Abstract
Tendons and ligaments are unique forms of connective tissue that are considered an integral part of the musculoskeletal system. The ultimate function of tendon is to connect muscles to bones and to conduct the forces generated by muscle contraction into movements of the joints, whereas ligaments connect bone to bone and provide joint stabilization. Unfortunately, the almost acellular and collagen I–rich structure of tendons and ligaments makes them very poorly regenerating tissues. Injured tendons and ligaments are considered a major clinical challenge in orthopedic and sports medicine. This Review discusses the several factors that might serve as molecular targets that upon activation can enhance or lead to tendon neoformation.
Introduction
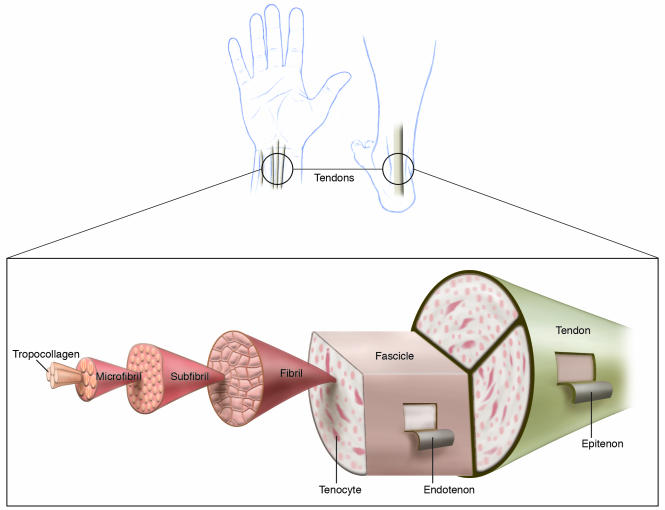
Tendons and ligaments are bundles of parallel fibers made of dense connective tissue that play an important role in mediating normal movement and stability of joints, respectively (1, 2) (Figure 1). Tendons and ligaments are similar in structure and are usually discussed in the same context. Therefore, the term tendon neoformation in this Review relates to the regeneration of both tendons and ligaments. Injury to these structures can cause significant joint instability, resulting in injury to other tissues and the development of degenerative joint diseases. Tendon healing starts with hematoma formation, followed by the formation of granulation tissue (3). Bone morphogenetic proteins (BMPs) and growth and differentiation factors (GDFs) are the main players in the latter process, which is followed by collagen fiber deposition and organization. Basic fibroblast growth factor (bFGF) seems to play a role during cell proliferation and invasion of vascular tissues into the healing tendon (4). Mechanical stimulation seems to be of great significance in tendon healing, contributing to mechanical strength in the regenerating tissue. However, most studies evaluating the role of mechanical stimulation during the healing process relate to animal studies, and the significance of mechanical stimulation in humans is still unclear (3).
Figure 1. Tendon structure and composition.
The structure of tendons is organized such that they provide resistance against the longitudinal stress generated by muscles. Chains of tropocollagen are longitudinally arranged and united into fibers that together form fibrils. Fibrils are organized and held in a linear direction by loose connective tissue called the endotenon such that they form fascicles. Fascicles are also packed by a loose connective tissue continuous with the endotenon that is called epitenon. The epitenon holds the structure of the tendon and provides its microvasculature. Reproduced from ref. 49.
In general, tendon injury occurs due to acute trauma or inflammation of either the tendon tissue or the surrounding tissues. This includes a range of conditions including tendonitis (inflammation of the tendon), tendinosis (tendon degeneration due to failure of the healing of injured tendon), bursitis (inflammation or irritation of the bursa, a small sac located between bone and tendon), epicondylitis (inflammation or damage to the area of an epicondyle of bone that may damage adjacent tendons), and complete tendon rupture, depending on the extent of the tissue damage (5, 6). The most common of these injuries are to the supraspinatus tendon of the rotator cuff, the Achilles tendon, the flexor tendons of the hand, and the anterior cruciate and medial collateral ligaments of the knee (7). Four options have been utilized for repair or replacement of damaged tendons: autografts, allografts, xenografts, and synthetic polymers. Implantation of synthetic polymers was a very popular surgical technique in the 1980s, but it frequently led to implant degeneration and failure (8, 9). Autografts (patellar tendon with bony attachments or two of four hamstring tendons harvested from the patient at the time of surgery) have produced the most satisfactory long-term results and are referred to as the “gold standard” for treating severe tendon injuries (10, 11). Donor site morbidity, which is often associated with pain, muscle atrophy, and tendonitis, remains the limiting factor for patellar tendon autografts and results in prolonged rehabilitation periods (12). The use of allografts is still at an experimental stage and might cause immune reactions (13–15) that could hinder tendon tissue remodeling (16, 17). The risks of disease transmission and infection, the lack of donors, and donor-recipient compatibility are additional significant obstacles to the use of allografts to repair and/or replace damaged tendons. The use of xenografts is still experimental as well, and the potential of this source is still questionable (18). In light of the disadvantages of current surgical solutions for tendon repair, the use of novel biological methods should be investigated. The focus of this Review is molecules that, through their activation or manipulation, might be targets for tendon neoformation.
Tendon morphogenesis and molecular markers of tendon development
The unique embryonic development of tendons is highly associated with muscle development in a sequential series of events (19–21). These events are initiated by formation of the somites, which are epithelial spheres on each side of the neural tube (19–21). The somites are later patterned into compartments that give rise to distinct cell lineages (19–21). The formation of muscles and the muscle fasciae during limb development is specified by several signaling events that involve sonic hedgehog (Shh), Wnt signaling, and other factors, such as myogenic differentiation 1 (MyoD) and paired box 3 (Pax3) (19).
In contrast to muscle, tendon morphogenesis is less understood. From most studies of limb tendon development, it seems that tendons first arise from the lateral plate mesoderm as tendon primordia, which subsequently divide into individual and distinct tendons (22, 23). The continued development of limb tendons seems to be more complicated, as the morphogenesis of proximal limb tendons is significantly different from the morphogenesis of distal tendons, and each type of tendon expresses different molecular markers during morphogenesis (20). Tenascin is a protein that can be detected in all tendon blastema (masses of undifferentiated cells) and proximal tendons, as well as tendon primordia and all differentiated tendons (20, 24). However, tenascin seems not to be a specific marker of tendons, since it is expressed by other cell types, including glial cells and chondrocytes (20, 24). A more specific marker of tendon development is scleraxis (Scx), a basic helix-loop-helix (bHLH) transcription factor that is expressed in mature tendons and ligaments of the limbs and trunk, as well as in their progenitors (25). The gene encoding Scx is expressed in all connective tissues that mediate attachment of muscle to bone in chick and mouse as well as in the progenitors of these connective tissues found in the early mesenchyme (25). Scx gene expression is induced in superficial mesenchyme–derived tendon progenitors by the adjacent ectoderm (25). Its expression is restricted to these cells by BMPs, which inhibit Scx gene expression, and this inhibition is antagonized by Noggin (25). In addition to Scx, the homeobox gene sine oculis–related homeobox 1 homolog (Six1) has been proposed as a potential “player” in the development of tendons (26). Six1 and Six2 are expressed in a complementary fashion during the development of mouse limb tendons, Six1 being expressed in dorsal extensor tendons and Six2 in the ventral flexor tendons of the digits (27, 28). These studies initially suggested that Six1 might be involved in the early development of tendons; however, Bonnin et al. (26) reported that, during limb development in mouse and chick, expression of the Six1 gene is distinct from tendon primordia and from tendons defined by Scx expression. In addition, analysis of Pax3–/– mice (mice in which tendons develop but not muscles) at E12.5 indicated that the nonmyogenic domains (the sites at which muscles should develop) in these mice displayed similar expression of both Six1 and Scx as the sites of limb development in WT mice at E12.5 (26). Later, at E13.5, the expression of Scx in Pax3–/– mice was downregulated, whereas Six1 expression remained similar to that in normal mice (26). One potential explanation for these data is that tendon development (represented by the expression of Scx) requires the normal development of the muscles. Finally, the authors (26) found that expression of Scx was not affected in Six1–/– mutant limbs; however, tendon development was still impaired due to the diminution of muscle tissue in these mice. Therefore, it now seems that the initial stages of tendon development are independent of Six1; however, lack of Six1 expression still affects the continuation of tendon development due to the lack of normal muscle development in its absence (26). Other markers of tendon development, such as tenomodulin (TeM), have also been described (29). Expression of the gene encoding TeM was found in association with the appearance of tenocytes (also called tendon fibroblasts), derived from tendon primordia, during chick development and is upregulated by retrovirus-mediated Scx expression in cultured tenocytes (29). These data suggest that TeM as a late marker of tendon morphogenesis and that expression of the gene encoding TeM is positively regulated by Scx in tenocytes.
It is important to note that there is still no evidence that the molecular markers of tendon morphogenesis are able to induce tendon neoformation upon their activation. However, we believe that a basic understanding of the molecules associated with tendon development is required to achieve neoformation of this tissue.
The molecular basis of tendon neoformation
Although none of the markers of tendon morphogenesis have been shown to be potential targets for tendon neoformation, there is some evidence that the activation of specific factors can elicit tendon neoformation. The most well documented of these factors are GDFs and Scx, and the potential of these factors to affect tendon neoformation when activated is discussed here.
GDFs.
GDFs are a subgroup of the TGF-β/BMP superfamily (30). Like all members of this superfamily, they are secreted as mature peptides forming homo- or heterodimers (30). Initial studies suggested that murine GDF5, GDF6, and GDF7 play a role in osteogenesis via the process of endochondral ossification, i.e., bone formation that starts with mesenchymal cell condensations that form a cartilage matrix that later calcifies to form mature bone (31, 32). Storm and Kingsley (33) were the first to identify Gdf5 as a joint-related marker in various locations in murine embryogenesis. These authors also examined the response of developing chick and mouse limbs to recombinant GDF5 and revealed that GDF5 was necessary and sufficient for both cartilage development and the restriction of joint formation to the appropriate location (33). Evidence of a role for GDF5 in tendon formation was provided by the investigation of GDF5-deficient mice; these mice displayed tendon abnormalities such as thinner patellar tendon, mainly due to altered collagen structure (34). Moreover, a developmental failure of the condyles (the ends of two bones that form the joint) and intra-articular ligament of the knee joint in GDF5-deficient mice was recently described (35). Interestingly, excessive death through apoptosis of mesenchymal cells was observed in the GDF5-deficient mouse in the area where the knee joint would develop (35). Together, these studies suggest a role for GDF5 in joint development; however, they provided little evidence of a role for GDF5 in tendon morphogenesis.
In addition to the effects of GDFs on skeletal morphogenesis in general and tendon formation in particular, GDFs were studied in adult animal models of tendon neoformation. Wolfman and colleagues (36) have shown that expression of human GDF5, GDF6, and GDF7 at ectopic sites in the adult animal demonstrate novel possible roles for these factors. GDFs showed the ability to induce ectopic formation of connective tissue rich in collagen I in a fashion that resembles neoformation of tendon and ligament (36). In addition, intramuscular or subcutaneous coimplantation of GFD5, GDF6, or GDF7 with BMP-2 resulted in the formation of tissue containing both bone and tendon, suggesting that GDFs exert a tenogenic effect even in the presence of BMP-2 and under osteogenic conditions (36). This report and others (37) provide significant evidence that GDFs have an effect on the regeneration or neoformation of tendon in the adult, as well as in tendon morphogenesis in the developing animal. Delivery of recombinant human GDF5 (rhGDF5) via sutures to the site of injured rat tendons resulted in enhanced healing and significantly higher ultimate tensile load and stiffness compared with control sutures containing no rhGDF5 (37).
To achieve effective healing and repair of injured tissue through exogenous intervention, such as delivery of growth factors (e.g., delivery of GDFs to torn tendon), it is crucial to understand the sequence of events that occur during the natural healing of this tissue. When tendon is injured, a hematoma is formed at the site of the injury, providing a matrix for the invading mesenchymal cells that later play an important role in the repair of the ruptured tendon (3). Injection of GDFs at the hematoma formation phase was suggested as a promising therapeutic approach for injured tendon healing (38). Delivery of a GDF5 transgene by means of adenoviral vectors to the site of ruptured rat Achilles tendon resulted in thicker, stronger tendon regenerates compared with those in the control group (after 8 weeks; ref. 39). It is important to note, though, that more cartilage was found in the treated tendons, a fact that might indicate possible complications in the healing process, as the resulting tendon might have impaired mechanical strength (39).
It seems that the aforementioned GDFs, especially GDF5, are good candidates for inducing tendon neoformation as well as enhancing tendon regeneration. However, the tendency of GDFs to induce cartilage and bone formation in vivo (40, 41) could hamper the use of those factors for tendon regeneration. Since the effects of GDFs were found to be dose dependent in a rat model — 300 μg of rhGDF5 induced cartilage and bone formation, whereas 500 μg induced only bone formation (41) — it is possible that fine-tuning of the factor amount will be sufficient to solve this problem and achieve controlled healing of tendon tissue.
Scx.
In addition to GDFs, intensive research has been invested in finding a molecular marker of tendon neoformation. Scx is the best-characterized marker of tendon morphogenesis, and there is increasing evidence that it might be a molecular marker of tendon neoformation.
Scx is a bHLH transcription factor (42) that can bind to DNA sequences containing the E-box consensus sequence through its bHLH motif (43). During mouse embryogenesis, Scx transcripts are strongly detected in both the zone of the limb bud tendon progenitors (25) and the somitic compartment of tendon progenitors called the syndetome (21).
Sequence analysis of Scx revealed that all of the conserved amino acids that define the bHLH family are present (44). However, other residues in the basic regions were different from other bHLH transcription factors, suggesting that Scx binds a specific set of E-boxes (44). Despite the fact that high levels of Scx transcripts were found in progenitors of tendons as well as other structures (e.g., cartilage and bone) that require secretion of high levels of extracellular matrix proteins such as collagen I and II (44), the role of Scx seems to be specifically restricted to the function of tendon progenitors (21). In both thoracic (chest) and cervical (neck) somites, Scx is localized to the anterior and posterior borders and does not overlap with MyoD at the center of the myotome. Thus, Scx is expressed in an anatomical location similar to, but nonoverlapping with, that of MyoD, which determines muscle morphogenesis. This suggests that Scx functions in tendon development in close association with muscle development but that its function does not overlap with that of MyoD (21). This is important because of the necessity of choosing molecular targets for tendon neoformation that will not cause muscle neoformation.
Although several reports have demonstrated a role for Scx in tendon morphogenesis, there is still no evidence that Scx activation can induce tendon neoformation. Scx binds to the E-box consensus sequence as a heterodimer with E12 (a member of the family of E-proteins that heterodimerize with bHLH proteins and bind DNA to regulate gene expression). In addition, Scx alone is a potent transactivator of gene expression through its multimerized DNA-binding site (44). Léjard et al. (45) reported that Scx regulates the expression of the gene encoding collagen, type 1, α1 (COL1a1) in tendon fibroblasts through two short elements named TSE1 and TSE2, which are needed for mouse Col1a1 expression in tendon fibroblasts (45).
The role(s) of Scx in embryogenesis could not be addressed for many years because homozygous knockout mice died during early embryogenesis (46). More recently, mutant mice homozygous for a null Scx allele (Scx–/– mice) have been found to be viable and display severely disrupted tendon differentiation and formation. The severity of this disruption was highly variable (47); some tendons, such as the force-transmitting and intermuscular tendons, were severely affected, whereas muscle-anchoring tendons and ligaments were totally unaffected. The study also showed that in Scx–/– mice, the processes of tendon progenitor condensation and differentiation were affected (47). In tendons that persisted in Scx–/– mice, tendon matrix was reduced and disorganized, and the cellular organization of the tendons was disrupted (47). These findings support the study by Léjard et al. (45) and suggest that Scx activates the expression of target genes involved in tendon development (45); however, the identity and function of these are still unknown.
In summary, we might conclude that the bHLH transcription factor Scx is an important marker of tendon neoformation. In addition, its involvement in tendon neoformation suggests that, if activated, Scx might be able to induce tendon regeneration. Molecular studies using animal models of tendon tissue repair and targeted expression of Scx should shed some light on the clinical potential of this factor.
The role of cell lines in tendon neoformation
Our group and collaborators have recently engineered the murine mesenchymal stem cell line C3H10T1/2 to coexpress BMP-2 and a biologically active truncated form of the Smad8 protein and used it to generate tendon neoformation (48, 49). The Smad proteins are a group of eight related intracellular proteins critical for transmitting signals from the cell-surface receptors of TGF-β/BMP superfamily members to the nucleus. Although Smad1 and Smad5 are well studied and have an important role in osteogenic differentiation (50), the exact role of Smad8 in osteogenesis was not described before. Although expression of BMP-2 in C3H10T1/2 cells induces osteogenesis, we observed that coexpression of the biologically active truncated Smad8 and BMP-2 induced tendon neoformation and blocked the differentiation of cartilage and bone tissues (48, 49). These results were noted both in vitro and in vivo. Indeed, the remarkable ability of the cells engineered to express both BMP-2 and the biologically active truncated Smad8 to fill the gap in a rat Achilles tenotomy model with tendon-like tissue makes the combination of stem cell and gene therapy highly attractive (48, 49).
Recently, two important studies have identified novel cell populations as candidates for neotendon formation (51, 52). Yokoi et al. (51) immortalized mouse dental follicle cells by engineering them to express a mutant form of the human papillomavirus type 16 (HPV16) E6 protein that lacked the PDZ domain–binding motif, resulting in a longer life span of these cells. When analyzed, these cells expressed tendon/ligament phenotype–related genes such as those encoding Scx, GDF5, EPH receptor A4 (EphA4), Six-1, and type I collagen. When implanted in vivo, these cells generated periodontal ligament-like tissue after four weeks (51). These results suggest that the aforementioned cell line might be useful in neotendon formation and in healing of tendon defects.
Bi et al. (52) have recently identified tendon stem/progenitor cells (TSPCs). These cells were demonstrated to be self-regenerating and had the capability of tenogenic differentiation. To test the feasibility of these cells as initiators of tendon neoformation, the researchers implanted GFP-expressing mouse TSPCs under the skin of mice together with different carriers to serve as a scaffold for the forming tissue. Tendon-like tissues were generated from the GFP-expressing TSPCs when implanted with Gelfoam, hydroxyapaptite/tricalcium phosphate (HA/TCP), or Matrigel as a carrier. The regenerated tendon-like tissues showed tendon-specific parallel alignments of collagen fibers and stained strongly for type I collagen, and the donor origin of the cells within the newly formed tendons was confirmed by their expression of GFP. Remarkably, when mouse TSPCs were treated with BMP-2 and then transplanted subcutaneously into immunocompromised mice, structures similar to osteotendinous junctions (termed entheses) were formed. More notably, when transplanted with HA/TCP onto the surface of mouse cranial bone, human TSPCs formed condensed collagen fibers that were inserted into the bone and were similar to Sharpey fibers (52). These striking results could pave the way for tendon neoformation and regeneration using progenitor cells. The ability to generate bone-ligament interface is specifically of great importance, as it can be useful in healing torn tendons and ligaments that require reattachment to bone.
Putting together the molecular puzzle to complete the clinical picture
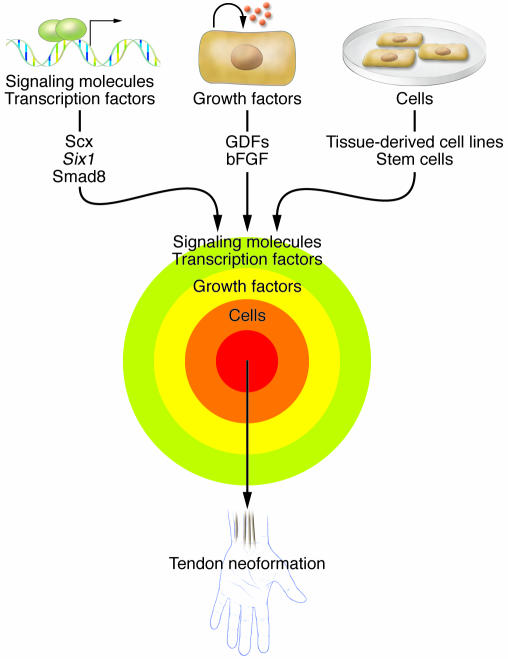
Tendon neoformation in the adult is of importance due to the fact that this process is critical for achieving complete and efficient healing of ruptured tendons. However, complete tendon healing requires the sequential and coordinated expression of several molecules and growth factors, each responsible for specific and distinct process. In addition, the presence of cells that would support the formation of new tissue is of great significance (Figure 2).
Figure 2. A proposed integrative approach toward achieving successful tendon neoformation.
To achieve successful tendon neoformation or regeneration, three main approaches have been described in the literature. Through activation of some transcription factors and signaling molecules (for example, Scx, Six1, and Smad8) that are involved in tendon/ligament morphogenesis, tendon neoformation might be successful. Growth factors such as GDFs have also been described as inducers or enhancers for tendon regeneration. Cells provide the progenitors or stem cells that respond to signals such as growth factors and, through activation of signaling molecules and transcription factors, differentiate into tendon/ligament. We propose that combining these three approaches is necessary to successfully achieve tendon neoformation.
The most promising candidate molecules that upon activation might lead to tendon neoformation have been briefly reviewed here. There might be several ways of activating these molecules for tendon regeneration in the clinic. When envisioning the use of GDFs for treating tendon defects, the use of recombinant proteins seems most relevant. Judging by the successful use of BMP-2 and BMP-7 in orthopedics for bone regeneration (53–55), it might be possible that recombinant GDFs could be approved for clinical use in the treatment of ruptured tendons with relative ease. It is important to note, though, that the use of megadoses of expensive recombinant proteins might limit this potential use. Scx and Smad8, both intracellular proteins, could be used via a gene therapy–based approach, since extracellular application of the proteins would not generate an effect in situ. Such approaches could include direct gene therapy (most probably using nonviral vectors) or even cell-based gene therapy (using genetically engineered autologous cells as gene carriers as well as building blocks for the regeneration process). Molecules that selectively activate Scx or its target genes also might be beneficial. However, extensive studies are needed to promote those solutions to the clinical arena, especially the characterization of an optimal factor that can induce tendon neoformation in various models of tendon injury.
Footnotes
Nonstandard abbreviations used: bHLH, basic helix-loop-helix; BMP, bone morphogenetic protein; GDF, growth and differentiation factor; MyoD, myogenic differentiation 1; Pax3, paired box 3; rhGDF5, recombinant human GDF5; Scx, scleraxis; Six1, sine oculis–related homeobox 1 homolog; TeM, tenomodulin; TSPC, tendon stem/progenitor cell.
Conflict of interest: The authors have declared that no conflict of interest exists.
Citation for this article: J. Clin. Invest. 118:439–444 (2008). doi:10.1172/JCI33944.
References
- 1.Roeleveld K., Baratta R.V., Solomonow M., van Soest A.G., Huijing P.A. Role of tendon properties on the dynamic performance of different isometric muscles. J. Appl. Physiol. 1993;74:1348–1355. doi: 10.1152/jappl.1993.74.3.1348. [DOI] [PubMed] [Google Scholar]
- 2.Sharma M., Langrana N.A., Rodriguez J. Role of ligaments and facets in lumbar spinal stability. Spine. 1995;20:887–900. doi: 10.1097/00007632-199504150-00003. [DOI] [PubMed] [Google Scholar]
- 3.Aspenberg P. Stimulation of tendon repair: mechanical loading, GDFs and platelets. A mini-review. Int. Orthop. 2007;31:783–789. doi: 10.1007/s00264-007-0398-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chang J., et al. Molecular studies in flexor tendon wound healing: the role of basic fibroblast growth factor gene expression. J. Hand Surg. [Am]. 1998;23:1052–1058. doi: 10.1016/S0363-5023(98)80015-4. [DOI] [PubMed] [Google Scholar]
- 5.Biundo J.J., Jr., Irwin R.W., Umpierre E. Sports and other soft tissue injuries, tendinitis, bursitis, and occupation-related syndromes. Curr. Opin. Rheumatol. 2001;13:146–149. doi: 10.1097/00002281-200103000-00008. [DOI] [PubMed] [Google Scholar]
- 6.Baring T., Emery R., Reilly P. Management of rotator cuff disease: specific treatment for specific disorders. Best Pract. Res. Clin. Rheumatol. 2007;21:279–294. doi: 10.1016/j.berh.2006.12.001. [DOI] [PubMed] [Google Scholar]
- 7.Carpenter J.E., Thomopoulos S., Soslowsky L.J. Animal models of tendon and ligament injuries for tissue engineering applications. Clin. Orthop. Relat. Res. . 1999;367(Suppl.):S296–S311. doi: 10.1097/00003086-199910001-00029. [DOI] [PubMed] [Google Scholar]
- 8.Olson E.J., et al. The biochemical and histological effects of artificial ligament wear particles: in vitro and in vivo studies. Am. J. Sports Med. 1988;16:558–570. doi: 10.1177/036354658801600602. [DOI] [PubMed] [Google Scholar]
- 9.Woods G.A., Indelicato P.A., Prevot T.J. The Gore-Tex anterior cruciate ligament prosthesis. Two versus three year results. Am. J. Sports Med. 1991;19:48–55. doi: 10.1177/036354659101900108. [DOI] [PubMed] [Google Scholar]
- 10.Shelbourne K.D., Vanadurongwan B., Gray T. Primary anterior cruciate ligament reconstruction using contralateral patellar tendon autograft. Clin. Sports Med. 2007;26:549–565. doi: 10.1016/j.csm.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 11.Poolman R.W., Abouali J.A., Conter H.J., Bhandari M. Overlapping systemic reviews of anterior cruciate ligament reconstruction comparing hamstring autograft with bone-patellar tendon-bone autograft: why are they different? J. Bone Joint Surg. Am. 2007;89:1542–1552. doi: 10.2106/JBJS.F.01292. [DOI] [PubMed] [Google Scholar]
- 12.Weitzel P.P., Richmond J.C., Altman G.H., Calabro T., Kaplan D.L. Future direction of the treatment of ACL ruptures. Orthop. Clin. North Am. 2002;33:653–661. doi: 10.1016/s0030-5898(02)00017-2. [DOI] [PubMed] [Google Scholar]
- 13.Jackson D.W., Simon T.M., Kurzweil P.R., Rosen M.A. Survival of cells after intra-articular transplantation of fresh allografts of the patellar and anterior cruciate ligaments. DNA-probe analysis in a goat model. J. Bone Joint Surg. Am. 1992;74:112–118. [PubMed] [Google Scholar]
- 14.Sabiston P., Frank C., Lam T., Shrive N. Allograft ligament transplantation. A morphological and biochemical evaluation of a medial collateral ligament complex in a rabbit model. Am. J. Sports Med. 1990;18:160–168. doi: 10.1177/036354659001800209. [DOI] [PubMed] [Google Scholar]
- 15.Jackson D.W., et al. A comparison of patellar tendon autograft and allograft used for anterior cruciate ligament reconstruction in the goat model. Am. J. Sports Med. 1993;21:176–185. doi: 10.1177/036354659302100203. [DOI] [PubMed] [Google Scholar]
- 16.Buckwalter, J.A., and Woo, S.L.-Y. 1988. Ligaments. In Injury and repair of the musculoskeletal soft tissues. J.A. Buckwalter and S.L.-Y. Woo, editors. American Academy of Orthopaedic Surgeons. Rosemont, Illinois, USA. [Google Scholar]
- 17.Noyes F.R., Butler D.L., Grood E.S., Zernicke R.F., Hefzy M.S. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J. Bone Joint Surg. Am. 1984;66:344–352. [PubMed] [Google Scholar]
- 18.Stone K.R., Abdel-Motal U.M., Walgenbach A.W., Turek T.J., Galili U. Replacement of human anterior cruciate ligaments with pig ligaments: a model for anti-non-gal antibody response in long-term xenotransplantation. Transplantation. 2007;83:211–219. doi: 10.1097/01.tp.0000250598.29377.13. [DOI] [PubMed] [Google Scholar]
- 19.Brent A.E., Tabin C.J. Developmental regulation of somite derivatives: muscle, cartilage and tendon. Curr. Opin. Genet. Dev. 2002;12:548–557. doi: 10.1016/s0959-437x(02)00339-8. [DOI] [PubMed] [Google Scholar]
- 20.Kardon G. Muscle and tendon morphogenesis in the avian hind limb. Development. 1998;125:4019–4032. doi: 10.1242/dev.125.20.4019. [DOI] [PubMed] [Google Scholar]
- 21.Brent A.E., Schweitzer R., Tabin C.J. A somitic compartment of tendon progenitors. Cell. 2003;113:235–248. doi: 10.1016/s0092-8674(03)00268-x. [DOI] [PubMed] [Google Scholar]
- 22.Hurle J., Hinchliffe J.R., Ros M.A., Critchlow M.A., Genis-Galvez J.M. The extracellular matrix architecture relating to myotendinous pattern formation in the distal part of the developing chick limb: an ultrastructural, histochemical and immunocytochemical analysis. Cell Differ. Dev. 1989;27:103–120. doi: 10.1016/0922-3371(89)90740-5. [DOI] [PubMed] [Google Scholar]
- 23.Ros M., Rivero F.B., Hinchliffe J.R., Hurle J.M. Immunohistological and ultrastructural study of the developing tendons of the avian foot. Anat. Embryol. (Berl.). 1995;192:483–496. doi: 10.1007/BF00187179. [DOI] [PubMed] [Google Scholar]
- 24.Chiquet M., Fambrough D.M. Chick myotendinous antigen. I. A monoclonal antibody as a marker for tendon and muscle morphogenesis. . J. Cell Biol. 1984;98:1926–1936. doi: 10.1083/jcb.98.6.1926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Schweitzer R., et al. Analysis of the tendon cell fate using Scleraxis, a specific marker for tendons and ligaments. Development. 2001;128:3855–3866. doi: 10.1242/dev.128.19.3855. [DOI] [PubMed] [Google Scholar]
- 26.Bonnin M., et al. Six1 is not involved in limb tendon development, but is expressed in limb connective tissue under Shh regulation. Mech. Dev. . 2005;122:573–585. doi: 10.1016/j.mod.2004.11.005. [DOI] [PubMed] [Google Scholar]
- 27.Oliver G., et al. Homeobox genes and connective tissue patterning. Development. . 1995;121:693–705. doi: 10.1242/dev.121.3.693. [DOI] [PubMed] [Google Scholar]
- 28.Dreyer S.D., et al. Lmx1b expression during joint and tendon formation: localization and evaluation of potential downstream targets. Gene Expr. Patterns. 2004;4:397–405. doi: 10.1016/j.modgep.2004.01.006. [DOI] [PubMed] [Google Scholar]
- 29.Shukunami C., Takimoto A., Oro M., Hiraki Y. Scleraxis positively regulates the expression of tenomodulin, a differentiation marker of tenocytes. Dev. Biol. 2006;298:234–247. doi: 10.1016/j.ydbio.2006.06.036. [DOI] [PubMed] [Google Scholar]
- 30.Herpin A., Lelong C., Favrel P. Transforming growth factor-beta-related proteins: an ancestral and widespread superfamily of cytokines in metazoans. Dev. Comp. Immunol. 2004;28:461–485. doi: 10.1016/j.dci.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 31.Chang S.C., et al. Cartilage-derived morphogenetic proteins. J. Biol. Chem. 1994;269:28227–28234. [PubMed] [Google Scholar]
- 32.Storm E.E., et al. Limb alterations in brachypodism mice due to mutations in a new member of the TGF-b superfamily. Nature. 1994;368:639–642. doi: 10.1038/368639a0. [DOI] [PubMed] [Google Scholar]
- 33.Storm E., Kingsley DM. Joint patterning defects caused by single and double mutations in members of the bone morphogenetic protein (BMP) family. Development. 1996;122:3969–3979. doi: 10.1242/dev.122.12.3969. [DOI] [PubMed] [Google Scholar]
- 34.Mikic B. Multiple effects of GDF-5 deficiency on skeletal tissues: implications for therapeutic bioengineering. Ann. Biomed. Eng. 2004;32:466–476. doi: 10.1023/b:abme.0000017549.57126.51. [DOI] [PubMed] [Google Scholar]
- 35.Harada M., et al. Developmental failure of the intra-articular ligaments in mice with absence of growth differentiation factor 5. Osteoarthr. Cartil. 2007;15:468–474. doi: 10.1016/j.joca.2006.09.003. [DOI] [PubMed] [Google Scholar]
- 36.Wolfman N.M., et al. Ectopic induction of tendon and ligament in rats by growth and differentiation factors 5, 6, and 7, members of the TGF-beta gene family. J. Clin. Invest. 1997;100:321–330. doi: 10.1172/JCI119537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dines J.S., et al. The effect of growth differentiation factor-5-coated sutures on tendon repair in a rat model. J. Shoulder Elbow Surg. 2007;16:S204–S207. doi: 10.1016/j.jse.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 38.Aspenberg P., Forslund C. Enhanced tendon healing with GDF 5 and 6. Acta Orthop. Scand. 1999;70:51–54. doi: 10.3109/17453679909000958. [DOI] [PubMed] [Google Scholar]
- 39.Rickert M., et al. Adenovirus-mediated gene transfer of growth and differentiation factor-5 into tenocytes and the healing rat Achilles tendon. Connect. Tissue Res. 2005;46:175–183. doi: 10.1080/03008200500237120. [DOI] [PubMed] [Google Scholar]
- 40.Hotten G.C., et al. Recombinant human growth/differentiation factor 5 stimulates mesenchyme aggregation and chondrogenesis responsible for the skeletal development of limbs. Growth Factors. 1996;13:65–74. doi: 10.3109/08977199609034567. [DOI] [PubMed] [Google Scholar]
- 41.Kakudo N., Wang Y.B., Miyake S., Kushida S., Kusumoto K. Analysis of osteochondro-induction using growth and differentiation factor-5 in rat muscle. Life Sci. 2007;81:137–143. doi: 10.1016/j.lfs.2007.04.038. [DOI] [PubMed] [Google Scholar]
- 42.Kadesch T. Consequences of heteromeric interactions among helix-loop-helix proteins. Cell Growth Differ. 1993;4:49–55. [PubMed] [Google Scholar]
- 43.Murre C., et al. Interactions between heterologous helix-loop-helix proteins generate complexes that bind specifically to a common DNA sequence. Cell. 1989;58:537–544. doi: 10.1016/0092-8674(89)90434-0. [DOI] [PubMed] [Google Scholar]
- 44.Cserjesi P., et al. Scleraxis: a basic helix-loop-helix protein that prefigures skeletal formation during mouse embryogenesis. Development. 1995;121:1099–1110. doi: 10.1242/dev.121.4.1099. [DOI] [PubMed] [Google Scholar]
- 45.Léjard V., et al. Scleraxis and NFATc regulate the expression of the pro-alpha1(I) collagen gene in tendon fibroblasts. J. Biol. Chem. 2007;282:17665–17675. doi: 10.1074/jbc.M610113200. [DOI] [PubMed] [Google Scholar]
- 46.Brown D., Wagner D., Li X., Richardson J.A., Olson E.N. Dual role of the basic helix-loop-helix transcription factor scleraxis in mesoderm formation and chondrogenesis during mouse embryogenesis. Development. 1999;126:4317–4329. doi: 10.1242/dev.126.19.4317. [DOI] [PubMed] [Google Scholar]
- 47.Murchison N., et al. Regulation of tendon differentiation by scleraxis distinguishes force-transmitting tendons from muscle-anchoring tendons. Development. 2007;134:2697–2708. doi: 10.1242/dev.001933. [DOI] [PubMed] [Google Scholar]
- 48.Hoffmann A., et al. Neotendon formation induced by manipulation of the Smad8 signalling pathway in mesenchymal stem cells. J. Clin. Invest. 2006;116:940–952. doi: 10.1172/JCI22689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Towler D.A., Gelberman R.H. The alchemy of tendon repair: a primer for the (S)mad scientist. J. Clin. Invest. 2006;116:863–866. doi: 10.1172/JCI28320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Cao X., Chen D. The BMP signaling and in vivo bone formation. Gene. 2005;357:1–8. doi: 10.1016/j.gene.2005.06.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yokoi T., et al. Establishment of immortalized dental follicle cells for generating periodontal ligament in vivo. Cell Tissue Res. 2007;327:301–311. doi: 10.1007/s00441-006-0257-6. [DOI] [PubMed] [Google Scholar]
- 52.Bi Y., et al. Identification of tendon stem/progenitor cells and the role of the extracellular matrix in their niche. Nat. Med. 2007;13:1219–1227. doi: 10.1038/nm1630. [DOI] [PubMed] [Google Scholar]
- 53.Biasibetti A., Aloj D., Di Gregorio G., Masse A., Salomone C. Mechanical and biological treatment of long bone non-unions. Injury. 2005;36(Suppl. 4):S45–S50. doi: 10.1016/j.injury.2005.10.013. [DOI] [PubMed] [Google Scholar]
- 54.De Biase P., Capanna R. Clinical applications of BMPs. Injury. 2005;36(Suppl. 3):S43–S46. doi: 10.1016/j.injury.2005.07.034. [DOI] [PubMed] [Google Scholar]
- 55.Villavicencio A.T., et al. Safety of transforaminal lumbar interbody fusion and intervertebral recombinant human bone morphogenetic protein-2. J. Neurosurg. Spine. 2005;3:436–443. doi: 10.3171/spi.2005.3.6.0436. [DOI] [PubMed] [Google Scholar]