Abstract
Background
While studies provide us with a cross-sectional analysis of QOL long-term after transplantation, relatively few longitudinal studies were found that allow us to understand changes in QOL over time. The purposes of our study were to describe QOL over time and identify predictors of QOL longitudinally from 5 – 10 years after heart transplantation.
Methods
The 555 enrolled patients who completed booklets of questionnaires were approximately 54 years at time of transplant (range = 21 – 75 years), 78% men, and 88% Caucasian. Patients completed nine self-report QOL instruments for this report. Statistical analyses included frequencies, means ± standard deviation (plotted over time), Pearson correlation coefficients, and multiple regression coupled with repeated measures.
Results
At 5 – 10 years after heart transplantation, recipients reported high levels of satisfaction with overall QOL and with health-related QOL that was stable over the 5 year period. Predictors of satisfaction with overall QOL (that individually accounted for 1% variance or more) were primarily psychosocial variables (overall model explaining 71% of variance), while predictors of satisfaction with QOL related to health and functioning (that also explained ≥ 1% variance) included symptom distress and physical function, as well as psychosocial variables (overall model explaining 72% of variance).
Conclusions
At 5 – 10 years after heart transplantation, QOL is positive and stable. Biopsychosocial variables predict satisfaction with overall QOL and health-related QOL. Understanding of these biopsychosocial provides direction for development of therapeutic strategies long-term after heart transplantation, so that patients can experience good post transplant outcomes.
Quality of life (QOL) is an important outcome to study in patients who undergo solid organ transplantation. With improved long-term post transplant survival, health care providers have extended their focus to include the study of QOL beyond the first few years after transplantation. In a cross-sectional study comparing QOL in a general population with adults who had undergone heart, liver, or kidney transplant more than 10 years earlier, researchers reported that recipient QOL approached that of the general population, although they did not experience a true return to normal status1. In another cross-sectional study, Politi et al.2 provided additional insight into QOL in heart transplant recipients who were more than 10 years post transplant and noted that while mental QOL was similar to the general population, physical QOL was significantly lower than that for the general population.
While studies such as those by Karam et al.1, Politi et al.2 and others3-7, provide us with a cross-sectional analysis of QOL long-term after transplantation, relatively few longitudinal studies were found that allow us to understand changes in QOL over time8-9. These studies were limited in that they described change over a 1 year time period9 or only examined change through 5 years after heart transplantation8.
The purposes of our study were to describe QOL over time and identify predictors of QOL longitudinally from 5 – 10 years after heart transplantation. QOL was defined as “the functional effect of an illness and its consequent therapy upon a patient, as perceived by the patient”10. Domains of QOL that were measured included physical and occupational function, psychological state, social interaction, and somatic sensation10.
METHODS
Sample
Patients who participated in this research were from a large, multi-site, prospective study of QOL outcomes between 5 – 10 years after heart transplantation. The non-random sample for our study was drawn from patients (n=1,437) who were transplanted between July 1, 1990 and June 30, 1999 at four medical centers in the United States (figure 1). There were 884 patients between 5 – 10 years post heart transplantation who were potentially eligible for recruitment into the study. The 553 patients who were not eligible for study recruitment died prior to consent (n=386) or transferred care to another institution (n=167).
Figure 1.
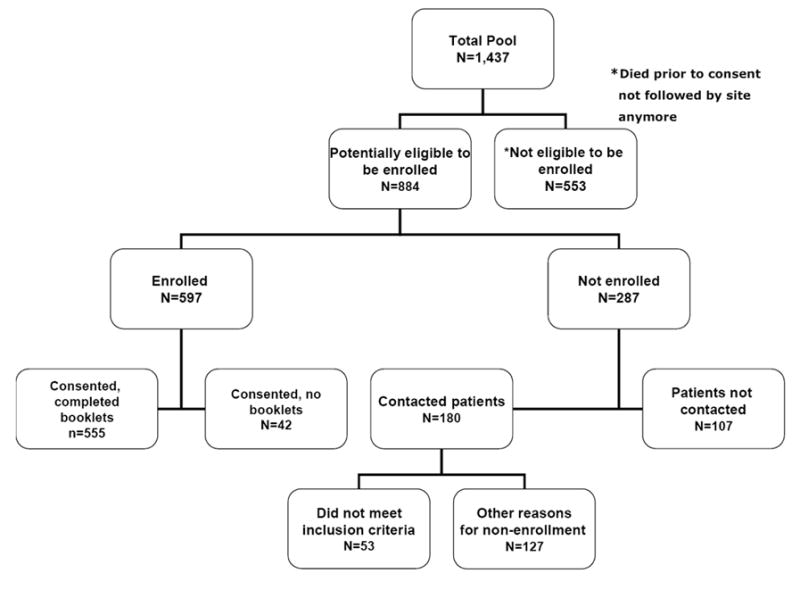
Study Sample
Study inclusion criteria were age ≥ 21 years, able to read and write English, and physically able to participate. Informed consent was received from 597 patients; however, only 555 patients provided informed consent and completed one or more booklets of questionnaires. Thus, our sample size for this report is comprised of 555 patients who were between 5 – 10 years post heart transplantation. The average period of follow-up was 2.5 years per patient. Our overall retention rate was 70%.
Instruments
Patients completed nine self-report QOL instruments for this report (see Table 1). These instruments were selected based on their relevance to this patient population and adequacy of psychometric support. Thus, the following instruments were completed by patients: Quality of Life Index – Cardiac Version IV12, Positive and Negative Affect Schedule – Expanded version (PANAS – X)13-15, Cardiac Depression Scale (CDS)16, Sickness Impact Profile17, Social Support Index18, Heart Transplant Symptom Checklist19, Heart Transplant Stressor Scale20, Jalowiec Coping Scale21, and Heart Transplant Intervention Scale22. Fatigue, sensitization, and response bias were controlled by varying the sequence of instruments compiled into a booklet for each time period.
Table 1.
Self-Report Instruments Used to Measure Quality of Life (QOL) and Factors Affecting QOL
| Instrument/author | Number of items | Domains of QOL | Subscales | Scoring |
|---|---|---|---|---|
| Quality of Life Index/Ferrans and Powers12 | 35 | Psychological state
Physical and occupational function Social Interaction |
Health/functioning
Socioeconomic Psychological/Spiritual Family |
Satisfaction with areas of life: 1-6
1 = very dissatisfied 6 = very satisfied |
| Heart Transplant Symptom Checklist/Grady et al19 | 89 | Somatic sensation
Psychological state |
Cardiopulmonary
Gastrointestinal Genitourinary Neurological Dermatological/soft tissue Psychological |
0-3
0 = not bothered at all 3 = very bothered |
| Heart Transplant Stressor Scale/Jalowiec et al20 | 81 | Physical and occupational function
Psychological state Social interaction |
Physical
Psychological Self-care Family Work/school/financial Hospital/clinic |
0-3
0= not stressful at all 3= very stressful |
| Sickness Impact Profile/Bergner et al17 | 136 | Physical and occupational function
Psychological state Social interaction |
Sleep/rest
Emotional behavior Self-care Home management Mobility Social interaction Ambulation Alertness Communication Recreation Eating Work |
Yes/No
Yes responses are weighted by amount of disability indicated |
| Jalowiec Coping Scale/Jalowiec21 | 60 | Psychological state | Confrontive
Evasive Optimistic Fatalistic Emotive Palliative Supportant Self-reliant |
Use of coping strategy: 0-3
0= never used 3=often used Effectiveness of coping strategy: 0-3 0= not helpful 3= very helpful |
| Heart Transplant Intervention Scale/Grady et al22 | 62 | Psychological state
Social interaction Physical and occupational function |
Information provision
Self-care teaching Emotional/supportive Family related Work/school/financial |
0-3
0= not helpful 3= very helpful |
| Social Support Index/Jalowiec et al18 | 15 | Social interaction | Tangible support
Emotional support |
1-4
1 = very dissatisfied 4 = very satisfied |
| Positive and Negative Affect Schedule/Watson and Clark13 | 52 | Psychological state | Fear
Hostility Guilt Sadness Joviality Self-assurance Attentiveness Fatigue Serenity |
1-5
1=very slightly or not at all 5= extremely |
| Cardiac Depression Scale/Hare and Davis16 | 26 | Psychological state | Sleep
Anhedonia Uncertainty Mood Cognition Hopelessness Inactivity |
1-7
Agreement or disagreement with individual anchors for each question |
Support for reliability and validity has been reported previously for each instrument: Quality of Life Index – Cardiac Version IV12, 23, 24, Positive and Negative Affect Schedule – Expanded version13, Cardiac Depression Scale16, Sickness Impact Profile17, 25, 26, Social Support Index18, Heart Transplant Symptom Checklist19, 27, Heart Transplant Stressor Scale20, Jalowiec Coping Scale21, and Heart Transplant Intervention Scale22. The adequacy of psychometric support has been demonstrated through use of these instruments in chronic illness populations, including patients with heart failure who subsequently underwent heart transplantation.
Clinical data were available from two sources: (1) in-hospital and outpatient medical records and (2) the Cardiac Transplant Research Database (CTRD). Data from medical records were collected by research coordinators every 6 months as part of this study. CTRD Registry data were collected external to this study. Clinical data included medical, surgical, and psychosocial history; United Network for Organ Sharing (UNOS) status at time of transplant; co-morbidities after transplant; hospitalizations, complications of heart transplantation (ie., acute rejection, infection, coronary allograft vasculopathy, and malignancy); and post transplant medications (immunosuppressants and other).
Procedures
The Institutional Review Boards at each of the four participating centers granted approval for conduct of both the study and the CTRD. Potential subjects who were ≥ 4.5 years post transplant were contacted by study coordinators. The study was explained and subjects who agreed to participate were enrolled in the study. After written consent was obtained, patients were given a booklet of questionnaires and asked to return the questionnaires within 2 – 3 days using a stamped, addressed envelope. Subsequently, patients were mailed questionnaires every 6 months between 5 and 10 years post transplant, based on the date of their transplant.
Completed booklets of questionnaires were sent from participating centers to Rush University Medical Center for screening and cleaning of data. Queries regarding incomplete or unclear booklet data were sent to the research coordinator who then contacted each patient to rectify queries. Booklets were re-checked at Rush and were mailed to the University of Alabama for computer entry of data.
Statistical Analyses
Data were analyzed using SAS version 8.2 (SAS, Cary, NC). Analyses included frequencies, means ± standard deviation (plotted over time), Pearson correlation coefficients, and multiple regression coupled with repeated measures. Initially, mean item, subscale, and total scale scores were calculated for patients. Prior to major analyses, data were converted to a standardized scale of 0.00 – 1.00 by dividing the item, subscale, and total scale scores by the maximum possible score for most instruments. Standardized scores were not calculated for the PANAS-X and CDS because the authors of these tools reported data using non-standardized scores.
Two regression analyses were performed. The dependent variables for the multiple regression analyses were the total satisfaction score and the satisfaction with health and functioning subscale score from the Quality of Life Index – Cardiac Version IV. The health and functioning subscale has 15 items (Table 2). We ran two analyses because we wanted to examine the relationships between the independent variables and overall quality of life as well as quality of life related more specifically to health. Correlations were performed between the dependent variable and proposed independent variables (demographic characteristics, clinical variables, and physical / psychosocial variables). No variables were found to be highly correlated with the dependent variable. Inter-item correlations among the independent variables were also examined and mlticollinearity was identified in <0.001% of variables and therefore was not a problem. All variables were subsequently entered into the regression model in groups (in the order identified above). The model fit was tested and acceptable. No influential outliers were identified; thus all subjects were retained in the anlayses. For all analyses, the level of significance was set at p = 0.05.
Table 2.
Health and functioning subscale of the Quality of Life Index12
| Subscale items |
|---|
| Health |
| Health care |
| Chest pain (angina) |
| Shortness of breath |
| Energy (fatigue) |
| Ability to take care of yourself without help |
| Control over life |
| Chances for living as long as you would like |
| Sex life |
| Ability to take care of family responsibilities |
| Usefulness to others |
| Worries |
| Things for fun |
| Chances for a happy future |
| Lifestyle changes |
RESULTS
Descriptive analyses
Demographic and clinical characteristics
The 555 enrolled patients who completed booklets of questionnaires were approximately 54 years at time of transplant (range = 21 – 75 years), 78% men, 88% Caucasian, 79% married, and 59% with more than a high school education (mean = 14 ± 2.9 years). Demographic and clinical characteristics of enrolled patients (n=597) were compared with characteristics of non-enrolled patients who were contacted and met study entry criteria (n=127) (Table 3). Significant differences between the two groups emerged only regarding age. Significantly more enrolled patients were older than non-enrolled patients. Both groups had similar numbers of acute rejection and infection episodes.
Table 3.
Characteristics of enrolled and not enrolled patients
| Characteristics | Enrolled in study (n=597) | Not enrolled in study with self exclusion (n=127) | p-value |
|---|---|---|---|
| Demographic | |||
| Age at transplant (years) (mean ± SD) | 53.6 ± 10.1 | 51.6 ± 10.5 | 0.05 |
| Gender (%) | |||
| Men | 79% | 79% | 0.99 |
| Women | 21% | 21% | |
| Race/ethnicity (%) | |||
| White | 87% | 81% | 0.09 |
| Black | 10% | 13% | |
| Hispanic | 1% | 2% | |
| Other | 2% | 4% | |
| Status I at transplant (%) | 63% | 61% | 0.62 |
| Clinical | |||
| Acute rejection (total # episodes) | 40 | 6 | 0.48 |
| Infection (total # episodes) | 65 | 10 | 0.41 |
Regarding clinical characteristics, ischemic cardiomyopathy and dilated cardiomyopathy accounted for the vast majority of causes of heart failure resulting in transplantation (56% and 32%, respectively). Sixty-one percent of patients were UNOS status 1 (ie., status1A or 1B) at time of transplant. Patients were typically New York Heart Association (NYHA) class I (mean = 1.3) between 5 - 10 years after heart transplantation. Patients were overweight (BMI=28.9 kg/m2). Hospital readmissions were uncommon at 5 – 10 years after transplant (0.2 readmissions / patient for a mean of 2.7 days / admission). Immunosuppression included cyclosporine (84%) or tacrolimus (16%), mycophenolate mofetil (52%) or azathioprine (48%), and steroids. Additionally, patients took an average of 8 non-immunosuppressant medications daily.
The most common co-morbidities (as per chart review) in these 555 patients after heart transplantation were: hypertension (87%), hyperlipidemia (78%), renal dysfunction (37%), cancer (including skin cancer) (27%), diabetes (27%), orthopedic problems (26%), psychological problems (23%), and gastrointestinal problems (22%). Patients reported having more than one co-morbidity (mean = 5 ± 2.6 co-morbidities / patient). Cumulative rates of acute rejection and infection from 5 – 10 years post transplant were 2.2 ± 2.0 and 0.8 ± 1.3, respectively, and 42% of patients had evidence of cardiac allograft vasculopathy (via coronary angiography).
Patterns of QOL at 5 – 10 years post transplant
At 5 – 10 years after heart transplantation, patients were very satisfied with their overall QOL (Figure 2). When patterns of satisfaction with QOL were examined across time by age, gender, and race, no significant differences emerged. Furthermore, patients were very satisfied with their health and functioning from 5 – 10 years after transplant (Figure 3). These findings also did not vary by age, gender, and race.
Figure 2.
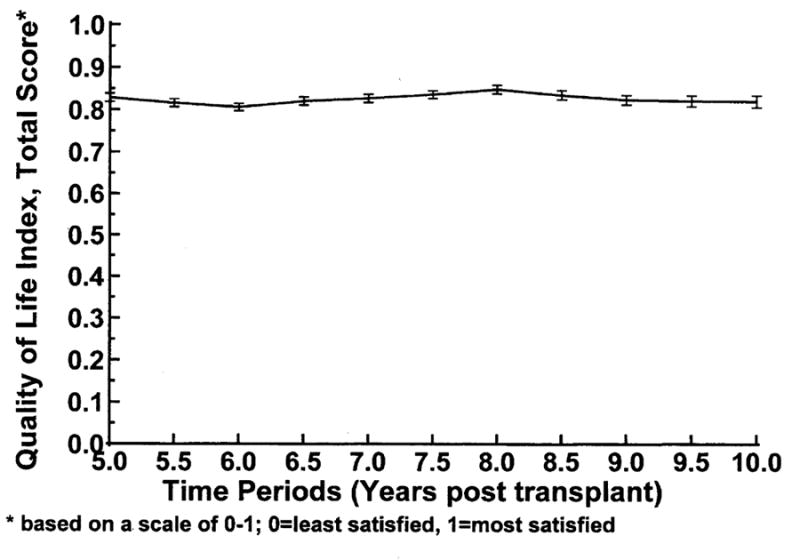
Satisfaction with Quality of Life 5- 10 Years after Heart Transplantation
Figure 3.
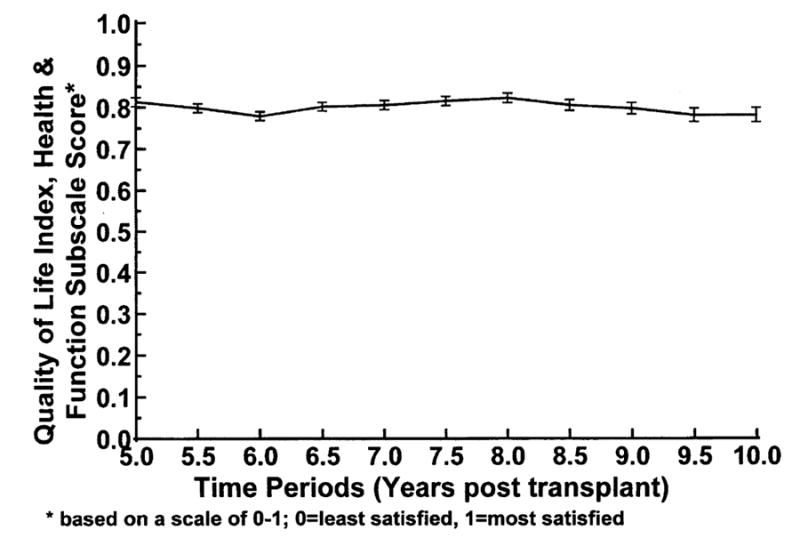
Satisfaction with Health and Functioning at 5 - 10 Years after Heart Transplantation
Multivariate analyses
Independent variables (demographic characteristics, clinical variables, and physical / psychosocial variables) that correlated significantly (p ≤ 0.05) with the two dependent variables were entered into two separate multiple regression equations, adjusted for time. Predictors of more satisfaction with overall QOL at 5 – 10 years after heart transplantation were less depression, fewer negative emotions (ie., hopelessness, sadness, and guilt), more positive emotions (ie., pleasure and joviality), less uncertainty, less fatigue, more satisfaction with emotional support, less family-related stress, use of more positive coping styles, less sleep disturbance, more social interaction, less dermatologic symptom distress, more helpfulness of self-care management interventions, not working, being married, not having an HMO insurance plan, and not having complications of heart transplantation (ie., acute rejection, vasculopathy, and genitourinary co-existing illnesses), accounting for 71% of variance (F=160.60, p<0.0001) (Table 4).
Table 4.
Predictors of Satisfaction with Quality of Life 5-10 years after Heart Transplantation
| Variable | Partial R-Square | Model R-Square | F Value | p value |
|---|---|---|---|---|
| Depression | 0.573 | 0.573 | 2691.26 | < .0001 |
| Joviality | 0.035 | 0.609 | 180.03 | < .0001 |
| Social Interaction | 0.025 | 0.634 | 141.41 | < .0001 |
| Satisfact with Emotional Support | 0.016 | 0.650 | 90.67 | < .0001 |
| Pleasure | 0.011 | 0.661 | 63.00 | < .0001 |
| Fatigue | 0.010 | 0.671 | 58.74 | < .0001 |
| Being married | 0.007 | 0.677 | 40.93 | < .0001 |
| Emotional Support Effectiveness | 0.003 | 0.680 | 19.83 | < .0001 |
| Emotional Behavior | 0.003 | 0.684 | 20.80 | < .0001 |
| Derm-Soft Tissue Symptom Distress | 0.003 | 0.686 | 16.65 | < .0001 |
| Hopelessness | 0.002 | 0.688 | 11.55 | 0.0007 |
| Degree of Family Stress | 0.002 | 0.690 | 10.85 | 0.001 |
| Not having an HMO insurance plan | 0.002 | 0.691 | 10.53 | 0.001 |
| Transplant event (total of rejection + infection + vasculopathy + malignancy) | 0.001 | 0.693 | 8.85 | 0.003 |
| Coronary Artery Vasculopathy | 0.002 | 0.695 | 11.22 | 0.0008 |
| Uncertainty | 0.002 | 0.696 | 9.80 | 0.002 |
| Sleep and Rest | 0.001 | 0.697 | 8.18 | 0.004 |
| Self-care Teaching Effectiveness | 0.001 | 0.698 | 7.52 | 0.006 |
| Use of confrontative coping | 0.001 | 0.700 | 7.06 | 0.008 |
| Use of self-reliant coping | 0.001 | 0.701 | 8.41 | 0.004 |
| Sadness | 0.001 | 0.702 | 7.82 | 0.005 |
| Fear | 0.001 | 0.703 | 6.37 | 0.01 |
| Alertness | 0.001 | 0.704 | 7.14 | 0.008 |
| Genitourinary/Urological Co-existing Illiness | 0.001 | 0.705 | 6.04 | 0.01 |
| Guilt | 0.001 | 0.706 | 4.99 | 0.03 |
| Hostility | 0.001 | 0.706 | 5.67 | 0.02 |
| Use of supportant coping | 0.001 | 0.707 | 4.92 | 0.03 |
| Work | 0.001 | 0.708 | 5.35 | 0.02 |
| Cumulative rejections | 0.001 | 0.709 | 5.56 | 0.02 |
| Satisfact with Tangible Support | 0.001 | 0.709 | 4.15 | 0.04 |
Predictors of more satisfaction with health and functioning at 5 – 10 years after heart transplantation were generally similar to predictors of more satisfaction with overall QOL. However, variables that accounted for ≥1% variance in this regression analysis that were not predictors of overall QOL were less dysfunction related to body care / movement and less cardiopulmonary symptom distress. All variables predicting more satisfaction with health and functioning, accounting for 72% of variance (F=162.30, p<0.0001) are listed in Table 5.
Table 5.
Predictors of Satisfaction with Health & Functioning at 5-10 years after Heart Transplantation
| Variable | Partial R-Square | Model R-Square | F Value | p value |
|---|---|---|---|---|
| Depression | 0.581 | 0.581 | 2773.76 | < .0001 |
| Sleep and rest | 0.035 | 0.616 | 182.78 | < .0001 |
| Joviality | 0.020 | 0.636 | 109.20 | < .0001 |
| Body Care and Movement | 0.020 | 0.655 | 114.19 | < .0001 |
| Fatigue | 0.009 | 0.664 | 52.86 | < .0001 |
| Pleasure | 0.007 | 0.672 | 44.66 | < .0001 |
| Cardiopulmonary Symptom Distress | 0.006 | 0.678 | 37.28 | < .0001 |
| Emotional Support Effectiveness | 0.005 | 0.682 | 29.98 | < .0001 |
| Recreation | 0.004 | 0.686 | 22.80 | < .0001 |
| Satisfaction with Emotional Support | 0.004 | 0.690 | 24.21 | < .0001 |
| Uncertainty | 0.003 | 0.693 | 19.70 | < .0001 |
| Coronary Artery Vasculopathy | 0.002 | 0.695 | 15.84 | < .0001 |
| Degree of Family Stress | 0.003 | 0.698 | 17.87 | < .0001 |
| Ambulation | 0.002 | 0.700 | 11.58 | 0.0007 |
| Hopelessness | 0.002 | 0.702 | 12.92 | 0.0003 |
| Transplant event (total of rejection + infection + vasculopathy + malignancy) | 0.002 | 0.703 | 11.76 | 0.0006 |
| Hostility | 0.001 | 0.705 | 9.27 | 0.002 |
| Emotional Behavior | 0.002 | 0.706 | 10.40 | 0.001 |
| Self Care Teaching Effectiveness | 0.001 | 0.708 | 8.92 | 0.003 |
| Derm-Soft Tissue Symptom Distress | 0.001 | 0.709 | 8.03 | 0.005 |
| Home Management | 0.001 | 0.711 | 5.76 | 0.02 |
| Cumulative rejections | 0.001 | 0.711 | 5.84 | 0.02 |
| Non-white | 0.001 | 0.712 | 5.48 | 0.02 |
| Work | 0.001 | 0.713 | 7.09 | 0.008 |
| Education, total years | 0.001 | 0.714 | 7.29 | 0.007 |
| Gout | 0.001 | 0.715 | 5.24 | 0.02 |
| Number of Co-Existing Illnesses | 0.001 | 0.716 | 6.86 | 0.009 |
| Work/School /Financial Effectiveness | 0.001 | 0.717 | 4.87 | 0.03 |
| Not having an HMO insurance plan | 0.001 | 0.717 | 4.62 | 0.03 |
| Male | 0.001 | 0.718 | 4.10 | 0.04 |
| Eating | 0.001 | 0.718 | 4.11 | 0.04 |
DISCUSSION
At 5 - 10 years after heart transplantation, recipients reported high levels of satisfaction with overall QOL and with health-related QOL that was stable over the 5 year period. These findings, which are similar to other studies of QOL1, 6, 28-30, suggest that patients are generally content with their lives long-term after heart transplantation. Predictors of satisfaction with QOL included a variety of biopsychosocial variables. At 5 - 10 years after transplantation, predictors of satisfaction with overall QOL (that individually accounted for 1% variance or more) were primarily psychosocial variables, while predictors of satisfaction with QOL related to health and functioning (that also explained ≥ 1% variance) included symptom distress and physical function, as well as psychosocial variables.
For both overall QOL and health / functioning QOL, the variable that explained the most variance in QOL was depression. Depression, one of the most common psychiatric conditions after heart transplantation, occurs most frequently early after heart transplantation, but new onset of depression continues to occur during the next several years post transplant31. Unfortunately, there are limited published data on depression more than 3 years post transplant. However, the body of literature documenting change over time in psychological symptoms (ex., mood disorders [including depression], anxiety, and somatic symptoms) after heart transplantation suggests that while psychological symptoms improve from before to after heart transplantation and decline over time early post transplant31, psychological symptom distress may actually increase long-term5, 8, 32, 33. Furthermore, we have previously reported that 19% of patients had clinically significant symptoms of depression at 5-6 years after heart transplantation34. Symptoms of depression, which are negatively related to quality of life, may be related to long-term complications of heart transplantation (ex., cardiac allograft vasculopathy) and co-morbidities (including renal dysfunction, diabetes, orthopedic problems, and malignancies). These limited data suggest the need to monitor patients for depression long-term after heart transplantation and refer for treatment as indicated. In addition, further research of depression long-term after heart transplantation is critical in order to move this important area of investigation forward.
Satisfaction with overall QOL was also strongly explained by social factors. Social interaction and being married were important variables that explained variance in overall QOL. Previous reports have generally demonstrated improvement in social functioning from before to after heart transplantation35-37 with continued improvement over time1, 5, 38. In addition, similar to our current findings, Barr et al.9 determined that being married is associated with better QOL.
Social support is an important factor when patients are listed for transplant and early after transplant. It is also important to understand whether social support is maintained or deteriorates over time. Satisfaction with social support as a predictor of satisfaction with QOL long-term after heart transplantation is a finding that has not been detected earlier after heart transplant. In our previous reports of predictors of QOL at 1 year39 and 5-6 years40 after heart transplantation, while univariate correlates between satisfaction with QOL and satisfaction with support were significant, satisfaction with support was not a multivariate predictor of QOL at either time period. An explanation of why social support was a significant predictor of QOL at 5 - 10 years after heart transplantation (and not earlier after transplant) is unclear. Perhaps social support variables were blocked by other psychological, physical, and symptom related variables that were more strongly related to satisfaction with overall QOL in the analyses at earlier time periods. Also, social support has been strongly associated with mood and anxiety disorders41, 42 earlier after heart transplantation. Thus, satisfaction with social support may be indirectly (ie., mediated through psychological distress) related to satisfaction with overall QOL early after transplant. Further study of social support both short-term and long-term after heart transplantation is warranted.
We also identified fatigue (which has both physical and psychological aspects) as an important variable that predicted satisfaction with overall QOL as well as satisfaction with health and functioning. Fatigue has been examined by other research teams after heart transplantation. Fatigue was correlated with worse QOL in the cross-sectional study by Rosenblum et al.3 at < 10 years after transplant. At both < 10 years43 and > 10 years2 after heart transplantation, researchers reported patient energy levels as comparable to the general population, while DeCampli et al.4 noted a trend toward lower energy levels in older patients (50-64 years) > 10 years post transplant as compared to an age-matched general population. One interesting study described moderately high levels of fatigue in women at > 1 year post heart transplantation44. In the same study, fatigue was further found to be correlated with older age and depression44. Given the complex nature of fatigue, assessment needs to include consideration of both physiological and psychological components with subsequent targeted recommendations for therapy.
Lastly, physical factors (ie., sleep / rest and body care / movement) and somatic sensation (ie., cardiopulmonary symptom distress) were strongly related to satisfaction with health and functioning at 5-10 years after heart transplantation. Sleep, mobility, and cardiopulmonary symptom distress have previously been reported to improve from before to after heart transplant35, 45 - 47. At 5-6 years after heart transplantation, disability related to body care / movement was low (mean score = 0.05 [0=no functional disability and 1=most functional disability])48. None-the-less, 46% of patients reported having some amount of functional disability in body care / movement48. At more than 10 years after heart transplantation, DeCampli et al.4 reported a trend toward lower mobility and sleep quality in older patients (50-64 years) as compared to an age-matched general population. Sleep was also an important predictor of satisfaction with QOL in our earlier report of QOL at 5-6 years after heart transplantation40. Thus, these physical factors and symptom distress require assessment and intervention, even long-term after heart transplantation.
Our study is limited by our assessment of QOL in heart transplant recipients who survived from 5 - 10 years after transplantation and were able and willing to answer our booklets of questionnaires. We enrolled 68% of eligible patients and retained 70% of patients in our study. The longitudinal study design, frequency of querying patients (ie., every 6 months), number of questionnaires, and moderately-large number of items per questionnaire may have reduced our retention of subjects. Thus, bias (resulting in underestimation or overestimation of QOL) may have been introduced when patients chose not to participate in our study of QOL outcomes or opted out of completing booklets of QOL questionnaires after study enrollment. In order to address and reduce the potential for bias, we have compared characteristics of patients who enrolled and did not enroll in our study, as well as determined reasons for non-completion of booklets after study enrollment. In addition, we had four research sites which were geographically diverse and thus increased the representativeness of our sample.
CONCLUSIONS
At 5 - 10 years after heart transplantation, QOL is positive and stable. Biopsychosocial variables predict satisfaction with overall QOL and health-related QOL. Understanding of these biopsychosocial variables (ex. depression, fatigue, and cardiopulmonary symptom distress) provides direction for development of therapeutic strategies long-term after heart transplantation, so that patients can experience good post transplant outcomes.
Acknowledgments
This research was funded by the NIH (National Institute of Nursing Research, R01 #NR005200); a grant-in-aid from the College of Nursing, Rush University; and intramural funding from the Rush Heart Institute, Rush University Medical Center.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Kathleen L. Grady, Northwestern Memorial Hospital, Chicago, IL.
David C. Naftel, University of Alabama Medical Center, Birmingham, AL.
Jon Kobashigawa, UCLA Medical Center, Los Angeles, CA.
Julie Chait, UCLA Medical Center, Los Angeles, CA.
James B. Young, The Cleveland Clinic Foundation, Cleveland, OH.
Dave Pelegrin, The Cleveland Clinic Foundation, Cleveland, OH.
Jennifer Czerr, The Cleveland Clinic Foundation, Cleveland, OH.
Alain Heroux, Loyola University Medical Center, Maywood, IL.
Robert Higgins, Rush University Medical Center, Chicago, IL.
Bruce Rybarczyk, Rush University Medical Center, Chicago, IL.
Mary McLeod, Rush University Medical Center, Chicago, IL.
Connie White-Williams, University of Alabama Medical Center, Birmingham, AL.
James K. Kirklin, University of Alabama Medical Center, Birmingham, AL.
References
- 1.Karam VH, Gasquet I, Delvart V, et al. Quality of life in adult survivors beyond 10 years after liver, kidney, and heart transplantation. Transplantation. 2003;76:1699–1704. doi: 10.1097/01.TP.0000092955.28529.1E. [DOI] [PubMed] [Google Scholar]
- 2.Politi P, Piccinelli M, Poli FP. Ten years of extended life: Quality of life among heart transplant survivors. Transplantation. 2004;78:257–63. doi: 10.1097/01.tp.0000133537.87951.f2. [DOI] [PubMed] [Google Scholar]
- 3.Rosenblum DS, Rosen ML, Pine AM, et al. Health status and quality of life following cardiac transplantation. Arch Phys Med Rehabil. 1993;74:490–3. doi: 10.1016/0003-9993(93)90111-m. [DOI] [PubMed] [Google Scholar]
- 4.DeCampli WM, Luikart H, Hunt S, et al. Characteristics of patients surviving more than ten years after cardiac transplantation. J Thorac Cardiovasc Surg. 1995;109:1103–15. doi: 10.1016/S0022-5223(95)70194-X. [DOI] [PubMed] [Google Scholar]
- 5.Hetzer R, Albert W, Hummel M, et al. Status of patients presently living 9 to 13 years after orthotopic heart transplantation. Ann Thorac Surg. 1997;64:1661–8. doi: 10.1016/s0003-4975(97)01091-6. [DOI] [PubMed] [Google Scholar]
- 6.Aravot D, Berman M, Ben-Gal T, et al. Functional status and quality of life of heart transplant recipients surviving beyond 5 years. Transplant Proc. 2000;32:731–2. doi: 10.1016/s0041-1345(00)00960-x. [DOI] [PubMed] [Google Scholar]
- 7.Salyer J, Flattery M, Joyner P, et al. Lifestyle and quality of life in long-term cardiac transplant recipients. J Heart Lung Transplant. 2003;22:309–21. doi: 10.1016/s1053-2498(02)00552-1. [DOI] [PubMed] [Google Scholar]
- 8.Bunzel B, Laederach-Hofmann K. Long-term effects of heart transplantation: The gap between physical performance and emotional well-being. Scand J Rehab Med. 1999;31:214–222. doi: 10.1080/003655099444380. [DOI] [PubMed] [Google Scholar]
- 9.Barr M, Schenkel FA, Van Kirk A, et al. Determinants of quality of life changes among long-term cardiac transplant survivors: Results from longitudinal data. J Heart Lung Transplant. 2003;22:1157–67. doi: 10.1016/s1053-2498(02)01224-x. [DOI] [PubMed] [Google Scholar]
- 10.Spilker B. Quality of life and pharmacoeconomics in clinical trials. 2. New York: Lippincott Williams & Wilkins; 1996. [Google Scholar]
- 11.Wilkinson G. Wide range achievement test. Wide Range Inc; Wilmington, DE: 1993. [Google Scholar]
- 12.Ferrans CE, Powers MJ. Quality of Life Index: Development and psychometric properties. Adv Nurs Sci. 1985;8:15–24. doi: 10.1097/00012272-198510000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Watson D, Clark LA. The PANAS-X: Preliminary manual for the positive and negative affect schedule-expanded form. Southern Methodist University; Dallas, TX: 1991. pp. 2–35. [Google Scholar]
- 14.Watson D. Intraindividual and interindividual analyses of positive and negative affect: Their relation to health, compliance, perceived stress, and daily activities. J Pers Soc Psychol. 1988;54:1020–30. doi: 10.1037//0022-3514.54.6.1020. [DOI] [PubMed] [Google Scholar]
- 15.Watson D. The viscitudes of mood measurement: Effects of varying descriptors, time frames, and response formats on measures of positive and negative affect. J Pers Soc Psychol. 1988;55:128–41. doi: 10.1037//0022-3514.55.1.128. [DOI] [PubMed] [Google Scholar]
- 16.Hare DL, Davis CR. Cardiac Depression Scale: Validation of a new depression scale for cardiac patients. J Psychosom Res. 1996;40(4):379–86. doi: 10.1016/0022-3999(95)00612-5. [DOI] [PubMed] [Google Scholar]
- 17.Bergner M, Bobbitt RA, Carter WB, et al. The Sickness Impact Profile: Development and final revision of a health status measure. Med Care. 1981;19:787–806. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Grady KL, Jalowiec A, White-Williams C, et al. Predictors of quality of life in patients with advanced heart failure awaiting transplantation. J Heart Lung Transplant. 1995;14:2–10. [PubMed] [Google Scholar]
- 19.Jalowiec A, Grady KL, White-Williams C. Symptom distress three months after heart transplantation. J Heart Transplant. 1997;16:604–14. [PubMed] [Google Scholar]
- 20.Jalowiec A, Grady KL, White-Williams C. Stressors in patients awaiting a heart transplant. Behav Med. 1994;19:145–54. doi: 10.1080/08964289.1994.9935185. [DOI] [PubMed] [Google Scholar]
- 21.Jalowiec A. The Jalowiec Coping Scale. In: Strickland OL, Dilorio C, editors. Measurement of nursing outcomes. 2. 3: Self care and coping. New York: Springer; 2003. pp. 71–87. [Google Scholar]
- 22.Grady KL, Jalowiec A, White-Williams C. Heart transplant candidates’ perception of helpfulness of health care provider interventions. Cardiovasc Nurs (AHA) 1993;29(5):33–7. [PubMed] [Google Scholar]
- 23.Ferans CE. Development of a Quality of Life Index for patients with cancer. Oncol Nurs Forum. 1990;17(Suppl 3):15–21. [PubMed] [Google Scholar]
- 24.Ferrans CE, Powers MJ. Psychometric assessment of the Quality of Life Index. Res Nurs Health. 1992;15:29–38. doi: 10.1002/nur.4770150106. [DOI] [PubMed] [Google Scholar]
- 25.Bergner M, Bobbitt RA, Pollard WE, Martin DP, Gilson BS. The Sickness Impact Profile: Validation of a health status measure. Med Care. 1976;14:57–67. doi: 10.1097/00005650-197601000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Pollard WE, Bobbitt RA, Bergner MB, Martin DP, Gilson GP. The Sickness Impact Profile: Reliability of a health status measure. Med Care. 1976;14:146–55. doi: 10.1097/00005650-197602000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Grady KL, Jalowiec A, Grusk BB, et al. Symptom distress in cardiac transplant candidates. Heart Lung. 1992;21(5):434–9. [PubMed] [Google Scholar]
- 28.Jones BM, Chang VP, Esmore D, et al. Psychological adjustment after cardiac transplantation. Med J Aust. 1988;149:118–22. doi: 10.5694/j.1326-5377.1988.tb120532.x. [DOI] [PubMed] [Google Scholar]
- 29.Jones BM, Taylor F, Downs K, Spratt P. Longitudinal study of quality of life and psychological adjustment after cardiac transplantation. Med J Aust. 1992;157:24–6. doi: 10.5694/j.1326-5377.1992.tb121602.x. [DOI] [PubMed] [Google Scholar]
- 30.Molzahn AE, Burton JR, McCormick P, et al. Quality of life of candidates for and recipients of heart transplants. Can J Cardiol. 1997;13(2):141–6. [PubMed] [Google Scholar]
- 31.Dew MA, DiMartini AF. Psychological disorders and distress after adult cardiothoracic transplantation. J Cardiovasc Nurs. 2005;20(5S):S51–66. doi: 10.1097/00005082-200509001-00007. [DOI] [PubMed] [Google Scholar]
- 32.Dobbels F, De Geest S, Martin S, et al. Prevalence and correlates of depression symptoms at 10 years after heart transplantation: Continuous attention required. Transplant Int. 2004;17:424–31. doi: 10.1007/s00147-004-0732-5. [DOI] [PubMed] [Google Scholar]
- 33.Evangelista LS, Doering LV, Dracup K, Vassilakis ME, Kobashigawa J. Hope, mood states and quality of life in female heart transplant recipients. J Heart Lung Transplant. 2003;22:681–6. doi: 10.1016/s1053-2498(02)00652-6. [DOI] [PubMed] [Google Scholar]
- 34.Rybarczyk B, Grady K, Naftel D, et al. Emotional adjustment five years after heart transplant: A multi-site study. Rehab Psychol. in press. [Google Scholar]
- 35.Grady KL, Jalowiec A, White-Williams C. Improvement in quality of life in patients with heart failure who undergo transplantation. J Heart Lung Transplant. 1996;15:749–57. [PubMed] [Google Scholar]
- 36.Bohachick P, Anton BB, Wooldridge PJ, et al. Psychosocial outcomes six months after heart transplant surgery: A preliminary report. Res Nurs Health. 1992;15:165–73. doi: 10.1002/nur.4770150303. [DOI] [PubMed] [Google Scholar]
- 37.Bunzel B, Grundbock A, Laczkovics A, et al. Quality of life after orthotopic heart transplantation. J Heart Lung Transplant. 1991;10:455–9. [PubMed] [Google Scholar]
- 38.Baumann LJ, Young CH, Egan JJ. Living with a heart transplant: Long-term adjustment. Transplant Int. 1992;5:1–8. doi: 10.1007/BF00337181. [DOI] [PubMed] [Google Scholar]
- 39.Grady KL, Jalowiec A, White-Williams C. Predictors of quality of life in patients at one year after heart transplantation. J Heart Lung Transplant. 1999;18:202–10. doi: 10.1016/s1053-2498(98)00048-5. [DOI] [PubMed] [Google Scholar]
- 40.Grady KL, Naftel DC, White-Williams C. Predictors of quality of life at 5 to 6 years after heart transplantation. J Heart Lung Transplant. 2005;24:1431–9. doi: 10.1016/j.healun.2004.08.012. [DOI] [PubMed] [Google Scholar]
- 41.Dew MA, Roth LH, Schulberg, et al. Prevalence and predictors of depression and anxiety-related disorders during the year after heart transplantation. Gen Hosp Psychiatry. 1996;18:48S–61S. doi: 10.1016/s0163-8343(96)00077-1. [DOI] [PubMed] [Google Scholar]
- 42.Dew MA, Kormos RL, DiMartini AF, et al. Prevalence and risk of depression and anxiety-related disorders during the first three years after heart transplantation. Psychosomatics. 2001;42:300–13. doi: 10.1176/appi.psy.42.4.300. [DOI] [PubMed] [Google Scholar]
- 43.Littlefield C, Abbey S, Fiducia D, et al. Quality of life following transplantation of the heart, liver, and lungs. Gen Hosp Psychiatry. 1996;18:36S–47S. doi: 10.1016/s0163-8343(96)00082-5. [DOI] [PubMed] [Google Scholar]
- 44.Reyes CJ, Evangelista LS, Doering L, et al. Physical and psychological attributes of fatigue in female heart transplant recipients. J Heart Lung Transplant. 2004;23:614–9. doi: 10.1016/S1053-2498(03)00310-3. [DOI] [PubMed] [Google Scholar]
- 45.Caine N, Sharples L, English T, et al. Prospective study comparing quality of life before and after heart transplantation. Transplant Proc. 1990;22:1437–9. [PubMed] [Google Scholar]
- 46.Fisher DC, Lake KD, Reutzel TJ, et al. Changes in health-related quality of life and depression in heart transplant recipients. J Heart Lung Transplant. 1995;14(2):373–81. [PubMed] [Google Scholar]
- 47.Butler JB, McCoin NS, Feurer ID, et al. Modeling the effects of functional performance and post-transplant comorbidities on health-related quality of life after heart transplantation. J Heart Lung Transplant. 2003;22:1149–56. doi: 10.1016/s1053-2498(02)01188-9. [DOI] [PubMed] [Google Scholar]
- 48.Grady KL, Naftel DC, Kirklin JK, et al. Predictors of physical functional disability at 5 to 6 years after heart transplantation. J Heart Lung Transplant. 2005;24:2279–85. doi: 10.1016/j.healun.2005.05.007. [DOI] [PubMed] [Google Scholar]


