Abstract
To present 58 cystic space-occupying formations of the spinal canal in 53 cases; these formations are called “juxtafacet cysts”. Fifty-Three patients (33 women and 20 men, with an average age of 60.8 years) were evaluated retrospectively by neurosurgery. All of the patients had received simple X-P, computed tomography (CT) and magnetic resonance imaging (MRI) before surgery. The neurological findings were evaluated on admission and in a follow-up review. Surgical intervention was performed on all patients and they underwent gross-total cyst removal. During surgery, the origin of a cyst was well observed. Follow-up data ranged from 6 to 46 months. Patient outcome was graded on a scale of excellent, good, or poor. Histological findings were evaluated. In 53 patients 58 cysts were identified. Four of the patients had multiple cysts. All cysts were associated with mobile spine. Fifty-five cysts were found in the lumbo-sacral region, two cysts were found in the cervico-thoracic region and one cyst in the thoracic region. Forty-two patients presented back pain and 52 patients presented radicular pain. Four patients had a cauda equina syndrome. Sensory disturbance was observed in 24 cases and motor weakness was observed in 21 cases. Claudication was observed in 19 cases. All cases with cervico-thoracic or thoracic cysts presented myelopathy. The duration of these clinical symptoms ranged from 10 days to 10 years. After surgery there was no case of a recurrent cyst during the follow-up period. Thirty-four cases had an excellent outcome, 18 a good outcome, and one a poor outcome. Out of 58 cysts 32 were joint cysts (11 synovial cysts, 21 ganglion cysts). A further 19 were flavum cysts, one was a posterior longitudinal ligament (PLL) cyst and six others were unknown pseudo cysts. In 34 of the cysts we found hemosiderin deposits and in eight amyloid deposits. Present investigation and findings in literature show a clear comparison of these cystic formations and the mobile part of the spine. An anatomical relation to a vertebral joint (“facet”) is only found in some of the cases (32 of 58). Further to that, the name “cyst” is not correct either, because most of the cystic formations are presented without a cell lining on their internal wall and therefore they are pseudo-cystic. We think that these cystic formations should be called “cystic formations of mobile spine” (CYFMOS) rather than “juxtafacet cysts”. A surgical intervention is the best treatment for these cysts if they cause a compression of nerve roots or/and of the spinal cord.
Keywords: Synovial cyst, Pseudo cyst, Ganglion cyst, Juxtafacet cyst, Mobile spine
Introduction
Since the appearance of magnetic resonance imaging (MRI), the diagnostic rates of spinal cystic lesions have increased rapidly. We can experience many spinal cystic lesions in a general clinic, such as the meningeal cyst, the juxtafacet cyst, the arachnoid cyst, etc. In particular, the term “juxtafacet cyst” was initially used by Kao [12, 13] to describe both synovial and ganglion cysts that are adjacent to the facet joint or arise from or grow into the ligament flavum. There are no clinical characteristic features associated with a juxtafacet cyst. But the aetiology is still unclear. On the other hand, in some cases of “juxtafacet cysts” another histological morphology and no anatomical relation to the vertebral joint was found (Table 1). Therefore the term “juxtafacet cyst” may possibly be unsuitable in the near future. We here describe 58 cysts of the spinal canal associated with mobile spine in 53 patients in detail with operative findings and histology. These cysts were so-called “juxtafacet cysts”.
Table 1.
Histological findings in cases of so-called “juxtafacet cyst” in literature
| Synovial cysts | Pseudo-cysts | Unclear: unknown cyst | ||
|---|---|---|---|---|
| Ganglion cysts | Flavum cysts | |||
| Authors | n | N | n | n |
| Abdullah et al. [1] | 3 | – | – | 1 |
| Azzam [2] | – | – | – | 1 |
| Kao et al. [12] | – | 2 | – | |
| Deinsberger et al. [5] | 8 | 5 | 3 | – |
| Eyster and Scott [7] | 11 | – | – | – |
| Finkelstein et al. [9] | 2 | – | – | – |
| Franck et al. [10] | 1 | – | – | – |
| Chimeno et al. [4] | – | 1 | – | |
| Kjerulf et al. [14] | 5 | – | – | – |
| Kornberg [15] | – | 1 | – | – |
| Sabo et al. [18] | 36 | 14 | 2? | – |
| Tatter et al. [19] | 1 | – | – | – |
| Vernet et al. [20] | – | – | 6 | – |
| Yarde et al. [21] | 8 | – | – | – |
| Total | 75 | 23 | 11 | 2 |
Authors are sorted alphabetically. n number of removed cysts
Clinical materials and methods
During the last 14 years, 53 patients with so called “juxtafacet cysts” were evaluated retrospectively in neurosurgical department of the University Hospital of Giessen, Germany. The 53 patients consisted of 33 women and 20 men, with an average age of 60.8 years (range: 17–81 years).
Before surgery, all of the patients had received simple X-P, computed tomography (CT), and magnetic resonance imaging (MRI). The neurological findings were evaluated on admission, and in a follow-up review. Patient outcome was graded on a scale of excellent, good, or poor: An “excellent” outcome meant no further discomfort and return to full activity; “good” meant normal neurological examinations with minimal complaints, for example, back or leg pain; and “poor” meant frequent, for example, back or leg pain with limitation of daily activity and/or neurological deficit. Operative procedures were reviewed. During surgery, the origin of a cyst was well observed. The removed cysts were histologically evaluated.
Results
Cyst location
Fifty-eight space-occupying cysts of the spinal canal were identified. Thirty-five cysts were on the right side, 23 were on the left side. Four patients had multiple cysts (Table 5). Fifty-five cysts were in the lumbo-sacral region, three cysts were at the L2/3 spinal level, 12 cysts were at L3/4, 28 cysts were at L4/5, one cyst was at L5/6, and 11 cysts were at L5/S1 level. Two further cysts were found at the C7/Th1 level, and one cyst was at the Th11/12 level.
Table 5.
Histological and histo-chemical findings of each patient with (so-called) “juxtafacet cyst”
| No | Age | Sex | Cyst location | Left/right | Macroscopic (intraoperative) | Microscopic | |||
|---|---|---|---|---|---|---|---|---|---|
| Joint/flavum/PLL cyst | Intracystic bleeding (+/−) | Synovial/pseudo cyst | Hemosiderin deposit (+/−) | Amyloid deposit (+/−) | |||||
| 1 | 79 | F | L4/5 | Right | Joint | − | Synovial cyst | − | − |
| 2 | 51 | F | L5/S1 | Right | Joint | − | Synovial cyst | − | − |
| 3 | 54 | F | L4/5 | Left | Joint | − | Synovial cyst | − | − |
| 4 | 70 | M | L3/4 | Right | Flavum | − | Pseudo | − | − |
| Left | Flavum | − | Pseudo | − | − | ||||
| 5 | 72 | M | L3/4 | Right | Flavum | − | Pseudo | − | − |
| Left | Flavum | − | Pseudo | − | − | ||||
| 6 | 64 | F | L5/S1 | Left | Joint | − | Synovial cyst | − | − |
| 7 | 46 | M | L5/S1 | Right | Joint | − | Synovial cyst | − | − |
| 8 | 53 | F | L4/5 | Right | Joint | − | Ganglion cyst | − | − |
| 9 | 50 | M | L5/S1 | Left | Joint | − | Ganglion cyst | − | − |
| 10 | 66 | F | L4/5 | Left | Joint | − | Ganglion cyst | + | − |
| 11 | 53 | F | L4/5 | Right | Joint | − | Ganglion cyst | − | − |
| 12 | 62 | F | Th11/12 | Left | Joint | − | Synovial cyst | + | − |
| 13 | 62 | M | L4/5 | Left | Joint | − | Ganglion cyst | − | − |
| 14 | 69 | F | L4/5 | Right | Joint | + | Synovial cyst | + | + |
| 15 | 53 | M | L2/3 | Right | Joint | − | Synovial cyst | + | − |
| 16 | 51 | F | L4/5 | Right | Joint | − | Ganglion cyst | − | − |
| 17 | 67 | M | L4/5 | Right | Flavum | − | Pseudo | + | − |
| 18 | 51 | M | L5/S1 | Right | Joint | − | Ganglion cyst | + | − |
| 19 | 69 | F | L5/S1 | Left | Joint | − | Ganglion cyst | + | − |
| 20 | 52 | F | L4/5 | Left | Joint | − | Ganglion cyst | − | − |
| 21 | 60 | F | L2/3 | Right | Flavum | − | Pseudo | + | − |
| L3/4 | Right | Joint | − | Synovial cyst | + | − | |||
| 22 | 60 | M | L3/4 | Right | Joint | − | Ganglion cyst | + | − |
| 23 | 51 | M | L4/5 | Right | Joint | − | Ganglion cyst | + | − |
| 24 | 58 | M | L4/5 | Right | Unclear | − | Pseudo | + | − |
| 25 | 81 | F | L2/3 | Right | Unclear | Yellowish fluid | Pseudo | + | − |
| 26 | 74 | F | C7/Th1 | Right | Joint | − | Ganglion cyst | + | − |
| 27 | 59 | F | L4/5 | Left | Joint | − | Ganglion cyst | + | + |
| 28 | 72 | M | L4/5 | Left | Flavum | + | Pseudo | + | + |
| 29 | 58 | M | C7/Th1 | Right | Joint | + | Synovial cyst | − | − |
| 30 | 67 | F | L3/4 | Right | Unclear | − | Pseudo | + | − |
| L3/4 | Left | Unclear | − | Pseudo | + | − | |||
| L4/5 | Left | Unclear | − | Pseudo | + | − | |||
| 31 | 54 | F | L5/S1 | Right | Joint | − | Ganglion cyst | + | − |
| 32 | 79 | F | L4/5 | Left | Joint | − | Ganglion cyst | + | − |
| 33 | 52 | F | L4/5 | Right | Joint | − | Ganglion cyst | − | − |
| 34 | 48 | M | L3/4 | Right | Flavum | Yellowish fluid | Pseudo | + | + |
| 35 | 47 | F | L5/S1 | Right | Joint | − | Ganglion cyst | + | − |
| 36 | 76 | F | L4/5 | Left | Flavum | Yellowish fluid | Pseudo | − | − |
| 37 | 53 | F | L5/6 | Right | Flavum | − | Pseudo | + | − |
| 38 | 52 | F | L4/5 | Right | Joint | − | Ganglion cyst | − | − |
| 39 | 55 | F | L4/5 | Left | Joint | − | Ganglion cyst | + | + |
| 40 | 72 | F | L3/4 | Right | Flavum | + | Pseudo | + | − |
| 41 | 57 | F | L4/5 | Right | Joint | − | Ganglion cyst | + | − |
| 42 | 62 | M | L4/5 | Left | Flavum | − | Pseudo | − | − |
| 43 | 77 | F | L5/S1 | Left | Flavum | − | Pseudo | − | − |
| 44 | 74 | F | L3/4 | Left | Flavum | + | Pseudo | + | + |
| 45 | 70 | M | L4/5 | Right | Joint | − | Ganglion cyst | + | − |
| 46 | 66 | F | L4/5 | Right | Flavum | − | Pseudo | + | − |
| 47 | 66 | M | L4/5 | Right | Unclear | − | Pseudo | + | + |
| 48 | 71 | F | L3/4 | Left | Flavum | + | Pseudo | + | + |
| 49 | 75 | F | L4/5 | Right | Flavum | + | Pseudo | + | − |
| 50 | 57 | M | L4/5 | Left | Joint | − | Synovial cyst | − | − |
| 51 | 60 | F | L5/S1 | Left | Flavum | − | Pseudo | + | − |
| 52 | 51 | M | L4/5 | Right | Flavum | − | Pseudo | − | − |
| 53 | 17 | M | L5/S1 | Right | PLL | + | Pseudo | − | − |
Findings and symptoms
Forty-two cases (79.2%) presented back pain and 52 cases (98.1%) presented radicular pain. One case had no pain. Four cases had cauda equina syndrome. Sensory disturbance in a radicular distribution was observed in 24 cases, and motor weakness in a radicular distribution was observed in 21 cases. Radicular claudication and claudication associated with cauda equina syndrome were observed in 19 cases. All cases of cervico-thoracic or thoracic lesion presented myelopathy (Table 2). The duration of these clinical symptoms ranged from 10 days to 10 years (17.66 months). Most of the patients (n = 48) had clear accompanying degenerative changes of the spine shown by X-P, CT or/and MRI. Four of the cases were associated with a lumbo-sacral (L5/S1) disc herniation and one case was associated with degenerative spinal instability also at L5/S1 level.
Table 2.
Clinical signs and findings in cases with “juxtafacet cysts”
| Symptom | n |
|---|---|
| Back pain | 42 |
| Radicular pain | 52 |
| Claudication | 19 |
| Sensory disturbances | 24 |
| Motor disturbances | 21 |
| Cauda equina syndrome | 4 |
| Myelopathy | 3 |
n number of patients
Treatment
In all patients surgical intervention was performed (Table 3). The cases associated with lumbar disc herniation also received a discectomy. Hemilaminotomy was performed in 41 cases (in three cases, with discectomy). Hemilaminectomy was performed in six cases. Bilateral laminotomy was performed in three cases (in one case, with discectomy). We performed laminectomy in two cases. The patient with the degenerative instability at L5/S1 level was treated with a posterior lumbar inter-body fusion (PLIF). Only in one case, lateral foraminotomy was performed because the cyst was located in ventro-lateral joint of L5/S1. All of the patients underwent gross-total cyst removal, which was combined with a partial arthrectomy. All surgical resected cysts were subjected to histological examination.
Table 3.
Surgical treatment in cases with “juxtafacet cysts”
| Treatment | n |
|---|---|
| Hemilaminotomy (three cases with discectomy) | 41 |
| Foraminotomy | 1 |
| Hemilaminectomy | 6 |
| Laminectomy (one case with PLIF) | 2 |
| Bilateral laminotomy (one case with discectomy) | 3 |
| Total | 53 |
n number of patients
Follow-up data
Follow-up data were available in all cases and ranged from 12 to 46 months (mean 14.4 months). One patient was re-operated because of lumbar disc herniation 2 years after the initial operation. There was no case of a recurrent spinal epidural cyst during the follow-up periods. Thirty-four patients (64.2%) had an excellent outcome, 18 (34.0%) a good outcome, and one patient a poor outcome. This patient had a history of severe myelopathy. In 17 cases postoperative MRI investigation after several (10–16) months was necessary, because these patients had low back pain. In these patients no recurrent cyst was found by “normal” postoperative MRI findings. None of the other patients had clinical signs of a recurrent cyst in the postoperative follow-up period.
Morphological findings
Macroscopic findings (intraoperative findings)
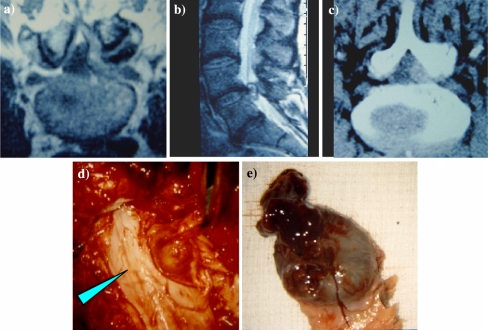
We confirmed the origin of a cyst, in as much detail as possible, during surgery (Table 4). Thirty-two joint cysts were intra-operatively evaluated, and after surgery this diagnosis was verified using histological methods. Nineteen of the other cysts were flavum cysts, another one was posterior longitudinal ligament (PLL) cyst, and the last six were unknown (unclear) cysts. There were 11 cysts with signs of an intracystic hemorrhage (eight cysts presented an old haematoma (Fig. 1, Table 5), in three further cysts, the fluid was yellowish color). And in those cases, two were joint cysts, seven were flavum cysts, one was a PLL cyst, and one was an unknown cyst.
Table 4.
Macroscopic and microscopic findings of resected cysts
| Macroscopic findings | n | Microscopic findings | n |
|---|---|---|---|
| Flavum cyst | 19 | Synovial cyst | 11 |
| Joint cyst | 32 | Ganglion cyst | 21 |
| Unclear cyst | 6 | Other pseudo cyst | 26 |
| PLL | 1 | Hemosiderin deposits | 34 |
| Total | 58 | Amyloid deposits | 8 |
| Total | 58 |
n number of the cysts
Fig. 1.
Flavum cyst with intra-cystic old haematoma, level L 4/5 (case number 28, male, 72 years). a MR-Imaging axial cut, b leftsided paramedian sagittal cut, c CT-Imaging axial cut, d intraoperative macroscopic findings (arrow show the cyst), and e resected flavum cyst with intra-cystic haematoma
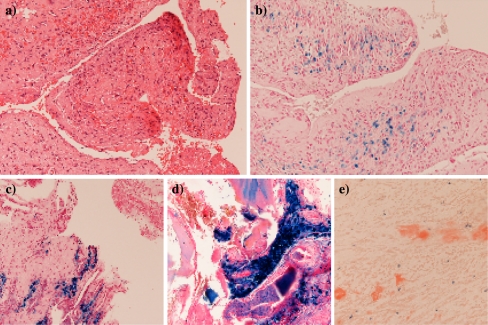
Microscopic findings
Two typical cysts were found based on microscopic histological examination (Table 4). One was a “synovial cyst,” having a synovial lining membrane; one was a “pseudo cyst,” having no synovial lining membrane. “Pseudo cysts” from joint were identified as “ganglion cysts”. Of all the surgically resected joint cysts (n = 32), 11 were synovial cysts, 21 were ganglion cysts. All 19 flavum cysts were “pseudo cysts”. The PLL cyst and all of the six unknown cysts were “pseudo cysts”, too.
Histochemical and histological findings are detailed reported in Table 5. Hemosiderin deposits were shown in 34 cysts, which were caused by old intra-cystic hemorrhage. Of all the cysts with hemosiderin deposits, four were synovial cysts, 13 were ganglion cysts, and 11 were flavum cysts.
All of the unknown cysts had hemosiderin deposits. On the other hand, amyloid deposits were shown in eight cysts, which were suspected of severe tissue degeneration. Of all the cysts with amyloid deposits, one was a synovial cyst, two were ganglion cysts, four were flavum cysts and one was an unknown cyst (Table 5; Fig. 2).
Fig. 2.
Histological findings in “juxtafacet” cysts: a, b Synovial cyst with focally detectable synovial cells covering a stroma with vascular granulation tissue. b In the granulation tissue Prussian blue-positive hemosiderin deposits can be seen. c Flavum cyst with focal Prussian blue-positive hemosiderin deposits in the wall of the pseudocyst. d Flavum cyst with extensive Prussian blue-positive hemosiderin deposits in the wall and in the “lumen” of the pseudocyst due to old intracystic bleeding. e Flavum cyst with focal Congo red-positive amyloid deposits
Discussion
Kao [12, 13] was the first to use the term “juxtafacet cyst”. To start with, the correctness of this term must be discussed. In the strict sense of word, “juxtafacet cyst” conventionally includes a cyst involving no joint, namely facet (such as a flavum cyst, for example). Therefore, some difficulty may arise in calling this cyst “facet cyst”. Certainly, many spinal cysts involving a joint have appeared in the relevant literature in the past as well as in our results. It is, however, required to estimate the pathogenesis of these cysts here. There are no previous reports, which presented an appearance of this cyst in a region except for the mobile spine. Th2 ∼ Th10 spines which greatly participate in holding ribs and forming the thorax are not basically referred to as “mobile spine”. It is thus considered that an exercise loading on the spine is greatly involved in the pathogenesis of these cysts similar to the mechanism to a disc herniation. This occurs frequently as result of a degenerative lumbar disc lesion. It can be applied to the concept that these cysts frequently occur in consequence of a lumbar spine stress (exercise loading) in addition to a degenerative lesion of the soft lumbar tissue [2–4, 7, 8, 14, 15, 18, 19, 21]. Though in fact it is most frequently the case that the dynamics of spine have the greatest exercise loading on a joint, some exercise loading is also given on its surrounding tissues such as PLL and ligamentum flavum without problems or tissue damage. As mentioned above, we think this cyst should be called “cystic formation of mobile spine” (CYFMOS) rather than “juxtafacet cyst” in the more strict sense of word.
Based on the perioperative findings, a classification of these cysts by different sites involved is possible. According to their location, they can be classified into three groups, joint (facet) cyst, flavum cyst and PLL cyst [1, 5, 9, 20]. It is of course true that the location of the cysts is hardly identified in some cases depending on the size of the resected cyst as seen in our report. However, these three locations seem to be appropriate as an origin of the cysts [6, 10, 16, 17]. Concerning the next step of histopathological classification, only two types are roughly considered, true cysts and pseudo cysts. A true cyst, so-called synovial cyst, has a synovial lining membrane. Based on this finding, a synovial cyst seems to be generated from synovium of facet. In our report as well, no synovial membrane could be found except in joint cysts. Some authors, however, described a synovial cyst originating from a ligamentum flavum [1, 11]. According to their reports, a synovial cyst is formed as a result of advanced degeneration of ligamentum flavum. In our opinion, it is not possible for a synovial cyst to originate from ligamentum flavum or PLL, which have no synovial membranes. In our study as well, no case was presented with a flavum cyst or PLL cyst, which are classified into synovial cyst histopathologically [18, 21]. In contrast to this, it is conceivable that pseudo cysts are a result of advanced degeneration of soft spinal tissue or of various performed joint cysts. A pseudo cyst (ganglion) may also have been generated from a synovial cyst after degeneration or destruction of synovial lining membrane. In consequence, it is naturally considered that flavum cysts and PLL cysts originated from degenerated ligamentum flavum and PLL, respectively are due to a chronic trauma, because: (1) a pseudo cyst was detected in almost all cases in which an amyloid deposit was found, and (2) a hemosiderin deposit was also detected in all cases in which an amyloid deposit was found (Tables 4 and 5). Namely, it seems that amyloid is especially deposit in the course of the degeneration progress. In response to greater exercise loading and more advanced tissue degeneration, hemorrhagic episodes may occur in a repeated manner (hemosiderin deposits and intra-cystic haematoma), and also amyloid may deposit in the soft tissue [10, 18, 19, 21]. Finally, no specific clinical symptoms are found in any of these cases. Symptoms may appear due to direct compression on so-called nerve root or spinal cord. The treatment of first choice against this disease is the surgical intervention as stated in previous reports [18], and the postoperative outcome is generally very good. Though a relapsed episode of this cyst is reported by some authors [18], it is rather a rare case.
Conclusion
We presented 58 cysts associated with mobile spine in 53 cases.
We think that these cysts should be called “cystic formations of mobile spine” (=CYFMOS) rather than “juxtafacet cysts” in the stricter sense of word.
A surgical intervention is the best treatment strategy for this cyst.
References
- 1.Abdullah AF, Chambers RW, Daut DP. Lumbar nerve root compression by synovial cysts of the ligamentum flavum. J Neurosurg. 1984;60:617–620. doi: 10.3171/jns.1984.60.3.0617. [DOI] [PubMed] [Google Scholar]
- 2.Azzam CJ. Midline lumbar ganglion/synovial cyst mimicking an epidural tumor: case report and review of pathogenesis. Neurosurgery. 1988;23:232–234. doi: 10.1227/00006123-198808000-00019. [DOI] [PubMed] [Google Scholar]
- 3.Baum JA, Hanley EN., Jr Intraspinal synovial cyst simulating spinal stenosis. A case report. Spine. 1986;11:487–489. doi: 10.1097/00007632-198606000-00018. [DOI] [PubMed] [Google Scholar]
- 4.Chimento GF, Ricciardi JE, Whitecloud TS. Intraspinal extradural ganglion cyst. J Spinal Disord. 1995;8:82–85. doi: 10.1097/00002517-199502000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Deinsberger W, Schindler C, Boeker DK. Juxta-facet cysts. Pathogenesis, clinical symptoms and therapeutic management. Nervenarzt. 1997;68:825–830. doi: 10.1007/s001150050200. [DOI] [PubMed] [Google Scholar]
- 6.Epstein NE, Hollingsworth R. Synovial cyst of the cervical spine. J Spinal Disord. 1993;6:182–185. [PubMed] [Google Scholar]
- 7.Eyster EF, Scott WR. Lumbar synovial cysts: report of eleven cases. Neurosurgery. 1989;24:112–115. doi: 10.1097/00006123-198901000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Feldman R, McCulloch J. Juxta facet cysts of the lumbar spine. Neuroorthopedics. 1987;4:31–35. [Google Scholar]
- 9.Finkelstein SD, Sayegh R, Watson P, Knuckey N. Juxta-facet cysts. Report of two cases and review of clinicopathologic features. Spine. 1993;18:779–782. doi: 10.1097/00007632-199305000-00020. [DOI] [PubMed] [Google Scholar]
- 10.Franck JI, King RB, Petro GR, Kanzer MD. A posttraumatic lumbar spinal synovial cyst. J Neurosurg. 1987;66:293–296. doi: 10.3171/jns.1987.66.2.0293. [DOI] [PubMed] [Google Scholar]
- 11.Giannini C, Scheithauer BW, Wenger DE, Unni KK. Pigmented villonodular synovitis of the spine: a clinical, radiological, and morphological study of 12 cases. J Neurosurg. 1996;84:592–597. doi: 10.3171/jns.1996.84.4.0592. [DOI] [PubMed] [Google Scholar]
- 12.Kao CC, Uihlein A, Bickel WH, Soule EH. Lumbar intraspinal extradural ganglion cyst. J Neurosurg. 1968;29:168–172. doi: 10.3171/jns.1968.29.2.0168. [DOI] [PubMed] [Google Scholar]
- 13.Kao CC, Winkler SS, Turner JH. Synovial cyst of spinal facet. Case report. J Neurosurg. 1974;41:372–376. doi: 10.3171/jns.1974.41.3.0372. [DOI] [PubMed] [Google Scholar]
- 14.Kjerulf TD, Terry DW, Jr, Boubelik RJ. Lumbar synovial or ganglion cysts. Neurosurgery. 1986;19:415–420. doi: 10.1097/00006123-198609000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Kornberg M. Nerve root compression by a ganglion cyst of the lumbar annulus fibrosus. A case report. Spine. 1995;20:1633–1635. doi: 10.1097/00007632-199507150-00013. [DOI] [PubMed] [Google Scholar]
- 16.Onofrio BM, Mih AD. Synovial cysts of the spine. Neurosurgery. 1988;22:642–647. doi: 10.1097/00006123-198804000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Patel SC, Sanders WP. Synovial cyst of the cervical spine: case report and review of the literature. AJNR. 1988;9:602–603. [PMC free article] [PubMed] [Google Scholar]
- 18.Sabo RA, Tracy PT, Weinger JM. A series of 60 juxtafacet cysts: clinical presentation, the role of spinal instability, and treatment. J Neurosurg. 1996;85:560–565. doi: 10.3171/jns.1996.85.4.0560. [DOI] [PubMed] [Google Scholar]
- 19.Tatter SB, Cosgrove GR. Hemorrhage into a lumbar synovial cyst causing an acute cauda equina syndrome. Case report. J Neurosurg. 1994;81:449–452. doi: 10.3171/jns.1994.81.3.0449. [DOI] [PubMed] [Google Scholar]
- 20.Vernet O, Fankhauser H, Schnyder P, Deruaz JP. Cyst of the ligamentum flavum: report of six cases. Neurosurgery. 1991;29:277–283. doi: 10.1097/00006123-199108000-00021. [DOI] [PubMed] [Google Scholar]
- 21.Yarde WL, Arnold PM, Kepes JJ, O’Boynick PL, Wilkinson SB, Batnitzky S. Synovial cysts of the lumbar spine: diagnosis, surgical management, and pathogenesis. report of eight cases. Surg Neurol. 1995;43:459–465. doi: 10.1016/0090-3019(95)80090-4. [DOI] [PubMed] [Google Scholar]