Abstract
Erythrocyte glutathione depletion has been linked to hemolysis and oxidative stress. Glutamine plays an additional antioxidant role through preservation of intracellular nicotinamide adenine dinucleotide phosphate (NADPH) levels, required for glutathione recycling. Decreased nitric oxide (NO) bioavailability, which occurs in the setting of increased hemolysis and oxidative stress, contributes to the pathogenesis of pulmonary hypertension (PH) in sickle cell disease (SCD). We hypothesized that altered glutathione and glutamine metabolism play a role in this process. Total glutathione (and its precursors) and glutamine were assayed in plasma and erythrocytes of 40 SCD patients and 9 healthy volunteers. Erythrocyte total glutathione and glutamine levels were significantly lower in SCD patients than in healthy volunteers. Glutamine depletion was independently associated with PH, defined as a tricuspid regurgitant jet velocity (TRV) of at least 2.5 m/s. The ratio of erythrocyte glutamine:glutamate correlated inversely to TRV (r = −0.62, P < .001), plasma arginase concentration (r = −0.45, P = .002), and plasma-free hemoglobin level (r = −0.41, P = .01), linking erythrocyte glutamine depletion to dysregulation of the arginine-NO pathway and increased hemolytic rate. Decreased erythrocyte glutathione and glutamine levels contribute to alterations in the erythrocyte redox environment, which may compromise erythrocyte integrity, contribute to hemolysis, and play a role in the pathogenesis of PH of SCD.
Introduction
The erythrocyte redox environment may contribute to the increased oxidative stress, hemolysis, and decreased nitric oxide (NO) bioavailability observed in pulmonary hypertension (PH), a common complication of hemolytic disorders. Reduced glutathione (gamma-glutamyl-cysteinyl-glycine; GSH) is the most abundant low-molecular weight thiol1 and the principal thiol redox buffer in erythrocytes.2,3 The red blood cell contributes up to 10% of whole-body GSH synthesis in humans.4–6 In addition to its role as a critical antioxidant, GSH possesses diverse biological functions involved in detoxification, cell proliferation and apoptosis, redox signaling, gene expression, protein glutathionylation, cytokine production, the immune response, mitochondrial function, and integrity as well as NO metabolism.7,8
Glutathione is synthesized from glutamate, cysteine, and glycine via reactions catalyzed by 2 cytosolic enzymes, gamma-glutamylcysteine ligase and GSH synthetase. The intracellular GSH concentration is the final result of a dynamic balance between the rate of GSH synthesis and the combined rate of intracellular GSH consumption and efflux. GSH is readily oxidized to glutathione disulfide (GSSG) by free radicals and reactive oxygen and nitrogen species. GSSG efflux from cells contributes to a net loss of intracellular GSH.1
Due to its high intracellular concentrations, GSH variations in oxidation states can significantly modify the redox environment of red blood cells. Within the erythrocyte, GSH may act as an antioxidant in scavenging reactive oxygen or nitrogen species, as a reductant to maintain protein thiols in a reduced state, or, conversely, as an adjunct in forming mixed disulfides with proteins.1,9,10 Extensive oxidation of intracellular GSH promotes oxidative damage to protein and lipids and compromises structural integrity of the red blood cell.
To prevent intracellular GSH loss, erythrocytes have a robust capacity for de novo GSH synthesis and for reducing GSSG. Since de novo synthesis of GSH is energetically expensive, efficient reduction of oxidized forms of GSH is absolutely essential. In all mammalian cells, electrons required for reducing GSSG or GSH mixed disulfides of proteins are principally derived from nicotinamide adenine dinucleotide phosphate (NADPH). The red blood cell (RBC) pentose phosphate pathway catalyzes the reduction of NADP to NADPH and is principally important to maintain sufficient NADPH pool needed for GSSG reduction. Additionally, NADP de novo synthesis also plays a significant role in maintaining the redox capacity of the NADPH/NADP couple.11 Thus, adequate recycling of GSH is dependent upon many factors, one ofwhich is NADPH bioavailability. Glutamine, an essential precursor in NADPH biosynthesis, is metabolized to the GSH substrate glutamate in the process of NADPH production.12 Glutamine thus plays an antioxidant role through preservation of intracellular NADPH, making it an important amino acid for GSH homeostasis.
Cellular GSH concentrations are significantly reduced in response to protein malnutrition, oxidative stress, aging, and many pathologic conditions,1,10 including sickle cell disease (SCD),13–18 a hemoglobinopathy associated with vasoocclusive and hemolytic complications.19–26 Sickle erythrocytes have a shortened survival time and are more susceptible to oxidant damage than red blood cells from healthy individuals.27–31 Many of the alterations in the redox environment known to occur in SCD can impact global GSH homeostasis, including decreased enzymatic activity of glutathione peroxidase,27,28 catalase28 and GSH reductase,15–17,32 impaired pentose phosphate shunt activity,32 increased superoxide and free radical generation,16,29,33–37 decreased NO bioavailability,20,21,23,38–45 and decreased NAD redox potential.46,47 Recently, erythrocyte GSH depletion has been linked to hemolysis, suggesting a direct role in erythrocyte viability.48
Erythrocyte GSH loss could be due to a variety of factors, including low substrate availability, dysfunctional GSH recycling, increased GSH consumption in a milieu of oxidative stress, increased efflux of GSSH, or a combination of these events. We hypothesized that altered glutathione and glutamine metabolism may play a role in hemolysis and the pathogenesis of PH related to SCD.
Methods
Subject recruitment and clinical evaluation
Subjects were recruited as part of the ongoing PH in SCD study approved by the Institutional Review Board at Boston Medical Center. SCD patients were enrolled when clinically stable during outpatient clinic visits. For this study, samples from only Hb-SS patients (SCD) and age- and racially matched healthy (Hb-AA) volunteers without coexistent cardiopulmonary disease were analyzed. After informed consent was obtained in accordance with the Declaration of Helsinki, all subjects underwent a screening questionnaire assessing their cardiopulmonary symptomatology, procurement of a blood sample, and a two-dimensional echocardiogram (Sonos 5500; Hewlett Packard, Palo Alto, CA). Standard M-mode measurements of the left and right atria and ventricles were made as described previously.49 The pulmonary artery systolic pressure (PASP) was estimated using the modified Bernoulli equation (p = 4V2 + right atrial pressure) to calculate pressure based upon the flow of the tricuspid regurgitant jet. PH was defined as a tricuspid regurgitant jet velocity (TRV) of at least 2.5 m/s (corresponding to a PASP ≥ 35 mmHg). It remains controversial as to whether the mortality risk in SCD associated with a TRV of at least 2.5 m/s26 reflects a causal relationship between PH and mortality per se or whether this represents a biomarker for disease severity. However, for the purposes of this study, PH in SCD is indicated by a TRV of at least 2.5 m/s,26 as this represents a group of high-risk patients.
Preparation of platelet-poor plasma and erythrocytes
At the time of study enrollment, peripheral blood samples were obtained in heparinized syringes, placed on ice, and centrifuged immediately at 2000g for 15 minutes at 4°C. Platelet-poor plasma was obtained by centrifuging the supernatant at 20 000g for 20 minutes43,50,51 and stored at −70°C until experimentation. For isolation of erythrocytes, the pellet was resuspended in saline and centrifuged at 2000g for 8 minutes. After removal of the supernatant, the pellet was resuspended in saline and centrifuged at 2000g for an additional 8 minutes. Samples were stored at −20°C until experimentation.
Study design
Glutamine, total glutathione (GSH + GSSG), and its precursors (glutamate, cysteine, and glycine) were assayed in the erythrocytes of 40 SCD patients and 9 controls. Arginase concentration and cell-free hemoglobin were determined in plasma for all patients. Plasma quantitative amino acids and total glutathione analysis were measured in 25 patients with SCD and 7 controls.
High-pressure liquid chromatography-linked tandem mass spectrometry
Cysteine (Cys), glutathione (GSH), glutathione-disulfide (GSSG), glycine (Gly), glutamine (Gln), and glutamate (Glu) of highest analytical grade were purchased from Sigma (St Louis, MO). Stable isotopes, cysteine (3,3,3′3′-D4), and glycine (13C2, 15N) were purchased from Cambridge Isotopes (Andover, MA). All HPLC solvents were of the analytical grade available from Fisher Scientific (Hampton, NH). Materials used for derivatization and HPLC reverse phase columns were part of the EZ-FAAST kit available from Phenomenex (Torrance, CA). Erythrocytes (20 μL of packed cells) were mixed with 180 μL of 5% perchloric acid (PCA) containing 1 mM diethylenetriamene pentaacetate (DTPA) and centrifuged at 13 000 rpm for 5 minutes. Acid soluble supernatant was collected and used for high-pressure liquid chromatography-linked tandem mass spectrometry (LC/MS/MS) analysis. Metabolites (see Table S1, available on the Blood website; see the Supplemental Materials link at the top of the online article) were detected using LC/MS/MS following derivatization with isopropylchloroformate, based on methods previously published by Husek et al,52 with the following modifications. An aliquot of culture media and cell pellets (1 × 106 cells) were mixed with equal volume of 10% PCA containing 1 mM DTPA. From these samples, the acid-soluble supernatants were collected following centrifugation at 14 000 rpm for 5 minutes. To the acidified supernatants, internal standard mix (Table S1, 10 μM) was added as an internal control, and solid phase extractions with a strong cation exchange resin (Phenomenex) were performed. Serum amino acid (SAA) metabolites were eluted with 100 μL elution buffer consisting of 0.1 N NaOH, 40% N-propanol, and 10% pyridine and mixed with 50 μL of derivatizing solution consisting of isooctane, chloroform, and isopropylchloroformate (75:40:10). The derivatized products were subsequently extracted with 200 μL isooctane and dried under a constant stream of nitrogen. Samples were reconstituted with a mobile phase consisting of methanol and water (80:20, v/v). Chromatographic separation of SAA metabolites was performed on C18 reversed-phase column (25 × 2 mm, 0.3 μm) from Phenomenex. The separation was performed under isocratic condition at a flow rate of 0.2 mL/min. Electrospray tandem mass spectrometric analysis was performed on Quattro Micro mass spectrometer from Micromass (Milford, MA) and analyzed using Masslinks software (v 3.1). Analytes were detected using the multiple reaction monitoring (MRM) scanning mode. The specific cone voltage and collision energy used for each metabolite is provided in Table S1, which also lists all of the internal standards used for quantification. Accurate quantification of thiol amino acid redox states is technically challenging.53 Details summarizing techniques used to maximize accuracy of glutathione measurements are found in Document S1.
Arginase concentration
Arginase concentration was measured using a double monoclonal sandwich enzyme immunoassay (ELISA) for the quantitative measurement of human liver-type arginase in serum (BioVendor Laboratory Medicine, Chandler, NC) according to the manufacturer's protocol.
Plasma-free hemoglobin
A human hemoglobin ELISA kit (Bethyl Laboratories, Montgomery, TX) was used to quantitatively measure concentrations according to the manufacturer's protocol.
Statistical analysis
All data analysis was performed on STATA version 10.0 (College Station, TX.) Results are expressed as means plus or minus SD unless otherwise specified. The paired t test and Pearson correlations were used to identify significant relationships between variables. Student t test with Welch correction was used when data sets demonstrated unequal variance. Cuzick rank sum test for trends was used when specified. Categorical data were analyzed using chi-square analysis and the Fisher exact test where appropriate. Multiple linear regression with a backward stepwise procedure was used to identify variables that were independently associated with TRV. Kruskal-Wallis and Mann-Whitney rank sum testing were used to confirm the most important correlates. A P value less than or equal to .05 was considered statistically significant.
Results
Subject characteristics
Blood samples and clinical information from 40 Hb-SS and 9 Hb-AA subjects aged 18 years and older were obtained (Tables 1, 2). Both the Hb-SS patients and healthy volunteers were predominantly female and of a similar age distribution. As would be expected, the Hb-SS patients had significantly higher TRV than the healthy volunteers (2.22 ± 0.41 vs 1.69 ±0.16 m/s, P < .001). Age was associated with rising TRV (r = 0.33, P = .04). Approximately 35% of both the Hb-SS patients with PH and without PH were taking hydroxyurea at the time of their study. None of the SCD subjects were on chronic transfusion therapy. Of the 17 patients with a TRV of at least 2.5 m/s, 14 had mild-moderate PH with a TRV of 2.5 to 2.9 m/s, while 3 patients had severe PH with a TRV of more than 3 m/s (range, 3.0-3.5 m/s), based on categories established by Gladwin and colleagues.26 All of the Hb-AA volunteers had normal echocardiograms and were asymptomatic. None of the recruited subjects were diabetic, alcohol abusers, or had a significant smoking history.
Table 1.
Summary of demographics for all subjects
| Hb-AA (n = 9) | Hb-SS (n = 40) | P | |
|---|---|---|---|
| Age, y (± SD) | 23.1 (± 6.3) | 28.5 (± 10.9) | .15 |
| Female, % | 78 | 60 | .32 |
| TRV, m/s (± SD) | 1.69 (± 0.16) | 2.22 (± 0.41) | <.001 |
Table 2.
Summary of clinical data for Hb-SS subjects
| TRV 2.5 m/s or over (n = 17) | TRV under 2.5 m/s (n = 23) | P | |
|---|---|---|---|
| Age, y (± SD) | 35.1 (± 13.2) | 29.6 (± 8.3) | .14 |
| Female, % | 71 | 52 | .24 |
| WHO/NYHA Class, % | — | ||
| I | 52.9 | 60.9 | .09 |
| II | 17.7 | 34.8 | — |
| III | 29.4 | 4.4 | — |
| TRV, m/s (± SD) | 2.59 (± 0.29) | 1.98 (± 0.21) | <.001 |
| Hydroxyurea use, % | 35.3 | 34.8 | .97 |
WHO/NYHA indicates World Health Organization/New York Heart Association; and —, not applicable.
Total glutathione levels
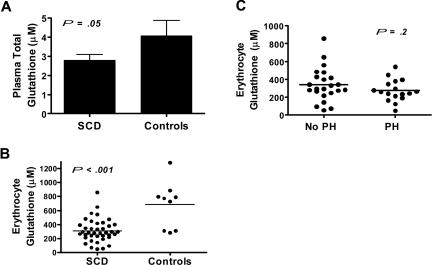
Total glutathione (GSH + GSSG) levels in plasma and within the erythrocyte were significantly lower in patients with SCD compared with healthy volunteers (Figure 1A,B). Severity of erythrocyte glutathione deficiency was similar in patients with PH when compared with those without PH (Figure 1C). Plasma and erythrocyte total glutathione levels did not correlate with TRV, age, blood pressure, plasma arginase concentration, or plasma-free hemoglobin level.
Figure 1.
Total glutathione level in patients with sickle cell disease compared with healthy controls and its association with pulmonary hypertension. Total glutathione (GSH + GSSG) levels in (A) plasma and (B) within the erythrocyte were significantly lower in patients with sickle cell disease (SCD, n = 40) compared with healthy volunteers (controls, n = 9). (C) Severity of erythrocyte glutathione deficiency was similar in patients with pulmonary hypertension (PH) when compared with those without PH (No PH)
Glutathione precursors (glutamate, cysteine, and glycine)
Plasma and erythrocyte GSH precursor concentrations in SCD and control samples are listed in Tables 3,4. Erythrocyte cysteine, the rate-limiting amino acid in GSH synthesis, did not correlate with total erythrocyte glutathione levels, implicating other mechanisms in erythrocyte GSH depletion. Levels of GSH amino acid precursors were similar in SCD patients with PH compared with those without PH.
Table 3.
Altered glutamine and glutathione precursors in plasma of SCD patients compared with healthy volunteers
| GSH precursors (μM) | Plasma |
||
|---|---|---|---|
| Controls | SCD | P | |
| Glutamate | 9 ± 2 | 18 ± 2 | .006* |
| Cysteine | 238 ± 15 | 267 ± 16 | .4 |
| Glycine | 32 ± 4 | 53 ± 4 | .01 |
| Glutamine | 708 ± 60 | 825 ± 55 | .3 |
Data are shown as average plus or minus SEM.
Unpaired t test performed with Welch correction for unequal variance.
Table 4.
Altered glutamine and glutathione precursors in erythrocytes of SCD patients compared with healthy volunteers, and in SCD patients by tricuspid regurgitant jet velocity
| GSH precursors (μM) | Erythrocytes |
SCD Erythrocyte |
||||
|---|---|---|---|---|---|---|
| Controls | SCD | P | TRV under 2.5 m/s | TRV 2.5 m/s or more | P | |
| Glutamate | 178 ± 11 | 288 ± 35 | .004* | 327 ± 49 | 235 ± 47 | .2 |
| Cysteine | 15 ± 2 | 21 ± 6 | 0.3* | 18 ± 5 | 22 ± 7 | .7 |
| Glycine | 274 ± 28 | 497 ± 63 | .002* | 519 ± 73 | 468 ± 113 | .1 |
| Glutamine | 990 ± 94 | 742 ± 99 | .08* | 934 ± 148 | 482 ± 92 | .01* |
Data are shown as average plus or minus SEM.
Unpaired t test performed with Welch correction for unequal variance.
Glutamine levels
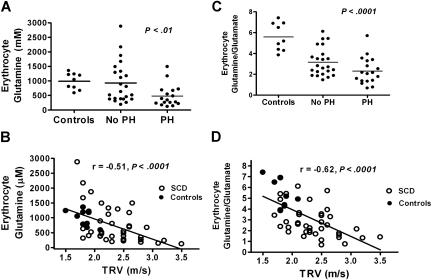
Plasma and erythrocyte glutamine levels in SCD patients and healthy volunteers are summarized in Table 3. A significant glutamine depletion occurred in SCD patients with PH compared with those without PH and healthy volunteers (Figure 2A). Glutamine levels inversely correlated with TRV (r = −0.51, P < .001, Figure 2B, including healthy volunteers, and r = −0.49, P = .001 when analyzing SCD patients only). Erythrocyte glutamine levels also correlated with age in patients with SCD (r = −0.35, P = .02). No correlations were identified with sex, hydroxyurea use, World Health Organization/New York Heart Association (WHO/NYHA) class, or systemic blood pressure.
Figure 2.
Erythrocyte glutamine depletion in sickle cell disease and its association with pulmonary hypertension. (A) Erythrocyte glutamine levels in healthy volunteers were similar to SCD patients without pulmonary hypertension (No PH, n = 23). However, glutamine levels were significantly decreased in SCD patients with a tricuspid regurgitant jet velocity (TRV) of at least 2.5 m/s on Doppler echocardiography (PH, n = 17) compared with SCD patients without PH (P < .001) and (B) erythrocyte glutamine levels inversely correlated with TRV on Doppler echocardiography (r = -0.51, P < .0001). (C) A significant reduction in the erythrocyte glutamine:glutamate ratio is identified in SCD compared with controls, with the lowest ratios identified in patients with PH. (D) The glutamine:glutamate ratio inversely correlated with TRV on Doppler echocardiography (r = −0.62, P < .001, Figure 2D), implicating glutamine bioavailability as a novel factor in the pathophysiology of PH.
Erythrocyte glutamine:glutamate ratio
A significant reduction in the erythrocyte glutamine:glutamate ratio occurred in SCD patients compared with healthy volunteers, with the lowest ratios observed in SCD patients with a TRV of at least 2.5 m/s (Figure 2C). The glutamine:glutamate ratio inversely correlated with TRV (r = −0.62, P < .001, Figure 2D including controls, r = −0.46, P = .003 in SCD patients only), implicating glutamine bioavailability as a novel factor in the pathophysiology of PH. These changes in the glutamine:glutamate ratio were predominantly caused by decreased erythrocyte glutamine levels rather than increased glutamate levels, suggesting that this was not due to increased cellular glutamate uptake. In patients with PH, the erythrocyte glutamate levels were trending downward, while glutamine levels dropped significantly (Table 4).
Erythrocyte glutamine:glutamate ratio also correlated with age in patients with SCD (r = −0.32, P = .04), while no correlations were identified with sex, hydroxyurea use, or WHO/NYHA class. However, the glutamine:glutamate ratio did correlate with diastolic blood pressure (r = 0.35, P = .02) and mean arterial pressure (r = 0.35, P = .03) in patients with SCD, while there was no association with either erythrocyte glutamine or glutamate alone. This relationship was even more robust when healthy volunteers were included in the analysis (r = 0.48, P < .001), suggesting a redox continuum in the red blood cell that may not be limited to patients with SCD. This paradoxical observation is not necessarily contradictory, given the multiple variables in addition to TRV that may independently contribute to symptomatology as reflected by the WHO/NYHA class, such as diastolic dysfunction and noncardiac etiologies of dyspnea.54 There was no association of systolic, diastolic, or mean arterial pressure with TRV or total erythrocyte glutathione levels in patients with SCD. To further investigate the relationship of blood pressure and cardiovascular disease in our patient cohort, we analyzed systemic blood pressures in patients with SCD in each category of WHO/NYHA class and found an increasing diastolic (65 ± 9, 69 ± 10, and 72 ± 11, P = .02) and mean arterial pressures (80 ± 9, 85 ± 8, and 88 ± 11, P = .08) by class severity (WHO/NHYA class I, II, and III, respectively), when analyzed by Cuzick rank sum test for trends, consistent with other published observations regarding blood pressure in SCD.26,54,55
Glutamine:glutamate ratio and markers of hemolytic rate
Plasma arginase concentration, a biomarker for hemolysis,21,22,26 was significantly higher in SCD patients compared with healthy volunteers (98 ± 17 vs 20 ± 6 ng/mL, P < .001) and strongly correlated with plasma-free hemoglobin (r = 0.85, P < .001). The glutamine:glutamate ratio, potentially a gauge of glutamine turnover, NADPH biosynthetic capacity, and oxidative stress, inversely correlated with both plasma arginase concentration (r = −0.45, P = .002) and plasma-free hemoglobin (r = −0.41, P = .01) levels, while there was no association with either glutamine or glutamate alone. This novel observation links lower erythrocyte glutamine:glutamate ratios to increased hemolysis and dysregulation of the arginine-NO pathway. No association of total erythrocyte glutathione levels and plasma arginase concentration or plasma-free hemoglobin in patients with SCD was identified, suggesting that erythrocyte glutamine bioavailability may play a greater role than GSH in erythrocyte susceptibility to oxidative stress and hemolysis.
Variables associated with tricuspid regurgitant jet velocity
The relationship between variables potentially associated with elevated TRV in patients with SCD are summarized in Table 5. Three covariants were found to be significant in this patient cohort through univariate regression analysis: erythrocyte glutamine level, erythrocyte glutamine:glutamate ratio, and age. In multiple regression analysis of TRV in patients with SCD, all variables listed in Table 5 were considered in a backward stepwise model fitting process. These regressions demonstrated that erythrocyte glutamine level remained an independent predictor of elevated TRV (n = 40, R2 = 0.24, adjusted P = .001 for all independent variables) and the only variable to maintain significance. A similar backwards stepwise regression analysis was performed to identify variables associated with erythrocyte glutamine levels and erythrocyte glutamine:glutamate ratio in patients with SCD. Covariates included in this model were TRV, diastolic blood pressure, age, plasma arginase concentration, WHO/NYHA class, sex, and hydroxyurea use. Only TRV was determined to be an independent predictor of erythrocyte glutamine depletion (P = .002), while both TRV and diastolic blood pressure were independently associated with erythrocyte glutamine:glutamate ratio (n = 40, R2 = 0.29, P = .002).
Table 5.
Association with TRV as measured by Pearson rank correlation coefficient (n = 40)
| Variable | r | P |
|---|---|---|
| Erythrocyte glutamine | −0.49 | .001 |
| Glutamine:glutamate ratio | −0.46 | .003 |
| Age, y | 0.33 | .04 |
| Plasma arginase concentration | 0.27 | .11 |
| Diastolic blood pressure | 0.17 | .29 |
| Sex | −0.14 | .40 |
| Hydroxurea use | −0.03 | .88 |
| WHO/NYHA class | 0.03 | .87 |
Discussion
PH is a significant risk factor for early mortality in SCD26 and is associated with both an increased hemolytic rate19–21,23,56,57 and oxidative stress.29,35,50,51,58–63 In hemolytic disorders such as SCD, the erythrocyte itself may be a major determinant of the global redox environment. It has been long established that sickle erythrocytes have increased concentrations of the reactive oxygen species compared with normal red blood cells.29,41 In the presence of alterations in the glutathione buffering system, it is likely that the erythrocytes of SCD patients with PH are incapable of handling the increased oxidant burden, and this might predispose to hemolysis.
Since divergence in the erythrocyte redox environment can contribute to both increased oxidative stress and hemolysis, alterations in glutathione and glutamine metabolism create a mechanistic model bridging 2 critical pathways in the pathogenesis of PH19–22,26,62–66 in hemolytic disorders. Cell-free hemoglobin42 and arginase22 are simultaneously released from the erythrocyte during hemolysis. Each of these molecules contribute to dysregulation of the arginine-NO pathway,20,22,67,68 are associated with the pathogenesis of PH and other subphenotypes of SCD,24,25,69 and are linked to increased mortality.20–22,26 Cell-free hemoglobin binds NO within the plasma, thereby reducing its bioavailability,42 while arginase rapidly consumes NO's substrate arginine.22 Plasma hemoglobin and arginase concentration are excellent biomarkers of hemolytic rate.19,21,22 In the current study, we demonstrated that the glutamine:glutamate ratio correlates inversely with plasma arginase and cell-free hemoglobin concentrations, suggesting a link between altered glutamine metabolism and hemolysis. The glutamine:glutamate ratio may therefore represent a novel biomarker of hemolysis and oxidative stress as well as PH. This ratio has been described as a marker of glutamine-glutamate cycling, particularly in the brain and cerebrospinal fluid,70 and represents a potential marker of poor outcome in traumatic brain injury.71 This ratio, however, has not yet been established as a biomarker of oxidative stress in the erythrocyte, as suggested by our data. Of all variables considered in univariate regression analysis, only age, glutamine bioavailability, and glutamine:glutamate ratio were associated with TRV in patients with SCD. Of these, only glutamine bioavailability maintained significance as an independent predictor of PH in a multiple regression model. The association of both erythrocyte glutamine and the glutamine:glutamate ratio with age is an interesting observation, especially considering the role of oxidative stress and GSH depletion in the aging process,6,10,53,72,73 and may represent a key mechanism that links older age to PH in SCD. The paradoxical correlation of the glutamine:glutamate ratio with diastolic and mean arterial pressure will need further elucidation in larger studies, given reports of the association between relatively elevated blood pressures and increased mortality risk in SCD.26,54,55
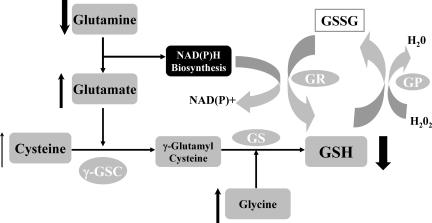
A dysregulation of glutathione metabolism occurs in SCD (Figure 3) and is further amplified in PH. In SCD, a reduction in the total glutathione pool occurs despite sufficient substrate availability in both plasma and within the sickle erythrocyte. Amino acid data from a larger cohort of more than 200 SCD patients confirmed a significant increase in all plasma GSH precursors in SCD patients compared with healthy volunteers, including cysteine,74 the rate-limiting amino acid for GSH synthesis, implicating other mechanisms in erythrocyte GSH depletion. Our findings are consistent with other studies suggesting that lower erythrocyte GSH in SCD patients is not reflective of reduced substrate availability or decreased synthesis, but rather increased GSH consumption.13,75 Glutathione depletion has long been known to occur in the plasma and erythrocytes of SCD patients.14,15,17,18,32,75 By evaluating subgroups of SCD patients with and without PH, we have identified a potential role for altered GSH metabolism and, specifically, glutamine depletion in one of the most devastating complications of SCD.
Figure 3.
Alterations in erythrocyte glutathione (GSH) metabolism in SCD. Normal GSH metabolism: GSH is a potent antioxidant responsible for maintaining cellular redox balance. GSH is synthesized from the amino acids glutamate, cysteine (the rate-limiting substrate), and glycine. Metabolism is catalyzed sequentially by 2 cytosolic enzymes, γ-glutamylcysteine synthetase (γ-GSC) and glutathione synthetase (GS). This pathway occurs in virtually all cells, including erythrocytes, although hepatocytes are the major producer and exporter of GSH. Glutamate and cysteine are catalyzed by γ-GSC to γ-glutamyl-cysteine, which is metabolized to GSH through the actions of GS. GSH is directly oxidized to GSSG during scavenging of free radicals. It is also enzymatically oxidized by glutathione peroxidase (GPx) during the reduction of hydrogen peroxide and other peroxides. GSSG is then reduced and recycled back to GSH by the NADPH-dependent glutathione reductase (GR). During NADH and NADPH biosynthesis, glutamine is converted to glutamate. Although this is a process independent of GSH synthesis, the byproduct of this reaction is used as a substrate for GSH synthesis, while providing the essential co-enzyme for the recycling of GSH from GSSG by NADPH-dependent glutathione reductase.1,9,10 Alterations in GSH metabolism in SCD: Arrows indicate increased substrate and decreased GSH concentrations within the erythrocyte of patients with SCD. Despite more than adequate substrate, including cysteine, the rate-limiting amino acid for GSH production, GSH levels are very low in sickle erythrocytes. Further aberrations in GSH metabolism occur in patients with PH. Most notable is the erythrocyte glutamine depletion that occurs in patients with PH, compared with healthy volunteers and SCD patients without PH, while glutamate levels (significantly higher in SCD patients without PH compared with controls) begin to trend down in SCD patients with PH. Erythrocyte glutamine concentration and the glutamine:glutamate ratio inversely correlate with Doppler echocardiography tricuspid regurgitant jet velocity, a clinical marker of early mortality in SCD.26
One mechanism by which decreased glutamine may influence the redox potential of the sickle erythrocyte is via the loss of NADPH biosynthesis capacity. NADPH is an essential cofactor required for GSH recycling, and low bioavailability would negatively impact on the conversion of GSSG to GSH, resulting in an overall increase in intracellular GSSG and potential efflux.1 The downstream effects of reduced NADPH synthesis include a loss in the overall GSH pool and a shift in the redox potential rendering the erythrocyte more susceptible to hemolysis. Clinical trials have demonstrated that altered erythrocyte NAD redox potential is improved by oral l-glutamine therapy,76,77 suggesting that glutamine limitation is playing a role in oxidative stress. However, it is also possible that systemic effects of glutamine supplementation improve oxidative stress parameters, leading to improved NAD redox potential independent of de novo NAD synthesis.
Dysfunctional NADPH biosynthesis has global pathological implications due to its role as a critical cofactor for a number of enzymes, including the NO synthases (NOS), responsible for the synthesis of NO from L-arginine.78 Given that decreased NO bioavailability is an important mechanism in the pathogenesis of PH,79 of SCD,42,22,80 this is an area to target in future studies. Recent reports suggest that intracellular GSH mediates the trafficking of endogenous NO.11,81 Ironically, both NO and GSH metabolism are disrupted in SCD and likely a mechanism by which oxidative stress, endothelial dysfunction, and hemolysis are enhanced. It is interesting to note that the glutamine:glutamate ratio correlated with markers of hemolysis, while total erythrocyte glutathione levels did not, especially since it has been established in previous studies that a direct correlation between NADPH, but not GSH, concentration and hemoglobin oxidant sensitivity exists.82 Erythrocyte glutamine bioavailability may represent a previously unappreciated link to hemolysis in SCD.
In addition to affecting GSH metabolism indirectly by altering NADPH biosynthesis, glutamine plays a role in the availability of the GSH precursor glutamate. During NADPH biosynthesis, intracellular glutamine is metabolized to glutamate. Glutamate is then available for GSH synthesis and other biological functions. Similar to the findings of Niihara and colleagues, in our study, glutamate levels were elevated in sickle erythrocytes, suggesting increased glutamine turnover.83 In support of this hypothesis is the presence of elevated NADPH levels in sickle erythrocytes.46 Increased NADPH biosynthesis likely occurs in SCD as a compensation for increased oxidative stress to maintain redox balance. These potential compensatory mechanisms may fail in patients with PH. We speculate that in patients with an elevated TRV, the ability to maintain normal erythrocyte glutamine stores are compromised, leading to decreased NADPH biosynthesis capacity and subsequent declines in glutamate levels. The distinction of SCD patients with and without PH was not made in prior studies evaluating erythrocyte GSH precursors, so the present work is the first to link these abnormalities to a specific disease subphenotype. Active transport of glutamate into the sickle erythrocyte is significantly increased in SCD for unclear reasons, and while glutamine transport Km is decreased, V(max) is increased compared with normal red blood cells.83 Although it remains to be determined whether these amino acid alterations are compensatory or pathological, our data suggest that higher erythrocyte glutamate and glutamine levels are protective against development of PH. Our findings clearly need to be confirmed in a larger population, however, the glutamine:glutamate ratio is a novel gauge of cellular oxidative stress that could represent a powerful biomarker of PH in SCD. Although causality between glutamine depletion and PH cannot be assumed, the correlation with TRV is as robust as other previously reported PH biomarkers in SCD, including N-terminal probrain natriuretic peptide (r = 0.50, P < .001),84 soluble vascular cell adhesion molecule-1 (VCAM-1, r = 0.22, P < .001),65 and the arginine/ornithine + citrulline ratio (ρ = −0.34, P < .001),22 biomarkers that along with PH itself, independently identify increased mortality risk in the SCD population.22,26,65,84 The value of erythrocyte amino acid analysis in SCD should be validated in future investigations, as it is more reflective of the total amino acid pools than plasma alone. In addition, selective derangement of red blood cell amino acid pools has systemic consequences that are poorly understood.
These data suggest a potential therapeutic role for glutamine supplementation in PH of SCD. Previous work has demonstrated that glutamine enhances NAD redox potential76,77,85 in SCD, although a specific role in PH has not yet been investigated. Arginine supplementation reduced pulmonary pressures in patients with PH and SCD.68,80 Additionally, arginine increased erythrocyte total glutathione levels in both humans86 and sickle cell transgenic mice.87 Numerous studies have demonstrated a potential role for antioxidants in the treatment of SCD,88–92 several of which have successfully targeted the glutathione pathway.93–95 Nutritional intervention might represent a safe therapeutic approach for SCD, and a combined antioxidant and supplement cocktail could offer augmented benefits over individual ingredients.90
In conclusion, decreased glutathione and glutamine levels occur in SCD and may contribute to alterations in the erythrocyte redox environment, leading to compromised erythrocyte integrity. It is through these mechanisms that glutathione and glutamine potentially contribute to the pathogenesis of PH of SCD. By gaining further insight into the pathogenic mechanisms responsible for the pulmonary vasculopathy observed in SCD, we hope to not only establish biomarkers for disease activity but also potentially alter treatment strategies, with the overall goal of impacting morbidity and mortality for these patients.
Supplementary Material
Acknowledgments
This work was supported in part by National Institutes of Health (NIH) grant HL-04386-05, grant UL1 RR024131-01 from the National Center for Research Resources (NCRR; a component of NIH) and NIH Roadmap for Medical Research (C.R.M.), HL R01 68970 and 1U54 HL 0708819 (M.H.S.), K 23 HL079003-01 (E.S.K.), the American Society of Hematology Minority Medical Student Award (D.A.B.), NIH 1U54 HL070583 (F.A.K.), and the Bruce and Giovanna Ames Foundation (J.H.S.).
Footnotes
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: M.S. performed research. B.A. performed research. F.K. helped design research plan, analyzed patient samples, analyzed data, and helped write the manuscript. E.K. designed and performed research, analyzed data, and helped write the manuscript. C.M. designed and performed research, analyzed data, and wrote the manuscript. J.S. performed research, analyzed samples, assisted with data analysis, and assisted in writing the manuscript. W.H. assisted with data re-analysis, performed statistical analysis on dataset including regression modeling and ROC generation, critically reviewed manuscript revision, and assisted in writing final revision. S.L. performed research and assisted with data analysis. D.A.B. assisted with sample collection and performed research. M.S. assisted with writing of the manuscript. E.V. analyzed data and assisted in writing of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Claudia R. Morris, Department of Emergency Medicine, Children's Hospital and Research Center Oakland, 747 52nd St, Oakland, CA 94609; e-mail: claudiamorris@comcast.net.
References
- 1.Griffith OW. Biologic and pharmacologic regulation of mammalian glutathione synthesis. Free Radic Biol Med. 1999;27:922–935. doi: 10.1016/s0891-5849(99)00176-8. [DOI] [PubMed] [Google Scholar]
- 2.Griffith OW. Glutathione turnover in human erythrocytes: inhibition by buthionine sulfoximine and incorporation of glycine by exchange. J Biol Chem. 1981;256:4900–4904. [PubMed] [Google Scholar]
- 3.Lunn G, Dale GL, Beutler E. Transport accounts for glutathione turnover in human erythrocytes. Blood. 1979;54:238–244. [PubMed] [Google Scholar]
- 4.Lyons J, Rauh-Pfeiffer A, Yu YM, et al. Blood glutathione synthesis rates in healthy adults receiving a sulfur amino acid-free diet. Proc Natl Acad Sci U S A. 2000;97:5071–5076. doi: 10.1073/pnas.090083297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reid M, Badaloo A, Forrester T, et al. In vivo rates of erythrocyte glutathione synthesis in children with severe protein-energy malnutrition. Am J Physiol Endocrinol Metab. 2000;278:E405–E412. doi: 10.1152/ajpendo.2000.278.3.E405. [DOI] [PubMed] [Google Scholar]
- 6.Reid M, Jahoor F. Glutathione in disease. Curr Opin Clin Nutr Metab Care. 2001;4:65–71. doi: 10.1097/00075197-200101000-00012. [DOI] [PubMed] [Google Scholar]
- 7.Jones DP. Redox potential of GSH/GSSG couple: assay and biological significance. Methods Enzymol. 2002;348:93–112. doi: 10.1016/s0076-6879(02)48630-2. [DOI] [PubMed] [Google Scholar]
- 8.Townsend DM, Tew KD, Tapiero H. The importance of glutathione in human disease. Biomed Pharmacother. 2003;57:145–155. doi: 10.1016/s0753-3322(03)00043-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Griffith OW, Bridges RJ, Meister A. Formation of gamma-glutamycyst(e) ine in vivo is catalyzed by gamma-glutamyl transpeptidase. Proc Natl Acad Sci U S A. 1981;78:2777–2781. doi: 10.1073/pnas.78.5.2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu G, Fang YZ, Yang S, Lupton JR, Turner ND. Glutathione metabolism and its implications for health. J Nutr. 2004;134:489–492. doi: 10.1093/jn/134.3.489. [DOI] [PubMed] [Google Scholar]
- 11.Fang YZ, Yang S, Wu G. Free radicals, antioxidants, and nutrition. Nutrition. 2002;18:872–879. doi: 10.1016/s0899-9007(02)00916-4. [DOI] [PubMed] [Google Scholar]
- 12.Newsholme P, Lima MM, Procopio J, et al. Glutamine and glutamate as vital metabolites. Braz J Med Biol Res. 2003;36:153–163. doi: 10.1590/s0100-879x2003000200002. [DOI] [PubMed] [Google Scholar]
- 13.Reid ME, Badaloo A, Forrester T, Jahoor F. In vivo rates of erythrocyte glutathione synthesis in adults with Sickle Cell Disease. Am J Physiol Endocrinol Metab. 2006;291:E73–E79. doi: 10.1152/ajpendo.00287.2005. [DOI] [PubMed] [Google Scholar]
- 14.Fujii S, Kaneko T. Selenium, glutathione peroxidase and oxidative hemolysis in sickle cell disease. Acta Haematol. 1992;87:105–106. doi: 10.1159/000204730. [DOI] [PubMed] [Google Scholar]
- 15.Saad S, Salles SI, Velho PE. Decreased reduced glutathione and glutathione reductase activity in subjects with hemoglobin C. Nouv Rev Fr Hematol. 1991;33:11–14. [PubMed] [Google Scholar]
- 16.Adelekan DA, Thurnham DI, Adekile AD. Reduced antioxidant capacity in paediatric patients with homozygous sickle cell disease. Eur J Clin Nutr. 1989;43:609–614. [PubMed] [Google Scholar]
- 17.Varma RN, Mankad VN, Phelps DD, Jenkins LD, Suskind RM. Depressed erythrocyte glutathione reductase activity in sickle cell disease. Am J Clin Nutr. 1983;38:884–887. doi: 10.1093/ajcn/38.6.884. [DOI] [PubMed] [Google Scholar]
- 18.Wetterstroem N, Brewer GJ, Warth JA, Mitchinson A, Near K. Relationship of glutathione levels and Heinz body formation to irreversibly sickled cells in sickle cell anemia. J Lab Clin Med. 1984;103:589–596. [PubMed] [Google Scholar]
- 19.Rother RP, Bell L, Hillmen P, Gladwin MT. The clinical sequelae of intravascular hemolysis and extracellular plasma hemoglobin: a novel mechanism of human disease. JAMA. 2005;293:1653–1662. doi: 10.1001/jama.293.13.1653. [DOI] [PubMed] [Google Scholar]
- 20.Kato GJ, Gladwin MT, Steinberg MH. Deconstructing sickle cell disease: reappraisal of the role of hemolysis in the development of clinical subphenotypes. Blood Rev. 2007;21:37–47. doi: 10.1016/j.blre.2006.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kato GJ, McGowan V, Machado RF, et al. Lactate dehydrogenase as a biomarker of hemolysis-associated nitric oxide resistance, priapism, leg ulceration, pulmonary hypertension, and death in patients with sickle cell disease. Blood. 2006;107:2279–2285. doi: 10.1182/blood-2005-06-2373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morris CR, Kato GJ, Poljakovic M, et al. Dysregulated arginine metabolism, hemolysis-associated pulmonary hypertension and mortality in sickle cell disease. JAMA. 2005;294:81–90. doi: 10.1001/jama.294.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hsu LL, Champion HC, Campbell-Lee SA, et al. Hemolysis in sickle cell mice causes pulmonary hypertension due to global impairment in nitric oxide bioavailability. Blood. 2007;109:3088–3098. doi: 10.1182/blood-2006-08-039438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nolan VG, Wyszynski DF, Farrer LA, Steinberg MH. Hemolysis-associated priapism in sickle cell disease. Blood. 2005;106:3264–3267. doi: 10.1182/blood-2005-04-1594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ballas SK, Marcolina MJ. Hyperhemolysis during the evolution of uncomplicated acute painful episodes in patients with sickle cell anemia. Transfusion. 2006;46:105–110. doi: 10.1111/j.1537-2995.2006.00679.x. [DOI] [PubMed] [Google Scholar]
- 26.Gladwin M, Sachdev V, Jison M, et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N Engl J Med. 2004;350:22–31. doi: 10.1056/NEJMoa035477. [DOI] [PubMed] [Google Scholar]
- 27.Chiu D, Lubin B. Abnormal vitamin E and glutathione peroxidase levels in sickle cell anemia: evidence for increased susceptibility to lipid peroxidation in vivo. J Lab Clin Med. 1979;94:542–548. [PubMed] [Google Scholar]
- 28.Das SK, Nair RC. Superoxide dismutase, glutathione peroxidase, catalase and lipid peroxidation of normal and sickled erythrocytes. Br J Haematol. 1980;44:87–92. doi: 10.1111/j.1365-2141.1980.tb01186.x. [DOI] [PubMed] [Google Scholar]
- 29.Hebbel RP, Eaton JW, Balasingam M, Steinberg MH. Spontaneous oxygen radical generation by sickle erythrocytes. J Clin Invest. 1982;70:1253–1259. doi: 10.1172/JCI110724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rank BH, Carlsson J, Hebbel RP. Abnormal redox status of membrane-protein thiols in sickle erythrocytes. J Clin Invest. 1985;75:1531–1537. doi: 10.1172/JCI111857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rice-Evans C, Omorphos SC, Baysal E. Sickle cell membranes and oxidative damage. Biochem J. 1986;237:265–269. doi: 10.1042/bj2370265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lachant NA, Davidson WD, Tanaka KR. Impaired pentose phosphate shunt function in sickle cell disease: a potential mechanism for increased Heinz body formation and membrane lipid peroxidation. Am J Hematol. 1983;15:1–13. doi: 10.1002/ajh.2830150102. [DOI] [PubMed] [Google Scholar]
- 33.Banerjee T, Kuypers FA. Reactive oxygen species and phosphatidylserine externalization in murine sickle red cells. Br J Haematol. 2004;124:391–402. doi: 10.1046/j.1365-2141.2003.04781.x. [DOI] [PubMed] [Google Scholar]
- 34.Hebbel RP, Morgan WT, Eaton JW, Hedlund BE. Accelerated autoxidation and heme loss due to instability of sickle hemoglobin. Proc Natl Acad Sci U S A. 1988;85:237–241. doi: 10.1073/pnas.85.1.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Schacter L, Warth JA, Gordon EM, Prasad A, Klein BL. Altered amount and activity of superoxide dismutase in sickle cell disease. FASEB J. 1988;2:237–243. doi: 10.1096/fasebj.2.3.3350236. [DOI] [PubMed] [Google Scholar]
- 36.Dias-Da-Motta P, Arruda V, Muscara M, Saad S. The release of nitric oxide and superoxide anion by neutrophils and mononuclear cells from patients with sickle cell anaemia. Brit J Haematol. 1996;93:333–340. doi: 10.1046/j.1365-2141.1996.4951036.x. [DOI] [PubMed] [Google Scholar]
- 37.Repka T, Hebbel RP. Hydroxyl radical formation by sickle erythrocyte membranes: role of pathologic iron deposits and cytoplasmic reducing agents. Blood. 1991;78:2753–2758. [PubMed] [Google Scholar]
- 38.Wood KC, Hebbel RP, Lefer DJ, Granger DN. Critical role of endothelial cell-derived nitric oxide synthase in sickle cell disease-induced microvascular dysfunction. Free Radic Biol Med. 2006;40:1443–1453. doi: 10.1016/j.freeradbiomed.2005.12.015. [DOI] [PubMed] [Google Scholar]
- 39.Morris CR, Kuypers FA, Larkin S, Vichinsky E, Styles L. Patterns of arginine and nitric oxide in sickle cell disease patients with vaso-occlusive crisis and acute chest syndrome. J Pediatr Hematol Oncol. 2000;22:515–520. doi: 10.1097/00043426-200011000-00009. [DOI] [PubMed] [Google Scholar]
- 40.Gladwin M, Schechter A, Ognibene F, et al. Divergent nitric oxide bioavailability in men and women with sickle cell disease. Circulation. 2003;107:271–278. doi: 10.1161/01.cir.0000044943.12533.a8. [DOI] [PubMed] [Google Scholar]
- 41.Aslan M, Freeman BA. Oxidant-mediated impairment of nitric oxide signaling in sickle cell disease—mechanisms and consequences. Cell Mol Biol (Noisy-le-grand) 2004;50:95–105. [PubMed] [Google Scholar]
- 42.Reiter C, Wang X, Tanus-Santos J, et al. Cell-free hemoglobin limits nitric oxide bioavailability in sickle cell disease. Nat Med. 2002;8:1383–1389. doi: 10.1038/nm1202-799. [DOI] [PubMed] [Google Scholar]
- 43.Hammerman SI, Klings ES, Hendra KP, et al. Endothelial cell nitric oxide production in acute chest syndrome. Am J Physiol. 1999;277:H1579–H1592. doi: 10.1152/ajpheart.1999.277.4.H1579. [DOI] [PubMed] [Google Scholar]
- 44.Nath KA, Shah V, Haggard JJ, et al. Mechanisms of vascular instability in a transgenic mouse model of sickle cell disease. Am J Physiol Regul Integr Comp Physiol. 2000;279:R1949–R1955. doi: 10.1152/ajpregu.2000.279.6.R1949. [DOI] [PubMed] [Google Scholar]
- 45.Eberhardt RT, McMahon L, Duffy SJ, et al. Sickle cell anemia is associated with reduced nitric oxide bioactivity in peripheral conduit and resistance vessels. Am J Hematol. 2003;74:104–111. doi: 10.1002/ajh.10387. [DOI] [PubMed] [Google Scholar]
- 46.Zerez CR, Lachant NA, Lee SJ, Tanaka KR. Decreased erythrocyte nicotinamide adenine dinucleotide redox potential and abnormal pyridine nucleotide content in sickle cell disease. Blood. 1988;71:512–515. [PubMed] [Google Scholar]
- 47.Lachant NA, Zerez CR, Tanaka KR. Relationship between the nicotinamide adenine dinucleotide redox potential and the 2,3-diphosphoglycerate content in the erythrocyte in sickle cell disease. Br J Haematol. 1989;72:265–271. doi: 10.1111/j.1365-2141.1989.tb07693.x. [DOI] [PubMed] [Google Scholar]
- 48.Li SD, Su YD, Li M, Zou CG. Hemin-mediated hemolysis in erythrocytes: effects of ascorbic acid and glutathione. Acta Biochim Biophys Sin. 2006;38:63–69. doi: 10.1111/j.1745-7270.2006.00127.x. [DOI] [PubMed] [Google Scholar]
- 49.Koyama J, Ray-Sequin PA, Falk RH. Prognostic significance of ultrasound myocardial tissue characterization in patients with cardiac amyloidosis. Circulation. 2002;106:556–561. doi: 10.1161/01.cir.0000023530.86718.b0. [DOI] [PubMed] [Google Scholar]
- 50.Klings E, Christman B, McClung J, et al. Increased F2 isoprostanes in the acute chest syndrome of sickle cell disease as a marker of oxidative stress. Am J Respir Crit Care Med. 2001;164:1248–1252. doi: 10.1164/ajrccm.164.7.2101020. [DOI] [PubMed] [Google Scholar]
- 51.Klings ES, Safaya S, Adewoye AH, et al. Differential gene expression in pulmonary artery endothelial cells exposed to sickle cell plasma. Physiol Genomics. 2005;21:293–298. doi: 10.1152/physiolgenomics.00246.2004. [DOI] [PubMed] [Google Scholar]
- 52.Husek P, Matucha P, Vrankova A, Simek P. Simple plasma work-up for a fast chromatographic analysis of homocysteine, cysteine, methionine and aromatic amino acids. J Chromatogr B Analyt Technol Biomed Life Sci. 2003;789:311–322. doi: 10.1016/s1570-0232(03)00104-1. [DOI] [PubMed] [Google Scholar]
- 53.Dalle-Donne I, Rossi R, Colombo R, Giustarini D, Milzani A. Biomarkers of oxidative damage in human disease. Clin Chem. 2006;52:601–623. doi: 10.1373/clinchem.2005.061408. [DOI] [PubMed] [Google Scholar]
- 54.Sachdev V, Machado RF, Shizukuda Y, et al. Diastolic dysfunction is an independent risk factor for death in patients with sickle cell disease. J Am Coll Cardiol. 2007;49:472–479. doi: 10.1016/j.jacc.2006.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pegelow CH, Colangelo L, Steinberg M, et al. Natural history of blood pressure in sickle cell disease: risks for stroke and death associated with relative hypertension in sickle cell anemia. Am J Med. 1997;102:171–177. doi: 10.1016/s0002-9343(96)00407-x. [DOI] [PubMed] [Google Scholar]
- 56.Ataga KI, Moore CG, Jones S, et al. Pulmonary hypertension in patients with sickle cell disease: a longitudinal study. Br J Haematol. 2006;134:109–115. doi: 10.1111/j.1365-2141.2006.06110.x. [DOI] [PubMed] [Google Scholar]
- 57.Mann JR, Cotter KP, Walker RA, Bird GW, Stuart J. Anaemic crisis in sickle cell disease. J Clin Pathol. 1975;28:341–344. doi: 10.1136/jcp.28.5.341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Osarogiagbon UR, Choong S, Belcher JD, Vercellotti GM, Paller MS, Hebbel RP. Reperfusion injury pathophysiology in sickle transgenic mice. Blood. 2000;96:314–320. [PubMed] [Google Scholar]
- 59.Belcher JD, Marker PH, Weber JP, Hebbel RP, Vercellotti GM. Activated monocytes in sickle cell disease: potential role in the activation of vascular endothelium and vaso-occlusion. Blood. 2000;96:2451–2459. [PubMed] [Google Scholar]
- 60.Belcher JD, Mahaseth H, Welch TE, et al. Critical role of endothelial cell activation in hypoxia-induced vasoocclusion in transgenic sickle mice. Am J Physiol Heart Circ Physiol. 2005;288:H2715–H2725. doi: 10.1152/ajpheart.00986.2004. [DOI] [PubMed] [Google Scholar]
- 61.Nath KA, Grande JP, Haggard JJ, et al. Oxidative stress and induction of heme oxygenase-1 in the kidney in sickle cell disease. Am J Pathol. 2001;158:893–903. doi: 10.1016/S0002-9440(10)64037-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Black SM, Fineman JR. Oxidative and nitrosative stress in pediatric pulmonary hypertension: roles of endothelin-1 and nitric oxide. Vascul Pharmacol. 2006;45:308–316. doi: 10.1016/j.vph.2006.08.005. [DOI] [PubMed] [Google Scholar]
- 63.Bowers R, Cool C, Murphy RC, et al. Oxidative stress in severe pulmonary hypertension. Am J Respir Crit Care Med. 2004;169:764–769. doi: 10.1164/rccm.200301-147OC. [DOI] [PubMed] [Google Scholar]
- 64.Grobe AC, Wells SM, Benavidez E, et al. Increased oxidative stress in lambs with increased pulmonary blood flow and pulmonary hypertension: role of NADPH oxidase and endothelial NO synthase. Am J Physiol Lung Cell Mol Physiol. 2006;290:L1069–L1077. doi: 10.1152/ajplung.00408.2005. [DOI] [PubMed] [Google Scholar]
- 65.Kato GJ, Martyr S, Blackwelder WC, et al. Levels of soluble endothelium-derived adhesion molecules in patients with sickle cell disease are associated with pulmonary hypertension, organ dysfunction, and mortality. Br J Haematol. 2005;130:943–953. doi: 10.1111/j.1365-2141.2005.05701.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Morris C, Kuypers F, Kato G, et al. Hemolysis-associated pulmonary hypertension in thalassemia. An NY Acad Sci. 2005;1054:481–485. doi: 10.1196/annals.1345.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Morris CR. Hemolysis-associated pulmonary hypertension in sickle cell disease: global disruption of the arginine-nitric oxide pathway. Curr Hypertens Rev. 2007;3:223–230. [Google Scholar]
- 68.Morris CR. New strategies for the treatment of pulmonary hypertension in sickle cell disease: the rationale for arginine therapy. Treat Respir Med. 2006;5:31–45. doi: 10.2165/00151829-200605010-00003. [DOI] [PubMed] [Google Scholar]
- 69.Nolan VG, Adewoye A, Baldwin C, et al. Sickle cell leg ulcers: associations with haemolysis and SNPs in Klotho, TEK and genes of the TGF-beta/BMP pathway. Br J Haematol. 2006;133:570–578. doi: 10.1111/j.1365-2141.2006.06074.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Hashimoto K, Engberg G, Shimizu E, Nordin C, Lindstrom LH, Iyo M. Elevated glutamine/glutamate ratio in cerebrospinal fluid of first episode and drug naive schizophrenic patients. BMC Psychiatry. 2005;5:6. doi: 10.1186/1471-244X-5-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Richards DA, Tolias CM, Sgouros S, Bowery NG. Extracellular glutamine to glutamate ratio may predict outcome in the injured brain: a clinical microdialysis study in children. Pharmacol Res. 2003;48:101–109. [PubMed] [Google Scholar]
- 72.Knight JA. The biochemistry of aging. Adv Clin Chem. 2000;35:1–62. doi: 10.1016/s0065-2423(01)35014-x. [DOI] [PubMed] [Google Scholar]
- 73.Sohal RS. Role of oxidative stress and protein oxidation in the aging process. Free Radic Biol Med. 2002;33:37–44. doi: 10.1016/s0891-5849(02)00856-0. [DOI] [PubMed] [Google Scholar]
- 74.Morris CR, Kato G, Poljakovic M, et al. The arginine-to-ornithine ratio: biomarker of arginase activity and predictor of mortality in sickle cell disease [abstract]. Blood. 2004;104:71a–72a. Abstract 233. [Google Scholar]
- 75.Kiessling K, Roberts N, Gibson JS, Ellory JC. A comparison in normal individuals and sickle cell patients of reduced glutathione precursors and their transport between plasma and red cells. Hematol J. 2000;1:243–249. doi: 10.1038/sj.thj.6200033. [DOI] [PubMed] [Google Scholar]
- 76.Niihara Y, Matsui NM, Shen YM, et al. L-glutamine therapy reduces endothelial adhesion of sickle red blood cells to human umbilical vein endothelial cells. BMC Blood Disord. 2005;5:4. doi: 10.1186/1471-2326-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Niihara Y, Zerez CR, Akiyama DS, Tanaka KR. Oral L-glutamine therapy for sickle cell anemia, I; subjective clinical improvement and favorable change in red cell NAD redox potential. Am J Hematol. 1998;58:117–121. doi: 10.1002/(sici)1096-8652(199806)58:2<117::aid-ajh5>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 78.Moncada S, Higgs A. The L-arginine-nitric oxide pathway. N Engl J Med. 1993;329:2002–2012. doi: 10.1056/NEJM199312303292706. [DOI] [PubMed] [Google Scholar]
- 79.Michelakis ED. The role of the NO axis and its therapeutic implications in pulmonary arterial hypertension. Heart Fail Rev. 2003;8:5–21. doi: 10.1023/a:1022150819223. [DOI] [PubMed] [Google Scholar]
- 80.Morris CR, Morris SM, Jr, Hagar W, et al. Arginine therapy: a new treatment for pulmonary hypertension in sickle cell disease? Am J Respir Crit Care Med. 2003;168:63–69. doi: 10.1164/rccm.200208-967OC. [DOI] [PubMed] [Google Scholar]
- 81.Andre M, Felley-Bosco E. Heme oxygenase-1 induction by endogenous nitric oxide: influence of intracellular glutathione. FEBS Lett. 2003;546:223–227. doi: 10.1016/s0014-5793(03)00576-3. [DOI] [PubMed] [Google Scholar]
- 82.Scott MD, Zuo L, Lubin BH, Chiu DT. NADPH, not glutathione, status modulates oxidant sensitivity in normal and glucose-6-phosphate dehydrogenase-deficient erythrocytes. Blood. 1991;77:2059–2064. [PubMed] [Google Scholar]
- 83.Niihara Y, Zerez CR, Akiyama DS, Tanaka KR. Increased red cell glutamine availability in sickle cell anemia: demonstration of increased active transport, affinity, and increased glutamate level in intact red cells. J Lab Clin Med. 1997;130:83–90. doi: 10.1016/s0022-2143(97)90062-7. [DOI] [PubMed] [Google Scholar]
- 84.Machado RF, Anthi A, Steinberg MH, et al. N-terminal pro-brain natriuretic peptide levels and risk of death in sickle cell disease. JAMA. 2006;296:310–318. doi: 10.1001/jama.296.3.310. [DOI] [PubMed] [Google Scholar]
- 85.Schaison G. Sickle cell anemia, an example of a constitutional disease of hemoglobin. Rev Stomatol Chir Maxillofac. 1983;84:144–148. [PubMed] [Google Scholar]
- 86.Morris CR, Suh JH, Vichinsky E, et al. Oral arginine increases erythrocyte glutathione levels in sickle cell disease: implications for pulmonary hypertension [abstract]. Blood. 2006:356a. Abstract 1208. [Google Scholar]
- 87.Dasgupta T, Hebbel RP, Kaul DK. Protective effect of arginine on oxidative stress in transgenic sickle mouse models. Free Radic Biol Med. 2006;41:1771–1780. doi: 10.1016/j.freeradbiomed.2006.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Ajayi OA, George BO, Ipadeola T. Clinical trial of riboflavin in sickle cell disease. East Afr Med J. 1993;70:418–421. [PubMed] [Google Scholar]
- 89.Muskiet FA, Muskiet FD, Meiborg G, Schermer JG. Supplementation of patients with homozygous sickle cell disease with zinc, alpha-tocopherol, vitamin C, soybean oil, and fish oil. Am J Clin Nutr. 1991;54:736–744. doi: 10.1093/ajcn/54.4.736. [DOI] [PubMed] [Google Scholar]
- 90.Ohnishi ST, Ohnishi T, Ogunmola GB. Sickle cell anemia: a potential nutritional approach for a molecular disease. Nutrition. 2000;16:330–338. doi: 10.1016/s0899-9007(00)00257-4. [DOI] [PubMed] [Google Scholar]
- 91.van der Dijs FP, Fokkema MR, Dijck-Brouwer DA, et al. Optimization of folic acid, vitamin B(12), and vitamin B(6) supplements in pediatric patients with sickle cell disease. Am J Hematol. 2002;69:239–246. doi: 10.1002/ajh.10083. [DOI] [PubMed] [Google Scholar]
- 92.Heyman MB, Vichinsky E, Katz R, et al. Growth retardation in sickle-cell disease treated by nutritional support. Lancet. 1985;1:903–906. doi: 10.1016/s0140-6736(85)91677-0. [DOI] [PubMed] [Google Scholar]
- 93.Udupi V, Rice-Evans C. Thiol compounds as protective agents in erythrocytes under oxidative stress. Free Radic Res Commun. 1992;16:315–323. doi: 10.3109/10715769209049184. [DOI] [PubMed] [Google Scholar]
- 94.Dumaswala UJ, Zhuo L, Mahajan S, et al. Glutathione protects chemokine-scavenging and antioxidative defense functions in human RBCs. Am J Physiol Cell Physiol. 2001;280:C867–C873. doi: 10.1152/ajpcell.2001.280.4.C867. [DOI] [PubMed] [Google Scholar]
- 95.Pace BS, Shartava A, Pack-Mabien A, Mulekar M, Ardia A, Goodman SR. Effects of N-acetylcysteine on dense cell formation in sickle cell disease. Am J Hematol. 2003;73:26–32. doi: 10.1002/ajh.10321. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.