Abstract
Degenerative changes of the cervical spine are commonly accompanied by a reduction or loss of the segmental or global lordosis, and are often considered to be a cause of neck pain. Nonetheless, such changes may also remain clinically silent. The aim of this study was to examine the correlation between the presence of neck pain and alterations of the normal cervical lordosis in people aged over 45 years. One hundred and seven volunteers, who were otherwise undergoing treatment for lower extremity problems in our hospital, took part. Sagittal radiographs of the cervical spine were taken and a questionnaire was completed, enquiring about neck pain and disability in the last 12 months. Based on the latter, subjects were divided into a group with neck pain (N = 54) and a group without neck pain (N = 53). The global curvature of the cervical spine (C2–C7) and each segmental angle were measured from the radiographs, using the posterior tangent method, and examined in relation to neck complaints. No significant difference between the two groups could be found in relation to the global curvature, the segmental angles, or the incidence of straight-spine or kyphotic deformity (P > 0.05). Twenty-three per cent of the people with neck pain and 17% of those without neck pain showed a segmental kyphosis deformity of more than 4° in at least one segment—most frequently at C4/5, closely followed by C5/6 and C3/4. The average segmental angle at the kyphotic level was 6.5° in the pain group and 6.3° in the group without pain, with a range of 5–10° in each group. In the group with neck pain, there was no association between any of the clinical characteristics (duration, frequency, intensity of pain; radiating pain; sensory/motor disturbances; disability; healthcare utilisation) and either global cervical curvature or segmental angles. The presence of such structural abnormalities in the patient with neck pain must be considered coincidental, i.e. not necessarily indicative of the cause of pain. This should be given due consideration in the differential diagnosis of patients with neck pain.
Keywords: Cervical spine, Neck pain, Sagittal profile, Lordosis, Kyphotic deformity
Introduction
Degenerative changes of the cervical spine, evident on radiographic examination, are part of the normal physiologic ageing process [16, 17]. The most typical changes observed include osteoarthritis of the facets with reduced joint space and disc space narrowing. In contrast to radicular symptomatology, which is anatomically defined and can usually be explained by the presence of osteophytes or narrowing of the intervertebral foramen at the corresponding vertebral level, there is still uncertainty as to whether more widespread clinical symptoms such as axial neck pain can be attributed to observed radiographic changes.
The prevalence of neck pain in the normal population aged over 40 is approximately 20% [7, 8] and hence the question of the clinical significance of such radiological changes is of great importance. The finding that degenerative changes of the cervical spine are common in asymptomatic individuals has challenged the notion of cause and effect [5]; on the other hand, systematic reviews reveal that degeneration shows a consistent (albeit weak) association with pain, at least for the lumbar spine [47]. Fewer studies have examined this phenomenon in the cervical spine: some have identified a relationship between the number of levels of cervical spine degeneration and the chronicity of the complaint or (in women only) the associated disability [37]; others have shown that asymptomatic individuals with degenerative changes of C6/7 are significantly more likely to develop neck pain in the future (10 years later) [16]; whilst others, still, have failed to find any significant relationship between degenerative changes and pain [11, 13, 17, 18].
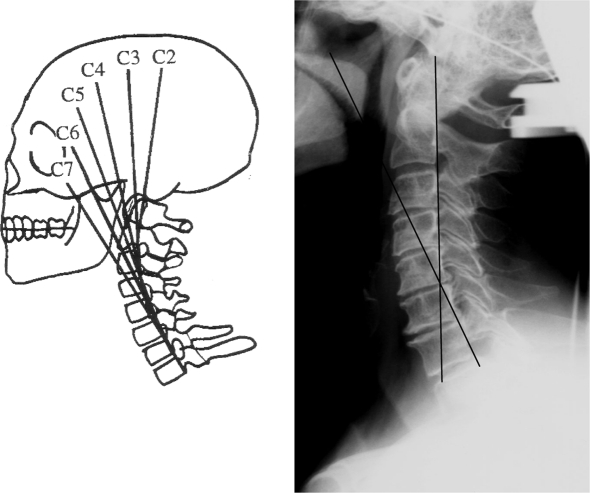
Degenerative changes of the cervical spine are often accompanied by a shortening of the anterior or posterior vertebral column [21, 49], which results in an alteration of the sagittal profile of the cervical spine [17]. The latter may occur on a segmental basis or may involve the whole cervical spine (Figs. 1, 2). There is much discussion in the literature as to whether, from a biomechanical point of view, the loss of the physiological lordosis could be a possible cause of pain, due to muscular imbalance [34] or, in the case of kyphotic deformities, due to structural overload of the anterior parts of the spine [24, 26]. Most of these studies have been in vitro experiments, although a recent study showed that, in individuals of around 40 years of age and with no kyphotic deformity, the mean cervical lordotic curve was lowest in a group with chronic neck pain and greatest in normal controls, with acute pain patients lying somewhere between the two [27]. Nonetheless, this was a retrospective radiographic study, and hence the data were not necessarily collected using standardised procedures.
Fig. 1.

Degenerative segmental kyphosis at C3/4
Fig. 2.

Degenerative global kyphosis
The aim of the present study was to examine whether the sagittal profile of the cervical spine and individual segments (in particular, the presence of kyphotic segments) show any association with the presence and severity of axial neck pain in volunteers over 45 years of age.
Methods
Participants
One hundred and seven volunteers (47 males), with an average age of 68 (range, 45–90) years, agreed to participate in the study, which was approved by the local Ethics Committee. The volunteers were patients over 45 years of age that were visiting the outpatient clinic of our hospital due to orthopaedic problems of the lower extremities. Seventy-three per cent of those who were asked agreed to participate. To obtain a representative group of “non-neck-pain-patients” and to increase the incidence of degenerative changes without prior trauma or serious spinal disease, the exclusion criteria were defined as follows:
previous trauma of the cervical spine;
currently undergoing medical treatment for neck pain;
systemic disease involving the cervical spine (e.g. rheumatoid arthritis);
age under 45 years.
Hence, the study was considered to be monitoring the prevalence and severity of “non-specific neck pain” rather than “cervical spine illness/spinal disease.”
Radiological assessment
The subject stood in a relaxed position, holding onto a support at the level of the chest (Fig. 3). Using the light beam of the X-ray machine, the shadow of a metal wire was projected onto the lateral aspect of the head and this was used to define the angle of inclination of the head. The angle to the horizontal line was adjusted to 20° and the head was orientated such that this line projected from the external opening of the ear to the eye (Fig. 3). The beam of the radiograph was centred 15 cm below the ear at a distance of 150 cm to the film plate.
Fig. 3.
Setup for the lateral cervical radiograph: a wire is stretched at 20° on an adjustable height pole and the shadow of this is projected onto the head, enabling standardisation of the head position in all participants
Cervical spine segmental angles were evaluated from the radiographs according to the posterior tangent technique originally described by Albers [2] and Gore et al. [17]. Harrison et al. [23] re-examined this technique and reported good inter- and intraobserver reliability, with a lower standard error of measurement (less than 2°) than that typically reported for Cobb angle measurements. The angle between the posterior wall of the vertebral body of C2 and C7 gave the total cervical curvature (Fig. 4), and the angles between the posterior walls of neighbouring segments gave the segmental angles. In four patients it was not possible to visualise C7 due to unfavourable anatomical conditions.
Fig. 4.
a Schematic diagram of the posterior tangent method of Harrison et al. [23]; btangent lines at the posterior vertebral body margins (here of C2 and C7) are drawn and the angle of these intersecting lines is measured
As no standard values for “normal” curvature could be found in the literature, we defined the curvatures as follows (negative = lordotic; positive = kyphotic), based on the typical error of measurement (with 95% confidence intervals) [29] for radiographic segmental angles [14, 23, 42]:
Total curvature:
Straight: −4° to +4°;
Lordotic: less than −4°;
Kyphotic: more than +4°.
Segmental curvature:
Straight: 0° to +4°;
Lordotic: less than −0°;
Kyphotic: more than +4°.
The proportion of segments (%) showing kyphosis was also calculated.
Subjective assessment
At the time of the investigation, no standardised and universally accepted self-rating questionnaires for the multidimensional assessment of cervical spine problems were available in the German language. As such, a custom-made questionnaire was used. It included questions on:
the presence or absence of neck pain in the last 12 months (yes/no). This was used to dichotomise patients into a PAIN and NO PAIN group for further analysis (see Sect. ”Discussion”);
the duration (in months) and frequency (occasionally, often, constant) of neck pain;
the intensity of neck pain [0–10 numerical rating scale (NRS)] when at its worst, at its best and on average;
the frequency (occasionally, often, constant) and intensity (0–10 NRS) of radiating pain;
difficulties swallowing (yes/no);
concurrent headache (yes/no);
sensory disturbances in the arm/hand (yes/no);
impairment of manual dexterity (yes/no);
difficulties getting to sleep/waking in the night due to neck pain (for each: never, occasionally, often, constant);
social restrictions due to neck pain (never, occasionally, often, constant);
restricted ability to do housework due to neck pain (never, occasionally, often, constant);
restricted work capacity due to neck pain (never, occasionally, often, constant);
use of over-the-counter analgesics for neck pain (yes/no);
medical treatment for neck pain (visit to the doctor, conservative treatment, surgical treatment; each yes/no).
Statistical analysis
Descriptive data are given as means (SD), or absolute numbers and percentages. Differences in continuous variables between the PAIN and NO PAIN group were examined using unpaired t-tests. Relationships between continuous variables were examined with Pearson correlation coefficients. Associations between pairs of categorical variables [e.g. the different categories of sagittal profile (straight–lordotic–kyphotic) and various clinical parameters listed in Table 1] were examined using the Chi-square test and Fisher’s exact test.
Table 1.
Pain and disability data for patients with neck pain
| Variable | Mean (SD) or number (%) |
|---|---|
| Duration of pain (months) | 67 (63) |
| Frequency of pain | Occasionally 22/54 (41%) |
| Often 26/54 (48%) | |
| Constant 6/54 (11%) | |
| Neck pain intensity, when at worst (0–10 NRS) | 4.4 (2.2) |
| Neck pain intensity, when at best (0–10 NRS) | 1.9 (1.5) |
| Neck pain intensity, average (0–10 NRS) | 2.8 (1.5) |
| Neck pain intensity at end of busy day (0–10 NRS) | 3.5 (2.2) |
| Radiating pain | 22/54 (41%) |
| Frequency of radiating pain (if present; N = 22) | Occasionally 11/22 (50%) |
| Often 9/22 (41%) | |
| Constant 2/22 (9%) | |
| Radiating pain intensity (if present; N = 22) | 3.0 (1.0) |
| Difficulties swallowing | 2/53 (4%) |
| Concurrent headache | 19/53 (36%) |
| Sensory disturbances in arm or hand | 24/53 (46%) |
| Impairment of motor function/manual dexterity | 6/53 (11%) |
| Difficulties getting to sleep due to neck pain | Never 18/52 (35%) |
| Occasionally 26/52 (50%) | |
| Often 7/52 (13%) | |
| Constant 1/52 (2%) | |
| Waking in the night due to neck pain | Never 38/52 (73%) |
| Occasionally 12/52 (23%) | |
| Often 2/52 (4%) | |
| Constant 0/52 (0%) | |
| Restricted social life due to neck pain | Never 38/52 (73%) |
| Occasionally 12/52 (23%) | |
| Often 2/52 (4%) | |
| Constant 0/52 (0%) | |
| Restricted ability to do housework due to neck pain | Never 29/52 (56%) |
| Occasionally 21/52 (40%) | |
| Often 2/52 (4%) | |
| Constant 0/52 (0%) | |
| Restricted work capacity due to neck pain (where applicable, N = 27) | Never 23/27 (85%) |
| Occasionally 4/27 (15%) | |
| Often 0/27 (0%) | |
| Constant 0/27 (0%) | |
| Use of over-the-counter analgesics | 17/54 (31%) |
| Visit to the doctor in the last 6 months due to neck pain | 8/52 (15%) |
| Conservative treatment for neck pain in last 6 months | 11/52 (21%) |
| Operative treatment for neck pain in last 12 months | 0/52 (0%) |
Data are from a maximum N = 54; where N < 54 this was due to occasional missing answers within the questionnaire
The data were analysed using the statistics program Statview 5.0 (SAS Institute, San Francisco, CA, USA). Significance was accepted at the 5% level.
Results
Comparability of the study groups
Fifty-four out of 107 volunteers declared having had neck pain in the last 12 months and these constituted the “pain group” (PAIN); 53 individuals had had no neck pain (NO PAIN) in the last 12 months.
The PAIN and NO PAIN groups were of comparable age [67.4 (SD 11.0, range 45–90) vs 68.7 (SD 10.0, range 50–86) years, respectively; P = 0.52], but differed significantly with regard to their gender distribution [39/54 (72%) vs 21/53 (40%) females, respectively; P=0.0007]. As such, in subsequent PAIN vs NO PAIN group comparisons, additional analyses were carried out for men and women separately, to ensure that gender was not acting as a confounding variable.
Pain characteristics of the PAIN group
Details of the pain history, clinical symptoms, pain and disability of the subjects in the PAIN group are shown in Table 1. Most had chronic mild to moderate pain, and the average duration was 67 (SD 63, range 1–360) months. The majority suffered with neck pain either often or occasionally; just under half of them also had radiating pain. Concurrent headache was reported in about one-third and sensory disturbances in almost half. Approximately two-thirds declared at least occasionally having difficulties getting to sleep due to neck pain; and about a quarter woke in the night due to pain. Just over a quarter felt their social life was somewhat restricted as a result of their neck pain, and almost half were restricted in their ability to do housework; few (15%) of those working reported work-related restrictions. About a third used over-the-counter pain medication. A minority (15%) had visited the doctor for neck pain, and approximately one-fifth had had some sort of conservative treatment. No one had undergone surgery of the cervical spine in the preceding 12 months.
Gender differences in pain characteristics
In the individuals reporting pain, there were no significant gender differences for the following parameters: frequency of pain (P = 0.76); duration of pain (P = 0.11); pain intensity (each P > 0.10); presence of radiating pain (P = 0.95); difficulties swallowing (P = 0.37); sensory disturbances (P = 0.13); impairment of motor function (P = 0.17); difficulties getting to sleep (P = 0.75) or being woken from sleep (P = 0.49); restrictions in social life (P = 0.71), housework (P = 0.68), and work capacity (P = 0.26); and use of analgesics (P = 0.99).
There was, however, a significant gender difference in the frequency of headaches (P = 0.009) and the use of non-operative treatment modalities (P = 0.025), with women reporting a higher frequency than men in each case; there was a slight, non-significant tendency for more medical consultations in women than men (P = 0.09).
Influence of gender and age on spinal curvature
There was no significant difference between men and women for either the global curvature C2–C7 [−23.0° (SD 13.1) and −24.1° (SD 10.3), respectively; P = 0.63] or individual segmental angles (all P > 0.05).
For the women, but not the men, the degree of lordosis (negative curvature) from C2–C7 showed a significant increase with increasing age (r=−0.44, P = 0.0006).
Influence of pain history on total and segmental curvature
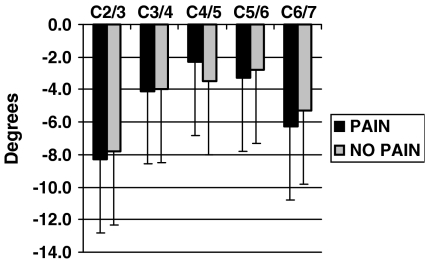
There were no significant differences between the PAIN and NO PAIN groups for either the total (C2–C7) curvature (Table 2) or the segmental curvature at any level (Fig. 5). When the sexes were examined separately, there were still no differences between PAIN and NO PAIN groups for the total curve but, in the men only, C2/3 was slightly less lordotic (by about 3°; P = 0.049) and C6/7 more lordotic (by about 4°; P = 0.04) in the PAIN group.
Table 2.
Mean global cervical curvature (C2–C7) in the PAIN and NO PAIN groups: for all subjects together, and then split according to those with a lordotic spine, a straight spine or a kyphotic spine (see definitions in the text)
| Category of cervical curvature | Cervical spine curvature (deg) | ||||
|---|---|---|---|---|---|
| PAIN group | NO PAIN group | P value | |||
| Mean (SD) | Count | Mean (SD) | Count | ||
| All | −24.3 (11.2) | 50 | −23.0 (12.0) | 53 | 0.57 |
| Lordotic | −25.2 (10.5) | 48 | −25.2 (10.1) | 48 | 0.98 |
| Straight | −3.0 (1.4) | 2 | −3.0 (2.0) | 4 | – |
| Kyphotic | 0 | +5.0 | 1 | – | |
Fig. 5.
Mean (SD) segmental angles in the PAIN and NO PAIN groups. No significant differences at any level
In the PAIN group, there were no significant correlations between the total or segmental curvature and any of the clinical features of the pain shown in Table 1.
Curvature categories vs neck pain group
There was no significant difference in the distribution of curvature categories between the PAIN and NO PAIN groups, for either the whole curve or the segmental angles (Table 3). This was also the case for all comparisons when the sexes were considered separately, with the exception of one level (C2/3), in women only, for which significantly (P = 0.01) more people in the NO PAIN (19%) than in the PAIN (0%) group were categorised as having a straight as opposed to lordotic segment (no kyphotic segments were recorded in either group).
Table 3.
Proportion of patients with each category of cervical curvature (lordotic, straight, kyphotic) in PAIN and NO PAIN groups
| Spinal segment | Group | Lordotic | Straight | Kyphotic | Chi-square P value |
|---|---|---|---|---|---|
| C2/3 | PAIN | 51/54 (94%) | 2/54 (4%) | 1/54 (2%) | 0.31 |
| NO PAIN | 48/53 (91%) | 5/53 (9%) | 0/53 (0%) | ||
| C3/4 | PAIN | 41/54 (76%) | 10/54 (18%) | 13/54 (6%) | 0.77 |
| NO PAIN | 37/53 (70%) | 12/53 (23%) | 4/53 (7%) | ||
| C4/5 | PAIN | 35/54 (65%) | 14/54 (26%) | 5/54 (9%) | 0.82 |
| NO PAIN | 37/53 (70%) | 11/53 (21%) | 5/53 (9%) | ||
| C5/6 | PAIN | 38/54 (70%) | 13/54 (24%) | 3/54 (6%) | 0.89 |
| NO PAIN | 37/53 (70%) | 14/53 (26%) | 2/53 (4%) | ||
| C6/7 | PAIN | 43/54 (86%) | 7/54 (14%) | 0/54 (0%) | 0.68 |
| NO PAIN | 47/53 (89%) | 6/53 (11%) | 0/53 (0%) | ||
| C2–C7 whole curve | PAIN | 48/50 (96%) | 2/50 (4%) | 0/50 (0%) | 0.45 |
| NO PAIN | 48/53 (91%) | 4/53 (7%) | 1/53 (2%) |
A segmental kyphotic deformity of >+4° in at least one segment was found in 12/52 (23%) individuals in the PAIN group vs 9/53 (17%) in the NO PAIN group (P = 0.47). In each case, the segment C4/5 was most commonly affected (9% of cases), followed by C3/4 (7%) and C5/6 (5%). Where kyphosis was observed, the mean kyphotic angle (6.5° vs 6.3°, in the PAIN and NO PAIN groups, respectively) and range of values for the kyphotic angle (+5° to +10° in both groups) did not differ between the groups (P > 0.05).
Other radiographic abnormalities
Amongst the whole volunteer group, one case of assimilation of the atlas and one congenital fusion of C2/3 were observed. Both of these were in the NO PAIN group.
Discussion
The methods described in the literature for the radiographic assessment of spinal curvature vary widely. There is general agreement that a lordotic curvature represents the “normal” or “ideal” situation for the cervical spine [22], but there is only vague information regarding the exact values and the recommended methods of measurement. In general, normal values have been reported to range from 20° to 35° for C2 to C7 [6, 17, 19, 30, 40] (see Table 4), but these appear to be highly dependent on the method of measurement used. Many studies in the literature report only a subjective classification, “kyphotic, straight or lordotic,” but this method of assessment has proven to be unreliable [28]. As such, we developed a new standard for assessment in the present study. We chose a tolerance of ±4° to accept as possible measurement error with 95% confidence intervals [14, 42], i.e. as the “minimal detectable change” [4], and hence defined “straight” for the global curvature as +4° to −4°, and lordotic and kyphotic as <−4° and >+4°, respectively.
Table 4.
The lordosis angles and incidence of straight or kyphotic curves in the various populations examined in the literature
| Study | No. of people | Symptoms | Age | Method | Cervical spine curvature(negative values indicate lordotic curvatures) | % Straight | % Kyphotic |
|---|---|---|---|---|---|---|---|
| Gore et al. [17] | 200 | No | 20–65 | C2–C7 (pT) | −23° (±21°) (higher in older women) | 9 | |
| Gore et al. [18] | 205 | Yes | 43 (±12) | C2–C7 (pT) | −24° (±14°) | 6.3 | |
| Harrison et al. [25] | 250 | No | 35 | C2–C7 (pT) | −34° (−16.5 to −66°) | 35 | |
| Nojiri et al. [40] | 313 | No | 11–77 | C2–C7 (pT) | −16.2° (±12.9°); −10.5° (±10.3°) | ||
| Owens and Hoiriis [41] | 113 | Yes and no (no influence of trauma/cervical complaint) | 28.8 | C2–C7 (pT) | −22.3° (±11.5°) | ||
| Wiegand et al. [51] | 186 | Yes | 38 (±13) | C2–C7 (pT) | −18.9 ± 12.3° | ||
| Plaugher et al. [44] | 48 | Yes | 44 | C2–C7 (Cobb) | −6.1 ± 11.4° (−53 to +17°) | ||
| Takeshima et al. [46] | 48 | Yes | 33 | C2–C7 (Cobb) | −17.5 ± 7.0° | ||
| Borden et al. [6] | 180 | No | 21–80 | C2–C7 (Kt) | 90% | 7.2 | 2 |
| Juhl et al. [30] | 116 | No | 10–65 | Aspect | 60% | 19 | 21 |
| Hald et al. [19] | 10,922 | No | 17–25 | Aspect | – | 7.4 | 3.3 |
N.B. the methodology is not always consistent across studies
pT posterior tangent method, Cobb Cobb method, Kt depth of curvature, Aspect categorisation in relation to the aspect
In most previous studies, the positioning of the volunteer during the radiograph has not been mentioned when interpreting the results. However, it is well known that factors such as the tilt of the pelvis, the adoption of a sitting or standing position, the shape of the backrest when sitting, and the head position can all influence the sagittal curve of the cervical spine [12, 28, 30, 33, 35, 45, 50]. We found that the angle between the horizontal line and the ear–eye line was easy to identify and lay mostly between 15° and 20° when the subject was encouraged to stand comfortably and fixate on a point at eye level. Hence, we defined and standardised this angle for all the tests at 20°. In most individuals, little adjustment from their natural position was required to achieve this 20° position. It is conceivable that certain deformities may have been masked and yet others may have been accentuated by constraining the head position this way; however, especially as it was close to the natural position for most individuals, it was considered that the benefits of standardisation would outweigh any possible disadvantages in this respect.
The results of our study showed no association between the sagittal alignment of the cervical spine (or its individual segments) and the presence of neck pain. Similarly, in the group with neck pain, there was no relationship between curvature and any index of symptom severity, such as pain intensity, disability, healthcare utilisation, etc. To the best of our knowledge, this is the first study to explicitly examine these relationships in detail, although the findings concur with those of a literature review that found little evidence to suggest that altered cervical curvatures are of prognostic or diagnostic significance [15]. In contrast, one recently published retrospective study found that the degree of lordosis as measured with the posterior tangent technique was able to distinguish, with moderate diagnostic accuracy, between individuals with and without chronic neck pain (sensitivity 0.46, specificity 0.97), and between those with and without acute neck pain (sensitivity 0.67, specificity 0.61) [27]. In the latter study, individuals who did not have a normal lordotic curve (i.e. any with a straight or kyphotic curve) were excluded; however, even excluding such patients from our data (see second row in Table 2), we still observed no significant difference between the PAIN and NO PAIN groups. The comparison study of Harrison et al. [27] was retrospective, and the control radiographic data were collected a good 10 years earlier (1988–1992) than those of the patients (collected 1997–2003). It was not stated whether identical methods were used in each case, and, in particular, whether positioning of the volunteer during imaging was carried out using standardised procedures (see discussion above, regarding the potential consequences of this). Interestingly, the mean curvatures for their control group (34.5°) were considerably higher than those previously reported for asymptomatic individuals in the literature (see Table 4), whereas their patients’ mean values (22.0° and 28.6°, for chronic and acute, respectively) were comparable to those reported for “normals” in other studies and for both groups in the present study.
Overall, our findings for the cervical spine appear to mirror the majority of those reported for the lumbar spine: whilst there is some suggestion that individuals with a flatter spine (reduced lordosis) have a slightly higher risk of developing low back pain [1], the vast majority of cross-sectional studies conclude that there is no significant difference in the degree of lordosis in people with and without back pain [20, 36, 39].
The lordotic shape is accepted as the “physiological” form [22], but the tolerance of the system is not well known and the point where a kyphotic deformity might start to cause problems remains unclear. This should be kept in mind when surgical procedures are planned. Some studies have highlighted the negative consequences of kyphotic cervical configurations after surgery, in terms of axial pain [32] or accelerated adjacent segment degeneration [31]. However, this may simply reflect the introduction of sudden change in a previously “balanced” profile. The fact that groups of individuals with and without neck pain do not show differences in their degree of lordosis at a global or segmental level does not mean that, for any given individual, a sudden alteration of his/her spinal curvature would not be detrimental. Hence, the risk and benefit of not only removing the pain source but also restoring “normal” alignment (i.e. normal for that individual) should be weighed-up carefully.
Certain limitations of the present study are worthy of mention. For ethical reasons, it was not possible to investigate the sagittal profile of the whole spine and, hence, any influence of the curvature of the lower spinal regions, a possible determinant of cervical spine curvature [6], remains uncertain. Another drawback was the initial selection of the volunteers. As they were patients from the lower extremities outpatient clinic, they likely represented a specific selection rather than a random sample of the normal population. None of them were specifically seeking treatment for neck pain in the hospital, and the study group was therefore considered to represent two comparable groups of patients with other musculoskeletal problems, differing in their history of “non-specific” neck pain. The symptoms in the PAIN group were generally of a mild to moderate, mostly chronic nature. It is possible that, had we taken patients who were actually seeking treatment for neck pain, and compared these with a completely asymptomatic group, we may have seen differences between the groups. Nonetheless, the fact that absolutely no relationships were observed between symptom severity—measured with a multidimensional array of items—and cervical spine curvature, tends to challenge this notion.
Group membership was decided on the basis of neck pain experienced in the preceding 12 months. In the age-group studied, it was considered that enquiring about “lifetime neck pain” may lead to recall bias [10, 38], and data on “current pain” may obscure any relationships with structural changes, a longer-term cumulative phenomenon. Hence, a period of 12 months was chosen as a compromise between the two. This has been shown to be a relevant time-span in previous studies concerning the clinical significance of structural abnormalities of the spine (e.g. [48]). In view of the recurrent and persistent nature of common neck pain [9], it can be assumed that if someone >45 years old is typically a “neck pain sufferer,” they will have experienced at least one episode in the last year; however we cannot rule out the possibility that some patients with no pain in the last 12 months were, indeed, at one-time, neck pain sufferers. In future studies, it may be of interest to enquire about lifetime pain experience and also pain on the day of the examination in relation to these deformities.
A further consideration in any study with “negative results” is the possibility that a type II error occurred, i.e. the study failed to identify “real” differences between the groups due to small group sizes and inadequate power. However, this seems an unlikely explanation of the current results, since with approximately 50 in each group there was sufficient power (85%) to detect a “clinically relevant” difference, i.e. with a moderate effect size (0.55), had one existed [3]. The only exception may have been for some of the secondary sub-group analyses of men and women separately, for which the group sizes were clearly smaller. Finally, with regards to the statistical analysis, we cannot rule out the possibility that the odd significant differences between the PAIN and NO PAIN groups (e.g. for men only, in relation to the segmental curvature at C2/3 and C6/7), may have represented spurious findings on account of the multiple testing carried out; this always increases the chances of committing a type I error. Although it is possible to correct for this with, for example, Bonferroni adjustments, there are equally good arguments to suggest that such corrections are not only unnecessary, but also inappropriate [43]. We hence chose not to make such corrections but, instead, to weigh up the likely biological plausibility of the incidental findings; in doing so, we found no convincing interpretation to indicate that our main conclusions did not hold—namely, that there was no significant association between deviations from the normal cervical spine lordosis and the presence, frequency or intensity of neck pain.
In conclusion, we suggest that when so-called “abnormalities” of the sagittal profile are observed in the older patient with neck pain they must be considered coincidental, i.e. not necessarily indicative of the cause of pain. This should be given due consideration in the differential diagnosis of patients with non-specific neck pain.
References
- 1.Adams MA, Mannion AF, Dolan P. Personal risk factors for first-time low back pain. Spine. 1999;24(23):2497–2505. doi: 10.1097/00007632-199912010-00012. [DOI] [PubMed] [Google Scholar]
- 2.Albers D (1954) Eine Studie über die Funktion der Halswirbelsäule bei dorsaler und ventraler Flexion. Fortschr Geb Röntgenstr 81:606–615 [PubMed]
- 3.Altman DG (1980) Statistics of ethics in medical research. III How large a sample? Br Med J [Clin Res] 281:1336–1338 [DOI] [PMC free article] [PubMed]
- 4.Beaton DE. Understanding the relevance of measured change through studies of responsiveness. Spine. 2000;25(24):3192–3199. doi: 10.1097/00007632-200012150-00015. [DOI] [PubMed] [Google Scholar]
- 5.Boden SD, McCowin PR, Davis DO, Dina TS, Mark AS, Wiesel S. Abnormal magnetic-resonance scans of the cervical spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72(8):1178–1184. [PubMed] [Google Scholar]
- 6.Borden AG, Rechtman AM, Gershon-Cohen J. The normal cervical lordosis. Radiology. 1960;74:806–809. doi: 10.1148/74.5.806. [DOI] [PubMed] [Google Scholar]
- 7.Bovim G, Schrader H, Sand T. Neck pain in the general population. Spine. 1994;19(12):1307–1309. doi: 10.1097/00007632-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Brattberg G, Thorslund M, Wikman A. The prevalence of pain in a general population. The results of a postal survey in a county of Sweden. Pain. 1989;37(2):215–222. doi: 10.1016/0304-3959(89)90133-4. [DOI] [PubMed] [Google Scholar]
- 9.Cote P, Cassidy JD, Carroll LJ, Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. Pain. 2004;112(3):267–273. doi: 10.1016/j.pain.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 10.Dawson EG, Kanim LE, Sra P, Dorey FJ, Goldstein TB, Delamarter RB, Sandhu HS (2002) Low back pain recollection versus concurrent accounts: outcomes analysis. Spine 27(9):984–993; discussion 994 [DOI] [PubMed]
- 11.Elias F. Roentgen findings in the asymptomatic cervical spine. NY State J Med. 1958;58(20):3300–3303. [PubMed] [Google Scholar]
- 12.Fineman S, Borrelli FJ, Rubinstein BM, Epstein H, Jacobson HG. The cervical spine: transformation of the normal lordotic pattern into a linear pattern in the neutral posture. J Bone Joint Surg Am. 1963;45:1179–1183. [PubMed] [Google Scholar]
- 13.Friedenberg ZB, Miller WT. Degenerative disc disease of the cervical spine. J Bone Joint Surg Am . 1963;45:1171–1178. [PubMed] [Google Scholar]
- 14.Frobin W, Brinckmann P, Leivseth G, Biggemann M, Reikeras O. Precision measurement of segmental motion from flexion–extension radiographs of the lumbar spine. Clin Biomech (Bristol, Avon) 1996;11(8):457–465. doi: 10.1016/S0268-0033(96)00039-3. [DOI] [PubMed] [Google Scholar]
- 15.Gay RE. The curve of the cervical spine: variations and significance. J Manipulative Physiol Ther. 1993;16(9):591–594. [PubMed] [Google Scholar]
- 16.Gore DR. Roentgenographic findings in the cervical spine in asymptomatic persons: a ten-year follow-up. Spine. 2001;26(22):2463–2466. doi: 10.1097/00007632-200111150-00013. [DOI] [PubMed] [Google Scholar]
- 17.Gore DR, Sepic SB, Gardner GM. Roentgenographic findings of the cervical spine in asymptomatic people. Spine. 1986;11(6):521–524. doi: 10.1097/00007632-198607000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Gore DR, Sepic SB, Gardner GM, Murray MP. Neck pain: a long-term follow-up of 205 patients. Spine. 1987;12(1):1–5. doi: 10.1097/00007632-198701000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Hald HJ, Danz B, Schwab R, Burmeister K, Bähren W. Radiographically demonstrable spinal changes in asymptomatic young men. Rofo. 1995;163(1):4–8. doi: 10.1055/s-2007-1015936. [DOI] [PubMed] [Google Scholar]
- 20.Hansson T, Bigos S, Beecher P, Wortley MD. The lumbar lordosis in acute and chronic low-back pain. Spine. 1984;9(1):154–156. doi: 10.1097/00007632-198503000-00008. [DOI] [PubMed] [Google Scholar]
- 21.Hardacker JW, Shuford RF, Capicotto PN, Pryor PW (1997) Radiographic standing cervical segmental alignment in adult volunteers without neck symptoms. Spine 22(13):1472–1480; discussion 1480 [DOI] [PubMed]
- 22.Harrison DD, Troyanovich SJ, Harrison DE, Janik TJ, Murphy DJ. A normal sagittal spinal configuration: a desirable clinical outcome. J Manipulative Physiol Ther. 1996;19(6):398–405. [PubMed] [Google Scholar]
- 23.Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B. Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine. 2000;25(16):2072–2078. doi: 10.1097/00007632-200008150-00011. [DOI] [PubMed] [Google Scholar]
- 24.Harrison DE, Harrison DD, Janik TJ, William Jones E, Cailliet R, Normand M. Comparison of axial and flexural stresses in lordosis and three buckled configurations of the cervical spine. Clin Biomech (Bristol, Avon) 2001;16(4):276–284. doi: 10.1016/S0268-0033(01)00006-7. [DOI] [PubMed] [Google Scholar]
- 25.Harrison DE, Bula JM, Gore DR. Roentgenographic findings in the cervical spine in asymptomatic persons: a 10-year follow-up. Spine. 2002;27(11):1249–1250. doi: 10.1097/00007632-200206010-00027. [DOI] [PubMed] [Google Scholar]
- 26.Harrison DE, Jones EW, Janik TJ, Harrison DD. Evaluation of axial and flexural stresses in the vertebral body cortex and trabecular bone in lordosis and two sagittal cervical translation configurations with an elliptical shell model. J Manipulative Physiol Ther. 2002;25(6):391–401. doi: 10.1067/mmt.2002.126128. [DOI] [PubMed] [Google Scholar]
- 27.Harrison DD, Harrison DE, Janik TJ, Cailliet R, Ferrantelli JR, Haas JW, Holland B. Modeling of the sagittal cervical spine as a method to discriminate hypolordosis: results of elliptical and circular modeling in 72 asymptomatic subjects, 52 acute neck pain subjects, and 70 chronic neck pain subjects. Spine. 2004;29(22):2485–2492. doi: 10.1097/01.brs.0000144449.90741.7c. [DOI] [PubMed] [Google Scholar]
- 28.Helliwell PS, Evans PF, Wright V. The straight cervical spine: does it indicate muscle spasm? J Bone Joint Surg Br. 1994;76(1):103–106. [PubMed] [Google Scholar]
- 29.Hopkins WG. Measures of reliability in sports medicine and science. Sports Med. 2000;30(1):1–15. doi: 10.2165/00007256-200030010-00001. [DOI] [PubMed] [Google Scholar]
- 30.Juhl JH, Miller SM, Roberts GW. Roentgenographic variations in the normal cervical spine. Radiology . 1962;78:591–597. [Google Scholar]
- 31.Katsuura A, Hukuda S, Saruhashi Y, Mori K. Kyphotic malalignment after anterior cervical fusion is one of the factors promoting the degenerative process in adjacent intervertebral levels. Eur Spine J. 2001;10(4):320–324. doi: 10.1007/s005860000243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kawakami M, Tamaki T, Yoshida M, Hayashi N, Ando M, Yamada H. Axial symptoms and cervical alignments after cervical anterior spinal fusion for patients with cervical myelopathy. J Spinal Disord. 1999;12(1):50–56. doi: 10.1097/00002517-199902000-00008. [DOI] [PubMed] [Google Scholar]
- 33.Kettner NW, Guebert GM. The radiology of cervical spine injury. J Manipulative Physiol Ther. 1991;14(9):518–526. [PubMed] [Google Scholar]
- 34.Kleinn F. Zur Rolle strukturell fixierter Kyphosen und Skoliosen bei chronischen Rückenbeschwerden. Orthop Praxis. 1998;34(7):456–459. [Google Scholar]
- 35.Kristjansson E, Jonsson H., Jr Is the sagittal configuration of the cervical spine changed in women with chronic whiplash syndrome? A comparative computer-assisted radiographic assessment. J Manipulative Physiol Ther. 2002;25(9):550–555. doi: 10.1067/mmt.2002.128371. [DOI] [PubMed] [Google Scholar]
- 36.Liebig EM, Kothe R, Mannion AF, Grob D. The clinical significance of the lumbar lordosis: relationship between lumbar spinal curvature and low back pain. Eur Spine J. 2000;9(4):286. [Google Scholar]
- 37.Marchiori DM, Henderson CN. A cross-sectional study correlating cervical radiographic degenerative findings to pain and disability. Spine. 1996;21(23):2747–2751. doi: 10.1097/00007632-199612010-00007. [DOI] [PubMed] [Google Scholar]
- 38.McKinnon ME, Vickers MR, Ruddock VM, Townsend J, Meade TW. Community studies of the health service implications of low back pain. Spine. 1997;22(18):2161–2166. doi: 10.1097/00007632-199709150-00014. [DOI] [PubMed] [Google Scholar]
- 39.Murrie VL, Dixon AK, Hollingworth W, Wilson H, Doyle TA. Lumbar lordosis: study of patients with and without low back pain. Clin Anat. 2003;16(2):144–147. doi: 10.1002/ca.10114. [DOI] [PubMed] [Google Scholar]
- 40.Nojiri K, Matsumoto M, Chiba K, Maruiwa H, Nakamura M, Nishizawa T, Toyama Y. Relationship between alignment of upper and lower cervical spine in asymptomatic individuals. J Neurosurg. 2003;99(1 Suppl):80–83. doi: 10.3171/spi.2003.99.1.0080. [DOI] [PubMed] [Google Scholar]
- 41.Owens EF, Hoiriis KT. Cervical curvature assessment using digitized radiographic analysis. Chiropr Res J. 1990;4:47–62. [Google Scholar]
- 42.Panjabi M, Chang D, Dvorak J. An analysis of errors in kinematic parameters associated with in vivo functional radiographs. Spine. 1992;17(2):200–205. doi: 10.1097/00007632-199202000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Perneger TV. What’s wrong with Bonferroni adjustments. BMJ. 1998;316(7139):1236–1238. doi: 10.1136/bmj.316.7139.1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Plaugher G, Cremata EE, Phillips RB. A retrospective consecutive case analysis of pretreatment and comparative static radiological parameters following chiropractic adjustments. J Manipulative Physiol Ther. 1990;13(9):498–506. [PubMed] [Google Scholar]
- 45.Refshauge K. Consistency of cervical and cervicothracic posture in standing. Aust J Physiother. 1994;40(4):235–240. doi: 10.1016/S0004-9514(14)60459-1. [DOI] [PubMed] [Google Scholar]
- 46.Takeshima T, Omokawa S, Takaoka T, Araki M, Ueda Y, Takakura Y. Sagittal alignment of cervical flexion and extension: lateral radiographic analysis. Spine. 2002;27(15):E348–E355. doi: 10.1097/00007632-200208010-00014. [DOI] [PubMed] [Google Scholar]
- 47.Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Spinal radiographic findings and nonspecific low back pain. A systematic review of observational studies. Spine. 1997;22(4):427–434. doi: 10.1097/00007632-199702150-00015. [DOI] [PubMed] [Google Scholar]
- 48.Videman T, Battie MC, Gibbons LE, Maravilla K, Manninen H, Kaprio J. Associations between back pain history and lumbar MRI findings. Spine. 2003;28(6):582–588. doi: 10.1097/00007632-200303150-00013. [DOI] [PubMed] [Google Scholar]
- 49.Weh L, Rottker H. Functional analysis of the cervical spine in healthy persons. Radiologe. 1990;30(2):87–91. [PubMed] [Google Scholar]
- 50.Weir DC. Roentgenographic signs of cervical injury. Clin Orthop Relat Res. 1975;109:9–17. doi: 10.1097/00003086-197506000-00003. [DOI] [PubMed] [Google Scholar]
- 51.Wiegand R, Kettner NW, Brahee D, Marquina N. Cervical spine geometry correlated to cervical degenerative disease in a symptomatic group. J Manipulative Physiol Ther. 2003;26(6):341–346. doi: 10.1016/S0161-4754(03)00068-X. [DOI] [PubMed] [Google Scholar]