Abstract
Poisoning may induce failure in multiple organs, leading to death. Supportive treatments and supplementation of failing organs are usually efficient. In contrast, the usefulness of cardiopulmonary bypass in drug-induced shock remains a matter of debate. The majority of deaths results from poisoning with membrane stabilising agents and calcium channel blockers. There is a need for more aggressive treatment in patients not responding to conventional treatments. The development of new antidotes is limited. In contrast, experimental studies support the hypothesis that cardiopulmonary bypass is life-saving. A review of the literature shows that cardiopulmonary bypass of the poisoned heart is feasible. The largest experience has resulted from the use of peripheral cardiopulmonary bypass. However, a literature review does not allow any conclusions regarding the efficiency and indications for this invasive method. Indeed, the majority of reports are single cases, with only one series of seven patients. Appealing results suggest that further studies are needed. Determination of prognostic factors predictive of refractoriness to conventional treatment for cardiotoxic poisonings is mandatory. These prognostic factors are specific for a toxicant or a class of toxicants. Knowledge of them will result in clarification of the indications for cardiopulmonary bypass in poisonings.
Introduction
Failure of various organs may result in the death of acutely poisoned patients. In the 1960s, sedative-induced respiratory failure was the leading cause of death in Western countries. In these cases, endotracheal intubation and mechanical ventilation dramatically improved the prognosis. Similarly, renal replacement therapy with dialysis prevents deaths related to toxicant-induced acute renal failure. Even drug-induced fulminant liver failure is successfully treated in selected cases by liver transplantation. In contrast, the usefulness of temporary mechanical assistance in drug-induced cardiac failure still remains a matter of debate [1,2].
However, promising results have been obtained using a combination of percutaneous cardiopulmonary support and cardiac resuscitation [3,4]. Furthermore, a recent report of the first series of acute poisonings treated with extra-corporeal life support (ECLS) [5], together with an increasing number of case reports [6-10], suggests it is necessary to define the place of this aggressive treatment for drug-induced cardiotropic toxicity.
Drug-induced cardiovascular shock: a leading cause of death
Over the past 30 years, improvements in the treatment of drug-induced cardiovascular shock have been due mainly to a better understanding of the different mechanisms of shock. Routine bedside haemodynamic examinations have provided evidence of the different mechanisms of drug-induced cardiovascular shock, which has enabled the selection of drugs to address the different components of shock. Within the same period of time, indications for mechanical ventilation were extended to conscious poisoned patients presenting with severe cardiovascular shock. Consequently, the prognosis of some cardiotropic drug poisonings improved. Indeed, in a prospective study with historical controls, the combination of epinephrine, diazepam and mechanical ventilation significantly improved the outcome of previously fatal chloroquine poisonings [11,12].
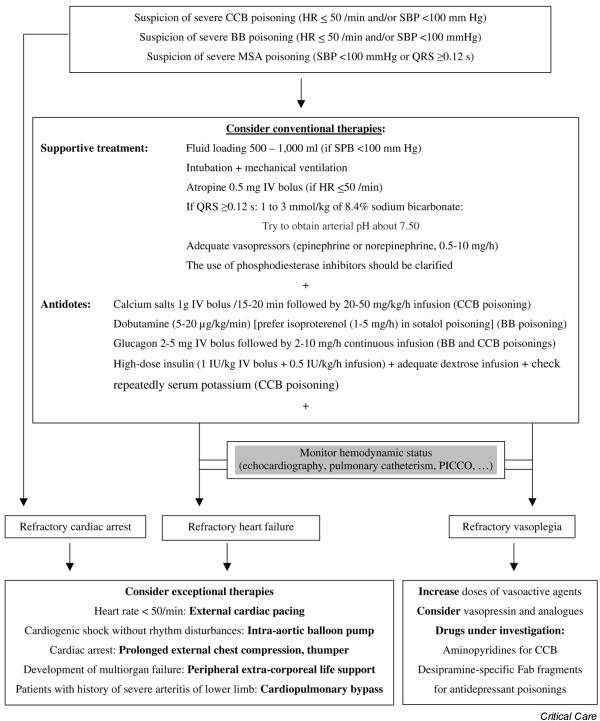
In addition to supportive treatment, a number of antidotes and specific treatments have been investigated (Figure 1). Among cardiotoxic drugs, however, only one antidote, digitalis-specific Fab fragments, has succeeded in improving the prognosis of digitalis poisoning. Digitalis-specific Fab fragments are highly efficient and should now be considered as first-line treatment for this formerly deadly poisoning [13].
Figure 1.
Proposed algorithm for the treatment of severe calcium-channel-blocker (CCB), beta-blocker (BB), and membrane-stabilizing agent (MSA) poisoning. This algorithm is based on series and case reports. HR, heart rate; SBP, systolic blood pressure.
There is no further need for anti-arrhythmics, endocardial pacemakers or even ECLS, which had been used in the past [14,15], providing that digoxin-specific Fab fragments are available [15]. However, the future of immunotherapy in the treatment of other cardiotoxic drug poisonings still remains uncertain. Desipramine-specific Fab fragments were shown to be efficient in experimental models [16,17] but the conclusion of clinical trials is still pending [18]. Similarly, colchicine-specific Fab fragments were also shown to be efficient in experimental models [19-23] but only one life-threatening human case has benefited from this treatment due to a shortage of specific Fab fragments [24].
In spite of treatment improvement, drug-induced cardiovascular failure still remains a leading cause of death. Among 847,483 poisonings in adults over 19 years of age, cardiovascular drugs were involved in 5.8% [25]; however, cardiovascular drugs accounted for about 19% of the total 1,261 poisoning fatalities. Calcium channel blockers and beta-blockers account for approximately 40% of cardiovascular drug poisonings reported to the American Association of Poison Control Centers (AAPCC) but represent more than 65% of deaths from cardiovascular medications [26]. In the 1980s, Henry and Cassidy [27] elegantly showed that, for a pharmacological class of drugs, the mortality rate is significantly increased in poisonings involving drugs with a membrane stabilising activity (MSA) in addition to their main pharmacological activity. Since then, the increase in mortality rate induced by drugs with a MSA has been consistently confirmed [28]. Unfortunately, despite decreased use of some cardiotoxic drugs and the withdrawal of dextropropoxyphene in some countries, many widely prescribed drugs still have a MSA (Table 1), so the finding of Henry and Cassidy still holds true today [28]. Indeed, venlafaxine [29] and citalopram [30] have been shown to induce severe cardiovascular shock and, recently, high dose bupropion was shown to induce intraventricular conduction defects [31].
Table 1.
Drugs having 'membrane stabilising activity' with the potential for severe cardiotoxicity depending on dose
| Anti-arrhythmics class I Vaughan Williams | Flecainide, disopyramide, cibenzoline, propafenone, quinidine, lidocaine, procainamide |
| Beta-blockers | Propranolol, acebutolol, nadoxolol, pindolol, penbutolol, labetalol, oxprenolol |
| Polycyclic antidepressants | Imipramine, desipramine, amitritptyline, clomipramine, dosulepin, doxepin, maprotiline |
| Selective serotonin reuptake inhibitors | Include venlafaxine, citalopram |
| Dopamine and norepinephrine uptake inhibitors | Include bupropion |
| Anti-epileptics | Include carbamazepine, phenytoin |
| Phenothiazines | Include thioridazine |
| Opioids | Include dextropropoxyphene |
| Antimalarial agents | Include chloroquine and quinine |
| Anaesthetic-recreational agents | Include cocaine |
Manifestations of severe cardiotoxicity
Severe cardiotoxicity may be evident, either at the time of presentation or during the course of poisoning, by the sudden onset of high degree atrio-ventricular block, asystole, pulse-less ventricular tachycardia or ventricular fibrillation. However, the most frequent presentation of severe cardiotoxicity is hypotension and even cardiovascular shock.
The delay in onset of life-threatening events depends on the toxicant and its galenic formulation, the ingested dose, the duration of QRS length on echocardiogram for the MSA, and the occurrence of mixed cardiotropic poisonings. The delay is up to two hours after ingestion for class I anti-arrhythmics [32] and of about six hours for polycyclic antidepressants [33], chloroquine [12] and beta blockers [34]. It should be noted that, in one case series, beta-blocker-induced cardiopulmonary arrest did not develop until patients were in the care of health care personnel in 59% of cases [35]. As in our personal experience, beta-blocker-induced cardiovascular shock may slowly progress after admission to hospital. In these cases, there is a misleading moderate increase in plasma lactate concentration, probably related to the protective effect of beta-blockers on glycolysis and lactate production in comparison with other cardiotoxic poisonings, while there is a severe impairment of microcirculation assessed by a decreasing urine output, an increased serum creatinine concentration, and a progressive alteration in liver function and coagulation tests. The delays in onset with calcium channel blockers have been clarified recently [36]. Asymptomatic patients are unlikely to develop symptoms if the interval between ingestion and the call is greater than six hours for immediate-release products, 18 hours for modified-release products other than verapamil, and 24 hours for modified-release verapamil.
It should be noted that drug-induced cardiovascular shock does not always result from a decrease in cardiac contractility. Many cases of drug-induced shock result from a combination of relative hypovolemia and arterial vasodilation. This point is well recognized for calcium channel blockers and more especially for dihydropyridines, including nifedipine [26]. It is less known for polycyclic antidepressants and chloroquine, while it can be underestimated for labetalol poisoning. Therefore, in drug-induced cardiovascular shock with apparent refractoriness to conventional treatment, it is mandatory to perform a haemodynamic examination using either right heart catheterization or echocardiography to assess the mechanisms of shock. Finally, only a few cases of shock result from cardiogenic shock refractory to conventional treatment. In a series of 137 consecutive cases admitted in our department of severe poisoning with a drug with MSA requiring catecholamine administration for shock in addition to specific treatments, the mortality rate was 28% (unpublished data). These data suggest two conclusions: first, 72% of severe patients had a favourable outcome in association with optimization of conventional treatment (Figure 1); and second, there is a need for more aggressive treatment in the subset of patients not responding to optimal conventional treatment. As stated in the Toxicologic-oriented advanced cardiac life support (TOX-ACLS) guidelines, evidence supports the use of circulatory assist devices such as intra-aortic balloon pumps (IABPs) and emergency cardiopulmonary bypass (CPB) in the management of drug-induced cardiovascular shock refractory to maximal therapy [1].
Experimental evidence of the efficiency of extracorporeal life support in cardiotoxic drug poisonings
Three experimental studies with control groups performed in various species, including dogs and swine, poisoned with membrane stabilising agents support the hypothesis that ECLS is life-saving in comparison with ACLS-treated animals. It is quite interesting to note that, among the large spectrum of cardiotoxic drugs, the authors of the experimental studies selected only drugs having MSA.
Freedman and colleagues [37] poisoned dogs with a 30 mg/kg bolus dose of lidocaine. In the control group, dogs were treated with antiarrhythmics, vasopressors, and cardio-version. Of the 8 animals, 6 died within 30 minutes after lidocaine infusion. In the ECLS group, none of the eight animals died. Furthermore, the total body clearance of lidocaine in the ECLS group was comparable to that in animals having received a non-toxic dose of lidocaine, 39.75 ± 4.16 ml/kg/minute and 38.29 ± 8.6 ml/kg/minute, respectively.
Martin and colleagues [38] poisoned 12 dogs with intravenous 1 mg/kg/minute desipramine until they arrested in spite of aggressive supportive care. Six were treated with up to two hours of ACLS with a thumper and six with ECLS. Dogs achieving return of spontaneous circulation to a sufficient degree to wean them from the thumper or ECLS were observed for one hour further. Return of spontaneous circulation occurred in one of six dogs in the thumper group and all six dogs in the ECLS group. Furthermore, the surviving dogs from the thumper and ECLS groups required a mean of 60 mg/kg versus 31 mg/kg norepinephrine and 2.2 mg versus no epinephrine, respectively, during the period of observation. In this model of severe desipramine toxicity, resuscitation with ECLS was superior to ACLS with a thumper.
Larkin and colleagues [39] poisoned 20 swine with intravenous amitriptyline 0.5 mg/kg/minute until systolic blood pressure dropped below 30 mmHg for 1 minute. The control group received supportive treatment, including intravenous fluids, sodium bicarbonate, and vasopressors. Control animals failing to respond to supportive measures after 5 minutes were given open-chest cardiac massage for 30 minutes or until return of spontaneous circulation. The ECLS group received only mechanical support by ECLS for 90 to 120 minutes. No sodium bicarbonate, antiarrhythmics, or cardiotonic agents were provided to the ECLS group during this resuscitation. All 20 animals experienced cardiac conduction delays, dysrhythmias and progressive hypotension within 30 minutes of receiving amitriptyline. Only one of the ten animals in the control group could be resuscitated. In contrast, the ten animals in the ECLS group had complete correction of the dysrhythmias, cardiac conduction abnormalities, and hypotension related to amitriptyline. Nine of these ten swine were easily weaned off bypass without any pharmacological intervention; however, one required nor-epinephrine to be weaned. The authors concluded that ECLS improved survival in this swine model of severe amitriptyline poisoning.
Temporary mechanical assistance of the poisoned failing heart
When evaluating the medical literature on this topic, it should be emphasized that different extracorporeal techniques have been used [40,41]. Unfortunately, the same word is used with different meanings.
Extracorporeal membrane oxygenation (ECMO) is used to treat refractory hypoxemia induced by the acute respiratory distress syndrome, and it has been used in a limited number of cases of severe drug-induced hypoxemia [7-9,42]. It is a venous-venous method providing oxygenation of venous blood; thus, there is no circulatory support. The use of ECMO for respiratory failure following ingestion or inhalation has the same limited indications as for other patients with respiratory failure [43]. It should be emphasized that data supporting an improvement in outcome are not available.
An IABP is an arterial device aimed at decreasing left ventricular afterload. It provides limited support of cardiac output, increasing it by about 20%. IABPs are the first choice for mechanical circulatory support and do play a certain beneficial role in the management of cardiogenic shock [44]. They have been used alone to treat life-threatening toxic manifestations induced by quinidine [45], propranolol [46], dextropropoxyphene [47], antihistamine [48] poisonings, and a combination of verapamil and atenolol [49] poisonings. Furthermore, an IABP has been used in combination with ECLS in a case of organophosphate poisoning [50]. However, IABPs do not work in patients with cardiac arrest. When dealing with cardiotoxic drugs, this is a major limitation as major events of cardiotoxic poisonings are ventricular tachycardia and fibrillation as well as electromechanical dissociation and refractory asystole.
CPB basically provides circulatory support, although it collects venous oxygen-desaturated blood in the right atrium and, thus, always requires an oxygenator, which is integrated within the circuitry. CPB requires sternotomy and both atrial and aortic cannulations. Thus, it is a surgical procedure whose use must be restricted to the operating room. CPB has been performed in cases of aconite [51], diltiazem [6], and verapamil [52] poisonings, and has been used in combination with an IABP in a case of prajmalinum poisoning [53]. CPB is an invasive method resulting in a number of potentially life-threatening complications. In one case of massive diltiazem poisoning treated with CPB, the procedure was prematurely terminated after 48 hours because of uncontrollable mediastinal haemorrhage (21 litres over 30 hours) [6]. Coagulopathy and extensive blood loss from mediastinal drains were reported during the course of aconite poisoning as well as further tamponade, necessitating evacuation of mediastinal haematoma [51].
ECLS (or CPB support or percutaneous cardiopulmonary support or extracorporeal circulation) also provides circulatory support. In contrast with CPB, ECLS can be performed using peripheral cannulations of both arterial and venous vessels. In adults, femoral vessels are the most frequently used. In infants, other vessels have also been used, including the carotid artery and internal jugular vein [54]. As for CBP, ECLS requires ECMO. ECLS may result in blood flows ranging from 1.5 to 6 l/minute, thus providing a complete supplementation of a failing or even arrested heart. The preferred method for cannulation remains a matter of debate. Percutaneous cannulation of femoral vessels is used. However, a blinded approach of vessels may cause laceration resulting in severe occult local bleeding. Furthermore, due to the size of the arterial cannula of about 15 to 17 F gauge, the occlusion of the vessel lumen by the cannula may result in arterial ischemia. A peripheral femoro-femoral shunt was shown able to prevent this severe complication of ECLS [5]. Cases in which ECLS has been used include imipramine [55], desipramine [54,56], carbamazepine [10], propranolol [57], acebutolol [58], disopyramide [59], quinidine [60], flecainide [54,61,62], verapamil [63], digoxin [15], and chloroquine [64] poisonings. Peripheral ECLS has been used in combination with an IABP in a case of organophosphate poisoning [50]. Babatasi and colleagues [5] and Massetti and colleagues [65] published a series of seven consecutive severe poisonings involving cardiotropic drugs and treated with ECLS using the peripheral bypass to prevent limb ischemia. Circulation in the cannulated limb was provided by a tube inserted distally into the superficial femoral artery and connected to the side port of the ECLS arterial line [65]. In contrast to other case reports, in this series the majority of poisonings resulted from mixed poisonings involving a combination of sotalol and verapamil in one case, acebutolol and meprobamate in two cases, propranolol, verapamil and betaxolol in one case, and various psychotropic drugs in one case; the single drug poisoning resulted from disopyramide ingestion [5].
ECLS is, however, an invasive method and may also result in life-threatening complications [2]. In a case of flecainide poisoning, ECLS was discontinued after ten hours because of persistent haemorrhage at the cannulation site [61]. Coagulopathy may result in severe bleeding requiring multiple transfusions despite the use of aprotinin infusion [62]. Femoral nerve palsy [62] and deep venous thrombosis [62] have also been reported. In this critical condition, severe haemorrhage has also been reported at sites other than the cannulation site. Auzinger and Scheinkestel [54] reported extensive diffuse retroperitoneal haemorrhage, attributable to a femoral catheter inserted under resuscitation conditions. In addition to haemorrhagic complications, ischemia of the cannulated limb may occur. In the series of seven poisoned patients reported by Massetti and colleagues [65], the first three patients had severe ischemic complications of the distal leg; two patients died and one patient underwent fasciotomy for a lower leg compartment syndrome. Furthermore, severe hypotension four hours after ECLS cessation has been reported in one patient [2]. Pulmonary oedema may require emergency decompression of the left atrium during an ECLS procedure [66]. However, to our knowledge, emergency decompression of the left atrium during ECLS has not been reported in poisoned patients treated with ECLS.
A biventricular assist device was used in one case of scombroid poisoning with refractory myocardial dysfunction [67]. The rationale of the authors to use a biventricular assist device rather than ECLS was pulsatile and adequate blood flow provided by the biventricular device with efficient unloading of the ventricle, and less circuit-related complications. However, the costs of both methods were not compared.
A review of the literature shows that temporary mechanical assistance of poisoned heart is feasible. Furthermore, the largest reported experience has resulted from the use of peripheral ECLS. However, an analysis of the medical literature dealing with extracorporeal assistance of poisoned failing heart does not allow one to draw any conclusions regarding the efficiency or the indications for this invasive method [2]. Regarding the different mechanisms of shock that may be observed in poisoned patients, it should be noted that ECLS should not be considered in shock related to arterial vasodilation. The global survival rate of poisoned patients having benefited from ECLS is about 79%, including many patients that experienced transitory or prolonged cardiac arrest. However, as the majority of cases were single case reports, it is reasonable to assume that failure of ECLS to allow recovery of poisoned patients has been under-reported while the lack of availability and access of patients to this treatment has been ignored. Interestingly, in the international Extracorporeal Life Support Registry Report of 2004, poisonings were not individualized as a cause of cardiac failure in adults [68]. Furthermore, the need to clarify the indications of aggressive management of cardiotropic toxicity is further supported by the recent report of the AAPCC's toxic exposure database. Indeed, in 2005, 676 poisoned patients received cardiopulmonary resuscitation. In contrast, ECMO was performed in only six poisoning cases [25].
Methodology to assess the efficiency of a new treatment is well known in clinical toxicology. The first step is to determine prognostic factors. It should be outlined that prognostic factors are specific for a toxicant or a class of toxicants. Thereafter, knowledge of prognostic factors of a poisoning of interest allows a clinical trial to be performed in a subset of patients with poor prognostic factors. This method was shown to be efficient in digitalis [69,70], chloroquine [11], and colchicine [24] poisonings. Unfortunately, prognostic factors able to predict refractoriness to conventional treatment of cardiotoxic drugs are unknown, except for digitalis [71]. Therefore, the true need for ECLS in the previously reported cases of cardiotoxic drug poisonings cannot be assumed. There is an urgent need to clarify these prognostic factors in order to advance understanding of both the indications as well as the efficiency of this invasive treatment. The report by Massetti and colleagues [65] on seven consecutive patients suggests that ECLS is promising in cardiotoxic poisoned patients. However, in this series, cardiotoxic drugs belonged to different toxicological classes, precluding any broad conclusion. Finally, peripheral ECLS permits one to institute ECLS outside the operating room and to begin immediate cardiopulmonary perfusion [72].
Several pre-requisites should be considered for the development of ECLS in a medical intensive care unit. There is a need to establish a close collaboration with a department of cardiac surgery [73]. Indeed, depending on local facilities, cardiac surgeons may decide whether ECLS will be performed inside the department of cardiac surgery, requiring the patient to be transferred to the surgical intensive care unit in a hospital with a cardiac surgery facility, or will be performed in the medical intensive care unit. The latter solution requires training of intensivists to some degree regarding the surgical approach of the femoral vessels at the Scarpa, while additional physicians and nurses have to be trained in the priming and handling of ECLS. Facilities must exist for coagulation tests as well as emergency blood supply. Cardiac surgeons must be available on a 24 hour a day basis to: discuss the indications for ECLS; insert the cannulae and start ECLS; provide local hemostasis; cope with local complications, including local bleeding and lower limb ischemia; address any complication related to the pump and membrane oxygenation; and withdraw the cannulae and perform vascular repair in case of favourable outcome.
Conclusion
The renewed interest regarding the efficiency and safety of temporary mechanical assistance of the poisoned heart has highlighted the frequency and high mortality rate of cardiotoxic drugs. There is a need for more aggressive treatment in the subset of patients not responding to conventional treatment. Experimental studies support the hypothesis that ECLS is life-saving in comparison with ACLS-treated animals. In contrast, the majority of human cases are single case reports, except for one series. Appealing clinical results have been reported supporting the assumption that further studies are needed to clarify prognostic factors of cardiotoxic drug poisonings and, therefore, the indications and usefulness of peripheral ECLS.
Abbreviations
AAPCC = American Association of Poison Control Centers; ACLS = advanced cardiac life support; CPB = cardiopulmonary bypass; ECLS = extracorporeal life support; ECMO = extracorporeal membrane oxygenation; IABP = intra-aortic balloon pump; MSA = membrane stabilising activity; SSRI = selective serotonin reuptake inhibitor.
Competing interests
The authors declare that they have no competing interests.
Note
This article is part of a thematic series on Toxicology edited by Philippe Lheureux.
Other articles in this series can be found online at http://ccforum.com/articles/theme-series.asp?series=CC_Toxic
Acknowledgments
Acknowledgements
We are indebted to Prof. Stephen W Borron for his critical review of the manuscript.
References
- Albertson TE, Dawson A, De Latorre F, Hoffman RS, Hollander JE, Jaeger A, Kerns WR, II, Martin TG, Ross MP. TOX-ACLS: toxicologic-oriented advanced cardiac life support. Ann Emerg Med. 2001;37:S78–S90. doi: 10.1067/mem.2001.114174. [DOI] [PubMed] [Google Scholar]
- Purkayastha S, Bhangoo P, Athanasiou T, Casula R, Glenville B, Darzi AW, Henry JA. Treatment of poisoning induced cardiac impairment using cardiopulmonary bypass: a review. Emerg Med J. 2006;23:246–250. doi: 10.1136/emj.2005.028605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees MR, Browne T, Sivananthan UM, Whittaker S, Hick D, Verma SP, Tan LB, Davies GA. Cardiac resuscitation with percutaneous cardiopulmonary support. Lancet. 1992;340:513–514. doi: 10.1016/0140-6736(92)91711-G. [DOI] [PubMed] [Google Scholar]
- Nichol G, Karmy-Jones R, Salerno C, Cantore L, Becker L. Systematic review of percutaneous cardiopulmonary bypass for cardiac arrest or cardiogenic shock states. Resuscitation. 2006;70:381–394. doi: 10.1016/j.resuscitation.2006.01.018. [DOI] [PubMed] [Google Scholar]
- Babatasi G, Massetti M, Verrier V, Lehoux P, Le Page O, Bruno PG, Khayat A. Severe intoxication with cardiotoxic drugs: value of emergency percutaneous cardiocirculatory assistance. Arch Mal Coeur Vaiss. 2001;94:1386–1392. [PubMed] [Google Scholar]
- Durward A, Guerguerian AM, Lefebvre M, Shemie SD. Massive diltiazem overdose treated with extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2003;4:372–376. doi: 10.1097/01.PCC.0000074273.50306.F5. [DOI] [PubMed] [Google Scholar]
- Pizon AF, Brooks DE. Fentanyl patch abuse: naloxone complications and extracorporeal membrane oxygenation rescue. Vet Hum Toxicol. 2004;46:256–257. [PubMed] [Google Scholar]
- Lai MW, Boyer EW, Kleinman ME, Rodig NM, Ewald MB. Acute arsenic poisoning in two siblings. Pediatrics. 2005;116:249–257. doi: 10.1542/peds.2004-1957. [DOI] [PubMed] [Google Scholar]
- Maclaren G, Butt W, Cameron P, Preovolos A, McEgan R, Marasco S. Treatment of polypharmacy overdose with multimodality extracorporeal life support. Anaesth Intensive Care. 2005;33:120–123. doi: 10.1177/0310057X0503300118. [DOI] [PubMed] [Google Scholar]
- Megarbane B, Leprince P, Deye N, Guerrier G, Resiere D, Bloch V, Baud FJ. Extracorporeal life support in a case of acute carbamazepine poisoning with life-threatening refractory myocardial failure. Intensive Care Med. 2006;32:1409–1413. doi: 10.1007/s00134-006-0257-8. [DOI] [PubMed] [Google Scholar]
- Riou B, Barriot P, Rimailho A, Baud FJ. Treatment of severe chloroquine poisoning. N Engl J Med. 1988;318:1–6. doi: 10.1056/NEJM198801073180101. [DOI] [PubMed] [Google Scholar]
- Clemessy JL, Taboulet P, Hoffman JR, Hantson P, Barriot P, Bismuth C, Baud FJ. Treatment of acute chloroquine poisoning: a 5-year experience. Crit Care Med. 1996;24:1189–1195. doi: 10.1097/00003246-199607000-00021. [DOI] [PubMed] [Google Scholar]
- Taboulet P, Baud FJ, Bismuth C. Clinical features and management of digitalis poisoning – rationale for immunotherapy. J Toxicol Clin Toxicol. 1993;31:247–260. doi: 10.3109/15563659309000392. [DOI] [PubMed] [Google Scholar]
- Schmidt W, Reissig M, Neuhaus KL. Percutaneous extracorporeal circulation in cardiogenic shock caused by combined poisoning with methyldigoxin, nifedipine and indapamide. Dtsch Med Wochenschr. 1995;120:996–1002. doi: 10.1055/s-2008-1055437. [DOI] [PubMed] [Google Scholar]
- Behringer W, Sterz F, Domanovits H, Schoerkhuber W, Holzer M, Foedinger M, Laggner AN. Percutaneous cardiopulmonary bypass for therapy resistant cardiac arrest from digoxin overdose. Resuscitation. 1998;37:47–50. doi: 10.1016/S0300-9572(98)00025-2. [DOI] [PubMed] [Google Scholar]
- Pentel PR, Keyler DE. Drug-specific antibodies as antidotes for tricyclic antidepressant overdose. Toxicol Lett. 1995;82–83:801–806. doi: 10.1016/0378-4274(95)03596-6. [DOI] [PubMed] [Google Scholar]
- Dart RC, Sidki A, Sullivan JB, Jr, Egen NB, Garcia RA. Ovine desipramine antibody fragments reverse desipramine cardiovascular toxicity in the rat. Ann Emerg Med. 1996;27:309–315. doi: 10.1016/S0196-0644(96)70265-2. [DOI] [PubMed] [Google Scholar]
- Heard K, Dart RC, Bogdan G, O'Malley GF, Burkhart KK, Donovan JW, Ward SB. A preliminary study of tricyclic antide-pressant (TCA) ovine FAB for TCA toxicity. Clin Toxicol (Phila) 2006;44:275–281. doi: 10.1080/15563650600584428. [DOI] [PubMed] [Google Scholar]
- Sabouraud A, Urtizberea M, Grandgeorge M, Gattel P, Makula ME, Scherrmann JM. Dose-dependent reversal of acute murine colchicine poisoning by goat colchicine-specific Fab fragments. Toxicology. 1991;68:121–132. doi: 10.1016/0300-483X(91)90015-S. [DOI] [PubMed] [Google Scholar]
- Urtizberea M, Sabouraud A, Cano N, Grandgeorge M, Rouzioux JM, Scherrmann JM. Reversal of murine colchicine toxicity by colchicine-specific Fab fragments. Toxicol Lett. 1991;58:193–198. doi: 10.1016/0378-4274(91)90173-4. [DOI] [PubMed] [Google Scholar]
- Sabouraud AE, Urtizberea M, Cano NJ, Grandgeorge M, Rouzioux JM, Scherrmann JM. Colchicine-specific Fab fragments alter colchicine disposition in rabbits. J Pharmacol Exp Ther. 1992;260:1214–1219. [PubMed] [Google Scholar]
- Sabouraud AE, Urtizberea M, Benmoussa K, Cano NJ, Scherrmann JM. Fab-bound colchicine appears to adopt Fab fragment disposition in rats. J Pharm Pharmacol. 1992;44:1015–1019. doi: 10.1111/j.2042-7158.1992.tb07084.x. [DOI] [PubMed] [Google Scholar]
- Sabouraud A, Redureau M, Gires P, Martinet M, Scherrmann JM. Effect of colchicine-specific Fab fragments on the hepatic clearance of colchicine. Drug Metab Dispos. 1993;21:997–1002. [PubMed] [Google Scholar]
- Baud FJ, Sabouraud A, Vicaut E, Taboulet P, Lang J, Bismuth C, Rouzioux JM, Scherrmann JM. Brief report: treatment of severe colchicine overdose with colchicine-specific Fab fragments. N Engl J Med. 1995;332:642–645. doi: 10.1056/NEJM199503093321004. [DOI] [PubMed] [Google Scholar]
- Lai MW, Klein-Schwartz W, Rodgers GC, Abrams JY, Haber DA, Bronstein AC, Wruk KM. 2005 Annual Report of the American Association of Poison Control Centers' national poisoning and exposure database. Clin Toxicol (Phila) 2006;44:803–932. doi: 10.1080/15563650600907165. [DOI] [PubMed] [Google Scholar]
- DeWitt CR, Waksman JC. Pharmacology, pathophysiology and management of calcium channel blocker and beta-blocker toxicity. Toxicol Rev. 2004;23:223–238. doi: 10.2165/00139709-200423040-00003. [DOI] [PubMed] [Google Scholar]
- Henry JA, Cassidy SL. Membrane stabilising activity: a major cause of fatal poisoning. Lancet. 1986;1:1414–1417. doi: 10.1016/S0140-6736(86)91558-8. [DOI] [PubMed] [Google Scholar]
- Henry JA, Alexander CA, Sener EK. Relative mortality from overdose of antidepressants. BMJ. 1995;310:221–224. doi: 10.1136/bmj.310.6974.221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mégarbane B, Bloch V, Deye N, Baud FJ. Pharmacokinetic/pharmacodynamic modelling of cardiac toxicity in venlafaxine overdose. Intensive Care Med. 2007;33:195–196. doi: 10.1007/s00134-006-0419-8. [DOI] [PubMed] [Google Scholar]
- Engebretsen KM, Harris CR, Wood JE. Cardiotoxicity and late onset seizures with citalopram overdose. J Emerg Med. 2003;25:163–166. doi: 10.1016/S0736-4679(03)00164-1. [DOI] [PubMed] [Google Scholar]
- Curry SC, Kashani JS, LoVecchio F, Holubek W. Intraventricular conduction delay after bupropion overdose. J Emerg Med. 2005;29:299–305. doi: 10.1016/j.jemermed.2005.01.027. [DOI] [PubMed] [Google Scholar]
- Koppel C, Oberdisse U, Heinemeyer G. Clinical course and outcome in class IC antiarrhythmic overdose. J Toxicol Clin Toxicol. 1990;28:433–444. doi: 10.3109/15563659009038586. [DOI] [PubMed] [Google Scholar]
- Boehnert MT, Lovejoy FH., Jr Value of the QRS duration versus the serum drug level in predicting seizures and ventricular arrhythmias after an acute overdose of tricyclic antidepressants. N Engl J Med. 1985;313:474–479. doi: 10.1056/NEJM198508223130804. [DOI] [PubMed] [Google Scholar]
- Love JN, Howell JM, Litovitz TL, Klein-Schwartz W. Acute beta blocker overdose: factors associated with the development of cardiovascular morbidity. J Toxicol Clin Toxicol. 2000;38:275–281. doi: 10.1081/CLT-100100932. [DOI] [PubMed] [Google Scholar]
- Love JN, Litovitz TL, Howell JM, Clancy C. Characterization of fatal beta blocker ingestion: a review of the American Association of Poison Control Centers data from 1985 to 1995. J Toxicol Clin Toxicol. 1997;35:353–359. doi: 10.3109/15563659709043366. [DOI] [PubMed] [Google Scholar]
- Olson KR, Erdman AR, Woolf AD, Scharman EJ, Christianson G, Caravati EM, Wax PM, Booze LL, Manoguerra AS, Keyes DC, et al. Calcium channel blocker ingestion: an evidence-based consensus guideline for out-of-hospital management. Clin Toxicol (Phila) 2005;43:797–822. doi: 10.1080/15563650500357404. [DOI] [PubMed] [Google Scholar]
- Freedman MD, Gal J, Freed CR. Extracorporeal pump assistance – novel treatment for acute lidocaine poisoning. Eur J Clin Pharmacol. 1982;22:129–135. doi: 10.1007/BF00542457. [DOI] [PubMed] [Google Scholar]
- Martin TG, Klain MM, Molner RL, Michelson EA, Schneider SM. Extracorporeal life support vs thumper after lethal desipramine OD (abstract) Vet Hum Toxicol. 1990;32:349. [Google Scholar]
- Larkin GL, Graeber GM, Hollingsed MJ. Experimental amitripty-line poisoning: treatment of severe cardiovascular toxicity with cardiopulmonary bypass. Ann Emerg Med. 1994;23:480–486. doi: 10.1016/S0196-0644(94)70066-4. [DOI] [PubMed] [Google Scholar]
- Bosquet C, Jaeger A. Thérapeutiques d'exception au cours des défaillances circulatoires et respiratoires d'origine toxique. Réanimation. 2001;10:402–411. doi: 10.1016/S1164-6756(01)00140-2. [DOI] [Google Scholar]
- Boettcher W, Merkle F, Weitkemper HH. History of extracorpo-real circulation: the invention and modification of blood pumps. J Extra Corpor Technol. 2003;35:184–191. [PubMed] [Google Scholar]
- Ishigami S, Hase S, Nakashima H, Yamada H, Dohgomori H, Natsugoe S, Aikou T. Intravenous chlorhexidine gluconate causing acute respiratory distress syndrome. J Toxicol Clin Toxicol. 2001;39:77–80. doi: 10.1081/CLT-100102884. [DOI] [PubMed] [Google Scholar]
- Banner W., Jr Risks of extracorporeal membrane oxygenation: is there a role for use in the management of the acutely poisoned patient? J Toxicol Clin Toxicol. 1996;34:365–371. doi: 10.3109/15563659609013805. [DOI] [PubMed] [Google Scholar]
- Menon V, Hochman J. Management of cardiogenic shock complicating acute myocardial infarction. Heart. 2002;88:531–537. doi: 10.1136/heart.88.5.531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shub C, Gau GT, Sidell PM, Brennan LA., Jr The management of acute quinidine intoxication. Chest. 1978;73:173–178. doi: 10.1378/chest.73.2.173. [DOI] [PubMed] [Google Scholar]
- Lane AS, Woodward AC, Goldman MR. Massive propranolol overdose poorly responsive to pharmacologic therapy: use of the intra-aortic balloon pump. Ann Emerg Med. 1987;16:1381–1383. doi: 10.1016/S0196-0644(87)80425-0. [DOI] [PubMed] [Google Scholar]
- Gillard P, Laurent M. Dextropropoxyphene-induced cardiogenic shock: treatment with intra-aortic balloon pump and milrinone. Intensive Care Med. 1999;25:335. doi: 10.1007/PL00003771. [DOI] [PubMed] [Google Scholar]
- Freedberg RS, Friedman GR, Palu RN, Feit F. Cardiogenic shock due to antihistamine overdose. Reversal with intra-aortic balloon counterpulsation. JAMA. 1987;257:660–661. doi: 10.1001/jama.257.5.660. [DOI] [PubMed] [Google Scholar]
- Frierson J, Bailly D, Shultz T, Sund S, Dimas A. Refractory cardiogenic shock and complete heart block after unsuspected verapamil-SR and atenolol overdose. Clin Cardiol. 1991;14:933–935. doi: 10.1002/clc.4960141114. [DOI] [PubMed] [Google Scholar]
- Kamijo Y, Soma K, Uchimiya H, Asari Y, Ohwada T. A case of serious organophosphate poisoning treated by percutaneus cardiopulmonary support. Vet Hum Toxicol. 1999;41:326–328. [PubMed] [Google Scholar]
- Fitzpatrick AJ, Crawford M, Allan RM, Wolfenden H. Aconite poisoning managed with a ventricular assist device. Anaesth Intensive Care. 1994;22:714–717. doi: 10.1177/0310057X9402200614. [DOI] [PubMed] [Google Scholar]
- Hendren WG, Schieber RS, Garrettson LK. Extracorporeal bypass for the treatment of verapamil poisoning. Ann Emerg Med. 1989;18:984–987. doi: 10.1016/S0196-0644(89)80465-2. [DOI] [PubMed] [Google Scholar]
- Pasic M, Potapov E, Kuppe H, Hetzer R. Prolonged cardiopulmonary bypass for severe drug intoxication. J Thorac Cardiovasc Surg. 2000;119:379–380. doi: 10.1016/S0022-5223(00)70195-4. [DOI] [PubMed] [Google Scholar]
- Auzinger GM, Scheinkestel CD. Successful extracorporeal life support in a case of severe flecainide intoxication. Crit Care Med. 2001;29:887–890. doi: 10.1097/00003246-200104000-00041. [DOI] [PubMed] [Google Scholar]
- Williams JM, Hollingshed MJ, Vasilakis A, Morales M, Prescott JE, Graeber GM. Extracorporeal circulation in the management of severe tricyclic antidepressant overdose. Am J Emerg Med. 1994;12:456–458. doi: 10.1016/0735-6757(94)90062-0. [DOI] [PubMed] [Google Scholar]
- Goodwin DA, Lally KP, Null DM., Jr Extracorporeal membrane oxygenation support for cardiac dysfunction from tricyclic antidepressant overdose. Crit Care Med. 1993;21:625–627. doi: 10.1097/00003246-199304000-00025. [DOI] [PubMed] [Google Scholar]
- McVey FK, Corke CF. Extracorporeal circulation in the management of massive propranolol overdose. Anaesthesia. 1991;46:744–746. doi: 10.1111/j.1365-2044.1991.tb09770.x. [DOI] [PubMed] [Google Scholar]
- Rooney M, Massey KL, Jamali F, Rosin M, Thomson D, Johnson DH. Acebutolol overdose treated with hemodialysis and extracorporeal membrane oxygenation. J Clin Pharmacol. 1996;36:760–763. doi: 10.1002/j.1552-4604.1996.tb04247.x. [DOI] [PubMed] [Google Scholar]
- Yoshida K, Kimura K, Hibi K, Nemoto T, Iwasawa Y, Hongo Y. A patient with disopyramide intoxication rescued by percutaneous cardiopulmonary support. J Cardiol. 1998;32:95–100. [PubMed] [Google Scholar]
- Tecklenburg FW, Thomas NJ, Webb SA, Case C, Habib DM. Pediatric ECMO for severe quinidine cardiotoxicity. Pediatr Emerg Care. 1997;13:111–113. doi: 10.1097/00006565-199704000-00007. [DOI] [PubMed] [Google Scholar]
- Yasui RK, Culclasure TF, Kaufman D, Freed CR. Flecainide overdose: is cardiopulmonary support the treatment? Ann Emerg Med. 1997;29:680–682. doi: 10.1016/S0196-0644(97)70257-9. [DOI] [PubMed] [Google Scholar]
- Corkeron MA, van Heerden PV, Newman SM, Dusci L. Extracorporeal circulatory support in near-fatal flecainide overdose. Anaesth Intensive Care. 1999;27:405–408. doi: 10.1177/0310057X9902700413. [DOI] [PubMed] [Google Scholar]
- Holzer M, Sterz F, Schoerkhuber W, Behringer W, Domanovits H, Weinmar D, Weinstabl C, Stimpfl T. Successful resuscitation of a verapamil-intoxicated patient with percutaneous cardiopulmonary bypass. Crit Care Med. 1999;27:2818–2823. doi: 10.1097/00003246-199912000-00035. [DOI] [PubMed] [Google Scholar]
- Mauriat P, Pouard P, Malhère T, Journois D, Lefèbvre D, Deny N. Assistance cardiocirculatoire percutanée en urgence au cours de l'intoxication aiguë grave par la chloroquine. Ann Fr Anesth Réan. 1993;12(Suppl):R105. [Google Scholar]
- Massetti M, Bruno P, Babatasi G, Neri E, Khayat A. Cardiopulmonary bypass and severe drug intoxication. J Thorac Cardiovasc Surg. 2000;120:424–425. doi: 10.1067/mtc.2000.109549. [DOI] [PubMed] [Google Scholar]
- Aiyagari RM, Rocchini AP, Remenapp RT, Graziano JN. Decompression of the left atrium during extracorporeal membrane oxygenation using a transseptal cannula incorporated into the circuit. Crit Care Med. 2006;34:2603–2606. doi: 10.1097/01.CCM.0000239113.02836.F1. [DOI] [PubMed] [Google Scholar]
- Grinda JM, Bellenfant F, Brivet FG, Carel Y, Deloche A. Biventricular assist device for scombroid poisoning with refractory myocardial dysfunction: a bridge to recovery. Crit Care Med. 2004;32:1957–1959. doi: 10.1097/01.CCM.0000139921.38352.3D. [DOI] [PubMed] [Google Scholar]
- Conrad SA, Rycus PT, Dalton H. Extracorporeal Life Support Registry Report 2004. Asaio J. 2005;51:4–10. doi: 10.1097/01.MAT.0000151922.67540.E9. [DOI] [PubMed] [Google Scholar]
- Smith TW, Haber E, Yeatman L, Butler VP. Reversal of advanced digoxin intoxication with Fab fragments of digoxin-specific antibodies. N Engl J Med. 1976;294:797–800. doi: 10.1056/NEJM197604082941501. [DOI] [PubMed] [Google Scholar]
- Hickey AR, Wenger TL, Carpenter VP, Tilson HH, Hlatky MA, Furberg CD, Kirkpatrick CH, Strauss HC, Smith TW. Digoxin immune Fab therapy in the management of digitalis intoxication: safety and efficacy results of an observational surveillance study. J Am Coll Cardiol. 1991;17:590–598. doi: 10.1016/s0735-1097(10)80170-6. [DOI] [PubMed] [Google Scholar]
- Bismuth C, Baud F, Dally S. Standardized prognosis evaluation in acute toxicology its benefit in colchicine, paraquat and digitalis poisonings. J Toxicol Clin Exp. 1986;6:33–38. [PubMed] [Google Scholar]
- Pasic M, Hetzer R. Cardiopulmonary bypass and severe drug intoxication. J Thorac Cardiovasc Surg. 2000;120:424–425. doi: 10.1067/mtc.2000.107825. [DOI] [PubMed] [Google Scholar]
- Mégarbane B, Leprince P, Deye N, Résière D, Guerrier G, Rettab S, Théodore J, Karyo S, Gandjbakhch I, Baud FJ. Emergency feasibility in medical intensive care unit of extracorporeal life support for refractory cardiac arrest. Intensive Care Med. 2007 doi: 10.1007/s00134-007-0568-4. [DOI] [PubMed] [Google Scholar]