Abstract
The requirement for major histocompatibility complex class II (MHC II) to initiate immune renal injury was studied in a murine model of CD4+ T cell–dependent crescentic glomerulonephritis (GN). C57BL/6 (MHC II+/+ ) mice developed crescentic GN with glomerular CD4+ T cell infiltration and renal injury, in response to a nephritogenic antigen (sheep globulin) planted on their glomerular basement membrane. MHC II–deficient C57BL/6 mice (MHC II−/− ) did not develop crescentic GN, CD4+ T cell infiltration, or injury, indicating that this form of immune glomerular injury is MHC II dependent. The requirement for MHC II expression by intrinsic renal cells was studied in chimeric mice, which expressed MHC II on bone marrow–derived cells and in the thymus, but not in the kidneys. These chimeric mice had normal T and B cell populations and MHC II expression in their spleens and lymph nodes and developed an immune response to systemically and cutaneously administered sheep globulin. However, they did not develop crescentic GN, CD4+ T cell infiltration, or renal injury in response to the sheep globulin planted in their glomeruli. These studies demonstrate that interaction of CD4+ T cells with intrinsic renal cells expressing MHC II is required for development of cell-mediated immune renal injury.
Keywords: major histocompatibility complex, glomerulonephritis, T lymphocyte, kidney, mice
Tcell responses are normally dependent on recognition of antigen bound to MHC molecules on the surface of APCs. MHC class I molecules are predominantly associated with CD8+ cytotoxic T cell responses. MHC class II (MHC II) molecules present antigens to CD4+ T cells, which stimulate antibody production and isotype switching and act as effector cells for local cell-mediated immune responses.
“Professional” APCs are bone marrow–derived cells that present antigen to naive T cells in secondary lymphoid tissues. After activation, T cells enter nonlymphoid tissues, where they can recognize antigen and initiate local immune responses. It is well accepted that MHC II is required during activation of naive CD4+ T cells in secondary lymphoid tissues. However, the functional contribution of MHC II on resident cells to the effector phase of cell- mediated immune injury targeted at specific tissues in vivo is unknown. MHC II expression can be stimulated on cells in many organs, including mesangial cells (1, 2) and proximal tubular cells in the kidney (3, 4). Thyroid epithelial cells expressing “aberrant” MHC II can present viral antigens to cloned human T cells in vitro (5).
Glomerular antibody deposition and/or accumulation of T cells is observed in the majority of cases of human glomerulonephritis (GN). These immune effectors localize in response to endogenous glomerular antigens or antigens deposited in glomeruli as components of immune complexes or because of their size or charge characteristics. In the most severe forms of human GN, glomerular injury is manifested by a “proliferative” histological pattern, accumulation of T cells and macrophages, proliferation of intrinsic glomerular cells, accumulation of cells and fibrin in Bowman's space (“crescents”), and rapid deterioration of renal function. Studies of crescentic forms of human (6, 7) and experimental GN (8, 9) suggest an important effector role for CD4+ T cells. Glomerular deposition of Ig is often sparse or absent in crescentic human GN (7), and in an experimental model, crescent formation has been demonstrated to be antibody independent (10). However, the role of glomerular MHC II expression in the local immune effector response is unknown.
MHC II-deficient mice have near complete elimination of mature CD4+ T cells in peripheral lymphoid organs and do not develop MHC II–dependent immune reactions (11). B cell responses to T cell–independent but not T cell– dependent antigens are preserved. These mice were used to determine the requirement for MHC II for development of crescentic GN in a CD4+ T cell–dependent murine model, initiated by a nephritogenic antigen planted on the glomerular basement membrane (GBM). The contribution of MHC II on intrinsic renal cells was studied in chimeric mice, which had functional CD4+ T cells but did not express MHC II on intrinsic renal cells.
Materials and Methods
Mice.
MHC II–deficient (MHCII−/−) mice, generated by targeted disruption of the MHCII Aa gene in C57BL/6 mice as described previously (11), were housed under specific pathogen– free conditions.
Generation of MHC II Chimeric Mice.
Chimeric mice (B6→ MHC−/−) expressing MHC II on bone marrow–derived cells but not in other organs were generated using previously described bone marrow and thymus transplantation protocols (12). MHCII−/− mice were thymectomized at 4 wk of age, irradiated with 700 rad at 7 wk of age, and transplanted with T cell–depleted bone marrow from B6 (C57BL/6) mice. After an additional 4 wk, mice were engrafted under the kidney capsule with a thymus from an irradiated (900 rad) newborn wild-type (WT) mouse. B6 mice were subjected to an identical transplantation process to generate control (B6→ B6) chimeras.
Assessment of Lymphocyte Populations in Chimeric Mice.
Lymphocyte subsets in pooled spleen and LN cell suspensions were assessed by flow cytometry using the following mAbs: FITC-conjugated anti-B220, PE-conjugated anti-CD4, PE-conjugated anti-CD8, and FITC-conjugated anti-CD3 (PharMingen, San Diego, CA) as described previously (10). MHC II expression on B cells was assessed using FITC-conjugated anti-MHCII (PharMingen).
Induction of anti-GBM GN and Assessment of Renal Injury.
Crescentic GN was initiated in mice by a single intravenous injection of 10 mg of sheep anti-GBM globulin, as described previously (13). Renal injury and other parameters were assessed 21 d later. Histological assessment was performed on 2-μm periodic acid-Schiff–stained kidney sections. Crescent formation was assessed in a minimum of 30 glomeruli, in a blinded protocol, as described previously (13, 14). Proteinuria was determined by the Bradford method over the final 24 h of each experiment as described (15). Creatinine clearance was calculated from the serum and urine creatinine concentrations, which were measured by the alkaline picric acid method using an autoanalyzer (Cobas Bio; L. Hoffman-La Roche Ltd., Basel, Switzerland).
Assessment of Humoral and Cellular Immune Effectors in Glomeruli.
Glomerular deposition of mouse IgG was assessed on cryostat-cut kidney tissue sections (4 μm) stained with serial dilutions of FITC-conjugated sheep anti–mouse IgG (Silenus, Hawthorn, Victoria, Australia) to determine the end point titer for detection in each animal. Glomerular T cell and macrophage accumulation was assessed on cryostat-cut spleen and kidney tissue sections (6 μm) stained to demonstrate macrophages and T cells using the two-layer peroxidase technique as described (10). The primary antibodies were H129 (monoclonal anti–mouse CD4; American Type Culture Collection, Rockville, MD) and M1/70 (monoclonal anti–mouse Mac-1; American Type Culture Collection). Sections of spleen provided a positive control, and protein G–purified rat Ig was substituted for primary mAb to provide a negative control. A minimum of 20 equatorially sectioned glomeruli were assessed per animal, and the results were expressed as cells per glomerular cross section (c/gcs).
Assessment of the Systemic Immune Response to Sheep Globulin.
Cutaneous delayed-type hypersensitivity (DTH) to the sheep globulin was assessed by intradermal challenge with 0.5 mg in 20 μl of PBS into the hind foot of mice, 20 d after the systemic administration of sheep anti–mouse GBM globulin, as described previously (14). Ovalbumin (Sigma-Aldrich Pty. Ltd., Castle Hill, NSW, Australia) injected into the opposite foot pad was used as a control. Circulating titers of mouse anti–sheep globulin antibody were measured by ELISA as described previously (10, 14). Optical densities (405 nm) were converted to micrograms per milliliter of antibody by reference to a standard curve generated with known concentrations of bound mouse IgG. Serum from six nonimmunized mice was used as normal control. Isotypes of anti–sheep globulin antibody were also measured by ELISA at a single dilution of mouse serum optimized for each isotype (1 in 20 for IgG2a, 1 in 40 for IgG1, IgG2b, and IgG3, and 1 in 80 for IgM) using horseradish peroxidase–conjugated goat anti–mouse IgG1, IgG2a, IgG2b, IgG3, and IgM (Southern Biotechnology Associates, Inc., Birmingham, AL) at a dilution of 1:4,000.
Experimental Design and Statistical Analysis.
The development of GN 21 d after anti-GBM globulin administration was studied in the following groups of mice: B6 (C57BL/6) mice (n = 7), MHCII−/− mice (n = 8), B6→ MHCII−/− chimeric mice (MHCII+/+ thymus and bone marrow in MHC−/− mice; n = 8), and B6→ B6 (control) chimeric mice (MHCII+/+ thymus and bone marrow in MHCII+/+ mice; n = 8). In addition, measurements of baseline renal function were performed on the following separate groups of nonnephritic mice: B6 (C57BL/6) mice (n = 8), MHCII−/− mice (n = 7), and B6→ B6 chimeric mice (n = 8). Results are presented as mean ± SEM. Statistical analysis was performed by one-way analysis of variance, with post hoc analysis using Fisher's protected least significant differences (PLSD) test.
Results
Development of Crescentic GN is MHC II Dependent.
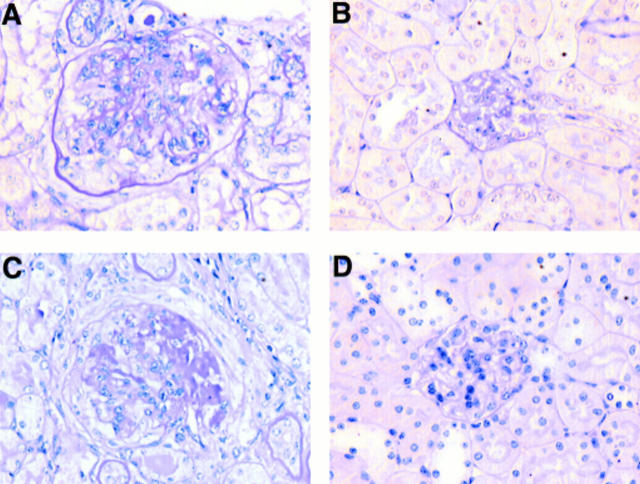
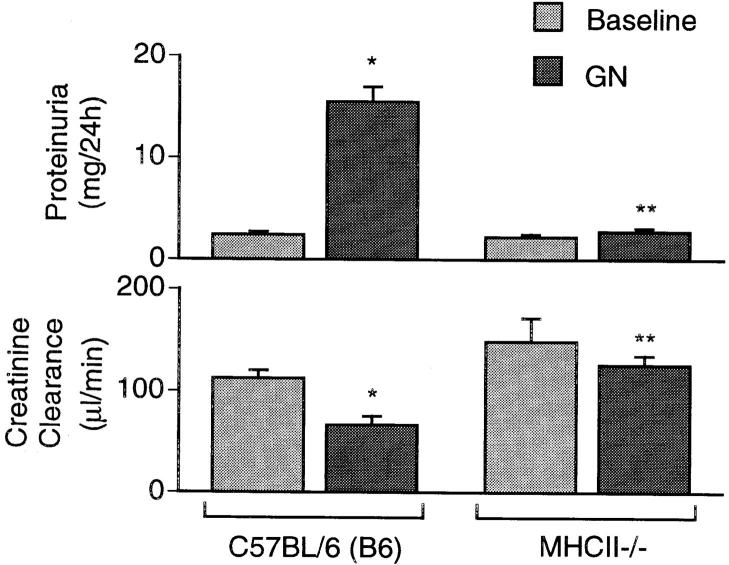
B6 (MHCII+/+) mice developed severe proliferative GN (Fig. 1 A) with crescents in 56.5 ± 5.2% of glomeruli. This resulted in significant proteinuria (15.5 ± 1.5 mg/24 h; baseline 2.4 ± 0.3 mg/24 h, P <0.0001) and impairment of renal function (creatinine clearance, 66.4 ± 9.0 μl/min; baseline 112.4 ± 7.7 μl/min, P = 0.0397) (Fig. 2), and was associated with evidence of systemic and local immune responses to sheep globulin. Mouse anti–sheep globulin antibody was present in the serum (125 ± 29 μg/ml specific mouse anti–sheep globulin antibody), and prominent linear deposition of mouse Ig was observed in glomeruli. Accumulation of CD4+ T cells (1.42 ± 0.37 c/gcs; normal 0.21 ± 0.4 c/gcs) and macrophages (2.21 ± 0.17 c/gcs; normal 0.37 ± 0.09 c/gcs) in glomeruli was also observed. In contrast, MHCII−/− mice did not develop proliferative GN (Fig. 1 B) or crescent formation (0% of glomeruli). Proteinuria was not increased (2.7 ± 0.3 mg/24 h; baseline 2.2 ± 0.3 mg/24 h), and renal function was preserved (creatinine clearance 125.7 ± 9.1 μl/min; baseline 148.6 ± 22.9 μl/ min) (Fig. 2). Specific anti–sheep globulin antibody in the serum was undetectable, as was glomerular deposition of mouse Ig. Glomerular CD4+ T cells (0.08 ± 0.01 c/cgs) and macrophages (0.40 ± 0.12 c/gcs) were not increased compared with the numbers observed in normal (nonnephritic) glomeruli.
Figure 1.
Histological appearance of the glomerular lesions, 21 d after anti-GBM globulin administration, in C57BL/6 (A), MHCII−/− (B), B6→ B6 (control) chimeric (C), and B6→ MHCII−/− chimeric mice (D). Periodic acid-Schiff stain, original magnification ×250.
Figure 2.
Proteinuria and creatinine clearance in normal (light gray bars) C57BL/6 (B6) and MHCII−/− mice, and 21 d after anti-GBM globulin administration (dark gray bars). *Significantly different from baseline values. **Significantly different from WT mice with GN.
B6→ MHCII− /− Chimeric Mice Express MHC II in Spleen and LN Cells and Have Normal Lymphocyte Subsets.
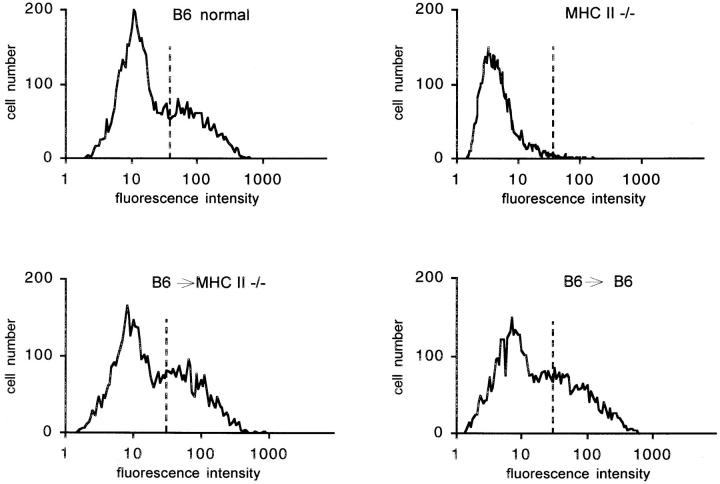
Lymphocyte subset populations and immune competence of chimeric mice were assessed 21 d after administration of anti-GBM globulin. Thymic grafts contained similar numbers of cells in both control (B6→ B6) and B6→ MHCII−/− chimeras (B6→ B6, 3.22 ± 0.48 × 107 cells per graft; B6→ MHCII−/− mice, 2.06 ± 0.14 × 107 cells per graft). Pooled splenic and LN lymphocyte populations in B6→ MHCII−/− mice (CD4+, 24.5 ± 5.0%; CD8+, 12.1 ± 4.5%; B220+, 45.4 ± 8.9% of CD3+) and B6→ B6 mice (CD4+, 22.1 ± 3.5%; CD8+, 10.0 ± 1.9%; B220+, 56.2 ± 7.0% of CD3+) were similar to those in a normal mouse (CD4+, 18.6%; CD8+, 11.9%; B220+, 44% of CD3+). Their splenic and LN B cells showed similar levels of MHC II expression (Fig. 3).
Figure 3.
Flow cytometry profiles demonstrating expression of MHC II on splenic and LN cells from normal C57BL/6 and MHCII−/− mice, and B6→ MHCII−/− and B6→ B6 mice with GN. Vertical dashed lines, Upper limit for background fluorescence.
B6→ MHCII− /− Chimeric Mice Develop a Systemic Immune Response to Sheep Globulin.
The systemic immune response to sheep globulin was similar in chimeric B6→ MHCII−/− mice and B6→ B6 controls. Both groups had similar amounts of specific mouse anti–sheep globulin antibody in their serum (B6→ MHCII−/− with GN, 158 ± 43 μg/ml; B6→ B6 controls with GN, 121 ± 29 μg/ml) and similar antigen-specific Ig isotype profiles (data not shown). Antigen-specific foot pad swelling after intradermal challenge (B6→ B6, 0.35 ± 0.03 mm; B6→ MHCII−/−, 0.27 ± 0.09 mm; WT, 0.29 ± 0.05 mm) indicated that cutaneous DTH to sheep globulin was equivalent. These data demonstrate that the CD4+ compartment in B6→ MHCII−/− mice is functional.
Absence of MHC II Expression by Intrinsic Glomerular Cells Prevents Development of Crescentic GN.
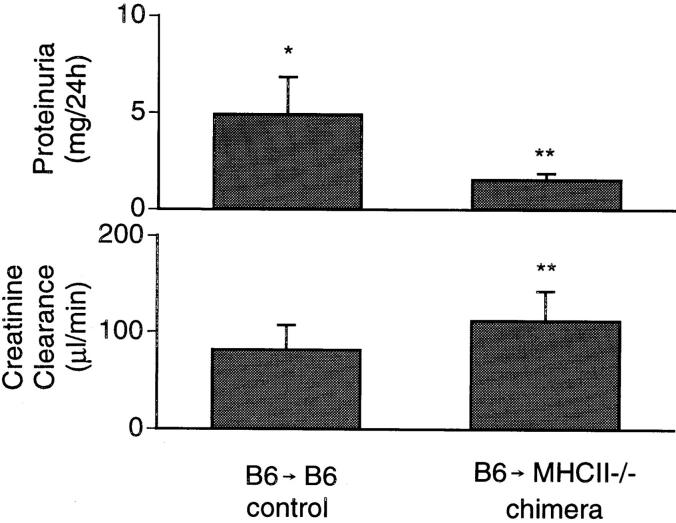
Control chimeric mice (B6→ B6) developed GN similar to B6 (nontransplanted) mice, with severe proliferative changes (Fig. 1 C) and crescents in 43.2 ± 8.9% of glomeruli. Deposition of mouse IgG (data not shown), accumulation of CD4+ T cells (1.17 ± 0.11 c/gcs) and macrophages (2.24 ± 0.14 c/cgs), and renal injury indicated by significant proteinuria (4.9 ± 1.9 mg/24 h; baseline 0.53 ± 0.10 mg/24 h, P <0.0001) and reduced creatinine clearance (88.1 ± 25.5 μl/min) were similar to B6 mice with GN. In contrast, chimeric mice (B6→ MHCII−/−) showed no proliferative changes in glomeruli (Fig. 1 D) and did not develop crescents (0% of glomeruli). Glomerular deposition of mouse Ig was unaffected; however, accumulation of CD4+ T cells (0.46 ± 0.08 c/gcs) and macrophages (0.74 ± 0.21 c/gcs) was markedly reduced. These mice did not develop significant proteinuria (2.7 ± 0.3 mg/24 h, P = 0.468 compared with the baseline in B6→ B6 mice) or impairment of renal function (creatinine clearance 122.3 ± 30.6 μl/min) (Fig. 4).
Figure 4.
Proteinuria and creatinine clearance in B6→ B6 (control) and B6→ MHCII−/− chimeric mice, 21 d after anti-GBM globulin. *Significantly different from baseline values. **Significantly different from B6 mice with GN.
Discussion
Previous studies have demonstrated that crescentic GN in C57BL/6 mice is T cell dependent in the effector phase (14). Injury requires CD4+ T cell–directed macrophage accumulation (13, 14) and does not require an autologous antibody response to the planted nephritogenic antigen (10). T cells and macrophages are evident in glomeruli within 7 d of administration of anti-GBM globulin, and their numbers progressively increase to day 21, as does renal injury (13). Using this model, our current studies demonstrate the requirement for MHC II expression for the development of this cell-mediated immune renal injury. MHC II–deficient mice failed to develop a systemic immune response to the nephritogenic antigen (with no detectable circulating antigen-specific antibody or DTH when challenged cutaneously) and did not develop a local immune response when this antigen was planted in their glomeruli.
Studies of murine lupus have demonstrated that autoantibodies and renal disease do not develop in MHC II–deficient MRL/lpr mice, despite the development of lymphadenopathy and massive expansion of CD4−CD8− (double negative) T cells (16). Renal injury in MRL/lpr mice is associated with glomerular deposition of immune complexes and is B cell dependent (17). Together with our current studies, they provide evidence for a pivotal role for MHC II in the development of both cell-mediated (CD4+- dependent) and antibody-dependent immune glomerular injury.
Chimeric mice were generated to identify the MHC II– expressing cell type recognized by CD4+ T cells in the glomerulus. They lacked MHC II expression on non-bone marrow–derived intrinsic renal cells but had normal levels of MHC II expression on bone marrow–derived cells. Analysis of spleen and LNs confirmed normal lymphocyte subsets and normal CD4+ to CD8+ T cell ratios in transplanted chimeric mice. Their systemic immune response to the nephritogenic antigen was intact. The circulating antigen-specific antibody levels and isotype profiles and the development of a local DTH reaction after cutaneous challenge demonstrated that these mice develop competent CD4+ T cell–dependent immune responses after antigen presentation by bone marrow–derived professional APCs. However, chimeric mice lacking MHC II in their kidneys failed to develop local (CD4+ T cell–dependent) immune injury when the same antigen was planted in their glomeruli. This demonstrates that MHC II expression by intrinsic renal cells is required for antigen-specific CD4+ T cell recruitment and initiation of cell-mediated immune renal injury.
Various renal cell types, including mesangial cells (1, 2) and tubular epithelial cells (3, 4), can express MHC II. CD4+ T cell lines and hybridomas can recognize antigen processed and presented by proximal tubular cells (4) and thyroid epithelial cells (5) in vitro, although less efficiently than with antigen processed by bone marrow–derived APCs. Endothelial cells also have the capacity to express MHC II (18, 19). Our current studies were not able to define which of these cell types are recognized by CD4+ T cells in the kidney. Despite the existence of MHC II+ (Ia+) cells in rat glomeruli (20) and MHC II+ dendritic cells in rodent (21, 22) and human kidneys (23), these bone marrow–derived cells are not sufficient to target the immune response to the kidney and initiate crescentic GN.
Upregulation or novel expression of MHC II by renal cells has been demonstrated in many conditions, including allograft rejection (24), GVHD (25), lupus nephritis (26), and IgA disease (27). Tubular epithelial cells can present antigen to T cell clones derived from kidneys of MRL/lpr mice, but their ability to perform this function in vivo has not been clearly demonstrated (28). MHCII−/− kidneys transplanted into MRL/lpr mice still develop GN and interstitial inflammatory cell infiltrates (29). This indicates that expression of MHC II by intrinsic renal cells is not required for development of this antibody-dependent form of GN, in which the immune effector response is targeted to the glomerulus (and other vascular beds) because of local immune complex deposition. In contrast, this study demonstrates that GN, initiated by a planted nephritogenic antigen and directed by CD4+ T cells, requires MHC II expression by intrinsic renal cells. These results provide the first demonstration of the functional importance of local MHC II expression by intrinsic renal cells for targeting an immune injury to the glomerulus.
Because a systemic immune response to the nephritogenic antigen was observed, it is likely that naive CD4+ T cells are activated in secondary lymphoid organs by professional APCs after intravenous antigen challenge. It is unlikely that intrinsic renal cells participate in this initial priming, although we cannot exclude such a role. However, any contribution of this to the subsequent immune response would seem negligible, as chimeric mice without MHC II in their kidneys develop a systemic immune response to the nephritogenic antigen that is indistinguishable from that in normal mice. Expression of MHC II by intrinsic renal cells would appear to be functionally important in the effector phase of this disease, but was not necessary for initiation of the primary immune response.
In conclusion, these studies provide evidence for MHC II–dependent CD4+ T cell–directed injury in crescentic GN. In addition, they demonstrate that in the effector phase of this disease, MHC II expression by intrinsic renal cells is required to direct the CD4+ T cell effector response in the glomerulus, and that MHC II on bone marrow– derived cells alone is not sufficient. This provides the first demonstration of a requirement for MHC II expression by nonprofessional APCs for development of a T cell–dependent injury. The approach of transplanting MHC-intact bone marrow and thymus into MHC-deficient mice may be used to explore the role of local MHC II expression in a variety of CD4+ T cell–dependent organ-specific immune diseases.
Table 1.
Serum Levels of Specific Mouse anti–sheep Globulin Antibody
| Group | Specific serum antibody | |
|---|---|---|
| μg/ml | ||
| B6 with GN | 125 ± 29 | |
| MHCII−/− with GN | Undetectable | |
| B6→ B6 with GN | 121 ± 14 | |
| B6→ MHCII−/− with GN | 158 ± 34 |
Acknowledgments
These studies were supported by grants from the National Health and Medical Research Council of Australia, and the Australian Kidney Foundation. S. Li is the recipient of a Monash Research Fund Postgraduate Scholarship. C. Kurts is supported by a fellowship from the Deutsche Forschungsgemeinschaft (grant Ku1063/1-2).
Footnotes
The technical help of Mr. P. Hutchinson and Ms. J. Tsoupas is gratefully acknowledged. We thank William Heath, Dianne Mathis, and Christophe Benoit for valuable discussions.
C. Kurts's current address is Department of Nephrology, Medizinische Hochschule, 30625, Hannover, Germany. E-mail: ckurts@compuserve.com
S. Li and C. Kurts contributed equally to this paper.
References
- 1.Martin M, Schwinzer R, Schellekens H, Resch K. Glomerular mesangial cells in local inflammation. Induction of the expression of MHC class II antigens by IFN-gamma. J Immunol. 1989;142:1887–1894. [PubMed] [Google Scholar]
- 2.Radeke HH, Emmendorffer A, Uciechowski P, von der Ohe J, Schwinzer B, Resch K. Activation of autoreactive T-lymphocytes by cultured syngeneic glomerular mesangial cells. Kidney Int. 1994;45:763–774. doi: 10.1038/ki.1994.101. [DOI] [PubMed] [Google Scholar]
- 3.Wuthrich RP, Glimcher LH, Yui MA, Jevnikar AM, Dumas SE, Kelley VE. MHC class II, antigen presentation and tumor necrosis factor in renal tubular epithelial cells. Kidney Int. 1990;37:783–792. doi: 10.1038/ki.1990.46. [DOI] [PubMed] [Google Scholar]
- 4.Hagerty DT, Allen PM. Processing and presentation of self and foreign antigens by the renal proximal tubule. J Immunol. 1992;148:2324–2330. [PubMed] [Google Scholar]
- 5.Londei M, Lamb JR, Bottazzo GF, Feldmann M. Epithelial cells expressing aberrant MHC class II determinants can present antigen to cloned human T cells. Nature. 1984;312:639–641. doi: 10.1038/312639a0. [DOI] [PubMed] [Google Scholar]
- 6.Neale TJ, Tipping PG, Carson SD, Holdsworth SR. Participation of cell-mediated immunity in deposition of fibrin in glomerulonephritis. Lancet. 1988;2:421–424. doi: 10.1016/s0140-6736(88)90413-8. [DOI] [PubMed] [Google Scholar]
- 7.Stilmant MM, Bolton WK, Sturgill BC, Couser WG. Crescentic glomerulonephritis without immune deposits: clinicopathologic features. Kidney Int. 1979;15:184–195. doi: 10.1038/ki.1979.24. [DOI] [PubMed] [Google Scholar]
- 8.Huang XR, Holdsworth SR, Tipping PG. Evidence for delayed-type hypersensitivity mechanisms in glomerular crescent formation. Kidney Int. 1994;46:69–78. doi: 10.1038/ki.1994.245. [DOI] [PubMed] [Google Scholar]
- 9.Tipping PG, Neale TJ, Holdsworth SR. T lymphocyte participation in antibody-induced experimental glomerulonephritis. Kidney Int. 1985;27:530–537. doi: 10.1038/ki.1985.43. [DOI] [PubMed] [Google Scholar]
- 10.Li S, Holdsworth SR, Tipping PG. Antibody independent crescentic glomerulonephritis in mu chain deficient mice. Kidney Int. 1997;51:672–678. doi: 10.1038/ki.1997.97. [DOI] [PubMed] [Google Scholar]
- 11.Kontgen F, Suss G, Stewart C, Steinmetz M, Bluethmann H. Targeted disruption of the MHC class II Aa gene in C57BL/6 mice. Int Immunol. 1993;5:957–964. doi: 10.1093/intimm/5.8.957. [DOI] [PubMed] [Google Scholar]
- 12.Kurts C, Kosaka H, Carbone FR, Miller JF, Heath WR. Class I-restricted cross-presentation of exogenous self-antigens leads to deletion of autoreactive CD8+T cells. J Exp Med. 1997;186:239–245. doi: 10.1084/jem.186.2.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tipping PG, Huang XR, Qi M, Van GY, Tang WW. Crescentic glomerulonephritis in CD4 and CD8 deficient mice: requirement for CD4 but not CD8 cells. Am J Pathol. 1998;152:1541–1548. [PMC free article] [PubMed] [Google Scholar]
- 14.Huang XR, Tipping PG, Li S, Holdsworth SR. Th1 responsiveness to nephritogenic antigens determines susceptibility to crescentic glomerulonephritis in mice. Kidney Int. 1997;51:94–103. doi: 10.1038/ki.1997.12. [DOI] [PubMed] [Google Scholar]
- 15.Bradford MM. A rapid and sensitive method for the quantitation of microgram quantities of protein utilizing the principle of protein-dye binding. Anal Biochem. 1976;72:248–254. doi: 10.1016/0003-2697(76)90527-3. [DOI] [PubMed] [Google Scholar]
- 16.Jevnikar AM, Grusby MJ, Glimcher LH. Prevention of nephritis in major histocompatibility complex class II-deficient MRL-lpr mice. J Exp Med. 1994;179:1137–1143. doi: 10.1084/jem.179.4.1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shlomchik MJ, Madaio MP, Ni D, Trounstein M, Huszar D. The role of B cells in lpr/lpr-induced autoimmunity. J Exp Med. 1994;180:1295–1306. doi: 10.1084/jem.180.4.1295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pober JS, Gimbrone MA, Jr, Cotran RS, Reiss CS, Burakoff SJ, Fiers W, Ault KA. Ia expression by vascular endothelium is inducible by activated T cells and by human gamma interferon. J Exp Med. 1983;157:1339–1353. doi: 10.1084/jem.157.4.1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Collins T, Korman AJ, Wake CT, Boss JM, Kappes DJ, Fiers W, Ault KA, Gimbrone MA, Jr, Strominger JL, Pober JS. Immune interferon activates multiple class II major histocompatibility complex genes and the associated invariant chain gene in human endothelial cells and dermal fibroblasts. Proc Natl Acad Sci USA. 1984;81:4917–4921. doi: 10.1073/pnas.81.15.4917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schreiner GF, Kiely JM, Cotran RS, Unanue ER. Characterization of resident glomerular cells in the rat expressing Ia determinants and manifesting genetically restricted interactions with lymphocytes. J Clin Invest. 1981;68:920–931. doi: 10.1172/JCI110347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mayrhofer G, Schon-Hegrad MA. Ia antigens in rat kidney, with special reference to their expression in tubular epithelium. J Exp Med. 1983;157:2097–2109. doi: 10.1084/jem.157.6.2097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Austyn JM, Hankins DF, Larsen CP, Morris PJ, Rao AS, Roake JA. Isolation and characterization of dendritic cells from mouse heart and kidney. J Immunol. 1994;152:2401–2410. [PubMed] [Google Scholar]
- 23.Bishop GA, Hall BM. Expression of leucocyte and lymphocyte adhesion molecules in the human kidney. Kidney Int. 1989;36:1078–1085. doi: 10.1038/ki.1989.303. [DOI] [PubMed] [Google Scholar]
- 24.Benson EM, Colvin RB, Russell PS. Induction of IA antigens in murine renal transplants. J Immunol. 1985;134:7–9. [PubMed] [Google Scholar]
- 25.Sinclair GD, Wadgymar A, Halloran PF, Delovitch TL. Graft-vs.-host reactions induce H-2 class II gene transcription in host kidney cells. Immunogenetics. 1984;20:503–511. doi: 10.1007/BF00364353. [DOI] [PubMed] [Google Scholar]
- 26.Wuthrich RP, Yui MA, Mazoujian G, Nabavi N, Glimcher LH, Kelley VE. Enhanced MHC class II expression in renal proximal tubules precedes loss of renal function in MRL/lpr mice with lupus nephritis. Am J Pathol. 1989;134:45–51. [PMC free article] [PubMed] [Google Scholar]
- 27.Yokoyama H, Takaeda M, Wada T, Ogi M, Tomosugi N, Takabatake T, Abe T, Yoshimura M, Kida H, Kobayashi K. Intraglomerular expression of MHC class II and Ki-67 antigens and serum gamma-interferon levels in IgA nephropathy. Nephron. 1992;62:169–175. doi: 10.1159/000187028. [DOI] [PubMed] [Google Scholar]
- 28.Kelley VR, Diaz-Gallo C, Jevnikar AM, Singer GG. Renal tubular epithelial and T cell interactions in autoimmune renal disease. Kidney Int Suppl. 1993;39:S108–S115. [PubMed] [Google Scholar]
- 29.Mukherjee R, Zhang Z, Zhong R, Yin ZQ, Roopenian DC, Jevnikar AM. Lupus nephritis in the absence of renal major histocompatibility complex class I and class II molecules. J Am Soc Nephrol. 1996;7:2445–2452. doi: 10.1681/ASN.V7112445. [DOI] [PubMed] [Google Scholar]