Abstract
Regular hooks lack initial fixation to the spine during spinal deformity surgery. This runs the risk of posterior hook dislodgement during manipulation and correction of the spinal deformity, that may lead to loss of correction, hook migration, and post-operative junctional kyphosis. To prevent hook dislodgement during surgery, a self-retaining pedicle hook device (SPHD) is available that is made up of two counter-positioned hooks forming a monoblock posterior claw device. The initial segmental posterior fixation strength of a SPHD, however, is unknown. A biomechanical pull-out study of posterior segmental spinal fixation in a cadaver vertebral model was designed to investigate the axial pull-out strength for a SPHD, and compared to the pull-out strength of a pedicle screw. Ten porcine lumbar vertebral bodies were instrumented in pairs with two different instrumentation constructs after measuring the bone mineral density of each individual vertebra. The instrumentation constructs were extracted employing a material testing system using axial forces. The maximum pull-out forces were recorded at the time of the construct failure. Failure of the SPHD appeared in rotation and lateral displacement, without fracturing of the posterior structures. The average pull-out strength of the SPHD was 236 N versus 1,047 N in the pedicle screws (P < 0.001). The pull-out strength of the pedicle screws showed greater correlation with the BMC compared to the SPHD (P < 0.005). The SPHD showed to provide a significant inferior segmental fixation to the posterior spine in comparison to pedicle screw fixation. Despite the beneficial characteristics of the monoblock claw construct in a SPHD, that decreases the risk of posterior hook dislodgement during surgery compared to regular hooks, the SPHD does not improve the pull-out strength in such a way that it may provide a biomechanically solid alternative to pedicle screw fixation in the posterior spine.
Keywords: Spinal deformities, Biomechanics, Pedicle screw, Self-retaining pedicle hook, Pull-out strength
Introduction
In spinal deformity surgery, a solid fixation of the instrumentation to the posterior thoracic and lumbar spinal structures can be achieved by the use of pedicle-, laminar-, or transverse process hooks or by the use of pedicle screws [3, 8]. Pedicle screws are generally used in the lumbar spine, however, both multiple segmental hooks and pedicle screws may be used in the thoracic spine. The choice to use either multiple segmental hooks or pedicle screws in the thoracic spine depends not only on the aimed amount of deformity correction and the associated risk of complications, but also on the biomechanical properties of both hooks and screws [16, 19].
From a biomechanical point of view, there is a principal difference in initial implant fixation to the posterior spine between hooks and pedicle screws. Pedicle screws immediately provide a solid segmental implant fixation to the posterior spine whereas hooks lack the property of an initial solid segmental implant fixation to the posterior spine. A solid posterior fixation to the spine with regular hooks can only be obtained after tightening of two opposite hooks to the rod in distraction or compression [21]. Obviously, all hook–rod and screw–rod connections have to be loosened temporarily during correction of the spinal deformity to allow translation and rotation of the rod in relation to the hooks and screws.
A frequently encountered problem with regular hooks during manipulation and correction of spinal deformities is posterior hook dislodgement, sometimes with fracturing of the lamina or transverse process. Hook dislodgement leads inevitably to diminished fixation of the rod to the posterior spine, with a risk of peri- and postoperative loss of correction, medial hook migration in the spinal canal, and post-operative junctional kyphosis [4, 8, 9, 14, 19, 24].
In order to obtain initial segmental hook fixation to the posterior structures of the spine and to prevent hook dislodgement during manipulation and correction of spinal deformities, a specialized self-retaining pedicle hook device (SPHD) is available. Theoretically, such a SPHD establishes an initial solid segmental fixation to the posterior structures of the spine, however, data concerning the biomechanical properties of such a SPHD are not available.
Initial segmental fixation of a SPHD to the posterior structures of the spine can be assessed by measurement of the posterior pull-out strength of such a device. The aim of this study is to test the posterior pull-out strength of a SPHD against pedicle screw fixation—a well accepted segmental posterior fixation method—in a cadaver vertebral model.
Materials and methods
Biomechanical testing was performed on ten fresh-frozen vertebrae (L2–L4) harvested from six immature pigs (weight 60–80 kg). All the animals were healthy before they were sacrificed, and none had been exposed to any factor that could affect to the bone quality. Each vertebrae was carefully disarticulated and meticulously cleaned of all remaining soft tissue. The moisture condition of the vertebrae was preserved with 0.9% saline until they were stored. The vertebrae were stored at minus 25°C until the moment they were used for the test.
Before testing, the bone mineral content (BMC) of each vertebral body was measured after they were thawed to room temperature. The BMC was determined using dual energy X-ray absorptiometry (DEXA; QDR 2000, Hologic Corporation, Waltham, MA, USA). The segments were scanned in the anteroposterior direction. The BMC was used as a measure for the bone mineral density (BMD).
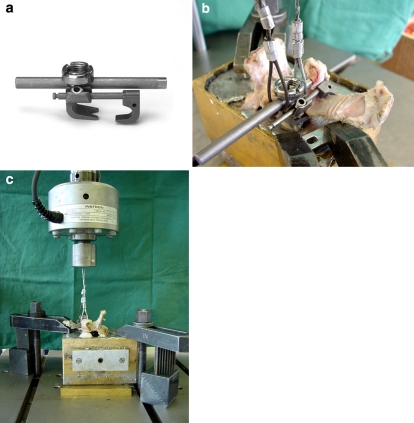
The SPHD and the pedicle screws (spine system evolution (SSE), B/Braun Aesculap, Tuttlingen, Germany) were tested in pairs in one vertebrae to exclude any influence of the BMD. The SPHD is made up of two counter-positioned hooks forming a fixed claw that grips part of the posterior spine solidly (Fig. 1a): a cranially positioned and caudally directed supratransverse hook with a connecting pin, and a caudally positioned and a cranially directed pedicle hook with both a central open slot for rod fixation and a lateral open slot for the above mentioned connection pin fixation. For pedicle screw fixation, a 5 mm diameter and 30 mm length monoaxial pedicle screw was used. The length of the screw was approximately 80% of the depth of the vertebral body, and the pedicle screw proved to fill the lumbar pig vertebral pedicle for > 70% in all vertebrae. The pedicle screws were inserted according to the standard procedure with the awl, probe finder and probe feeler by direct visual control and by using an image intensifier. A tap was not used. All pedicle screws were controlled and documented by radiographs in two directions, and proved to be in the centre of the pedicle.
Fig. 1.
a The self-retaining pedicle hook device (SPHD) consists of two counter-positioned hooks fixed by a connecting pin, forming a claw that grips the posterior vertebral segment firmly. b Specimen with the SPHD potted in a bismuth alloy before applied axial pull-out forces. c Materials testing system with the specimens potted in a bismuth alloy and the vertebral body positioned so that the flat surface of the bismuth was perpendicular to the pedicle before applied axial pull-out forces on the SPHD
In preparation to biomechanical testing, the vertebral bodies were thawed to room temperature. Each vertebra was potted in a casting-mould and buried in a low-melting-point bismuth alloy (Sonderweichlot 301, A 301, Degussa AG, Wolfgang, Germany; melting point 48°C), so that the posterior wall of the vertebral body, the pedicle and the lamina were left unexposed to the bismuth (Fig. 1b). The vertebral body was rotated in the axial direction, so that the flat surface of the bismuth was perpendicular to the pedicle, in order to have the pull-out forces along the axis of the pedicle. Screws were tested first, since we suspected that testing of the hooks might damage the posterior structures of the vertebrae. The casting-mould was perpendicular placed under the testing machine (Instron 8872, Corp., Canton, MA, USA).
A short rod was inserted into the head of the pedicle screw or into the head of the SPHD and fixed with a closure screw. The pull-out force was directed perpendicular to the short rod along the axis of the screw or SPHD head, by using an iron wire with a constant displacement rate of 5 mm/min (Fig. 1c). While pulling, the load and displacements values were entered in the computer ten times a second and data acquisition was performed through materials testing software (Fast Track 2, Instron Corporation). The pull-out force was applied until the bone-implant system broke. From the obtained force-deformation curves, the pull-out strength was calculated. The pull-out strength was defined as the maximum force in Newtons until failure. Failure was defined as the point at which maximum load was recorded in the load displacement curves for each specimen. Values of pull-out strength were corrected for the BMC, and are shown as mean ± standard deviation. In order to estimate the role of bone density on the fixation strength, the correlation between BMC and the pull-out strength of both, the pedicle screw and the SPHD, were calculated. Paired t test was performed to compare the mean pull-out strength between the pedicle screw group and the SPHD group. For all statistical tests, the significance level was set at a P value less than 0.05.
Results
Failure of the pedicle screw fixation and SPHD fixation as occurred with the maximum pull-out force was macroscopically analysed. In all cases the screw broke out by failure of the screws to anchor in the bone and pedicle without fracturing the posterior structures of the vertebral body. Failure of the SPHD occurred by rotation and lateral displacement of the claw, without fracturing the lamina in nine out of the ten cases.
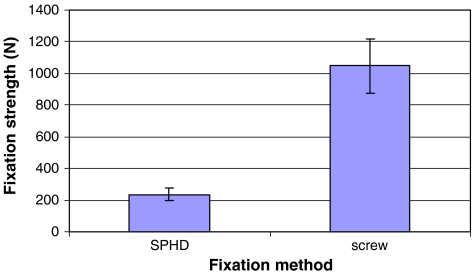
In the load displacement curves recorded for each specimen, the load peak was always the highest followed by a significant drop in load. The average load to failure of the ten measurements for the SPHD and the pedicle screws are presented in Fig. 2. The average load to failure of the pedicle screws was 1,046.8 ± 173.1 N (n = 10) and 236.2 ± 39.8 N for the SPHD (P < 0.001). The average BMC of the vertebrae was 0.735 ± 0.060 g/cm2. The pull-out strength of the pedicle screws showed greater correlation with the BMC (R2 = 0.4811) compared to the pull-out strength of the SPHD and the BMC (R2 = 0.1343).
Fig. 2.
Load to failure shown as mean ± standard deviation of the ten measurements for the SPHD and the pedicle screws
Discussion
The SPHD is a segmental posterior fixation device aimed to avoid the risk of hook dislodgement during manipulation and correction of spinal deformities. The aim of the present study was to investigate the biomechanical properties of the SPHD that may provide an alternative to segmental pedicle screw fixation in the posterior spine. This was performed by testing the axial pull-out strength of the SPHD against pedicle screw fixation, a well accepted segmental posterior fixation method in spinal deformity surgery.
The results of this biomechanical study showed that the resistance to pull-out forces of a SPHD was significantly inferior to that of a pedicle screw. The pull-out strength of the SPHD proved to be 23% of the pull-out strength of the pedicle screw. These results are comparable to other studies [15, 21]. Both Liljenqvist and Roach showed in separate studies inferior pull-out forces of regular hooks in comparison to pedicle screw fixation [15, 21]. However, the average pull-out strength of the SPHD in our study was found less than previously reported pull-out strength with regular hooks. These differences may be explained by a different study protocol. Firstly, in their studies both Liljenqvist and Roach reported the pull-out forces of regular hooks in a double-hook claw configuration after tightening the hooks to the rod in compression [15, 21]. In these studies, the pull-out force is applied to a double-hook claw construct and the pull-out force is directed centrically above the lamina without any possible rotation. With the use of a SPHD, however, the pull-out force is applied to the head of the pedicle hook that is located more caudally to the pedicle and the lamina. As a result of the laterosuperior location of the counter-positioned hook, the pull-out forces resulted in a lateral rotating movement of the SPHD, centred around the pedicle. Therefore, the biomechanics of a single hook–rod fixation in a SPHD cannot be compared with a double-hook claw configuration. Secondly, former studies reported pull-out measurements on fresh human thoracic vertebrae. We performed our biomechanical pull-out measurements on immature lumbar pig cadaver vertebrae, since fresh human vertebrae were not available at our institute. We chose for lumbar pig vertebrae because they show to be most closely modelled to the human L4 vertebrae [18]. The thoracic spine of a pig could not be used because of the enormous anatomical differences. As a result, the absolute biomechanical measurements of a pig cadaver vertebral model cannot be compared with biomechanical measurements in fresh human thoracic vertebrae.
We found a correlation between the pull-out strength and the BMD. The correlation between the pull-out strength and the BMD in pedicle screw fixation was significant (48%), which is consistent with the results of previous studies [6, 11, 12]. The correlation we found between the pull-out strength of the SPHD and the BMD was 13%. This low correlation of the pull-out strength with hooks corresponds with results found by Hackenberg [11].
The pull-out strength was measured successively on the pedicle screw and SPHD in each vertebral body until the bone-implant system broke. We tested the pedicle screws first, since we expected damage of the posterior structures of the vertebrae caused by the pull-out of the SPHD. Nevertheless, the bone-implant failure of the SPHD proved to occur without fracture of the posterior structures in nine out of the ten tests. In addition, all screws were pulled out linearly, without any macroscopic damage to the posterior structures of the vertebral body.
The failure mechanism of the SPHD proved to be in rotation without fracturing of the posterior spinal structures. This can be explained by the eccentric position of the hook-rod fixation in relation to the point of force application on the posterior spinal structures. The head of the hook-rod fixation of the SPHD is located caudally to the pedicle and lamina (Fig. 1a). During the applied pull-out forces at the SPHD, rotation of the connecting pin inside the hook occurred, resulting in rotation and lateral displacement of the SPHD. Thus the failure modus of the SPHD was a rotational dislodgment of the connecting pin inside the hook. The implant itself proved to be the weak point of the construct and not the fixation to the bone. The advantage of this failure mechanism, however, is the prevention of damaging the posterior fixation structures of the spine in case of applying more than approximately 200 N on the SPHD during manipulation and correction of the spinal deformity. Revision of the pin-hook connection deign of the SPHD may prevent rotation of the connecting pin inside the hook and improve the pull-out strength of the device. Finally, after tightening the SPHD in distraction or compression to the rod, the pedicle hook acts as a regular pedicle hook and can be compared biomechanically to all other regular pedicle hooks.
Holding forceps, rod fixation clamps, hook protectors, or special blockers have been developed to fix a regular hook to the posterior spine temporally. However, these instruments disturb the surgical field and tend to dislodge the hook as a result of the long lever arm. Augmentation of the pedicle hook to the lamina and pedicle by a small screw has been proposed for pedicle hook fixation [1, 2, 5–7]. These special pedicle hooks solve these disadvantages of regular hooks partially, however, fixation of a small screw in the same pedicle that is used for the pedicle hook fixation weakens the pedicle and increases the risk of pedicle fracture [6, 10]. In addition, the direction of forces during manipulation and correction cannot be applied in all directions. Recently, the use of pedicle screws has been advised in the thoracic spine for spinal deformity surgery [22, 23]. However, upper thoracic pedicle screws are still controversial in the treatment of spinal deformities. Misplacement of the pedicle screw in the thoracic spine has been reported up to 25% of cases [17]. Not only does this end in poor fixation but also in neurologic and vascular complications [13, 20, 25].
Obviously, measurements of axial pull-out strength describes only one of the force directions expressed on the SPHD during manipulation and correction of spinal deformities throughout surgery. In clinical practice, laterally directed forces and rotation will be applied also to the implant before tightening. Additional standardised measurements of the SPHD in all dimensions are necessary to assess the complete biomechanical properties of such a device. However, this proposal has not yet been evaluated as a guideline for studying load failure of posterior spinal implants.
In conclusion, the SPHD showed to provide a significantly weaker segmental fixation to the posterior spine in comparison to pedicle screw fixation. Despite the fact that the characteristics of this monoblock claw construct in a SPHD provides evident practical benefits to regular hooks during the surgical procedure, it does not improve the pull-out strength in such a way that it may provide a biomechanically solid alternative to pedicle screw fixation in the posterior spine.
Acknowledgments
Acknowledgments to B/Braun Aesculap Netherlands for providing the implants. There was no financial assistance provided. Non of the authors has any financial interest in B/Braun Aesculap or any of the material presented.
References
- 1.Arlet V, Marchesi D, Aebi M. Correction of adolescent idiopathic thoracic scoliosis with a new type of offset apical instrumentation: preliminary results. J Spinal Disord. 1998;11:404–409. doi: 10.1097/00002517-199810000-00007. [DOI] [PubMed] [Google Scholar]
- 2.Arlet V, Papin P, Marchesi D, Aebi M. Adolescent idiopathic thoracic scoliosis: apical correction with specialized pedicle hooks. Eur Spine J. 1999;8:266–271. doi: 10.1007/s005860050171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barr SJ, Schuette AM, Emans JB. Lumbar pedicle screws versus hooks. Results in double major curves in adolescent idiopathic scoliosis. Spine. 1997;22:1369–1379. doi: 10.1097/00007632-199706150-00016. [DOI] [PubMed] [Google Scholar]
- 4.Been HD, Kalkman CJ, Traast HS, Ongerboer dV Neurologic injury after insertion of laminar hooks during Cotrel-Dubousset instrumentation. Spine. 1994;19:1402–1405. doi: 10.1097/00007632-199404150-00021. [DOI] [PubMed] [Google Scholar]
- 5.Berlemann U, Cripton P, Nolte LP, Lippuner K, Schlapfer F. New means in spinal pedicle hook fixation. A biomechanical evaluation. Eur Spine J. 1995;4:114–122. doi: 10.1007/BF00278923. [DOI] [PubMed] [Google Scholar]
- 6.Berlemann U, Cripton PA, Rincon L, Nolte LP, Schlapfer F. Pull-out strength of pedicle hooks with fixation screws: influence of screw length and angulation. Eur Spine J. 1996;5:71–73. doi: 10.1007/BF00307831. [DOI] [PubMed] [Google Scholar]
- 7.Berlet GC, Boubez G, Gurr KR, Bailey SI. The USS pedicle hook system: a morphometric analysis of its safety in the thoracic spine. Universal Spine System. J Spinal Disord. 1999;12:234–239. [PubMed] [Google Scholar]
- 8.Bridwell KH. Spinal instrumentation in the management of adolescent scoliosis. Clin Orthop Relat Res. 1997;335:64–72. [PubMed] [Google Scholar]
- 9.Bridwell KH, Hanson DS, Rhee JM, Lenke LG, Baldus C, Blanke K. Correction of thoracic adolescent idiopathic scoliosis with segmental hooks, rods, and Wisconsin wires posteriorly: it’s bad and obsolete, correct? Spine. 2002;27:2059–2066. doi: 10.1097/00007632-200209150-00018. [DOI] [PubMed] [Google Scholar]
- 10.Cohen-Gadol AA, Dekutoski MB, Kim CW, Quast LM, Krauss WE. Safety of supplemental endplate screws in thoracic pedicle hook fixation. J Neurosurg. 2003;98:31–35. doi: 10.3171/spi.2003.98.1.0031. [DOI] [PubMed] [Google Scholar]
- 11.Hackenberg L, Link T, Liljenqvist U. Axial and tangential fixation strength of pedicle screws versus hooks in the thoracic spine in relation to bone mineral density. Spine. 2002;27:937–942. doi: 10.1097/00007632-200205010-00010. [DOI] [PubMed] [Google Scholar]
- 12.Halvorson TL, Kelley LA, Thomas KA, Whitecloud TS, III, Cook SD. Effects of bone mineral density on pedicle screw fixation. Spine. 1994;19:2415–2420. doi: 10.1097/00007632-199411000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Kothe R, Panjabi MM, Liu W. Multidirectional instability of the thoracic spine due to iatrogenic pedicle injuries during transpedicular fixation. A biomechanical investigation. Spine. 1997;22:1836–1842. doi: 10.1097/00007632-199708150-00008. [DOI] [PubMed] [Google Scholar]
- 14.Krag MH. Biomechanics of thoracolumbar spinal fixation. A review. Spine. 1991;16:S84–S99. doi: 10.1097/00007632-199103001-00014. [DOI] [PubMed] [Google Scholar]
- 15.Liljenqvist U, Hackenberg L, Link T, Halm H. Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Acta Orthop Belg. 2001;67:157–163. [PubMed] [Google Scholar]
- 16.Liljenqvist U, Lepsien U, Hackenberg L, Niemeyer T, Halm H. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336–343. doi: 10.1007/s00586-002-0415-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine. 1997;22:2239–2245. doi: 10.1097/00007632-199710010-00008. [DOI] [PubMed] [Google Scholar]
- 18.McLain RF, Yerby SA, Moseley TA. Comparative morphometry of L4 vertebrae: comparison of large animal models for the human lumbar spine. Spine. 2002;27:E200–E206. doi: 10.1097/00007632-200204150-00005. [DOI] [PubMed] [Google Scholar]
- 19.Muschik M, Schlenzka D, Robinson PN, Kupferschmidt C. Dorsal instrumentation for idiopathic adolescent thoracic scoliosis: rod rotation versus translation. Eur Spine J. 1999;8:93–99. doi: 10.1007/s005860050136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Papin P, Arlet V, Marchesi D, Rosenblatt B, Aebi M. Unusual presentation of spinal cord compression related to misplaced pedicle screws in thoracic scoliosis. Eur Spine J. 1999;8:156–159. doi: 10.1007/s005860050147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Roach JW, Ashman RB, Allard RN. The strength of a posterior element claw at one versus two spinal levels. J Spinal Disord. 1990;3:259–261. doi: 10.1097/00002517-199009000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Suk SI, Kim WJ, Lee SM, Kim JH, Chung ER. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine. 2001;26:2049–2057. doi: 10.1097/00007632-200109150-00022. [DOI] [PubMed] [Google Scholar]
- 23.Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine. 1995;20:1399–1405. doi: 10.1097/00007632-199506000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Ooy A, Geukers CW. Results of CD operation in idiopathic scoliosis. Acta Orthop Belg. 1992;58(Suppl 1):129–133. [PubMed] [Google Scholar]
- 25.Vanichkachorn JS, Vaccaro AR, Cohen MJ, Cotler JM. Potential large vessel injury during thoracolumbar pedicle screw removal. A case report. Spine. 1997;22:110–113. doi: 10.1097/00007632-199701010-00018. [DOI] [PubMed] [Google Scholar]