Abstract
Patients with coeliac artery occlusion often remain asymptomatic due to the rich collateral blood supply (pancreaticoduodenal arcades) from the superior mesenteric artery. However, division of the gastroduodenal artery (GDA) during pancreaticoduodenectomy may result in compromised blood supply to the liver, stomach and spleen. Postoperative complications associated with this condition are rarely reported in the literature. We report two cases of coeliac artery occlusion encountered during pancreaticoduodenectomy, one of which was complicated by hepatic ischaemia and total gastric infarction postoperatively. Based on our experience and review of the literature, a management algorithm for coeliac artery stenosis encountered during pancreaticoduodenectomy is proposed
Introduction
In patients with coeliac artery stenosis, ligation of the gastroduodenal artery during pancreaticoduodenectomy seldom results in clinically significant ischaemia due to the rich collateral circulation (gastroduodenal-pancreaticoduodenal) from the superior mesenteric artery (SMA). We report two cases of coeliac artery occlusion encountered during pancreaticoduodenectomy, one of which was complicated by hepatic ischaemia and total gastric infarction postoperatively.
Case reports
Case 1
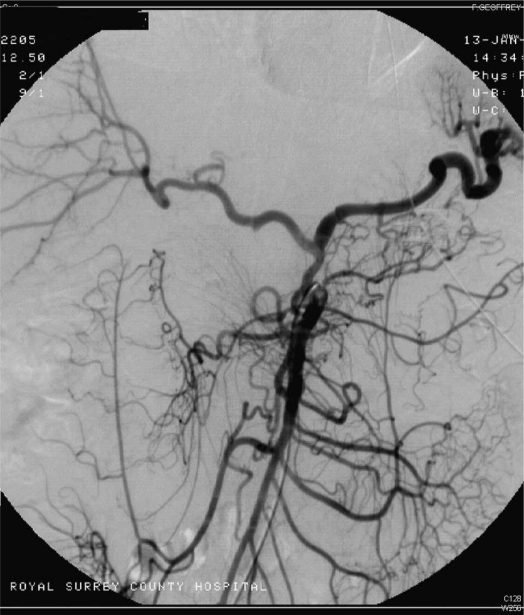
A 56-year-old man underwent pylorus-preserving pancreaticoduodenectomy for intraductal papillary mucinous adenocarcinoma (IPMT) of the head of pancreas with an Imanaga reconstruction. During surgery the gastroduodenal artery (GDA) was noted to be dilated and traversing the tumour in the head of pancreas. Clamping of the GDA resulted in reduced pulsation in the common hepatic artery, although the liver still appeared viable. Since it was impossible to preserve the GDA, en bloc resection of tumour with the GDA was carried out. Postoperatively the patient developed a transient rise in alanine transaminase (ALT), peaking at 834 IU/L on the second postoperative day. On the sixth postoperative day, the patient became profoundly acidotic with septic shock, and underwent an emergency laparotomy. The stomach was found to be necrotic with complete disintegration of the lesser curve, close to the gastro-oesophageal junction. In addition, there was dehiscence of the pyloro-jejunostomy anastomosis. The spleen was viable with no sign of ischaemia. A total gastrectomy was performed with a Roux-en-Y reconstruction. His postoperative recovery was complicated by the development of a late enterocutaneous fistula from the oesophago-jejunostomy. Four weeks later he collapsed and passed malaena. Angiography showed complete absence of the coeliac artery (Figure 1). The splenic artery was seen to arise from the SMA as did an aberrant right hepatic artery. He made a slow recovery and was discharged home 4 months after the operation.
Figure 1. .
Postoperative superior mesenteric angiography in case 1 shows contrast in the right hepatic and splenic arteries and these are clearly branches of a common trunk of the SMA.
Case 2
A 57-year-old male underwent pancreaticoduodenectomy for adenocarcinoma of the head of the pancreas. At laparotomy, an aberrant right hepatic artery was found to arise from the SMA and was dissected off the head of the pancreas. Division of the GDA resulted in disappearance of pulse in the left hepatic artery. It was clear that he had a large GDA with retrograde supply from the SMA to the left hepatic and the left gastric arteries. The inferior pancreaticoduodenal arcade below the tumour was dissected clear without compromising the resection margin. After resection of the tumour with the main part of GDA, the inferior pancreaticoduoduodenal artery was re-anastomosed to the stump of the GDA to supply the left hepatic and left gastric arteries. After a standard Kausch-Whipple reconstruction the patient's postoperative recovery was uneventful and he was discharged on the eighth postoperative day.
Discussion
In patients with coeliac artery stenosis or occlusion, division of the GDA during pancreaticoduodenectomy may result in compromised blood supply to the liver, stomach and spleen, leading to visceral ischaemia, infarction or anastomotic leak 1. The incidence of coeliac artery stenosis on angiographic examination is reported to be between 12 and 24% in European series and 2–7% in Asian series 2. Suggested causes of coeliac axis stenosis are atherosclerosis, acute and chronic dissection (during angiography), and compression of the coeliac axis by the median arcuate ligament 3,4,5; the latter has been described as particularly common in the Asian population. Coeliac artery stenosis is usually an innocuous condition as the blood supply to the liver, stomach and spleen may be sustained through well-developed collateral pathways from the SMA, in particular the pancreaticoduodenal arcades and the dorsal pancreatic artery 4. Prevalence of coeliac trunk occlusion is estimated at 2–4% of all pancreatoduodenectomies 3,5,6,7. The diagnosis of coeliac artery occlusive disease can usually be made preoperatively if sagittally reformatted, spiral CT imaging or mesenteric angiography is carried out. If these techniques are not performed preoperatively, a test occlusion of the GDA during pancreatoduodenectomy is recommended to identify this problem 8, although a false-negative test may occur 1,9.
Postoperative complications following pancreaticoduodenectomy associated with coeliac artery stenosis are rarely reported in the literature. At the National Cancer Centre Hospital in Tokyo, Nara et al. reported two cases of hepatic abscesses in seven patients with coeliac artery stenosis 3, which developed at postoperative days 30 and 62, respectively, following pancreaticoduodenectomy. In a multicentre survey carried out in Switzerland, 5 of 22 patients with coeliac artery stenosis who underwent pancreaticoduodenectomy developed complications (morbidity = 23%) associated with the coeliac artery stenosis, with 2 fatalities (mortality = 9%) 7. Anastomotic leaks from the hepaticojejunal and gastrojejunal anastomoses could arise as a result of compromised vascular supply in patients with coeliac artery occlusion, and the aetiology of this complication is rarely appreciated and reported in the literature.
In some patients, the median arcuate ligament compresses the coeliac artery and dissection to release this ligament often results in restoration of flow within the coeliac artery, with success rates varying from 29% to 71% 3,5,6. Otherwise, dissection to preserve the collateral arcades from the SMA may be carried out in patients with uninvolved vessels 8,10. Often, this is not possible and resection of the collateral arcades is necessary to remove the tumour. In such cases, vascular reconstruction with autologous vein graft should be carried out, either between the splenic artery and iliac artery 11 or between the aorta and common hepatic artery 12.
In the present series, we report two cases of coeliac artery occlusion encountered during pancreaticoduodenectomy. In case 1, clamping of the GDA resulted in reduced pulsation in the hepatic artery. Neither the stomach nor the liver showed any sign of ischaemia at surgery. As the liver has a dual blood supply from the hepatic artery and portal vein, ligation of the hepatic artery usually carries no clinical consequences. We did not dissect the common hepatic artery to its origin to the coeliac trunk, nor did we attempt to dissect out the left gastric artery. Total gastric necrosis after pancreaticoduodenectomy is an unreported complication. The stomach is normally easily sustained by the left gastric artery and the short gastrics after division of the gastric vessels near the pyloro-duodenal junction. In both patients, the blood supply to the upper abdominal viscera was derived by retrograde flow from the SMA via the GDA–pancreaticoduodenal arcades. In case 1 the postoperative mesenteric angiogram (Figure 1) showed no evidence of a coeliac artery, and the blood supply to the right liver and spleen was derived from vessels from the SMA. It seems likely this patient either had complete coeliac occlusion, or alternatively, absence of the coeliac artery. In case 2, division of the GDA resulted in marked decrease in blood supply to the liver and in the light of previous experience, the GDA was revascularized from the inferior pancreatoduodenal artery. In both cases, preoperative arterial imaging, either mesenteric angiography or CT-reformatted arteriography, would have been useful in delineating the anatomy. It can be difficult to delineate the vascular anatomy during the operation because of distortion due to the tumour. We recommend CT-reformatted angiography as part of the routine work-up. If preoperative vascular imaging is unavailable and coeliac artery stenosis is suspected intraoperatively, Doppler ultrasonography may show a decrease in hepatic arterial signals after the GDA is clamped. In such patients, Nara et al. recommended arterial reconstruction of the hepatic artery to minimize the risk of liver ischaemia 3.
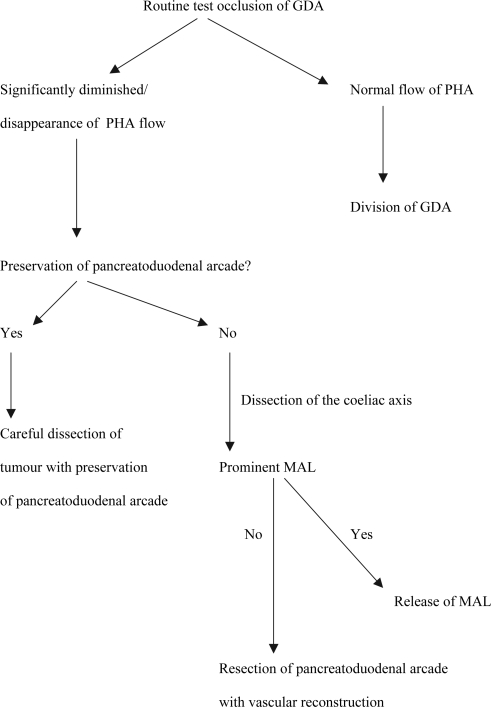
Based on our experience and review of the literature, a management algorithm (Figure 2) for coeliac artery stenosis (or absence) encountered during pancreaticoduodenectomy is proposed. A test occlusion of the GDA should be carried out before division of this vessel. If a significant decrease in blood flow to the liver is encountered (loss of pulsation or Doppler signals), the common hepatic artery should be traced to the origin of coeliac artery. If a prominent median arcuate ligament is found compressing on the coeliac axis, then division of this structure may restore blood supply to the coeliac artery. Otherwise, preservation of the GDA–pancreaticoduodenal arcade or arterial reconstruction using direct anastomosis or autologous vein graft should be carried out to restore flow from the SMA.
Figure 2. .
Management algorithm for patients with coeliac artery stenosis during pancreaticoduodenectomy. GDA, gastroduodenal artery; PHA, proper hepatic artery; MAL, median arcuate ligament.
Acknowledgements and disclosures
There are no disclosures.
References
- 1.Portolani N, Tiberio GA, Coniglio A, Baiocchi G, Vettoretto N, Giulini SM. Emergency celiac revascularisation for supramesocolic ischaemia during pancreaticoduodenectomy: report of a case. Surg Today. 2004;34:616–18. doi: 10.1007/s00595-004-2755-z. [DOI] [PubMed] [Google Scholar]
- 2.Kwon JW, Chung JW, Song SY, Lim HG, Myung JS, Choi YH, et al. Transcatheter arterial chemoembolization for hepatocellular carcinomas in patients with coeliac axis occlusion. J Vasc Interv Radiol. 2002;13:689–94. doi: 10.1016/s1051-0443(07)61845-4. [DOI] [PubMed] [Google Scholar]
- 3.Nara S, Sakamoto Y, Shimada K, Sano T, Kosuge T, Takahashi Y, et al. Arterial reconstruction during pancreatoduodenectomy in patients with coeliac axis stenosis – utility of Doppler ultrasonography. World J Surg. 2005;29:885–9. doi: 10.1007/s00268-005-7878-x. [DOI] [PubMed] [Google Scholar]
- 4.Song SY, Chung JW, Kwon JW, Joh JH, Shin SJ, Kim HB, et al. Collateral pathways in patients with celiac axis stenosis: angiogragphic-spiral CT correlation. Radiographics. 2002;22:881–93. doi: 10.1148/radiographics.22.4.g02jl13881. [DOI] [PubMed] [Google Scholar]
- 5.Farma JM, Hoffman JP. Nonneoplastic celiac axis occlusion in patients undergoing pancreatico-duodenectomy. Am J Surg. 2007;193:341–4. doi: 10.1016/j.amjsurg.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 6.Kurosaki I, Hatakeyama K, Nihei KE, Oyamatsu M. Celiac axis stenosis in pancreatico-duodenectomy. J Hepatobiliary Pancreat Surg. 2004;11:119–24. doi: 10.1007/s00534-003-0871-6. [DOI] [PubMed] [Google Scholar]
- 7.Berney T, Pretre R, Chassot G, Morel P. Ischaemic risk in the case of celiac trunk occlusion in patients undergoing pancreatico-duodenectomy. Multicentre study and review of literature. Ann Chir. 1999;53:273–9. [PubMed] [Google Scholar]
- 8.Murakami Y, Uemura K, Yokoyama Y, Sasaki M, Morifuji M, Hayashidani Y, et al. Celiac axis occlusion with replaced common hepatic artery and pancreatoduodenectomy. J Gastrointest Surg. 2004;8:520–2. doi: 10.1016/j.gassur.2004.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Machado MA, Herman P, Montagnini AL, Costa ML, Nishinari K, Wolosker N, et al. Hepatogastroenterology. 2004;51:1671–73. [PubMed] [Google Scholar]
- 10.Pelloni A, Gertsch P. [Cephalic duodenopancreatectomy with preservation of pancreaticoduodenal arcades in coeliac trunk occlusion.] Ann Chir 2000;125:660–4(in French). [DOI] [PubMed] [Google Scholar]
- 11.Okamoto H, Suminaga Y, Toyama N, Konishi F, Kawahito H. Autogenous vein graft from iliac artery to splenic artery for celiac occlusion in pancreatico-duodenectomy. J Hepatobiliary Pancreat Surg. 2003;10:109–12. doi: 10.1007/s10534-002-0831-7. [DOI] [PubMed] [Google Scholar]
- 12.Miyata M, Takao T, Okuda A, Sasako Y, Sunada S. Pancreatoduodenectomy for periampullary cancer with celiac occlusion: a case report. Surgery. 1988;103:261–3. [PubMed] [Google Scholar]