Abstract
Objectives
This study sought to describe the evolution, use, and user satisfaction of a patient Web site providing a shared medical record between patients and health professionals at Group Health Cooperative, a mixed-model health care financing and delivery organization based in Seattle, Washington.
Design
This study used a retrospective, serial, cross-sectional study from September 2002 through December 2005 and a mailed satisfaction survey of a random sampling of 2,002 patients.
Measurements
This study measured the adoption and use of a patient Web site (MyGroupHealth) from September 2002 through December 2005.
Results
As of December 2005, 25% (105,047) of all Group Health members had registered and completed an identification verification process enabling them to use all of the available services on MyGroupHealth. Identification verification was more common among patients receiving care in the Integrated Delivery System (33%) compared with patients receiving care in the network (7%). As of December 2005, unique monthly user rates per 1,000 adult members were the highest for review of medical test results (54 of 1,000), medication refills (44 of 1,000), after-visit-summaries (32 of 1,000), and patient–provider clinical messaging (31 of 1,000). The response rate for the patient satisfaction survey was 46% (n = 921); 94% of survey respondents were satisfied or very satisfied with MyGroupHealth overall. Patients reported highest satisfaction (satisfied or very satisfied) for medication refills (96%), patient–provider messaging (93%), and medical test results (86%).
Conclusion
Use and satisfaction with MyGroupHealth were greatest for accessing services and information involving ongoing, active care and patient–provider communication. Tight integration of Web services with clinical information systems and patient–provider relationships may be important in meeting the needs of patients.
Introduction
Several health care institutions have implemented secure patient Web sites that integrate online health services into the patient–provider relationship and into clinical care. Patient Web sites that provide patient access to electronic medical records (EMR) and electronic patient–provider communication can support more transparent and active sharing of personal health information. Promoting patient access to EMRs and patient–provider messaging through the Web may encourage patient activation and more effective partnerships with providers. 1–8 Early, small-scale studies of patient Web sites suggest that patients may particularly value secure messaging with physicians and access to medical records. 7,9–12 Patients also seem to value online medication refill services. 11 To inform future development of online services for patients, we need to better understand what services are used and valued by patients in community health care settings.
We performed a study of a patient Web site at Group Health Cooperative (Group Health), a mixed-model health care system in Washington and Idaho. The patient Web site, MyGroupHealth, was developed in 2000 as part of a larger redesign of care at Group Health that targeted patient-centered access to care. In keeping with the goal of redesigning around patients’ needs, Group Health integrated the patient Web site into clinical care and patient–provider relationships before full implementation of the clinical information system for providers. MyGroupHealth offered different services to patients depending on whether care occurred in Group Health’s Integrated Delivery System or in its contracted network of providers. Compared with patients in the network, patients in the Integrated Delivery System had access to a more extensive shared EMR and to secure electronic messaging with providers. Patients receiving care in the contracted network had access to a more limited set of personal health services, including review of an active medication list, requests for medication refills, and secure messaging with a pharmacist. We first describe development of MyGroupHealth. Next, we report on MyGroupHealth access, use, and satisfaction based on earlier small-scale and qualitative studies. 7,9–11 Related hypotheses include: (1) registration for MyGroupHealth would grow for all Group Health patients; (2) among patients in the Integrated Delivery System, registration would grow more quickly after implementation of the shared EMR; and (3) patient use and satisfaction would be the greatest for secure patient–provider messaging, review of medical test results, and medication refills.
Methods
Setting and Population
Group Health Cooperative is a mixed-model health care financing and delivery organization in Washington State and North Idaho. Over 300,000 members receive care through Group Health’s Integrated Delivery System, which includes 20 Group Health–owned facilities and over 500 Group Health physicians. Approximately 200,000 additional Group Health members receive care through a network of contracted physicians and other health care providers across Washington State.
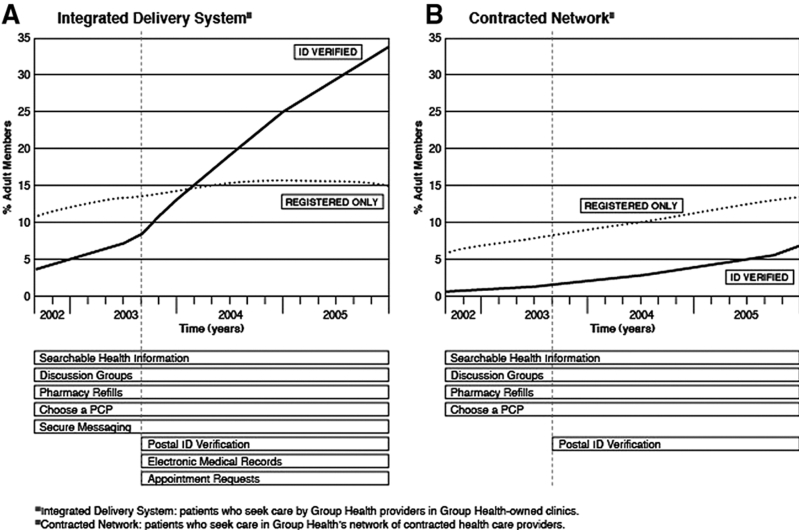
In August of 2000, Group Health established the MyGroupHealth Web site. Over the next three years, Group Health continued to add and enhance services on the site. In August 2001, the patient Web site began to offer different services to Group Health patients depending on whether a patient received care in the Integrated Delivery System or in Group Health’s contracted network. A member was considered in the Integrated Delivery System if he or she had a primary care provider in a Group Health–owned clinic. ▶ shows the MyGroupHealth services available from August 2003 onward according to whether a patient received care in the Integrated Delivery System or the contracted network. ▶ show the times that these services were available for patients.
Table 1.
Table 1 Patient Services on MyGroupHealth Web Site
| Service | Level of Access | Location of Provider | ||
|---|---|---|---|---|
| Registration Only ∗ | ID Verification† | Integrated Delivery System‡ | Contracted Network§ | |
| Healthwise knowledge base | X | X | X | X |
| Discussion groups | X | X | X | X |
| Health assessment tools | X | X | X | X |
| Choose a primary care provider | X | X | X | X |
| Appointment requests | X | X | ||
| Shared medical record | ||||
| Pharmacy refills and list of medications | X | X | X | |
| Secure messaging to and from health care team | X | X | ||
| Medical test results | X | X | ||
| After-visit summaries | X | X | ||
| Medical conditions | X | X | ||
| List of allergies | X | X | ||
| Immunization history | X | X | ||
∗ Registration only: patients entered Group Health identification number and a self-selected password on the Group Health Web site.
† ID verification: after confirmation of personal identity at a Group Health clinic or through the U.S. mail, patients entered a temporary password provided by Group Health and signed a user agreement.
‡ Integrated Delivery System: patients who seek care by Group Health providers in Group Health–owned clinics.
§ Contracted Network: patients who seek care in Group Health’s network of contracted health care providers.
Figure 1.
Access to MyGroupHealth by adult members.
The MyGroupHealth patient Web site had two levels of security. At the initial level (registration only), a patient created a password-protected account on the Web site. At this level, the user of MyGroupHealth could not exchange personally identifiable health information with Group Health. All health information or assessment tools at this level, with the exception of discussion groups, did not retain or share information beyond the user’s session. Members could access discussion groups on several topics and were encouraged to create a nonidentifying pseudonym in these groups. Group Health discouraged disclosure of personally identifiable information in the discussion groups. If personally identifying information was disclosed in the discussion groups, Group Health’s facilitator assessed the information and determined if it warranted removal.
The second and higher level of security provided access to the medical record shared between a patient and his or her providers. Access to this security level required each patient to complete an additional step verifying the patient’s identity (ID verification) to ensure that the patient was the person seeking access to his or her medical record. After this step, patients signed the MyGroupHealth User Agreement (Appendix A, available as a JAMIA online only data supplement at www.jamia.org). At this second level of security, patients and Group Health providers shared clinical and other personal health information. All information shared by a patient in this environment was part of the medical record and available to a patient’s Group Health providers.
During the study period, Group Health provided two different means of obtaining ID verification for access to the second level of security. Between August 2000 and August 2003, patients could only gain access by first presenting valid identification (a driver’s license or passport) at a Group Health clinic. Patients then received a temporary password for access to services. The patient changed the password at the next sign-on to MyGroupHealth. Beginning in August 2003, patients could also ID-verify for enhanced services through an online request for a temporary password that was sent through the United States Postal Service to a patient’s home address. The temporary password was active for 14 days from the time of request.
Transactions over the patient Web site were considered part of care provided to members of Group Health. Group Health providers were salaried and were expected to engage in secure messaging with patients. Group Health did not carve out pay for staff to provide electronic services to patients. Providers were given an incentive of $5 per message beyond their salary to encourage electronic patient–provider messaging. Group Health did not consider this a reimbursement. Secure messages from patients to a personal physician or other provider were first routed to the appropriate provider by support staff to ensure a timely reply. Individual providers were responsible for handling secure messages from patients or referring the message to a nurse for an appropriate reply. Physicians and other staff were accountable for meeting expectations for patient communication through messaging. Response time was tracked every day. If messages were not responded to within one business day, the physician was contacted and offered assistance in meeting patient expectations. Secure messages between patients and providers automatically became part of the EMR.
Refill requests over the patient Web site were handled by pharmacists. A provider’s support staff handled appointment requests. Normal test results were visible to patients on MyGroupHealth at the same time they were available for the physician. Physicians could send messages alongside any result visible by patients, and each medical test result was hyperlinked to an explanation of the test in the Healthwise knowledge base. Most abnormal laboratory tests also were automatically released to patients on MyGroupHealth at the same time the tests became available for physicians to review. Some abnormal laboratory test results as well as all pathology and radiology results required manual release by physicians. In June 2004, Group Health began sending notification messages to the regular e-mail accounts of all patients with new laboratory test results who had a MyGroupHealth account. These messages alerted patients that new results were available to view on MyGroupHealth.
All Group Health physicians delivering ambulatory care in the Integrated Delivery System used the EpicCare clinical information system (Epic Systems Corp., Verona, WI), which integrates clinical communication and information processes into a single interface. This interface included electronic patient scheduling, physician order entry (e.g., laboratory tests, prescriptions, referrals), systematic clinical documentation, clinical decision support, clinical messaging among physicians, secure online messaging with patients, and automated reminders at the point of care.
Patients receiving care in Group Health’s contracted network had more limited functionality on MyGroupHealth. Providers in this network were in predominantly rural, private-practice settings. At the time of the study, these practices did not have clinical information systems that could link with MyGroupHealth. For patients receiving care in the contracted network and who were ID-verified, MyGroupHealth had pharmacy services similar to those in the Integrated Delivery System, including access to a list of current and historical medications along with a medication refill service that provided free mailing of medications to a patient’s home.
As of March 2007, Group Health had not received reports of violations of the Health Insurance Privacy and Portability Act or broad security breaches. One potential and temporary security breach occurred when a member’s online record was accessed inappropriately by a family member who had the patient’s password but did not have durable power of attorney for health care (DPOA) for the patient. A request for a change in password associated with this access to the patient Web site triggered a confirmation letter to the son, who had DPOA. The son contacted Group Health’s Customer Service Center, and the password was changed to restrict access to only the son with DPOA. Group Health knows of no other real or potential security breaches.
Design
We performed a retrospective, serial, cross-sectional study of the adoption and use of the patient Web site from September 1, 2002, through December 31, 2005, and a cross-sectional satisfaction survey of patients who used MyGroupHealth in August 2004. The Group Health institutional review board approved our study.
Study of Patient Web Site ID Verification and Use
The study of patient ID verification and use of MyGroupHealth followed a retrospective, serial cross-sectional study design. All patients who received care in the Integrated Delivery System or in the contracted network from September 1, 2002, to January 31, 2005, were included in the study. We obtained enrollment data and MyGroupHealth use data from Group Health administrative databases. During the study period, we measured access to MyGroupHealth through the cumulative monthly registration and ID verification of patients. We measured MyGroupHealth use by determining the number of unique monthly users of individual MyGroupHealth services. The population of patients adopting MyGroupHealth was divided into two groups reflecting the different levels of access to MyGroupHealth services. The first group encompassed those who completed the first of a two-level registration process. This group (registration only) had access to basic MyGroupHealth services (▶). The second group encompassed those who had gone through the second step of registration (ID verification) for access to enhanced services such as EMRs and secure messaging. Patients in both of the registration groups (registration only and ID verification) were further divided into those who received primary care in the Integrated Delivery System and those who received care in the contracted network of providers.
To evaluate the impact of full implementation of the shared record on Web site ID verification in the Integrated Delivery System, we compared cumulative ID verification during the 16 months before and the 16 months after the implementation of Epic’s MyChart (August 2003). We compared cumulative patient ID verification among patients in the contracted network for the same period to test the isolated impact of adding the option of postal ID verification to in-person ID verification.
To test for differences in the rates of use over time, we compared the use of those services thought to be most actively part of clinical care (secure messaging, laboratory results reporting, after-visit summaries, and medication refills) to other services of the shared record (allergy list, immunization list, appointment scheduling, and diagnoses list). Access and use data were obtained monthly from August 2003 to December 2005. Due to high monthly variability in Web site use data, we selected December of each calendar year as representative of Web site use for the evaluation of change in use rates over time.
Among members receiving care in the Integrated Delivery System, we compared selected demographic and health characteristics in those with and without ID verification for the patient Web site. Due to the limits of data availability among members receiving care in the contracted network, we limited this analysis to members in the Integrated Delivery System. Members with Medicaid insurance were grouped with members in Washington State’s Basic Health Plan, an insurance program for low-income individuals and families not qualifying for Medicaid. Expected clinical need was assessed with the six Resource Utilization Bands of the Adjusted Clinical Group case-mix system. 13–15
Patient Satisfaction Survey
We conducted a patient satisfaction survey of patients who used MyGroupHealth in August 2004 (Appendix B, available as a JAMIA online only data supplement at www.jamia.org). A survey cover letter from the Medical Director of Group Health provided basic information about the survey. Survey questions were based on a patient satisfaction questionnaire formerly used to evaluate annual patient satisfaction with Group Health.
We randomly sampled 2,002 Group Health patients who, during August 2004, had access to enhanced MyGroupHealth services and who had used secure clinical messaging, requested an appointment over MyGroupHealth, viewed the results of 10 or more medical tests, or viewed 10 or more pages of the Healthwise knowledge base. We chose this sampling strategy to achieve a common baseline of user experience for assessing satisfaction with the Web site’s different services.
The survey was administered on paper and mailed to the sample group in mid-September 2004. Mailed surveys were used instead of Web surveys to preserve Group Health’s standard for limiting e-mail contact with patients to alerts or prompts when a new secure message or test result was available to view on MyGroupHealth. This helped ensure that Group Health fulfilled a consistent expectation by patients that all e-mail was focused on alerting them to issues directly related to their care. Additionally, mailed surveys minimized potential response bias and risk of low response rate associated with missing or incorrect patient e-mail addresses in Group Health’s administrative systems.
Respondents were asked to rate satisfaction on a 5-point Likert scale from “very satisfied” to “very dissatisfied”. Respondents could also answer “not applicable” for any question. At the end of the survey, participants were also asked to provide additional feedback about MyGroupHealth’s relevance to their health care needs. Surveys were collected for four weeks after the mailing. No follow-up contacts were made with nonrespondents. Nine hundred twenty-one patients completed the survey (overall response rate 46%). Respondents were similar in age (most common age group, 50 to 59 years) and gender (61% female) to the overall ID-verified population. Respondents rated an average of 5.45 (SD = 1.59) of the 7 questions. The proportion of respondents answering “not applicable” for survey questions ranged from 12.5% for pharmacy refills to 35.6% for appointment requests.
Statistical Analysis
Demographic characteristics were summarized separately for patients in the Integrated Delivery System and in the contracted network. Chi-square tests were used to test for demographic differences between groups. To evaluate the impact of the inclusion of enhanced Web site services and the implementation of ID verification through the postal service, we fit piecewise-linear regression models to estimate the change in cumulative adoption (ID verification) of the patient Web site over time. The models fit a change point at September 2003, corresponding to the first month in which the enhanced Web site services and postal ID verification were available. We compared the regression coefficient for time (slope of the regression line) before and after September 2003 separately for the Integrated Delivery System and contracted network patient groups.
Linear regression models also were used to evaluate whether use of specific Web site services increased at a more rapid rate than other services. Web site services were separated into two groups: (1) services most actively part of clinical care and patient–provider communication, including secure messaging, laboratory results reporting, after-visit summaries, and medication refills; and (2) the remaining Web site services, including allergy list, immunization list, appointment scheduling, and medical condition list. Regression models fit a common slope (rate of change in the number of unique monthly users per 1,000 patients over time) within each of the two groups of Web site services, but allowed for individual intercepts for each service type.
To evaluate patient satisfaction with Web site services, we used the McNemar test for equal proportions to test the proportion of respondents satisfied (satisfied or very satisfied) and the proportion very satisfied with each specific MyGroupHealth service compared with the proportion of satisfaction with MyGroupHealth overall. Statistical procedures were performed using STATA statistical software, version 9 (StataCorp LP, College Station, TX). 16
Results
▶ shows selected characteristics of patients who received care in the Integrated Delivery System compared with the contracted network as of December 2005. Compared with patients who received care in the network, patients in the Integrated Delivery System were older (p < 0.01), less likely to have commercial or Medicaid insurance, and more likely to have Medicare insurance (p < 0.01).
Table 2.
Table 2 Characteristics of the Group Health Cooperative Member Population, January 2006
| Characteristics |
Location of Provider | ||
|---|---|---|---|
| Total | Integrated Delivery System ∗ | Contracted Network† | |
| (n = 527,603) | (n = 325,634) | (n = 201,969) | |
| Age, % | |||
| 0–14 yr | 18 | 15 | 21 |
| 15–53 yr | 53 | 52 | 56 |
| 54–65 yr | 18 | 19 | 16 |
| 66+ yr | 12 | 15 | 8 |
| Male, % | 47 | 46 | 47 |
| Insurance type, % | |||
| Commercial | 90 | 89 | 90 |
| Medicare | 6 | 8 | 4 |
| Medicaid | 4 | 3 | 6 |
∗ Integrated Delivery System: patients who seek care by Group Health providers in Group Health–owned clinics.
† Contracted Network: patients who seek care in Group Health’s network of contracted health care providers.
Study of Patient Web Site ID-Verification and Use
Access to MyGroupHealth
Cumulative ID verification for access to MyGroupHealth increased throughout the study period. For combined Integrated Delivery System and contracted network enrollment, ID verification for access to all available MyGroupHealth services increased from 13,579 (3%) in September 2002 to 105,047 (25%) in December 2005. Registration limited to basic MyGroupHealth services increased from 38,876 (9%) to 60,284 (14%) during the same period.
▶ show the cumulative percent of adult members who were ID verified for access to all services and the percent registered for access to basic services only. In the Integrated Delivery System (▶A), ID verification increased continuously from 5% in September 2002 to 33% in December 2005. Registration for access limited to basic services increased initially from 11% in September 2002 to 15% in January 2004 and then stayed between 15% and 16% for the remaining 23 months of the study period. In the contracted network (▶B), ID verification and basic registration were both less common than in the Integrated Delivery System. ID verification in the contracted network (▶B) increased continuously from 0.5% to 6% during the study period. Registration for access limited to basic services also increased continuously during the study period from 5% to 13%. In the contracted network, the percent of members who were ID verified for enhanced access (pharmacy refills and a personal medication list) never increased above the percent of members with registration limited to basic services. In the Integrated Delivery System, cumulative ID verification began to exceed basic registration in February 2004.
Enhancements to MyGroupHealth in August 2003 were associated with a significant increase in ID verification among members in the Integrated Delivery System. In the Integrated Delivery System, piecewise-linear regression models comparing cumulative ID verification before and after August 2003 showed that trends were different (p < 0.001), with a mean monthly change in cumulative ID verification of 0.58% of members before enhancements and 0.90% after enhancements. Cumulative increases in ID verification did not have a discernible plateau during the study period. In the contracted network, monthly cumulative ID verification in the prestudy and poststudy periods also differed (p < 0.001), with mean monthly change in ID verification rate of 0.08% of members during the prestudy period and of 0.19% during the poststudy period.
▶ shows selected demographic and health characteristics of members receiving care in the Integrated Delivery System who were and were not ID-verified for the patient Web site. Members who were ID-verified were more likely to be female (p < 0.01), have commercial insurance (p < 0.01), and have higher expected clinical need (p < 0.01).
Table 3.
Table 3 Characteristics of Adult Group Health Members in the Integrated Delivery System ∗ With and Without ID Verification for MyGroupHealth, December 2005
| Characteristic | ID Verification† | No ID Verification‡ |
|---|---|---|
| n = 89,903 | n = 179,961 | |
| Age in years, mean (SD) | 52 (15) | 49 (19) |
| Male, % | 41 | 47 |
| Insurance type, % | ||
| Commercial | 89 | 84 |
| Medicare | 7 | 8 |
| Medicaid | 2 | 3 |
| Expected clinical need, % | ||
| None | 5 | 18 |
| Very low | 5 | 7 |
| Low | 13 | 17 |
| Moderate | 54 | 43 |
| High or very high | 22 | 16 |
∗ Integrated Delivery System: patients who seek care by Group Health providers in Group Health–owned clinics.
† ID verification: after confirmation of personal identity at a Group Health clinic or through the U.S. mail, patients entered a temporary password provided by Group Health and signed a user agreement.
‡ No ID verification: includes patients with no known access to the MyGroupHealth Web site and those who have only accessed the Web site through a Group Health identification number and a self-selected password (registration only).
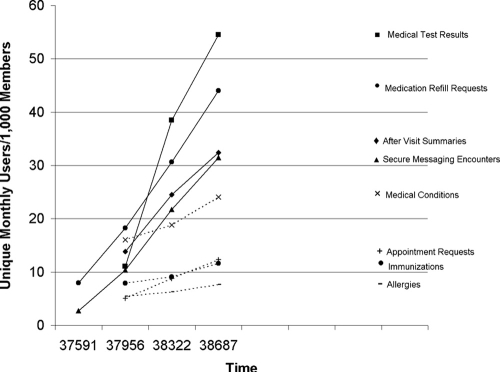
Use of the Shared Record
All portions of the shared EMR had increases in unique monthly use rates. ▶ shows the unique monthly users of each Web service for every 1,000 members with Group Health insurance where the service was available. The member denominator for this figure is the total number of individuals enrolled in Group Health insurance for that year, regardless of whether a member sought care with a provider during the time period. At the end of the study (December 2005), unique monthly users per 1,000 adult members for MyGroupHealth services were as follows, from highest to lowest: review of medical test results (54 of 1,000), medication refills (44 of 1,000), after-visit summaries (32 of 1,000), patient–provider clinical messaging (31 of 1,000), medical condition review (24 of 1,000), appointment requests (12 of 1,000), immunization review (12 of 1,000), and allergy review (8 of 1,000). Among those ID-verified and in the Integrated Delivery System, 49% sent or replied to one or more secure messages from Group Health providers between January 1, 2004, and March 31, 2005. In December 2005, 16% of those ID-verified patients who had medical tests at Group Health viewed their results on the patient Web site.
Figure 2.
Use of shared electronic record services on MyGroupHealth.
Changes in rates of use (characterized as the number of unique monthly users) differed by section of the shared record. Viewing test results, sending and receiving secure messages, requesting medication refills, and viewing after-visit summaries had an annual average increase of 12.2 unique monthly users of 1,000 members (95% confidence interval 10.0 to 14.5) compared with an annual increase of 2.7 unique monthly users per 1,000 members (95% confidence interval 0.4 to 5.7) for viewing immunization lists, allergy lists, medical condition lists, and requesting appointments. These two average increases in monthly use were significantly different (p < 0.001).
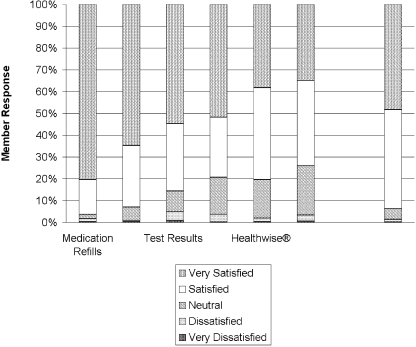
Satisfaction Survey
Results of the satisfaction survey are summarized in ▶ and ▶. Among respondents, 48% were very satisfied and 94% were satisfied (satisfied or very satisfied) with MyGroupHealth overall (▶). The proportion of respondents reporting that they were very satisfied with medication refills (81%) and secure messaging (65%) was significantly higher than the proportion very satisfied with MyGroupHealth overall (p < 0.001). Respondents were also somewhat more likely to report being very satisfied with test results (55%) compared with MyGroupHealth overall (p = 0.04). There was no difference between the proportions very satisfied with appointments (52%) and MyGroupHealth overall (p = 0.23). The proportion very satisfied with the Healthwise information (38%) and the provider directory (35%) was significantly lower than the proportion very satisfied with MyGroupHealth overall (p < 0.001). The proportion reporting that they were satisfied with medication refills (96%) and secure messaging (93%) did not differ significantly from the proportion satisfied with MyGroupHealth overall (94%). The proportion satisfied with the other services was significantly lower than the proportion satisfied with MyGroupHealth overall (p < 0.001).
Figure 3.
MyGroupHealth member satisfaction survey.
Table 4.
Table 4 MyGroupHealth Patient Satisfaction Survey
| n | Very Satisfied % | p Value ∗ | Satisfied or Very Satisfied % | p Value ∗ | |
|---|---|---|---|---|---|
| MyGroupHealth overall | 896 | 48 | Comparison | 94 | Comparison |
| Individual Services | |||||
| Medication Refills | 767 | 81 | <0.001 | 96 | 0.09 |
| Secure Messaging | 709 | 65 | <0.001 | 93 | 0.08 |
| Test Results | 741 | 55 | 0.04 | 86 | <0.001 |
| Appointments | 533 | 52 | 0.23 | 79 | <0.001 |
| Healthwise® | 684 | 38 | <0.001 | 80 | <0.001 |
| Provider Directory | 606 | 35 | <0.001 | 74 | <0.001 |
∗ p Value for the McNemar test of equal proportions comparing satisfaction of patients with individual MyGroupHealth services to satisfaction with MyGroupHealth overall.
Discussion
This study of a secure patient Web site in a large, mixed-model health care system found that use and satisfaction with the Web site was greatest for accessing services and information involving ongoing, active care and patient–provider communication. Viewing medical test results and after-visit summaries, requesting medication refills, and participating in secure clinical messaging with providers were the most commonly used portions of the Web site and showed the most increase in use over the course of the study. Compared with other services on the Web site, patients reported the highest satisfaction with viewing medical test results, requesting medication refills, and participating in secure clinical messaging with providers. The rate of ID verification for access to the Web site increased when these shared record services between patients and providers were integrated in August 2003. Other portions of the shared record on the Web site, including viewing immunizations, allergies, and medical conditions, had a slower uptake in use and were used less overall.
We found that access to the Web site was more common among patients receiving care in the Integrated Delivery System compared with those receiving care in the contracted network. By the end of the study period in December 2005, 33% of patients receiving care in the Integrated Delivery System had access to enhanced services (including the shared record) compared with 9% of patients receiving care in the contracted network. ID-verified members in the Integrated Delivery System were somewhat older with higher expected clinical need compared with those members who were not ID verified. In the Integrated Delivery System, patients mainly sought access to enhanced Web site services, including the shared medical record. Basic registration in this population served mainly as a stepping stone toward the enhanced services provided with ID verification. In contrast, patients receiving care in the contracted network were more likely to continue with access limited to basic services only. Fewer patients went on to obtain access to enhanced services, which for this population were limited to refills of medications and access to a medication history. Access to Web site services in the Integrated Delivery System compared with the network suggests that patients in the Integrated Delivery System particularly valued access to enhanced services.
We were surprised by the relatively common and increasing use of after-visit summaries by patients. These summaries are provided to all patients after an in-person outpatient encounter with a Group Health provider. In addition to a list of active medications, medical tests that were ordered at the visit, and referral instructions ordered at the visit, the after-visit summary also includes patient education material and documentation of care plans entered by the provider. The growing use of the after-visit summary on MyGroupHealth may reflect patients’ desire for information about their conditions and the plan of care. 17–19 Recent survey studies suggest that patients are motivated to access their medical record by unmet information and care needs. 20,21 After-visit summaries on MyGroupHealth may fill this need better than access to physician notes because these summaries can provide a patient with a focused plan of care combined with personalized educational material hyperlinked to other resources. Our results showing higher ID verification among patients with higher expected clinical need also suggests that patients may be using the Web site’s services to help manage ongoing health conditions.
Two studies have reported on patient Web sites with shared medical records that included secure messaging between patients and providers. Similar to our findings, these studies found that access to medical test results and secure messaging with physicians are used by 22 and particularly valuable to patients. 10 Both of these studies were from large health care institutions (Beth Israel Deaconess Medical Center and Palo Alto Medical Foundation) in which the patient Web site was widely available to patients and physicians. Physician adoption seemed to be important in whether patients signed up for and used online services. Weingart et al. 22 reported that 11% (or 15,504) of all primary care patients had known access to the patient Web site at Beth Israel Deaconess Medical Center; physicians had between 0 and 98% of their panels enrolled for online services. 22 More similar to our findings, Tang et al. 12 reported that 30% (or approximately 50,000) of all primary care patients had access to the patient Web site at the Palo Alto Medical Foundation; although overall physician participation was not reported, 90% of physicians reported being satisfied with the patient Web site. 10 In 2004, 490 of 550 Group Health physicians (89%) participated in secure clinical messaging with patients. 23 These early studies suggest that patient Web sites seem to have the most value and the greatest adoption when patient and providers use them together to support patients’ active health care needs.
One study has reported on an early patient Web site with more limited functionality. In that study from Kaiser Permanente’s Integrated Delivery System, members had Web site access to a medication refill service, an appointment request service, and an online structured template for asking medical or prescription drug questions. Among the over 3,000,000 patients in the Kaiser health plan for which the Web site was available, patients most commonly used medication refills (1.3% of members) and appointment scheduling (1.7% of members). At the end of the three-year study, 8.6% of patients had signed up for Web site services. 24 The pattern of uptake in access to this patient Web site was similar to that of ID verification seen for MyGroupHealth in Group Health’s contracted network. At the end of our study period, 6% of Group Health patients receiving care in the contracted network had gained access to MyGroupHealth’s enhanced services. These versions of the Kaiser and Group Health patient Web sites provided a largely similar set of functionality (Group Health patients in the contracted network could not request appointments). In both of these patient Web sites, a medication refill service integrated with a personal medication list was not enough to drive Web site access above 10% of the member population over a three-year period.
This study has several limitations. The study describes patient Web site use in a limited manner, focusing on registration, ID verification, and unique monthly use; future studies should further examine demographic, health status, and other characteristics of users and nonusers of the patient Web sites. At least one other study suggests widening disparities associated with patient Web site adoption over time. 24 We did not examine the attrition rate of MyGroupHealth use by patients. The continuous increase in unique monthly users, however, suggests that overall attrition was likely to be minimal. Our measures of adoption are limited. Future metrics should attempt to tie adoption more closely with patient value and include health outcomes. We did not directly address the role of Group Health physicians in patient access and use of MyGroupHealth, which has been identified in other early patient Web site studies as a key element for engaging patients in online access to the medical record and patient–provider messaging. 7,21,22,25 We did not measure providers’ time doing phone, secure messaging, and in-person encounters with patients. Future studies should evaluate not only providers’ time in using these services, but also patients’ time in using health systems with and without this access, consistent with a patient-centered perspective. The study is vulnerable to unmeasured and uncontrolled changes in the characteristics of the Group Health population that could be associated with adoption of MyGroupHealth. Although patients in the Integrated Delivery System were older and were less likely to be on Medicaid, the differences between the two groups were modest and unlikely to account for the wide discrepancy seen for MyGroupHealth registration and ID verification. Limitations of the patient satisfaction survey included the survey’s modest response rate, which makes the results significantly vulnerable to response bias; inability to determine which aspects of a user’s experience accounted for a satisfaction rating (e.g., usability, content, response time); and surveying only active users of the patient Web site, which could have missed inactive users or nonusers that may have elected to not use the site because of a perceived lack of benefit. Patient Web sites, including Group Health’s, also remain in the early phases of development. All studies, including the one reported here, have occurred relatively early in the adoption of patient Web sites. Access to patient Web sites is likely to continue to grow, especially as new Web site functions are implemented and integrated into care. In this study, there was no visible plateau in the percent of Group Health members continuing to sign up for access to the shared medical record on MyGroupHealth.
The results of this study also should be viewed in the context of Group Health’s organizational characteristics and its broader efforts to improve patient access to care. Within the Integrated Delivery System, a Group Health patient’s care and EMR are coordinated across relationships with primary and specialty providers. In settings such as this, where most or all of the care is delivered in a single organization, patients may find particular value in shared EMRs and provider messaging. MyGroupHealth also was part of a multifaceted access initiative targeting better phone, in-person, and online access for patients. Group Health underwent large workflow, staffing, training, and incentive restructuring to support these combined access efforts. Because Group Health is both the insurance and the care delivery organization, Group Health also could be creative with addressing the widely cited barrier of reimbursement for electronic communications with patients. 26 Integrated care combined with patient-centered system reform may be important for achieving significant patient adoption of and satisfaction with Web services.
Our results should inform personal health record developers and policy makers. Personal health record efforts limited to providing a common medication list or claims data from insurers are not likely to achieve significant adoption. The use and value of Web-based medication lists and refill services seem to be tied to a larger constellation of services that are part of a shared EMR between patients and health care providers. The value of online health services for patients also seems to depend on the support of proactive communication between patients and health care providers. Personal health records focusing on the transfer of largely archived information in the EMR are less likely to be of value to patients than personal health records that connect patients and providers around medical test results, medication refills, and care plans. Because most patients receive care across a variety of separate practice settings and health care institutions, personal health record developers face a formidable challenge. Success will require interoperability of information systems and shared communication functionality across the largely fragmented U.S. health care system.
We found that access, use, and satisfaction with a patient Web site was associated with providing a constellation of shared medical record services that are well integrated with clinical care. Developers of patient Web sites and personal health records should consider focusing initial efforts on providing a set of functionality that supports patient–provider communication and engages patients with the information in the medical record that is most relevant to ongoing care.
Footnotes
This study was supported by the Agency for Health Care Research and Quality (Grant No. R03 HS014625-01) and by the Robert Wood Johnson Foundation’s Changes in Health Care Financing and Organization Initiative (Grant No. 52229).
References
- 1.Greenfield S, Kaplan S, Ware Jr JE. Expanding patient involvement in careEffects on patient outcomes. Ann Intern Med 1985;102:520-528. [DOI] [PubMed] [Google Scholar]
- 2.Greenfield S, Kaplan SH, Ware Jr JE, Yano EM, Frank HJ. Patients’ participation in medical care: effects on blood sugar control and quality of life in diabetes J Gen Intern Med 1988;3:448-457. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan SH, Greenfield S, Ware Jr JE. Assessing the effects of physician-patient interactions on the outcomes of chronic disease Med Care 1989;27(suppl):110-127. [DOI] [PubMed] [Google Scholar]
- 4.Maly RC, Bourque LB, Engelhardt RF. A randomized controlled trial of facilitating information giving to patients with chronic medical conditions: effects on outcomes of care J Fam Pract 1999;48:356-363. [PubMed] [Google Scholar]
- 5.Bronson DL, Costanza MC, Tufo HM. Using medical records for older patient education in ambulatory practice Med Care 1986;24:332-339. [DOI] [PubMed] [Google Scholar]
- 6.Ross SE, Lin CT. The effects of promoting patient access to medical records: a review J Am Med Inform Assoc 2003;10:129-138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ralston JD, Revere D, Robins LS, Goldberg HI. Patients’ experience with a diabetes support programme based on an interactive electronic medical record: qualitative study BMJ 2004;328:1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Committee on the Quality of Healthcare in America, Institute of Medicine Crossing the Quality Chasm: A New Health System for the 21st CenturyWashington, DC: National Academy Press; 2001.
- 9.Goldberg HI, Ralston JD, Hirsch IB, Hoath JI, Ahmed KI. Using an Internet Comanagement Module to improve the Quality of Chronic Disease Care Jt Comm J Qual Saf 2003;29:443-451. [DOI] [PubMed] [Google Scholar]
- 10.Tang PC, Lansky D. The missing link: bridging the patient–provider health information gap. Electronic personal health records could transform the patient–provider relationship in the twenty-first century Health Aff (Millwood) 2005;24:1290-1295. [DOI] [PubMed] [Google Scholar]
- 11.Hassol A, Walker JM, Kidder D, et al. Patient experiences and attitudes about access to a patient electronic health care record and linked web messaging J Am Med Inform Assoc 2004;11:505-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tang PC, Ash JS, Bates DW, Overhage JM, Sands DZ. Personal health records: definitions, benefits, and strategies for overcoming barriers to adoption J Am Med Inform Assoc 2006;13:121-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johns Hopkins University. Clinical Groups (ACG) Assignment Software (Version 7.0 for Windows). Baltimore: Johns Hopkins University, 1990-2006.
- 14.Starfield B, Weiner J, Mumford L, Steinwachs D. Ambulatory care groups: a categorization of diagnoses for research and management Health Serv Res 1991;26:53-74. [PMC free article] [PubMed] [Google Scholar]
- 15.Weiner JP, Starfield BH, Lieberman RN. Johns Hopkins Ambulatory Care Groups (ACGs)A case-mix system for UR, QA and capitation adjustment. HMO Pract 1992;6:13-19. [PubMed] [Google Scholar]
- 16.StataCorp Stata Statistical Software9th ed.. College Station, TX: Statistical Software; 2005.
- 17.Tang PC, Newcomb C. Informing patients: a guide for providing patient health information J Am Med Inform Assoc 1998;5:563-570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jackson JL, Kroenke K. The effect of unmet expectations among adults presenting with physical symptoms Ann Intern Med 2001;134:889-897. [DOI] [PubMed] [Google Scholar]
- 19.Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness Ann Intern Med 1997;127:1097-1102. [DOI] [PubMed] [Google Scholar]
- 20.Fowles JB, Kind AC, Craft C, Kind EA, Mandel JL, Adlis S. Patients’ interest in reading their medical record: relation with clinical and sociodemographic characteristics and patients’ approach to health care Arch Intern Med 2004;164:793-800. [DOI] [PubMed] [Google Scholar]
- 21.Connecting for Health Achieving Electronic Connectivity in Healthcare: A Preliminary Roadmap from the Nations Public and Private Sector LeadersNew York: Markle Foundation; 2004.
- 22.Weingart SN, Rind D, Tofias Z, Sands DZ. Who uses the patient internet portal? The PatientSite experience J Am Med Inform Assoc 2006;13:91-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Carrell D, Ralston J. Messages, Strands and Threads: Measuring Electronic Patient–provider MessagingAmerican Medical Informatics Association Annual Session. American Medical Informatics Association; Washington, D.C., October 22–26 2005.
- 24.Hsu J, Huang J, Kinsman J, et al. Use of e-Health services between 1999 and 2002: a growing digital divide J Am Med Inform Assoc 2005;12:164-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kittler AF, Carlson GL, Harris C, et al. Primary care physician attitudes towards using a secure Web-based portal designed to facilitate electronic communication with patients Inform Prim Care 2004;12:129-138. [DOI] [PubMed] [Google Scholar]
- 26.Liederman EM, Morefield CS. Web messaging: a new tool for patient-physician communication J Am Med Inform Assoc 2003;10:260-270. [DOI] [PMC free article] [PubMed] [Google Scholar]