Abstract
Posterior instrumentation through the pedicle is a common surgery. Understanding the morphometry of the pedicle and the anatomy of adjacent neural structures should help decrease the risk of postoperative complications. T1–L5 segments from 15 sets of human vertebrae were separated into individual vertebrae and the morphometric characteristics of the thoracic and lumbar spine and the safe zone of the pedicle were analyzed. T11–L5 segments from six human cadavers were dissected. Measurements were taken from the pedicle to the dura and nerve roots superiorly, inferiorly, medially, and laterally, and the transverse angles of the nerve roots were measured. Pedicles were widest in L5 and narrowest in T4 in the transverse plane, and widest in T11 or T12 and narrowest in T1 in the sagittal plane. In individual pedicle, the ranges of the safe zone width and height were 3.4–7.7 and 8.6–13.7 mm, respectively, in T1–T10; and 7.2–17.8 and 13.9–16.7 mm, respectively, in T11–L5. The transverse angle of the pedicle decreases progressively from T1 to T12, then increase from L1 to L5. In sagittal angle, the largest angle localized at T2 and the smallest at L5. The mean distances from pedicles to adjacent neural structures were greater superiorly and laterally than inferiorly and medially. The lateral distance between nerve root and the pedicle ranged from 2.4 to 9.6 mm in lumbar spine. This study provides potential safe zones for the application of through-pedicle procedures to help decrease the risk of postoperative complications.
Keywords: Posterior instrumentation, Morphometry, Thoracic and lumbar spine, Safe zone, Through-pedicle procedures
Introduction
In 1985, Roy-Camille first applied the pedicle screw plating system for the lumbar spine, since then pedicle screw fixation has become an increasingly popular technique of instrumentation to treat spinal disorders by providing stable fixation and correcting spinal deformities [13, 25]. The first operative experience of percutaneous vertebroplasty was performed in 1987 by Galibert et al. [12] which was a case of hemangioma of C2 vertebra. Since then, transpedicular approach of vertebroplasty was developed. In the case of osteoporotic compression fracture, vertebroplasty with polymethylmethacrylate or kyphoplasty with an inflatable bone tamp (IBT) is performed percutaneously through the transpedicular or extrapedicular approach to the vertebral body. These two methods increase the strength and stiffness of the vertebral body and decrease postoperative complications and pain sensation [1, 2, 16, 17, 23, 24]. Transpedicularly implanted anterior support is a new concept based on kyphoplasty with IBT, which might overcome the structural limitation of the posterior approach and the surgical difficulty of the anterior approach [5, 6]. However, potential drawbacks include screw failure and damage to the adjacent neurovascular structures [11, 19, 26, 28]. In 1988, Roy-Camille et al. reported that about 10% of pedicle screws were placed incorrectly [4, 13, 25]. Weinstein et al. reported an overall failure rate of 21% from cadaveric studies [4, 27]. Several studies have investigated the morphometry of vertebrae using different experimental techniques such as plain film, CT scan, and direct cadaveric dissections to identify the precise insertion point of pedicle screws and to prevent postoperative sequelae [3, 8, 9, 14, 21, 22, 29]. In 1997, Ebraheim et al. measured the anatomic distances between the pedicles and adjacent neural structures in the thoracolumbar spine and showed that true safe distances between the pedicles and neural structures existed [7, 10]. In clinically transpedicular procedures, such as revision of pedicle screws, bone biopsy, bone grafting, and restoration of vertebral body via vertebroplasty or kyphoplasty, which may not limit inside the pedicle in whole process. Even some surgical procedures intended penetrating through extrapedicularly and entered into vertebral body, which so called in-out-in technique. The purpose of this study was to investigate the anatomic morphometry of the pedicles and the relationships between pedicles and the adjacent neural structures, and to identify a potential safe distance existed peri-pedicularly.
Materials and methods
Fifteen sets of human vertebrae (eight males, seven females) and six cadavers (three males, three females) were obtained from the Department of Anatomy, National Defense Medical Center in Taipei City, Taiwan. Each vertebra from T1 to L5 was separated individually. Cadavers with gross deformities such as scoliosis or kyphosis were excluded. All cadavers were Taiwanese and average body size for the population.
The dry vertebra measurements were performed using Vernier calipers with a resolution of 0.1 mm and standard goniometer with accuracy of 1°. Six parameters were measured in the thoracic and lumbar vertebrae: the anatomic width, height of the pedicle isthmus, safe zone width, height of the pedicle, transverse and sagittal angles of pedicle (Fig. 1). The safe zone width was defined as the distance from the lateral cortex of the body to the medial cortex of the ipsilateral pedicle in the top (overhead) view. The safe zone height was defined as the distance from the upper end plate of the body to the inferior cortex of the ipsilateral pedicle in the lateral (side) view. However, the safe zone width and height were smaller than the true pedicle dimensions in T1 to T10 owing to the axis of the pedicle, the true safe zone width and height in T1 to T10 were equivalent to the pedicle dimensions (Fig. 2). Transverse angle of the pedicle was defined as the angle between the pedicle axis and a line parallel to the vertebral midline measured in the transverse plane. Sagittal angle of the pedicle was defined as the angle between the pedicle axis and the superior border of vertebral body in the sagittal plane (Fig. 1).
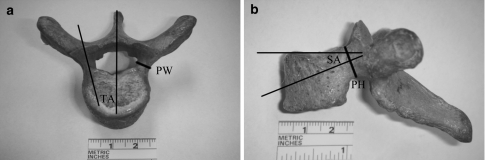
Fig. 1.
The narrowest dimension in both the transverse and sagittal planes were chosen as the pedicular width (PW) and height (PH). The transverse (TA) and sagittal angle (SA) of the pedicle were obtained (see the description of text)
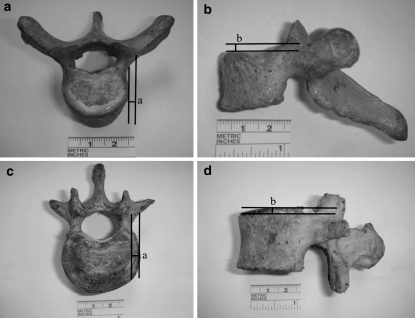
Fig. 2.
Top and side views of the upper thoracic and lumbar vertebrae are shown. In the upper thoracic vertebrae (a, b), the pedicle inclined more cranially and laterally. The cortex of the pedicle is out of the upper end plate and lateral border of the vertebral body. In the lower thoracic or the lumbar vertebrae (c, d), the cortex of pedicle are within the borders of the vertebral body. The difference between the cortex of the pedicle and the borders of the vertebral body are labeled as a and b
Six cadavers were placed in the prone position and the posterior lower thoracic and lumbar spines were obtained after removal of all soft tissue. The spinous processes, lamina, superior and inferior facets, and transverse processes were removed to expose the dura, nerve roots, and pedicles (Fig. 3a). Five parameters were measured from T11 to L5: The transverse root angle was measured between the midline of the dura and the axis of spinal nerve root, and four linear measurements were made between the pedicle cortex and the nerve root in the superior, inferior, medial, and lateral directions (Fig. 3b). All symmetrical structures were measured bilaterally. All data from the 15 sets of human vertebrae and six cadavers were analyzed and averaged, and the data are presented as mean ± standard deviation (SD). All symmetrical data were compared using Student’s t test.
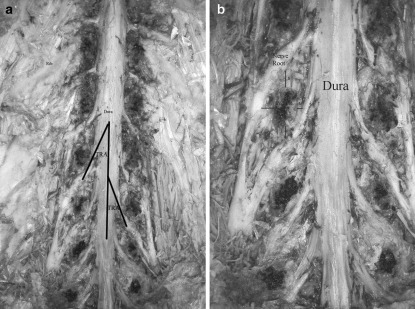
Fig. 3.
a Lower-thoracic and lumbar spines were dissected to expose the pedicle, dura, and nerve roots. The transverse root angles (TRA) from T11 to L5 were measured between the axis of dura and nerve root and averaged. b The superior (S), inferior (I), medial (M), and lateral (L) distances between the cortex of the pedicle and neural structures were measured and averaged. No mobilization of neural structures during dissection was evident
Results
Six measurements were obtained for each dry vertebra from T1 to L5 and five measurements were obtained for each cadaver from T11 to L5. The cumulative summaries are listed in Tables 1, 2, 3, 4 and Figs. 4, 5 and 6.
Table 1.
Measurements of pedicle width, height, and safe zone width, height (mean ± standard deviation)
| Pedicle width (mm) | Pedicle height (mm) | Safe zone width (mm) | Safe zone height (mm) | |||||
|---|---|---|---|---|---|---|---|---|
| Left | Right | Left | Right | Left | Right | Left | Right | |
| T1 | 7.7 ± 1.2 | 7.6 ± 1.1 | 8.7 ± 1.0 | 8.6 ± 1.1 | 7.7 ± 1.2 | 7.6 ± 1.1 | 8.7 ± 1.0 | 8.6 ± 1.1 |
| T2 | 5.6 ± 0.8 | 5.3 ± 0.7 | 10.3 ± 0.9 | 10.3 ± 0.8 | 5.6 ± 0.8 | 5.3 ± 0.7 | 10.3 ± 0.9 | 10.3 ± 0.8 |
| T3 | 4.1 ± 0.8 | 3.9 ± 0.7 | 10.4 ± 1.1 | 10.4 ± 1.2 | 4.1 ± 0.8 | 3.9 ± 0.7 | 10.4 ± 1.1 | 10.4 ± 1.2 |
| T4 | 3.6 ± 0.7 | 3.4 ± 0.6 | 10.2 ± 1.0 | 10.4 ± 1.2 | 3.6 ± 0.7 | 3.4 ± 0.6 | 10.2 ± 1.0 | 10.4 ± 1.2 |
| T5 | 3.7 ± 0.7 | 3.9 ± 0.8 | 10.3 ± 1.1 | 10.8 ± 1.2 | 3.7 ± 0.7 | 3.9 ± 0.8 | 10.3 ± 1.1 | 10.8 ± 1.2 |
| T6 | 3.9 ± 0.9 | 4.0 ± 1.0 | 10.1 ± 1.2 | 10.3 ± 1.1 | 3.9 ± 0.9 | 4.0 ± 1.0 | 10.1 ± 1.2 | 10.3 ± 1.1 |
| T7 | 4.4 ± 1.0 | 4.4 ± 1.1 | 10.4 ± 1.3 | 10.4 ± 1.2 | 4.4 ± 1.0 | 4.4 ± 1.1 | 10.4 ± 1.3 | 10.4 ± 1.2 |
| T8 | 4.8 ± 1.1 | 4.8 ± 1.2 | 10.9 ± 1.4 | 10.8 ± 1.3 | 4.8 ± 1.1 | 4.8 ± 1.2 | 10.9 ± 1.4 | 10.8 ± 1.3 |
| T9 | 5.3 ± 1.2 | 5.2 ± 1.3 | 12.3 ± 1.2 | 12.4 ± 1.2 | 5.3 ± 1.2 | 5.2 ± 1.3 | 12.3 ± 1.2 | 12.4 ± 1.2 |
| T10 | 5.8 ± 1.4 | 5.5 ± 1.2 | 13.6 ± 1.5 | 13.7 ± 1.6 | 5.8 ± 1.4 | 5.5 ± 1.2 | 13.6 ± 1.5 | 13.7 ± 1.6 |
| T11 | 7.4 ± 1.3 | 7.0 ± 1.1 | 14.9 ± 1.4 | 15.3 ± 1.3 | 7.6 ± 1.3 | 7.2 ± 1.1 | 15.7 ± 1.4 | 16.0 ± 1.3 |
| T12 | 7.4 ± 1.4 | 7.7 ± 1.5 | 15.2 ± 1.5 | 15.0 ± 1.4 | 8.2 ± 1.4 | 8.5 ± 1.5 | 16.7 ± 1.5 | 16.6 ± 1.4 |
| L1 | 6.4 ± 1.6 | 6.5 ± 1.7 | 13.6 ± 1.4 | 13.7 ± 1.5 | 8.5 ± 1.6 | 8.3 ± 1.7 | 16.2 ± 1.4 | 15.8 ± 1.5 |
| L2 | 7.4 ± 1.7 | 7.0 ± 1.8 | 14.0 ± 1.7 | 14.1 ± 1.8 | 10.0 ± 1.7 | 9.8 ± 1.8 | 15.2 ± 1.7 | 16.2 ± 1.8 |
| L3 | 9.3 ± 1.9 | 9.0 ± 1.8 | 13.9 ± 1.6 | 13.9 ± 1.7 | 10.1 ± 1.9 | 10.2 ± 1.8 | 16.1 ± 1.6 | 16.2 ± 1.7 |
| L4 | 11.6 ± 2.1 | 12.2 ± 2.3 | 12.5 ± 2.2 | 13.0 ± 2.3 | 12.0 ± 2.1 | 13.0 ± 2.3 | 13.9 ± 2.2 | 14.9 ± 2.3 |
| L5 | 17.5 ± 2.6 | 17.7 ± 2.7 | 12.3 ± 2.3 | 12.7 ± 2.1 | 17.6 ± 2.6 | 17.8 ± 2.7 | 14.8 ± 2.3 | 15.3 ± 2.1 |
Table 2.
Measurements of transverse and sagittal angle of pedicle (mean ± standard deviation)
| Transverse angle (deg) | Sagittal angle (deg) | |||
|---|---|---|---|---|
| Left | Right | Left | Right | |
| T1 | 27.8 ± 4.1 | 28.6 ± 4.5 | 12.4 ± 2.3 | 10.8 ± 1.8 |
| T2 | 26.1 ± 3.2 | 26.6 ± 4.1 | 18.6 ± 3.1 | 19.2 ± 3.5 |
| T3 | 22.4 ± 3.7 | 24.2 ± 3.5 | 16.4 ± 2.5 | 16.8 ± 2.4 |
| T4 | 23.1 ± 2.6 | 22.6 ± 3.4 | 15.3 ± 2.1 | 14.7 ± 2.2 |
| T5 | 17.3 ± 2.8 | 19.1 ± 2.9 | 17.6 ± 2.7 | 18.1 ± 2.3 |
| T6 | 15.6 ± 2.4 | 15.2 ± 2.1 | 16.1 ± 2.2 | 16.9 ± 2.5 |
| T7 | 12.5 ± 1.7 | 13.1 ± 2.2 | 14.3 ± 2.0 | 12.5 ± 1.8 |
| T8 | 14.2 ± 1.5 | 13.4 ± 1.2 | 13.8 ± 2.2 | 14.5 ± 2.5 |
| T9 | 10.9 ± 1.6 | 14.1 ± 2.3 | 12.7 ± 1.9 | 13.4 ± 1.7 |
| T10 | 8.4 ± 1.3 | 9.6 ± 1.5 | 13.2 ± 2.4 | 13.7 ± 1.6 |
| T11 | 8.1 ± 1.6 | 7.9 ± 1.3 | 12.4 ± 1.8 | 11.9 ± 1.5 |
| T12 | 7.4 ± 1.5 | 8.4 ± 1.4 | 10.2 ± 1.7 | 11.2 ± 1.4 |
| L1 | 8.3 ± 3.1 | 8.6 ± 2.5 | 5.4 ± 1.2 | 6.8 ± 2.1 |
| L2 | 11.5 ± 2.7 | 13.2 ± 2.8 | 5.1 ± 0.9 | 5.8 ± 1.5 |
| L3 | 14.1 ± 3.4 | 16.4 ± 3.7 | 4.6 ± 0.7 | 5.4 ± 0.8 |
| L4 | 19.7 ± 3.2 | 18.1 ± 3.4 | 3.5 ± 0.8 | 3.2 ± 0.6 |
| L5 | 25.3 ± 4.7 | 23.4 ± 3.9 | 2.8 ± 0.7 | 3.0 ± 0.8 |
Table 3.
Anatomic parameters of transverse root angle (mean ± standard deviation)
| Nerve root | Transverse root angle (deg) | |
|---|---|---|
| Left | Right | |
| T11 | 70.6 ± 5.2 | 75.2 ± 7.8 |
| T12 | 58.6 ± 7.4 | 60.0 ± 5.2 |
| L1 | 40.2 ± 9.4 | 40.0 ± 7.8 |
| L2 | 38.0 ± 4.2 | 38.0 ± 6.6 |
| L3 | 35.4 ± 3.8 | 37.8 ± 4.2 |
| L4 | 37.2 ± 8.2 | 40.0 ± 6.4 |
| L5 | 28.6 ± 3.4 | 29.0 ± 4.1 |
Table 4.
Anatomic parameters of distance of the pedicle to the dura sac and nerve root (mean ± standard deviation)
| Pedicle | Superior distance to nerve root (mm) | Inferior distance to nerve root (mm) | Medial distance to dura sac (mm) | Lateral distance to nerve root (mm) | ||||
|---|---|---|---|---|---|---|---|---|
| Left | Right | Left | Right | Left | Right | Left | Right | |
| T11 | 4.5 ± 0.6 | 4.7 ± 0.7 | 3.0 ± 0.3 | 3.1 ± 0.4 | 1.0 ± 0.1 | 1.3 ± 0.2 | a | a |
| T12 | 5.0 ± 1.2 | 5.3 ± 1.4 | 3.4 ± 0.4 | 3.8 ± 0.5 | 1.1 ± 0.2 | 1.5 ± 0.2 | a | a |
| L1 | 5.7 ± 1.1 | 5.8 ± 1.0 | 2.6 ± 0.3 | 2.6 ± 0.5 | 2.0 ± 0.3 | 2.0 ± 0.2 | 9.4 ± 2.1 | 9.6 ± 2.5 |
| L2 | 5.5 ± 0.9 | 5.8 ± 0.8 | 2.6 ± 0.6 | 2.5 ± 0.4 | 1.8 ± 0.1 | 2.0 ± 0.1 | 4.5 ± 1.2 | 4.7 ± 1.1 |
| L3 | 6.1 ± 1.2 | 6.1 ± 1.6 | 2.3 ± 0.5 | 2.6 ± 0.6 | 1.7 ± 0.2 | 1.8 ± 0.1 | 4.2 ± 0.4 | 4.3 ± 0.5 |
| L4 | 4.7 ± 0.6 | 5.0 ± 0.4 | 2.0 ± 0.4 | 2.2 ± 0.3 | 1.9 ± 0.3 | 2.1 ± 0.2 | 3.5 ± 0.4 | 3.5 ± 0.3 |
| L5 | 4.1 ± 0.3 | 4.7 ± 0.4 | 2.0 ± 0.2 | 1.9 ± 0.3 | 1.9 ± 0.2 | 1.9 ± 0.1 | 2.4 ± 0.2 | 2.6 ± 0.4 |
aThe direction of nerve root is parallel to the direction of rib cage. Long lateral distance (>10 mm) to the nerve root in T11and T12 pedicles are noted
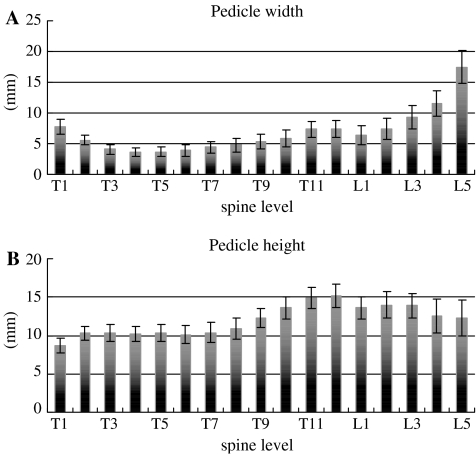
Fig. 4.
The graphs of relationship between the dimension of the pedicle and spine levels
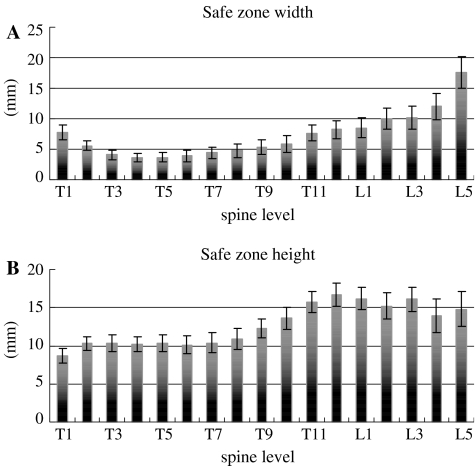
Fig. 5.
The graphs of relationship between the safe zone of the pedicle and spine levels
Fig. 6.
The graphs of relationship between the pedicle angles and spine levels
Pedicle width and height
The pooled data on pedicle width and height are listed in Table 1 and presented as graphs in Fig. 4. The pedicle width and height varied between individuals and between levels, although these dimensions did not differ significantly between the right and left sides. The pedicle width of the thoracic segment decreased dramatically from T1 to T4 and then increased gradually to T12. The pedicle width of the lumbar segment increased gradually from L1 to L4 and increased sharply at L5. In both males and females, the widest pedicle width (17.6 mm) was located at L5 and the narrowest was located at T4 (3.5 mm) or T5 (3.8 mm). The pedicle height of the thoracic segment increased gradually from T1 to T12. The pedicle height of the lumbar segment gradually decreased from L2 to L5, and the pedicle height of L1 (13.7 mm) was slightly smaller than that of L2 (14.1 mm). In both males and females, the largest pedicle height was located at T11 (15.1 mm) or T12 (15.1 mm) and the smallest at T1 (8.7 mm).
Safe zone of pedicle width and height
The pooled data are listed in Table 1 and presented as graphs in Fig. 5. The safe zone of pedicle width was 3.4–7.7 mm for T1–T10, 7.2–10.0 mm for T11–L2, and 10.1–17.8 mm for L3–L5. The safe zone of pedicle height was 8.6–13.7 mm for T1–T10 and 13.9–16.7 mm for T11–L5.
Transverse and sagittal angle of the pedicle
The transverse and sagittal angles of pedicle in the thoracolumbar spines are shown in Table 2 and presented as graphs in Fig. 6. A consistent trend is seen in the transverse angles of thoracolumbar vertebrae. The largest angle is seen at T1 with the mean of 28.2° and shallowest at T12 with the mean of 7.9°. It decreases progressively from T1 to T12, then increases progressively from L1 to L5. In the sagittal angle, the largest and shallowest angles are seen in T2 and L5 with the mean of 18.9° and 2.9°, respectively.
Transverse nerve root angle
The transverse nerve root angles in the lower thoracic and lumbar spines are shown in Table 3. The transverse nerve root angles were 58.6°–75.2° in the lower thoracic spine (T11 and T12) and 28.6°–40.2° in the lumbar spine. The dimensions did not differ significantly between the right and left sides. The angles of the nerve roots in the lower thoracic spine were positioned more cranially, nearly parallel to the rib cage, than those of the lumbar spine.
Distances between pedicle and adjacent neural structures
The pooled data on the distances between the pedicle and the adjacent neural structures are listed in Table 4. The superior distances (4.5–5.3 mm) were slightly greater than the inferior distances (3.0–3.8 mm) in the lower thoracic spine. The superior distances (4.1–6.1 mm) were much greater than the inferior distances (1.9–2.6 mm) in the lumbar spine. The pedicles were closer to the dura in the lower thoracic spine (1.0–1.5 mm) than in the lumbar spine (1.9–2.1 mm). Because the direction of the lower thoracic nerve roots was nearly parallel to the direction of the rib cage, the lateral distances in the lower thoracic spine was greater (>10 mm) than in the lumbar spine (2.4–9.6 mm). In the lumbar spine, the lateral distance was greatest in the L1 pedicle (9.5 mm) and smallest in the L5 (2.5 mm). The dimensions did not differ significantly between the right and left sides.
Discussion
In 1985, Roy-Camille first applied the pedicle screw plating system for the lumbar spine, since then spinal pedicle fixation has become a popular method of spinal instrumentation [13, 25]. To prevent impingement of the neural structures, accurate and safe pathway of the pedicle is important and requires precise and accurate knowledge of bony and neural structures. Many authors have described the morphometric aspects of the thoracic and lumbar spine and the details of the pedicle sizes and dimensions by means of CT scan, plain image, direct specimen measurement and quantitative 3-dimensional anatomic technique [3, 8, 9, 14, 15, 21, 22, 29].
We directly measured the dimensions from the T1 to L5 vertebrae in 15 whole dry vertebrae. The general trend of our measurement of the pedicle dimensions was consistent with that of Panjabi et al. in the thoracic spine, Olsewski et al. in the lumbar spine, and Zindrick and Hou et al. in the thoracolumbar spine. However, the pedicle width in L5 was different from the studies of Hou and Berry et al., whose results at L5 were smaller than in our study. The pedicle heights of our study were smaller compared with the results from the aforementioned studies. The transverse angle of the pedicles showed smaller angle laterally in T10–L1 and increased upward and downward in the thoracolumbar vertebrae. The sagittal angle of the pedicles showed decreased trend from T2 to L5. The definition of safe zone in our study is far-out boundary of peri-pedicle area that can be identified from the clinical imaging study. The safe zone width was less than the true pedicle width in T1–T10 and greater than the true pedicle width in T11–L5. The safe zone height was less than the true pedicle height in T1–T6, did not differ from the true pedicle height in T7–T10, and was greater than the true pedicle height in T11–L5. Hence, the true safe zone width and height in the upper and mid-thoracic spine (T1–T10) are the true pedicle width and height because the pedicle angles incline more superiorly and laterally in the upper thoracic vertebrae. No previous studies quantitatively measured anatomic safe zone of the pedicle width and height. But in fact, the axis of the pedicle is oblique in the axial plane, the safe zone of the pedicle is also decided by the transverse and sagittal angles of the pedicle except the dimensions of the pedicle. These preliminary data including safe zone width, height and pedicular angles are practicable and useful in fluoroscopy-guided spinal surgery.
Previous anatomic evaluation has focused on the morphometric study of vertebrae and the selection of the starting point of the pedicle screw. Only a few studies have reported on the anatomic relationship between the pedicles and adjacent neural structures [7, 10, 18, 20]. Louis described the general locations of the spinal cord and nerve roots relative to the vertebral column [18]. Ebraheim et al. quantified the distance between the pedicle and adjacent neural structures. They concluded that the superior and lateral sides of the pedicles were safer than the inferior and medial sides in the lumbar spine, and that the lateral, superior, and inferior sides were equally safe in the thoracic spine. They also concluded that the transverse root angles were 57.1°–84.0° in the low thoracic spine (T10–T12) and 33.7°–39.2° in the lumbar spine [7, 10]. We observed similar values: transverse root angles of 58.6°–75.2° in the low thoracic spine (T11 and T12) and 28.6°–40.2° in the lumbar spine. We found that, in the lower thoracic spine, the nerve roots were nearly parallel to the rib direction, the superior and inferior distances were similar, and the lateral distances were greater. In the lumbar spine, the superior distances were greater than the inferior distances because of the caudal direction of the nerve roots. The lateral distance of the lumbar pedicle to the nerve roots was 2.4–9.6 mm and was smaller in the lower lumbar spine. Both our study and previous cadaveric studies measured the mean distances from the low thoracic and lumbar pedicles to the adjacent neural structures, but we believe we are the first to measure the lateral mean distances. The broad definition of the true safe zone around the pedicle should include the pedicle and the distances between the pedicles and the neural structures (i.e., the extrapedicular distance). Nerve roots are relatively mobile outside the neuroforamen and safely retracted lateral to the pedicle. Besides, the directions of the nerve roots are 3-dimension (3D) in anatomy. In our study, we measured the distance just under 2D which are not truly shortest distance in 3D space. Besides, the nerve roots may be retracted or shrunk in post-mortem cadavers. Among these factors, the true distance between the neural structures and the pedicle are shorter than our study.
The “all-through-pedicle” procedure is a new concept and includes the idea of a true safe zone, which could be applied in many surgeries, such as bone biopsy, bone grafting, pedicle screws, vertebroplasty, and kyphoplasty, even those that penetrate the upper and lateral walls of pedicle. The “in-out-in” technique is performed in the upper and mid-thoracic spine because of different morphometry of the pedicles and adjacent neural structures. According to the concepts of the “all-through-pedicle” and the “in-out-in” techniques, the data of safe zone might provide surgeon to approach the vertebral body by means of the pedicle more comfortably.
Conclusion
Knowledge of the potential safe zones of the pedicle and potential safe zone between the pedicles and adjacent neural structures in the thoracic and lumbar spine are important when performing pedicular surgery. In our study, we first quantitatively investigated the safe zone width and height of the pedicles and the lateral distance between the pedicles and neural structures. The true safe zone width and height of the pedicles in the upper and mid-thoracic spine are equal to the true pedicle width and height. However, the safe zone of the pedicle is also decided by the transverse and sagittal angles of the pedicle. The relationship between the pedicles and adjacent neural structures showed no obvious difference compared to Ebraheim’s study. The lateral distance in lower thoracic spine was much wider because the nerve root is nearly parallel to the rib direction, but otherwise in lumbar spine. We believed that it could provide more detail safe range evaluation if the pedicle is disrupted during spine surgery.
References
- 1.Belkoff SM, Jasper LE, Stevens SS. An ex vivo evaluation of an inflatable bone tamp used to reduce fractures within vertebral bodies under load. Spine. 2002;27:1640–1643. doi: 10.1097/00007632-200208010-00009. [DOI] [PubMed] [Google Scholar]
- 2.Belkoff SM, Mathis JM, Fenton DC, Scribner RM, Reiley ME, Talmadge K. An ex vivo biomechanical evaluation of an inflatable bone tamp used in the treatment of compression fracture. Spine. 2001;26:151–156. doi: 10.1097/00007632-200101150-00008. [DOI] [PubMed] [Google Scholar]
- 3.Berry JL, Moran JM, Berg WS, Steffee AD. A morphometric study of human lumbar and selected thoracic vertebrae. Spine. 1987;12:362–367. doi: 10.1097/00007632-198705000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Boachie-Adjei O, Girardi FP, Bansal M, Rawlins BA. Safety and efficacy of pedicle screw placement for adult spinal deformity with a pedicle-probing conventional anatomic technique. J Spinal Disord. 2000;13:496–500. doi: 10.1097/00002517-200012000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Chen HH, Wang WK, Li KC, Chen TH. Biomechanical effects of the body augmenter for reconstruction of vertebral body. Spine. 2004;29:E382–E387. doi: 10.1097/01.brs.0000139308.65813.70. [DOI] [PubMed] [Google Scholar]
- 6.Cottle W, Budney D, Moreau M, Raso J, Greenhill B. A transpedicularly implanted anterior spinal support. J Spinal Disord. 1995;8:479–485. doi: 10.1097/00002517-199512000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Ebraheim NA, Jabaly G, Xu R, Yeasting RA. Anatomic relations of the thoracic pedicle to the adjacent neural structures. Spine. 1997;22:1553–1557. doi: 10.1097/00007632-199707150-00002. [DOI] [PubMed] [Google Scholar]
- 8.Ebraheim NA, Rollins JR, Xu R, Yeasting RA. Projection of the lumbar pedicle and its morphometic analysis. Spine. 1996;21:1296–1300. doi: 10.1097/00007632-199606010-00003. [DOI] [PubMed] [Google Scholar]
- 9.Ebraheim NA, Xu R, Ahmad M, Yeasting RA. Projection of the thoracic pedicle and its morphometric analysis. Spine. 1997;22:233–238. doi: 10.1097/00007632-199702010-00001. [DOI] [PubMed] [Google Scholar]
- 10.Ebraheim NA, Xu R, Darwich M, Yeasting RA. Anatomic relations between the lumbar pedicle and the adjacent neural structures. Spine. 1997;22:2338–2341. doi: 10.1097/00007632-199710150-00003. [DOI] [PubMed] [Google Scholar]
- 11.Esses SI, Sachs BL, Dreyzin V. Complications associated with the technique of pedicle screw fixation. Spine. 1993;18:2231–2239. doi: 10.1097/00007632-199311000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Galibert P, Deramond H, Rosat P, Le Gars D. Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie. 1987;33:166–168. [PubMed] [Google Scholar]
- 13.Gertzbein SD, Robbins SE. Accuracy of pedicular screw placement in vivo. Spine. 1990;15:11–14. doi: 10.1097/00007632-199001000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Hou S, Hu R, Shi Y. Pedicle morphology of the lower thoracic and lumbar spine in a Chinese population. Spine. 1993;18:1850–1855. doi: 10.1097/00007632-199310000-00021. [DOI] [PubMed] [Google Scholar]
- 15.Krag MH, Weaver DL, Beynnon BD, Haugh LD. Morphometry of the thoracic and lumbar spine related to transpedicular screw placement for surgical spinal fixation. Spine. 1988;13:27–32. doi: 10.1097/00007632-198801000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Lieberman IH, Dudeney S, Reinhardt MK, Bell G. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26:1631–1638. doi: 10.1097/00007632-200107150-00026. [DOI] [PubMed] [Google Scholar]
- 17.Lieberman I, Reinhardt MK. Vertebroplasty and kyphoplsty for osteolytic vertebral collapse. Clin Orthop. 2003;415S:176–186. doi: 10.1097/01.blo.0000093841.72468.a8. [DOI] [PubMed] [Google Scholar]
- 18.Louis R. Topographic relationships of the vertebral column, spinal cord, and nerve roots. Anat Clin. 1978;1:3–12. doi: 10.1007/BF01654344. [DOI] [Google Scholar]
- 19.Matsuzaki H, Tokuhashi Y, Matsumoto F, Hoshino M, Kiuchi T, Toriyama S. Problems and solutions of pedicle screw plate fixation of lumbar spine. Spine. 1990;15:1159–1165. doi: 10.1097/00007632-199011010-00014. [DOI] [PubMed] [Google Scholar]
- 20.Mirkovic SR, Schwartz DG, Glazier KD. Anatomic considerations in lumbar posterolateral percutaneous procedures. Spine. 1995;20:1965–1971. doi: 10.1097/00007632-199509150-00001. [DOI] [PubMed] [Google Scholar]
- 21.Olsewski JM, Simmons EH, Kallen FC, Mendel FC, Severin CM, Berens DL. Morphometry of the lumbar spine: Anatomical perspectives related to transpedicular fixation. J Bone Joint Surg. 1990;72A:541–549. [PubMed] [Google Scholar]
- 22.Panjabi MM, Takata K, Goel V, Federico D, Oxland T, Duranceau J, Krag M. Thoracic human vertebrae. Quantitative three-dimensional anatomy. Spine. 1991;16:888–901. doi: 10.1097/00007632-199108000-00006. [DOI] [PubMed] [Google Scholar]
- 23.Phillips FM, Ho E, Campbell-Hupp M, McNally T, Wetzel FT, Gupta P. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine. 2003;28:2260–2267. doi: 10.1097/01.BRS.0000085092.84097.7B. [DOI] [PubMed] [Google Scholar]
- 24.Phillips FM. Minimally invasive treatments of osteoporotic vertebral compression fractures. Spine. 2003;28:S45–S53. doi: 10.1097/00007632-200308011-00009. [DOI] [PubMed] [Google Scholar]
- 25.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop. 1986;203:7–17. [PubMed] [Google Scholar]
- 26.Suk S, Lee CK, Kim W, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. doi: 10.1097/00007632-199506000-00012. [DOI] [PubMed] [Google Scholar]
- 27.Weinstein JN, Spratt KF, Spengler D, Brick C, Reid S. Spinal pedicle fixation: Reliability and validity of roentgenogram-based assessment and surgical factors on successful screw placement. Spine. 1988;13:1012–1018. doi: 10.1097/00007632-198809000-00008. [DOI] [PubMed] [Google Scholar]
- 28.West JL, Ogilvie JW, Bradford DS. Complications of the variables screw plate pedicle screw fixation. Spine. 1991;16:576–579. doi: 10.1097/00007632-199105000-00016. [DOI] [PubMed] [Google Scholar]
- 29.Zindrick MR, Wiltse LL, Doornik A, Widell EH, Knight GW, Patwardhan AG, Thomas JC, Rothman SL, Fields BT. Analysis of the morphometric characteristics of the thoracic and lumbar pedicles. Spine. 1987;12:160–166. doi: 10.1097/00007632-198703000-00012. [DOI] [PubMed] [Google Scholar]