Abstract
Aim of the study
This pilot study was designed to examine the relationships among spirituality and psychosocial factors in a sample of 52 adult males living with human immunodeficiency virus (HIV) disease and to determine the most reliable spirituality measure for a proposed longitudinal study.
Background
HIV disease is among the most devastating of illnesses, having multiple and profound effects upon all aspects of the biopsychosocial and spiritual being. Although research has suggested relationships among various psychosocial and spiritual factors, symptomatology and physical health, much more research is needed to document their potential influences on immune function, as well as health status, disease progression, and quality of life among persons with HIV disease.
Methods
This descriptive correlational study explored the relationships of spirituality and psychosocial measures. Spirituality was measured in terms of spiritual perspective, well-being and health using three tools: the Spiritual Perspective Scale, the Spiritual Well-Being Scale, and the Spiritual Health Inventory. Five psychosocial instruments were used to measure aspects of stress and coping: the Mishel Uncertainty in Illness Scale, Dealing with Illness Scale, Social Provisions Scale, Impact of Events Scale, and Functional Assessment of HIV Infection Scale. The sample was recruited as part of an ongoing funded study. The procedures from the larger study were well-defined and followed in this pilot study. Correlational analyses were done to determine the relationship between spirituality and the psychosocial measures.
Findings
The findings indicate that spirituality as measured by the existential well-being (EWB) subscale of the Spiritual Well-Being Scale was positively related to quality of life, social support, effective coping strategies and negatively related to perceived stress, uncertainty, psychological distress and emotional-focused coping. The other spirituality measures had less significant or non significant relationships with the psychological measures.
Conclusions
The study findings support the inclusion of spirituality as a variable for consideration when examining the psychosocial factors and the quality of life of persons living with HIV disease. The spiritual measure that best captures these relationships is the EWB subscale of the Spiritual Well-Being Scale.
Keywords: spirituality, HIV disease, spiritual perspective, health, well-being, psychosocial measures, stress, quality of life, uncertainty, coping
Introduction
Recent advances in treatment modalities have made human immunodeficiency virus (HIV) infection more treatable as a chronic illness. HIV disease is a condition accompanied by multiple stressors which include the management of treatment regimens that have become increasingly complex, while long-term benefit of pharmacotherapies remains a source of uncertainty. Disease management often requires significant lifestyle modifications and adaptation of daily activities to the demands of prescribed treatment regimens. In addition to stressful disease-management issues, persons living with HIV experience ongoing psychosocial stressors, both interpersonal and intrapersonal, associated with diagnosis of a life-threatening chronic illness. These multiple, severe, and unrelenting stressors profoundly affect the individual’s quality of life and tax existing coping resources (McCain & Cella 1995, Wilson et al. 1997, Robinson et al. 1999).
Assisting individuals who are living with HIV requires attention to the whole person. Holism involves understanding the relationships among biological, psychological, social and spiritual dimensions of individuals (Dossey & Dossey 1998). HIV infection is a disease that impacts the well-being of individuals through all of these dimensions. The purpose of this research was to explore the relationships of spirituality, psychological and social factors in persons living with HIV.
Review of literature
In a growing body of literature, immunosuppression is increasingly being assocsiated with psychosocial stress, suggesting that the trajectory of HIV disease may be influenced by the degree of stress individuals experience (McCain & Zeller 1996, Cole & Kemeny 1997). Research related to stress and HIV has been approached in a variety of ways. Perceived stress has been directly linked with increased depression and psychological distress in numerous studies with the HIV population (Folkman et al. 1993, McCain & Cella 1995, McCain et al. 1996). Psychological distress has been shown to be directly related to HIV symptomatology (Hayes et al. 1992, Perry et al. 1992, Linn et al. 1993). Further, psychological distress and perceived loss of control have been related to immunosuppression (Antoni et al. 1991, Herbert & Cohen 1993).
Studies related to spirituality and HIV disease reflect four broad research foci: making meaning, coping, centrality to illness and wellness. Most studies are descriptive or exploratory in design, with few intervention studies reported. From a study using an 8-week stress reduction intervention, Astin (1997) reported decreased physical and psychological symptoms and increased sense of self-control and spiritual awareness among participants. In a qualitative study of 34 women living with HIV, Dunbar et al. (1998) reported that the women sought ways to use their experience of HIV disease as a vehicle for psychological and spiritual growth. Of 117 African-American men and women living with HIV disease, Coleman and Holzemer (1999) found that existential well-being, a spiritual indicator of purpose and meaning, was significantly related to participants’ psychological well-being.
The central role of spirituality in chronic illnesses has been examined in several studies. Investigators examining cultural differences and the contributing etiological factors for HIV and other chronic diseases have reported that individuals often attribute their illness to spiritual distress and beliefs (Stolley & Koenig 1997, Marbella et al. 1998). In studies in which spirituality was not a major study variable, findings nevertheless indicated its centrality to the illness and the need to offer complementary therapies addressing spirituality (Fryback & Reinert 1997). When spiritual interventions were not offered, patients sought spiritual assistance in their cultural communities. Fryback and Reinert (1999) later found spirituality to be an essential contributor to feelings of health and well-being, with spirituality being viewed as a bridge between hopelessness and meaningfulness in the lives of 15 study participants with cancer or HIV/acquired immunodeficiency syndrome (AIDS).
Nurses have taken a central role in exploring the relationship between spirituality and wellness in HIV and other chronic diseases. Several nurse investigators have reported the positive effects of spirituality on HIV disease outcomes and various dimensions of well-being. Hall (1998) explored the role of spirituality in dealing with advanced HIV disease, concluding that after suffering, spirituality frames one’s life. Peri (1995) discussed numerous ways that nurses could intervene to promote spirituality in persons with AIDS, thereby improving their well-being. Nokes et al. (1995) found that 100% of a convenience sample of 145 persons with HIV disease used some form of complementary therapy that included a spiritual component. Patients reported that spiritual practices provided relief from symptoms and, in some instances, changed the illness outcome. In a study of 100 persons with HIV or AIDS, Carson and Green (1992) found that those who were spiritually well and who were able to find meaning and purpose in their lives were also hardier. Lamendola and Newman (1994) reported positive relationships between spirituality, social support and coping responses. Kendall (1994) described the core process of wellness spirituality in her grounded theory as being essential to the health and well-being of 29 HIV-infected men. The domain of spirituality is included in nursing models of quality of life in chronic disease (Ferrell et al. 1995, Ferrans 1996).
HIV disease is among the most devastating of illnesses, having multiple and profound effects upon all aspects of the biopsychosocial and spiritual being. Although research has suggested relationships among various psychosocial and spiritual factors, symptomatology and physical health, much more research is needed to document their potential influences on immune function, as well as health status, disease progression, and quality of life among persons with HIV disease (McCain & Zeller 1996).
Framework
The theoretical framework for this research integrates the cognitive-transactional model of stress within the psychoneuroimmunology (PNI) paradigm used in studies with persons living with HIV disease (McCain & Smith 1994, Zeller et al. 1996). In the cognitive-transactional model, perceived stress, psychosocial functioning, quality of life and somatic health are psychologically mediated by coping strategies and resources (Billings & Moos 1984, Lazarus & Folkman 1984). In the revised version of the PNI model as proposed by the current work of McCain et al., critical psychosocial concepts include: (a) the stressors of illness-related uncertainty and perceived psychological stress associated with living with HIV disease; (b) the psychosocial mediator of coping strategies; (c) the stress process moderators of social support and spirituality and (d) the adaptational outcomes of illness-related psychological distress and quality of life.
Purpose
Our findings reported here were obtained as baseline data in a pilot study exploring spirituality within an ongoing project that examined the relationship of stress and PNI processes in persons living with HIV. Recognizing the accepted view of social and psychological factors in supporting immune function, and the anticipated similar effect of spirituality, the primary aim of the pilot study was to examine the relationships among spirituality and the psychosocial variables included in the PNI framework. An additional goal was to determine which of three spirituality measures would most effectively reflect these relationships. It was hypothesized that spirituality measures would be: (a) positively related to quality of life and social support and (b) inversely related to illness-related psychological distress and perceived stress.
Methods
The data reported in this article to demonstrate the relationships of spirituality and psychosocial variables were baseline data collected for a spirituality intervention pilot study using a quasi-experimental time series design. Data collection occurred at three intervals: on admission to the study as baseline data, after completion of an 8-week spiritual intervention and at a 6-month follow-up appointment.
After receiving approval by our Institutional Review Board, a convenience sample of 52 adult males who were living with HIV disease were recruited by advertising in two local newspapers, through flyers posted at clinic sites within the community and at a large urban medical centre, and at local churches and organizations known to have contact with individuals living with HIV. Criteria for participation were that participants be at least 18 years of age, able to read and speak English, aware of the diagnosis of HIV disease, and deemed to be physically capable of attending the intervention and completing the 6-month follow-up requirement (as evidenced by a Karnofsky Performance score of at least 60). Exclusion criteria included: (a) significant psychiatric illnesses, (b) cognitive impairment, (c) severe protein-calorie malnutrition and (d) taking steroids or immunomodulatory drugs (other than antiretroviral medications). Screening for these exclusions was part of the admission process for the ongoing PNI study. The sample size is deemed adequate to meet the objectives of this pilot study.
Demographic data (age, race and marital status) were obtained from the participants after research consent forms were signed. Upon enrolment, three spirituality measures were administered, in addition to five psychosocial questionnaires. The tools were administered to participants in conference rooms in the clinical laboratory of a large medical centre where many of the participants receive treatment for their HIV disease. The tools were completed by the participants in approximately 30 minutes. Specimens were also collected to measure immune function but are not reported with these data. The data collection process and the facilities used in this pilot are those used to test the full PNI model in the larger-funded project.
Validity and reliability data are reported for the eight psychosocial and spiritual measures administered to participants in this study (see Table 1). Spirituality was measured in terms of spiritual perspective, well-being, and health, using three tools: The spiritual perspective scale (SpS), the spiritual well-being scale (SWBS), and the spiritual health inventory (SHI). The SpS is a 10-item, Likert type scale developed to measure the significance of spirituality in one’s life and the extent to which one engages in spiritually related interactions. The SpS is scored by calculating the arithmetic mean. Total scores range from 1·0 to 6·0.
Table 1.
Selected psychometric data for instruments
| Instrument | References | Validity | Reliability |
|---|---|---|---|
| SpS | Reed(1986, 1987) | Criterion-related validity and discriminate validity have been demonstrated | α = 0·90, current α = 0·92 |
| SWBS |
Paloutzian and Ellison (1982)
Broten (1991) Carson and Green (1992) |
SWB factored into RWB and EWB; face validity suggested by examination of item content; SWB scores correlated in predictable ways with other scales | Test-retest reliability coefficients: 0·93(SWB)
0·96 (RWB) 0·86 (EWB) α = 0·89 (SWB), current α = 0·88 α = 0·87 (RWB), current α = 0·88 α = 0·78 (EWB), current α = 0·75 |
| SHI | Highfield (1992) | Content and construct validity based on literature review, expert panel, and factor analysis | α = 0·77, current α = 0·87 |
| MUIS |
McCain and Cella (1995)
McCain et al. (1996) |
Predictive and discriminant validity supported by correlations with stress levels and mood disturbance | α = 0·83, current α = 0·87 |
| DIS |
Cella et al. (1996)
McCain and Cella (1995) McCain et al. (1996) McCain et al. (1998) Peterman et al. (1997) |
Predictive and discriminant validity supported by correlations with quality of life, mood disturbance and uncertainty | Stress: α = 0·83, current α = 0·85
Coping: α = 0·80−0·87, current α = 0·77−0·86 |
| SPS | Kelly et al. (1993) | Trends (NS) for increased SPS after interventions | Not reported, current α = 0·90 |
| IES |
Antoni et al. (1991)
Ironson et al. (1990) Perry et al. (1992) McCain et al. (1996) |
Increased IES after HIV and diagnosis; increased IES related to increased HIV symptoms; decreased IES after intervention | Not reported
Not reported α = 0·85−0·86, current α = 0·92 |
| FAHI |
Cella et al. (1996)
Peterman et al. (1997) McCain et al. (1996) |
FAHI sensitive to stage of illness; increased emotional dimension after intervention | α = 0·85−0·86
α = 0·92 α = 0·91, current α = 0·92 |
The SWBS is a 20-item Likert type scale consisting of 11 positively worded items and nine negatively worded items. It was developed by Paloutzian and Ellison (1982) as a general measure of spiritual well-being. Possible scores range from 20 to 120. Subscale scores are derived for religious well-being and existential well-being, with higher scores indicating greater well-being. The scale has been used with persons with HIV disease as a predictor of hardiness (Carson & Green 1992).
The SHI was developed by Highfield (1992) and has been used primarily to study patients with cancer. The patient’s version of the instrument is a self-report of spiritual health that includes positive and negative expressions. The 31-item Likert type scale measures three factors: self-acceptance, relationships and hope. Total scores range from 31 to 155.
The five psychosocial instruments used to measure aspects of the stress process were the Mishel uncertainty in illness scale (MUIS), dealing with illness scale (DIS), social provisions scale (SPS), impact of events scale (IES), and functional assessment of HIV infection scale (FAHI) (see Table 1). The MUIS is a well-validated, reliable measure of uncertainty associated with illness (Mishel 1984). Higher scores on this 33-item scale indicate higher uncertainty in the areas of symptomatology, diagnosis, treatment, relationships with caregivers and prognosis (Mishel & Epstein 1990). The MUIS has been shown to be reliable in research with individuals living with HIV (McCain & Cella 1995, McCain et al. 1996).
The DIS, comprised of stress and coping subscales, was used to assess stress levels and coping patterns (McCain & Gramling 1992). The format for the stress subscale taps the process of cognitive appraisal by enabling respondents to indicate the level of desirability as well as the personal impact of events. Positive and negative stress subscale scores are derived by separately summing the items indicated as having a positive or negative personal impact. Scoring schemes for the coping subscale enable assessment of both the theoretical foci of coping and the factor-analytically derived coping methods of maintaining a positive attitude, adapting to illness and withholding. Items are approximately equally distributed across the theoretical dimensions of problem-focused, emotion-focused, and appraisal-focused coping. Higher scores reflect more frequent use of the various coping strategies. Previous studies have supported the validity and reliability of the DIS for the study population (McCain & Cella 1995, Cella et al. 1996, McCain et al. 1996).
Social support was measured using the revised 24-item SPS, a measure of six social provisions or components of social support. The SPS has demonstrated excellent construct validity and internal consistency in other populations (Cutrona & Russell 1987), but use with the HIV population has been limited.
The IES is a 15-item instrument which was used to measure the subjective impact of living with HIV disease. Using the IES, psychological distress specific to living with HIV disease has been previously documented in the form of avoidant and/or instrusive thoughts related to the illness (Ironson et al. 1990, Perry et al. 1992, McCain & Cella 1995, McCain et al. 1996). Higher scores on the subscales of intrusive and avoidance thinking indicate higher psychological distress.
The FAHI scale is a disease-specific extension of the general version of the functional assessment of cancer therapy (FACT-G) scale (Cella et al. 1993), measuring the quality of life in people with HIV infection. The 55-item revised FAHI (version 3) includes subscales of physical, social/family, emotional and functional well-being; relationship with physician; and additional concerns specific to HIV infection. Higher scores indicate greater quality of life. The FAHI has demonstrated excellent psychometric performance, including sensitivity to stage of illness and to intervention in previous studies (Cella et al. 1996, McCain et al. 1996).
The data were analysed using correlations. The use of numerous bivariate correlations in this pilot study presents a threat of Type I error. For a conservative estimate of meaningful magnitude, a power analysis for n = 50, power = 0·80, and α = 0·07 yields a moderately high effect size 0·70 (Lipsey 1990). An effect size 0·70 equates with a sample correlation 0·36 (Cohen 1988). Thus, only those correlations 0·40 and greater and significant at P ≤ 0·01 were considered clinically meaningful. With future studies and larger sample size, variable intercorrelations need to be examined using structural equation modelling or other multivariate approaches.
Findings
In this pilot, the sample of 52 males were a mean age of 39 years, 61% African-American, and 55% single. Moderately high spirituality scores were reported (SpS mean=5·08, SD=0·84, range=1·9–6; SWBS mean=91, SD=16·2, range 42–117; SHI mean=113, SD=14·2, range 79–147). As expected, there were high intercorrelations among the three spiritual measures. Most notably, the SWBS total score was moderately highly correlated with the SHI (r=0·70) and the SpS (r=0·72), while the SpS and SHI were more modestly related (r=0·43). The SpS was highly correlated with the religious well-being (RWB) subscale of the SWBS (r=0·80) and moderately correlated with the existential well-being (EWB) subscale (r=0·41).
Correlational analyses were used to examine the nature of relationships among spirituality and the psychosocial factors of perceived stress, uncertainty, psychological distress, social support, coping strategies and quality of life. Predicted significant relationships as proposed in the ‘Framework’ were found among the psychosocial variables (see Figure 1). For instance, quality of life was positively related to social support; physical, social and functional well-being; and appraisal-focused coping, while negatively related to uncertainty, perceived stress, psychological distress in the form of avoidant and intrusive thoughts, and emotion-focused coping. Social support was positively related to effective coping strategies (problem and appraisal-focused coping) and quality of life and negatively related to uncertainty. These findings were significant at P ≤ 0·01 and consistent with previous findings (McCain & Cella 1995, McCain et al. 1996).
Figure 1.
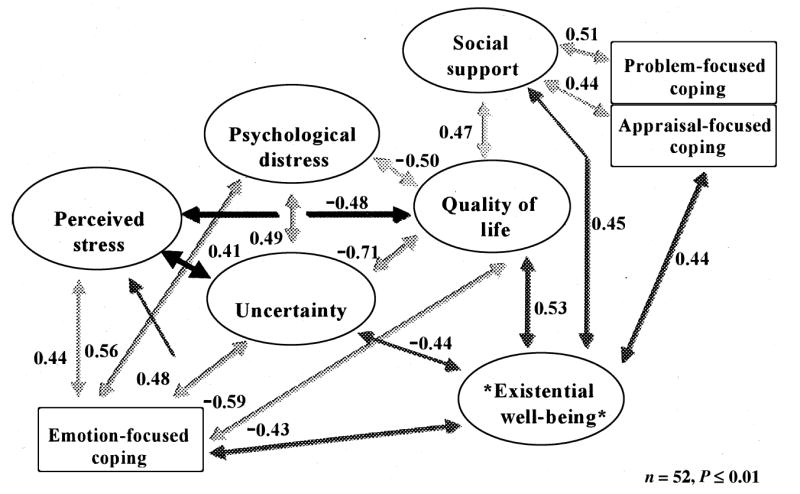
Statistical model of the relationships among psychosocial and spiritual variables.
Hypothesized relationships among spirituality and psychosocial measures were generally supported. The spirituality measures that demonstrated significant relationships with the study variables were the SHI and the EWB subscale of the SWBS (see Table 2). Of the spirituality measures, the EWB subscale demonstrated the strongest correlations with other study variables. There were strong negative relationships between the EWB, MUIS, and emotion-focused coping subscale of the DIS. Other relationships found and not specifically hypothesized were positive relationships with appraisal-focused coping and the emotional, social, physical and functional well-being subscales of the FAHI as well as the total quality of life scale. As illustrated in Figure 1, spirituality as indicated by the EWB subscale was positively related to quality of life (FAHI) and social support (SPS) (see Figure 1 for other significant relationships between EWB and the psychosocial variables).
Table 2.
Significantly correlated spiritual measures and psychosocial variables (r/P) (n = 52)
| SHI | EWB | |
|---|---|---|
| FAHI | ||
| Physical well-being | 0·24 | 0·41 |
| 0·08 | 0·002 | |
| Social well-being | 0·41 | 0·36 |
| 0·002 | 0·009 | |
| Emotional well-being | 0·55 | 0·46 |
| 0·0001 | 0·0005 | |
| Functional well-being | 0·55 | 0·52 |
| 0·0001 | 0·0001 | |
| Quality of life total | 0·52 | 0·53 |
| 0·0001 | 0·0001 | |
| DIS | ||
| Perceived stress | −0·33 | −0·35 |
| 0·01 | 0·01 | |
| SPS | ||
| Social support | 0·39 | 0·45 |
| 0·003 | 0·0007 | |
| MUIS | ||
| Uncertainty | −0·44 | −0·44 |
| 0·0012 | 0·0012 | |
| IES | ||
| Intrusive thinking | −0·45 | −0·40 |
| 0·0009 | 0·003 | |
| Psychological distress total | −0·41 | −0·36 |
| 0·002 | 0·001 | |
| DIS | ||
| Appraisal-focused coping | 0·59 | 0·44 |
| 0·0001 | 0·001 | |
| Problem-focused coping | 0·37 | 0·32 |
| 0·005 | 0·02 | |
| Emotion-focused coping | −0·65 | −0·43 |
| 0·001 | 0·009 | |
The EWB subscale of the SWBS accounted for most of these significant findings of this pilot study. While the SHI performed in a similar manner (see Table 2), the only highly significant relationships found for the RWB and SpS were with appraisal- and problem-focused coping.
Discussion
The results indicated that the three spirituality instruments behaved differently in the correlational analyses with the study variables. The moderately high intercorrelations between the SHI, SpS and SWBS were not consistently seen in the results and may indicate measures of different aspects of spirituality as a construct. The EWB subscale was highly correlated with the study variables and in the expected directions. The SHI performed similarly but not as strongly. The SpS and RWB demonstrated limited correlations with the psychosocial variables and may measure the presence of spirituality (a frequency measure) or religious beliefs.
Conclusions
The study findings support the inclusion of spirituality as a variable for consideration when examining the psychosocial factors and the quality of life of persons living with HIV disease. It is also noted that the spiritual measure that best captures these relationships is the EWB subscale of the SWBS. The SHI performs well as a spiritual measure as evidenced by the highly significant correlations, but because of its length (31 items) and the lack of significant correlation with physical well-being, it is viewed less positively as the instrument of choice.
Implications
Templeton (1995) in ‘The Humble Approach’ described the spiritual wandering of the first 40 years of life finally leading to spiritual growth and maturity. In this sample of 52 adult males (mean age of 39 years), there were reported moderately high scores of spirituality and higher levels of existential well-being and quality of life.
The integration of body, mind and spirit in healthy individuals leads to a balanced, healthy life. Among persons living with HIV, spirituality coupled in an integral manner with social and psychological well-being may lengthen life or enhance the quality of life. The centrality of spirituality within the PNI model was supported by this preliminary work. Further research is proposed to test these relationships in larger samples or different populations of patients. The authors recommend the use of the SWBS, specifically the EWB, as a measure of spirituality.
Acknowledgments
This study was funded as a pilot study by the A.D. Williams Foundation at Virginia Commonwealth University, as part of a larger study funded by the National Institute of Nursing Research, award #RO1 NR04395; Nancy L. McCain, DSN, Principal Investigator. The research was supported by the General Clinical Research Center of Virginia Commonwealth University/Medical College of Virginia Hospitals, award #MO1 RR00065 from the National Institutes of Health; John N. Clore, MD, Project Director.
Contributor Information
Inez Tuck, School of Nursing, Virginia Commonwealth University, Richmond, Virginia, USA.
Nancy L. McCain, School of Nursing, Virginia Commonwealth University, Richmond, Virginia, USA.
Ronald K. Elswick, Jr, Schools of Medicine and Nursing, Virginia Commonwealth University, Richmond, Virginia, USA.
References
- Antoni MH, Baggett L, Ironson G, LaPerriere A, August S, Klimes N, Schneiderman N, Fletcher MA. Cognitive-behavioral stress management intervention buffers distress responses and immunologic changes following notification of HIV-1 seropositivity. Journal of Counseling and Clinical Psychology. 1991;59:906–915. doi: 10.1037//0022-006x.59.6.906. [DOI] [PubMed] [Google Scholar]
- Astin JA. Stress reduction through mindfulness meditation: effects on psychological symptomatology, sense of control and spiritual experiences. Psychotherapy and Psychosomatics. 1997;66:97–106. doi: 10.1159/000289116. [DOI] [PubMed] [Google Scholar]
- Billings AG, Moos RH. Coping, stress, and social resources among adults with unipolar depression. Journal of Personality and Social Psychology. 1984;46:877–891. doi: 10.1037//0022-3514.46.4.877. [DOI] [PubMed] [Google Scholar]
- Broten PS. Spiritual Care given by Nurses and Spiritual Well-being of Terminally Ill Cancer Patients. Western Michigan University; Kalamazoo: 1991. Unpublished Doctoral Dissertation. [Google Scholar]
- Carson VB, Green H. Spiritual well being: a predictor of hardiness in patients with acquired immunodeficiency syndrome. Journal of Professional Nursing. 1992;8:209–220. doi: 10.1016/8755-7223(92)90082-a. [DOI] [PubMed] [Google Scholar]
- Cella DF, Tulsky DS, Gray G, Sarafian B, Linn E, Bonomi A, Silberman M, Yellen SB, Winicour P, Brannon J. The functional assessment of cancer therapy scale: development and validation of the general measure. Journal of Clinical Oncology. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- Cella DF, McCain NL, Peterman AH, Mo F, Wolen D. Development and validation of the functional assessment of human immunodeficiency virus infection (FAHI) quality of life instrument. Quality of Life Research. 1996;5:450–463. doi: 10.1007/BF00449920. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Cole SW, Kemeny ME. Psychobiology of HIV infection. Critical Reviews in Neurobiology. 1997;11:289–321. doi: 10.1615/critrevneurobiol.v11.i4.30. [DOI] [PubMed] [Google Scholar]
- Coleman CL, Holzemer WL. Spirituality, psychological well-being, and HIV symptoms for African Americans living with HIV disease. Journal of the Association of Nurses in AIDS Care. 1999;10:42–50. doi: 10.1016/S1055-3290(06)60231-8. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Russell DW. The provisions of social relationships and adaptation to stress. In: Jones WH, Perlman D, editors. Advances in Personal Relationships. Vol. 1. JAI Press; Greenwich, CT: 1987. pp. 37–67. [Google Scholar]
- Dossey BM, Dossey L. Attending to holistic care. American Journal of Nursing. 1998;98:35–38. [PubMed] [Google Scholar]
- Dunbar HT, Mueller W, Medina C, Wolf T. Psychological and spiritual growth in women living with HIV. Social Work: Journal of the National Association of Social Workers. 1998;43:144–154. doi: 10.1093/sw/43.2.144. [DOI] [PubMed] [Google Scholar]
- Ferrans CE. Development of a conceptual model of quality of life. Scholarly Inquiry for Nursing Practice: An International Journal. 1996;10:293–304. [PubMed] [Google Scholar]
- Ferrell BR, Dow KH, Leigh S, Ly J, Gulasekaram P. Quality of life in long-term cancer survivors. Oncology Nursing Forum. 1995;22:915–922. [PubMed] [Google Scholar]
- Folkman S, Chesney M, Pollack L, Coates T. Stress, control, coping, and depressive mood in human immunodeficiency virus-positive and -negative gay men in San Francisco. Journal of Nervous and Mental Disease. 1993;181:409–416. doi: 10.1097/00005053-199307000-00002. [DOI] [PubMed] [Google Scholar]
- Fryback PB, Reinert BR. Alternative therapies and control for health in cancer and AIDS. Clinical Nurse Specialist. 1997;11:64–69. doi: 10.1097/00002800-199703000-00010. [DOI] [PubMed] [Google Scholar]
- Fryback PB, Reinert BR. Spirituality and people with potentially fatal diagnoses. Nursing Forum. 1999;34:13–22. doi: 10.1111/j.1744-6198.1999.tb00231.x. [DOI] [PubMed] [Google Scholar]
- Hall BA. Patterns of spirituality in persons with advanced HIV disease. Research in Nursing and Health. 1998;21:143–153. doi: 10.1002/(sici)1098-240x(199804)21:2<143::aid-nur5>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Hayes RB, Turner H, Coates TJ. Social support, AIDS-related symptoms, and depression among gay men. Journal of Consulting and Clinical Psychology. 1992;60:463–469. doi: 10.1037//0022-006x.60.3.463. [DOI] [PubMed] [Google Scholar]
- Herbert TB, Cohen S. Stress and immunity in humans: a meta-analytic review. Psychosomatic Medicine. 1993;55:364–379. doi: 10.1097/00006842-199307000-00004. [DOI] [PubMed] [Google Scholar]
- Highfield MF. Spiritual health of oncology patients. Cancer Nursing. 1992;15:1–8. [PubMed] [Google Scholar]
- Ironson G, LaPerriere A, Antoni M, O’Hearn P, Schneiderman N, Klimes N, Fletcher MA. Changes in immune and psychological measures as a function of anticipation and reaction to news of HIV-1 antibody status. Psychosomatic Medicine. 1990;52:247–270. doi: 10.1097/00006842-199005000-00001. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Murphy DA, Bahr GR, Kalichman SC, Morgan MG, Stevenson Y, Koob JJ, Brasfield TL, Bernstein BM. Outcome of cognitive-behavioral and support group brief therapies for depressed, HIV-infected persons. American Journal of Psychiatry. 1993;150:1679–1686. doi: 10.1176/ajp.150.11.1679. [DOI] [PubMed] [Google Scholar]
- Kendall J. Wellness spirituality in homosexual men with HIV infection. Journal of the Association of Nurses in AIDS Care. 1994;5:28–34. [PubMed] [Google Scholar]
- Lamendola FP, Newman MA. The paradox of HIV/AIDS as expanding consciousness. Advances in Nursing Science. 1994;16:131–124. doi: 10.1097/00012272-199403000-00004. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, Appraisal, and Coping. Springer; New York: 1984. [Google Scholar]
- Linn JG, Monnig RL, Cain VA, Usoh D. Stage of illness, level of HIV symptoms, sense of coherence and psychological functioning in clients of community-based AIDS counseling centers. Journal of the Association of Nurses in AIDS Care. 1993;4:24–32. [PubMed] [Google Scholar]
- Lipsey MW. Design Sensitivity. Sage Publications; Newbury Park, CA: 1990. [Google Scholar]
- Marbella AM, Ignace G, Diehr S, Harris M. Use of Native American healers among Native American patients in an urban Native American health center. Archives of Family Medicine. 1998;7:182–185. doi: 10.1001/archfami.7.2.182. [DOI] [PubMed] [Google Scholar]
- McCain NL, Cella DF. Correlates of stress in HIV disease. Western Journal of Nursing Research. 1995;17:141–155. doi: 10.1177/019394599501700203. [DOI] [PubMed] [Google Scholar]
- McCain NL, Gramling LF. Living with dying: coping with HIV-disease. Issues in Mental Health Nursing. 1992;13:271–284. doi: 10.3109/01612849209078778. [DOI] [PubMed] [Google Scholar]
- McCain NL, Lyon DE, Higginson R, Settle J, Robins JL, Fisher EJ. Revision of HIV center medical staging. Journal of the Association of Nurses in AIDS Care. 1998;9(5):19–23. doi: 10.1016/s1055-3290(98)80029-0. [DOI] [PubMed] [Google Scholar]
- McCain NL, Smith JC. Stress and coping in the context of psychoneuroimmunology: a holistic framework for nursing practice and research. Archives of Psychiatric Nursing. 1994;VIII:221–227. doi: 10.1016/0883-9417(94)90063-9. [DOI] [PubMed] [Google Scholar]
- McCain NL, Zeller JM. Psychoneuroimmunological studies in HIV disease. Annual Review of Nursing Research. 1996;14:23–55. [PubMed] [Google Scholar]
- McCain NL, Zeller JM, Cella DF, Urbanski PA, Novak RM. The influence of stress management training in HIV disease. Nursing Research. 1996;45:246–253. doi: 10.1097/00006199-199607000-00009. [DOI] [PubMed] [Google Scholar]
- Mishel MH. Perceived uncertainty and stress in illness. Research in Nursing and Health. 1984;7:163–171. doi: 10.1002/nur.4770070304. [DOI] [PubMed] [Google Scholar]
- Mishel MH, Epstein D. Uncertainty in Illness Scales Manual. University of North Carolina School of Nursing; Chapel Hill, NC: 1990. [Google Scholar]
- Nokes KM, Kendrew J, Longo M. Alternative/complementary therapies used by persons with HIV disease. Journal of the Association of Nurses in AIDS Care. 1995;6:19–24. doi: 10.1016/S1055-3290(95)80005-0. [DOI] [PubMed] [Google Scholar]
- Paloutzian RF, Ellison CW. Loneliness, spiritual well-being and the quality of life. In: Peplau LA, Perlman D, editors. Loneliness: A Sourcebook of Current Theory, Research and Therapy. John Wiley & Sons; New York: 1982. pp. 224–237. [Google Scholar]
- Peri TA. Promoting spirituality in persons with acquired immunodeficiency. Holistic Nursing Practice. 1995;10:68–76. doi: 10.1097/00004650-199510000-00011. [DOI] [PubMed] [Google Scholar]
- Perry S, Fishman B, Jacobsberg L, Frances A. Relationships over 1 year between lymphocyte subsets and psychosocial variables among adults with infection by human immunodeficiency virus. Archives of General Psychiatry. 1992;49:396–401. doi: 10.1001/archpsyc.1992.01820050060010. [DOI] [PubMed] [Google Scholar]
- Peterman AH, Mo R, Cella D, McCain NL. Psychometric validation of the revised functional assessment of human immunodeficiency virus infection (FAHI) quality of life instrument. Quality of Life Research. 1997;6:572–584. doi: 10.1023/a:1018416317546. [DOI] [PubMed] [Google Scholar]
- Reed PG. Religiousness among terminally ill and healthy adults. Research in Nursing and Health. 1986;9:35–41. doi: 10.1002/nur.4770090107. [DOI] [PubMed] [Google Scholar]
- Reed PG. Spirituality and well-being in terminally ill hospitalized adults. Research in Nursing and Health. 1987;10:335–344. doi: 10.1002/nur.4770100507. [DOI] [PubMed] [Google Scholar]
- Robinson FP, Mathews HH, Witek-Janusek L. Stress and HIV disease progression: psychoneuroimmunological framework. Journal of the Association of Nurses in AIDS Care. 1999;10:21–23. doi: 10.1016/S1055-3290(06)60229-X. [DOI] [PubMed] [Google Scholar]
- Stolley JM, Koenig H. Religion/spirituality and health among elderly African Americans and Hispanics. Journal of Psychosocial Nursing and Mental Health Services. 1997;35:32–38. doi: 10.3928/0279-3695-19971101-14. [DOI] [PubMed] [Google Scholar]
- Templeton JM. The Humble Approach. Templeton Foundation Press; Philadelphia, PA: 1995. [Google Scholar]
- Wilson HS, Hutchinson SA, Holzemer WL. Salvaging quality of life in ethnically diverse patients with advanced HIV/ AIDS. Qualitative Health Research. 1997;7:75–87. [Google Scholar]
- Zeller JM, McCain NL, Swanson B. Psychoneuroimmunology: an emerging framework for nursing research. Journal of Advanced Nursing. 1996;23:657–664. doi: 10.1111/j.1365-2648.1996.tb00034.x. [DOI] [PubMed] [Google Scholar]


