Abstract
DAP12 (KARAP) is a transmembrane signaling adaptor for a family of innate immunoreceptors that have been shown to activate granulocytes and monocytes/macrophages, amplifying production of inflammatory cytokines. Contrasting with these data, recent studies suggest that DAP12 signaling has an inhibitory role in the macrophage response to microbial products (Hamerman, J.A., N.K. Tchao, C.A. Lowell, and L.L. Lanier. 2005. Nat. Immunol. 6:579–586). To determine the in vivo role for DAP12 signaling in inflammation, we measured the response of wild-type (WT) and DAP12−/− mice to septic shock. We show that DAP12−/− mice have improved survival from both endotoxemia and cecal ligation and puncture–induced septic shock. As compared with WT mice, DAP12−/− mice have decreased plasma cytokine levels and a decreased acute phase response during sepsis, but no defect in the recruitment of cells or bacterial control. In cells isolated after sepsis and stimulated ex vivo, DAP12 signaling augments lipopolysaccharide-mediated cytokine production. These data demonstrate that, during sepsis, DAP12 signaling augments the response to microbial products, amplifying inflammation and contributing to mortality.
DAP12 (KARAP) is a transmembrane signaling adaptor associated with a family of activating immunoreceptors, including the KIRs, Ly49s, NKG2C/E, TREMs, SIRP-β1, CD200R, MDL-1, and others (1–4). These receptors are expressed on the surface of NK cells and myeloid cells, including macrophages, granulocytes, dendritic cells, osteoclasts, and microglia. DAP12 contains cytoplasmic immunoreceptor tyrosine-based activation motifs (ITAMs; references 1–3). Engagement of a DAP12-associated receptor induces tyrosine phosphorylation of the ITAM by Src kinases. The phosphorylated ITAM recruits the protein tyrosine kinases Syk and ZAP70, triggering phosphorylation of multiple downstream mediators, including PI-3K, PLC-γ, c-Cbl, Grb-2, and Vav, that ultimately lead to cellular activation (1–3, 5).
We previously showed that antibody ligation of the DAP12-associated receptor TREM-1 on granulocytes and monocytes induces release of the inflammatory cytokines TNF-α and IL-8 (6). In vivo, blockade of the DAP12-associated receptor TREM-1 was associated with reduced inflammation and increased survival from endotoxemia or septic peritonitis (7). These observations suggest a role for DAP12 and at least one of its associated receptors in the amplification of the inflammatory response induced by pathogens and their components. Consistent with this, DAP12 transgenic mice exhibited increased systemic inflammation and mortality during endotoxemia (8). Moreover, overexpression of DAP12 increased hepatic granulomatous inflammation elicited by zymosan A, whereas blockade of TREM-1 reduced granuloma formation (9).
In contrast to the established role for DAP12 in activating inflammatory responses, experiments with DAP12-deficient macrophages found no defect in TNF-α or nitric oxide production after ex vivo stimulation of peritoneal macrophages with LPS, suggesting that these cells have no intrinsic defect in the response to microbial products (10). Moreover, Hamerman et al. (11) have recently reported that macrophages derived from DAP12-deficient mice have an increased response to low concentrations of microbial products and that DAP12−/− mice are more sensitive to LPS after pretreatment with the TNF-α–sensitizing reagent d-galactosamine than are WT mice. Collectively, these results suggest an inhibitory role for DAP12 in regulating the inflammatory response and conflict with the described role of DAP12 in activating myeloid cells and previous data implicating the DAP12-associated receptor TREM-1 in exacerbating inflammation, endotoxemia, and septic shock.
To address this conflict, we sought to understand the function of DAP12 in physiologically relevant models of inflammation. To this end, we measured the contribution of DAP12 to septic shock induced by endotoxemia and cecal ligation and puncture (CLP).
Results and Discussion
DAP12 signaling contributes to inflammation and mortality from endotoxemia
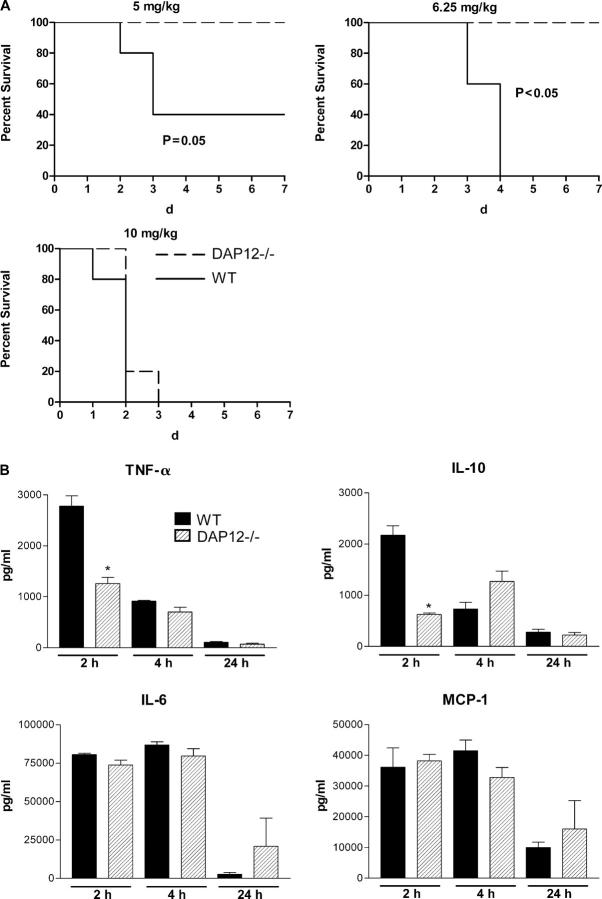
To determine if DAP12 contributed to the in vivo response to endotoxin, we subjected WT and DAP12−/− mice to i.p. injections of LPS and monitored them for survival. DAP12-deficient mice tolerated doses of 5 and 6.25 mg/kg of endotoxin, which resulted in 60–100% mortality in WT mice (Fig. 1 A). However, DAP12-deficient mice were not completely refractory to endotoxin and died at a dose of 10 mg/kg (Fig. 1 A). Thus, DAP12 signaling contributes to endotoxemia, although it is not required for the response to LPS.
Figure 1.
DAP12 signaling augments mortality and inflammatory cytokine levels during endotoxemia. (A) Survival of WT and DAP12−/− mice after endotoxemia was measured at three different doses: 5, 6.25, and 10 mg/kg (n = 5 for all doses). At both 5 and 6.25 mg/kg, DAP12−/− mice had improved survival as compared with WT mice (P ≤ 0.05 by the log-rank test). At 10 mg/kg, both strains died. (B) Plasma was harvested from WT and DAP12−/− mice 2 (n = 5–6), 4 (n = 3), or 24 (n = 3) h after injection of 5 mg/kg LPS. At 2 h, WT mice had increased levels of TNF-α and IL-10 (*, P < 0.05 vs. WT by the Mann-Whitney test).
Endotoxin causes shock by inducing macrophage production of TNF-α and other proinflammatory cytokines (12). To determine if DAP12 signaling exacerbated endotoxemia by increasing cytokine production, we measured cytokine levels in mice treated with 5 mg/kg of endotoxin. It has been shown that inflammatory cytokine levels peak after 1–3 h of endotoxemia infection (12). We found that 2 h after injection of LPS, both WT and DAP12−/− mice had elevated circulating levels of TNF-α, IL-6, MCP-1, and IL-10. When compared with DAP12−/− mice, WT animals had significantly higher levels of TNF-α and IL-10. By 4 h, TNF-α and IL-10 were reduced in WT mice, and the levels were equal to the DAP12−/− animals (P < 0.05; Fig. 1 B). We conclude that DAP12 signaling can augment inflammatory cytokine production acutely.
Mortality and inflammation from septic peritonitis is augmented by DAP12
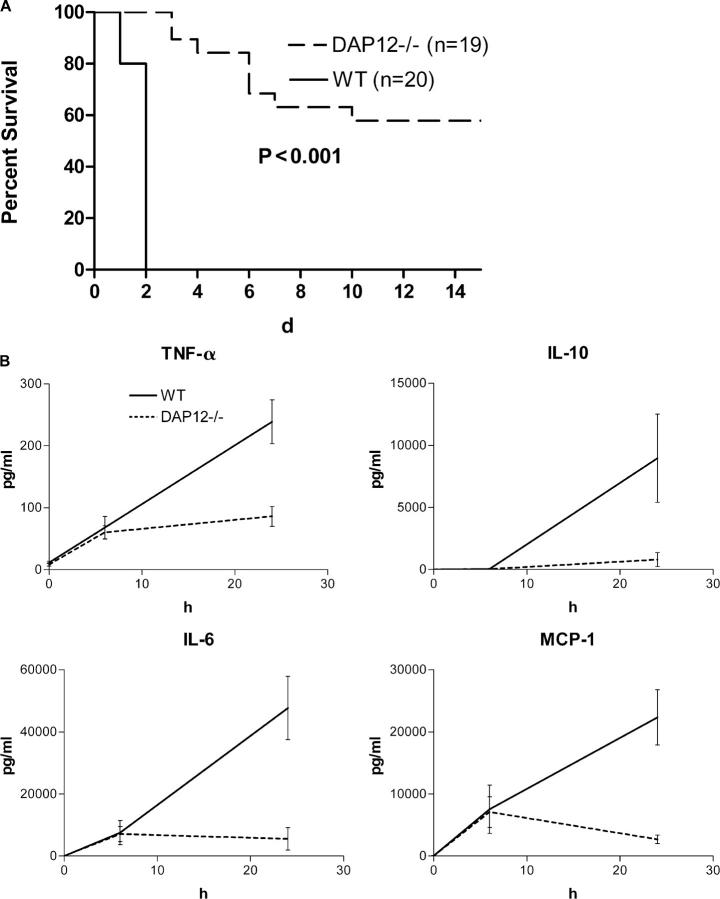
Although mortality from endotoxin is mediated by inflammation and overproduction of cytokines, surviving authentic sepsis requires attenuating the inflammatory response, as well as achieving bacterial control (13). To determine the role of DAP12 in survival of sepsis, we subjected WT and DAP12-deficient mice to CLP, a clinically relevant model of bacterial peritonitis. We found that DAP12−/− mice were highly resistant to CLP (WT, n = 20, 0% survival; DAP12−/−, n = 19, 60% survival; Fig. 2 A).
Figure 2.
DAP12 signaling augments mortality and inflammatory cytokine levels during bacterial sepsis. WT and DAP12−/− mice were subjected to CLP, and survival (A) and cytokine production (B) were assessed. DAP12−/− mice (n = 19) are resistant to CLP as compared with WT mice (n = 20; P < 0.001 by the log-rank test). Plasma was harvested from WT or DAP12−/− mice before CLP (n = 5) and either 6 (n = 6) or 24 (n = 12–15) h after CLP, and cytokine levels were measured. At 6 h, we found elevated but equal levels of MCP-1, IL-6, and TNF-α in WT and DAP12−/− mice. By 24 h, WT mice had significantly higher levels of MCP-1, IL-6, TNF-α, and IL-10 (P < 0.05 by the Mann-Whitney test). Values shown are SEM.
Sepsis is associated with high circulating cytokine levels that contribute to shock (13). To determine if DAP12 contributed to cytokine production during sepsis, we measured cytokine levels in the plasma of WT and DAP12-deficient mice 6 and 24 h after CLP. At 6 h, WT and DAP12−/− mice had measurable plasma levels of IL-6, MCP-1, and TNF-α, but there was no difference between the two groups. Between 6 and 24 h, WT plasma cytokine levels had increased dramatically such that by 24 h after the onset of sepsis, the WT mice had significantly higher levels of IL-6, MCP-1, TNF-α, and IL-10 than did DAP12−/− mice (P < 0.05; Fig. 2 B). These data demonstrate that DAP12 signaling contributes to cytokine production during sepsis.
To determine if there were other DAP12-regulated factors mediating the increased sepsis mortality of WT mice as compared with DAP12−/− animals, we examined plasma proteins from these mice using two-dimensional difference gel electrophoresis (14). Plasma was isolated from WT and DAP12−/− mice 24 h after CLP, and plasma proteins were resolved by isoelectric point and size. Relative abundance of the individual gel features was compared between the two genotypes, and features that were substantially different in four independent experiments were isolated and identified by mass spectrometry. We identified seven differentially regulated proteins in 13 gel features (some proteins are represented by multiple gel features). Data are expressed as the fold change in average florescence of DAP12−/− versus WT (Table I). The proteins identified in this unbiased approach were previously described as acute phase reactants (15–20). Positive acute phase proteins (proteins known to increase in response to inflammation, i.e., apolipoprotein A-IV [15], hemopexin [16], and complement component 3 [16]) accounted for three out of seven identified proteins. Negative acute phase proteins (those known to decrease with inflammation) accounted for four out of seven proteins: major urinary protein (17), antithrombin III (18), gelsolin (19), and MHC Q10 (20). For every individual protein, the acute phase response was attenuated in DAP12−/− mice. This was manifest as lower levels of positive acute phase proteins and higher levels of negative acute phase proteins. Collectively, these data show reduced plasma cytokine levels and a reduced acute phase response in DAP12−/− mice, demonstrating a role for DAP12 in triggering inflammation.
Table I.
Differential plasma proteins induced by sepsis in DAP12−/− versus WT mice
| Differentially represented plasma proteins |
Fold change | p-value |
|---|---|---|
| Positive acute phase reactants | ||
| Apolipoprotein A-IV | −1.56 | 0.05 |
| Hemopexin | −3.68 | 0.024 |
| Complement component 3 | −3.17 | 0.0005 |
| Negative acute phase reactants | ||
| Antithrombin | 1.69 | 0.0047 |
| Gelsolin | 1.72 | 0.0018 |
| Major urinary protein | 3.49 | 0.006 |
| MHC Q10 α chain | 2.13 | 0.04 |
Proteomic analysis of plasma from DAP12−/− and WT mice 24 h after CLP identified seven differentially regulated proteins. Identified proteins were previously described as acute phase reactants (15–20), demonstrating a role for DAP12 in inducing the acute phase response during sepsis. Mean fluorescence intensity was compared using the Student's t test. Data are expressed as the fold change of DAP12−/− versus WT.
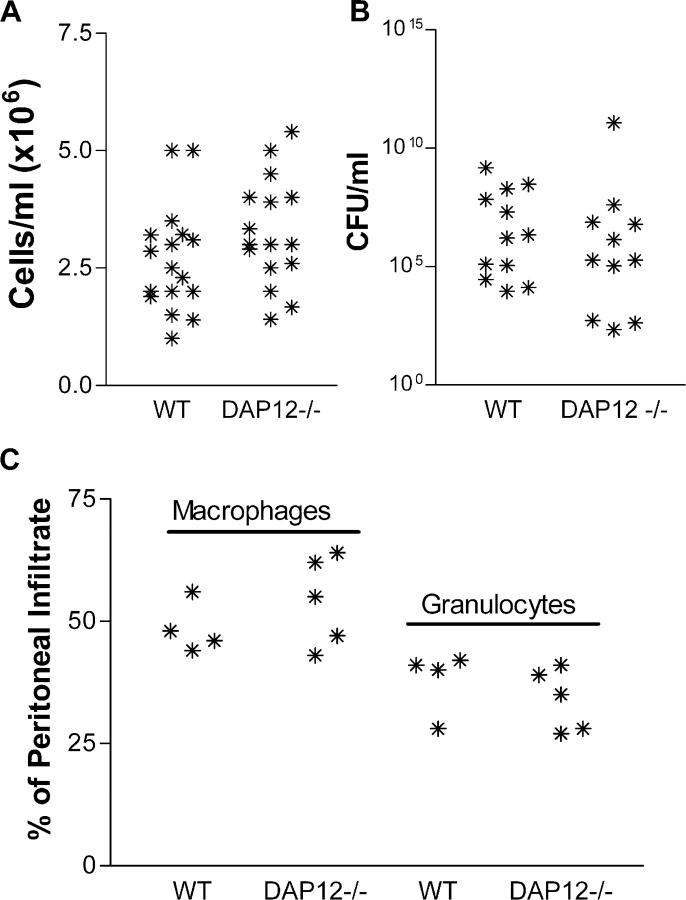
DAP12 is not required for recruitment of cells or bacterial killing
We hypothesized that the absence of DAP12 could also result in a decreased cellular response to peritonitis. To address this question, we measured the number and type of cells recruited to the peritoneum during sepsis. We found equal numbers of cells in the peritoneum of WT and DAP12−/− mice 24 h after the onset of sepsis (Fig. 3 A). By analyzing surface markers on these cells, we found that in both WT and DAP12−/− mice, 50–60% of the cells were macrophages (defined as CD11b+GR1lo) and 30–40% were granulocytes (defined as CD11b+GR1hi; Fig. 3 C). The absence of DAP12 does not appear to alter the recruitment of cells to the peritoneum during sepsis. We also asked if there was a deficit in bacterial control in the absence of DAP12 signaling. To determine if DAP12 mediates bacterial control, we measured bacterial load in the peritoneum at 24 h. We found no remarkable difference in peritoneal infection between WT and DAP12−/− mice (Fig. 3 B), demonstrating that DAP12 is not required to control the peritoneal infection during sepsis.
Figure 3.
DAP12 signaling does not contribute to cellular recruitment or bactericidal activity. 24 h after CLP, peritoneal exudate was harvested by peritoneal lavage. Total cell numbers (A; n = 16–17), bacterial load (B; n = 11–12), and distribution of cell types (C; n = 4–5) were measured. We found no difference between WT and DAP12−/− mice. Each asterisk represents a measurement for a single mouse.
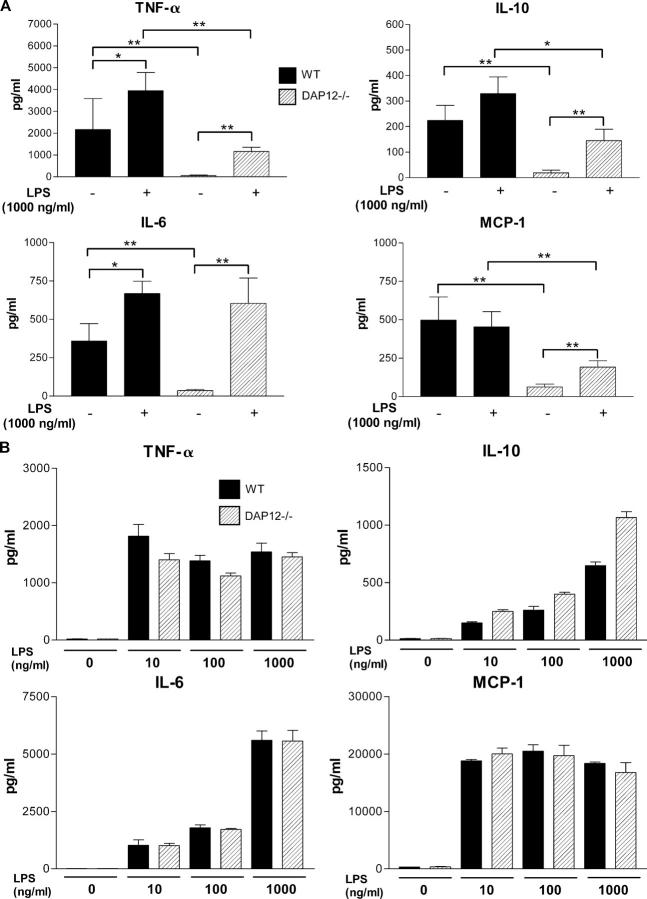
DAP12 signaling augments in vitro cytokine production of peritoneal macrophages obtained from septic mice
Although our observations indicate that in vivo DAP12 signaling augments cytokine production, previously published data demonstrated that there is no defect in ex vivo macrophage activation in the absence of DAP12 (10). To address this apparent discrepancy, we measured cytokine production by peritoneal exudate cells induced by sepsis. Peritoneal cells were isolated by peritoneal lavage and tested for their ability to produce cytokines ex vivo either without or with LPS stimulation. We found that cells isolated from the peritoneum of both WT and DAP12−/− mice after CLP produced cytokines in the absence of any additional stimulation (Fig. 4 A). However, cells isolated from WT mice produced more MCP-1, TNF-α, and IL-10 as compared with cells isolated from DAP12−/− mice. Although the cells are cultured in the presence of antibiotics, we cannot determine if this cytokine secretion reflects stimulation by bacterial products carried over from the frankly septic peritoneal lavage fluid or if this cytokine production reflects activation induced by previous stimulation in vivo. To normalize the stimulation via Toll-like receptors (TLRs) and to exclude the possibility of differential carryover of microbial products, we treated the cells with 1 μg/ml LPS, which resulted in maximal stimulation and increased cytokine production by WT and DAP12−/− cells. Under these conditions, we found that WT cells were always considerably more efficient at cytokine production than DAP12−/− cells (Fig. 4 A). Remarkably, when we examined ex vivo cytokine production by thioglycollate-elicited peritoneal exudate cells from WT and DAP12−/− mice, we found no statistically significant differences in IL-10, IL-6, MCP-1, or TNF-α (Fig. 4 B), whereas there was a trend toward an increase in IL-10 production by DAP12−/− cells. We conclude that DAP12 signaling augments cytokine production only in macrophages stimulated in vivo by septic peritonitis.
Figure 4.
DAP12 signaling augments ex vivo cytokine production by macrophages after sepsis but not sterile peritonitis. WT and DAP12−/− mice were subjected to CLP, and peritoneal cells were harvested after 24 h (n = 8–12). (A) Cells were cultured ex vivo with or without stimulation with 1 μg/ml LPS, and levels of cytokine in the supernatant were measured. With no stimulation, WT cells (black bars) produced more IL-6, MCP-1, TNF-α, and IL-10 as compared with DAP12−/− cells (hatched bars; *, P < 0.05; **, P < 0.01 by the Mann-Whitney test). After LPS stimulation, WT cells produced increased amounts of TNF-α, MCP-1, and IL-10. (B) Cells were also harvested 72 h after i.p. injection of thioglycollate broth and cultured ex vivo with (10, 100, or 1,000 ng/ml) or without LPS (n = 3 for all cultures). There was no statistically significant difference between WT and DAP12−/− cells, although there was a trend toward increased IL-10 by the DAP12−/− cells with maximal stimulation. Values shown are SEM.
Concluding remarks
Our data show that DAP12 augments the inflammatory response induced by endotoxemia or authentic sepsis by four measures: increasing circulating cytokine levels, increasing the acute phase response, augmenting cellular inflammatory cytokine production, and, ultimately, increasing mortality. These data are consistent with the previously described role for the DAP12-associated receptor TREM-1 in septic shock (7) and support a physiologic function of DAP12 in activating granulocytes and/or macrophages.
Hamerman et al. (11) have recently shown that bone marrow–derived macrophages derived from DAP12-deficient mice are hyperresponsive to TLR ligands and produce increased amounts of TNF-α in response to low levels of TLR stimulation. Moreover, these authors show that DAP12-deficient mice are more susceptible than WT animals to endotoxin after the mice have been treated with the TNF-α sensitizing agent galactosamine (11). d-galactosamine treatment sensitizes mice to TNF-α by blocking hepatic protein synthesis, and galactosamine-induced mortality can be prevented by strategies that neutralize TNF-α (21). These data suggest that DAP12 inhibits activation of macrophages and/or granulocytes, at least in the presence of low levels of TLR stimulation. However, the relevance of this model to clinical sepsis (or the physiologic response to bacterial infection) is unclear because the mortality in this model occurs within 12 h. This contrasts with the models of septic shock that we use (simple endotoxemia and CLP), which more adequately recapitulate the clinical situation where mortality occurs over multiple days.
The discrepancy between our results and those of Hamerman et al. may be explained by the differential pathogenesis of the two models. Mortality by endotoxemia after d-galactosamine treatment is mediated by TNF-α (21), and death occurs within 12 h of injection with LPS. TNF-α also contributes mortality from simple endotoxemia, but other factors, including IL-1 (22), HMGB-1 (23), and MIF (24), participate in endotoxemic death; moreover, death after simple endotoxemia occurs over 3–5 d (13). Therefore, it is possible that high concentrations of LPS, elevated inflammatory cytokines, and an extended time course of inflammation in simple endotoxemia may induce the expression of high affinity DAP12-associated receptor–ligand pairs that can synergize with TLR-mediated pathways to drive cytokine production as described for ligation of TREM-1 on macrophages or granulocytes (6). Consistent with this hypothesis, we have previously shown that microbial products induce expression of TREM-1 (6). In the d-galactosamine model, the low levels of LPS and the reduced time course of disease may induce only low affinity DAP12-associated receptor–ligand interactions. As a result, DAP12 may preferentially recruit inhibitory mediators, including c-Cbl, or other undescribed mediators, leading to an alternative signaling pathway analogous to that induced by ligation of FcRγ (25). This alternative activation could modulate or antagonize TLR-mediated signaling.
These differential roles of DAP12 signaling may allow for “fine tuning” of the cellular response to infection in vivo. The range of endotoxin levels tested by Hamerman et al. ex vivo correlates with circulating plasma LPS levels in both mouse (26) and human sepsis (27). In contrast, LPS levels at the site of infection can be dramatically higher. For example, peritoneal LPS levels after CLP can range to 20 ng/ml (26), past the range for an inhibitory function of DAP12. Thus, even though low LPS concentrations distal to the site of infection may prevent unnecessary DAP12-mediated inflammation, at the nidus of infection, in the presence of high concentrations of LPS, DAP12 may become completely activated and synergize the TLR to mediate cytokine production.
Materials and Methods
Mice
DAP12−/− mice (28) were backcrossed onto the C57BL/6 background. The genetic background was analyzed by simple sequence length polymorphism typing, and the colony was expanded after >99% of the genome was derived from the C57BL/6 strain. WT C57BL/6 controls were purchased from Taconic Labs. All studies were approved by the Washington University School of Medicine Animal Studies Committee.
CLP and endotoxemia
Sepsis was induced by CLP. Mice were anesthetized with 2.5% halothane, and the cecum was exteriorized through an abdominal incision. The cecum was ligated distal to the ileocecal valve and punctured twice with a 25-gauge needle. The cecum was replaced, the abdomen was closed with 4–0 silk sutures, and the mice were given 1.0 ml of normal saline s.c. for volume resuscitation. Endotoxemia was induced by i.p. injection of LPS (Salmonella abortus equi; Sigma-Aldrich), dissolved in 0.2 ml PBS, at the dose indicated in the figures.
Peritoneal cell isolation and characterization
Peritoneal cells were isolated by peritoneal lavage with 3 × 5 ml PBS. Cells were washed twice with 10 ml of normal saline and were resuspended in RPMI 1640 with 10% FCS, 2 mM glutamine, 100 μg/ml kanamycin, 1 mM Na-pyruvate, and 100 μg/ml of nonessential amino acids. Sterile peritonitis was induced by i.p. injecting 1.5 ml of thioglycollate media, and cells were harvested 72 h after the insult. To determine the total number of peritoneal cells, peritoneal fluid was diluted 1:10 in 3% acetic acid to lyse erythrocytes, and nucleated cells were enumerated on a hemocytometer. Cell differential in the peritoneal fluid was determined by flow cytometry. Peritoneal cells were stained with anti-CD11b–FITC (BD Biosciences) and anti-GR1–PE (BD Biosciences) for 20 min on ice. Cells were washed twice and acquired on a flow cytometer (FACSCalibur; BD Biosciences. Macrophages were defined as CD11b+/GR1lo; granulocytes were defined as CD11b+/GR1hi. For ex vivo cytokine production, peritoneal cells were isolated by peritoneal lavage and cultured overnight in the presence of LPS at the concentrations indicated in the figures. To determine bacterial load in the peritoneal fluid, 100 μl of peritoneal fluid was serially diluted 1:10 in sterile PBS and was plated on sheep's blood agar plates. Colonies were counted after overnight incubation at 37°C.
Cytokine determination
Cytokines were measured using a cytometric bead array Mouse Inflammation Kit (552364; BD Biosciences) according to the manufacturer's recommendations. Samples were acquired on a flow cytometer.
Proteomic analysis of plasma
Sample preparation.
Immunoglobulins were removed using protein A affinity chromatography (ProSep A; Millipore), and the resultant material was desalted by gel filtration chromatography. Protein concentrations were determined using a modified Lowry method (PlusOne 2-D Quant; GE Healthcare). A pooled internal standard was prepared, comprising equal amounts of each of the 10 experimental samples. Protein samples were labeled with charge-matched cyanine dyes (GE Healthcare) as previously described (14). Equal protein loading of WT plasma, DAP12−/− plasma, and the 10-sample pool was based on protein assay results. Each of the five pairs of WT and DAP12−/− samples were combined with 50 μl of the pooled internal standard and were diluted by the addition of 300 μl of rehydration buffer (7 M urea/2 M thiourea, 4% CHAPS, and 0.5% vol/vol ampholytes, pH 3–10).
Two-dimensional gel electrophoresis and imaging
Labeled proteins were separated in two dimensions. In brief, each combined sample (450 μl final volume) was rehydrated into a 24- cm, 3–10 nonlinear immobilized pH gradient (IPG) strip (GE Healthcare), using a three-step voltage protocol: 500 V, held for 500 V hours (Vh); 1,000 V, held for 1,000 Vh; and 8,000 V, held for 64,000 Vh. After focusing, proteins were reduced and alkylated by placing the IPG strips in 10 ml of equilibration buffer (50 mM Tris, pH 8.8, 6 M urea, 30% glycerol, 2% SDS, and bromphenol blue) containing 50 mg of freshly prepared dithiothreitol for 15 min at room temperature, followed by adding 600 mg iodoacetamide in 10 ml of equilibration buffer. IPG strips were then rinsed with 1× SDS running buffer (25 mM Tris, 192 mM glycine, and 0.1% SDS) and layered on 10% polyacrylamide gels and sealed with agarose (1% wt/vol in 1× running buffer). Second-dimension SDS-PAGE separation was performed on all five gels simultaneously using 5 W/gel for the first 15 min, followed by 1 W/gel for 17 h with circulating buffer (20°C) in the lower buffer chamber. The labeled-pool, WT, and DAP12−/− proteins in each gel were individually imaged using specific excitation/emission wavelengths for each dye (Cy2, 488/520; Cy3, 520/580; Cy5, 620/670) using an imager (Typhoon; GE Healthcare).
Gel image analysis.
The DeCyder Differential In-gel Analysis software module (GE Healthcare) was used for “within-gel” image analysis for all sham/CLP samples as previously described (29). The DeCyder Biological Variation Analysis (BVA) module was then used to match all 15 protein-spot maps from the five gels using the Cy2 (pool) image. Those gel features matched by the software were manually inspected for accuracy and corrected. Images of plasma from replicate samples were grouped within BVA, and differentially expressed proteins were defined as those gel features with a value of P < 0.05 using an unpaired student's t test for the comparison of WT with DAP12−/−.
Gel feature processing.
Gel features were selected for excision in the DeCyder software. The 1.8-mm central cores of the selected gel features were excised robotically (ProPic; Genomic Solutions) and transferred to a 96-well source plate. The gel pieces were digested in situ with trypsin (Promega) as previously described (30). A 0.5-μl aliquot of each digest was removed and mixed with a matrix solution of 0.5 μl α-cyano-hydroxycinnamic acid (Premix; Agilent Technologies). The mixture was spotted on a stainless steel target for matrix-assisted laser desorption ionization (MALDI) mass spectrometry.
Protein identification by mass spectrometry.
Spectra of the peptide pools were obtained on a MALDI-TOF/TOF instrument (ABI4700; Applied Biosystems). MALDI mass spectra (∼100) were acquired for each digest and internally calibrated using trypsin autolysis peaks, and the top seven most abundant signals (within m/z 900–2,000) were automatically selected for tandem analysis. Precursor masses corresponding to a list of contaminant masses commonly observed in this laboratory were excluded from the list of precursor masses for tandem analysis. The peptide fragmentation spectra were processed using Data Explorer (version 4.5; Applied Biosystems). After centroiding and background subtraction, the spectra were used to search the National Center for Biotechnology Information nonredundant database using MASCOT (version 1.9; Matrix Sciences).
Statistical analysis
Statistical analysis was performed with GraphPad Prism software (GraphPad). All cytokine determinations were compared by the nonparametric Mann-Whitney test. All survival curves were compared by the log-rank test.
Acknowledgments
We would like to thank Drs. Susan Gilfillan and Marina Cella for providing expert advice and direction in the execution of these studies. We thank Dr. Emil R. Unanue for reading the manuscript.
This work was supported in part by a training grant (T32 GM 08795) from the National Institute of General Medical Sciences (to J.E. McDunn), by institutional resources provided by Washington University to the Proteomics Center (to R.R. Townsend), and by a grant (P41 RR 00954) from the National Centers of Research Resources of the National Institutes of Health.
The authors have no conflicting financial interests.
References
- 1.Vivier, E., J.A. Nunes, and F. Vely. 2004. Natural killer cell signaling pathways. Science. 306:1517–1519. [DOI] [PubMed] [Google Scholar]
- 2.Lanier, L.L., and A.B. Bakker. 2000. The ITAM-bearing transmembrane adaptor DAP12 in lymphoid and myeloid cell function. Immunol. Today. 21:611–614. [DOI] [PubMed] [Google Scholar]
- 3.Barclay, A.N., G.J. Wright, G. Brooke, and M.H. Brown. 2002. CD200 and membrane protein interactions in the control of myeloid cells. Trends Immunol. 23:285–290. [DOI] [PubMed] [Google Scholar]
- 4.Taylor, P.R., L. Martinez-Pomares, M. Stacey, H.H. Lin, G.D. Brown, and S. Gordon. 2005. Macrophage receptors and immune recognition. Annu. Rev. Immunol. 23:901–944. [DOI] [PubMed] [Google Scholar]
- 5.McVicar, D.W., and D.N. Burshtyn. 2001. Intracellular signaling by the killer immunoglobulin-like receptors and Ly49. Sci. STKE. 2001:RE1. [DOI] [PubMed]
- 6.Bouchon, A., J. Dietrich, and M. Colonna. 2000. Cutting edge: inflammatory responses can be triggered by TREM-1, a novel receptor expressed on neutrophils and monocytes. J. Immunol. 164:4991–4995. [DOI] [PubMed] [Google Scholar]
- 7.Bouchon, A., F. Facchetti, M.A. Weigand, and M. Colonna. 2001. TREM-1 amplifies inflammation and is a crucial mediator of septic shock. Nature. 410:1103–1107. [DOI] [PubMed] [Google Scholar]
- 8.Lucas, M., L. Daniel, E. Tomasello, S. Guia, N. Horschowski, N. Aoki, D. Figarella-Branger, S. Gomez, and E. Vivier. 2002. Massive inflammatory syndrome and lymphocytic immunodeficiency in KARAP/DAP12-transgenic mice. Eur. J. Immunol. 32:2653–2663. [DOI] [PubMed] [Google Scholar]
- 9.Nochi, H., N. Aoki, K. Oikawa, M. Yanai, Y. Takiyama, Y. Atsuta, H. Kobayashi, K. Sato, M. Tateno, T. Matsuno, et al. 2003. Modulation of hepatic granulomatous responses by transgene expression of DAP12 or TREM-1-Ig molecules. Am. J. Pathol. 162:1191–1201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bakker, A.B., R.M. Hoek, A. Cerwenka, B. Blom, L. Lucian, T. McNeil, R. Murray, L.H. Phillips, J.D. Sedgwick, and L.L. Lanier. 2000. DAP12-deficient mice fail to develop autoimmunity due to impaired antigen priming. Immunity. 13:345–353. [DOI] [PubMed] [Google Scholar]
- 11.Hamerman, J.A., N.K. Tchao, C.A. Lowell, and L.L. Lanier. 2005. Enhanced Toll-like receptor responses in the absence of signaling adaptor DAP12. Nat. Immunol. 6:579–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beutler, B.A., I.W. Milsark, and A. Cerami. 1985. Cachectin/tumor necrosis factor: production, distribution, and metabolic fate in vivo. J. Immunol. 135:3972–3977. [PubMed] [Google Scholar]
- 13.Remick, D.G., D.E. Newcomb, G.L. Bolgos, and D.R. Call. 2000. Comparison of the mortality and inflammatory response of two models of sepsis: lipopolysaccharide vs. cecal ligation and puncture. Shock. 13:110–116. [DOI] [PubMed] [Google Scholar]
- 14.Unlu, M., M.E. Morgan, and J.S. Minden. 1997. Difference gel electrophoresis: a single gel method for detecting changes in protein extracts. Electrophoresis. 18:2071–2077. [DOI] [PubMed] [Google Scholar]
- 15.Tu, G.F., F. De Jong, J. Apostolopoulos, M. Nagashima, N. Fidge, G. Schreiber, and G. Howlett. 1987. Effect of acute inflammation on rat apolipoprotein mRNA levels. Inflammation. 11:241–251. [DOI] [PubMed] [Google Scholar]
- 16.Gabay, C., and I. Kushner. 1999. Acute-phase proteins and other systemic responses to inflammation. N. Engl. J. Med. 340:448–454. [DOI] [PubMed] [Google Scholar]
- 17.Gervois, P., R. Kleemann, A. Pilon, F. Percevault, W. Koenig, B. Staels, and T. Kooistra. 2004. Global suppression of IL-6-induced acute phase response gene expression after chronic in vivo treatment with the peroxisome proliferator-activated receptor-alpha activator fenofibrate. J. Biol. Chem. 279:16154–16160. [DOI] [PubMed] [Google Scholar]
- 18.Niessen, R.W., R.J. Lamping, P.M. Jansen, M.H. Prins, M. Peters, F.B. Taylor Jr., J.J. de Vijlder, J.W. ten Cate, C.E. Hack, and A. Sturk. 1997. Antithrombin acts as a negative acute phase protein as established with studies on HepG2 cells and in baboons. Thromb. Haemost. 78:1088–1092. [PubMed] [Google Scholar]
- 19.Mounzer, K.C., M. Moncure, Y.R. Smith, and M.J. Dinubile. 1999. Relationship of admission plasma gelsolin levels to clinical outcomes in patients after major trauma. Am. J. Respir. Crit. Care Med. 160:1673–1681. [DOI] [PubMed] [Google Scholar]
- 20.Lew, A.M., W.L. Maloy, and J.E. Coligan. 1986. Characteristics of the expression of the murine soluble class I molecule (Q10). J. Immunol. 136:254–258. [PubMed] [Google Scholar]
- 21.Silverstein, R. 2004. D-galactosamine lethality model: scope and limitations. J. Endotoxin Res. 10:147–162. [DOI] [PubMed] [Google Scholar]
- 22.Alexander, H.R., G.M. Doherty, C.M. Buresh, D.J. Venzon, and J.A. Norton. 1991. A recombinant human receptor antagonist to interleukin 1 improves survival after lethal endotoxemia in mice. J. Exp. Med. 173:1029–1032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang, H., O. Bloom, M. Zhang, J.M. Vishnubhakat, M. Ombrellino, J. Che, A. Frazier, H. Yang, S. Ivanova, L. Borovikova, et al. 1999. HMG-1 as a late mediator of endotoxin lethality in mice. Science. 285:248–251. [DOI] [PubMed] [Google Scholar]
- 24.Calandra, T., B. Echtenacher, D.L. Roy, J. Pugin, C.N. Metz, L. Hultner, D. Heumann, D. Mannel, R. Bucala, and M.P. Glauser. 2000. Protection from septic shock by neutralization of macrophage migration inhibitory factor. Nat. Med. 6:164–170. [DOI] [PubMed] [Google Scholar]
- 25.Mosser, D.M. 2003. The many faces of macrophage activation. J. Leukoc. Biol. 73:209–212. [DOI] [PubMed] [Google Scholar]
- 26.Opal, S.M., J.E. Palardy, N.A. Parejo, and A.A. Creasey. 2001. The activity of tissue factor pathway inhibitor in experimental models of superantigen-induced shock and polymicrobial intra-abdominal sepsis. Crit. Care Med. 29:13–17. [DOI] [PubMed] [Google Scholar]
- 27.Opal, S.M., P.J. Scannon, J.L. Vincent, M. White, S.F. Carroll, J.E. Palardy, N.A. Parejo, J.P. Pribble, and J.H. Lemke. 1999. Relationship between plasma levels of lipopolysaccharide (LPS) and LPS-binding protein in patients with severe sepsis and septic shock. J. Infect. Dis. 180:1584–1589. [DOI] [PubMed] [Google Scholar]
- 28.Kaifu, T., J. Nakahara, M. Inui, K. Mishima, T. Momiyama, M. Kaji, A. Sugahara, H. Koito, A. Ujike-Asai, A. Nakamura, et al. 2003. Osteopetrosis and thalamic hypomyelinosis with synaptic degeneration in DAP12-deficient mice. J. Clin. Invest. 111:323–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tonge, R., J. Shaw, B. Middleton, R. Rowlinson, S. Rayner, J. Young, F. Pognan, E. Hawkins, I. Currie, and M. Davison. 2001. Validation and development of fluorescence two-dimensional differential gel electrophoresis proteomics technology. Proteomics. 1:377–396. [DOI] [PubMed] [Google Scholar]
- 30.Havlis, J., H. Thomas, M. Sebela, and A. Shevchenko. 2003. Fast-response proteomics by accelerated in-gel digestion of proteins. Anal. Chem. 75:1300–1306. [DOI] [PubMed] [Google Scholar]