Abstract
Background
Up to 38% of inpatient medication errors occur at the administration stage. Although they reduce prescribing errors, computerized provider order entry (CPOE) systems do not prevent administration errors or timing discrepancies. This study determined the degree to which CPOE medication orders matched actual dose administration times.
Methods
At a 658-bed academic hospital with CPOE but lacking electronic medication administration charting, authors randomly selected adult patients with eligible medication orders from historical 1999–2003 CPOE log files. Retrospective manual chart audits compared expected (from CPOE) and actual timing of medication administrations. Outcomes included: dose omissions, median lag times between ordered and charted administrations, unauthorized doses, wrong dose errors, and the rate of nurses’ medication schedule shifting.
Results
Dose omissions occurred in 756 of 6019 (12.6%) audited administration opportunities; only 313 of the omissions (5.2% of opportunities) were unexplained. Wrong doses and unexpected doses occurred for 0.1% and 0.7% of opportunities, respectively. Median lag from expected first dose to actual charted administration time was 27 minutes (IQR 0-127). Nursing staff shifted from ordered to alternate administration schedules for 10.7% of regularly scheduled recurring medication orders. Chart review identified reasons for dose omissions, delays, and dose shifting.
Conclusion
Inpatient CPOE orders are legible and conveyed electronically to nurses and the pharmacy. Nonetheless, ward-based medication administrations do not consistently occur as ordered. Medication administration discrepancies are likely to persist even after implementing CPOE and bar-coded medication administration unless recommended interventions are made to address issues such as determining the true urgency of medication administration, avoiding overlapping duplicative medication orders, and developing a safe means for shifting dosing schedules.
Background
Following publication of the 1999 Institute of Medicine report, “To Err is Human: Building a Safer Health Care System,” 1 many medical centers initiated quality improvement programs to reduce medication errors. Several institutions documented that computerized provider order entry (CPOE) systems could locally reduce errors through better-formed, more correct medication orders. 2,3 Such CPOE systems have generated alerts for improper dosages, 4 allergies, 5 and drug-drug interactions. 6 Hospitals also reported improved safety and efficiency through implementing computer-generated (paper-based) Medication Administration Records (CMAR), Electronic Medication Administration Records (EMAR), or Bar Coded Medication Administration (BCMA) systems that cross-verify drug, patient, and order before administration occurs. 7–9 Early BCMA system adopters reported reduced administration error rates ranging from 2% 9 to 86%. 7,10
To evaluate CPOE-based medication ordering practices and inpatient medication administration procedures, the current study 1) assessed the extent to which CPOE-generated medication orders corresponded to actual administration times, and 2) identified administration errors that persist in the CPOE environment. The study examined dose timing discrepancies and unexplained administration errors. It did not investigate errors that occurred at the prescribing or dispensing levels.
Methods
Setting
The study included adult patient sub-acute, acute, and critical care units at Vanderbilt University Hospital (VUH), a 658-bed tertiary care academic facility in Nashville, Tennessee. During the period of study (1999–2003), all participating hospital units used an institutionally developed CPOE system that captured all patient orders. Physicians entered approximately 75% of orders (for medications, ancillary tests, and nursing care, etc.). The remaining 25% were entered by other care team members, usually based on physicians’ verbal or written orders. All CPOE orders were well-formed and legible. 3,5 The CPOE system generated drug dosing, allergy-related, and drug-drug interaction warnings and processed 12,000 to 15,000 orders daily.
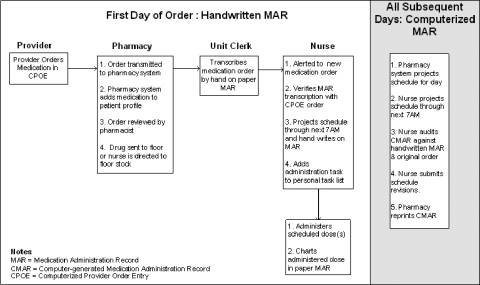
During the period analyzed, VUH used a CMAR for medication charting, but no EMAR or BCMA. Following entry of a medication order, the CPOE system transmitted it electronically to the hospital pharmacy system. Licensed pharmacists reviewed each order within the pharmacy system, and entered any changes into the CPOE system. The hospital’s medication administration process (▶) incorporated a CMAR used by the nursing service. On the first day of a new medication order, nurses augmented the paper CMAR document by handwriting any new medication’s schedule. Thus, for all new medication orders, from the immediate time of order generation until 7:00AM the next day, presence of the new orders was documented through manually writing (transcribing) the order onto the previously printed CMAR. On subsequent days, the new computer-generated CMAR included the previously ordered medication.
Figure 1.
Medication administration process for hybrid handwritten MAR, CMAR, and CPOE system.
Eligibility
The study utilized the institutional quality control log file containing all past CPOE orders. The project created a derivative de-identified file that included all medication orders on eligible adults (18 years or older) admitted between August 1999 and July 2003. The CPOE orders were inclusive—members of a patient’s care team collectively entered all of the patient’s orders into the CPOE system. Orders initially written on paper were entered into the CPOE system so that a complete record of the orders were formed (unless in a downtime that lasted >72 hours, or if downtime written orders were one-time and previously completed). The Vanderbilt University Institutional Review Board reviewed and approved this study.
The study audited six commonly prescribed medication classes: 1) loop diuretics, 2) thiazide diuretics, 3) non-steroidal anti-inflammatory medications (NSAIDs), 4) potassium supplements and potassium sparing diuretics, 5) angiotensin converting enzyme (ACE) inhibitors and angiotensin receptor blocking (ARB) agents, and 6) class III antiarrhythmics. These drugs were selected in part due to the commonality of their regularly scheduled use, and in part because authors were conducting a concomitant study of laboratory side effects of medications that involved these six classes of drugs.
Charts were eligible for review if adult patients admitted during the study period to designated hospital units had a drug order for one of the study medications with ordered duration of at least 72 hours. Approximately 30 charts per study drug class (190 charts total) were randomly selected for audit. The study nurse compared CPOE-based expected administration times (as might be projected by a BCMA application) to actual administration (or omission) times in patients’ paper charts. Omission times were both implicit (expected based on schedule but not charted) and explicit (initialed by nurse and circled as “held” or “not given” with or without a reason). Extra doses not matching CPOE-projected drug administration times comprised “unexpected” administrations.
Auditing excluded medications administered conditionally (via “PRN” and “sliding scale” orders), as well as orders for total parenteral nutrition, large volume IV infusions (e.g., D5/W) and topical medications (except nitroglycerin). For targeted charts, the audit included administration records for the index drug and up to four other randomly-selected, study medications (if ordered on the chart being audited); the study also audited up to two randomly selected non-study-related medications for some patients, if ordered. Auditing for each selected medication covered the entire course of scheduled therapy for the first ten days of hospital admission, including dose or route changes.
The interpretation of “compound” orders—requesting immediate administration of a first dose followed later by regularly spaced administration of additional doses—proved challenging. For example, consider an order “Furosemide 180 MG IV 1ST NOW Q12H” that was entered into the CPOE system 5 minutes prior to the hospital unit’s next standard administration time for an every 12 hour schedule. If interpreted literally, the order might mean that two doses should be given 5 minutes apart. The study auditing expectations were that only one first dose should be administered (rather than two closely spaced doses) if the unit-specific administration time for the first recurring (second absolute) dose of a “first now and every NN hours” order fell within one-half of the inter-dose interval (i.e., < NN/2) from the time of order entry.
Study Outcome Measures
American Society of Hospital Pharmacists 11 medication error definitions, per Allan and Barker, 12 helped to define study outcomes. The current study characterized: a) omission errors (failure to give medication before subsequent dose due); b) unauthorized dose errors (additional, “unexpected” doses); c) wrong dose errors (when dose given differed from that prescribed); and d) wrong time errors (dose administered > 60 minutes before or after scheduled time). The current study audit included two additional measures of potentially erroneous dose timing: e) time to first administration (time from first “scheduled” to first actual administration); and f) dose shifting (systematic shifting by more than 60 minutes in same direction of scheduled administrations for at least 2 consecutive doses). All of the above categories were considered “timing discrepancies” for purposes of this study. The study used observed distributional percentiles—e.g., the median or 50th percentile (median) and the interquartile range (25th to 75th percentile or IQR). Dose shifting altered an entire dosing schedule. Omissions were classified as either “justified”—when the nurse charted a clear explanation (e.g., a note explaining that a missed dose occurred when the patient had an x-ray)—or “errors”.
The study also explored whether verbal orders were initiated more rapidly than written orders, since verbal order initiation did not require transcription by a unit clerk (see ▶) and because urgent patient requirements might have motivated many verbal orders.
Results
From August 1, 1999 to July 31, 2003, there were 120,716 admissions to VUH; 10,484 (9%) of those admissions were eligible for the study based on adult age and an order for an eligible study drug lasting 72 hours. ▶ describes the audited sample population.
Table 1.
Table 1 Patient Cohort Demographics, Orders, and Doses by Category
| NSAID | KCL/KCL Sparing Diuretic | ACEI/ARB | Class III Antiarrhythmic | Loop Diuretic | Thiazide Diuretic | All Other Drugs | Total | |
|---|---|---|---|---|---|---|---|---|
| Patients Selected by Index ∗ | 30 | 33 | 32 | 27 | 34 | 34 | 190 | |
| Median Age at Admission | 74 | 55 | 67 | 66 | 58 | 68 | 64 | |
| Patients, Number | 91 | 96 | 71 | 31 | 97 | 51 | 190 | 190 |
| Orders Audited, Number | 136 | 268 | 120 | 56 | 318 | 64 | 540 | 1502 |
| Doses Audited, Number | 704 | 635 | 592 | 327 | 932 | 316 | 2513 | 6019 |
∗ The selected charts were audited for up to five study drugs. Patients were frequently on drugs from multiple drug categories, so the number of patients in each category could be larger than the number of patients “selected” for the category.
Patients Selected by Index = Number of patients selected in the sample cohort for each medication class. All patients included were selected by medication class. No patients were “selected” for the non-study drugs; Median Age at Admission = Median age in years at the time of the patient’s admission; Patients, Number = The total number of patients with orders in the drug class. Since each patient selected was audited for up to five of the study drugs and two randomly selected non-study drugs for some patients, the number of patients audited in each class is greater than the number of patients selected to the cohort for the drug class; Orders Audited, Number = The total number of orders audited for the drug class. For each sampled medication, all orders for that medication in the first ten days of the admission were audited. For example, if potassium chloride was a sampled medication, all scheduled orders for potassium, regardless of strength, route, frequency, or duration, were audited; Doses Audited, Number = The number of doses audited for sampled drugs. For example, a twice daily order lasting two days would have had four doses audited.
The audit of 190 charts (95 males and 95 females) covered 1307 inpatient administration-days, with median audited days per patient of 6.9 (IQR 4.5–10.0). By design, the study truncated auditing of 59 patient records after hospital day ten. The 1502 audited medication orders involved 6019 medication administration opportunities. Auditing classified 756 administrations as omissions (12.6%); 443 had explanations (see ▶); thus, the 313 remaining omissions were errors, comprising 5.2% of dose opportunities. We analyzed the results at the individual order level and at the dose level (see ▶). ▶
Table 2.
Table 2 Documentation (or lack thereof) for 756 Omitted Medication Doses
| Omission Category | Reason | Frequency (%) |
|---|---|---|
| Unexplained or Unknown | Not charted—reason unknown ∗ | 282 (37.3) |
| Not on administration record for date/time† | 31 (4.1) | |
| Partially Explained | Held, reason not documented | 80 (10.6) |
| Patient post operative/unable to swallow | 7 (0.9) | |
| Fully Explained | Held for medical reasons | 165 (21.8) |
| Patient refused | 55 (7.3) | |
| Ordered and discontinued within 60 minutes | 29 (3.8) | |
| Patient off floor | 24 (3.2) | |
| Patient discharged | 24 (3.2) | |
| Patient taking nothing by mouth | 22 (2.9) | |
| Discontinued prior to shifted schedule | 19 (2.5) | |
| Drug not available on ward | 9 (1.2) | |
| Patient near terminal/care withdrawn | 6 (0.8) | |
| No intravenous access | 3 (0.4) | |
| Total | 756 (100) |
∗ Not charted—reason unknown coded for orders that were transcribed to the medication administration record but were neither charted as given nor charted as not given.
† Not on administration record coded for orders that did not appear on medication record (and also not charted). The order may not have been transcribed to the medication administration record.
The reason for the omissions in the Unexplained or Unknown category is unknown.
Omissions in the Partially Explained category were not fully documented. The omission was assumed to be intentional because the dose was circled as held or the chart notes indicated the patient was immediately post operative and not taking oral fluids.
Omissions in the Fully Explained category were fully documented and with appropriate reasons for holding or omitting the dose.
Table 3.
Table 3 Number of Doses, Omissions, and Unexpected Doses by Location at Administration
| Medical Non-ICU | Surgical Non-ICU | Medical ICU | Surgical ICU | Post-Op Care Recovery | Skilled Nursing ∗ | Total | |
|---|---|---|---|---|---|---|---|
| Number of Dose Opportunities | 2993 | 1518 | 436 | 468 | 351 | 253 | 6019 |
| % of Total Dose Opportunities | 49.7 | 25.2 | 7.2 | 7.8 | 5.8 | 4.2 | 100.0 |
| Omissions Unexplained/unknown | 132 | 111 | 21 | 18 | 28 | 3 | 313 |
| Multi-Dose | 117 | 84 | 16 | 13 | 21 | 3 | 254 |
| One-Time Dose | 15 | 27 | 5 | 5 | 7 | 59 | |
| Percent of total dose opportunities | 4.4 | 7.3 | 4.8 | 3.8 | 8.0 | 1.2 | 5.2 |
| Unexpected Doses | 17 | 9 | 4 | 8 | 2 | 0 | 40 |
| Percent of Total doses | 0.6 | 0.6 | 0.9 | 1.7 | 0.6 | 0.0 | 0.7 |
| Wrong Time Administrations† | 461/2761 | 246/1289 | 79/393 | 63/419 | 53/319 | 14/245 | 916/5426 |
| Percent Wrong Time | 16.7 | 19.1 | 20.1 | 15.0 | 16.6 | 5.7 | 16.9 |
∗ Only 7 patients were included from Skilled Nursing.
† The denominator excluded orders with dose shifting as explained in the text. Dose shifting was defined as two or more consecutive doses shifted 61 minutes or more in the same direction in an order with equally spaced dose intervals. Number of Dose Opportunities = Number of audited doses by type of unit. Dose opportunities includes omitted, administered, scheduled, and unexpected doses; Omissions Unexplained/unknown = Total omissions with no explanation for the un-administered dose. Omissions that were partially or fully explained are excluded; Multi-Dose = Orders with more than one scheduled dose for administration; One-time Dose = Orders with only one scheduled dose for administration; Unexpected Doses = Doses administered in addition to “scheduled” doses, usually at the start or end of the order; Wrong Time = Doses administered > 60 minutes before or after scheduled time. Only doses administered in orders that were not “dose shifted” are included. The numerator is the number of wrong time doses and the denominator is the number of dose opportunities in orders that were not “dose shifted”.
Table 4.
Table 4 Number of Discrepancies per 100 Orders
| Discrepancy Type | Per Hundred | Orders with Discrepancies | Total Orders |
|---|---|---|---|
| Total Discrepancies | 54.3 | 816 | 1502 |
| Dose Shifts in Regular Spaced Interval | 10.7 | 92 | 860 |
| Unexpected Administrations | 2.5 | 38 | 1502 |
| Omissions | 16.4 | 246 | 1502 |
| One-time Dose Orders | 9.0 | 59 | 655 |
| Multi Dose Orders | 22.1 | 187 | 847 |
| Wrong Dose | 0.3 | 4 | 1502 |
| Dose Shift or Wrongtime Combined | 43.0 | 646 | 1502 |
| Unexpected, Wrong Dose, Omission | 18.9 | 284 | 1502 |
Total Discrepancies = Orders with at lease one dose with one or more of the discrepancies listed in the table, e.g., dose shift, omission, wrong time; Dose Shifts = Orders with systematic shifting by more than 60 minutes in same direction of scheduled administrations for at least 2 consecutive doses; Unexpected Administration = Orders with at least one extra dose not matching CPOE-projected drug administration times; Omission = Orders with at least one dose omitted with no explanation for the un-administered dose. Omissions that were partially or fully explained are excluded; Multi-Dose = Orders with more than one scheduled dose for administration; One-time Dose = Orders with only one scheduled dose for administration; Wrong Dose = Orders with at least one dose given in a different amount from that prescribed; Dose Shift or Wrongtime Combined = Orders with a at lease one dose given > 60 minutes before or after scheduled administration time and/or at least two consecutive doses shifted 61 or more minutes in the same direction; Unexpected, Wrong Dose, Omission = Orders with at least one unexpected dose, wrong dose, and/or unexplained omission.
Six wrong doses (all under-dosages) were discovered on the CMAR (0.1%); for three (two of which were for acetaminophen, which was included as a “randomly added secondary medication” as part of the study auditing protocol), half the ordered dose was given. Two potassium chloride infusions, ordered as multiple split infusion doses, had administered doses less than ordered because some of the later infusion doses were omitted. Forty unexpected administrations occurred (0.7%), most often at the beginning or end of the series of ordered administrations for a medication.
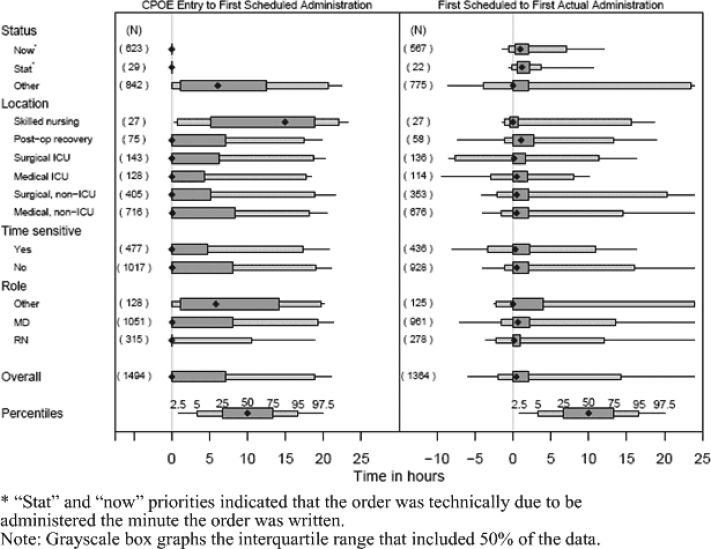
The study examined whether timeliness of medication initiation correlated with ordering characteristics, including: 1) order priority (stat, now, or routine); 2) entering individual’s title (analysis assumed all verbal orders were entered by staff nurses), and 3) patient location. Forty-three percent of all sampled orders had “stat” or “now” priority. The median time from first scheduled to actual administration was 73 minutes for “stat” orders (IQR 35–130, N = 22), 58 minutes for “now” orders (IQR 14–127, N = 567), and 0 minutes for all other (“routine”) orders (IQR 0–126, N = 775) (see ▶). The notice time, from order entry to first scheduled administration, was (by definition) 0 minutes for “stat” orders (N = 29) and “now” orders (N = 623), and had a median of 364 minutes for all other (“routine”) orders (IQR 70–746, N = 842).
Figure 2.
Lead time from CPOE entry to first scheduled and first actual administration.
To compare the timeliness of verbal versus written orders, the project examined the entering individual’s title. Verbal orders entered by nurses were administered closer to scheduled times than were physician-entered orders (nurse-entered median = 11 minutes, IQR 0–60, N = 278 versus physician-entered median = 40 minutes, IQR 0–130, N = 961). Timeliness was higher for verbal (nurse-entered) orders despite shorter notice times for these types of orders (nurse entered median = 0 minutes, IQR 0–0, N = 315; versus physician-entered median = 3 minutes, IQR 0–486, N = 1051). It was not possible to determine whether nurses entered verbal orders into the CPOE system immediately upon receipt.
Time from first scheduled to actual first medication administration was similar for acute and intensive care units, while the sub-acute unit had the smallest documented delay from first scheduled dose to actual first administration, 0 minutes. With a median lead time of almost 15 hours, the sub-acute unit also had the greatest time to prepare for starting new orders (time from CPOE entry to first scheduled administration).
Dose shifts occurred for 10.7% of medications ordered with regularly spaced intervals (e.g. “every 6 hours”), and the median shift time among them was 140 minutes (IQR 77–205). If the study employed traditional definitions (see ▶), orders where nurses “shifted” the administration schedule from the projected schedule would have been classified as wrong time errors.
Overall, 54.3% of medication orders studied had one or more administration discrepancies, including 43% with administration timing discrepancies (see ▶). Excluding dose-shifted orders produces a wrong-time dose rate of 16.9% of scheduled opportunities.
Discussion
This study documented that delays in medication administration still occurred in an environment where CPOE-based ordering had eliminated delays related to transcribing and transporting orders to the pharmacy. Using stringent criteria, one or more medication administrations did not match CPOE-based expectations for 54.3% of medication orders. However, most such discrepancies were probably clinically insignificant for the types of medications in the current study: 43% of the discrepancies were due to administration schedule shifts or wrong-time administrations, and only 18.9% met Allan and Barker’s other criteria for administration errors.
Delays in Administration
Delays in timely delivery of medications to patients result from: a) inefficient delivery of new orders to the pharmacy (chiefly a problem of paper-based ordering practices); b) slow dispensing from the pharmacy to the patient’s hospital location; and c) postponed delivery to the patient of medications as scheduled, once medications were present on the patient unit and available to dispense.
Because CPOE systems deliver well-formed orders almost instantaneously to the pharmacy, where they are promptly processed by pharmacists (average processing time at VUH, 5 minutes), order-processing delays due to manual ordering were eliminated after CPOE installation. Those pre-CPOE delays include time required: a) to manually write orders on the chart and flag the chart as having new orders; b) for a unit clerk to see the flagged chart; c) to send the orders to the pharmacy via pneumatic tube or fax, and d) for the pharmacist to manually enter written orders into the pharmacy dispensing computer system.
Scheduling of Doses
Previous studies have shown a wide disparity in wrong-time error rates, ranging from 0.5% 13 to 35.7%, 14 perhaps reflecting difficulty in determining “correct” expected administration times. In addition, the difference between a wrong time administration and an omission depends on the length of the administration delay, e.g. if the dose was delayed past the time the subsequent dose was due, a wrong time dose became an omission. EMAR and BCMA systems must address the difficult challenge of determining “correct” administration times, in particular the “correct” start time, because the effort required for nurses to modify the scheduled administration time in an electronic system will be higher than for a paper-based system. Although establishing standard administration times has been proposed as an approach to determining the “correct” administration time, this is unlikely to be a total solution. For example, some of the schedule shifts in this study were for daily medications that the patient had been taking in the evening at home. Daily medications in hospital settings were typically given during the day, not in the evening. Accommodating the patient’s prior medication regime has been an appropriate reason to shift the medication schedule and should be accommodated in electronic systems. In addition, the paper-based CMAR typically did not project administration times on the first day of the order, but doing so constitutes a requirement for EMAR/BCMAs. For example, the conundrum of interpreting combination schedules for series scheduled orders (e.g., “now and bid”) did not effect the CMAR because the first day of the order was manually interpreted and transcribed by nursing staff. Installed BCMA/EMAR systems would need to interpret the ordering provider’s intentions and/or warn of potentially overlapping dose schedules and seek nursing staff intervention to avoid conflicts.
Omission of Doses
As this study’s dose omission rate (5.2% of opportunities) matched those previously reported (4.6% 15 to 9.9% 16 ), it was evident that CPOE per se did not reduce all types of administration errors. We believe that installing a BCMA/EMAR system would potentially reduce some omissions in the following categories from ▶:
a) Not charted-reason unknown—BCMA/EMAR could improve charting for omissions in the current study that were due to simple oversights, when the drug was given but not charted or when administration was held or omitted for a good reason but neither the omission nor the reason were charted. However, some unexplained omissions are likely to continue even with real-time BCMA/EMAR systems. For example, nurses might fail to give a scheduled dose or chart a reason when they unexpectedly have to attend to a life-threatening emergency for a patient in a room nearby to the index patient.
b) Order not present on administration record for date/time—BCMA/EMAR systems could reduce some omissions that occur because the nurse is unaware of the order. However, these systems would not impact errors of omission that occur due to the nurse’s urgent duties elsewhere. In addition, BCMA/EMAR systems typically do not serve as order notification vehicles, so the nurse must actively look elsewhere for new medication orders.
c) Medication ordered and discontinued within 60 minutes—Errors due to a wrong or erroneous actual medication order could potentially increase with the implementation of BCMA/EMAR technology. The current lag (30–60 minutes) between ordering and administration (predominantly for “stat” or “now” orders) allows time for corrections when faulty orders are detected, whereas the window for corrections would be greatly reduced with BCMA/EMAR technology replacing the slower manual transcription process.
Two interviewed nurses indicated that different physicians can issue conflicting orders for the same drug (divergent dosing schemes). While this type of error may be more prevalent in academic settings with teams of providers, it also can occur in settings where an attending physician and a hospitalist care for the patient as a team. Nurses typically must contact a single physician for definitive clarification of the conflicting orders. When such conflicting orders were not cancelled, falsely elevated “omitted dose” counts occurred if nurses followed only one dosing schedule while (correctly) ignoring that of the second physician.
Initiation of First Doses
The present study found median “expected to actual first administration” delays of 58–73 minutes for “now” and “stat” orders, and 27 minutes for orders overall. The finding that now and stat orders incurred longer delays was unexpected, as was the high proportion of “now” orders. The convenience of ordering drugs to start immediately versus the complexity of considering when the drug would be started if it was deferred to the “regular” vs. the “now” schedule may have contributed to the high proportion of “now” orders. Several factors may explain how “urgent” orders incur longer delays than routine orders. First, the “notice” time, i.e., the interval from order generation to time of first expected dose, was much shorter for “now” or “stat” orders than for routine orders (0 vs. 364 minutes). Longer notice times allowed the pharmacy more time to deliver medications, and nurses more time to plan to administer them. Second, in a CPOE environment, high priority drug orders conveyed verbally gave ordering physicians opportunity to describe exactly how urgent or life-critical an order may be, while physician-entered CPOE orders typically had “comment” fields of limited length in which to convey reasons for urgency; in some systems, comments may not even be visible with the main display of the order. Medication delivery time for a CPOE order was dependent on nurses’ awareness of the order, conflicting high-priority work agendas, and whether the medication was already stocked on the patient’s ward. Several published studies measured time from order inception (writing in chart or entry into CPOE system) to medication administration (patient physically receiving drug). 17–20 These studies reported significant reductions when going from manual (written) ordering to CPOE-based ordering but even with CPOE, turnaround times ranged from 83-168 minutes in acute care settings, and 318 minutes in a rehabilitation unit.
Limitations of Current Study
The current study had several limitations. First, retrospective chart reviews could not detect documentation errors related to medication administrations (e.g., when the nurse accidentally charted an administration time off by one hour), and errors requiring direct observation (e.g., giving the wrong drug to the wrong patient). Direct observation of medication administrations has been demonstrated to detect significantly more errors than chart review. 21 Nelson et. al. 22 found that nurses documented administrations separately from the actual administration 52% of the time. Authors chose the 60-minute threshold for “wrong-time” administration errors because the authors believed that it is unlikely that most legitimate charting variances (time difference between actual administration and time charted by nurse) would exceed 60 minutes. While a 30 minute delay in administration is unacceptable for some medications (e.g., giving morphine for a patient with severe pain), for the drugs in the current study, 60 minutes was deemed reasonable as a discrepancy threshold.
Second, with the patient chart as the data source for the current study, the project could not attempt to analyze the clinical impact of the observed medication timing errors. The effects of timing errors and errors of omission were rarely recognized clinically, in that they were not commented upon in patient charts. When maintenance of specific serum concentrations of a drug is desired, timing of doses is critical for drug administrations. 23,24 The study could not determine a priori when it was clinically important to administer a medication with precise timing, because that involves knowledge of clinical indications and of desired medication effects. Poon et. al. 25 described use of generic clinical scenarios to help judge the severity of potential adverse drug events averted during the pharmacy dispensing process. This approach holds promise as a starting point for analyzing clinical impact of administration errors.
Third, only six medication classes were sampled as the current study’s primary targets for auditing. The study excluded some drug classes, such as insulin. The six medication classes were therapies likely to require frequent order modifications to titrate to the desired therapeutic effect. Current study results may not generalize to orders that have fewer order modifications or to other classes of medications that were not analyzed. Fourth, other types of CPOE-associated administration errors may occur but were not counted in the present study. For example, an error may occur if clinicians fail to renew a medication with an “automatic” discontinuation interval (e.g. after 72 hours), e.g., if the clinician inappropriately ignores the renewal reminders generated by the system and the order automatically lapses. A final limitation of the study is that the study hospital is a large academic facility that had a fully implemented CPOE system, placing it in a very small minority (<9.6%) 26 of U.S. hospitals. The study site, VUH, also had developed its CPOE system, placing it in and even smaller minority.
Recommendations to Improve Medication Ordering and Administration Practices
The current study characterized a number of remediable causes of delayed medication administration that would not be addressed, per se, by nationally recommended safety measures, such as implementation of CPOE or BCMA.
Specific problems and approaches to prevent or correct them include:
-
1 Medication administration timing discrepancies and administration errors arose in part because of interactions among four key roles: the clinician who issued a medication order; the CPOE-system scheduler that processed it; the “downstream” pharmacy dispensing system that further processed, dispensed, and scheduled the medication administration; and, the standard medication administration practices of the patient’s nursing unit. Many of the problems observed in this study arose when the clinician, CPOE system, or pharmacy system did not know or understand the administration practices of the ward. For example, a medication ordered to be given “each morning” may be routinely administered at 8:00AM in the medical ICU, at 6:00AM on a surgical ward, and at 10:00AM on a sub-acute care unit. An order placed at 7:00AM to non-urgently start a new medication, to be given each morning, would start the next day on the previously noted surgical ward, but the day of order entry in the medical ICU and the sub-acute care unit (1 hour and 3 hours after order entry, respectively). Nurses might have shifted dosing schedules to begin today instead of tomorrow, if the nurse believed that doing so was in the patient’s best interest.
System developers and clinical end-users should alter templates for CPOE orders to better capture the ordering clinician’s sense of urgency for starting a medication. There has been a mismatch between the clinician’s goal for starting the order and the organization’s care-based process for starting the order. CPOE has been geared more toward the scheduling function of pharmacy dispensing systems, rather than to capturing the clinician’s expectation. The authors suggest that CPOE systems explicitly convey ordering physicians’ expectations for the time-criticality of medication administration, while at the same time incorporating flexibility in scheduling consistent with clinical urgency. This would allow nurses to focus on the time-critical therapies. Specifically, the authors believe that clinicians should express desired start times for CPOE medication orders as follows (based on their own experiences with CPOE, in addition to current study results):- a give first dose immediately (within 10 minutes) for potentially life-critical medications. Such orders would always require special efforts to assure that the nurse and pharmacy are aware of the order, e.g., requiring direct ordering provider to nurse verbal communication. Steps should be taken to rapidly procure and administer the medication, e.g., sending a “runner” to the pharmacy to rush the medication to the bedside, and disrupting the nurses’ normal sequence of tasks to give the medication. Such urgency might require a different nurse on the patient’s unit to give the medication if the primary nurse is otherwise engaged. An example would be an order to give intravenous 50% dextrose to a patient in hypoglycemic coma.
- b give first dose within 1 hour. This would allow standard (usually rapid) methods of delivery of the medication to the ward, but might require the nurse to administer the medication at a nonstandard time for “usual ward practices.” An example might be an order for an antibiotic that is being given for a non-life-threatening but serious infection, to start within one hour.
- c give first dose sometime today or within the next 12 hours, according to ward nursing schedule. An example would be an order for a medication that the patient was taking at home, for treating a stable, controlled condition, such as hydrochlorothiazide for controlled hypertension.
-
d give first dose within 24 hours, according to the ward’s nursing schedule. An example might be an order for a laxative of choice daily in a patient not suffering from constipation.With this prioritization, the pharmacy and nursing units could deliver medications in a manner that matched the ordering clinicians’ intentions for starting the new medication, and nurses would have realistic goals for the timely administration of medications.
2 The discrepancies between expected administration time and actual administration time raise the risk of duplicate, overlapping or conflicting orders. The study observed this phenomenon for orders for potassium and for diuretics. Although duplicate medication order alerts have been implemented in many CPOE systems, they sometimes cause so many false positives alerts (e.g. with different forms of insulin being administered at the same time) that this feature is “turned off.” The authors believe that all CPOE systems should change so as to alert users when they enter potentially duplicate orders for the same medication (at any dose), when separate doses of the medication are to be given within a “closely spaced time.” Such alerting should extend to warning when doses ordered for “now” overlap with recently administered one-time orders that were technically “discontinued” because the dose was given (and hence may not be readily visible in decision support that only tracks active orders). In addition to CPOE-based decision support, BCMA systems could also provide similar duplicate therapy alerting at the time of administration, which represents the final opportunity to avoid a potential adverse drug event.
3 When hospital, pharmacy, or unit policy requires that an ordered dose of a medication be administered as serial smaller aliquots (i.e., as several “split doses” rather than one larger, supra-maximal dose), CPOE systems should not allow clinicians to order an arbitrarily large composite dose with the expectation that the pharmacy will automatically split the dose. For example, the study sample included an order for “80 mEq of potassium chloride IV” which, as written, might be misinterpreted as a single 80 mEq dose by an individual not familiar with hospital policy. VUH hospital policy prevents the pharmacy from dispensing and nursing from administering more than 20 mEq of potassium chloride per hour in separate dose IV bags. In effect, the order would always be executed as four sub-orders. In fact, the traditional definition of administration errors would describe splitting the 80 mEq dose into 20 mEq doses as an error of “unexpected doses.” Obviously, composite orders in a CPOE system are problematic in execution.2 Although other safeguards prevented the potentially devastating consequences of an error in the administration of the intravenous potassium chloride, this dangerous medication is one where the Institute for Safe Medication Practices recommends extraordinary strategies. The risk of error is reduced if CPOE systems only allow clinicians to order the maximum “split size” dose allowed by policy (20 mEq/hour in the above example) as multiple, individual (e.g., “per hour”) doses. The split size dosing strategy has the further advantage of more directly matching the dose ordered to the projected administration for EMAR or BCMA systems.
4 Finally, the authors recommend that both CPOE systems and pharmacy dispensing systems be modified to accommodate the wide variety of medication administration schedules that occur on diverse hospital units. The CPOE system should be “forgiving” for routine and relatively safe therapies and incorporate procedures, reminders, and checklists for more dangerous medications. For example, when a clinician user enters an order for multiple potassium chloride infusions, the user could be required to view a graphical display of the patient’s serum potassium and serum creatinine values over the past week, and be shown a list of those medications that the patient has ordered that might affect potassium excretion (e.g. spironolactone or ACE inhibitors). The dosage and timing of each infusion could be constrained by the CPOE system to be within safe limits. Furthermore, the system might require ordering of “stat” serum potassium levels between each infusion.27, 28
The authors recommend future study of medication administration processes to determine, a classification of medications based on “timing criticality” for administration. Such criteria would pair indications for therapy specific medications and “window of opportunity” for both initial dosing and for variance from scheduled dose timing for subsequent recurring doses. For example, a patient receiving morphine for severe cancer related pain might only have a maximum allowed variance of 10–15 minutes from a specified dosing schedule, whereas a patient receiving daily hydrochlorothiazide for stable hypertension might have an allowed variance of up to 12 hours. Such research is beyond the scope of the present study, but could form a useful basis for alerts related to BCMA systems tied to CPOE systems in the future.
Conclusion
There has been a national expectation and hope that CPOE and BCMA will eliminate most medication administration errors. This study suggests that some important problems inherent in medication scheduling and administration may persist unless specific action is taken to address them.
Acknowledgments
The authors thank Ms. Joyce Green for her assistance with administrative aspects of the project and Drs. Joshua Denny and Kevin Johnson for help in reviewing this manuscript.
Footnotes
This work is supported in part by the National Institutes of Health, National Library of Medicine, grant 1 R01 LM007995-01 and by NIH Grant 1 R01 LM007995-01 from the National Library of Medicine.
References
- 1.Donaldson MS, Kohn LT, Corrigan J. To err is human: building a safer health systemWashington, D.C: National Academy Press; 2000. [PubMed]
- 2.Potts AL, Barr FE, Gregory DF, Wright L, Patel NR. Computerized physician order entry and medication errors in a pediatric critical care unit Pediatrics 2004;113(1 Pt 1):59-63. [DOI] [PubMed] [Google Scholar]
- 3.King WJ, Paice N, Rangrej J, Forestell GJ, Swartz R. The effect of computerized physician order entry on medication errors and adverse drug events in pediatric inpatients Pediatrics 2003;112(3 Pt 1):506-509. [DOI] [PubMed] [Google Scholar]
- 4.Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety: a systematic review Archives of internal medicine 2003;163(12):1409-1416. [DOI] [PubMed] [Google Scholar]
- 5.Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors JAMA 1998;280(15):1311-1316. [DOI] [PubMed] [Google Scholar]
- 6.Kuperman GJ, Teich JM, Gandhi TK, Bates DW. Patient safety and computerized medication ordering at Brigham and Women’s Hospital The Joint Commission journal on quality improvement 2001;27(10):509-521. [DOI] [PubMed] [Google Scholar]
- 7.Coyle GA, Heinen M. Evolution of BCMA within the Department of Veterans Affairs Nursing Administration Quarterly 2005;29(1):32-38. [DOI] [PubMed] [Google Scholar]
- 8.Oren E, Shaffer ER, Guglielmo BJ. Impact of emerging technologies on medication errors and adverse drug events Am J Health Syst Pharm 2003;60(14):1447-1458. [DOI] [PubMed] [Google Scholar]
- 9.Englebright JD, Franklin M. Managing a new medication administration process J Nursing Admin 2005;35(9):410-413. [DOI] [PubMed] [Google Scholar]
- 10.Johnson CL, Carlson RA, Tucker CL, Willette C. Using BCMA software to improve patient safety in Veterans Administration Medical Centers J Healthc Inf Manag 2002;16(1):46-51. [PubMed] [Google Scholar]
- 11.ASHP Standard definition of a medication error American journal of hospital pharmacy 1982;39(2):321. [PubMed] [Google Scholar]
- 12.Allan EL, Barker KN. Fundamentals of medication error research American journal of hospital pharmacy 1990;47(3):555-571. [PubMed] [Google Scholar]
- 13.Calabrese AD, Erstad BL, Brandl K, Barletta JF, Kane SL, Sherman DS. Medication administration errors in adult patients in the ICU Intensive Care Medicine 2001;27(10):1592-1598. [DOI] [PubMed] [Google Scholar]
- 14.van den Bemt PM, Fijn R, van der Voort PH, Gossen AA, Egberts TC, Brouwers JR. Frequency and determinants of drug administration errors in the intensive care unit Crit Care Med 2002;30(4):846-850. [DOI] [PubMed] [Google Scholar]
- 15.Grasso BC, Genest R, Jordan CW, Bates DW. Use of chart and record reviews to detect medication errors in a state psychiatric hospital PsychiatrServ 2003;54(5):677-681. [DOI] [PubMed] [Google Scholar]
- 16.Fontan JE, Maneglier V, Nguyen VX, Loirat C, Brion F. Medication errors in hospitals: computerized unit dose drug dispensing system versus ward stock distribution system PharmWorld Sci 2003;25(3):112-117. [DOI] [PubMed] [Google Scholar]
- 17.Mekhjian HS, Kumar RR, Kuehn L, Bentley TD, Teater P, Thomas A, et al. Immediate benefits realized following implementation of physician order entry at an academic medical center J Am Med Inform Assoc 2002;9(5):529-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cordero L, Kuehn L, Kumar RR, Mekhjian HS. Impact of computerized physician order entry on clinical practice in a newborn intensive care unit J Perinatol 2004;24(2):88-93. [DOI] [PubMed] [Google Scholar]
- 19.Lehman ML, Brill JH, Skarulis PC, Keller D, Lee C. Physician Order Entry impact on drug turn-around times AMIA Annu Symp Proc 2001:359-363. [PMC free article] [PubMed]
- 20.Jensen J. The Effects of Computerized Provider Order Entry on Medication Turn-around Time: A Time-to-first Dose Study at the Providence Portland Medical Center AMIA Annu Symp Proc 2006:384-388. [PMC free article] [PubMed]
- 21.Flynn EA, Barker KN, Pepper GA, Bates DW, Mikeal RL. Comparison of methods for detecting medication errors in 36 hospitals and skilled-nursing facilities Am J Health Syst Pharm 2002;59(5):436-446. [DOI] [PubMed] [Google Scholar]
- 22.Nelson NC, Evans RS, Samore MH, Gardner RM. Detection and prevention of medication errors using real-time bedside nurse charting J Am Med Inform Assoc 2005;12(4):390-397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davey P, Brown E, Fenelon L, Finch R, Gould I, Hartman G, et al. Interventions to improve antibiotic prescribing practices for hospital inpatients Cochrane database of systematic reviews (Online) 2005(4):CD003543. [DOI] [PubMed]
- 24.Hermida RC, Ayala DE, Calvo C, et al. Differing administration time-dependent effects of aspirin on blood pressure in dipper and non-dipper hypertensives Hypertension 2005;46(4):1060-1068. [DOI] [PubMed] [Google Scholar]
- 25.Poon EG, Cina JL, Churchill W, et al. Medication dispensing errors and potential adverse drug events before and after implementing bar code technology in the pharmacy Ann Intern Med 2006;145(6):426-434. [DOI] [PubMed] [Google Scholar]
- 26.Ash JS, Gorman PN, Seshadri V, Hersh WR. Computerized physician order entry in U.S. hospitals: results of a 2002 survey J Am Med Inform Assoc 2004;11(2):95-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuperman GJ, Bobb A, Payne TH, et al. Medication-related Clinical Decision Support in Computerized Provider Order Entry Systems: A Review J Am Med Inform Assoc 2007;14(1):29-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Horsky J, Kuperman GJ, Patel VL. Comprehensive Analysis of a Medication Dosing Error Related to CPOE J Am Med Inform Assoc 2005;12(4):377-382. [DOI] [PMC free article] [PubMed] [Google Scholar]