Summary points
Lower urinary tract symptoms are bothersome yet often under-reported by older men
Symptom severity generally progresses over time but is rarely life threatening
Many clinical and lifestyle factors can cause or worsen the symptoms but can be modified by simple interventions
Asking about how bothersome the symptoms are and how they affect the patient’s quality of life is useful for considering whether to suggest additional treatment
Benign prostatic hyperplasia does not increase risk of prostate cancer but is associated with higher levels of prostate specific antigen
These levels are associated with prostate volume and may be useful when combined with symptom and health status measures for assessing potential effectiveness of treatment options
Most men can be assessed and treated by primary care clinicians on the basis of the severity of their symptoms and how bothersome they are
Additional diagnostic evaluations include diaries, uroflowmetry, bladder pressure studies, urinary tract imaging, and urethrocystoscopy
Lower urinary tract symptoms in older men are common and bothersome, leading to considerable use of healthcare services.1 2 Symptoms may reflect obstructive voiding (weak urine flow, hesitancy, straining, and incomplete emptying) or bladder storage problems (frequency, urgency, and nocturia). Lower urinary tract symptoms are often considered to be due to benign prostatic hyperplasia (BPH) or benign prostatic enlargement. However, such symptoms are common in women, as well as in men with prostate glands that are not enlarged.3 4 The symptoms can be caused by overactivity of the bladder’s detrusor muscle, non-urological conditions, medications, or lifestyle factors. This article provides evidence to guide primary care doctors in the diagnosis of men with lower urinary tract symptoms, with an emphasis on BPH. A second article, to be published soon, will focus on management.
What causes lower urinary tract symptoms due to BPH?
The pathophysiology of benign prostatic enlargement involves hyperplasia of the epithelial and stromal components of the prostate gland, which leads to progressive obstruction of urine flow and increased activity of the detrusor muscle.5 These secondary urodynamic changes are thought to result in the typical symptoms of bladder storage such as frequency and nocturia and voiding symptoms such as poor flow and intermittent stream. For simplicity, these complaints are grouped together as lower urinary tract symptoms. Although the precise relation between symptoms, prostate enlargement, and obstruction is not certain, removal of prostatic tissue in affected men improves symptoms, urodynamic function, and quality of life.
What is the prevalence and natural course of lower urinary tract symptoms?
BPH is the most common benign neoplasia in men. Lower urinary tract symptoms due to BPH are regarded as a chronic condition that increases in frequency and severity with age. In men 50 years or older in England, Scotland, and Wales, 41% described symptoms classed as moderate to severe, but only 18% reported that they had received a clinical diagnosis of BPH. Quality of life and general health status decreased as severity of symptoms increased; however, only about 1 in 10 respondents was aware of the availability of prescription drugs or surgical options for BPH.6 Storage and voiding symptoms were self reported by 51% and 26% respectively of men aged 39 and older from five European countries, with the prevalence of reporting increasing with age (table ).3 Results from other national surveys suggest that despite being common and bothersome, lower urinary tract symptoms often go undiagnosed or untreated.7 8 Mild symptoms do not greatly affect quality of life, but the impact of severe symptoms is similar to chronic conditions such as hypertension, diabetes, angina, and gout.9
Percentage of men with lower urinary tract symptoms*
| Urinary symptoms | Age (years) | All ages | ||
|---|---|---|---|---|
| ≤39 | 40-59 | ≥60 | ||
| Storage | ||||
| Any storage symptom | 38 | 51 | 74 | 51 |
| Nocturia at least once a night | 34 | 48 | 72 | 49 |
| Urgency | 7 | 9 | 19 | 11 |
| Frequency | 5 | 6 | 11 | 7 |
| Any urinary incontinence | 2 | 5 | 10 | 5 |
| Voiding | ||||
| Any voiding symptom | 20 | 24 | 37 | 26 |
| Intermittency | 6 | 8 | 14 | 8 |
| Slow stream | 4 | 7 | 19 | 9 |
| Strain | 4 | 7 | 10 | 7 |
| Terminal dribbling | 12 | 13 | 19 | 14 |
*Adapted from Irwin et al.3
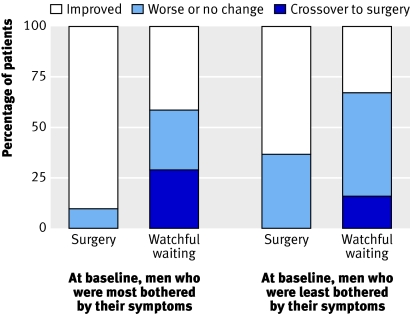
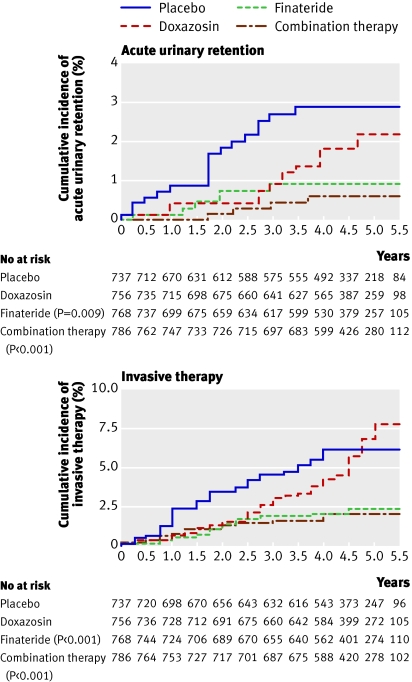
Few risk factors exist for BPH, other than age and possibly obesity.10 Slow progression of symptoms and bothersome effects of these symptoms are common features of BPH. About 14% of men with moderate to severe symptoms had clinically noticeable worsening of their symptoms during five years of follow-up.11 More serious complications—such as acute urinary retention (1-3% over five years), renal insufficiency, or the need for surgical intervention—are uncommon.12,13,14 In a randomised comparison with transurethral resection of the prostate, a quarter of men with moderate symptoms assigned to receive advice alone had prostate surgery for progressive symptoms or other signs of BPH progression during a three year follow-up15 (fig 1). However, in a more recent study of men with benign prostatic enlargement and moderate to severe baseline symptoms, only 6% of men receiving placebo had acute urinary retention or needed BPH surgery after five years11 (fig 2). Therefore, the vast majority of men even with moderate to severe symptoms do not need surgery for many years.
Fig 1 Severity of symptoms after three years of follow-up in men with benign prostatic hyperplasia treated with transurethral resection of the prostate or watchful waiting, relative to how bothersome their symptoms were at baseline. Adapted from Wasson et al
Fig 2 Cumulative incidence of acute urinary retention and invasive therapy for BPH. Adapted from McConnell et al
What diagnostic tests should be used routinely in men with lower urinary tract symptoms?
History, physical examination, and laboratory and urodynamic tests are used to identify the presence, severity, and aetiology of lower urinary tract symptoms and to guide treatment, including the need for referral to urologists. History can determine if the symptoms are caused by other medical conditions (poorly controlled diabetes, neurological disorders, urinary tract infections, chronic abacterial prostatitis, overactive bladder), medications, (diuretics, anticholinergics, antidepressants),16 or lifestyle factors (caffeine, alcohol, excess intake of liquids).
A validated questionnaire—usually the international prostate symptoms scale17—is a simple and reliable method to assess the presence, type, and severity of symptoms and the response to treatment (box). Completion of the questionnaire yields a total score ranging from 0 to 35 (1-7 for mild symptoms; 8-19 for moderate; and 20-35 for severe). In the questionnaire, one question (about how men feel about their current urinary symptoms) yields a score for quality of life (0=delighted, 6=terrible). Other health status questions directly ask how bothersome urinary symptoms are. Although symptom severity correlates with scores for quality of life and how bothersome symptoms are, variation may exist. For example, some men with relatively minor symptoms feel terrible or find their symptoms very bothersome, whereas other men with severe symptoms may be bothered by them much.
International prostate symptom scale
Scoring system
Ask the patient seven questions (below) about his urinary symptoms. Answers are on a scale of 0-5, depending on severity of the problem. For the first six questions the choice of answers is: not at all (score 0); less than one time in five (1); less than half the time (2); about half the time (3); more than half the time (4); almost always (5). For the final question, the choices are: never (0); once (1); twice (2); three times (3); four times (4); five or more times (5). Add the scores to give the total score and thus the severity category for symptoms (mild <8; moderate 8-19; severe 20-35). A further question—on quality of life (below)—produces a quality of life score
Questions
1 Over the past month, how often have you had a sensation of not emptying your bladder completely after you finished urinating?
2 Over the past month, how often have you had the urge to urinate again less than two hours after you finished urinating?
3 Over the past month, how often have you found you stopped and started again several times when you urinated?
4 Over the past month, how often have you found it difficult to postpone urination?
5 Over the past month, how often have you had a weak urinary stream? (Please compare with your stream size at age 30)
6 Over the past month, how often have you had to push or strain to begin urination?
7 Over the past month, how many times did you most typically get up to urinate from the time you went to bed at night until the time you got up in the morning?
Question on quality of life in relation to urinary symptoms
If you were to spend the rest of your life with your urinary condition the way it is now, how would you feel about that? Delighted (0), pleased (1), mostly satisfied (2), mixed feelings (3), mostly dissatisfied (4), unhappy (5), terrible (6)
Patient response on the quality of life question is a strong predictor for determining if interventions are indicated.17 The presence of urinary incontinence, retention, haematuria, dysuria, or acute change in symptoms can indicate other conditions or complications of BPH. These patients often need to be referred to a urologist for further evaluation even if they have not reported their symptoms as bothersome. Abdominal examination to detect palpable bladder is indicated if obstruction of the bladder outlet is suspected. Fear that lower urinary tract symptoms may be caused by prostate cancer is a major reason that men consult their doctor.18 However, men can be reassured that those with lower urinary tract symptoms are not at higher risk of having prostate cancer than men without these symptoms.19 20 Therefore, although measurement of prostate specific antigen and digital rectal examination are widely used to try to detect cancer, these approaches are not routinely indicated. Levels of prostate specific antigen are associated with prostate volume; when combined with symptom severity and how bothersome the symptoms are, the antigen levels can be helpful in estimating treatment effectiveness. Widespread measurement of prostate specific antigen is likely to lead to increased falsely abnormal findings and subsequent diagnostic tests (see www.cancerscreening.nhs.uk/prostate/).
Evidence based guidelines indicate that diagnostic studies are not usually required or helpful for primary care management.21 22 Optional evaluations (based on unique patient situations or on a general practitioner’s preferences) include ultrasonography for estimation of residual urine volume; urinary diaries (for recording frequency and volume of voiding) particularly if nocturia is prominent; urine analysis to exclude infection; and measurement of serum creatinine concentration if renal insufficiency or urinary retention is suspected. Primary care physicians may have access to, and skills to interpret, urodynamic testing such as uroflowmetry, although such testing is often done by urologists.
What additional diagnostic tests are used in secondary care?
The reasons for conducting additional diagnostic tests include patient reassurance or explanation, objective assessment of symptoms, diagnostic precision, ranking of treatment options, and prediction of treatment outcome.
Diaries
Completion of a voiding diary by the patient over a few days gives an assessment of storage symptoms such as nocturia, gives information on daily bladder capacity, and can indicate other causes of lower urinary tract symptoms, such as nocturnal polyuria or excessive fluid intake. Diaries can also be used as a basis for educating the patient about self management or for suggesting alternative treatments such as diuretics.23
Uroflowmetry
Objective measurement of variables such as maximum flow rate and volume of residual urine after voiding gives useful information on micturition, and the results can to some extent predict the likelihood of disease progression and response to treatment. For example, a low flow rate suggests obstruction and may be associated with a better outcome after transurethral resection of the prostate, although underactivity of the detrusor muscle can result in the same findings. It is advisable to take serial flow measurements (at least two of voided volumes over 150 ml) to ensure that interpretation is based on a representative void.22
Bladder pressure studies
Pressure measurement (cystometry) during bladder filling and voiding defines several urodynamic abnormalities, including overactivity (or underactivity) of the detrusor muscle and obstruction of the bladder outlet. The results are useful in predicting the response to treatment such as antimuscarinics for overactivity of the detrusor muscle and transurethral resection of the prostate for obstruction of the bladder outlet. They also provide an important baseline for men who fail to benefit from surgery. Despite these advantages the clinical value of cystometry is debated, mainly because of the need for catheterisation; cystometry is generally confined to men with complicating factors such as urge incontinence or severe comorbidity, where accurate prediction of outcome is of greater importance.22 24
Urinary tract imaging
Imaging of the urinary tract, apart from ultrasound estimation of residual urine, is no longer considered routine for men with lower urinary tract symptoms. Ultrasound examination of the kidneys and bladder can be useful for identifying stones in men with urinary tract infections and for seeing tumours if haematuria is detected by urine analysis. Detected abnormalities usually require further imaging by computed tomography or intravenous urography. Estimation of prostate size by abdominal or transrectal ultrasonography may help to predict benefit from combined treatment with α blockers and 5α reductase inhibitors and may also guide surgical management.11 21 22
Urethrocystoscopy
Visual inspection of the urethra and bladder is important in men with dysuria or haematuria as it can show mucosal abnormalities such as bladder tumours. Inspection may also be necessary for differentiating urethral strictures from prostatic causes of obstruction in younger men or those who have had previous transurethral surgery.
Sources and selections criteria
We searched Medline and the Cochrane Library up toNovember 2007 for randomised trials, systematic reviews, evidence reports, and recent evidence based guidelines from the American Urological Association, European Urological Association, and the National Institute for Health and Clinical Excellence.
Additional educational resources
PatientPlus (www.patient.co.uk/showdoc/40002437/)—Comprehensive, free, up to date health information as provided by general practitioners to patients during consultations
Foundation for Informed Medical Decision Making (www.fimdm.org)—Provides information to help patients make sound decisions affecting their health and wellbeing
Health Dialog (www.healthdialog.com)—Provides care management and analytical services
Cochrane Library (www.cochrane.org)—Publishes systematic reviews of the effects of healthcare interventions
Ongoing research
Characterisation of genetic and molecular events linked with symptomatic benign prostatic hyperplasia
The National Collaborating Centre for Acute Care hosted by the Royal College of Surgeons of England has recently been commissioned by the National Institute of Health and Clinical Excellence (NICE) to develop an evidence based clinical guideline on the management of benign prostatic hyperplasia. Their recommendations should be available in 2009
Unanswered questions
Which assessment tools and diagnostic tests give useful prediction of treatment response?
Can the contributions of (a) benign prostatic hyperplasia and (b) dysfunction of the detrusor muscle to lower urinary tract symptoms be differentiated?
Benign prostatic hyperplasia and dysfunction of the detrusor muscle both contribute to lower urinary tract symptoms, but how can the two causes be differentiated?
Contributors: Both authors conceived the idea; contributed intellectual content; acquired and analysed evidence; and wrote, reviewed, and edited the manuscript.
Competing interests: None declared.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1.Wei JT, Calhoun EA, Jacobsen SJ. Benign prostatic hyperplasia. In: Litwin MS, Saigal CS, eds. Urologic diseases in America US Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases. Washington, DC: US Government Publishing Office, 2007. (pp 43-70 ). NIH publication no 07-5512.
- 2.Foley CL, Taylor C, Kirby RS. Counting the cost of treating benign prostatic hyperplasia. BJU Int 2004;93:250-2. [DOI] [PubMed] [Google Scholar]
- 3.Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the epic study. Eur Urol 2006;50:1306-15. [DOI] [PubMed] [Google Scholar]
- 4.Kupelian V, Wei JT, O’Leary MP, Kusek JW, Litman HJ, Link CL, et al. Prevalence of lower urinary tract symptoms and effect on quality of life in a racially and ethnically diverse random sample. The Boston area community health (BACH) survey. Arch Intern Med 2006;166:2381-7. [DOI] [PubMed] [Google Scholar]
- 5.Berry SJ, Coffey DS, Walsh PC, Ewing LL. The development of human benign prostatic hyperplasia with age. J Urol 1984;132:474-9. [DOI] [PubMed] [Google Scholar]
- 6.Trueman P, Hood SC, Nayak USL, Mrazek MF. Prevalence of lower urinary tract symptoms and self-reported diagnosed “benign prostatic hyperplasia” and their effect on quality of life in a community-based survey of men in the UK. BJU Int 1999;83:410-5. [DOI] [PubMed] [Google Scholar]
- 7.Platz EA, Smit E, Curhan GC, Nyberg LM. Giovannucci E. Prevalence of and racial/ethnic variation in lower urinary tract symptoms and noncancer prostate surgery in US men. Urology 2002;59:877-83. [DOI] [PubMed] [Google Scholar]
- 8.Garraway WM, Collins GN, Lee RJ. High prevalence of benign prostatic hypertrophy in the community. Lancet 1991;338:469-71. [DOI] [PubMed] [Google Scholar]
- 9.Welch G, Weinger K, Barry MJ. Quality-of-life impact of lower urinary tract symptom severity: results from the health professionals follow-up study. Urology 2002;59:245-50. [DOI] [PubMed] [Google Scholar]
- 10.Zucchetto A, Tavani A, Dal Maso L, Gallus S, Negri E, Talamini R, et al. History of weight and obesity through life and risk of benign prostatic hyperplasia. Int J Obes (Lond) 2005;29:798-803. [DOI] [PubMed] [Google Scholar]
- 11.McConnell JD, Roehrborn CB, Bautistia OM, Andriole GL Jr, Dixon CM, Kusek JW, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med 2003;349:2387-98. [DOI] [PubMed] [Google Scholar]
- 12.Meigs JB, Barry MJ, Giovannucci E, Rimm EB, Stampfer MJ, Kawachi I. Incidence rates and risk factors for acute urinary retention: the health professionals follow-up study. J Urol 1999;162:376-82. [PubMed] [Google Scholar]
- 13.Jacobsen SJ, Jacobson DJ, Girman CJ, Roberts RO, Rhodes T, Guess HA, et al. Natural history of prostatism: Risk factors for acute urinary retention. J Urol 1997;158:481-7. [DOI] [PubMed] [Google Scholar]
- 14.Fitzpatrick JM. The natural history of benign prostatic hyperplasia. BJU Int 2006;97(suppl 2):3-6. [DOI] [PubMed] [Google Scholar]
- 15.Wasson JH, Reda DJ, Bruskewitz RC, Elinson J, Keller AM, Henderson WG. A comparison of transurethral surgery with watchful waiting for moderate symptoms of benign prostatic hyperplasia. The Veterans Affairs Cooperative Study Group on Transurethral Resection of the Prostate. N Engl J Med 1995;332:75-9. [DOI] [PubMed] [Google Scholar]
- 16.Su L, Guess HA, Girman CJ, Jacobsen SJ, Oesterling JE, Panser LA, et al. Adverse effects of medications on urinary symptoms and flow rate: a community-based study. J Clin Epidemiol 1996;49:483-7. [DOI] [PubMed] [Google Scholar]
- 17.Barry MJ, Fowler FJ Jr, O’Leary MP, Bruskewitz RC, Holtgrewe HL, Mebust WK, et al. The American Urological Association symptom index for benign prostatic hyperplasia. The Measurement Committee of the American Urological Association. J Urol 1992;148:1549-57. [DOI] [PubMed] [Google Scholar]
- 18.Brown CT, O’Flynn E, van der Meulen J, Newman S, Mundy AR, Emberton M. The fear of prostate cancer in men with lower urinary tract symptoms: should symptomatic men be screened? BJU Int 2003;91:30-2. [DOI] [PubMed] [Google Scholar]
- 19.Young JM, Muscatello DJ, Ward JF. Are men with lower urinary tract symptoms at increased risk of prostate cancer? A systematic review and critique of the available evidence. BJU Int 2000;85:1037-48. [DOI] [PubMed] [Google Scholar]
- 20.Wilt TJ, Thompson IM. Clinically localised prostate cancer. BMJ 2006;133:1102-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Urological Association. Guideline on the management of benign prostatic hyperplasia (BPH) www.auanet.org/guidelines/bph.cfm (updated 2006).
- 22.European Association of Urology. Guidelines on benign prostatic hyperplasia. www.uroweb.org/fileadmin/user_upload/Guidelines/11%20BPH.pdf (updated 2004).
- 23.Schafer W, Abrams P, Liao L, Mattiasson A, Pesce F, Spangberg A, et al. Good urodynamic practices: uroflowmetry, filling cystometry, and pressure-flow studies. Neurourol Urodynamics 2002;21:261-74. [DOI] [PubMed] [Google Scholar]
- 24.Sullivan J, Lewis P, Howell S, Williams T, Shepherd AM, Abrams P. Quality control in urodynamics: a review of urodynamic traces from one centre. BJU Int 2003;91:201-7. [DOI] [PubMed] [Google Scholar]