Abstract
Objectives
It is of potentially great public health importance to determine whether youth-onset anxiety disorders are associated with increased prevalence of subsequent bipolar I disorder (BD) among adults, and to identify risk factors for BD in this population.
Methods
The 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions was used to identify respondents with social phobia, panic disorder, or generalized anxiety disorder that onset in youth (<19 years) and was not preceded by a major depressive, manic, or mixed episode (N=1,571; 572 males, 999 females). The prevalence of BD among subjects with, versus without, these youth-onset anxiety disorders was examined. Variables that could be associated with increased risk of BD among subjects with youth-onset anxiety disorders were examined, including conduct disorder, youth-onset substance use disorders (SUD), and family history of depression and/or alcoholism. Analyses were computed separately for males and females.
Results
The prevalence of BD was significantly greater among adults with, versus without, primary youth-onset anxiety disorders for both males (15.9% vs 2.7%; χ2=318.4, df=1, p<0.001) and females (13.8% vs 2.9%; χ2=346.2, df=1, p<0.001). Youth-onset anxiety disorders remained significantly associated with BD after controlling for interceding major depression, and this was true for each of the specific anxiety disorders examined. Among males with youth-onset primary anxiety disorders, conduct disorder and loaded family history of depression were associated with significantly increased risk of BD. Among females, conduct disorder and loaded family history of alcoholism were associated with significantly increased risk of BD.
Conclusions
The prevalence of BD was elevated among subjects with youth-onset primary anxiety disorders, particularly if comorbid conduct disorder was present. Future studies are needed to confirm these findings prospectively, and to develop preventive strategies for populations at risk.
Keywords: bipolar I disorder, anxiety, panic, alcohol, drug, substance
BACKGROUND
There is convergent evidence from clinical and epidemiologic studies of adults that anxiety disorders are among the most frequent and burdensome comorbidities of bipolar I disorder (BD). In particular, with respect to BD, anxiety disorders are associated with earlier age of onset, poorer treatment response (Feske et al, 2000), exacerbated illness course and severity (Goodwin and Hoven, 2002; Boylan et al, 2004; Keller, 2006; Otto et al, 2006), and suicidality (Dilsaver and Chen, 2003). Previous studies have also demonstrated that anxiety disorders among youth are significant predictors of later BD in adulthood (Goodwin and Hamilton, 2002; Johnson et al, 2000; Kessler et al, 1997; Kim-Cohen et al, 2003; Perugi et al, 2001), and anxiety disorders predate BD among most youth with comorbid anxiety disorders and BD (Dickstein et al, 2005; Dilsaver and White, 1986; Masi et al, 2001; Wagner, 2006). This is important because antidepressants are first-line pharmacotherapy for child and adolescent anxiety disorders (Varley and Smith, 2003; Bernstein and Shaw, 1997) and such treatment risks unmasking latent BD among youth with underlying diathesis (Faedda et al, 2004; Go et al, 1998). Therefore it is of utmost clinical and public health relevance to begin to identify risk factors for BD among youth with anxiety disorders. Seminal studies have documented specific risk factors for the emergence of BD among youth initially presenting with major depression (DelBello et al, 2003; Geller et al, 2001; Akiskal et al, 1995; Strober and Carlson, 1982), and findings from these studies continue to inform clinical practice. However, the factors associated with later BD among youth with anxiety disorders have yet to be examined.
Another question that has arisen relates to the specificity of the association between youth anxiety disorders and BD. Birmaher and colleagues (2002) have suggested that panic disorder may be specifically associated with BD among youth, however other studies have reported high rates of a variety of anxiety disorders among youth with BD (Dickstein et al, 2005; Harpold et al, 2005). Kessler and colleagues (1997) examined the association of antecedent anxiety disorders with later BD using data from the National Comorbidity Survey, and found that anxiety disorders, particularly generalized anxiety disorder and panic disorder, confer an exceedingly high risk of subsequent BD. In fact, the odds ratio for antecedent anxiety disorders predicting BD (31.2) approached that of antecedent affective disorders (i.e., major depressive episode or dysthymia; odd ratio 36.7). However, findings from that study pertained only to a specific group of BD subjects with euphoric mania with attendant grandiosity and decreased need for sleep.
Previous studies have been able to demonstrate increased risk for BD among large samples of subjects with antecedent anxiety disorders. However, with modest numbers of subjects with BD (N=10 to N=29) these studies have not been able to examine specific factors that confer particular risk for BD among those with anxiety disorders (Johnson et al, 2000; Kessler et al, 1997; Kim-Cohen et al, 2003). One such factor that may predict BD among people with youth-onset anxiety disorders is conduct disorder. Conduct disorder is exceedingly common in youth BD (Biederman et al, 1999), and the prevalence of antisocial personality disorder is roughly double among adults with BD as compared to those with any anxiety disorder (20.6% vs 9.2%) (Grant et al, 2005). Another factor that may predict BD is substance use disorder (SUD; i.e. substance abuse or dependence). The Epidemiologic Catchment Area study found that whereas anxiety disorders are associated with an odds ratio of 1.7 for any SUD, BD is associated with an odds ratio of 7.9 for any SUD (Regier et al, 1990), and this finding has since been replicated (Grant et al, 2004). It could be expected that SUD in the context of an anxiety disorder may confer or reflect added risk of BD. Finally, family history of depression (Weissman et al, 2006) and of alcoholism (Winokur et al, 1996) have been associated with BD, and may be expected to confer added risk of BD to those with youth-onset anxiety disorders. Data regarding family history of BD were not available for this study.
A large-scale study is needed in order to address three central questions: 1) are primary youth-onset anxiety disorders (i.e. not preceded by mania or depression) predictive of later DSM-IV BD, including cases of irritable mania? [Cases in which depression preceded anxiety are not included in the present study because it is already known that youth-onset depression is frequently the initial mood episode of BD (DelBello et al, 2003; Geller et al, 2001; Akiskal et al, 1995; Strober and Carlson, 1982), whereas the same is not true for anxiety disorders.] 2) do different anxiety disorders confer different risks of BD? 3) among adults with primary youth-onset anxiety disorders, which clinical and demographic variables distinguish those who develop BD from those who do not? The following hypotheses are offered: 1) youth-onset primary anxiety disorders are significant predictors of BD; 2) panic disorder most strongly predicts BD among the three anxiety disorders examined; 3) conduct disorder, SUD, and loaded family history of depression and/or alcoholism are significant predictors of BD among subjects with primary youth-onset anxiety disorders. This study examined primary youth-onset social phobia, panic disorder, and generalized anxiety disorder. Separation anxiety disorder, post-traumatic stress disorder, and obsessive-compulsive disorder were not included in the survey on which this study was based, and could not be examined in this study.
METHOD
Subjects
Subjects were identified from among the respondents of the 2001-2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). This study focused on 1571 respondents (572 males, 999 females) with lifetime social phobia, panic disorder (with or without agoraphobia), and generalized anxiety disorder, who reported that at least one of these anxiety disorders onset prior to the age of 19 and was not preceded by a depressive, manic, or mixed episode (i.e., primary anxiety disorder). The NESARC is a representative sample of the United States conducted by the National Institute on Alcoholism and Alcohol Abuse (NIAAA). A detailed description of the NESARC has been described elsewhere (Grant et al, 2004a). Briefly, 43,093 non-institutionalized civilian respondents, 18 years and older, completed face-to-face computer-assisted personal interviews. The overall survey response rate was 81%.
Assessment
Approximately 1800 lay interviewers with an average of 5 years’ related experience administered the NESARC using laptop computer-assisted software. Interviewers completed 10 days of centralized, standardized training sessions. The NIAAA Alcohol Use Disorder and Associated Disabilities Interview Schedule-DSM-IV Version (AUDADIS-IV) was used to generate the diagnoses presented in this report. The AUDADIS-IV diagnoses of personality disorders, substance use disorders (Grant et al, 2004b), and mood and anxiety disorders (Grant et al, 2004a; Grant et al, 2005), have demonstrated reliability and validity. Reliability of the BD diagnosis (κ=0.59) is fair (Grant et al, 2005), while the reliability is excellent for alcohol diagnoses (κ >/=0.74) and drug diagnoses (κ >/=0.79)(Grant et al, 2004b). The anxiety disorders included in the present study are social phobia, panic disorder (with and without agoraphobia), and generalized anxiety disorder, and these have fair to good reliability (κ =0.42-0.52)(Grant et al, 2003). Reliability for antisocial personality disorder is good (κ =0.67)(Grant et al, 2004b). Reliability for the diagnosis of conduct disorder without a diagnosis of antisocial personality disorder has not been determined; however, the dimensional scale associated with this disorder has good reliability (intraclass coefficient = 0.67) (Grant et al, 2003). Age at onset of BD (i.e., age at first manic/mixed episode), and ages at onset for the other diagnoses discussed, as well as family history and demographic variables were all determined from the AUDADIS-IV.
Only cases of independent mood and anxiety disorders are included in the analyses (i.e., not solely related to substance use or medical conditions; see Grant et al, 2004a). Moreover, anxiety disorders that are temporally preceded by the onset of mania or depression are not considered in this study.
This study examined loaded family history of depression and of alcoholism. Subjects were systematically queried regarding whether their relatives had ever been “depressed” or “an alcoholic or problem drinker”. Loaded family history was defined as reported history of the condition either in both parents or in a parent and grandparent in the same lineage. This study also examined SUD and conduct disorder as predictors of BD. SUD comprised any substance abuse or dependence other than nicotine or caffeine. For the purpose of this retrospective study, SUD was considered present if there was at least one SUD that onset prior to the age of 19 and was not preceded by a manic or mixed episode. Similarly, conduct disorder was considered present if onset of conduct disorder was not preceded by a manic or mixed episode.
Statistical analyses
Student’s t-test was used to compare differences between groups on dimensional measures, while chi-square analysis was used to detect differences on categorical measures. Logistic regression analyses were conducted to test the hypothesis that youth-onset anxiety disorders overall (i.e., presence of any of the three anxiety disorders examined) are associated with later BD. Logistic regression analyses were also conducted in order to examine the unique contribution of primary youth-onset social phobia, panic disorder, and generalized anxiety disorder to variance in BD in the overall NESARC sample. Finally, logistic regression analyses were conducted for the 1571 subjects with youth-onset anxiety disorders in order to examine the specific contribution of conduct disorder, SUD, loaded family history of alcoholism, and loaded family history of depression to variance in BD.
Current age was the only demographic variable examined for which there were significant between-group differences, and was therefore included as a covariate in the logistic regressions. Analyses also controlled for the presence of depression that onset consequent to the anxiety disorder. This was done in order to examine the unique contribution of primary anxiety disorders to variance in BD. Analyses were conducted separately for males and females owing to the known gender differences in comorbidity in BD (Hendrik et al, 2000; Baldassano et al, 2005). Moreover, a preliminary logistic regression analysis confirmed that there was a significant interaction between gender and youth-onset anxiety as it relates to predicting BD (χ2=6.9, df=1, p=0.009). Exploratory cross-tabulation analyses were conducted in order to examine for differences in the lifetime prevalence BD among adults with primary youth-onset anxiety disorders as compared to primary adult-onset anxiety disorders.
Statistical analyses were performed using SPSS version 14 (SPSS Inc, Chicago, Illinois). Weighting procedures were not used since this study is not intended to provide population prevalence estimates for any of the diagnoses described herein. These estimates have been previously reported (Grant et al, 2004a, 2004b).
RESULTS
Demographic characteristics of 572 males and 999 females with youth-onset primary anxiety disorders are presented in Table 1. The mean age for subjects with BD was significantly younger as compared to subjects without BD. These groups did not differ significantly, however, in terms of sex, race, or mean annual income.
Table 1.
Demographic Characteristics of 1571 Adults with Youth-Onset Anxiety Disorders with and without Lifetime Bipolar I Disorder
| With Bipolar I Disorder | Without Bipolar I Disorder | ||||
|---|---|---|---|---|---|
| N | % | N | % | χ2 | |
| Female | 138/229 | 60.3 | 861/1342 | 64.2 | 1.3 |
| White | 183/229 | 79.9 | 1135/1342 | 84.6 | 3.1 |
| Mean | SD | Mean | SD | t | |
| Age | 39.1 | 14.3 | 43.0 | 16.3 | 3.3** |
| Incomeˆ | 19.2 | 22.6 | 24.9 | 4.1 | 1.9 |
p<0.01
Annual personal income, expressed in thousands of dollars
The first question addressed in this study is whether BD is significantly more prevalent among adults with, as compared to without, youth-onset primary anxiety disorders. Among both males and females, those with a history of youth-onset anxiety disorders had significantly greater prevalence of BD, and this was true for each of the specific anxiety disorders as well (Table 2). Logistic regression analyses demonstrated that primary youth-onset anxiety disorders are uniquely and significantly associated with BD, after controlling for the presence of depression that onset consequent to anxiety, among both males (χ2=117.0, df=1, p<0.001) and females (χ2=112.6, df=1, p<0.001). The corresponding adjusted odds ratios were 4.1 (95% confidence interval [CI] = 3.2-5.4) for males and 3.0 (95% CI = 2.5-3.7) for females.
Table 2.
Lifetime Prevalence of Bipolar I Disorder among Adult Males and Females with versus without Primary Youth-Onset Anxiety Disorders
| Subjects with Lifetime Bipolar I Disorder, N (%) | ||||||
|---|---|---|---|---|---|---|
| Predictor Variable Present | Predictor Variable Absent | |||||
| N | % | N | % | χ2 | Odds Ratio (95% CIˆ) | |
| Males: | ||||||
| Any Anxiety Disorder | 91/572 | 15.9 | 488/17946 | 2.7 | 318.4*** | 6.8 (5.3-8.6) |
| Social Phobia | 74/513 | 14.4 | 505/18005 | 2.8 | 222.4*** | 5.8 (4.5-7.6) |
| Panic Disorder | 17/62 | 27.4 | 562/18456 | 3.0 | 121.2*** | 12.0 (6.8-21.1) |
| Generalized Anxiety Disorder | 18/51 | 35.3 | 561/18467 | 3.0 | 174.7*** | 17.4 (9.7-31.1) |
| Females: | ||||||
| Any Anxiety Disorder | 138/999 | 13.8 | 694/23576 | 2.9 | 346.2*** | 5.3 (4.3-6.4) |
| Social Phobia | 118/873 | 13.5 | 714/23702 | 3.0 | 284.0*** | 5.0 (4.1-6.2) |
| Panic Disorder | 20/122 | 16.4 | 812/24453 | 3.3 | 63.4*** | 5.7 (3.5-9.3) |
| Generalized Anxiety Disorder | 29/127 | 22.8 | 803/24448 | 3.3 | 147.6*** | 8.7 (5.7-13.3) |
CI=confidence interval
p<0.001
The second question addressed in this study is whether the different anxiety disorders confer different risks of BD. Youth-onset social phobia was associated with a significantly increased prevalence of BD among both males and females (Table 2). Youth-onset panic disorder and generalized anxiety disorder were associated with even greater prevalence of BD (Table 2). Most strikingly, greater than one third of males and nearly one quarter of females with youth-onset generalized anxiety disorder in the present sample had BD, corresponding with odds ratios of 17.4 (95% CI 9.7-31.1) and 8.7 (95% CI 5.7-13.3), respectively. Logistic regression analyses examined the independent contribution of each of the three anxiety disorders to the variance in BD. Social phobia was uniquely and significantly associated with BD (after controlling for the other anxiety disorders and intercedent depression), among both males (χ2=56.1, df=1, p<0.001) and females (χ2=64.3, df=1, p<0.001). Similarly, youth-onset panic disorder was uniquely associated with BD among both males (χ2=17.1, df=1, p<0.001) and females (χ2=7.5, df=1, p=0.006). Youth-onset generalized anxiety disorders was also a significant predictor of BD among males (χ2=12.2, df=1, p<0.001) and females (χ2=6.9, df=1, p=0.009). Among males, the adjusted odds ratios for social phobia, panic disorder, and generalized anxiety disorder were 3.1 (95% CI = 2.3-4.2), 3.9 (95% CI = 2.1-7.5), and 3.3 (95% CI = 1.7-6.3) respectively. Among females, the adjusted odds ratios for social phobia, panic disorder, and generalized anxiety disorder were 2.6 (95% CI = 2.1-3.3), 2.1 (95% CI = 1.2-3.5), and 1.9 (95% CI = 1.2-3.0) respectively.
The third question addressed in this study is whether factors including family history of depression and alcoholism, and personal history of conduct disorder and SUD during youth, are associated with significantly increased prevalence of BD among adults with youth-onset primary anxiety disorders. Table 3 presents the relative prevalence of BD for youth-onset anxiety subjects with and without these factors. Males with conduct disorder, loaded family history of depression, and loaded family history of alcoholism had significantly greater prevalence of BD as compared to males without these predictors. In contrast, SUD was not significantly associated with the prevalence of BD. Each of these four predictor variables was associated with significantly increased prevalence of BD among females. Logistic regression analyses examined the unique contribution of each of the four predictor variables to variance in BD among subjects with youth-onset anxiety disorders. Significant predictors of BD among males with youth-onset anxiety disorders included conduct disorder (χ2=20.0, df=1, p<0.001) and loaded family history of depression (χ2=12.5, df=1, p<0.001), whereas SUD (χ2=1.1, df=1, p=0.29) and loaded family history of alcoholism (χ2=1.6, df=1, p=0.21) were not significantly associated with BD. The odds ratio for conduct disorder was 3.4 (95% CI=2.0-5.7) and for loaded family history of depression was 2.5 (95% CI = 1.5-4.2). Significant predictors of BD among females with youth-onset anxiety disorders included conduct disorder (χ2=9.6, df=1, p=0.002) and loaded family history of alcoholism (χ2=6.1, df=1, p=0.014), whereas SUD (χ2=0.4, df=1, p=0.51) and loaded family history of depression (χ2=1.8, df=1, p=0.18) were not significantly associated with BD. The odds ratio for conduct disorder was 2.4 (95% CI =1.4-4.2) and for loaded family history of alcoholism was 1.7 (95% CI = 1.1-2.6).
Table 3.
Factors Associated with Lifetime Bipolar I Disorder among Adult Males and Females with Primary Youth-Onset Anxiety Disorders
| Subjects with Lifetime Bipolar I Disorder, N (%) | ||||||
|---|---|---|---|---|---|---|
| Predictor Variable Present | Predictor Variable Absent | |||||
| N | % | N | % | χ2 | Odds Ratio (95% CI1) | |
| Males (N=572): | ||||||
| Conduct Disorder | 38/112 | 33.9 | 53/460 | 11.5 | 33.8*** | 2.9 (1.8-4.7) |
| Substance Abuse/Dependence | 72/449 | 16.0 | 19/123 | 15.4 | 0.0 | 1.0 (0.6-1.8) |
| Loaded Family History Alcohol | 23/84 | 27.4 | 68/488 | 13.9 | 9.7** | 2.0 (1.2-3.3) |
| Loaded Family History Depression | 37/123 | 30.1 | 54/449 | 12.0 | 23.5*** | 2.5 (1.6-4.0) |
| Females (N=999): | ||||||
| Conduct Disorder | 23/77 | 29.9 | 115/922 | 12.5 | 18.1*** | 2.4 (1.4-4.0) |
| Substance Abuse/Dependence | 24/122 | 19.7 | 114/877 | 13.0 | 4.0* | 1.5 (0.9-2.4) |
| Loaded Family History Alcohol | 43/198 | 21.7 | 95/801 | 11.9 | 13.0*** | 1.8 (1.2-2.7) |
| Loaded Family History Depression | 53/283 | 18.7 | 85/716 | 11.9 | 8.0** | 1.6 (1.1-2.3) |
CI=confidence interval
p<0.05
p<0.01
p<0.001
Exploratory analyses were conducted to examine whether youth-onset anxiety disorders confer a greater risk of later BD as compared to adult anxiety disorders (Figure 1). Among all subjects with primary anxiety disorders, those with any youth-onset anxiety disorders had significantly greater prevalence of BD as compared to those with solely adult-onset anxiety disorders (14.6% vs 8.2%; χ2=38.5, df=1, p<0.001). However, the results were not uniform across different anxiety disorders. Among subjects with social phobia, the prevalence of BD was not significantly different among those with youth onset (13.9%) as compared to adult onset (11.0%; χ2=2.0, df=1, p=0.16). In contrast youth-onset panic disorder was associated with significantly greater prevalence of BD as compared to adult-onset panic disorder (20.0% vs 6.7%; χ2=36.5, df=1, p<0.001). Youth-onset generalized anxiety disorder was also associated with significantly greater prevalence of BD as compared to adult-onset generalized anxiety disorder (26.4% vs 10.7%; 11%; χ2=31.8, df=1, p<0.001).
Figure 1.
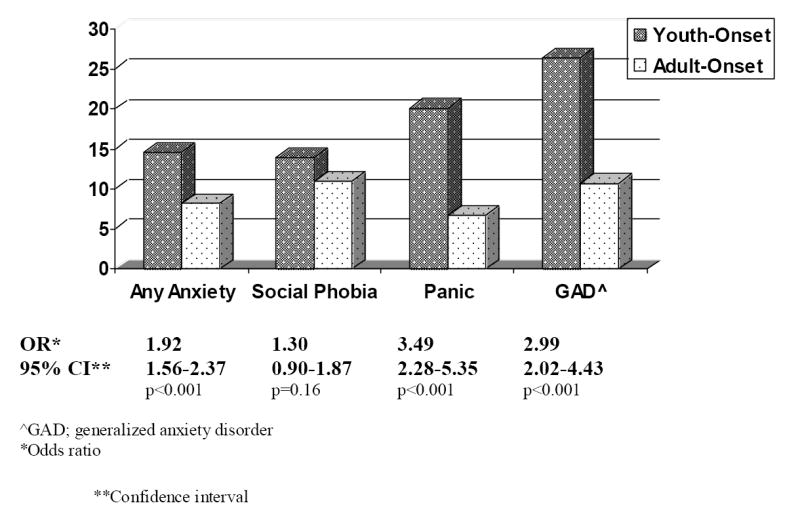
Prevalence of Bipolar I Disorder among Adults with Youth- vs Adult-Onset Primary Anxiety Disorders
DISCUSSION
The central finding of this study is that the prevalence of BD among adults, both males and females, who report primary youth-onset social phobia, panic disorder, or generalized anxiety disorder is markedly and significantly greater as compared to adults without a history of these disorders. Moreover, the presence of primary youth-onset anxiety disorders remains significantly associated with later BD after controlling for important factors including major depression that onset subsequent to the anxiety disorder. These findings are derived from a large representative sample of adults, and pertain to DSM-IV BD, whether characterized by euphoric mania, irritable mania, or both. Previous data from the National Comorbidity Survey similarly demonstrated increased prevalence of BD among adults with antecedent anxiety disorders (Kessler et al, 1997). However, mania that was exclusively irritable was not counted towards a diagnosis of BD in that study. In addition, the potential confounding effect of major depression was not considered. Therefore, present findings replicate those from an earlier epidemiologic survey, extend these findings to the full spectrum of bipolar I disorder, and confirm that the association between antecedent anxiety disorders and later BD cannot be explained by major depression interceding anxiety and mania.
This study also sought to examine whether different anxiety disorders confer different risk of BD. Initial cross-tabulation analyses suggested that generalized anxiety disorder is most strongly associated with later BD, with odds ratios of 17.4 and 8.7 among males and females respectively. However, logistic regression analyses failed to confirm that generalized anxiety disorder is most strongly associated with later BD. After controlling for age, interceding major depression, and the presence of other primary anxiety disorders, the adjusted odds ratios for BD ranged narrowly among both males (3.1-3.9) and females (1.9-2.6).
Exploratory analyses that sought to examine whether the risk of BD conferred by antecedent anxiety disorders differed on the basis of anxiety age-of-onset showed that the prevalence of BD among subjects with primary youth-onset social phobia was not significantly different from the prevalence of BD among subjects with primary adult-onset social phobia. However, subjects with primary youth-onset panic disorder and generalized anxiety disorder had significantly greater prevalence of BD as compared to subjects with adult-onset of these conditions. Therefore, results of the present study suggest that primary panic disorder and primary generalized anxiety disorder among youth may be particularly powerful harbingers of later BD.
Finally, this study attempted to identify factors that confer increased risk of BD among subjects with youth-onset primary anxiety disorders. Conduct disorder was a significant predictor of BD among both males and females. Approximately one in three subjects with youth-onset primary anxiety disorders and conduct disorder met criteria for BD in adulthood. In contrast, the presence of youth-onset SUD was not significantly associated with BD among either males or females. Finally, loaded family history of depression, but not of alcoholism, was significantly associated with BD among males, and loaded family history of alcoholism, but not of depression, was significantly associated with BD among females.
The risk of BD conferred by conduct disorder could be expected from the results of previous studies. Kessler and colleagues (1997) found that conduct disorder was one of only 4 significant predictors of BD, the other 3 of which were anxiety disorders. Similarly, a British birth-cohort study found that conduct disorder was associated with an odds ratio for later BD (2.5) which approached that of major depression (3.3)(Kim-Cohen et al, 2003). However, neither of these studies examined the contribution of conduct disorder to the risk for BD among subjects with anxiety disorders specifically. Present findings suggest that co-occurring youth-onset anxiety disorders and conduct disorder are associated with exceedingly high prevalence of BD in adulthood.
The hypothesis that SUD would be a significant predictor of BD among adults with youth-onset anxiety disorders was not supported. There is previous evidence that antecedent SUD are not generally associated with increased risk of BD. Data from the National Comorbidity Survey indicate that among all types of substance use, only cocaine use and stimulant abuse/dependence are significant predictors of later BD (Kessler et al, 1997). Although it was anticipated that the risk for BD conferred by SUD would be significant when examining solely subjects with youth-onset anxiety disorders, this was not confirmed.
Multiple logistic regression analyses showed that whereas loaded family history of depression was a significant predictor of BD among males, loaded family history of alcoholism was a significant predictor of BD among females. This despite the fact that among subjects with BD, there were no significant differences between males and females in terms of loaded family history of depression or alcoholism (results not shown). There are no previous studies that address gender differences in the contribution of familial alcoholism or depression to the prevalence of BD among probands with primary anxiety disorders. The literature regarding such gender differences among subjects with mood disorders in general is inconclusive. Dawson and Grant (1998) reported that loaded family history of alcoholism (defined as 50% of relatives affected) confers a greater risk of major depression for males as compared to females. Others have reported an increased prevalence of alcoholism among male relatives of women with mood disorders, and increased prevalence of mood disorders among female relatives of male alcoholics (Liskow et al, 1982; Winokur et al, 1970). In contrast, Weissman and colleagues (1984) found that proband gender does not affect rates of mood disorders among relatives of probands with BD and major depression. Future studies are need to clarify whether there are gender differences in the contribution of familial alcoholism and depression to variability in BD in general and among subjects with primary anxiety disorders specifically.
Several limitations of this study must be considered. The primary limitation of this study is its reliance on lay interviewer-administered structured interviews to determine diagnoses. Another limitation is that ages of onset of the disorders examined herein were ascertained retrospectively and as such are subject to recall bias. Adults who experienced more severe anxiety disorders as youth may be more likely to recall these disorders, which may in turn impact present findings and limit the degree to which the results generalize to all youth-onset anxiety disorders. One of the strengths of this study is the examination of multiple specific anxiety disorders. However, the 2001-2002 NESARC, from which this study is derived, does not yield diagnoses for obsessive-compulsive disorder, post-traumatic stress disorder, or separation anxiety disorder, and this limited the detail in which this study could examine the association between anxiety disorders and BD. This study examined bipolar I disorder specifically, and present findings may not generalize to bipolar II disorder or bipolar disorder not otherwise specified. Finally, this study was limited by the number of predictors of BD that could be examined. For example, data regarding family history of BD was not available. This study examined family history of depression and alcoholism, however specific details regarding diagnosis (e.g., major depression vs dysthymia, alcohol abuse versus dependence) were not available. Information regarding potentially mania-inducing serotonergic or noradrenergic medication was also not ascertained.
Despite these limitations, present findings confirm and extend those of previous studies. Primary youth-onset anxiety disorders are associated with significantly increased prevalence of BD among adults, and this is especially true when comorbid conduct disorder is present. Future studies employing prospective longitudinal methodology are needed in order to further elaborate on present findings: to provide estimates of the risk of later BD among youth initially presenting with anxiety disorders, and to identify variables that confer added risk of BD among youth with anxiety disorders. To date there are no reliable markers of latent BD diathesis, whether genotypic or endophenotypic, and therefore clinical variables and family history are the mainstay of risk estimation. Relying exclusively on family history of BD is problematic because the majority of people with BD do not have a family history of BD (Rice et al, 1987; Joyce et al, 2004). Therefore, identification of psychiatric predictors of BD is of paramount importance for the development of interventions aimed at preventing BD among those at high risk, and for more accurate assessment of the risks and benefits of serotonergic and noradrenergic medications in this population. Studies of the offspring of parents with BD provide a platform from which to develop preventative strategies for averting BD in a genetically high-risk population. Similar studies are needed in order to guide efforts at averting BD among persons who are at high risk on the basis of early psychiatric manifestations such as anxiety disorders.
Acknowledgments
This research was supported by the Psychiatric Epidemiology Program, Department of Psychiatry, University of Toronto (B.I. Goldstein).
The NESARC is supported by the National Institute on Alcohol Abuse and Alcoholism, Bethesda, Md, with supplemental support from the National Institute on Drug Abuse, Bethesda. The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of the sponsoring organizations.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Akiskal HS, Maser JD, Zller PJ, Endicott J, Coryell W, Keller M, Warshaw M, Clayton P, Goodwin F. Switching from ‘unipolar’ to bipolar II: an 11-year prospective study of clinical and temperamental predictors in 559 patients. Arch Gen Psychiatry. 1995;52:114–123. doi: 10.1001/archpsyc.1995.03950140032004. [DOI] [PubMed] [Google Scholar]
- Baldassano CF, Marangell LB, Gyulai L, Ghaemi SN, Joffe H, Kim DR, Sagduyu K, Truman CJ, Wisniewski SR, Sachs GS, Cohen LS. Gender differences in bipolar disorder: retrospective data from the first 500 STEP-BD participants. Bipolar Disord. 2005;7:465–470. doi: 10.1111/j.1399-5618.2005.00237.x. [DOI] [PubMed] [Google Scholar]
- Bernstein GA, Shaw K. Practice parameters for the assessment and treatment of children and adolescents with anxiety disorders. J Am Acad Child Psychiatry. 1997;36:69S–84S. doi: 10.1097/00004583-199710001-00006. [DOI] [PubMed] [Google Scholar]
- Biederman J, Faraone SV, Chu MP, Wozniak J. Further evidence of a bidirectional overlap between mania and conduct disorder in children. J Am Acad Child Psychiatry. 1999;38:468–476. doi: 10.1097/00004583-199904000-00021. [DOI] [PubMed] [Google Scholar]
- Birmaher B, Kennah A, Brent D, Ehmann M, Bridge J, Axelson D. Is bipolar disorder specifically associated with panic disorder in youths? J Clin Psychiatry. 2002;63:414–419. doi: 10.4088/jcp.v63n0507. [DOI] [PubMed] [Google Scholar]
- Boylan KR, Bieling PJ, Marriott M, Begin H, Young LT, MacQueen GM. Impact of comorbid anxiety disorders on outcome in a cohort of patients with bipolar disorder. J Clin Psychiatry. 2004;65:1106–1113. doi: 10.4088/jcp.v65n0813. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF. Family history of alcoholism and gender: their combined effects on DSM-IV alcohol dependence and major depression. J Stud Alcohol. 1998;59:97–106. doi: 10.15288/jsa.1998.59.97. [DOI] [PubMed] [Google Scholar]
- DelBello MP, Carlson GA, Tohen M, Bromet EJ, Schwiers M, Strakowski SM. Rates and predictors of developing a manic or hypomanic episode 1 to 2 years following a first hospitalization for major depression with psychotic features. J Child Adolesc Psychopharmacol. 2003;13:173–185. doi: 10.1089/104454603322163899. [DOI] [PubMed] [Google Scholar]
- Dickstein DP, Rich BA, Binstock AB, Pradella AG, Towbin KE, Pine DS, Leibenluft E. Comorbid anxiety in phenotypes of pediatric bipolar disorder. J Child Adolesc Psychopharmacol. 2005;4:534–548. doi: 10.1089/cap.2005.15.534. [DOI] [PubMed] [Google Scholar]
- Dilsaver SC, Chen YW. Social phobia, panic disorder, and suicidality in subjects with pure and depressive mania. J Affect Disord. 2003;77:173–177. doi: 10.1016/s0165-0327(02)00114-3. [DOI] [PubMed] [Google Scholar]
- Dilsaver SC, White K. Affective disorders and associated psychopathology: a family history study. J Clin Psychiatry. 1986;47:2162–2169. [PubMed] [Google Scholar]
- Feske U, Frank E, Mallinger AG, Houck PR, Fagiolini A, Shear MK, Grochocinski VJ, Kupfer DJ. Anxiety as a correlate of response to the acute treatment of bipolar I disorder. Am J Psychiatry. 2000;157:956–962. doi: 10.1176/appi.ajp.157.6.956. [DOI] [PubMed] [Google Scholar]
- Faedda GL, Baldessarini RJ, Golvinsky I, Austin NB. Treatment-emergent mania in pediatric bipolar disorder: a retrospective case review. J Affect Disord. 2004;82:149–158. doi: 10.1016/j.jad.2003.12.011. [DOI] [PubMed] [Google Scholar]
- Geller B, Zimerman B, Williams M, Bolhofner K, Craney JL. Bipolar disorder at prospective follow-up of adults who had prepubertal major depressive disorder. Am J Psychiatry. 2001;158:125–127. doi: 10.1176/appi.ajp.158.1.125. [DOI] [PubMed] [Google Scholar]
- Go FS, Malley EE, Birmaher B, Rosenberg DR. Manic behaviors associated with fluoxetine in three 12- to 18-year-olds with obsessive-compulsive disorder. J Child Adolesc Psychopharmacol. 1998;8:73–80. doi: 10.1089/cap.1998.8.73. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Hamilton SP. The early-onset fearful panic attack as a predictor of severe psychopathology. Psychiatry Res. 2002;109:71–79. doi: 10.1016/s0165-1781(01)00357-2. [DOI] [PubMed] [Google Scholar]
- Goodwin RD, Hoven CW. Bipolar-panic comorbidity in the general population: prevalence and associated morbidity. J Affect Disord. 2002;70:27–33. doi: 10.1016/s0165-0327(01)00398-6. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule –IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Huang B. Co-occurrence of 12-month mood and anxiety disorders and personality disorders in the US: results from the national epidemiologic survey on alcohol and related conditions. J Psychiatr Res. 2005;39:1–9. doi: 10.1016/j.jpsychires.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou P, Dufour MC, Compton W, Pickering RP, Kaplan K. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004a;61:807–816. doi: 10.1001/archpsyc.61.8.807. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004b;61:361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Hasin DS, Dawson DA, Chou SP, Ruan WJ, Huang B. Prevalence, correlates, and comorbidity of bipolar I disorder and axis I and II disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2005;66:1205–1215. doi: 10.4088/jcp.v66n1001. [DOI] [PubMed] [Google Scholar]
- Harpold TL, Wozniak J, Kwon A, Gilbert J, Wood J, Smith L, Biederman J. Examining the association between pediatric bipolar disorder and anxiety disorders in psychiatrically referred children and adolescents. J Affect Disord. 2005;88:19–26. doi: 10.1016/j.jad.2005.05.016. [DOI] [PubMed] [Google Scholar]
- Hendrik V, Altshuler LL, Gitlin MJ, Delrahim S, Hammen C. Gender and bipolar illness. J Clin Psychiatry. 2000;61:393–396. doi: 10.4088/jcp.v61n0514. [DOI] [PubMed] [Google Scholar]
- Johnson JG, Cohen P, Brook JS. Associations between bipolar disorder and other psychiatric disorders during adolescence and early adulthood: a community-based longitudinal investigation. Am J Psychiatry. 2000;157:1679–1681. doi: 10.1176/appi.ajp.157.10.1679. [DOI] [PubMed] [Google Scholar]
- Joyce PR, Doughty CJ, Wells JE, Walsh AES, Admiraal A, Lill M, Olds RJ. Affective disorders in the first-degree relatives of bipolar probands: results from the South Island Bipolar Study. Compr Psychiatry. 2004;45:168–174. doi: 10.1016/j.comppsych.2004.02.005. [DOI] [PubMed] [Google Scholar]
- Keller MB. Prevalence and impact of comorbid anxiety and bipolar disorder. J Clin Psychiatry. 2006;67(suppl 1):5–7. [PubMed] [Google Scholar]
- Kessler RC, Rubinow DR, Holmes C, Abelson JM, Zhao S. The epidemiology of DSM-III-R bipolar I disorder in a general population survey. Psychol Med. 1997;27:1079–1089. doi: 10.1017/s0033291797005333. [DOI] [PubMed] [Google Scholar]
- Kim-Cohen J, Caspi A, Moffitt TE, Harrington HL, Milne BJ, Poulton R. Prior juvenile diagnoses in adults with mental disorder. Arch Gen Psychiatry. 2003;60:709–717. doi: 10.1001/archpsyc.60.7.709. [DOI] [PubMed] [Google Scholar]
- Liskow B, Mayfield D, Thiele J. Alcohol and affective disorder: assessment and treatment. J Clin Psychiatry. 1982;43:144–147. [PubMed] [Google Scholar]
- Masi G, Toni C, Perugi G, Mucci M, Millepiedi S, Akiskal HS. Anxiety disorders in children and adolescents with bipolar disorder: a neglected comorbidity. Can J Psychiatry. 2001;46:797–802. doi: 10.1177/070674370104600902. [DOI] [PubMed] [Google Scholar]
- Otto MW, Simon NM, Wisniewski SR, Miklowitz DJ, Kogan JN, Reilly-Harrington NA, Frank E, Nierenberg AA, Marangell LB, Sagduyu K, Weiss RD, Miyahara S, Thase ME, Sachs GS, Pollack MH. Prospective 12-month course of bipolar disorder in out-patients with and without comorbid anxiety disorders. Br J Psychiatry. 2006;189:20–25. doi: 10.1192/bjp.bp.104.007773. for the STEP-BP Investigators. [DOI] [PubMed] [Google Scholar]
- Perugi G, Akiskal HS, Toni C, Simonini E, Gemignani A. The temporal relationship between anxiety disorders and (hypo)mania: a retrospective examination of 63 panic, social phobic and obsessive-compulsive patients with comorbid bipolar disorder. J Affect Disord. 2001;67:199–206. doi: 10.1016/s0165-0327(01)00433-5. [DOI] [PubMed] [Google Scholar]
- Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse: Results from the Epidemiologic Catchment Area (ECA) study. JAMA. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Rice J, Reich T, Andreasen NC, Endicott J, Van Eerdewegh M, Fishman R, Hirschfeld RM, Klerman GL. The familial transmission of bipolar illness. Arch Gen Psychiatry. 1987;44:441–447. doi: 10.1001/archpsyc.1987.01800170063009. [DOI] [PubMed] [Google Scholar]
- Strober M, Carlson G. Bipolar illness in adolescents with major depression: clinical, genetic, and psychopharmacologic predictors in a three- to four-year prospective follow-up investigation. Arch Gen Psychiatry. 1982;39:549–555. doi: 10.1001/archpsyc.1982.04290050029007. [DOI] [PubMed] [Google Scholar]
- Varley CK, Smith CJ. Anxiety disorders in the child and teen. Pediatr Clin North Am. 2003;50:1107–1138. doi: 10.1016/s0031-3955(03)00070-1. [DOI] [PubMed] [Google Scholar]
- Wagner KD. Bipolar disorder and comorbid anxiety disorders in children and adolescents. J Clin Psychiatry. 2006;67(suppl1):16–20. [PubMed] [Google Scholar]
- Weissman MM, Gershon ES, Kidd KK, Prusoff BA, Leckman JF, Dibble E, Hamovit J, Thompson WD, Pauls DL, Guroff JJ. Psychiatric disorders in the relatives of probands with affective disorders. Arch Gen Psychiatry. 1984;41:13–21. doi: 10.1001/archpsyc.1984.01790120015003. [DOI] [PubMed] [Google Scholar]
- Weissman MM, Wickramaratne P, Nomura Y, Warner V, Pilowsky D, Verdeli H. Offspring of depressed parents: 20 years later. Am J Psychiatry. 2006;163:1001–1008. doi: 10.1176/ajp.2006.163.6.1001. [DOI] [PubMed] [Google Scholar]
- Winokur G, Coryell W, Endicott J, Keller M, Akiskal H, Solomon D. Familial alcoholism in manic-depressive (bipolar) disease. Am J Med Genet. 1996;67:197–201. doi: 10.1002/(SICI)1096-8628(19960409)67:2<197::AID-AJMG10>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- Winokur G, Reich T, Rimmer J, Pitts FN., Jr Alcoholism, III: diagnosis and familial psychiatric illness in 259 alcoholic probands. Arch Gen Psychiatry. 1970;23:104–111. doi: 10.1001/archpsyc.1970.01750020008002. [DOI] [PubMed] [Google Scholar]


