Abstract
Background. Caroli's disease (CD) is a benign congenital disorder characterized by segmental cystic dilatation of the intrahepatic biliary ducts. Therapeutic strategy includes medical treatment, percutaneous, endoscopic or surgical drainage of the affected bile ducts, liver resection or transplantation. The aim of this study was to analyse the results and long-term follow-up of a consecutive series of patients who underwent surgical treatment for CD. Patients and methods. Between 1995 and 2005, 10 patients were surgically treated for CD. Variables evaluated were: age, gender, clinical presentation, diagnostic procedures, percutaneous and surgical treatments, histopathological analysis and outcome. Results. The average age of the patients was 45.8 years. Recurrent cholangitis was the main clinical manifestation (70%). In unilateral CD a liver resection was performed in nine patients (left lateral sectionectomy in seven, left hepatectomy in one and right hepatectomy in one). In bilateral disease a cholecystectomy, duct exploration, hepaticojejunostomy and liver biopsy of both lobes were performed. Average follow-up was 60 months. All the patients are alive and free of symptoms without recurrence in the remnant liver. Discussion. Liver resection is the preferred therapeutic option for unilateral CD, demonstrating good results in long-term follow-up. In bilateral disease, hepaticojejunostomy could be considered as an alternative or a previous step to liver transplantation, which still remains the ultimate option.
Keywords: liver surgery, Caroli's disease, Caroli's syndrome, bile duct cyst type V
Introduction
Caroli's disease (CD) is a benign congenital disorder, characterized by unilobar or bilobar segmental cystic dilatation of the intrahepatic biliary tract. It corresponds to type V choledochal cyst as classified by Todani et al. 1. The first report was by Todd in 1818 but Jaques Caroli in 1958 defined the disease precisely with its different types 2,3,4. Autosomal recessively inherited in most cases, the pathogenesis of the dilatation in the intrahepatic biliary tree is considered to be due to a lack of normal involution of the ductal plate 5. Two different kinds of disease are described: a simple one (CD) and a complex type associated with congenital hepatic fibrosis (Caroli's syndrome, CS) 6,7,8.
Clinical symptoms of CD include recurrent cholangitis, right upper quadrant abdominal pain and jaundice, development of stones and liver abscess, usually followed by a progressive loss of quality of life and death due to uncontrolled sepsis 9. In CS, portal hypertension and hepatic fibrosis are responsible for the clinical manifestations. Various renal disorders have been described in association with these liver diseases, including autosomal polycystic kidney disease, medullary sponge kidney and medullary cystic disease 10.
Ultrasound, computed tomography (CT) scan, percutaneous transhepatic cholangiography, endoscopic cholangiopancreatography (ERCP) and magnetic resonance cholangiopancreatography (MRCP) are performed to establish the diagnosis 11,12,13.
Treatment of CD depends on the localization and extension of the disease. Endoscopic, percutaneous or surgical drainage of the bile ducts, liver resection and orthotopic liver transplantation (OLT) appear to be different options for the treatment of patients with symptomatic CD 14,16,17.
The aim of this retrospective study was to analyse the clinical features of the disease and the results of surgical treatment in 10 adult patients with CD treated at the Liver Transplantation and Surgical Divisions of the Hospital Dr C. Argerich, Buenos Aires and Hospital Italiano of La Plata, Argentina.
Patients and methods
The case notes of 10 patients treated at Hospital Dr Cosme Argerich and Hospital Italiano of La Plata with a diagnosis of CD, between October 1995 and December 2005, were reviewed retrospectively. Patients were selected from the Liver Transplantation and Surgical Division prospective computerized database and were verified using records of each patient. Data covering demographic features, clinical symptoms, biochemical and radiologic examinations, prior therapeutic interventions, surgical procedure, complications, duration of hospital stay and long-term outcome were analysed. Histopathological analysis was performed in all patients. Diagnosis of cholangitis was based on the presence of intermittent right upper quadrant pain, intermittent fever, transient jaundice and increased biochemical markers. Postoperative follow-up consisted of laboratory tests, CA 19-9 levels and ultrasound, performed every 3 months during the first year and then every 6 months.
Results
Seven patients were males. The median age was 45.8 years (range 27–82). Clinical presentation consisted of recurrent cholangitis complicated by intrahepatic calculi in seven patients, recurrent acute pancreatitis in one and abdominal pain in two. Four of the patients had previously undergone an open cholecystectomy for symptomatic gallstones.
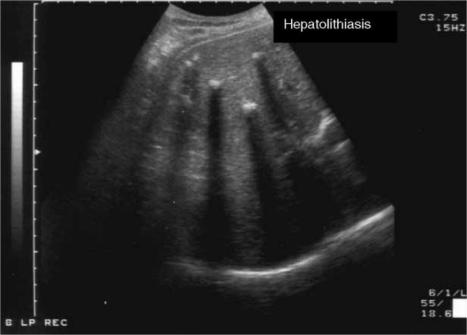
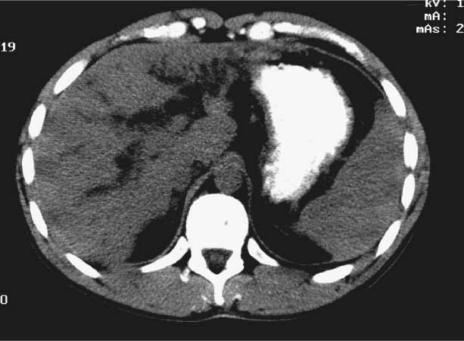
In all patients the diagnosis was established preoperatively by means of an abdominal ultrasound and CT scan that revealed the unilateral or bilateral dilated intrahepatic bile ducts, hepatolithiasis and cystic cavities or abscess (Figures 1 and 2). MRCP and ERCP were carried out in four and three patients, respectively. Owing to recurrent cholangitis, three patients required percutaneous biliary drainage (Figure 3). Nine patients had unilobar disease and one had bilobar compromise. The time range between the onset of symptoms and treatment after diagnosis was 2–60 months. There was no associated polycystic kidney disease or portal hypertension. At resection all patients were free of septic complications.
Figure 1. .
Ultrasound in bilateral Caroli's disease. Multiple stones in dilated intrahepatic bile ducts.
Figure 2. .
CT in bilateral Caroli's disease. Severe dilatation of the bile ducts.
Figure 3. .
Percutaneous transcatheter cholangiography in bilateral Caroli's disease. Dilated bile ducts with stones and abscess.
Surgical technique
Liver resection was performed by standard technique. Intraoperative ultrasound was routinely performed. Intermittent Pringle manoeuvre was only required in one patient. After operation all patients were monitored in the intensive care unit. No patients required blood replacement in the perioperative period. Considering the extent of the disease, the surgical procedures were as follows. (A) Monolobar disease: left lateral sectionectomy in seven patients, left hepatectomy in one and right hepatectomy in another. Additional procedures performed were bile duct exploration with T tube in two patients and biopsy of the remnant liver in four. (B) Bilobar disease: cholecystectomy, intrahepatic bile duct exploration with multiple stone removal, liver biopsy and end-to-side Roux-en-Y hepaticojejunostomy with stent drainage in one patient.
Complications
There were two complications in one patient, a wound dehiscence and an intra-abdominal abscess from the cut surface treated by surgical drainage and repaired by means of a polypropylene mesh. There were no biliary complications. The perioperative mortality rate was 0%.
Pathological analysis
Macroscopically the excised livers presented saccular or fusiform dilatation of segmental or principal bile ducts with visible stones. Histology showed biliary hamartomas, biliary ramifications and periductal granulomatous reaction. There was no patient with congenital hepatic fibrosis (CS) or cirrhosis. Biopsies of the remnant livers showed normal histology. In the case with bilobar compromise, CD characteristics and moderate fibrosis were demonstrated.
Follow-up
Median follow-up was 60 months (range 12–148). All patients are alive, free of symptoms. No patient had recurrence of CD. The patient with hepaticojejunostomy presented laboratory tests, CA 19-9, ultrasound and cholangioMRCP in the normal range at 63 months. A control liver biopsy demonstrated no changes in the degree of fibrosis from the time of surgery.
Discussion
CD, a congenital disorder of the intrahepatic bile ducts due to a ductal plate malformation, integrates the ‘fibrocystic’ group, characterized by a variable degree of fibrosis and ectasia 5. The level of the intrahepatic biliary tree affected by the ductal plate malformation is in relation with the pathogenesis of different kind of diseases. In CD, the large and proximal intrahepatic bile ducts are affected, in CS and congenital hepatic fibrosis the smaller ones and in polycystic liver disease and von Meyenburg complexes the more peripheral interlobular ducts 5,18. The finding of an unbalanced translocation between chromosomes 3 and 8 suggests that loss of distal 3p and/or gain of 8q is of importance in the pathogenesis of CD 19. It is an autosomal recessive disease and is associated with polycystic kidney disease and hepatic fibrosis 20. It corresponds to the type V bile duct cyst as incorporated by Todani et al. in Alonso-Lej et al. classification 1,21,22. Considered a quite rare entity, with 150 cases reported in the literature, several series include not only patients with CD but also with CS 10,14,17,23. Our population consisted only of patients with CD and the average duration of symptoms was in accordance with other reports 6,14.
Bacterial cholangitis is the most frequent presentation and life-threatening complication of CD 4,8,12,24. Usually caused by Gram-negative bacilli, it has a recurrent course and despite different antibiotic associations the medical treatment is often not satisfactory. It is documented by the presence of stone obstruction with bile stasis, dilated biliary ducts containing purulent material and mixed bacterial infections 25. Cholangitis may appear spontaneously but can also appear following invasive diagnostic and therapeutic procedures. In the present study three patients required percutaneous biliary drainage before definitive treatments. Acute pancreatitis was also reported by other authors 26,27. In a multi-institutional study from Argentina, acute pancreatitis was found in 6% of patients with hepatolithiasis and Pimentel et al. reported it in 23% of 26 patients with CD 24.
Although ultrasound and CT are widely used to investigate patients with CD, MRCP presents advantages to depict the entire biliary tree 13,28. Guy et al. identified three main patterns of CD in MRCP: (a) multiple cystic ectasias connected with fusiform dilatations, (b) isolated fusiform dilatations with multiple calculi and (c) solitary dilatation of the left bile ducts with cysts and multiple calculi 29. Treatment of CD depends on the clinical features and localization of the biliary abnormality.
When the disease is localized to one hepatic lobe, most commonly the left, hepatectomy or sectionectomy must be indicated 6,8. Symptomatic relief after partial hepatectomy was complete and permanent in 100% of patients in this series. Ulrich et al. have treated 39 patients with CD in a 12-year period. In 32 of them, they performed the same resective procedure 17. Gillet et al. showed that in patients with unilateral CD, numerous interventional procedures (endoscopic, percutaneous or surgical) were performed before a definitive treatment 6.
Dysplasia of the biliary epithelium generated by bile stasis and chronic inflammation can develop a malignant transformation to cholangiocellular carcinoma in 5–14% of patients with CD 11,30,31. A higher incidence is reported in unilateral cases 6,30.
In reference to the bilateral CD we present a 33-year-old man treated by Roux-en-Y hepaticojejunostomy. Bilio-digestive anastomosis after thorough cleaning of the biliary tree is an option and has been advocated by different authors as a first stage in CD with bilateral involvement 4,8,12,14,17,22. OLT has been suggested as a possible therapeutic approach, principally in patients with CS associated with portal hypertension and in cases with recurrent cholangitis due to bilateral disease when other medical treatments have been ineffective 10,16,25,32. It avoids the development of cholangiocarcinoma that with the exception of study protocols is considered a contraindication to transplantation 25,33. However, in the UNOS Database in a 17-year period (1988–2005) only 95 patients were transplanted for CD and CS. Concerns around OLT in this disease are the choice of the appropriate time for transplant and the problem of exposing young healthy individuals to the risks and consequences of the transplant and immunosuppression itself. In our study follow-up, the patient with bilateral disease showed normal liver function and non-progressive fibrosis at 63 months. Medical treatment with ursodeoxycholic acid could be useful in patients with bilateral CD, as was demonstrated by Ros et al. with a total and partial stone dissolution of 15% and 45%, respectively 34.
In conclusion, our results demonstrate that surgical resection is the best curative option for patients with unilateral symptomatic CD. Left lateral sectionectomy was the most common resection in this series. In bilateral disease hepaticojejunostomy could be an optional treatment that offers long-term survival and avoids liver transplantation in early stages.
Acknowledgements and disclosures
No disclosures.
References
- 1.Todani T, Watanabe Y, Narusue M, Tabuchi K, Okajima K. Congenital bile duct cysts: Classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263–9. doi: 10.1016/0002-9610(77)90359-2. [DOI] [PubMed] [Google Scholar]
- 2.Caroli J, Soupault R, Kossakowski J, Plocker L, Paradowska [Congenital polycystic dilation of the intrahepatic bile ducts; attempt at classification] Sem Hop. 1958;34:488–95/SP. [PubMed] [Google Scholar]
- 3.Caroli J, Couinaud C, Soupault R, Porcher P, Eteve J. [A new disease, undoubtedly congenital, of the bile ducts: unilobar cystic dilation of the hepatic ducts] Sem Hop. 1958;34:496–502/SP. [PubMed] [Google Scholar]
- 4.Madjov R, Chervenkov P, Madjova V, Balev B. Caroli's disease. Report of 5 cases and review of literature. Hepatogastroenterology. 2005;52:606–9. [PubMed] [Google Scholar]
- 5.Desmet VJ. Ludwig symposium on biliary disorders – part I. Pathogenesis of ductal plate abnormalities. Mayo Clin Proc. 1998;73:80–9. doi: 10.4065/73.1.80. [DOI] [PubMed] [Google Scholar]
- 6.Gillet M, Favre S, Fontolliet C, Halkic N, Mantion G, Heyd B. [Monolobar Caroli's disease. Apropos of 12 cases] Chirurgie. 1999;124:13–18. doi: 10.1016/s0001-4001(99)80037-3. [DOI] [PubMed] [Google Scholar]
- 7.Harjai MM, Bal RK. Caroli syndrome. Pediatr Surg Int. 2000;16:431–2. doi: 10.1007/s003839900323. [DOI] [PubMed] [Google Scholar]
- 8.Kassahun WT, Kahn T, Wittekind C, Mossner J, Caca K, Hauss J, et al. Caroli's disease: liver resection and liver transplantation. Experience in 33 patients. Surgery. 2005;138:888–98. doi: 10.1016/j.surg.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 9.Knoop M, Keck H, Langrehr JM, Peter FJ, Ferslev B, Neuhaus P. [Therapy of unilobar Caroli syndrome by liver resection] Chirurg. 1994;65:861–6. [PubMed] [Google Scholar]
- 10.Levy AD, Rohrmann CA, Jr, Murakata LA, Lonergan GJ. Caroli's disease: radiologic spectrum with pathologic correlation. AJR Am J Roentgenol. 2002;179:1053–7. doi: 10.2214/ajr.179.4.1791053. [DOI] [PubMed] [Google Scholar]
- 11.Balsells J, Margarit C, Murio E, Lazaro JL, Charco R, Vidal MT, et al. Adenocarcinoma in Caroli's disease treated by liver transplantation. HPB Surg. 1993;7:81–6. doi: 10.1155/1993/61048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Benhidjeb T, Muller JM, Gellert K, Zanow J, Rudolph B. [Current therapy of bile duct cysts. II. Intrahepatic cysts (Caroli syndrome)] Chirurg. 1996;67:238–43. [PubMed] [Google Scholar]
- 13.Lopez CA, Munoz BA, Herrera MD, Moreno SO, Flores MM, Perez JJ. [Diagnosis of Caroli's disease with conventional ultrasonography and echo-Doppler] Rev Esp Enferm Dig. 1994;85:387–9. [PubMed] [Google Scholar]
- 14.Dagli U, Atalay F, Sasmaz N, Bostanoglu S, Temucin G, Sahin B. Caroli's disease: 1977–1995 experiences. Eur J Gastroenterol Hepatol. 1998;10:109–12. [PubMed] [Google Scholar]
- 16.Waechter FL, Sampaio JA, Pinto RD, vares-da-Silva MR, Cardoso FG, Francisconi C, et al. The role of liver transplantation in patients with Caroli's disease. Hepatogastroenterology. 2001;48:672–4. [PubMed] [Google Scholar]
- 17.Ulrich F, Steinmuller T, Settmacher U, Muller AR, Jonas S, Tullius SG, et al. Therapy of Caroli's disease by orthotopic liver transplantation. Transplant Proc. 2002;34:2279–80. doi: 10.1016/s0041-1345(02)03235-9. [DOI] [PubMed] [Google Scholar]
- 18.Sato Y, Harada K, Kizawa K, Sanzen T, Furubo S, Yasoshima M, et al. Activation of the MEK5/ERK5 cascade is responsible for biliary dysgenesis in a rat model of Caroli's disease. Am J Pathol. 2005;166:49–60. doi: 10.1016/S0002-9440(10)62231-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Parada LA, Hallen M, Hagerstrand I, Tranberg KG, Johansson B. Clonal chromosomal abnormalities in congenital bile duct dilatation (Caroli's disease) Gut. 1999;45:780–2. doi: 10.1136/gut.45.5.780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Taylor AC, Palmer KR. Caroli's disease. Eur J Gastroenterol Hepatol. 1998;10:105–8. doi: 10.1097/00042737-199802000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Nicholl M, Pitt HA, Wolf P, Cooney J, Kalayoglu M, Shilyansky J, et al. Choledochal cysts in western adults: complexities compared to children. J Gastrointest Surg. 2004;8:245–52. doi: 10.1016/j.gassur.2003.12.013. [DOI] [PubMed] [Google Scholar]
- 22.Soreide K, Korner H, Havnen J, Soreide JA. Bile duct cysts in adults. Br J Surg. 2004;91:1538–48. doi: 10.1002/bjs.4815. [DOI] [PubMed] [Google Scholar]
- 23.Ammori BJ, Jenkins BL, Lim PC, Prasad KR, Pollard SG, Lodge JP. Surgical strategy for cystic diseases of the liver in a western hepatobiliary center. World J Surg. 2002;26:462–9. doi: 10.1007/s00268-001-0250-x. [DOI] [PubMed] [Google Scholar]
- 24.Pimentel FM. Enfermedad de Caroli. Rev Chilena de Cirugia. 2004;56:426–33. [Google Scholar]
- 25.Sans M, Rimola A, Navasa M, Grande L, Garcia-Valdecasas JC, Andreu H, et al. Liver transplantation in patients with Caroli's disease and recurrent cholangitis. Transpl Int. 1997;10:241–4. doi: 10.1007/s001470050050. [DOI] [PubMed] [Google Scholar]
- 26.Espinoza R, San MS, Court F, Vera E, Ferreira R, Croxatto H. [Hepatic resection in localized Caroli disease] Rev Med Chil. 2003;131:183–9. [PubMed] [Google Scholar]
- 27.Garcia VR, Diaz BJ, Moreno Monteagudo JA, Correa JA, Garcia Buey ML, Pajares Garcia JM. [Acute pancreatitis in Caroli's syndrome] Rev Esp Enferm Dig. 1997;89:133–6. [PubMed] [Google Scholar]
- 28.Asselah T, Ernst O, Sergent G, L'hermine C, Paris JC. Caroli's disease: a magnetic resonance cholangiopancreatography diagnosis. Am J Gastroenterol. 1998;93:109–10. doi: 10.1111/j.1572-0241.1998.109_c.x. [DOI] [PubMed] [Google Scholar]
- 29.Guy F, Cognet F, Dranssart M, Cercueil JP, Conciatori L, Krause D. Caroli's disease: magnetic resonance imaging features. Eur Radiol. 2002;12:2730–6. doi: 10.1007/s00330-002-1471-6. [DOI] [PubMed] [Google Scholar]
- 30.Abdalla EK, Forsmark CE, Lauwers GY, Vauthey JN. Monolobar Caroli's disease and cholangiocarcinoma. HPB Surg. 1999;11:271–6. doi: 10.1155/1999/70985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Totkas S, Hohenberger P. Cholangiocellular carcinoma associated with segmental Caroli's disease. Eur J Surg Oncol. 2000;26:520–1. doi: 10.1053/ejso.1999.0936. [DOI] [PubMed] [Google Scholar]
- 32.Schiano TD, Fiel MI, Miller CM, Bodenheimer HC, Jr, Min AD. Adult presentation of Caroli's syndrome treated with orthotopic liver transplantation. Am J Gastroenterol. 1997;92:1938–940. [PubMed] [Google Scholar]
- 33.Takatsuki M, Uemoto S, Inomata Y, Egawa H, Kiuchi T, Hayashi M, et al. Living-donor liver transplantation for Caroli's disease with intrahepatic adenocarcinoma. J Hepatobiliary Pancreat Surg. 2001;8:284–6. doi: 10.1007/s005340170030. [DOI] [PubMed] [Google Scholar]
- 34.Ros E, Navarro S, Bru C, Gilabert R, Bianchi L, Bruguera M. Ursodeoxycholic acid treatment of primary hepatolithiasis in Caroli's syndrome. Lancet. 1993;342:404–6. doi: 10.1016/0140-6736(93)92817-d. [DOI] [PubMed] [Google Scholar]