Abstract
Electronic prescribing has improved the quality and safety of care. One barrier preventing widespread adoption is the potential detrimental impact on workflow. We used time-motion techniques to compare prescribing times at three ambulatory care sites that used paper-based prescribing, desktop, or laptop e-prescribing. An observer timed all prescriber (n = 27) and staff (n = 42) tasks performed during a 4-hour period. At the sites with optional e-prescribing >75% of prescription-related events were performed electronically. Prescribers at e-prescribing sites spent less time writing, but time-savings were offset by increased computer tasks. After adjusting for site, prescriber and prescription type, e-prescribing tasks took marginally longer than hand written prescriptions (12.0 seconds; −1.6, 25.6 CI). Nursing staff at the e-prescribing sites spent longer on computer tasks (5.4 minutes/hour; 0.0, 10.7 CI). E-prescribing was not associated with an increase in combined computer and writing time for prescribers. If carefully implemented, e-prescribing will not greatly disrupt workflow.
Introduction
Although electronic prescribing (e-prescribing) has improved the quality and safety of patient care, several barriers have prevented widespread adoption. One significant barrier is the potential detrimental impact on physician and staff workflow. We evaluated the time-efficiency of e-prescribing in ambulatory care.
Background
Enthusiasm for the use of medical informatics as a tool to improve clinical decision-making and reduce medical errors began in the 1960’s. 1,2 Early visionaries of electronic health records (EHR) cited inclusion of note documentation, direct order entry and decision support capabilities as necessary elements to improve care. 3 By the late 1980’s vast improvements in technology generated more widespread interest and, in 1991, the Institute of Medicine published its landmark report on EHRs. 4 The report and its 1997 update 5 recommended that EHRs should support patient care, improve quality of care, enhance productivity of healthcare professionals, support research, accommodate future developments and ensure confidentiality.
Computerized physician order entry (CPOE) systems, including electronic prescribing (e-prescribing), are an integral component of the EHR. 6 Landmark studies have demonstrated the positive impact of e-prescribing systems in the reduction of medication errors and adverse drug events. 7–9 However, system design is crucial to avoid replacing old errors with new, computer-facilitated errors. 10,11 Adoption of EHRs in the ambulatory setting has been slow, 6,12–14 although data from 2005 indicate that momentum is picking up, in that one-quarter of office-based physicians report at least partial adoption of an EHR. 15
Many barriers have hindered the adoption of EHRs and e-prescribing systems, including the misalignment of financial incentives; 6,16 the high cost of purchase, implementation and maintenance of systems; 13,17 the immaturity of software products and vendors; 17,18 the lack of integration between EHR systems; 6 and physician resistance. 6,17 A survey conducted by the Massachusetts Medical Society in 2003 revealed a large gap between physicians’ perceived value of e-prescribing and their intent to adopt this practice. 6 Their reluctance to embrace the changeover from paper to computerized systems was based, in large part, on the perception that e-prescribing is time-inefficient. 6 To achieve acceptance and high adoption rates, e-prescribing systems must become as quick and easy to use as paper-based methods.
Few studies have evaluated the impact of CPOE on the workflow of physicians or nurses. 19–23 Studies that have been conducted have employed a variety of methods to capture time data. The CPOE systems evaluated varied greatly in their design and functionality. None focused exclusively on e-prescribing. Our study describes the effect of e-prescribing on physician and staff time. This information is important for ambulatory care clinics considering, or in the process of, implementing e-prescribing who are concerned about the potential impact on workflow.
Research Question
We designed a study to compare the time-efficiency of paper-based versus e-prescribing for physicians, and staff in ambulatory care clinics. In this baseline analysis, we present the results of a cross-sectional comparison of prescribing efficiency at three sites at different stages of e-prescribing implementation. We plan to conduct a controlled pre-post comparison once all three locations have adopted desktop e-prescribing at the point of care.
Methods
Setting
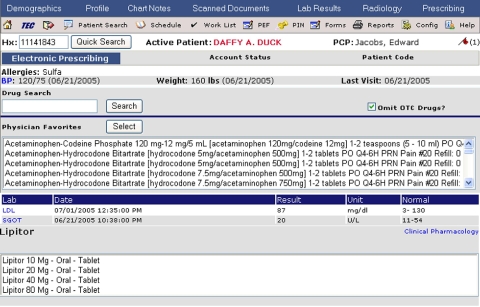
We collected data at The Everett Clinic (TEC), a multi-specialty integrated health-system with fourteen locations throughout the northern Puget Sound region. TEC employs 225 physicians and approximately 1,300 staff members. There are an estimated 2,300 patient visits each weekday; approximately 2.5 million prescriptions are written annually. TEC first implemented an internally-developed EHR system in 1995; adding modules and enhancements over time. At the time of study initiation, the system included chart notes, laboratory tests and imaging reports. Internally-developed e-prescribing capabilities have been rolled out to each of the fourteen TEC locations since 2003. The e-prescribing system uses point-and-click functionality and allows physicians to generate new or renewed prescriptions for their patients (▶). The e-prescribing system uses the Multum™ drug database (Cerner, Denver, CO) for medication and strength selection. Providers have the option of using pre-specified medication directions or writing free-text directions. The system obliges the prescriber to complete all prescription details before being able to sign it. These prescriptions can be printed out for the patient or e-faxed directly to any one of over 200 pharmacies. Prescriptions are automatically added to the patient’s EHR medication list. Discontinued medications, and reason for discontinuation, are also available for review. The e-prescribing system optimizes medication selection by providing an automatically generated list of physician-specific favorites, based on the TEC formulary, and by calculating appropriate weight-based, pediatric dosing. Clinic staff can use the system to initiate a prescription by filling in the pertinent information and sending the prescription to the provider for review and authorization. System security will not allow a prescription to be generated until it has been signed by a person licensed to prescribe medications. The system can be used to create patient registries for management of chronic disease states. To facilitate adoption, a basic e-prescribing system was implemented initially. Over time, enhancements such as drug-drug interaction checking and clinical decision support alerts for laboratory monitoring are added. These enhancements were not in place at the time of the study.
Figure 1.
Screen shot of e-prescribing system.
Study Design and Methods
Our study was conducted at three clinic sites: Silver Lake, that at the time of the data collection, did not have e-prescribing capabilities (SL-paper); Harbour Pointe, that had implemented e-prescribing via desktops in the physicians’ offices and at nursing stations (HP-desktop); and Snohomish, that had implemented e-prescribing on wireless laptops in the examination rooms and on desktops at nursing stations (SN-laptop). The e-prescribing sites in our study had been using the e-prescribing system for more than one year at the time of data collection. The three sites each had between 8 and 15 prescribers and 13 to 25 staff working in family practice, pediatric, internal medicine or walk-in clinics.
We used time-motion methods to evaluate prescriber and staff tasks. Time-motion methods are considered the gold standard, 24 as they capture the subject’s tasks continuously throughout a set time interval. An alternative method, known as work-sampling, records the tasks being performed by subjects at randomly selected time intervals throughout the work day. 24,25 Work-sampling is less resource intensive and allows several subjects to be tracked during the day, but risks missing infrequent tasks of interest, such as prescriptions.
Training
We collected data sequentially at each site between February 2005 and January 2006. A total of six observers collected data. Each observer received training in time-motion methods and use of the data collection instrument. This training involved several hours of data collection on a physician at a fourth clinic location not included in the study. After the training session, the observers were encouraged to ask questions about the appropriate categorization of clinical tasks and any other issues. If necessary, a second training session was arranged for further familiarization with data collection.
At each site we organized a pre-study meeting where prescribers (physicians, physician’s assistants and advanced registered nurse practitioners) and staff [registered nurses (RNs), medical assistants (MAs)] were informed of the goals of the study and the precautions taken to maintain confidentiality. At the meeting, we asked for written informed consent to participate in the study. The majority of prescribers (82%) and staff (71%) consented. We followed each consenting participant during one morning (approximately 8:00 am–12:00 noon) or afternoon (1:00 pm–5:00 pm) period. During that period, all patients scheduled to see the prescriber or staff member were given a study information sheet. Each patient was asked to provide oral consent for the observer to be present during the consultation. At the request of the prescriber, staff member or the patient, the observation could be stopped and continued once the subject had moved on to a different task. These unobserved time periods were excluded from the analysis. The University of Washington Human Subjects Committee approved all study procedures.
Data Collection
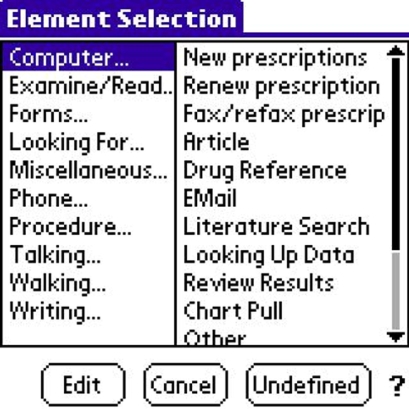
We collected data using Timer Pro™ software (Applied Computer Services Inc., Englewood, CO) on a Palm® Tungsten handheld PDA device. The software allowed the observer to select a task from a list of major and minor task categories (▶). Timing began as soon as the major task category was selected with the stylus. If a task category was selected erroneously, the observer could over-write the original selection without pausing the timing. The observer could also add notes to describe the task being performed. Timing for one task ended as soon as the observer selected a new task category. Data stored on the PDA were downloaded into Excel® 2000 (Microsoft Corp, Redmond, WA) for analysis.
Figure 2.
Screen from the Palm® PDA showing the major task categories and the computer-related minor task categories.
We used the task categories defined by Overhage et al. in their time-motion study of ambulatory care physicians. 20 The observer first selects the major category of task that is being performed (e.g., writing, computer, phone, talking, walking, examining) and then selects the minor task category being undertaken (e.g., writing: charts, computer: e-mail). Overhage defined 72 specific tasks that a physician might perform. We modified the minor-task categories slightly in order to more fully reflect tasks related to prescribing (e.g., new or renew prescription, fax prescription), and tasks that are performed by staff (e.g., schedule appointment) (see Appendix for full task list). For analyses, each specific task can be grouped into overall task types: direct patient care, indirect patient care (reading, writing or other), administrative or miscellaneous.
Statistical Analyses
Our aim was to measure whether e-prescribing was time-neutral for prescribers and staff. First, we measured the impact of e-prescribing on overall workflow by examining time spent on major task categories (e.g., computing, writing tasks). We used unpaired t-tests to calculate the mean difference and 95% confidence interval (95% CI) in the minutes per hour that prescribers and staff spent on various task categories at the e-prescribing versus the paper-based prescribing site. Second, we selected two specific prescription-related events performed by prescribers (new and renew prescriptions) and compared the amount of time it took to perform these tasks by computer versus by hand. A prescription-related event could comprise more than one prescription if multiple medications were written on the same script or entered in the computer consecutively. We used a linear mixed effects model clustered by prescriber to compare prescription event times, after adjusting for intra-site random effects and an indicator for the fixed effect of prescription type (new or renewed). Third, we used unpaired t-tests to compare the minutes per hour that staff spent on the phone or at the facsimile machine communicating with the pharmacy at the e-prescribing and paper-based prescribing sites. Finally, we calculated the proportion of prescriber and staff time spent in direct patient care, indirect patient care, administrative and miscellaneous tasks. We externally validated our time motion data by comparing it to data captured electronically in the practice management system. All analyses were conducted in SPSS® 13.0 or R™ statistical software.
Results
Almost 82% (27/33) of prescribers consented to participate in the study (▶). The practice-specialty distribution of participating prescribers was similar at each site. We observed prescribers for an average of 3.6 hours. We were unable to observe prescribers for a mean of 13 minutes due to patient or prescriber request. 71% (42/59) of staff consented to participate. The average number of hours per observation was similar to that in the prescribers group.
Table 1.
Table 1 Characteristics of Prescribers, RNs/MAs, and Staff
| SL—Paper | HP—Desktop | SN—Laptop | Total | |
|---|---|---|---|---|
| Prescribers |
||||
| Consented (%) | 8/10 (80%) | 11/15 (73%) | 8/8 (100%) | 27/33 (82%) |
| Specialty | ||||
| Family Practice | 3 | 4 | 4 | 11 |
| Pediatrics | 1 | 2 | 1 | 4 |
| WIC | 2 | 2 | 1 | 5 |
| Internal Med | 2 | 3 | 2 | 7 |
| Females (%) | 3 (38%) | 3 (27%) | 5 (63%) | 11/27 (41%) |
| Mean Age in Years | 44 | 46 | 46 | 45 |
| Mean Hours Observed | 3.54 | 3.61 | 3.81 | 3.65 |
| Mean Time Unable to Observe | 19.8 mins | 12.7 mins | 7.7 mins | 13.3 mins |
| Staff |
||||
| RNs: 7 | RNs: 12 | RNs: 3 | RNs: 22 | |
| MAs: 4 | MAs: 9 | MAs: 7 | MAs: 20 | |
| Number Observed/Number of Potential Subjects (%) | 11/21 (52%) | 21/25 (84%) | 10/13 (77%) | 42/59 (71%) |
| % Female | 11/11 (100%) | 20/21 (95%) | 10/10 (100%) | 41/42 (98%) |
| Mean Age | 44 | 37 | 49 | 43 |
| Mean Hours Observed | 3.52 | 3.61 | 3.77 | 3.62 |
| Mean Time Unable to Observe | 1.0 mins | 1.9 mins | 0.5 mins | 1.3 mins |
MA = medical assistant; mins = minutes; RN = Registered nurse; WIC = Walk-in clinic; SL = Silver Lake; HP = Harbour Pointe; SN = Snohomish.
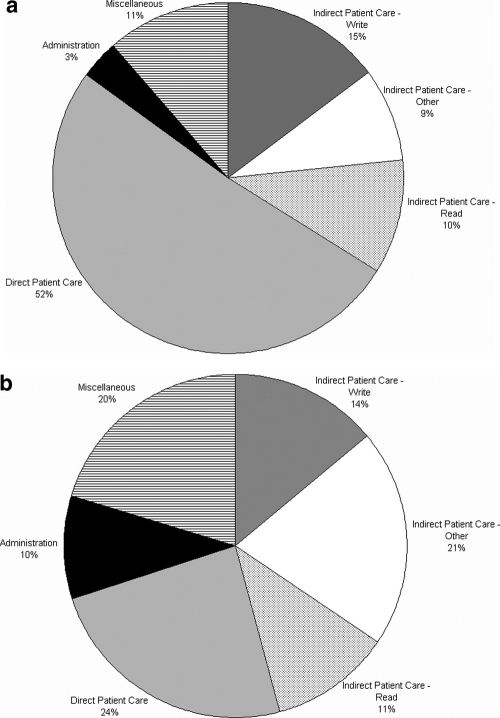
Prescriber Time
At all three sites combined, about one half of prescriber time was spent on direct patient care activities such as taking the patient’s medical history, examining and educating the patient (▶a). A further one third of time was spent on indirect patient care; most commonly these were activities such as reading or writing in the chart and dictating notes. The remaining 15 percent of time was spent on administrative or miscellaneous activities such as talking with colleagues, walking inside the clinic and checking e-mail.
Figure 3.
a) Task categories of prescribers; b) Task categories of staff.
On average, prescribers at the two e-prescribing sites spent significantly less time less per hour (−3.0 minutes; −5.6, −0.2 CI) on writing tasks than prescribers at the paper-based site (▶). Conversely, prescribers at the e-prescribing sites spent more time per hour on computer-based tasks (3.9 minutes; 0.3, 7.5 CI). These changes offset each other, there was no significant increase in the total amount of time spent on handwritten and computing tasks, combined, at the e-prescribing sites (1.0 minutes; −3.4, 5.3). There was variation between sites in other task categories. Prescribers at the paper-based site spent a higher proportion of their time examining patients and relatively less time talking with colleagues (▶).
Table 2.
Table 2 Prescribers’ Time Spent on Specific Task Categories ∗
| Task Category | SL—Paper Mins. per Hr (n = 8) | HP—Desktop Mins. per Hr (n = 11) | SN—Laptop Mins. per Hr (n = 8) | Weighted Mean Difference (95% CI) Between e-prescribing and Paper-based Sites Mins. per Hr |
|---|---|---|---|---|
| Computer Tasks | 3.8 | 7.4 | 8.1 | 3.9 (0.3, 7.5)† |
| Writing Tasks | 8.7 | 5.5 | 5.9 | −3.0 (−5.6, −0.2)† |
| Computer and Writing Tasks, combined† | 12.4 | 12.9 | 14.0 | 1.0 (−3.4, 5.3) |
| Talking to Patient or Family | 19.0 | 17.8 | 20.3 | −0.1 (−5.5, 5.2) |
| Talking Colleague/Other | 6.6 | 11.6 | 8.2 | 3.6 (−0.2, 7.3) |
| Examining Patient | 8.9 | 4.9 | 5.3 | −3.8 (−5.8, −1.9)† |
| Examine Chart/Other | 6.1 | 5.7 | 5.3 | −0.6 (−2.7, 1.5) |
| Other Tasks—Total | 0.2 (−3.2, 3.6) | |||
| Procedure | 2.1 | 1.5 | 1.9 | |
| Phone Colleague/Other | 0.5 | 1.0 | 1.0 | |
| Walking | 1.3 | 1.0 | 1.5 | |
| Looking For | 0.5 | 0.9 | 0.7 | |
| Phone Patient | 0.3 | 1.2 | 1.0 | |
| Other | 1.3 | 1.6 | 0.8 |
∗ We provide detail on task categories that took up ≥7.5% of time at one or more site. Other tasks are grouped as ‘other’.
† p < 0.05.
SL = Silver Lake; HP = Harbour Pointe; SN = Snohomish.
During the observation period, prescribers performed 242 prescription-related events at all sites (▶). Over 69 percent of events related to new prescriptions (168/242). At the two sites with optional e-prescribing, between 75% and 86% of prescription events were written electronically. On average, prescription events took longer at the site that used laptop e-prescribing. However, this phenomenon was not limited to e-prescriptions; hand-written new prescriptions also took longer at this site. After adjustment for site, prescriber and type of prescription (new/renew) handwritten prescription events took fractionally less time than e-prescription events (adjusted mean difference: 12.0 seconds; −1.6, 25.6 CI).
Table 3.
Table 3 Prescription-related Events (Prescribers)
| Hand Written Prescription Event Seconds per Event (n) | e-prescription Event Seconds per Event (n) | Adjusted Mean Difference ∗ | |
|---|---|---|---|
| SL—Paper | 47.6 (68) | N/A (0) | — |
| HP—Desktop | 38.1 (26) | 43.6 (79) | 9.5 (−9.8, 28.8) |
| SN—Laptop | 63.1 (10) | 72.5 (59) | 9.8 (−23.4, 43.1) |
| All Sites | 46.7 (104) | 56.0 (138) | 12.0 (−1.6, 25.6) |
| New Prescriptions | 45.6 (88) | 61.2 (80) | 15.4 (−10.4, 41.2) |
| Renew Prescriptions | 52.9 (16) | 48.7 (58) | 4.0 (−17.9, 26.0) |
∗ Mean additional time spent for an e-prescription compared to a handwritten prescription calculated from the linear mixed effects model adjusting for prescriber and type of prescription (new/renew).
SL = Silver Lake; HP = Harbour Pointe; SN = Snohomish.
Staff Time
Compared to prescribers, staff spent a greater proportion of their time (30 percent) on administrative and miscellaneous tasks (▶b). Most frequently, these activities involved talking to colleagues, walking inside the clinic, examining the schedule and sorting paperwork. A greater proportion of their time was also spent on other forms of indirect patient care such as speaking with patients on the telephone. Direct patient care was more limited and most frequently involved taking the patient’s medical history, measuring weight and blood pressure, and giving vaccinations.
In comparison to medical assistants, registered nurses tended to spend a larger proportion of their time on computer-based tasks and speaking to patients on the telephone (▶). Nurses at the e-prescribing sites spent approximately five minutes more per hour on the computer than their counterparts at the paper-based site (5.4 minutes; 0.0, 10.7 (CI)). Although nurses spent slightly less time on writing tasks (−0.9 minutes; −2.5, 0.7 (CI)) at the e-prescribing sites, this was not statistically significant and did not offset additional computing time. Nurses at the paper-based site spent more time on other miscellaneous tasks, most frequently, restocking examination rooms, examining patients, looking for charts, or unoccupied. At all three sites combined, nurses spent only a small proportion of their time (1.1 minutes per hour) on prescription or formulary related facsimiles or phone calls, there was no significant difference in this proportion between e-prescribing and paper-based sites (weighted mean difference, −0.2 minutes; −1.3, 1.0 (CI)).
Table 4.
Table 4 Staff Time Spent on Specific Task Categories ∗
| Task Category | Registered Nurses |
Medical Assistants |
||||||
|---|---|---|---|---|---|---|---|---|
| SL—Paper Mins. per Hr (n = 7) | HP—Desktop Mins. per Hr (n = 12) | SN—Laptop Mins. per Hr (n = 3) | Weighted Mean Difference (95% CI) Mins. per Hr | SL—Paper Mins. per Hr (n = 4) | HP—Desktop Mins. per Hr (n = 9) | SN—Laptop Mins. per Hr (n = 7) | Weighted Mean Difference (95% CI) Mins. per Hr | |
| Computer Tasks | 12.1 | 17.8 | 16.1 | 5.4 (0.0, 10.7)† | 5.9 | 9.7 | 8.9 | 3.4 (−0.1, 7.0) |
| Writing Tasks | 4.7 | 3.9 | 3.3 | −0.9 (−2.5, 0.7) | 4.5 | 5.3 | 2.4 | −0.4 (−6.2, 5.4) |
| Computer and Writing Tasks, combined ∗ | 16.9 | 21.7 | 19.4 | 4.4 (−2.2, 11.0) | 10.4 | 15.0 | 11.3 | 3.0 (−1.9, 7.9) |
| Talking Colleague/Other | 8.4 | 7.9 | 7.2 | −0.7 (−5.0, 3.5) | 12.9 | 15.7 | 7.4 | −0.8 (−7.8, 6.2) |
| Examine Chart/Other | 4.6 | 6.2 | 2.0 | 0.8 (−2.1, 3.6) | 3.9 | 10.3 | 7.8 | 5.3 (0.6, 9.9)‡ |
| Phone Colleague/Other | 5.4 | 8.0 | 7.2 | 2.4 (−1.7, 6.5) | 3.0 | 4.3 | 3.8 | 1.1 (−2.1, 4.3) |
| Walking | 4.4 | 3.9 | 2.3 | −0.9 (−2.5, 0.7) | 5.7 | 6.1 | 5.6 | 0.2 (−3.1, 3.5) |
| Talking to Patient or Family | 3.5 | 0.8 | 3.3 | −2.2 (−5.1, 0.7) | 3.5 | 0.7 | 10.3 | 1.4 (−2.2, 5.0) |
| Phone Patient | 7.1 | 6.5 | 7.5 | −0.4 (−4.7, 3.8) | 0.9 | 0.1 | 2.1 | 0.1 (−1.9, 2.1) |
| Procedure | 2.5 | 3.1 | 6.9 | 1.3 (−1.5, 4.2) | 3.1 | 1.9 | 5.9 | 0.6 (−3.5, 4.7) |
| Other, miscellaneous | 7.2 | 2.1 | 4.2 | −3.4 (−5.1, −1.7)‡ | 16.7 | 5.9 | 5.9 | −10.8 (−27.0, 5.5) |
| Prescription or formulary related fax or phone call | 1.2 | 1.0 | 1.3 | −0.2 (−1.3, 1.0) | 0.3 | 1.0 | 0.8 | 0.6 (−0.4, 1.5) |
∗ We provide detail on task categories that took up ≥7.5% of time at one or more site. Other tasks are grouped as ‘other’.
‡ P ≤ 0.05.
SL = Silver Lake; HP = Harbour Pointe; SN = Snohomish.
There was a non-significant trend for medical assistants at the e-prescribing sites to spend a higher proportion of their time on computer-based tasks (3.4 minutes; −0.1, 7.0 (CI)). Medical assistants at the e-prescribing sites also spent significantly more time examining charts and paperwork (5.3 minutes, 0.6, 9.9 (CI)). The large difference in medical assistant time spent on other miscellaneous tasks was not statistically significant and largely due to one staff member who spent a substantial period unoccupied due to patient non-attendance. There was no significant difference between e-prescribing and paper-based sites in the proportion of time that medical assistants spent on prescription or formulary related facsimiles or phone calls (0.6 minutes; −0.4, 1.5 (CI)).
Discussion
The results of our study revealed that e-prescribing did not greatly disrupt prescriber or staff workflow. Prescribers and staff spent more time on the computer at the e-prescribing sites, but, for prescribers, this additional time was compensated for by less time making written notes and orders. It is likely that the introduction of e-prescribing coincided with and reinforced a general shift in physician work patterns away from paper-based methods and toward computerization. The relatively high utilization of e-prescribing at the two sites where it was optional suggests general acceptance of this method among prescribers.
National data indicate that, in 2004, 64% of ambulatory care visits included an order for one or more new or continued medication; 26 this proportion has remained relatively stable over time. 27 In 2004, an average of 1.7 medications were ordered per ambulatory care visit, 26 an increase from 1.2 medications per visit in 1991. 27 Given the increasing volume of prescriptions in ambulatory care, it is essential that e-prescribing does not introduce any additional burden on physician or staff time. We did not find evidence to support the statement of Schade et al. 14 that fully implemented e-prescribing will offer substantial savings in physician and office staff time. We found that the mean time spent per prescription-related event was approximately 12 seconds longer for e-prescribing events. Although this result was not statistically significant, such an increase per prescription-related event may be clinically important. The 27 prescribers performed an average of 9 prescription-related events during the 3.5 hour observation period, suggesting that, over the course of the day, e-prescribing might contribute an additional 3 to 5 minutes to clinicians’ time. In our view, this small increment can be justified if e-prescribing improves the safety and quality of patient care.
Both nurses and medical assistants at the e-prescribing sites spent more time on computer tasks. E-prescribing, that allows computer-faxing directly to the retail pharmacy, may minimize transcription errors and improve the transmission process. This, in turn may benefit clinic support staff by reducing the amount of time spent phoning or faxing prescriptions to the pharmacy. However in our observations of staff, we did not find any substantial differences in the amount of time they spent using the fax machine or conducting pharmacy related telephone conversations. At all three sites, these tasks comprised a very small proportion (<2%) of the day. This finding is contrary to anecdotal evidence suggesting that prescriptions, particularly requests for renewals, are a time consuming task for clinic staff. 28 In part, this discrepancy might be due to the difficulty in adequately categorizing multi-layered and overlapping activities using time motion methods. For example, a ten minute telephone call from a patient primarily discussing symptoms might, in fact, be a pretext for a prescription renewal request. Therefore some activities, indirectly related to prescriptions, might be categorized under “phone patient” in our analysis. However, time spent on this task category did not differ significantly between staff at the paper-based and e-prescribing clinics.
The complete impact of e-prescribing on the clinic workforce is difficult to fully quantify. The increasing reliance on computers, particularly evident among the nurses in our study, may influence job satisfaction and outlook even if it does not introduce any workflow inefficiencies. Therefore, in concurrent work we are conducting focus groups with staff and prescribers to evaluate their expectations of e-prescribing prior to implementation and, subsequently, their views after implementation.
We tracked prescriber, nurse and medical assistant activities because they are an essential part of the ambulatory clinic team and deal with the bulk of prescription activities. Other groups will also be affected by e-prescribing. For example, receptionists, pharmacists and patients are involved in the process of safely and efficiently filling a prescription. Evaluation of all of these groups was beyond the scope of this cross-sectional study. However, we intend to conduct a before and after evaluation of receptionists at the clinic transitioning from paper-based to e-prescriptions in order to measure the impact of e-prescribing on tasks such as routing incoming prescription renewal requests to prescribers and faxing responses back to the pharmacy.
E-prescribing has the potential to be an important step toward improving the quality of patient care. Work in the inpatient setting has demonstrated a 55 percent reduction in the rate of serious medication errors following the introduction of computerized prescribing. 7 Evidence of the benefit of e-prescribing in the ambulatory setting is scarce. In one of the few studies to address this issue, Gandhi et al. found a non-significant trend toward lower error rates at clinics with basic e-prescribing systems compared to clinics with paper-based prescribing. 29 She and her colleagues have suggested that more sophisticated e-prescribing products that feature safety alerts, formulary alerts, dose calculators, and medication selection aids may be necessary to significantly reduce error rates in the ambulatory setting. However, each additional feature requires extra attention by prescribers. Non-specific alerts that raise frequent, petty or even false alarms will waste time and be ignored. 30,31 Given that prescriber buy-in is vital, it will be important to measure the impact of more sophisticated e-prescribing systems on clinicians’ time.
A recent systematic review identified twelve studies that compared the time-efficiency of paper-based records and EHR systems for physicians. 32 Few studies were based in the ambulatory setting 20,23 and none was focused solely on e-prescribing. These studies employed a variety of methods (i.e., work sampling, time-motion, surveys) to capture data. The EHR systems evaluated in each study were different in scope. Given this heterogeneity, it is not surprising that the results varied widely from a 22 percent reduction to a 328 percent increase in physician time, associated with the use of an EHR. Only three of the twelve studies reported that EHR resulted in physician time-savings. This demonstrates that, in many cases, physician concerns about the detrimental impact of EHRs on workflow are justified. On the other hand, it also indicates that an EHR does not inevitably introduce inefficiencies for physicians. Our primary result was that the average e-prescription took 12 seconds (27%) longer than a handwritten prescription, although this difference was not statistically significant. This finding falls well within the range reported by the systematic review. 32 Our results suggest that well-designed EHRs and e-prescribing systems might result in important improvements in the quality of care without greatly disrupting prescriber workflow.
One limitation of our study is that we were unable to track prescribing-related work that was conducted from home or beyond the four hour observation periods. Data from the e-prescribing system indicate that, during the period of our study, 84% of prescriptions at the two e-prescribing sites were performed between 8 AM and 5 PM. Our prescribers report that one of the primary efficiencies of e-prescribing is the ability to authorize renewals and send e-faxes from home.
Timing of clinical activities can be problematic when the individual observed is multi-tasking, for example writing a prescription and talking to a patient, or when the individual switches rapidly back and forth between two overlapping tasks. In these situations we standardized data collection by instructing the observer to prioritize prescription-related activities. Additionally, it was difficult for observers to identify all prescription-related events. Some non-specific tasks, for example locating medical charts, may, in fact, be caused by a need to look up past medications, but it is impossible for passive observers to definitively categorize them as prescription-related.
A limitation of our cross-sectional study design is that it is difficult to control for differences between clinics, other than e-prescribing, which might influence work patterns. To minimize this problem we selected three similar sized sites from the same integrated health system that had a similar mix of medical specialties. The fact that e-prescriptions took marginally longer both between sites and within sites where e-prescribing was optional suggests that differences are truly related to the e-prescribing system. We intend to conduct a follow up time-motion study after all three sites have switched to using the e-prescribing system at the point of care, to assess whether our initial findings are confirmed.
Time motion data rely on observers being able to reliably and unobtrusively categorize tasks. We provided training for all observers, but did not formally test inter-observer agreement. Overhage et al and Pizziferri et al have also studied ambulatory care physicians using almost identical data collection methods. 20,23 Comparison of our results to the range observed in the previous two studies provides support for the validity of time motion methods used. The proportions of physician time spent on direct patient care (52% in our study; 46%–49% range in previous studies), indirect patient care (34%; 33%–37% range), administration (3%; 2%–2% range) and miscellaneous tasks (11%; 12%–20% range) were similar between the three studies.
It is unclear why both hand written and electronic prescriptions took longer at the site with optional laptop prescribing. This may be due to differences in the types of medications prescribed, number of medications per script, or inter-physician variance in prescribing manner. Follow up data, once all sites have adopted desktop e-prescribing in the examination room, will allow us to explore this issue. Potentially, the availability of desktop computers at the point of care will improve the efficiency of e-prescribing by reducing time spent accessing the nearest terminal and minimizing the connectivity problems that can occur with wireless laptop prescribing.
It is difficult to assess the generalizability of our findings. Our study was set in community clinics that are not affiliated with large teaching hospitals. In this respect, we believe our findings will be relevant to many other community clinics that are currently considering investing in e-prescribing. Our data include many young patients attending pediatric and family medicine clinics. The number of medications per visit increases markedly after age 45, 26 therefore differences in the efficiency of hand written and e-prescriptions would be magnified at clinics with more elderly patients. Finally, our results are limited to an internally-developed e-prescribing system that had not implemented several clinical decision support functions (e.g. safety alerts, diagnosis-based reminders). We anticipate that many of these features would lead to longer e-prescribing times, which in some cases may not be justified by reductions in medication errors.
Conclusion
Two ambulatory clinic sites have successfully implemented e-prescribing. E-prescriptions were not associated with an increase in the total amount of time that prescribers spent on computer- and writing-tasks. There was no statistically significant increase in the time taken to accomplish e-prescriptions compared to handwritten prescriptions. These results suggest that carefully implemented e-prescribing will not greatly disrupt the workflow of prescribers and that this should not be a substantial barrier to the adoption of e-prescribing. This, coupled with the benefits in quality and safety, provide encouraging information to those planning to implement this emerging technology.
Footnotes
Funding for this research was provided by the Agency for Healthcare Research and Quality (AHRQ Grant number: 5UC1HS015319). The authors are grateful to Dr Al Fisk for his help in the design and implementation of the study at the Everett Clinic. Marie Bach and Julie Jaeger provided valuable assistance in collecting time-motion data. We also thank the physicians, clinic staff, and patients of the Everett Clinic for allowing us to collect the time and motion data on clinical activity. Preliminary data from this paper were presented at the AHRQ Patient Safety and Health IT Conference (Washington DC, June 4–7th 2006). The views expressed in this paper are solely those of the authors.
References
- 1.Lindberg DA. National Library of Medicine: the view at 150 years J Am Soc Inf Sci 1987;38(1):34-39. [DOI] [PubMed] [Google Scholar]
- 2.McDonald CJ. Protocol-based computer reminders, the quality of care and the non-perfectability of man N Engl J Med 1976;295(24):1351-1355. [DOI] [PubMed] [Google Scholar]
- 3.Berner ES, Detmer DE, Simborg D. Will the wave finally break?A brief view of the adoption of electronic medical records in the United States. J Am Med Inform Assoc 2005;12(1):3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dick RS, Steen EB. The Computer-Based Patient Record: An Essential Technology for Health Care, Revised EditionWashington, DC: National Academies Press; 1991. [PubMed]
- 5.Dick RS, Steen EB, Detmer DE. The Computer-Based Patient Record: An Essential Technology for Health Care, Revised EditionWashington, DC: National Academies Press; 1997. [PubMed]
- 6.Ash JS, Bates DW. Factors and forces affecting EHR system adoption: report of a 2004 ACMI discussion J Am Med Inform Assoc 2005;12(1):8-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bates DW, Leape LL, Cullen DJ, Laird N, Petersen LA, Teich JM, et al. Effect of computerized physician order entry and a team intervention on prevention of serious medication errors JAMA 1998;280(15):1311-1316. [DOI] [PubMed] [Google Scholar]
- 8.Bates DW, Teich JM, Lee J, Seger D, Kuperman GJ, Ma’Luf N, et al. The impact of computerized physician order entry on medication error prevention J Am Med Inform Assoc 1999;6(4):313-321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Teich JM, Merchia PR, Schmiz JL, Kuperman GJ, Spurr CD, Bates DW. Effects of computerized physician order entry on prescribing practices Arch Intern Med 2000;160(18):2741-2747. [DOI] [PubMed] [Google Scholar]
- 10.Han YY, Carcillo JA, Venkataraman ST, Clark RS, Watson RS, Nguyen TC, et al. Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system Pediatrics 2005;116(6):1506-1512. [DOI] [PubMed] [Google Scholar]
- 11.Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, et al. Role of computerized physician order entry systems in facilitating medication errors JAMA 2005;293(10):1197-1203. [DOI] [PubMed] [Google Scholar]
- 12.eHealth Initiative Electronic prescribing: Toward maximum value and rapid adoptionWashington, DC: eHealth Initiative; 2004.
- 13.Gans D, Kralewski J, Hammons T, Dowd B. Medical groups’ adoption of electronic health records and information systemsPractices are encountering greater-than-expected barriers to adopting an EHR system, but the adoption rate continues to rise. Health Aff (Millwood) 2005;24(5):1323-1333. [DOI] [PubMed] [Google Scholar]
- 14.Schade CP, Sullivan FM, de Lusignan S, Madeley J. e-Prescribing, efficiency, quality: lessons from the computerization of UK family practice J Am Med Inform Assoc 2006;13(5):470-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Burt CW, Hing E, Woodwell D. Electronic medical record use by office-based physiciansUnited States: National Center for Health Statistics; 2005.
- 16.Middleton B, Hammond WE, Brennan PF, Cooper GF. Accelerating U.S. EHR adoption: how to get there from here. recommendations based on the 2004 ACMI retreat J Am Med Inform Assoc 2005;12(1):13-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Poon EG, Blumenthal D, Jaggi T, Honour MM, Bates DW, Kaushal R. Overcoming barriers to adopting and implementing computerized physician order entry systems in U.S. hospitals Health Aff (Millwood) 2004;23(4):184-190. [DOI] [PubMed] [Google Scholar]
- 18.Halamka J, Aranow M, Ascenzo C, Bates DW, Berry K, Debor G, et al. E-Prescribing collaboration in Massachusetts: early experiences from regional prescribing projects J Am Med Inform Assoc 2006;13(3):239-244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bates DW, Boyle DL, Teich JM. Impact of computerized physician order entry on physician time Proc Annu Symp Comput Appl Med Care 1994:996. [PMC free article] [PubMed]
- 20.Overhage JM, Perkins S, Tierney WM, McDonald CJ. Controlled trial of direct physician order entry: effects on physicians’ time utilization in ambulatory primary care internal medicine practices J Am Med Inform Assoc 2001;8(4):361-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shu K, Boyle D, Spurr C, Horsky J, Heiman H, O’Connor P, et al. Comparison of time spent writing orders on paper with computerized physician order entry Medinfo 2001;10(Pt 2):1207-1211. [PubMed] [Google Scholar]
- 22.Tierney WM, Miller ME, Overhage JM, McDonald CJ. Physician inpatient order writing on microcomputer workstationsEffects on resource utilization. JAMA 1993;269(3):379-383. [PubMed] [Google Scholar]
- 23.Pizziferri L, Kittler AF, Volk LA, Honour MM, Gupta S, Wang S, et al. Primary care physician time utilization before and after implementation of an electronic health record: a time-motion study J Biomed Inform 2005;38(3):176-188. [DOI] [PubMed] [Google Scholar]
- 24.Finkler SA, Knickman JR, Hendrickson G, Lipkin Jr. M, Thompson WG. A comparison of work-sampling and time-and-motion techniques for studies in health services research Health Serv Res 1993;28(5):577-597. [PMC free article] [PubMed] [Google Scholar]
- 25.Sittig DF. Work-sampling: a statistical approach to evaluation of the effect of computers on work patterns in healthcare Methods Inf Med 1993;32(2):167-174. [PubMed] [Google Scholar]
- 26.Hing E, Cherry DK, Woodwell DA. National Ambulatory Medical Care Survey: 2004 summary Adv Data 2006;374:1-33. [PubMed] [Google Scholar]
- 27.Schappert SM. National Ambulatory Medical Care Survey: 1991 summary Vital Health Stat 1994;13(116):1-110. [PubMed] [Google Scholar]
- 28.Lowes R. Streamlining Rx renewal requests Med Econ 2005;82(3):50-51. [PubMed] [Google Scholar]
- 29.Gandhi TK, Weingart SN, Seger AC, Borus J, Burdick E, Poon EG, et al. Outpatient prescribing errors and the impact of computerized prescribing J Gen Intern Med 2005;20(9):837-841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.van der Sijs H, Aarts J, Vulto A, Berg M. Overriding of drug safety alerts in computerized physician order entry J Am Med Inform Assoc 2006;13(2):138-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Weingart SN, Toth M, Sands DZ, Aronson, MD, Davis RB, Phillips RS. Physicians’ decisions to override computerized drug alerts in primary care Arch Intern Med 2003;163(21):2625-2631. [DOI] [PubMed] [Google Scholar]
- 32.Poissant L, Pereira J, Tamblyn R, Kawasumi Y. The impact of electronic health records on time efficiency of physicians and nurses: a systematic review J Am Med Inform Assoc 2005;12(5):505-516. [DOI] [PMC free article] [PubMed] [Google Scholar]