Abstract
Fusion of cervical spine in kyphotic alignment has been proven to produce an acceleration of degenerative changes at adjacent levels. Stand-alone cages are reported to have a relatively high incidence of implant subsidence with secondary kyphotic deformity. This malalignment may theoretically lead to adjacent segment disease in the long term. The prospective study analysed possible risk factors leading to cage subsidence with resulting sagittal malalignment of cervical spine. Radiographic data of 100 consecutive patients with compressive radiculo-/myelopathy due to degenerative disc prolapse or osteophyte formation were prospectively collected in those who were treated by anterior cervical discectomy and implantation of single type interbody fusion cage. One hundred and forty four implants were inserted altogether at one or two levels as stand-alone cervical spacers without any bone graft or graft substitute. All patients underwent standard anterior cervical discectomy and the interbody implants were placed under fluoroscopy guidance. Plain radiographs were obtained on postoperative days one and three to verify position of the implant. Clinical and radiographic follow-up data were obtained at 6 weeks, 3 and 6 months and than annually in outpatient clinic. Radiographs were evaluated with respect to existing subsidence of implants. Subsidence was defined as more than 2 mm reduction in segmental height due to implant migration into the adjacent end-plates. Groups of subsided and non-subsided implants were statistically compared with respect to spacer distance to the anterior rim of vertebral body, spacer versus end-plate surface ratio, amount of bone removed from adjacent vertebral bodies during decompression and pre- versus immediate postoperative intervertebral space height ratio. There were 18 (18%) patients with 19 (13.2%) subsided cages in total. No patients experienced any symptoms. At 2 years, there was no radiographic evidence of accelerated adjacent segment degeneration. All cases of subsidence occurred at the anterior portion of the implant: 17 cases into the inferior vertebra, 1 into the superior and 1 into both vertebral bodies. In most cases, the process of implant settling started during the perioperative period and its progression did not exceed three postoperative months. There was an 8.7° average loss of segmental lordosis (measured by Cobb angle). Average distance of subsided intervertebral implants from anterior vertebral rim was found to be 2.59 mm, while that of non-subsided was only 0.82 mm (P < 0.001). Spacer versus end-plate surface ratio was significantly smaller in subsided implants (P < 0.001). Ratio of pre- and immediate postoperative height of the intervertebral space did not show significant difference between the two groups (i.e. subsided cages were not in overdistracted segments). Similarly, comparison of pre- and postoperative amount of bone mass in both adjacent vertebral bodies did not show a significant difference. Appropriate implant selection and placement appear to be the key factors influencing cage subsidence and secondary kyphotisation of box-shaped, stand-alone cages in anterior cervical discectomy and fusion. Mechanical support of the implant by cortical bone of the anterior osteophyte and maximal cage to end-plate surface ratio seem to be crucial in the prevention of postoperative loss of lordosis. Our results were not able to reflect the importance of end-plate integrity maintenance; the authors would, however, caution against mechanical end-plate damage. Intraoperative overdistraction was not shown to be a significant risk factor in this study. The significance of implant subsidence in acceleration of degenerative changes in adjacent segments remains to be evaluated during a longer follow-up.
Keywords: Cervical vertebrae surgery, Spinal fusion, Equipment failure analysis, Postoperative complications, Subsidence
Introduction
Stand-alone interbody fusion cages represent an alternative for anterior cervical fusion in the treatment of cervical degenerative disc disease. The reason for development of similar fusion device was the avoidance of complications arising from the use of autologous bone graft. Cage-assisted anterior cervical discectomy and fusion (ACDF) has proven to be a safe and effective procedure in available studies. Clinical outcomes have been encouraging in one- and two-level procedures [4, 9–11, 13, 15] and reliability was shown even in three- and four-level surgeries [5]. Cervical intervertebral disc replacement by means of stand-alone cage can restore physiologic disc height, provide immediate load bearing support to the anterior column [6] and may facilitate arthrodesis.
On the other hand, there is also evidence documenting relatively frequent complications in stand-alone cage-assisted ACDF. The most commonly discussed complication seems to be cage subsidence. In a small series of eight patients Gercek et al. [3] reported even 62.5% rate of settled rectangular cages and Bartels et al. [1] recently reported the incidence of 29.2% in 69 patients. The subject of subsidence tendency has also been analysed in cadaver laboratory testing [16, 17]. However, results from larger clinical studies are still lacking and direct correlation of the complication with the anatomical parameters of cervical spine also remains unclear. The authors have experience with more than 300 cervical spine surgeries using different types of rectangular (box-shaped) stand-alone cages. The experience left a deep conviction that implant subsidence may arise either from suboptimal surgical technique, including inadequate preparation of the adjacent end-plates and intraoperative segmental overdistraction or from inappropriate cage selection with biomechanically unsound positioning.
We, therefore, conducted a prospective study of one hundred consecutive patients, operated on by a single type of stand-alone cage with specific emphasis on subsidence behaviour. The authors calculated the incidence of implant settling, analysed its effect on local cervical spine anatomy in sagittal plane and also tried to evaluate the influence of selected local factors on the tendency of the device to migrate through the adjacent vertebral end-plates.
Material and methods
We conducted a prospective collection of clinical and radiological data in patients undergoing ACDF, where interbody fusion in one or two motion segments was facilitated by subsequent insertion of titanium box-shaped cage Cespace® (Aesculap, Germany) (Fig. 1). One hundred consecutive patients who completed at least 2-year postoperative follow-up were qualified for the analysis. The age of patients ranged from 29 to 63 years (average 47.8 years, mean age 49), 50% male, 50% female. Altogether, 144 implants were inserted in this cohort (56 single and 88 two-level procedures). Anatomical distribution of discectomies is depicted in graph 1. All patients initially presented with radiculopathy and/or myelopathy due to concordant disc herniation, osteophyte formation or posterior longitudinal ligament hypertrophy. Patients previously treated by anterior cervical fusion or by another surgical procedure as well as those, who subsequently underwent posterior decompression for persistent circumferential stenosis, were excluded from the study. Patients with known osteoporosis or at risk of it as a consequence of another treatment (e.g. corticosteroid therapy) or disease (e.g. renal failure) were stabilised by plate and bicortical screws and were also excluded. Postoperative follow-up time ranged from 24 to 62 months (average 43 months).
Fig. 1.
Cervical intervertebral device evaluated in this study. The Cespace® has a rectangular box design with central opening that can be filled by cancelous bone or bone substitute. The porous coating of both superior and inferior aspects converging in 5° should facilitate bony ingrowth
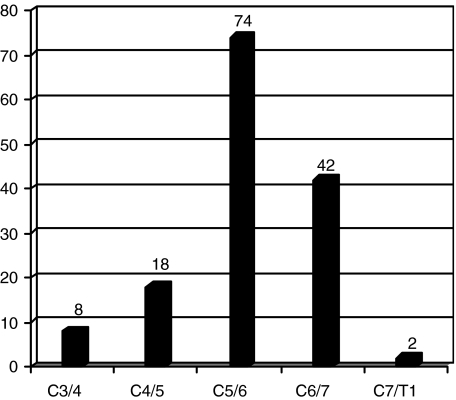
Graph 1.
Anatomical distribution of implants in the 100 consecutive patients
Surgical technique
All patients underwent a standard anterior cervical discectomy through a right-sided anterolateral retropharyngeal approach. Vertebral body distractors were placed and both the disc material and posterior longitudinal ligament were removed. Anterior osteophytes were left intact removing just eventual marginal portion in the plane of the end-plate while the posterior ones were cleared after the discectomy and resection of the posterior longitudinal ligament. Adequate decompression of neural structures was verified using a blunt probe. During the discectomy, special attention was paid to avoiding damage to the bony layer of both adjacent end-plates. The size of the implant was determined by cage trials and lateral fluoroscopy. Both the end-plates were subsequently sharply punctured by a fastigiated metal instrument in their centre part (decortication) and the cage inserted without any bone graft or graft substitute. All patients were kept in a semi-rigid collar until the first postoperative day and then mobilised without an external orthosis.
Radiological evaluation
Plain antero-posterior and lateral radiographs were obtained on the first and third postoperative days. The second set and all subsequent films were supplemented by a lateral flexion–extension view. These films were also taken 6 weeks, 3 and 6 months after surgery and then annually. All lateral radiographs were performed in standardized sitting positions. The patients were sitting at the stool with arms hanging down loosely or with applied traction in order to display the cervico-thoracic area if necessary. The position of the head was upright with horizontal gaze. The reproducibility of our radiographs was obtained by the standardized source-to-image and object-to-image receptor (cassette) distance. Subsidence at the radiographs was defined as cage migration of 3 mm or more into the adjacent vertebral body. The migration along the superior and/or inferior end-plates was labelled as settling of the implant. Any observed change in local anatomical relationships as seen in sagittal plane was measured using Cobb angles. For these measurements, lateral radiographs performed on the first postoperative day and at 6 months were used (Fig. 2).
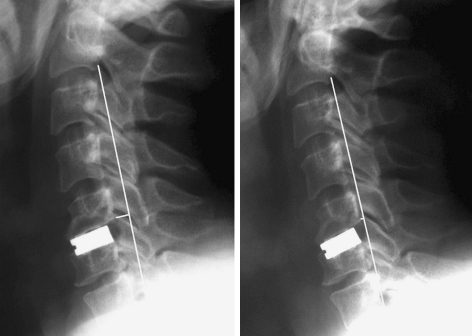
Fig. 2.
An illustrative case of implant subsidence in a 51-year-old man with C5/6 degenerative disc disease who underwent a discectomy with stand-alone intervertebral cage. Comparison of postoperative lateral study with 6-month radiograph demonstrates kyphotic malalignment at the operated segment together with straightening of cervical lordosis
The following anatomical data were evaluated as possible risk factors for subsidence:
Distance of the implant from the anterior rim of the cranial vertebra;
Intraoperative distraction of the involved segment;
Amount of bone material removed from adjacent vertebral bodies during the decompression;
Relative size of the contact area of the implant to the surface of the contiguous end-plate.
The above measurements and ratio calculations are illustrated in Fig. 3. All measurements were obtained in collaboration with an independent radiologist.
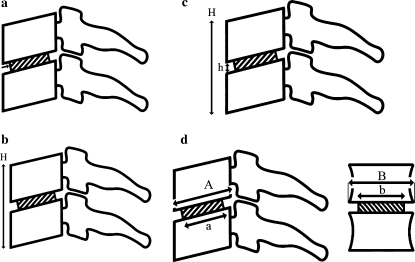
Fig. 3.
a Distance of the implant to the anterior rim of the cranial vertebral body measurement. b Intraoperative distraction of motion segment was calculated from postoperative (post H) and preoperative (pre H) segmental height: intraoperative distraction = (post H/pre H) × 100%. c Intraoperative diminution of segmental bone material was assed by post- and preoperative quotient of the segmental height (H) reduced by intervertebral space height (h): segmental bone material reduction = [post (H−h)/pre (H−h)] × 100%. d Assessment of relative interface contact area was carried out on preoperative and postoperative AP and lateral radiographs. It was calculated as a proportion of cage interface area (a × b) from the end-plate surface (A × B) area: relative interface contact area = (a × b/A × B) × 100%
Statistical analysis
For statistical analysis the numerical results were processed using t test at 95% confidence interval (P = 0.05).
Results
Nineteen (13.2%) out of 144 inserted cages in 18 (18%) patients were found to have subsided according to our criteria. A total of 8 out of 55 single-level and 11 out of 44 two-level cages showed evidence of settling. The characteristics of patients with subsided implants are described in Table 1. In the majority of cases (ten cages, 52.6%), subsidence was already apparent from the radiographs taken during the perioperative period (until postoperative day 3). The rest of the cases were apparent at the 6-week follow-up. The degree of device impaction showed no evidence of progression beyond 3 months. There were also intervertebral ossifications mimicking subsidence leading to intervertebral bone bridging in long term. All appeared clearly on the films more than 6 months after the surgery in both complicated and non-complicated implants. These morphological changes, however, did not cause reduction in the segmental height, did not affect sagittal alignment and were not classified as a subsidence.
Table 1.
Demographic and anatomical characteristics, localisation and loss of segmental lordosis in subsided implants
| Parameter | |
|---|---|
| Age at the time of surgery (average/mean/extent) | 51.2 years/51/73 |
| Gender ratio (male:female) | 2.5:1 |
| Level of subsidence | |
| C5/6 | 10 |
| C6/7 | 9 |
| Incidence of settling in | |
| One-level fusions | 14.5% (8 cages) |
| Two-level fusions | 12.5% (11 implants) |
| Site of device subsidence | |
| Anterior into the superior vertebra | 1 |
| Anterior into the inferior vertebra | 17 |
| Anterior superior + inferior vertebra | 1 |
| Loss of segmental lordosis 6 months after the surgery measured by Cobb angle (average/mean/extent) | 8.7°/9°/5°–17° |
All subsided implants did so at the ventral portion, mostly across the superior end-plate of caudal vertebra (17 implants, 89.5%): one cage migrated into the caudal endplate of cranial vertebra (5.3%) and one simultaneously into both adjacent vertebral bodies (5.3%).
Cage subsidence resulted in sagittal imbalance in all cases. The average segmental Cobb angle change was measured as high as 8.7° (range 5–13°, mean change 9°). This alteration was accompanied by straightening of cervical lordosis, although no case of complete curve reversal (global cervical kyphosis) was observed in our study. During the 2-year follow-up, there were no radiographic signs of progressive degenerative changes in any of the adjacent segments. Furthermore, no patient in this cohort underwent another surgical procedure during the follow up. Fusion rate comparison was not the subject of this study; however, subsidence did not interfere with bone fusion rates.
The average distance of the implant from anterior rim of the superior vertebral body was 2.59 mm (range 0–4 mm, mean distance 2.5 mm) in subsided implants (group A) and 0.81 mm (range 0–6 mm, mean distance 0 mm) in implants without migration (group B). This difference was statistically significant (P < 0.001). A comparison of the ratios of the implant surface area to the upper end-plate surface area revealed significantly (P < 0.001) smaller numbers in the group A versus group B, 54.1% (range 36–76.5%, mean ratio 55%) versus 62.3% (range 38–89.5%, mean 62.4%), respectively. The degree of distraction was assessed by comparing post- and pre-operative disc space heights and this ratio was expressed in percentage. There was no statistically significant difference (P = 0.780) between group A and group B implants. The ratios were 152% (range 100–233%, mean ratio 150%) and 170% (range 100–400%, mean ratio 150%), respectively. Finally, there was no difference between the pre- and post-operative ratio of the bone mass in both adjacent vertebral bodies with 99% (range 83–100%) in implants belonging to the group A and 97% (range 83–100%, mean 100%) in the group B (P = 0.233).
Discussion
Despite the fact that migration of cages into the adjacent end-plates did not change subjective or clinical status in any of our patients during short-term follow-up, this morphological complication should not be taken lightly. The local loss of cervical lordosis is deemed to be a risk factor contributing to progression of degenerative changes in adjacent segments [7]. Mechanisms by which kyphotic malalignment contributes to accelerated degenerative process may involve both the change of dynamic kinematics of cervical spine [12] and increased biomechanical stress on the anterior vertebral elements in neighbouring segments. Progression of structural changes at adjacent segments may lead to re-operation during the long-term follow-up, hence the importance of analysis of the data and subsequent stress given on prevention of stand-alone fusion device subsidence.
Proper end-plate preparation during segmental decompression seems to play a significant role in implant subsidence. Fürderer et al. [2], in their biomechanical study on bovine spine specimens compared subsidence tendency of cervical interbody implants of different designs. In rectangular implants, they documented higher resistance to axial loading as long as the end-plate remained intact. Therefore, intra-operative preparation of the intervertebral space should find a balance between two goals: (a) to maintain a good mechanical condition of the end-plates (subsidence prevention) and (b) to allow sufficient vascular ingrowth into the space that is intended to be osteo-integrated (fusion induction). It is relatively controversial how to achieve those two goals at the same time because some portion of the end-plate needs to be removed to obtain bony fusion and yet excessive removal may risk subsequent subsidence. In biomechanical, destructive compression test [8], a centrally located point of decortication was documented to be mechanically superior and in our series, multiple central perforations seem to be sufficient to initiate implant osteointegration. Our results were not able to reflect the importance of end-plate integrity maintenance as no significant difference was found between adjacent vertebral body bone mass between subsided and non-subsided groups.
It is well known that mechanical strength of bone increases as bone mineral density (BMD) increases. Therefore, BMD of the vertebral body may be of importance in predicting mechanical strength of the cage-end-plate interface [8]. The anterior osteophyte represents an area of cervical vertebral body with superior BMD that may give optimal biomechanical support to the interbody implant. The advantage of biomechanical support conducted by anterior osteophyte becomes apparent, especially when majority of the subsidence is localized ventrally. This assumption was confirmed in our study when higher distance of the implant from the anterior tip of the vertebral body positively correlated with incidence of subsidence. In case of anterior osteophyte finding at the operated segment, the authors would suggest removing just marginal portion at the plane of end-plate to obtain sufficient access to the intervertebral space. Dense cortical bone of the osteophyte should be left in order to prevent implant subsidence.
Also the size of contact area of the cage-end-plate interface may play an important role in prevention of cage subsidence. Larger contact area provides higher mechanical resistance. Our results proved this hypothesis when subsided implants were shown to be significantly smaller as compared to non-complicated prostheses.
Last of the analysed risk factors was the intra-operative intervertebral space distraction. In a cadaveric, biomechanical study, Truumees et al. [14] demonstrated that larger interbody grafts resulted in significantly higher distractive forces during the insertion. Larger distraction forces, on the other hand, caused higher static compression forces on an intervertebral implant. Intraoperative overdistraction together with larger intervertebral device could thus potentially be associated with higher subsidence tendency. This tendency, however, has not been proven in our study since there was no difference between the subsided and non-subsided groups in terms of disc space distraction.
Conclusion
Subsidence of rectangular, stand-alone cages in anterior cervical fusion was found in a significant number of patients in this study. The migration of the device into the adjacent vertebral body was associated with segmental loss of lordosis. Despite the kyphotisation seen at the involved disc levels, the overall alignment between C2 and C7 did not change significantly. Both, position of the implant within the disc space and its size relative to the endplate, influenced the risk of subsequent subsidence. Our results were not able to reflect the importance of end-plate integrity maintenance and the tendency to develop subsidence in intra-operatively over-distracted segments has not been proven. Device impaction was asymptomatic in all patients but a longer follow-up is needed to determine whether implant subsidence results in progression of degenerative process in adjacent cervical segments.
References
- 1.Bartels RH, Donk RD, Feuth T. Subsidence of stand-alone cervical carbon fiber cages. Neurosurgery. 2006;58:502–508. doi: 10.1227/01.NEU.0000197258.30821.50. [DOI] [PubMed] [Google Scholar]
- 2.Furderer S, Schollhuber F, Rompe JD, Eysel P. Influence of design and implantation technique on the risk of progressive sintering of various cervical vertebrae cages. Orthopade. 2002;31:466–471. doi: 10.1007/s00132-001-0289-2. [DOI] [PubMed] [Google Scholar]
- 3.Gercek E, Arlet V, Delisle J, Marchesi D. Subsidence of stand-alone cervical cages in anterior interbody fusion: warning. Eur Spine J. 2003;12:513–516. doi: 10.1007/s00586-003-0539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hacker RJ. A randomised prospective study of an anterior cervical fusion device with a minimum of 2 years follow-up results. J Neurosurg (Spine 2) 2000;93:222–226. doi: 10.3171/spi.2000.93.2.0222. [DOI] [PubMed] [Google Scholar]
- 5.Hwang S, Lin C, Lieu A, Lee K, Kuo T, Hwang Y, Su Y, Howing S. Three-level and four-level anterior cervical discectomies and titanium cage-aughmented fusion with and without plate fixation. J Neurosurg (Spine 1) 2004;2:160–167. doi: 10.3171/spi.2004.1.2.0160. [DOI] [PubMed] [Google Scholar]
- 6.Kadziora F, Pflugmacher R, Schafer J, Born C, Duda G, Haas NP, Mittlmeier T. Biomechanical comparision of cervical spine interbody fusion cages. Spine. 2001;26:1850–1857. doi: 10.1097/00007632-200109010-00007. [DOI] [PubMed] [Google Scholar]
- 7.Katsuura A, Hukuda S, Suruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10:320–324. doi: 10.1007/s005860000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lim TH, Kwon H, Jeon CH, Kim JG, Sokolowski M, Natarajan R, An HS, Andersson GB. Effect of endplate conditions and bone mineral density on the compressive strength of the graft-endplate interface in anterior cervical spine fusion. Spine. 2001;26:951–956. doi: 10.1097/00007632-200104150-00021. [DOI] [PubMed] [Google Scholar]
- 9.Meier U, Grave A, Hajdukova A. Clinical experience with Cespace, the new intervertebral disc spacer by Aesculap for spondylodesis of the cervical spine in comparision with similar products by Weber, Intromed and AcroMed. Neurosurg Q. 2003;13:40–50. doi: 10.1097/00013414-200303000-00004. [DOI] [Google Scholar]
- 10.Payer M, May D, Reverdin A, Tessitore E. Implantation of an empty carbon fibre composite frame cage after single-level anterior cervical discectomy in the treatment of cervical disc herniation: preliminary results. J Neurosurg (Spine 2) 2003;98:143–148. doi: 10.3171/spi.2003.98.2.0143. [DOI] [PubMed] [Google Scholar]
- 11.Profeta G, Falco R, Ianniciello G, Profeta L, Cigliano A, Raja AI. Preliminary experience with anterior cervical microdiscectomy and interbody titanium cage fusion (Novus CT-Ti) in patients with cervical disc disease. Surg Neurol. 2000;53:417–426. doi: 10.1016/S0090-3019(00)00207-X. [DOI] [PubMed] [Google Scholar]
- 12.Takeshima T, Omokawa S, Tataoka T, Araki M, Ueda Y, Takakura Y. Sagittal alignment of cervical flexion and extension: lateral radiographic analysis. Spine. 2002;27:E348–E355. doi: 10.1097/00007632-200208010-00014. [DOI] [PubMed] [Google Scholar]
- 13.Thome C, Leheta O, Krauss JK, Zevgaridis D. A prospective randomized comparison of rectangular titanium cage fusion and iliac crest autograft fusion in patients undergoing anterior cervical discectomy. J Neurosurg Spine. 2006;4:1–9. doi: 10.3171/spi.2006.4.1.1. [DOI] [PubMed] [Google Scholar]
- 14.Truumees E, Demetropoulos CK, Yang KH, Herkowitz HN. Effects of disc distractive forces on graft compression in an anterior cervical discectomy model. Spine. 2002;27:2441–2445. doi: 10.1097/00007632-200211150-00005. [DOI] [PubMed] [Google Scholar]
- 15.Vavruch L, Hedlund R, Javid D, Leszniewski W, Shalabi A. A prospective randomised comparision between the Cloward procedure and a carbon fiber cage in the cervical spine: a clinical and radiological study. Spine. 2002;27:1694–1701. doi: 10.1097/00007632-200208150-00003. [DOI] [PubMed] [Google Scholar]
- 16.Wilke HJ, Kettler A, Claes L. Stabilizing effect and subsidence tendency of three different cages and bone cement for the fusion of the cervical spine segments. Orthopade. 2002;31:472–480. doi: 10.1007/s00132-001-0288-3. [DOI] [PubMed] [Google Scholar]
- 17.Wilke HJ, Kettler A, Goetz C, Claes L. Subsidence resulting from simulated postoperative neck movements: an in vitro investigation with a new cervical fusion. Spine. 2000;25:2762–2770. doi: 10.1097/00007632-200011010-00008. [DOI] [PubMed] [Google Scholar]