Abstract
Minimally invasive techniques have revolutionized the management of a variety of spinal disorders. The authors of this study describe a new instrument and a percutaneous technique for anterior odontoid screw fixation, and evaluate its safety and efficacy in the treatment of patients with odontoid fractures. Ten patients (6 males and 4 females) with odontoid fractures were treated by percutaneous anterior odontoid screw fixation under fluoroscopic guidance from March 2000 to May 2002. Their mean age at presentation was 37.2 years (with a range from 21 to 55 years). Six cases were Type II and four were Type III classified by the Anderson and D’Alonzo system. The operation was successfully completed without technical difficulties, and without any soft tissue complications such as esophageal injury. No neurological deterioration occurred. Satisfactory results were achieved in all patients and all of the screws were in good placement. After a mean follow-up of 15.7 months (range 10–25 months), radiographic fusion was documented for 9 of 10 patients (90%). Neither clinical symptoms nor screw loosening or breakage occurred. Our preliminary clinical results suggest that the percutaneous anterior odontoid screw fixation procedure using a new instrument and fluoroscopy is technically feasible, safe, useful, and minimally invasive.
Keywords: Odontoid process, Fracture, Percutaneous, Screw fixation, Minimally invasive spinal surgery
Introduction
Fracture of the odontoid of the axis is a common injury in the cervical spine. Its treatment remains quite challenging because of the associated risk owing to the complex anatomy of the cranio–cervical junction. The conservative treatment includes cervical orthoses, halo vests, and jackets, which may allow for the fracture to fuse without the need for surgical intervention [17, 20, 22, 24]. However, these methods are poorly tolerated in the elderly and the multiply injured patients [18, 19]. Moreover, type II fractures and shallow type III odontoid fractures, based on the classification of Anderson and D’Alonzoare [2], are mechanically unstable injuries. When these fractures are treated conservatively, rates of nonunion and pseudoarthrosis are high [5].
Given the suboptimal outcomes observed with conservative management strategies, some authors have recommended primary posterior C1–C2 arthrodesis as the treatment of choice [6, 10]. Despite excellent rates of fusion by way of posterior arthrodesis of C1 and C2, this technique can lead to compromise the rotation of atlanto-axial joints by 45°, flexion and extension by 15° [14]. Anterior odontoid screw fixation is ideal for fixation of unstable odontoid fractures and is superior to posterior C1–C2 arthrodesis as it preserves C1–C2 rotational movement and obviates the need for autograft bone harvest. This method has become increasingly popular, since the time it was introduced by Bohler [4], and it is now widely used to treat unstable type II and shallow type III odontoid fractures. In reviewing the literature, anterior screw fixation of acute odontoid fractures had good results, with fusion rates from 81 to 100% [1, 3, 4, 8, 9, 13, 15, 23].
Recently, Hashizume et al. [12] described the use of an endoscopic system for anterior screw fixation of the odontoid fracture in order to minimize the surgical invasion and to avoid soft tissue injuries. Kazan et al. [16] first reported technical details using a special instrument and a percutaneous technique for closed anterior fication of odontoid fracture in their cadaveric study. To our knowledge, there have been no reports of clinical studies on the safety and efficacy of the percutaneous anterior odontoid screw technique. Ten cases with odontoid fractures from March 2000 to May 2002 were treated with percutaneous anterior screw fixations in our institution and good functional results were achieved. In this preliminary report, the authors discuss the clinical application of this new procedure.
Materials and methods
Description of instrument
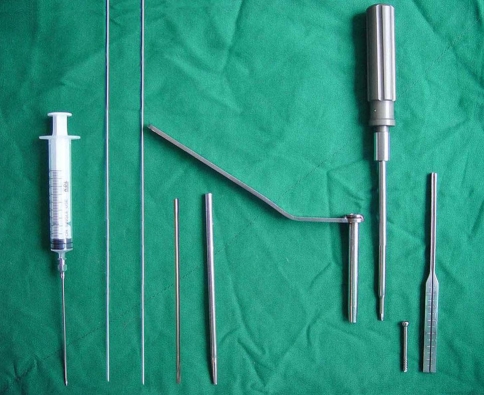
A system of tools was developed by one of the authors (Y.L.C) to facilitate insertion of a cannulated screw percutaneously. These tools are composed of the following instruments (Fig. 1).
The puncture needle is 1.3 mm in internal diameter, 110 mm in length, and 1.4 mm in external diameter. The distal end of the needle is connected with an injection syringe.
Two Kirschner wires (K-wire) of 1.2 mm, one with a blunt tip and another with a sharp tip.
The cannulated drill bit is 1.4 mm in internal diameter, 150 mm in length, and 2.5–3.0 mm in external diameter.
The guide tube is 1.3 mm in internal diameter, 150 mm in length, and 5.0 mm in external diameter.
The protection tube is 5.1 mm in internal diameter, 95 mm in length, and 6 mm in external diameter.
The cannulated hexagon screwdriver, the self-tapping screw, and the depth gauge.
Fig. 1.
Photograph showing tools for percutaneous anterior screw fixation. (Left to right): puncture needle connected with an injection syringe, K-wire with a blunt tip, K-wire with a sharp tip, cannulated drill bit, guide tube, protection tube, cannulated hexagon screwdriver, self-tapping screw, and depth gauge
Patient population
The clinical study proposal was approved by the medical ethical committee of the authors’ institution. Ten cases with odontoid fractures from March 2000 to May 2002 were treated with percutaneous anterior screws fixations within a mean of 3 days after injury in our institution (Table 1). There were six males and four females. Their mean age at presentation was 37.2 years (with a range from 21 to 55 years). Six cases were Type II and four were Type III classified by the Anderson and D’Alonzo system [2]. The causes of the injury were vehicle accidents (4 cases), pedestrians being hit by cars (3), falls from a height (2), motorcycle accidents (1).
Table 1.
Demographic and operative data of the patients
| No. | Age (years) | Sex | Cause of trauma | Symptom | Anderson and D’Alonzo type of odontoid fracture | Displacement (mm) | Follow up (months) | Results |
|---|---|---|---|---|---|---|---|---|
| 1 | 25 | M | Two-vehicle accident | Neck pain | II | 4, P | 10 | Union |
| 2 | 45 | M | Pedestrian-struck accident | Neck pain | II | 0, N | 14 | Union |
| 3 | 38 | F | Pedestrian-struck accident | Neck pain | III | 0, N | 12 | Union |
| 4 | 51 | M | Fall | Neck pain | III | 7, P | 10 | Nonunion |
| 5 | 42 | M | Two-vehicle accident | Neck pain | II | 0, N | 17 | Union |
| 6 | 21 | F | Two-vehicle accident | Neck pain | III | 2, A | 23 | Union |
| 7 | 23 | F | Motor-cycle accident | Neck pain | II | 11, P | 21 | Union |
| 8 | 47 | M | Pedestrian-struck accident | Neck pain | II | 3, P | 25 | Union |
| 9 | 55 | F | Fall | Neck tenderness | II | 0, N | 15 | Union |
| 10 | 25 | M | Two-vehicle accident | Neck pain | III | 3, A | 10 | Union |
M male, F female, N no displacement of odontoid process, A anterior displacement of odontoid process, P posterior displacement of odontoid process
The preoperative radiographic examinations, including lateral view, AP view and open-mouth view of plain X-ray films and CT scans of the odontoid, found displacement more than 5 mm in two patients, less than 5 mm in four cases, and four without displacement. There were no other spinal column injuries identified in the group.
Operative technique
Preoperatively, the ability to obtain a near-anatomic reduction must be ensured. All patients with displaced odontoid fractures underwent reduction of the malalignment using Gardner-Wells tong skull traction, and serial cervical lateral radiographs were taken to confirm an anatomic reduction of the fracture.
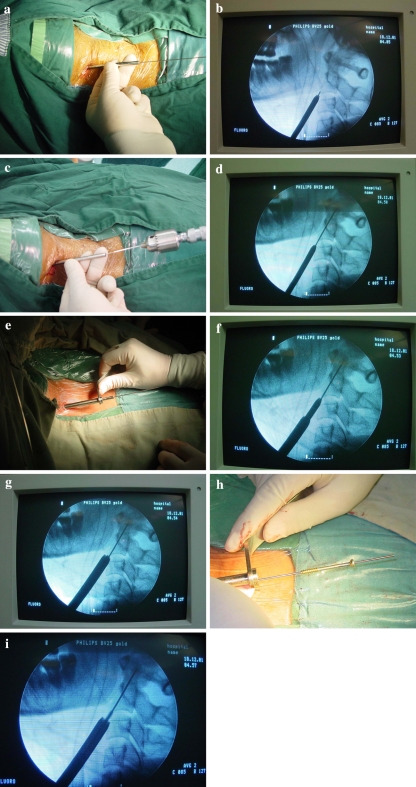
After fiberoptic nasotracheal intubation, the patient was positioned supine with a small roll behind the shoulders to allow slight neck extension. Two high-resolution image intensifiers were available. A radiolucent bite was placed in the patient’s mouth to facilitate the open-mouth view. The lateral masses of C1, the vertebral body of C2, and the odontoid process could be visualized under anterior/posterior and lateral fluoroscopy. Before attempting anterior odontoid screw fixation, the patient’s head was secured using Gardner-Wells tongs with 2 kg of traction applied. Reduction status of the fracture was assessed under fluoroscopic visualization. If necessary, gentle flexion and extension manoeuvres might be applied to achieve adequate reduction monitored on the screen. The head was then kept in position with sand bags on either side and fixed with plastering tape. Firstly, a 25–30 ml of NaCl% 0.9 was given from the cervical prevertebral fascia to the skin between the carotid sheath and the trachea and esophagus complex. In this way, the injection separates the neurovascular bundle as well as the esophagus and trachea [16]. Medial to the right sternocleidomastoid muscle, at approximately the level of C4–5-disc space, an initial incision of 5 mm was made. If necessary, the incision was extended to 1.0 cm maximum. The platysma was then divided, and the fascia of the sternocleidomastoid sharply incised along its medial border. Blunt dissection was used to arrive at the anterior border of the spinal column with the aid of a hemostat. Under the image intensifier control, a puncture needle, 1.2 mm in diameter, connected with a 10 ml syringe, was inserted into the potential space between the carotid sheath and trachea-oesophageal complex. If no bleeding was seen in the syringe when it was drawn back, the syringe was disconnected; a 1.2 mm K-wire with a blunt tip was then inserted inside the puncture needle. The puncture needle was removed and the guide tube overpassed the K-wire. Blunt dissection was performed slightly within the avascular plane by using the guide tube and K-wire, then cephalad to the C2–3 disc space and extended to the prevertebral area. Under fluoroscopic control, the initial starting point for the guide tube was in the middle of the AP view, and was at the anterior aspect of the C2–C3 disc space of the lateral view to attain the proper angle. In this way, the entry point for the K-wire was allowed to be at the anterior inferior lip of C2. After the guide tube was anchored and the trajectory deemed appropriate, the K-wire with a blunt tip was withdrawn and the guide tube was left in place. The sharp tipped K-wire was inserted through the guide tube until the pin reached the entry point (Fig. 2a, b), and was then advanced into the odontoid distal fragment with a power-drill (Fig. 2c, d). The drilling path directed to the posterior superior tip of the odontoid process. Sometimes, the K-wire was needed to drill through the disc material below the anterior inferior endplate of C2 to obtain a proper screw entry site (the anterior aspect of the inferior margin of C2 in the midline). After the K-wire was positioned satisfactorily, the depth of penetration by the drill was determined by the depth gauge. Along the guide tube, a protection tube with 6 mm outer diameter and 5.1 mm inner diameter was advanced (Fig. 2e–g), and the guide tube was subsequently taken out. The protection tube position was maintained throughout the operation to protect the soft tissues. A recess for the screw head was then made with the cannulated drill bit sliding over the K-wire. Care must be taken to avoid advancing the K-wire further as the drilling is performed. A 3.5 mm self-tapping cannulated screw with partial threads was placed over the K-wire, inside the protection tube (Fig. 2h, i), and into the tip of the fragment. The end of the K-wire needs to be held with a needle holder to avoid the advancement of the K-wire when the screw is being inserted into the bone. The screw length should be 1 or 2 mm shorter than the measured length if a gap between the fractured bone surface and the threads of the screw must cross the fracture line because the lag effect derives only from final tightening of the screw to increase compression and to approximate the fracture line. The wire and the tube were removed, the wound was checked for hemostasis, and closure completed in layers with one stitch. For all the 10 patients, the fracture was fixed with a single screw. Flexion and extension of the patient’s neck was manipulated, and spinal stability and screw placement was verified under fluoroscopy. A single suture closed the incision.
Fig. 2.
a, b The guide tube containing a sharp tipped K-wire was placed at the desired entry point. c, d The guide K-wire was advanced into the odontoid with a power drill until the tip of it was penetrated. e–g The protection tube over the guide tube was inserted into the inferior border of the C2 body. h, i The screw was inserted through the protection tube and advanced into the odontoid
Postoperatively, oral antibiotics were administered to the patients as a routine. The patients were allowed ambulatory activities on the postoperative day-two. They were fitted with a soft collar for 12 weeks.
Results
In all patients, the operation was successfully performed in a completely percutaneous invasive procedure. The operation time averaged 85 min. The intraoperative bleeding was 15 ml on average. Successful positioning of the odontoid screws and immediate spinal stabilization was achieved in all patients (Fig. 3a–d). No procedure-related deaths or no other complications associated with an anterior retropharyngeal approach, including esophageal and pharyngeal perforation, hemorrhage, and airway obstruction, were identified in this series, and all patients remained in neurologically stable condition.
Fig. 3.
a, b Preoperative X-ray showing type II odontoid fracture. c, d Postoperative X-ray showing appropriate screw position in same patient
Radiographs of lateral view and open-mouth odontoid view were obtained postoperatively and repeated at 2, 6, 12-weeks’ interval to assess bone healing and alignment. Computerized tomographies may be necessary to assess union. The period of follow-up varied from 10 to 25 months (mean, 15.7 months). No screw breakage or cutting-out occurred. Solid union of the odontoid process could be seen in the nine patients (90%). The fracture lines could still be seen in one case, but the odontoid fragments kept in place and no degree of motion was revealed in the dynamic radiograph. None of our patients had any symptomatology related to the anterior odontoid fixation procedure at the final follow-up. In addition, all of them had returned to a preoperative style of life. Regarding the clinical gross examination of the mobility of our patients during flexion, extension, rotation and lateral bending, we found all mobility had remained quite functional.
Discussion
The anterior odontoid screw fixation technique was first reported in the literature in 1982 [4]. It is the only operative treatment that enables direct osteosynthesis of the odontoid fracture. Immediate stability is achieved to the odontoid, thus decreasing the need for postoperative rigid external immobilization. And it is less surgically traumatic than posterior procedures. Subsequent reports have demonstrated a very high rate of clinical success [1, 3, 8, 9, 13, 15, 23]. But the dissection, just like the common open procedures, needs extensive exposure and care should be taken to avoid injuring adjacent nerves and blood vessels. Drainage should also be placed in the wound postoperatively. Currently, minimally invasive techniques are becoming more widespread in the surgical specialties. As a minimally invasive fixation method, percutaneous anterior odontoid screw fixation was described first by Kazan et al. [16], but their description lacked clinical investigation. To our knowledge, this is the first report of a percutaneous anterior odontoid screw fixation method that is solely fluoroscopically assisted, verifying its safety and technical feasibility in the clinical study.
The specially designed instrument allows odontoid screw fixation percutaneously. Dickman et al. [7] and Apfelbaum et al. [3] had developed the tube systems for successful screw insertion. However, their instrumentations normally are intended for an open surgery, and the spikes of the tube do not allow them to be used in percutaneous invasive procedures. Kazan et al. [16] reported the use of a similar instrument in a cadaveric study. But the device they designed is not yet available commercially. Our instrumentation and technique has several advantages. The main advantage of this technique is its minimally invasive character and direct access to the target site that resembles the open procedure. This percutaneous procedure requires less dissection and exposure of normal tissue during the surgical approach, which can result in decreased blood loss, less postoperative pain and a much quicker recovery. In the current study, there was also no intro-operative complication with a 5–10 mm skin incision (Fig. 4). This is comparable with a 60–70 mm skin incision in the traditional open surgery. Second, the use of the new tube system may reduce the incidence of injury to the surrounding soft tissue, such as the esophagus, trachea, recurrent laryngeal nerve, and carotid artery. Third, the system does not allow bending of the K-wire during the drilling because there is no gap between the innermost tube and the K-wire. Moreover, usage of a cannulated screw that is placed over thin K-wire with which the screw path is drilled decreases the risk of losing the initially drilled pilot hole during subsequent tapping and screw implantation.
Fig. 4.
Postoperative skin incision after percutaneous anterior odontoid screw fixation
Careful patient selection is crucial to achieve successful odontoid screw fixation. Similar to open procedure, we consider percutaneous odontoid screw fixation typically indicated in Type II and shallow Type III fractures when the fracture line runs obliquely downward and backward or horizontal. It is contraindicated when the fracture line is downward and forward. In addition, some physical characteristics such as short neck, significant cervical kyphosis, concomitant thoracic kyphosis, and barrel chest deformity, may interfere with the ideal screw trajectory. Finally, it is important to note that a previous operation that has been performed in the anterior neck is not a contraindication for the open odontoid screw fixation, but is absolute contraindication for this percutaneous procedure.
One-screw fixation may allow axial rotation of the odontoid around the screw, which could result in a lower fusion rate. In this study, we have used one screw and have not observed this complication. In contrast to an open procedure, where the surrounding anatomy is directly visualized, insertion of the second screw is associated with more additional risks in a percutaneous procedure. Moreover, several studies have demonstrated no biomechanical or clinical outcome difference in patients stabilized with one versus two odontoid screws [9, 11, 21].
Anterior odontoid screw fixation can potentially result in any of the complications related to the surgical approach, including postoperative hematomas, dysphagia, hoarseness, or vascular or neural structure injuries. Hashizume et al. [12] reported one patient with odontoid fracture who was operated on using endoscopy to avoid soft tissue involvement. This technique, however, is a highly specialized procedure; and the main obstacle is that vision often becomes blurred due to bleeding. Kazan et al. [16] showed that the percutaneous anterior odontoid screw fixation method was safe. In their cadaveric study, they did not find any serious injury in the parapharyngeal and neurovascular areas of the necks of the cadavers after this procedure. In our series, no complications associated with an anterior retropharyngeal approach occurred in these 10 patients. We emphasize that the guide tube containing K-wire should move up and down slightly within the avascular plane and extended cephalad to the C2–3 disc space under fluoroscopic guidance before it extended to the prevertebral area. This manipulation is the most important stage of the procedure. In this way, the trachea and esophagus are retracted medially, and the sternocleidomastoid muscle and the carotid sheath are mobilized laterally.
Although there are many potential advantages to this percutaneous procedure, percutaneous anterior odontoid screw fixation is technically more demanding than the open technique. Therefore, the surgeon needs sufficient experience of open operations. Also, as a novel surgical technique, a steep learning curve is associated with the development of proficient technical skills. From our experience in the cadaveric lab and our initial operative trials, this technique can be mastered quickly. So we believe that this technique has a short learning curve. The average operative time was 85 min. Early in the surgeon’s learning curve, the duration of this procedure was increased compared with that of conventional open procedure; with experience, the operative times was reduced to 30–45 min, less than those required for the open procedure.
The authors of the current study believe that the percutaneous technique of anterior odontoid screw fixation is a safe and reliable procedure if the following requirements are considered. The first requirement is a thorough knowledge of the underlying three-dimensional spinal anatomy. Familiarity with the anatomy allows the surgeon to safely perform the procedure without exposing structures that are not being surgically treated. Secondly, it also requires thorough preoperative planning and meticulous surgical technique. During drilling and tapping, the soft tissues must be protected continuously, because the percutaneous procedure is performed without direct visualization. Thirdly, biplanar fluoroscopy is essential intraoperatively to visualize the correct angle for screw insertion in both the sagittal and the coronal planes. This can be challenging for surgeons who have not had significant experience using two-dimensional images to determine their three-dimensional surgical position. Finally, this new technique requires significant practice to acquire the skills necessary to perform them safely. So, to gain more experience, the authors recommend thorough training on cadaver specimens before the technique is performed on patients.
Conclusion
The fluoroscopically assisted percutaneous anterior odontoid screw fixation method is a technically feasible, safe, useful, and minimally invasive technique. Although there are several pitfalls with the procedure, careful preoperative planning and strict attention to properly selecting the insertion point, insertion angle and depth, with specially designed percutaneous cannulated system can make this percutaneous procedure effective and practicable. The preliminary results of our study are promising, but a proper evaluation will require more extended studies.
References
- 1.Aebi M, Etter C, Coscia M. Fractures of the odontoid process. Treatment with anterior screw fixation. Spine. 1989;14:1065–1070. doi: 10.1097/00007632-198910000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–1674. [PubMed] [Google Scholar]
- 3.Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93(Suppl):S227–S236. doi: 10.3171/spi.2000.93.2.0227. [DOI] [PubMed] [Google Scholar]
- 4.Bohler J. Anterior stabilization for acute fractures and non-unions of the dens. J Bone Joint Surg Am. 1982;64:18–27. [PubMed] [Google Scholar]
- 5.Clark CR, White AA., III Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985;67:1340–1348. [PubMed] [Google Scholar]
- 6.Coyne TJ, Fehlings MG, Wallace MC, Bernstein M, Tator CH. C1–C2 posterior cervical fusion: long-term evaluation of results and efficacy. Neurosurgery. 1995;37:688–692. doi: 10.1097/00006123-199510000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Dickman CA, Foley KT, Sonntag VK, Smith MM. Cannulated screws for odontoid screw fixation and atlantoaxial transarticular screw fixation technical note. J Neurosurg. 1995;83:1095–1100. doi: 10.3171/jns.1995.83.6.1095. [DOI] [PubMed] [Google Scholar]
- 8.ElSaghir H, Bohm H. Anderson type II fracture of the odontoid process: results of anterior screw fixation. J Spinal Disord. 2000;13:527–530. doi: 10.1097/00002517-200012000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Fountas KN, Kapsalaki EZ, Karampelas I, Feltes CH, Dimopoulos VG, Machinis TG, Nikolakakos LG, Boev AN, III, Choudhri H, Smisson HF, Robinson JS. Results of long-term follow-up in patients undergoing anterior screw fixation for type II and rostral type III odontoid fractures. Spine. 2005;30:661–669. doi: 10.1097/01.brs.0000155415.89974.d3. [DOI] [PubMed] [Google Scholar]
- 10.Fujii E, Kobayashi K, Hirabayashi K. Treatment in fractures of the odontoid process. Spine. 1988;13:604–609. doi: 10.1097/00007632-198813060-00002. [DOI] [PubMed] [Google Scholar]
- 11.Graziano G, Jaggers C, Lee M, Lynch W. A comparative study of fixation techniques for type II fractures of the odontoid process. Spine. 1993;18:2383–2387. doi: 10.1097/00007632-199312000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Hashizume H, Kawakami M, Kawai M, Tamaki T. A clinical case of endoscopically assisted anterior screw fixation for the type II odontoid fracture. Spine. 2003;28:E102–E105. doi: 10.1097/00007632-200303010-00024. [DOI] [PubMed] [Google Scholar]
- 13.Henry AD, Bohly J, Grosse A. Fixation of odontoid fractures by an anterior screw. J Bone Joint Surg Br. 1999;81:472–477. doi: 10.1302/0301-620X.81B3.9109. [DOI] [PubMed] [Google Scholar]
- 14.Hohl M. Normal motions in the upper portion of the cervical spine. J Bone Joint Surg Am. 1964;46:1777–1779. [PubMed] [Google Scholar]
- 15.Jenkins JD, Coric D, Branch CL., Jr A clinical comparison of one- and two-screw odontoid fixation. J Neurosurg. 1998;89:366–370. doi: 10.3171/jns.1998.89.3.0366. [DOI] [PubMed] [Google Scholar]
- 16.Kazan S, Tuncer R, Sindel M. Percutaneous anterior odontoid screw fixation technique. A new instrument and a cadaveric study. Acta Neurochir (Wien) 1999;141:521–524. doi: 10.1007/s007010050334. [DOI] [PubMed] [Google Scholar]
- 17.Lind B, Sihlbom H, Nordwall A. Halo-vest treatment of unstable traumatic cervical spine injuries. Spine. 1988;13:425–432. doi: 10.1097/00007632-198804000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Montesano PX, Anderson PA, Schlehr F, Thalgott JS, Lowrey G. Odontoid fractures treated by anterior odontoid screw fixation. Spine. 1991;16(Suppl):S33–S37. doi: 10.1097/00007632-199103001-00007. [DOI] [PubMed] [Google Scholar]
- 19.Pepin JW, Bourne RB, Hawkins RJ. Odontoid fractures, with special reference to the elderly patient. Clin Orthop. 1985;193:178–183. [PubMed] [Google Scholar]
- 20.Ryan MD, Taylor TK. Odontoid fractures. A rational approach to treatment. J Bone Joint Surg Br. 1982;64:416–421. doi: 10.1302/0301-620X.64B4.7096414. [DOI] [PubMed] [Google Scholar]
- 21.Sasso R, Doherty BJ, Crawford MJ, Heggeness MH. Biomechanics of odontoid fracture fixation. Comparison of the one- and two-screw technique. Spine. 1993;18:1950–1953. doi: 10.1097/00007632-199310001-00004. [DOI] [PubMed] [Google Scholar]
- 22.Schweigel JF. Management of the fractured odontoid with halo-thoracic bracing. Spine. 1987;12:838–839. doi: 10.1097/00007632-198711000-00002. [DOI] [PubMed] [Google Scholar]
- 23.Subach BR, Morone MA, Haid RW, Jr, McLaughlin MR, Rodts GR, Comey CH. Management of acute odontoid fractures with single-screw anterior fixation. Neurosurgery. 1999;45:812–819. doi: 10.1097/00006123-199910000-00015. [DOI] [PubMed] [Google Scholar]
- 24.Wang GJ, Mabie KN, Whitehill R, Stamp WG. The nonsurgical management of odontoid fractures in adults. Spine. 1984;9:229–230. doi: 10.1097/00007632-198404000-00001. [DOI] [PubMed] [Google Scholar]