Abstract
Aim
To assess the changes in health-related quality of life in patients discharged from the intensive care unit (ICU).
Methods
At the General University ICU, Trauma Hospital in Athens, 242 patients were enrolled prospectively over a study period of 18 months. Out of these, 116 participants (47.9%) completed all survey components at 6, 12, and 18 months. We used Quality of Life-Spanish (QOL-SP) to assess the health-related quality of life. Patients or their relatives were interviewed on ICU admission and at 6, 12, and 18 months after discharge from the ICU.
Results
Mean quality of life score of the patients increased from 2.9 ± 4.8 (out of maximum 25 points) on ICU admission to 7.0 ± 7.2 points at 6 months after discharge, and then decreased to 5.6 ± 6.9 points at 18 months (P<0.001; Friedman test). Multilinear regression analysis showed that the variables which had the strongest association with the quality of life on admission were age (P = 0.002) and male sex (P = 0.001), whereas age (P<0.001), length of ICU stay (P<0.001), and male sex (P = 0.002) had the strongest association 18 months after discharge from the ICU. Survival rate was 66.9% at discharge from ICU and 61.6% at hospital discharge. There were 33% deaths in the ICU, 5.3% in the hospital, and 6.2% after ICU discharge. There were 7.4% patients lost to follow-up.
Conclusions
After discharge from the ICU, patients’ quality of life was poor and showed an improvement at 18 months after discharge, but was still worse than on admission. Age, ICU length of stay, and male sex were the factors that had the strongest impact on the quality of life on admission and at 18 months after discharge from the ICU.
The cost of intensive care and limited resources directed to patients with a poor prognosis raise questions about the utilization of such resources. Since the need for intensive care in several countries exceeds its availability (1), intensive care specialists are forced to admit those patients who will benefit most. There is an increasing pressure that the assessment of long-term survival and quality of life of survivors should be incorporated into outcome evaluation of intensive care unit (ICU) (2).
Instruments for assessing quality of life in critically ill patients surviving intensive care include EuroQol-5D (EQ-5D), Nottingham Health Profile (NHP), Sickness Impact Profile (SIP), Medical Outcomes Study 36-item Short Form (SF-36), and Quality Of Life-Spanish (QOL-SP) (3). These instruments aim to evaluate the aspects of health important for all patients. Several cross-sectional studies have used generic, multidimensional quality of life instruments to compare health-related quality of life of intensive care patients with the that of the general population and found a considerable deterioration in the former group (3,4). However, such evidence may be misleading if pre-hospitalization health-related quality of life is not taken into account.
Quality of life is an important endpoint in assessing long-term results of intensive care, but the ideal timing for such an assessment is still unclear. This topic has been covered in some reports dealing with pre-ICU assessment of health-related quality of life (3). QOL-SP questionnaire, developed by Fernandez et al (5), is specifically designed for critically ill patients. This is one of the few instruments that have been validated in a critical care population, but it is neither widely used nor well known in the critical care community. A few studies have used QOL-SP to assess medical (6), surgical (7), or multiple trauma patients (8), and to measure the quality of life before ICU, as well as the changes in quality of life from baseline to 6 and 24 months.
Despite its limitations, we used this instrument to assess the changes in health-related quality of life in people who survived critical illness in a Greek medical-surgical ICU at 6, 12, and 18 months after ICU discharge, and to compare these data with their pre-admission status.
Patients and methods
Study population
This prospective observational study was conducted in a 7-bed university medical-surgical ICU located in a university-affiliated trauma hospital in Athens, Greece, from September 1, 2002 to September 30, 2004. All 263 consecutive patients admitted to the ICU in two years were eligible for the study. The inclusion criteria required the participants to be medical and/or surgical ICU patients aged ≥14 years who stayed in the ICU≥24 hours and to undergo a measurement of quality of life ≥30 days after ICU discharge (3). Demographic data on all patients were collected prospectively and included age, gender, admission diagnosis, length of ICU stay, illness severity score (SAPS II) (9), and mortality (at ICU, in hospital, at 6, 12, and 18 months). Severity of illness at admission was estimated according to the APACHE II score (10). Primary outcomes included survival and health-related quality of life.
Of the 263 consecutive patients admitted to the ICU during the two years of study period, 242 patients were enrolled in the study (70.2% men and 29.8% women); 21 patients (8%) were excluded from the study because they were <14 years old (n = 4) and remained in the ICU for ≤24 hours (n = 17). Patients’ characteristics are shown in Table 1 and the most common diagnostic groups in Table 2.
Table 1.
Demographic and clinical characteristics of 242 intensive care unit (ICU) patients (mean ± standard deviation)*
| No. of patients |
||||
|---|---|---|---|---|
| Patient characteristics | total | study sample | died or lost to follow-up | P† |
| N |
242 |
116 |
126 |
|
| Male sex (n, %) |
170 (70) |
88 (76) |
82 (65) |
|
| Age (yrs) |
58.2 ± 21 |
51.2 ± 21 |
65.8 ± 17.0 |
<0.001 |
| ICU stay (days)* |
11.7 ± 11.9 |
13.1 ± 14.5 |
18.6 ± 27.4 |
NS |
| APACHE II |
17.5 ± 8.0 |
14.5 ± 6.5 |
21.5 ± 6.7 |
<0.001 |
| SAPS II | 49.9 ± 18.4 | 41.6 ± 12.4 | 59.8 ± 16.0 | <0.001 |
Table 2.
Primary diagnostic category of the intensive care unit (ICU) population
| No. (%) of patients |
|||
|---|---|---|---|
| Category | total (n = 242) | study sample (n = 116) | died or lost to follow-up (n = 126) |
| Major surgery* |
64 (26.5) |
42 (36.2) |
22 (17.5) |
| Heart failure |
24 (9.9) |
9 (7.8) |
15 (11.9) |
| Respiratory failure |
14 (5.8) |
5 (4.3) |
9 (7.1) |
| Trauma† |
51 (21.0) |
33 (28.5) |
18 (14.3) |
| Head trauma |
20 (8.3) |
6 (5.2) |
14 (11.1) |
| Sepsis |
22 (9.1) |
3 (2.6) |
19 (15.1) |
| Stroke |
26 (10.7) |
5 (4.3) |
21 (16. 7) |
| Miscellaneous‡ | 21 (8.7) | 13 (11.2) | 8 (6.4) |
*Abdominal, chest, or orthopedic surgery (no cardiac).
†Trauma in regions other than the head.
‡Acute renal failure, pulmonary embolism, drug overuse, status epilepticus, and acute necrotizing pancreatitis.
Quality of Life-Spanish questionnaire
Health-related quality of life measurement was estimated by means of the QOL-SP, second edition (5). This instrument can be completed easily and quickly by a large number of patients or their close family members, via direct or telephone interview. It fulfills the criteria recommended for critical care use and essential requirements of validity and reproducibility when applied to critically ill patients (5-8). The validity and reliability of the QOL-SP has been confirmed for critically ill patients (5,11). The questionnaire has 15 items relevant to ICU patients, grouped into the following three subscales: basic physiological activities (BPA, 4 items), normal daily activities (NDA, 8 items), and emotional state (ES, 3 items). The questionnaire scores range between 0-29 points. The BPA subscale ranges from 0-9 points, NDA from 0-15 points, and ES from 0-5 points. A score of 0 points signifies normality, with a higher score corresponding to a lower quality of life. The questionnaire completed on ICU admission retrospectively assessed the patient’s perceived health-related quality of life two months prior to the ICU admission. The follow-up questionnaire reflected the patient’s current life situation. We also grouped the quality of life scores into four levels (6): level I = normal (0-1 points), level II = mild (2-5 points), level III = moderate (6-9 points), level IV = severe (10 points).
Within the first 24 hours after the ICU admission, all eligible consenting patients were asked to complete the health-related quality of life questionnaire via direct interview by a trained investigator. When the patient was unable to respond, the questionnaire was completed by a close family member living in the same household with the patient. A telephone interview was made with the participants 6, 12, and 18 months after ICU discharge to examine their outcome and quality of life. Non-responders received one phone reminder. Two trained investigators conducted the survey. The same investigator always conducted the baseline and follow-up interviews. The ethics committee of the hospital approved the protocol, and informed consent was obtained from the patients or their relatives.
Statistical analysis
All variables were tested for normality with Kolmogorov-Smirnov test. Descriptive statistics were determined for all primary variables, ie, age, gender, admission diagnosis, APACHE II and SAPS II scores, ICU length of stay, and mortality at ICU discharge and at 6, 12, and 18 months after discharge. The data are expressed as mean ± standard deviation (SD). We used t test to compare the means of continuous normally distributed data and Mann-Whitney test for non-normally distributed data. Quality of life measurements were compared between the baseline and follow-up (Friedman test, Wilcoxon signed-rank test). A multilinear regression analysis was performed to identify the factors associated with quality of life on ICU admission and after ICU discharge. Data were analyzed using Statistical Package for the Social Sciences, version 13.0 (SPSS Inc., Chicago, IL, USA). All statistical tests were two-sided and P value <0.05 was considered to indicate statistical significance.
Results
Survival
Survival was calculated for the original cohort of 242 patients. The survival rate at discharge from the ICU was 66.9% (162/242) and 61.6 at hospital discharge (12 and 18 months). Overall, 108 (44.6%) patients died during the follow-up; 80 (33%) in the ICU, 13 (5.37%) in the hospital, and 15 (6.19%) at 18 months after discharge. Consequently, cumulative mortality rate of the original cohort of 242 patients was 41.7% at 6 months and 44.6% at 18 months. Because some patients died from those lost to follow up, survival cannot be calculated for the rest of the time after hospital discharge.
Health related quality of life
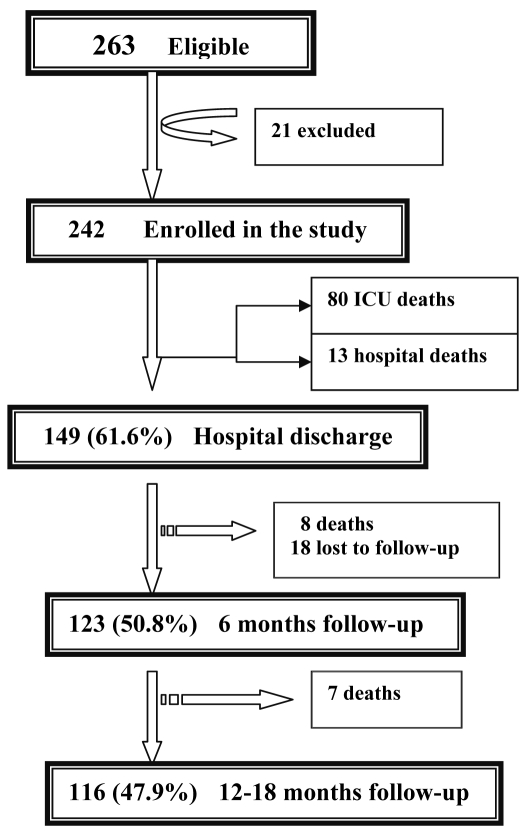
Baseline health-related quality of life questionnaire was distributed to 242 patients on ICU admission. Almost 90% of the baseline questionnaires were completed in a direct interview with the patient’s family member. During the follow-up, the number of patients responding to the questionnaire at 6 to 18 months after ICU discharge varied considerably: 123 (50.8%) questionnaires were completed at 6 months and 116 (47.9%) at 12 and 18 months. All the questionnaires during the follow-up were completed in a phone interview, approximately half with patients and half with their family members. During the follow-up, 108 patients died and 18 (7.4%) were lost to follow-up (4 of them moved abroad and 14 could not be contacted). Nevertheless, for statistical clarity, the following analysis was limited to those 116 patients (study population) who completed all survey components (Figure 1).
Figure 1.
Enrollment of intensive care patients and follow-up for 18 months after intensive care.
Mean stay in the ICU was 13 days. The total mean score of pre-ICU quality of life of 116 patients was 2.9 ± 4.8 points out of the maximum 25. Mean quality of life deteriorated, ie the score increased from 2.9 points on ICU admission to 7.0 points at 6 months after ICU discharge, and then decreased to 5.6 points at 18 months (Table 3). The scores on the QOL-SP subscales also increased at 6 months, compared with the values at admission, and then decreased at 18 months after discharge. However, at all time points the scores were higher than at admission. Friedman test showed that mean absolute values of quality of life for all patients were different at 0, 6, 12, and 18 months (P<0.001).
Table 3.
Quality of Life Questionnaire (Spanish) scores (mean ± standard deviation) for study group (n = 116) on admission and at 6, 12, and 18 months after ICU discharge*
| Subscale |
Score at |
||||
|---|---|---|---|---|---|
| admission | 6 months | 12 months | 18 months | P | |
| Overall |
2.90 ± 4.80 |
7.00 ± 7.21 |
5.99 ± 7.01 |
5.62 ± 6.94 |
<0.05† |
| Basic Physiological Activities (BPA) |
0.20 ± 1.0 |
0.69 ± 1.97 |
0.57 ± 1.81 |
0.53 ± 1.70 |
<0.05‡ |
| Normal Daily Activities (NDA) |
1.95 ± 3.01 |
4.63 ± 4.41 |
4.05 ± 4.28 |
3.76 ± 4.28 |
<0.05† |
| Emotional State (ES) | 0.74 ± 1.48 | 1.67 ± 1.73 | 1.36 ± 1.74 | 1.28 ± 1.71 | <0.05‡ |
*Quality of Life Questionnaire, Spanish version (5).
†Wilcoxon signed-rank test comparisons were made between admission and 6, 12, and 18 mo after ICU discharge.
‡Comparisons were made between admission and 6 and 12 mo after ICU. There was no significant difference of quality of life scores between 12 and 18 mo for BPA (P = 0.102) and ES (P = 0.063).
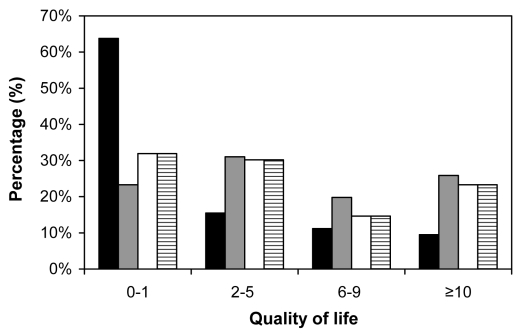
Two-tailed comparisons between individual time points showed that mean absolute values differed at all times points (P<0.001), except BPA (P = 0.102) and ES (P = 0.063) scores at 12 and 18 months. The scores on the NDA subscale showed a significant decrease from 6 to 18 months (P<0.001). When we grouped the patients according to their quality of life score in four levels as follows: level 1 = normal (0-1 points), level 2 = mild (2-5 points), level 3 = moderate (6-9 points), Level 4≥severe (10 points) (6) we found that there was more deterioration at 18 months if premorbid quality of life score was worse and vice versa. There were 63.8% patients with normal quality of life score (0-1 points) on ICU admission, 23.2% after 6 months, and 31.9% after 12 and 18 months (Figure 2).
Figure 2.
Percentage of patients according to the level of their quality of life score on intensive care admission and after 6, 12, and 18 months. Level 1 = 0-1 points, Level 2 = 2-5 points, Level 3 = 6-9 points, Level 4 ≥ 10 points. The first column of each level represents ICU admission, the second 6 months, the third 12 months, and the fourth 18 months.
The pre-ICU quality of life score in 18 patients lost to follow-up was 5.26 ± 5.29 points, which is higher than that of the study population, but the difference was not significant (P = 0.053). Study population and patients lost to follow-up had different results on NDA subscale (3.6 ± 3.5) (P = 0.040), but not on BPA (0.46 ± 1.06) and ES (1.2 ± 1.69) (P = 0.330 and P = 0.440, respectively) (Table 4).
Table 4.
Demographics and quality of life score on admission of 18 patients lost to follow-up (mean ± standard deviation)*
| Characteristic | |
|---|---|
| Sex M/F |
10/8 |
| Age (yrs) |
61.5 ± 20.8 |
| ICU stay (days) |
17.1 ± 32.9 |
| APACHE II |
17.3 ± 5.1 |
| SAPS II |
47.3 ± 10.2 |
| Quality of Life Score |
5.3 ± 5.3 |
| Quality of Life Subscale: |
|
| Basic Physiological Activities |
0.5 ± 1.1 |
| Normal Daily Activities |
3.6 ± 3.5 |
| Emotional State | 1.2 ± 1.7 |
Out of 116 patients, 112 (96%) returned to their previous place of residence and 4 (4%) were transferred to long-term care institutions. During the follow-up, 15 patients presented a new disease, 6 developed psychosis, 3 dementia, 2 epilepsy, 7 cardio respiratory failure, and 3 remained in a vegetative state.
Multivariate analysis
Multilinear regression analysis was performed in the study population to identify factors influencing the quality of life. Dependent variables were quality of life score on admission and changes in the quality of life score from baseline to 18 months after discharge. The variables with the strongest positive association with quality of life on admission were male sex (B = 3.270, P = 0.001) and age (B = 0.63, P = 0.002); and male sex (B = 3.934, P = 0.002), age (B = 0.129, P<0.001), and length of stay (B = 0.138, P<0.001) at 18 months after ICU discharge.
Discussion
This study examined the long-term outcome of critically ill patients who were discharged from the ICU. Although quality of life deteriorated after ICU discharge, a slow improvement was achieved. The overall quality of life and the quality of certain life domains showed a significant deterioration at 6 months after ICU admission and an important improvement from 12 to 18 months in all patients; however, this improvement was not uniform. The analysis suggested that age, length of ICU stay, and male sex were important risk factors influencing poor quality of life at 18 months after discharge from the ICU.
Many studies assessed the quality of life at 6 (6,12,13), 9 (14), and 12 months (15,16), and some had even longer follow-ups, such as 18 (17) and 24 months (18) or more than 2 years (19,20). When comparing the quality of life before and after ICU discharge, our results were quite similar to other studies assessing the quality of life at 12 and 18 months after ICU discharge (4,8,16,21-23). These studies showed that quality of life of patients after ICU discharge was significantly poorer than the preadmission status (4,8,16) or that of the general population (21-23). The deterioration in patients’ quality of life after ICU discharge found in most of the studies occurred due to the physical impact of critical illness. After a period of critical illness, patients often find themselves unable to accomplish even the simplest physical tasks without exhaustion. A variety of aspects of physical status may contribute to an impaired physical functioning and this may have an important impact on the quality of life (24).
Most of our patients showed an improvement in their quality of life 18 months after ICU discharge, principally by improving their normal daily activities. It seems that our study population needed more time to overcome the influence of the stress related to ICU and improve their emotional state. Several studies have assessed the natural progression of patients’ quality of life and reported that quality of life in survivors improved over time after ICU discharge (3,19,25). However, this improvement was not uniform across domains, and the time in which the quality of life could stabilize and return to that of the general population remains unclear. Cuthbertson et al (25) found a decrease in physical component scores 3 months after ICU discharge and then a slow increase to pre-morbid levels by the end of the first year. In a recent review (3), it was demonstrated that the quality of life in ICU survivors improved over time in most domains, but remained lower than in general population throughout the long-term follow-up. Studies showed that physical functioning rapidly improved, whereas mental health usually showed none or slow improvement. Kaarlola et al (19) found that a marked improvement was detected in psychological domains between 1 and 6 years after discharge from the ICU. In contrast to our findings, Wehler et al (6) reported that the quality of life of medical patients stabilized at 6 months after ICU discharge or regained its preadmission level.
Age, duration of stay, and male sex were the factors which had the strongest impact on the quality of life in our patients. Deterioration in quality of life increased with increased length of ICU stay and patients’ age. The study showed that male sex had a positive association with quality of life. Our findings are consistent with those reported by others (3,26). Age, gender, severity of illness, and length of ICU stay or preadmission quality of life score were the factors that had the strongest association with the quality of life of patients after the ICU discharge.
The limitations of our study include the lack comparison with a matched population and the fact that different studies used different quality of life instruments. Also, the Greek translation of this instrument has not been validated. However, our study may present an important advantage concerning the assessment of quality of life in the examined cohort. This assessment was repeated during the 18-month study period, which made us easier to understand the natural progression of our patients’ quality of life.
In conclusion, when evaluating the long-term outcome of ICU patients, the optimal timing of the assessment is essential because the emotional domain seem to improve slowly. This study showed that quality of life in our patients was substantially reduced after ICU discharge as opposed to preadmission. Eighteen months after ICU admission, quality of life status of most survivors showed an improvement but was still worse than on admission. This follow-up time is too short for a reliable assessment of the recovery in critically ill patients, since patients often need a longer time to get accustomed to new, and often more restricted, circumstances.
Acknowledgment
This study was partly financed by the Greek Ministry of Health. The authors thank Ricardo Rivera-Fernandez from the Project for the Epidemiological Analysis of Critical Care Patients for his permission to use the quality of life questionnaire, and Darin Peterson MPH, BSN for his assistance in the preparation of the manuscript.
References
- 1.Heyland DK, Konopad E, Noseworthy TW, Johnston R, Gafni A. Is it 'worthwhile' to continue treating patients with a prolonged stay (>14 days) in the ICU? An economic evaluation. Chest. 1998;114:192–8. doi: 10.1378/chest.114.1.192. [DOI] [PubMed] [Google Scholar]
- 2.Garrouste-Orgeas M, Carlet J. Predicting whether the ICU can help older patients: score needed. Crit Care. 2005;9:331–2. doi: 10.1186/cc3750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dowdy DW, Eid MP, Sedrakyan A, Mendez-Tellez PA, Pronovost PJ, Herridge MS, et al. Quality of life in adult survivors of critical illness: a systematic review of the literature. Intensive Care Med. 2005;31:611–20. doi: 10.1007/s00134-005-2592-6. [DOI] [PubMed] [Google Scholar]
- 4.Chaboyer W, Elliott D. Health-related quality of life of ICU survivors: review of the literature. Intensive Crit Care Nurs. 2000;16:88–97. doi: 10.1054/iccn.1999.1582. [DOI] [PubMed] [Google Scholar]
- 5.Fernandez RR, Cruz JJ, Mata GV. Validation of a quality of life questionnaire for critically ill patients. Intensive Care Med. 1996;22:1034–42. doi: 10.1007/BF01699224. [DOI] [PubMed] [Google Scholar]
- 6.Wehler M, Martus P, Geise A, Bost A, Mueller A, Hahn EG, et al. Changes in quality of life after medical intensive care. Intensive Care Med. 2001;27:154–9. doi: 10.1007/s001340000769. [DOI] [PubMed] [Google Scholar]
- 7.Rivera-Fernández R, Sánchez-Cruz JJ, Abizanda-Campos R, Vázquez-Mata G. Quality of life before intensive care unit admission and its influence on resource utilization and mortality rate. Crit Care Med. 2001;29:1701–9. doi: 10.1097/00003246-200109000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Vazquez Mata G, Rivera Fernandez R, Perez Aragon A, Gonzalez Carmona A, Fernandez Mondejar E, Navarrete Navarro P. Analysis of quality of life in polytraumatized patients two years after discharge from an intensive care unit. J Trauma. 1996;41:326–32. doi: 10.1097/00005373-199608000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Le Gall JR, Loirat P, Alperovitch A, Glaser P, Granthil C, Mathieu D, et al. A simplified acute physiology score for ICU patients. Crit Care Med. 1984;12:975–7. doi: 10.1097/00003246-198411000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–29. doi: 10.1097/00003246-198510000-00009. [DOI] [PubMed] [Google Scholar]
- 11.Capuzzo M, Grasselli C, Carrer S, Gritti G, Alvisi R. Validation of two quality of life questionnaires suitable for intensive care patients. Intensive Care Med. 2000;26:1296–303. doi: 10.1007/s001340000579. [DOI] [PubMed] [Google Scholar]
- 12.Hurel D, Loirat P, Saulnier F, Nicolas F, Brivet F. Quality of life 6 months after intensive care: results of a prospective multicenter study using a generic health status scale and a satisfaction scale. Intensive Care Med. 1997;23:331–7. doi: 10.1007/s001340050336. [DOI] [PubMed] [Google Scholar]
- 13.Granja C, Teixeira-Pinto A, Costa-Pereira A. Quality of life after intensive care–evaluation with EQ-5D questionnaire. Intensive Care Med. 2002;28:898–907. doi: 10.1007/s00134-002-1345-z. [DOI] [PubMed] [Google Scholar]
- 14.Graf J, Koch M, Dujardin R, Kersten A, Janssens U. Health-related quality of life before, 1 month after, and 9 months after intensive care in medical cardiovascular and pulmonary patients. Crit Care Med. 2003;31:2163–9. doi: 10.1097/01.CCM.0000079607.87009.3A. [DOI] [PubMed] [Google Scholar]
- 15.Eddleston JM, White P, Guthrie E. Survival, morbidity, and quality of life after discharge from intensive care. Crit Care Med. 2000;28:2293–9. doi: 10.1097/00003246-200007000-00018. [DOI] [PubMed] [Google Scholar]
- 16.Konopad E, Noseworthy TW, Johnston R, Shustack A, Grace M. Quality of life measures before and one year after admission to an intensive care unit. Crit Care Med. 1995;23:1653–9. doi: 10.1097/00003246-199510000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Garcia Lizana F, Peres Bota D, De Cubber M, Vincent JL. Long-term outcome in ICU patients: what about quality of life? Intensive Care Med. 2003;29:1286–93. doi: 10.1007/s00134-003-1875-z. [DOI] [PubMed] [Google Scholar]
- 18.Kvale R, Flaatten H. Changes in health-related quality of life from 6 months to 2 years after discharge from intensive care. Health Qual Life Outcomes. 2003;1:2. doi: 10.1186/1477-7525-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaarlola A, Pettila V, Kekki P. Quality of life six years after intensive care. Intensive Care Med. 2003;29:1294–9. doi: 10.1007/s00134-003-1849-1. [DOI] [PubMed] [Google Scholar]
- 20.Flaatten H, Kvale R. Survival and quality of life 12 years after ICU. A comparison with the general Norwegian population. Intensive Care Med. 2001;27:1005–11. doi: 10.1007/s001340100960. [DOI] [PubMed] [Google Scholar]
- 21.Wright JC, Plenderleith L, Ridley SA. Long-term survival following intensive care: subgroup analysis and comparison with the general population. Anaesthesia. 2003;58:637–42. doi: 10.1046/j.1365-2044.2003.03205.x. [DOI] [PubMed] [Google Scholar]
- 22.Brooks R, Kerridge R, Hillman K, Bauman A, Daffurn K. Quality of life outcomes after intensive care. Comparison with a community group. Intensive Care Med. 1997;23:581–6. doi: 10.1007/s001340050376. [DOI] [PubMed] [Google Scholar]
- 23.Badia X, Diaz-Prieto A, Gorriz MT, Herdman M, Torrado H, Farrero E, et al. Using the EuroQol-5D to measure changes in quality of life 12 months after discharge from an intensive care unit. Intensive Care Med. 2001;27:1901–7. doi: 10.1007/s00134-001-1137-x. [DOI] [PubMed] [Google Scholar]
- 24.Broomhead LR, Brett SJ. Clinical review: Intensive care follow-up–what has it told us? Crit Care. 2002;6:411–7. doi: 10.1186/cc1532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cuthbertson BH, Scott J, Strachan M, Kilonzo M, Vale L. Quality of life before and after intensive care. Anaesthesia. 2005;60:332–9. doi: 10.1111/j.1365-2044.2004.04109.x. [DOI] [PubMed] [Google Scholar]
- 26.Vazquez Mata G, Rivera Fernandez R, Gonzalez Carmona A, Delgado-Rodriguez M, Torres Ruiz JM, Raya Pugnaire A, et al. Factors related to quality of life 12 months after discharge from an intensive care unit. Crit Care Med. 1992;20:1257–62. doi: 10.1097/00003246-199209000-00012. [DOI] [PubMed] [Google Scholar]