects of and interactions between load and brace as appropriate, and are marked
NS where not significant
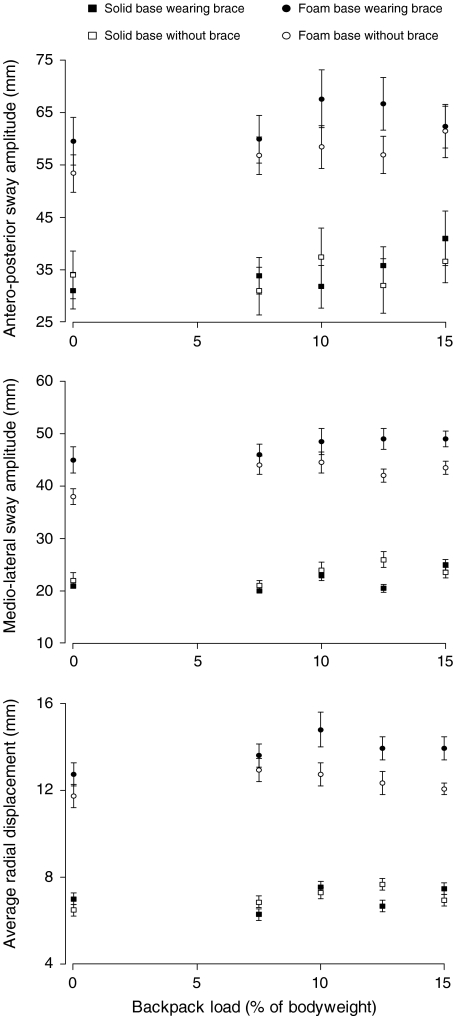
Fig. 1.
The antero-posterior, medio-lateral and average radial displacements at each of the backpack loads for the different bracing and base conditions. Mean values are plotted with the standard error indicated by the error bars
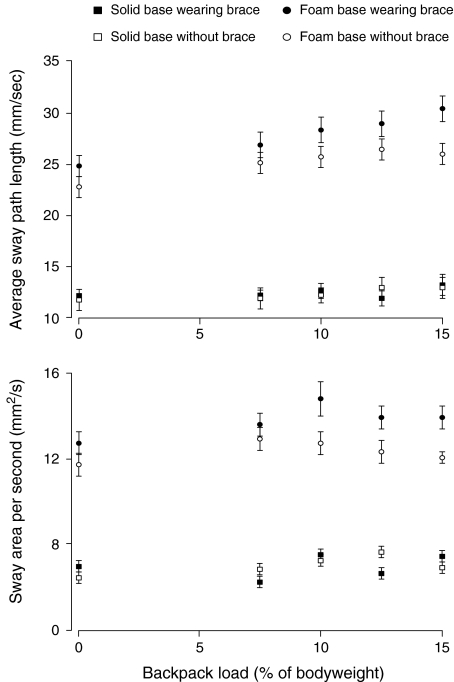
The participants standing on the foam base showed significant main effects of backpack loading on the AP sway amplitude, the average sway path length, the sway area per second, and the short term diffusion coefficient (Table 3), all of which increased with increasing backpack load (Figs. 1, 2, 3). Significant effects of bracing were also seen on the ML sway amplitude, the average radial displacement and the average sway path length (Table 3), with the values for all of these parameters being lower without the brace at all of the recorded backpack loads (Figs. 1, 2). The short-term diffusion coefficient for the participants standing on the foam base was noticeably higher at all backpack loads while wearing the brace (Fig. 3), but this effect was not found to be significant (P = 0.064). There also appeared to be a trend in the short term diffusion coefficient for the participants standing on the foam base where the effect of load was more evident while wearing the brace than without it, illustrated by the steeper overall gradient of the “foam base wearing brace” data points in the top plot of Fig. 3 as compared to the “foam base without brace” data points in the same plot. Again, however, this interaction between loading and bracing was not found to be significant (P = 0.163), and no significant interactions were found between backpack loading and bracing for any of the recorded parameters for either the solid or the foam base.
Fig. 2.
The average sway path length and sway area per second at each of the backpack loads for the different bracing and base conditions. Mean values are plotted with the standard error indicated by the error bars
Fig. 3.
The short-term diffusion coefficient, mean sway frequency and scaling exponent at each of the backpack loads for the different bracing and base conditions. Mean values are plotted with the standard error indicated by the error bars
As can be seen from these figures, the mean values of the recorded COP motion parameters during static balance were consistently higher in the group standing on the foam base than in the group standing on the solid base, with the exception of the scaling exponent, which was consistently higher in the group standing on the solid base (Fig. 3).
Discussion
Postural sway during quiet standing is typically quantified by parameters derived from the motion of the COP. Studies have shown that multiple measures are required to characterize this motion [14], and that measures related to both the amplitude and the velocity or frequency of the sway are required. A recent study indicated that the most sensitive measures were obtained from the single class of measures of stabilogram diffusion coefficients [15]. The measures used in this study include both amplitude and frequency terms of the COP motion as well as the short-term diffusion coefficient [29].
A pure repeated measures design with all participants stood on both the foam and the solid base would have been preferable to minimizing the between-subject effect. However, as the experiment was conducted in two stages, a mixed repeated measures experimental design was therefore employed in this study and the results for the different bases were analyzed separately rather than as a sub-analysis of the three-way repeated measures ANOVA. Ideally, the curve patterns of each of the participants would also be the same to avoid any confounding influence that different degrees and levels of scoliotic curvature may have. It would also be useful if the results obtained could be compared against those obtained from a control group of normal schoolgirls. However, ethical considerations do not allow the bracing of participants without any clinical purpose, and as such the inclusion of a normal group would have not added significantly to the study.
The results of this study indicate that bracing may affect the balance function of schoolgirls with AIS, but only when the visual and proprioceptive systems are simultaneously challenged, i.e. where the participant stands on the foam base with her eyes closed. Under such conditions, participants generally show a more marked deterioration in balance function with increasing load when wearing the brace than without the brace. There are several mechanisms by which wearing the brace could affect the balance of the participants. As the backpack has to be worn on top of the brace, then it will be slightly posterior to the position when the participant is not wearing the brace, and such a change in the position of the center of gravity of the backpack may affect the balance function. However, this change in the position of the backpack while wearing the brace will affect the participants standing on the solid and foam bases equally, and would not immediately account for the effect of bracing only being obvious in the participants standing on the foam base. Another mechanism by which bracing may affect the balance function is by limitation of the trunk motion between the thoracic and sacral spine, which may in turn restrict the ability of the trunk to contribute to the maintenance of balance. Under normal circumstances, balance is generally maintained by an “ankle strategy” where the motion required to maintain the COP within the base of stance is predominantly around the ankles [28], but as the challenge to balance increases, the strategy for maintaining balance shifts towards motion of the pelvis and trunk [28]. This may account for the different effects of wearing the brace while standing on the solid base and foam base: when the proprioceptive feedback mechanism is not challenged (standing on the solid base), then an ankle strategy may be sufficient to maintain balance, and as a result the increased rigidity between the pelvis and trunk due to the brace will not affect the balance function. However, when the challenge to balance is increased by standing on the foam base, the ankle strategy may no longer be sufficient to maintain balance, and any increasing reliance on motion of the pelvis and trunk to maintain balance may mean that participants are likely to perform relatively poorly when wearing the brace. While this study indicated that bracing affected patients with AIS only when proprioception was challenged by standing on the foam base, a previous study [24] indicated that wearing a brace caused deterioration of static balance performance in participants presumably standing on a solid base. However, detailed experimental details and results were not reported.
While the immediate effects of wearing a brace appear to be a decrease in stability of quiet stance, Adler et al. [1] found that patients with progressive scoliosis who had undergone bracing performed significantly better in balance tests than patients with progressive scoliosis who had not undergone bracing (the braces were not worn during testing). As a result, they suggested that the orthosis might have a therapeutic effect compensating for deficiencies in balance in patients with AIS. These results may not be inconsistent with those presented here, as the immediate challenge to balance caused by the brace may have a long term training effect resulting in gradual improvement of balance function. Further longitudinal prospective studies would be useful to identify the long-term effect of bracing on balance function. It should also be noted that the present study is restricted to an investigation of the immediate effects of loading on balance function, and that the duration of the carriage of the load may have a significant effect on the balance parameters as muscular fatigue becomes evident. Likewise, only one carriage method was considered with the pack suspended over both shoulders, whereas backpack carriage over one shoulder is frequently found, and further studies to investigate the effects of these factors are recommended.
Conclusion
Overall, the quiet standing balance of schoolgirls undergoing bracing treatment for AIS is sensitive to backpack load and shows significant dependence on reliable somatosensory input. Under normal circumstances, bracing does not appear likely to have an immediate effect on balance function, but when somatosensory input is challenged, bracing may result in poorer balance ability and greater sensitivity to backpack loading. The implications of increased risk of loss of balance of AIS patients undergoing bracing may become an important consideration under such circumstances.
References
- 1.Adler N, Bleck EE, Rinsky LA, Young W. Balance reactions and eye-hand coordination in idiopathic scoliosis. J Orthop Res. 1986;4:102–107. doi: 10.1002/jor.1100040113. [DOI] [PubMed] [Google Scholar]
- 2.Bradford DS, Lonstein JE, Moe JH, Ogilvie JW, Winter RB. Moe’s textbook of scoliosis and other spinal deformity, 2nd. Philadelphia: Saunders; 1987. [Google Scholar]
- 3.Byl NN, Holland S, Jurek A, Hu SS. Postural imbalance and vibratory sensitivity in patients with idiopathic scoliosis: implications for treatment. J Orthop Sports Phys Ther. 1997;26:60–68. doi: 10.2519/jospt.1997.26.2.60. [DOI] [PubMed] [Google Scholar]
- 4.Cavallo CM, Hlavaty TM, Tamase MG. A pilot study for the development of a primary prevention program: what is the average weight of a fourth grader’s backpack? Work. 2003;20:137–158. [PubMed] [Google Scholar]
- 5.Chen PQ, Wang JL, Tsuang YH, Liao TL, Huang PI, Hang YS. The postural stability control and gait pattern of idiopathic scoliosis adolescents. Clin Biomech. 1998;13(Suppl 1):S52–S58. doi: 10.1016/S0268-0033(97)00075-2. [DOI] [PubMed] [Google Scholar]
- 6.Chow DH, Kwok ML, Au-Yang AC, Holmes AD, Cheng JC, Yao FY, Wong MS. The effect of backpack load on the gait of normal adolescent girls. Ergonomics. 2005;48:642–656. doi: 10.1080/00140130500070921. [DOI] [PubMed] [Google Scholar]
- 7.Chow DHK, Kwok MLY, Cheng JCY, Lao MLM, Holmes AD, Au-Yang A, Yao FYD, Wong MS. The effect of backpack weight on the standing posture and balance of schoolgirls with adolescent idiopathic scoliosis and normal controls. Gait Posture. 2005;24:173–181. doi: 10.1016/j.gaitpost.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Collins JJ, DeLuca CJ. Open-loop and closed-loop control of posture: a random walk analysis of center-of-pressure trajectories. Exp Brain Res. 1993;95:308–318. doi: 10.1007/BF00229788. [DOI] [PubMed] [Google Scholar]
- 9.Gauchard GC, Lascombes P, Kuhnast M, Perrin PP. Influence of different types of progressive idiopathic scoliosis on static and dynamic postural control. Spine. 2001;26:1052–1058. doi: 10.1097/00007632-200105010-00014. [DOI] [PubMed] [Google Scholar]
- 10.Harris GF, Knox TA, Larson SJ Jr, AS, Millar EA (1982) A method for the display of balance platform center of pressure data. J Biomech 15:741–745 [DOI] [PubMed]
- 11.Hong Y, Cheung CK. Gait and posture responses to backpack load during level walking in children. Gait Posture. 2003;17:28–33. doi: 10.1016/S0966-6362(02)00050-4. [DOI] [PubMed] [Google Scholar]
- 12.Jeong BY. Respiration effect on standing balance. Arch Phys Med Rehabil. 1991;72:642–645. [PubMed] [Google Scholar]
- 13.Keppel G. Design and analysis: a researchers handbook. 3rd. Upper Saddle River: Prentice-Hall; 1991. [Google Scholar]
- 14.Kitabayashi T, Demura S, Noda M. Examination of the factor structure of center of foot pressure movement and cross reliability. J Physiol Anthropol Appl Hum Sci. 2003;22:265–272. doi: 10.2114/jpa.22.265. [DOI] [PubMed] [Google Scholar]
- 15.Maurer C, Peterka RJ. A new interpretation of spontaneous sway measures based on a simple model of human postural control. J Neurophysiol. 2005;93:189–200. doi: 10.1152/jn.00221.2004. [DOI] [PubMed] [Google Scholar]
- 16.McIlroy WE, Maki BE. Preferred placement of the feet during quiet stance: development of a standardized foot placement for balance testing. Clin Biomech. 1997;12:66–70. doi: 10.1016/S0268-0033(96)00040-X. [DOI] [PubMed] [Google Scholar]
- 17.Morton SM, Bastian AJ. Relative contributions of balance and voluntary leg-coordination deficits to cerebellar gait ataxia. J Neurophysiol. 2003;89:1844–1856. doi: 10.1152/jn.00787.2002. [DOI] [PubMed] [Google Scholar]
- 18.Negrini S, Carabalona R. Backpacks on! Schoolchildren’s perceptions of load, associations with back pain and factors determining the load. Spine. 2002;27:187–195. doi: 10.1097/00007632-200201150-00014. [DOI] [PubMed] [Google Scholar]
- 19.Perdriolle R, Becchetti S, Vidal J, Lopez P. Mechanical process and growth cartilages. Essential factors in the progression of scoliosis. Spine. 1993;18:343–349. doi: 10.1097/00007632-199303000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Peterka RJ. Postural control model interpretation of stabilogram diffusion analysis. Biol Cybern. 2000;82:335–343. doi: 10.1007/s004220050587. [DOI] [PubMed] [Google Scholar]
- 21.Rougier P, Caron O. Center of gravity motions and ankle joint stiffness control in upright undisturbed stance modeled through a fractional Brownian motion framework. J Mot Behav. 2000;32:405–413. doi: 10.1080/00222890009601390. [DOI] [PubMed] [Google Scholar]
- 22.Sahlstrand T, Lindstrom J. Equilibrium factors as predictors of the prognosis of adolescent idiopathic scoliosis. Clin Orthop Rel Res. 1982;152:232–236. [PubMed] [Google Scholar]
- 23.Sahlstrand T, Petruson B. A study of labyrinthine function in patients with adolescent idiopathic scoliosis. Acta Orthop Scand. 1979;50:759–769. doi: 10.3109/17453677908991307. [DOI] [PubMed] [Google Scholar]
- 24.Sales Gauzy J, Domenech P, Dupui P, Montoya R, Cahuzac JP. Effect of bracing on postural balance in idiopathic scoliosis. Health Technol Inform. 2002;88:239–240. [PubMed] [Google Scholar]
- 25.Sheir-Neiss GI, Krus RW, Rahman T, Jacobson LP, Pelli JA. The association of backpack use and back pain in adolescents. Spine. 2003;28:922–930. doi: 10.1097/00007632-200305010-00015. [DOI] [PubMed] [Google Scholar]
- 26.Smith RM, Emans JB. Sitting balance in spinal deformity. Spine. 1992;17:1103–1109. doi: 10.1097/00007632-199209000-00016. [DOI] [PubMed] [Google Scholar]
- 27.Wiersema BM, Wall EJ, Foad SL. Acute backpack injuries in children. Pediatrics. 2003;111:163–166. doi: 10.1542/peds.111.1.163. [DOI] [PubMed] [Google Scholar]
- 28.Winter DA. Anatomy, biomechanics and control of balance during standing and walking. Waterloo: Waterloo Biomechanics; 2005. [Google Scholar]
- 29.Wolff DR, Rose J, Jones VK, Bloch DA, Oehlert JW, Gamble JG. Postural balance measurements for children and adolescents. J Orthop Res. 1998;16:271–275. doi: 10.1002/jor.1100160215. [DOI] [PubMed] [Google Scholar]
- 30.Yamada K, Yamamoto H, Nakagawa Y, Tezuka A, Tamura T, Kawata S. Etiology of idiopathic scoliosis. Clin Orthop. 1984;184:50–57. [PubMed] [Google Scholar]