Abstract
To retrospectively study the long-term outcome of patients after anterior cervical discectomy without fusion (ACD) compared to results published on the long-term outcome after ACD with fusion (ACDF). We reviewed the charts of all patients receiving ACD surgery between 1985 and 2000 to analyze the direct post-operative results as well as complications of the surgery. Moreover, 102 patients, randomly selected, were interviewed with the neck disability index to study possible persisting complaints up to 18 years after ACD surgery. A total of 551 Patients were identified. Two months post-operative follow up at the outpatient clinic revealed that 90.1% of patients were satisfied with the result of ACD surgery. At the time of the survey, this percentage had dropped to 67.6%. In addition, 20.6% and 11.8% had obtained moderate to severe complaints, respectively, in daily-life activities. Complaints were mainly localized in the neck region and occasionally provoked radiating pain in the arm. On the short term, ACD leads to a satisfied outcome. Over the longer term, patients report increasing complaints. The increase in complaints at the time of the survey may be the result of ongoing degenerative effects. Compared to published data on ACDF, there is no superiority of any fusion technique compared to ACD alone.
Keywords: Cervical, Discectomy, Surgery, Outcome
Introduction
Cervical spondylosis and disk herniation are frequent causes of arm pain. When conservative treatment fails, surgical decompression can be considered. The most common surgical techniques are discectomy with or without fusing the two adjacent intervertebral bodies. Robinson and Smith [3, 33, 34, 38] introduced the anterior cervical decompression technique without microscope, but with fusion by inserting a bone graft harvested from the iliac crest of the patient. Hankinson and Wilson [18] improved the procedure with the use of an operating microscope; however, they performed the surgery without leaving a graft behind; the results of both types of surgery were entirely comparable [1, 12, 20].
In time several modifications of these surgical techniques have been made [6, 10, 28]. In addition, to enhance fusion, anterior plating procedures have been developed. These plating procedures provide immediate stability and maintain spinal alignment [20, 22]. The outcome of these studies has ranged from no significant improvement in clinical outcome [22, 40] to increased fusion rates and fewer re-operations possibly due to the stabilizing effects of plating [9, 23, 44, 45]. Finally, more recently, artificial intervertebral disc replacements have been used to try to simulate the natural situation and motion of the spinal column [8]. Although the first results have been promising [16, 26], some have presented cases in which as adverse effect fusion around the prosthesis occurred [5].
Performing anterior cervical discectomy with fusion (ACDF) has proven to be successful in relieving arm pain and has been considered as the golden standard for this kind of surgery. However, ACDF has not been proven to be better than anterior cervical discectomy without fusion (ACD) [20]. Especially, in Europe ACD alone is still being used as a surgical procedure. In this study, we retrospectively study the long-term clinical outcome after ACD surgery and compare this with the long-term outcome of ACDF surgery as reported in literature.
Materials and methods
The database of the neurosurgical department of Leiden University Medical Center (LUMC), Leiden, The Netherlands, was searched for patients on whom single level ACD surgery was performed between 1985 and 2000. All patients’ charts were studied for level and side of surgery, pre operative symptoms, post operative results, possible complications and follow up at the outpatient clinic. At random, 102 patients were subjected to a survey by phone concerning their complaints at that time using the Neck Disability Index (NDI) [42]. Patients from all years of the study were included. The questionnaire consisted of ten questions, each containing six statements (A–F). The sections concerned impairments like pain and abilities like personal care, lifting, reading, driving, and recreation. For each section, subjects choose the statement that best described their status. The chosen statements received scores: statement A = 0; statement B = 1; C = 2; D = 3; E = 4; F = 5. Total scores ranged from 0 (highest level of function) to 50 (lowest level of function). We used the Fairbank et al. [13] grading system to grade the patients’ outcome at the time of the survey. According to Fairbank et al. [13] clinicians can calculate the “percentage of disability” with scores of 0–10 for minimal disability. Scores ranging from 10 to 20 stands for moderate disability in which patients are comprised in their daily activities; however they manage to balance their activities in relation to the complaints. More than 20 points is considered to give restrictions in daily care and result in patients needing to stop certain activities because of their neck complaints and are graded severe.
Patients with moderate to severe complaints were also analyzed by sorting them according to the year they received ACD surgery. The follow-up period at the time of the survey was then calculated by subtracting the year of the surgery from the year of the survey. Finally, the average NDI score at the time of the survey was related to these follow-up periods to study the correlation between complaints and time after surgery.
Discharge from the hospital usually occurred the day after surgery, unless patients complained about severe dysphagia with minimal oral intake or complications occurred. First follow up at the outpatient clinic was done 6 weeks after surgery.
Surgical technique
Patients were operated by several surgeons joining the neurosurgical team at the LUMC. Nevertheless, all surgeons performed ACD surgery as previously described [36] in the same manner. Briefly, a transverse incision is being used. Using optical magnification and by passing medially from the carotid sheath and laterally from the esophagus and trachea, the anterior aspect of the cervical spine can be reached. After identification of the correct level, the anterior longitudinal ligament is cut and the intervertebral disc excised. Finally, the endplates are removed from the cartilage to induce fusion.
Results
A total of 551 patients were identified, of which 324 were men and 227 women. The age ranged between 17 and 84 years. We were able to retrieve 456 of the 551 charts of the patients. The level of surgery is depicted in Table 1.
Table 1.
Level of surgery (n = 456)
| C2–C3 | 0% (n = 0) |
| C3–C4 | 2.0% (n = 9) |
| C4–C5 | 5.9% (n = 27) |
| C5–C6 | 40.1% (n = 183) |
| C6–C7 | 47.8% (n = 218) |
| C7–Th1 | 4.2% (n = 19) |
C cervical, Th thoracic
Pre-operatively, 41.2% (n = 190) of the patients had pain in the right arm, 48.9% (n = 223) in the left, while 9.9% (n = 43) either had pain in both arms or did not have a clear radiating pain in an arm. Next to the radiating pain, 19.6% (n = 89) had this in combination with (subjective) motor deficits and 7.1% (n = 32) had complaints of myelopathia.
Post-operatively, complications occurred in 10.5% (n = 48), ranging from minor complications including urinary tract infections and pneumonia in 3.7% (n = 17) to more severe complications resulting in a second operation and an increased hospital stay such as progressive neurological loss (0.7%, n = 3) or a hematoma (0.9%, n = 4). Hoarseness occurred in 2.2% (n = 10) (Table 2).
Table 2.
Complications (out of n = 456)
| Increased neurological deficits | 0.7% (n = 3) |
| Hoarseness | 2.2% (n = 10) |
| Hematoma | 0.9% (n = 4) |
| Re-operation | 3.1% (n = 14) |
| Others | 3.7% (n = 17) |
| Total | 10.5% (n = 48) |
Follow-up at the outpatient clinic 6 weeks after surgery revealed that 90.1% (n = 411) of patients were satisfied with the surgery, although regularly numbness of the top of the digits persisted. In 9.9% (n = 43) patients’ complaints remained as existed pre-operatively.
At the time of the survey, the post-operative follow-up period of the patients (n = 102) differed from 3 years up to 18 years, with a median and mean of 7 years. The NDI [42] revealed that in 67.6% (n = 69) of the patients, complaints had not returned and new neck complaints had not occurred. Furthermore, 20.6% (n = 21) of patients had moderate complaints in the neck, which allowed them to continue their daily activities with some adaptations. Finally, 11.8% (n = 12) had severe complaints such as pain in neck and head, problems in daily personal care, reading and driving difficulties and had to stop certain activities (Table 3).
Table 3.
Neck disability score of n = 102 patients
| Score | Patients | Score | Patients |
|---|---|---|---|
| 0 | 44 | 21–25 | 5 |
| 1–5 | 18 | 26–30 | 4 |
| 6–10 | 7 | 31–35 | 1 |
| 11–15 | 12 | 36–40 | 1 |
| 16–20 | 9 | 41–45 | 1 |
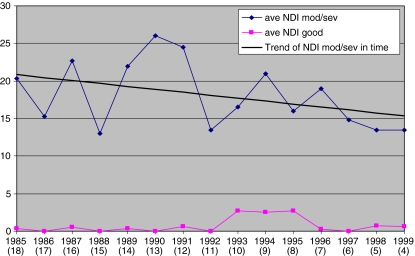
Patients with a good outcome were found at all follow up periods, without a clear preference (Fig. 1). Evaluation of the moderate and severe complaints in time showed that this group of patients increased their complaints in time after surgery. Figure 1 shows a graph of the average NDI score for each year of surgery. In Table 4, the mean NDI score has been calculated in brackets of 5-year follow-up. The table does not show a clear deterioration in complaints over time, however, by adding a trend line in the graph it becomes clear that there is an increase in complaints with an increase of follow-up time after surgery. The line drops 10 points in NDI score over the 15 years of follow up, which means that each year an increase of 0.67 points in complaints can be estimated (Fig. 1 and Table 4).
Fig. 1.
Average neck disability scores of patients with good or moderate to severe outcomes at the time of the survey related to the year of surgery. In blue the average scores of moderate to severe patients for each year of surgery between 1985 and 2000 and in black a trend line was added to reveal an increase in complaints after a longer follow up period after single level anterior cervical spine surgery. In pink the average scores of patients with a good outcome. Between brackets are the total years of follow up at the time of the survey
Table 4.
Average NDI score good (<10) or moderate/severe (>10) of patients in time (±SD)
| Follow-up (Years) | Mean NDI good | Mean NDI mod/sev |
|---|---|---|
| 1–5 | 0.88 ± 0.2 | 15.4 ± 4.3 |
| 6–10 | 1.15 ± 1.3 | 20.3 ± 5.3 |
| 11–15 | 0.23 ± 1.1 | 18.7 ± 2.3 |
SD standard deviation, NDI neck disability index, mod moderate, sev severe
Discussion
Literature and medical technology have focused on different fusion techniques in ACD surgery [2, 17]. Several groups report their results of ACDF using different techniques: allograft, autograft, cages with different designs and plating dynamic or not, with as most important outcome that the use of autograft is superior to allograft and that the postoperative neck-pain after surgery is relieved quicker after ACDF [6, 27, 28, 30]. Only a few studies have compared ACD alone with fusion techniques and they all do not show any superiority of a fusion method compared to ACD without fusion [1, 11, 12, 20, 29, 30]. Avoidance of the use of implants reduces costs of surgery. More importantly, these studies revealed that ACD alone resulted in a shorter surgery procedure, hospital stay and sick leave [1, 12, 35]. A frequently reported complication of autologous grafting from the iliac crest is post-operative pain at the donor site, which has been reported to result in up to 22% additional morbidity [30]. Although a more elegant needle technique has reduced this percentage, at 2 weeks post-operatively 12% of patients still has persisting complaints of pain at the donor site [4]. Other complications include wound hematoma, infection, pelvic fracture and nerve palsy at the donor site region [20]. An alternative to prevent this morbidity is the use of allografts [37, 41, 43]. Unfortunately, allografts are expensive, incorporate more slowly and carry the potential risk of disease transmission [20] (Table 5).
Table 5.
Characteristics of each surgical procedure
| ACD | ACDF |
|---|---|
| Similar outcome to ACDF on long term | Similar outcome to ACD on long term |
| Lower risk hoarseness (2.2% versus 5%) | Quicker neck pain relief after surgery |
| No additional morbidity of a donor site | Better sagittal alignment |
| Lower costs | Additional morbidity: pain at donor site |
| Shorter length surgical procedure | Possible complications at donor site |
| Shorter hospital stay | (Hematoma, infection, pelvic fracture) |
ACD anterior cervical discectomy, ACDF anterior cervical discectomy with fusion
In this study, 2.2% of patients had complaints of hoarseness direct post-operative. It has been reported that this percentage is approximately 5% after ACDF [31] (Table 5). Although 80% of vocal cord paralysis recovers within 12 months, this is an invalidating complication for the patient.
Sagittal profiles of the spinal cord have been hypothesized to influence loads on spinal tissue and influence outcome after spinal surgery [24, 25]. It is believed that ACDF surgery maintains sagittal alignment superiorly to ACD surgery, which should result in a better outcome after surgery and thus on the long term in less disability for the patients. Studies on sagittal alignment in the cervical spine have mainly focused on laminoplasty or arthroplasty [21, 25] showing a proper radiological position on the short term. Despite these radiological findings, clinically there has been no significant improvement in outcome on the longer term [32]. Moreover, it has also been published that single-level procedures may lead to a local kyphosis, but do not influence the sagittal alignment as much as multi-level surgery [21]. In our study we provide long-term results of the clinical outcome of single-level surgery in which our patients have similar disability to ACDF surgery.
Although, initially the postoperative outcome is good in more than 90% of the patients, the outcome score on the longer term gradually decreased as the follow up time after surgery increased in a subgroup of the patients. Patients who are doing well after surgery are found without a significant difference at all time points, however patients with moderate to severe complaints can be found increasingly in time after surgery. The increase of complaints at the time of the survey may be the result of ongoing degenerative effects. Only a few studies have been published focusing on a long follow-up period after cervical spine procedures compared to ACDF and therefore it is hard to address the ongoing degenerative effects in the cervical spine. The few that are published have mainly focused on posterior foraminotomy without fusion compared to ACDF, demonstrating similar rates of adjacent segment disease with an annual incidence of 2–3% [19]. Additionally, the increase in complaints is in accordance with the outcome scores after different spine surgeries [7, 14, 15].
Conclusion
Since the complication rate is higher with ACD surgery combined with fusion using autologous material or more expensive in case of the use of alternatives to autologous bone, fusion should at least offer minimal advantages on the long term. Our results show that ACD surgery is certainly not inferior to the results of ACDF. In fact they are comparable. Because the superiority of any fusion procedure has never been proven, it has been suggested that fusion might not be necessary at all [12, 39]. Although, initially the postoperative outcome is good, over the longer term the patients report increasing complaints. Taking into consideration that the long-term complaints may well be the result of ongoing degenerative disc disease, a prospective randomized trial is needed to address the necessity of ACD with or without fusion.
References
- 1.Abd-Alrahman N, Dokmak AS, Abou-Madawi A. Anterior cervical discectomy versus anterior cervical fusion, clinical and radiological outcome study. Acta Neurochir. 1999;141(10):1089–1092. doi: 10.1007/s007010050487. [DOI] [PubMed] [Google Scholar]
- 2.Anderson DG, Albert TJ. Bone grafting, implants, and plating options for anterior cervical fusions. Orthop Clin North Am. 2002;33(2):317–328. doi: 10.1016/S0030-5898(01)00011-6. [DOI] [PubMed] [Google Scholar]
- 3.Aronson N, Filtzer Dl, Bugan M. Anterior cervical fusion by the Smith–Robinson approach. J Neurosurg. 1968;29:397–404. [PubMed] [Google Scholar]
- 4.Bartels RH. Single-blinded prospective randomized study comparing open versus needle technique for obtaining autologous cancellous bone from the iliac crest. Eur Spine J. 2005;14(7):649–653. doi: 10.1007/s00586-004-0818-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartels RH, Donk R. Fusion around cervical disc prosthesis: case report. Neurosurgery. 2005;57(1):E194. doi: 10.1227/01.NEU.0000163419.59635.78. [DOI] [PubMed] [Google Scholar]
- 6.Baskin DS, Ryan P, Sonntag V, Westmark R, Widmayer MA. A prospective, randomized, controlled cervical fusion study using recombinant human bone morphogenetic protein-2 with the CORNERSTONE-SR allograft ring and the ATLANTIS anterior cervical plate. Spine. 2003;28(12):1219–1225. doi: 10.1097/00007632-200306150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Bolini G, Docquier PL, Viehweger E, Launay F, Jouve JL. Thoracolumbar hemivertebrae resection by double approach in a single procedure: long term follow-up. Spine. 2006;31(15):1745–1757. doi: 10.1097/01.brs.0000224176.40457.52. [DOI] [PubMed] [Google Scholar]
- 8.Bryan VE., Jr Cervical motion segment replacement. Eur Spine J. 2002;11(suppl):92–97. doi: 10.1007/s00586-002-0437-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Caspar W, Geisler FH, Pitzen T, Johnson TA. Anterior cervical plate stabilization in one- and two-level degenerative disease: overtreatment or benefit? J Spinal Disord. 1998;11:1–11. doi: 10.1097/00002517-199802000-00001. [DOI] [PubMed] [Google Scholar]
- 10.Cloward RB. The anterior approach for removal of ruptured cervical discs. J Neurosurg. 1958;15:602–617. doi: 10.3171/jns.1958.15.6.0602. [DOI] [PubMed] [Google Scholar]
- 11.la Torre M, Martinez-Quinones JV, Isla A, Arguello C, Bendala A, Casado J, Blazquez MG. Anterior cervical discectomy with and without bone grafting. Multicentric comparative study. J Bone Joint Surg Br. 1995;77B(Suppl 1):24. [Google Scholar]
- 12.Dowd GC, Wirth FP. Anterior cervical discectomy: is fusion necessary? J Neurosurg. 1999;90(1):8–12. doi: 10.3171/spi.1999.90.1.0008. [DOI] [PubMed] [Google Scholar]
- 13.Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–273. [PubMed] [Google Scholar]
- 14.Fu TS, Lai PL, Tsai TT, Niu CC, Chen LH, Chen WJ. Long-term results of disc excision for recurrent lumbar disc herniation with or without posterolateral fusion. Spine. 2005;30(24):2830–2834. doi: 10.1097/01.brs.0000190393.15369.94. [DOI] [PubMed] [Google Scholar]
- 15.Gelalis ID, Stafilas KS, Korompilias AV, Zacharis KC, Beris AE, Xenakis TA. Decompressive surgery for degenerative lumbar spinal stenosis:long-term results. Int Orthop. 2006;30(1):59–63. doi: 10.1007/s00264-005-0030-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goffin J, Casey A, Kehr P, Liebig K, Lind B, Logroscino C, Pointillart V, Calenbergh F, Loon J. Preliminary clinical experience with the Bryan Cervical Disc Prosthesis. Neurosurgery. 2002;51:840–845. doi: 10.1097/00006123-200209000-00048. [DOI] [PubMed] [Google Scholar]
- 17.Hacker RJ, Cauthen JC, Gilbert TJ, Griffith SL. A prospective randomized multicenter clinical evaluation of an anterior cervical fusion cage. Spine. 2000;25(20):2646–2655. doi: 10.1097/00007632-200010150-00017. [DOI] [PubMed] [Google Scholar]
- 18.Hankinson HI, Wilson CB. Use of the operating microscope in anterior cervical discectomy without fusion. J Neurosurg. 1975;43:452–456. doi: 10.3171/jns.1975.43.4.0452. [DOI] [PubMed] [Google Scholar]
- 19.Hillibrand AS, Robbins M. Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J. 2004;4(6):190S–194S. doi: 10.1016/j.spinee.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 20.Jacobs WCH, Anderson PG, Van Limbeek J, Willems PC, Pavlov P (2004) Single or double-level anterior interbody fusion techniques for cervical degenerative disc disease. Cochrane Database Sys Rev 4:CD 004958 [DOI] [PubMed]
- 21.Johnson JP, Lauryssen C, Cambron HO, Pashman R, Regan JJ, Anand N, Bray R. Sagittal alignment and the Bryan cervical artificial disc. Neurosurg Focus. 2004;17(6):E14. doi: 10.3171/foc.2004.17.6.14. [DOI] [PubMed] [Google Scholar]
- 22.Johnson MG, Fisher CG, Boyd M, Pitzen T, Oxland TR, Dvorak MF. The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine. 2004;29(24):2815–2820. doi: 10.1097/01.brs.0000151088.80797.bd. [DOI] [PubMed] [Google Scholar]
- 23.Kaiser MG, Haid RW, Subach BR, Barnes B, Rodts GE. Anterior cervical plating enhances arthrodesis after discectomy and fusion with cortical allograft. Neurosurgery. 2002;50:229–236. doi: 10.1097/00006123-200202000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Kawakami M, Tamaki T, Ando M, Yamada H, Yoshida M. Relationships between sagittal alignment of the cervical spine and morphology of the spinal cord and clinical outcomes in patients with cervical spondylotic myelopathy treated with expansive laminoplasty. J Spinal Disord Tech. 2002;15(5):391–397. doi: 10.1097/00024720-200210000-00008. [DOI] [PubMed] [Google Scholar]
- 25.Keller TS, Colloca CJ, Harrison DD, Harrison DE, Janik TJ. Influence of spine morphology on intervertebral disc loads and stresses in asymptomatic adults:implications for the ideal spine. Spine J. 2005;5(3):297–309. doi: 10.1016/j.spinee.2004.10.050. [DOI] [PubMed] [Google Scholar]
- 26.LaFuente J, Casey ATH, Petzold A, Brew S. The Bryan cervical disc prosthesis as an alternative to arthrodesis in the treatment of cervical spondylosis. J Bone Joint Surg. 2005;87-B:508–512. doi: 10.1302/0301-620X.87B4.15436. [DOI] [PubMed] [Google Scholar]
- 27.Lofgren H, Johannsson V, Olsson T, Ryd L, Levander B. Rigid fusion after Cloward operation for cervical disc disease using autograft, allograft, or xenograft: a randomized study with radiostereometric and clinical follow-up assessment. Spine. 2000;25(15):1908–1916. doi: 10.1097/00007632-200008010-00008. [DOI] [PubMed] [Google Scholar]
- 28.Madawi AA, Powell M, Crockard HA. Biocompatible oesteoconductive polymer versus iliac graft. A prospective comparative study for the evaluation of fusion pattern after anterior cervical discectomy. Spine. 1996;21(18):2123–2139. doi: 10.1097/00007632-199609150-00013. [DOI] [PubMed] [Google Scholar]
- 29.Martins AN. Anterior cervical discectomy with and without interbody bone graft. J Neurosurg. 1976;44:290–295. doi: 10.3171/jns.1976.44.3.0290. [DOI] [PubMed] [Google Scholar]
- 30.McConnel JR, Freeman BJ, Debnath UK, Grevitt MP, Prince HG, Webb JK. A prospective randomized comparison of coralline hydroxyapatite with autograft in cervical interbody fusion. Spine. 2003;28(4):317–323. doi: 10.1097/00007632-200302150-00002. [DOI] [PubMed] [Google Scholar]
- 31.Morpeth JF, Williams MF. Vocal cord paralysis after anterior cervical discectomy and fusion. Laryngoscope. 2000;110(1):43–46. doi: 10.1097/00005537-200001000-00009. [DOI] [PubMed] [Google Scholar]
- 32.Pickett GE, Mitsis DK, Sekhon LH, Sears WR, Duggal N. Effects of a cervical disc prosthesis on segmental and cervical spine alignment. Neurosurg Focus. 2004;17(3):E5. doi: 10.3171/foc.2004.17.3.5. [DOI] [PubMed] [Google Scholar]
- 33.Robinson RA, Smith GW. Anterolateral cervical disc removal and interbody fusion for cervical disc syndrome. Bull John Hopkins Hosp. 1955;96(Suppl):223–224. [Google Scholar]
- 34.Robinson RA. Anterior and posterior cervical spine fusion. Clin Orthop. 1964;35:34–62. [PubMed] [Google Scholar]
- 35.Rosenorn J, Hansen EB, Rosenorn MA. Anterior cervical discectomy with or without fusion: a prospective study. J Neurosurg. 1983;59(2):252–255. doi: 10.3171/jns.1983.59.2.0252. [DOI] [PubMed] [Google Scholar]
- 36.Savitz MH. Anterior cervical discectomy without fusion or instrumentation: 25 years’ experience. Mount Sinai J Med. 2000;67(4):314–317. [PubMed] [Google Scholar]
- 37.Savolainen S, Rinne J, Hernesniemi J. A prospective randomized study of anterior single-level cervical disc operations with long-term follow-up: surgical fusion is unnecessary. Neurosurgery. 1998;43(1):51–55. doi: 10.1097/00006123-199807000-00032. [DOI] [PubMed] [Google Scholar]
- 38.Smith GW, Robinson RA. The treatment of certain cervical-spine disorders by anterior removal of the intervertebral disc and interbody fusion. J Bone Joint Surg. 1958;40:607–624. [PubMed] [Google Scholar]
- 39.Sonntag VK, Klara P. Controversy in spine care: is fusion necessary after anterior cervical discectomy? Spine. 1996;21:1111–1113. doi: 10.1097/00007632-199605010-00025. [DOI] [PubMed] [Google Scholar]
- 40.Troyanovich SJ, Stroink AR, Kattner KA, Dornan WA, Gubina I. Does anterior plating maintain cervical lordosis versus conventional fusion techniques? A retrospective analysis of patients receiving single-level fusions. J Spinal Disord Tech. 2002;15:69–74. doi: 10.1097/00024720-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 41.Vaccaro AR, Singh K, Haid R, Kitchel S, Wuisman P, Taylor W, Branch C, Garfin S. The use of bio-absorbable implants in the spine. Spine J. 2003;3(3):227–237. doi: 10.1016/S1529-9430(02)00412-6. [DOI] [PubMed] [Google Scholar]
- 42.Vernon H, Mior S. The neck disability index:a study of reliability and validity. J Manipulat Physiol Ther. 1991;14(7):409–415. [PubMed] [Google Scholar]
- 43.Young WF, Rosenwasser RH. An early comparative analysis of the use of fibular allograft versus autologous iliac crest graft for interbody fusion after anterior cervical discectomy. Spine. 1993;18(9):1123–1124. doi: 10.1097/00007632-199307000-00002. [DOI] [PubMed] [Google Scholar]
- 44.Yue WM, Brodner W, Highland TR. Long-term results after anterior cervical discectomy and fusion with allograft and plating:a 5- to 11-year radiologic and clinical follow-up study. Spine. 2005;30(19):2138–2144. doi: 10.1097/01.brs.0000180479.63092.17. [DOI] [PubMed] [Google Scholar]
- 45.Zoega B, Karholm J, Lind B. Plate fixation adds stability to two-level anterior fusion in the cervical spine. A randomized study using radiosterometry. Eur Spine J. 2000;7(4):302–307. doi: 10.1007/s005860050079. [DOI] [PMC free article] [PubMed] [Google Scholar]