Abstract
The present investigation evaluated a moderational role of anxiety sensitivity (fear of anxiety and anxiety-related states; McNally, 2002) in the relation between smoking status and anxiety/depressive symptoms in a Russian epidemiological sample (n = 390; 197 females, Mean age = 43.55). Consistent with prediction, anxiety sensitivity moderated the association of smoking status with indices of anxiety and depressive symptoms; the effects were evident after controlling for the variance accounted for by alcohol use problems, environmental stress (past month), and gender. These findings are discussed with regard to the role of anxiety sensitivity in etiologic connection between smoking and panic-related processes.
Keywords: Smoking, Panic, Anxiety, Comorbidity, Anxiety Sensitivity, Depression
Research has increasingly highlighted clinically significant relations between smoking and anxiety symptoms (e.g., intensity of anxiety symptoms) and certain disorders (McCabe et al., 2004). Of the anxiety disorders, there appears to be a notable association between smoking and panic attacks, panic disorder, and agoraphobia (see Zvolensky & Bernstein, 2005; Zvolensky, Feldner et al., 2005, for reviews). For instance, epidemiological (Lasser et al., 2000), community (Hayward et al., 1989), and clinical (Baker-Morissette et al., in press; Himle et al., 1988; Pohl et al., 1992) studies have found that smoking is more common among those with panic-related problems (i.e., panic attacks, panic disorder, and agoraphobia) compared to those without such problems. Other work has found that smoking increases the risk for developing panic attacks and panic disorder in the future (Breslau & Klein, 1999; Breslau et al., 2004; Johnson et al., 2000; Isensee et al., 2003) and may exacerbate (concurrently) the severity of such anxiety problems (McLeish et al., 2006; Zvolensky, Forsyth et al., 2002; Zvolensky, Kotov et al., 2003; Zvolensky, Leen-Feldner et al., 2004; Zvolensky, Schmidt, & McCreary, 2003)
Although promising, considerably less is known as to whether other panic-related risk factors may influence the relation between smoking and panic processes (i.e., moderational effects; Ising, 2006). In a moderational model, the association between smoking and panic is dependent on another risk factor (Baron & Kenny, 1986). An important variable relevant to the etiology of panic psychopathology is anxiety sensitivity (AS), a cognitive-based risk factor for anxiety psychopathology defined as the fear of anxiety and anxiety-related sensations (McNally, 2002; Reiss & McNally, 1985). Specifically, AS is a trait-like cognitive characteristic that can predispose individuals to the development of anxiety-related problems. Available data are generally consistent with the AS model of panic vulnerability (Hayward et al., 2000; Maller & Reiss, 1992; Schmidt et al., 1997, 1999; Schmidt et al., in press; Weems et al., 2002; Zvolensky & Forsyth, 2002).
Models of smoking-panic comorbidity predict that these two vulnerabilities should interplay in a clinically meaningful manner (Zvolensky & Bernstein, 2005; Zvolensky, Schmidt, & Stewart, 2003). Specifically, it is theoretically predicted that AS may enhance the association between smoking and panic-related problems. High AS smokers compared to nonsmokers would theoretically be more apt to perceive internal withdrawal symptoms as aversive with greater frequency and perhaps other aspects of smoking (e.g., health impairment) and therefore have a greater opportunity to learn that internal cues are emotionally distressing. In the absence of more adaptive methods for coping with such internal stressors, high AS smokers may thus be more apt to experience greater degrees of anxiety symptoms and learn to cognitively respond to such sensations in a maladaptive manner. Such emotionally distressing events may trigger efforts to cope with the stressors by smoking, a perspective supported by research on AS and coping motives (Comeau et al., 2001; Novak et al., 2003; Stewart et al., 1997; Zvolensky, Bonn-Miller et al., 2006) as well as outcome expectancies (Zvolensky, Feldner et al., 2004).
Here, it is noteworthy that high AS smokers are often interested in quitting (Zvolensky, Baker et al., 2004), yet more apt to fail in their attempts to quit (Brown et al., 2001; Zvolensky, Bernstein et al., in press; Zvolensky, Bonn-Miller et al., in press). Moreover, past work has indicated an association between AS and depressed affect (Cox et al., 1999; Otto et al., 1995; Schmidt et al., 1998). Ultimately, if such persons did not successfully quit smoking, theoretical models suggest that they could place themselves at risk for depressed affect by virtue of the continued struggle with forward-feed cycle of emotional distress, and smoking-oriented coping to regulate such affect (Zvolensky, Bernstein, Yartz et al., in press). That is, they may be more apt to experience depressive symptoms secondary to their inability to quit smoking despite frequent attempts to do so; a position supported by clinical case reports (Beckham et al., 2006; Zvolensky, Lejuez et al., 2003). This type of model predicts that an AS by smoking status relation would be applicable to anxiety, panic, and depressive symptoms, but not negative affect more generally (Zvolensky & Bernstein, 2005).
The above AS-smoking model indicates a moderating role of this cognitive factor (AS) for the association between smoking and panic symptoms and related affect processes. Empirical data, although highly limited, is consistent with such perspective. For example, one study found an interaction between smoking status and AS among adolescents within a biological challenge paradigm (Leen-Feldner, Zvolensky et al., in press). Specifically, the combination of high levels of AS and being a current smoker compared to a non-smoker (i.e., between group test) predicted greater self-reported panic symptoms in response to a voluntary hyperventilation procedure among this sample of youth (Leen-Feldner, Zvolensky et al., in press). No effects were evident for psychophysiological indices of responsivity.
Though AS-smoking findings are promising, extant research is limited in three notable respects. First, it is unclear whether the moderator model is valid in adulthood. Extending past work is therefore important to enhance generalizability of past findings to an adult stage of the lifespan. This type of work will be most informative when it employs representative sampling methods. Second, previous work has not explored whether the AS by smoking interaction contributes to anxiety above and beyond other theoretically-relevant factors related to both anxiety-related symptoms and smoking. For example, alcohol use problems, life stress, and gender are related to panic psychopathology, AS, and smoking status (Barlow, 2002; Taylor, 1999). Thus, there is a need for a more sophisticated test of the AS-smoking model to account for these factors. To the extent the AS-smoking interaction is apparent above these other variables, further confidence in this effect would be established. Third, the previous investigation focused on youth from the United States (U.S.). Replication of these findings in a country outside of the U.S. would significantly strengthen confidence in the theorized vulnerability model, and moreover, facilitate understanding of cultural influences on AS-smoking processes. Russia is one country whereby such work can be usefully extended, as AS has been successfully studied in this country with conceptual equivalence to work in the U.S. (Kotov et al., 2005). And finally, the AS-smoking model suggests that an interactive effect may be apparent between these factors for depressive as well as panic symptoms (Zvolensky & Bernstein, 2005). Past work has not conducted analyses focused on a wider range of affect symptoms than panic symptoms. As such, future work would benefit by exploring the AS-smoking model in relation to panic as well as depressive symptoms.
Together, the overarching aim of the present investigation was to test a clinically-relevant theoretical prediction derived from a smoking-panic model among adults (Zvolensky & Bernstein, 2005). The core objective was to replicate and uniquely extend extant research on the AS-smoking status interactive association completed in adolescents from the U.S. Participants in the present study were a large representative sample of the adult population from Moscow, Russia (n = 390). It was hypothesized that, after accounting for the theoretically-relevant variables of gender, alcohol use problems, and life stress, AS status would moderate the relation between smoking status and anxiety symptoms and panic-related catastrophic thinking about bodily events. Specifically, it was expected that high AS smokers, relative to all other variable combinations, would report the highest levels of anxiety symptoms and panic-relevant catastrophic thinking. This hypothesis was driven by panic-smoking conceptual models (Zvolensky & Bernstein, 2005) and empirical evidence among youth (Leen-Feldner, Zvolensky et al., in press) linking AS and smoking to panic. Additionally, it was hypothesized that smoking status would interact with anxiety sensitivity to account for depressive symptoms. To the extent that high AS smokers struggle with a continued cycle of anxiety-related symptoms and smoking to cope with such distress (Zvolensky, Feldner et al., 2004), they should be more apt to experience greater degrees of depressed affect. Finally, as a test of model’s specificity, no interactive effect was hypothesized for general negative emotional symptoms. According to extant smoking-panic theory (Zvolensky & Bernstein, 2005), the interactive AS by smoking status model should be relatively specific to anxiety and depressive states rather than general negative mood.
Materials and Methods
Participants
The sample was drawn from the population of adult residents of Moscow. Participants were recruited during the spring and summer of 2002 using a geographic sampling method (see Zvolensky, Kotov et al., 2005), for a complete description). The final sample consisted of 390 participants, and was matched to the census on age and income with no more than one percentage point difference for each demographic category. We were not able to match the sample perfectly on education and somewhat over-sampled individuals with college education. Twenty-four percent of the total sample (n = 95) reported being current smokers (simply endorsing current smoking status); a rate generally in accord with smoking rates reported elsewhere (CDC, 1999). The smokers in the present study smoked a mean of 15.6 (SD = 6.1) cigarettes per day, smoked tobacco for the first time at age of 14.0 (SD = 4.3), and started smoking regularly, which was defined as smoking at least once a week for at least two months in a row, at age of 19.4 (SD = 5.2). On average, they smoked a total of 21.5 (SD = 13.1) years in their life. Overall, the participants in this study were 50.5% female, 61.8% college educated and had an average age of 43.55 years (SD = 16.4 years); a full range of incomes was represented.
Measures
Assessment adaptation procedures. All measures were adapted using a multistage procedure in accordance with contemporary standards for instrument translation. This adaptation process is fully explained in a separate report (see Kotov et al., 2005, for details).
Smoking. Participants who were smokers completed a modified form of the CDC (1999) smoking history assessment, which indexed a wide variety of smoking history characteristics (e.g., number of cigarettes per day).
The Anxiety Sensitivity Index (ASI) is a 16-item questionnaire in which respondents indicate on a five-point Likert-type scale (0 = very little to 4 = very much) the degree to which they fear the negative consequences of anxiety symptoms (Reiss et al., 1986). The ASI has three lower-order factors that all load on a single higher-order factor across diverse populations (Zinbarg et al., 1997). The lower-order factors represent Physical, Psychological, and Social Concerns, and the higher-order factor represents the Global AS construct. In the present investigation, we utilized the total ASI score, as it represents the global-order AS factor and therefore takes into consideration different types of fears, including fears of panic-related somatic, cognitive, and social cues. The ASI has demonstrated good internal consistency across diverse populations (Peterson & Reiss, 1992), including Russians (Kotov et al., 2005); the measure was similarly reliable in the present investigation, with a coefficient alpha of .88.
The Mood and Anxiety Symptom Questionnaire (MASQ) is a comprehensive measure of anxiety and depressive symptoms (Watson et al., 1995). The MASQ shows excellent convergence with other measures of anxiety and depression (Watson et al., 1995). In this study, we only used the Anxious Arousal and Anhedonic Depressive scales of the MASQ (MASQ-AA and MASQ-AD), which measures presence of “pure” anxiety symptoms and depressive symptoms, respectively, during the past week. The Russian MASQ was reliable, with the coefficient alpha of .85 for MASQ-AA and .90 for MASQ-AD.
The Agoraphobic Cognitions Questionnaire (ACQ) asks participants to rate the frequency of 14 maladaptive thoughts about anxiety and panic attack symptoms (Chambless et al., 1984). There are items regarding both social/behavioral concerns and physiological concerns. Scores on the ACQ can be computed by using a total score or two separate scores for the social/behavior and physiological components. The ACQ has good internal consistency, test-retest reliability, and convergent validity with other established measures (Arrindell, 1993; Warren et al., 1990; Warren et al., 1989; Yartz et al., 2005). Existing research indicates that in Russian samples the ACQ shows high convergence with measures of anxiety and is clearly distinct from indexes of AS (Zvolensky, Kotov et al., 2005); thus, we utilized the ACQ total score as a global index of cognitive symptoms of anxiety. It was internally consistent in the present sample (coefficient alpha = .85).
The Positive Affect Negative Affect Schedule (PANAS) is a mood measure commonly used in psychopathology research (Watson et al., 1988). It assesses two global dimensions of affect: negative and positive. Only the negative affect scale (PANAS-NA) was used in this study, as a measure of subjective distress (past week). A large body of literature supports validity of the PANAS (Watson, 2000). The Russian version of this scale was reliable (coefficient alpha = .89).
Alcohol Use Disorders Identification Test (AUDIT) is a widely used measure for the detection of alcohol problems. The AUDIT was constructed by World Health Organization investigators specifically for international use (Babor et al., 1992). There is an impressive body of evidence affirming validity and utility of the AUDIT (e.g., Saunders et al., 1993). The reliability of the scale in this study was excellent (coefficient alpha = .93).
The Index of Environmental Stress (IES) asks a participant to indicate whether during the past month he or she has been exposed to each of 20 aversive conditions listed in the index. The IES is based on a validated measure of perceived life strain developed by American and Ukrainian scientists to study psychological consequences of the Chernobyl nuclear plant explosion (Adams et al. 2002). The IES assesses perceived exposure to a variety of aversive conditions, including a lack of basic necessities (e.g. “you lack necessary medical help”), financial hardship (e.g. “you do not have enough money to buy everything necessary for your family”), sense of insecurity (e.g. “you are very afraid of a terrorist attack”), social stressors (e.g. “you are separated with your children”), and strenuous conditions in the family environment (e.g. “almost everyday you have to take care of your elderly parents or sick family member”).
Results
Zero-Order Correlations for Theoretically-Relevant Variables
Zero-order correlations were first computed to examine relations between predictor and criterion variables. Smoking status was significantly associated with agoraphobic cognitions; there was no association between smoking status and anxious arousal as well as anhedonic depressive symptoms, and negative affect. The ASI total score was not significantly associated with anhedonic depressive symptoms, but was associated with agoraphobic cognitions, anxious arousal, and negative affect, even when a conservative alpha level was set (p < .01). Table 1 provides the zero-order correlational matrix and descriptive data for all theoretically relevant variables. There was no association between ASI total score and smoking status.
Table 1.
Descriptive Data and Zero-order Relations among Theoretically-Relevant Variables
| Gender | IES | AUDIT | Smoke | ASI | MASQ-AA | MASQ-AD | ACQ | PANAS-NA | Mean (SD) | |
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | 1 | .10* | −.32** | −.37** | .04 | .01 | −.01 | .01 | .01 | 49.5% Male |
| IES | 1 | .23** | −01 | .10 | .19** | .44** | .14** | .23** | 3.17 (3.2) | |
| AUDIT | 1 | .25** | .09 | −.01 | .18** | −.02 | .26** | 3.88 (5.5) | ||
| Smoke | 1 | .00 | .09 | .03 | .13** | .02 | 24% Smokers | |||
| ASI | 1 | .43** | .03 | .42** | .52** | 17.34 (11.3) | ||||
| MASQ-AA | 1 | .21** | .74** | .41** | 6.46 (8.0) | |||||
| MASQ-AD | 1 | .01 | .22** | 40.61 (14.6) | ||||||
| ACQ | 1 | .30** | 5.59 (6.4) | |||||||
| PANAS-NA | 1 | 6.41 (6.9) |
Note. * = p < .05; ** = p < .01; Gender: coded as 1 = male, 2=female; IES: The Index of Environmental Stress (Adams et al. 2002); AUDIT: Alcohol Use Disorders Identification Test (Babor et al., 1992); Smoke: Smoking Status, coded as 1 = smoker, 0 = non-smoker; ASI: Anxiety Sensitivity Index – Total Score (Reiss et al., 1986); MASQ-AA: Mood and Anxiety Symptom Questionnaire – Anxious Arousal (Watson et al., 1995); MASQ-AD: Mood and Anxiety Symptom Questionnaire – Anhedonic Depression (Watson et al., 1995); ACQ: Agoraphobic Cognitions Questionnaire (Chambless et al., 1984); PANAS-NA: Positive Affect Negative Affect Schedule – Negative Affect Scale (Watson et al., 1988).
Hierarchical Regression Equations
The main and interactive relationships between AS and smoking status were evaluated in relation to the primary dependent variables using a hierarchical multiple regression procedure (Cohen & Cohen, 1983). Separate models were constructed for predicting anxious arousal, anhedonic depression, agoraphobic cognitions, as well as negative affect. Gender, alcohol use problems (continuous index on the AUDIT), and environmental stress (past month) were entered as covariates at level one in the model to evaluate whether the predictor variables were associated with the dependent variables above and beyond the effects due to gender, alcohol use problems, and environmental stress. At the second level, the main effects for ASI total score and smoking status (smoker/not) were simultaneously entered into the model as a set in order to evaluate the individual variance accounted for by these variables. At the third level, the interaction term between ASI and smoking status was entered into the model.
Results of the four regression analyses are presented in Table 2. For anxious arousal, there was a significant effect for environmental stress, but not gender or alcohol use at the first level of the analysis. After accounting for the variance associated with variables at level 1, there was a significant main effect for both smoking status and AS (see Table 2). Consistent with prediction, there was a significant interaction at the third level in the model.
Table 2.
Smoking Status by Anxiety Sensitivity Predicting Anxiety Symptoms, Depressive Symptoms, Agoraphobic Cognitions, and Negative Affect
| ΔR² | t (each predictor) | β | sr² | p | |
|---|---|---|---|---|---|
| Criterion Variable: Anxiety Symptoms | |||||
| Step 1 | .03 | <.01 | |||
| Gender (1=Male, 2=Female) | −.82 | −.05 | .00 | ns | |
| Alcohol Use (AUDIT) | −1.23 | −.07 | .00 | ns | |
| Index of Environmental Stress (IES) | 3.47 | .19 | .03 | <.01 | |
| Step 2 | .20 | <.01 | |||
| Smoking Status (1=yes, 0=no) | 2.15 | .11 | .01 | <.05 | |
| Anxiety Sensitivity (ASI total score) | 9.37 | .44 | .20 | <.01 | |
| Step 3 | .01 | <.05 | |||
| Smoking Status X Anxiety Sensitivity | 2.38 | .21 | .02 | <.05 | |
| Criterion Variable: Agoraphobic Cognitions | |||||
| Step 1 | 02 | ns | |||
| Gender (1=Male, 2=Female) | −.65 | −.04 | .00 | ns | |
| Alcohol Use (AUDIT) | −1.20 | −.07 | .00 | ns | |
| Index of Environmental Stress (IES) | 2.73 | .15 | .02 | <.01 | |
| Step 2 | .19 | <.01 | |||
| Smoking Status (1=yes, 0=no) | 3.16 | .16 | .03 | <.01 | |
| Anxiety Sensitivity (ASI total score) | 8.87 | .42 | .18 | <.01 | |
| Step 3 | .02 | <.01 | |||
| Smoking Status X Anxiety Sensitivity | 3.02 | .26 | .02 | <.01 | |
| Criterion Variable: Depressive Symptoms | |||||
| Step 1 | .20 | <.01 | |||
| Gender (1=Male, 2=Female) | −.46 | −.02 | .00 | ns | |
| Alcohol Use (AUDIT) | 1.55 | .08 | .01 | ns | |
| Index of Environmental Stress (IES) | 8.51 | .42 | .17 | <.01 | |
| Step 2 | .00 | ns | |||
| Smoking Status (1=yes, 0=no) | −.02 | −.00 | .00 | ns | |
| Anxiety Sensitivity (ASI total score) | −.13 | −.01 | .00 | ns | |
| Step 3 | .01 | <.05 | |||
| Smoking Status X Anxiety Sensitivity | 2.06 | .18 | .01 | <.05 | |
| Criterion Variable: Negative Affect | |||||
| Step 1 | .10 | <.01 | |||
| Gender (1=Male, 2=Female) | 1.52 | .08 | .01 | ns | |
| Alcohol Use (AUDIT) | 4.82 | .26 | .06 | <.01 | |
| Index of Environmental Stress (IES) | 2.66 | .14 | .02 | <.01 | |
| Step 2 | .26 | <.01 | |||
| Smoking Status (1=yes, 0=no) | −.47 | −.02 | .00 | ns | |
| Anxiety Sensitivity (ASI total score) | 12.15 | .52 | .29 | <.01 | |
| Step 3 | .00 | ns | |||
| Smoking Status X Anxiety Sensitivity | −.91 | −.07 | 00 | ns | |
Note. β = standardized beta weight; sr² = squared partial correlation. Gender: coded as 1 = male, 2=female; IES: The Index of Environmental Stress (Adams et al. 2002); AUDIT: Alcohol Use Disorders Identification Test (Babor et al., 1992); Smoke: Smoking Status, coded as 1 = smoker, 0 = non-smoker; ASI: Anxiety Sensitivity Index – Total Score (Reiss et al., 1986); MASQ-AA: Mood and Anxiety Symptom Questionnaire – Anxious Arousal (Watson et al., 1995); MASQ-AD: Mood and Anxiety Symptom Questionnaire – Anhedonic Depression (Watson et al., 1995); ACQ: Agoraphobic Cognitions Questionnaire (Chambless et al., 1984); PANAS-NA: Positive Affect Negative Affect Schedule – Negative Affect Scale (Watson et al., 1988).
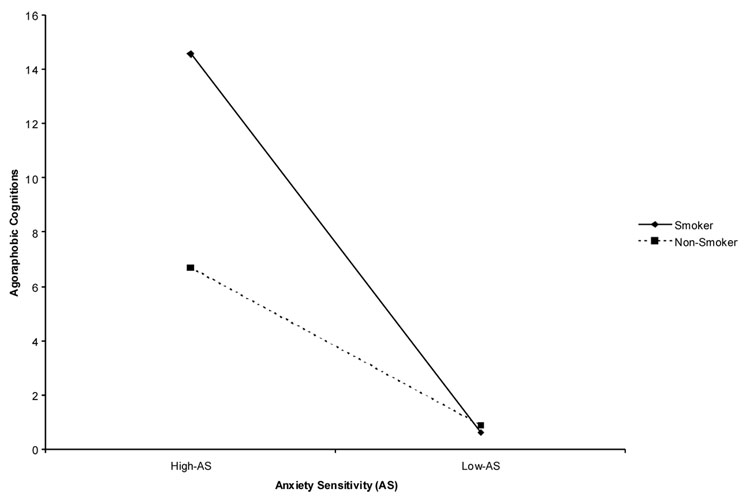
For the second regression, predicting agoraphobic cognitions, there was again a significant effect for environmental stress, but no effect for gender or alcohol use problems at the first level of the analysis. At the second level, there was a significant main effect for both AS and smoking status. As predicted, there was a significant interaction at the third level of the model (see Table 2).
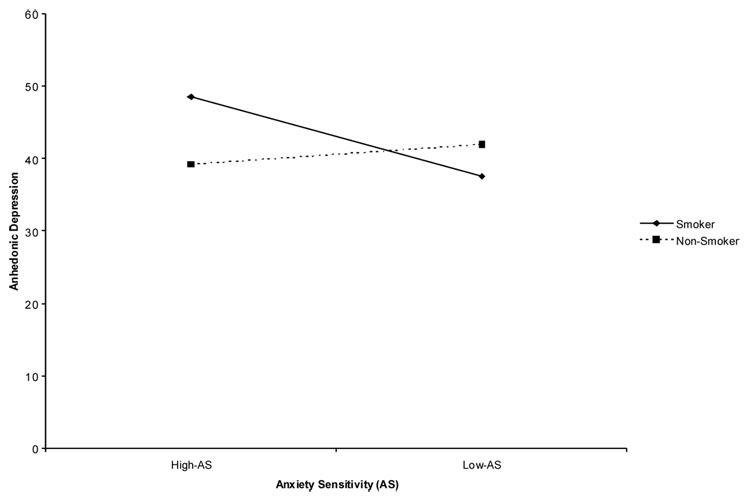
In regard to anhedonic depressive symptoms, there was a significant effect for environmental stress, but not for gender or alcohol use problems. At the second level, there were no significant main effects for either AS or smoking status. As predicted, there was a significant interaction at the third level of the model (see Table 2).
For the final regression, examining variance in negative affect, there was again a significant effect for both environmental stress and alcohol use (AUDIT), but no effect for gender at the first level of the analysis. At the second level, there was a significant main effect for AS, but not smoking status. As predicted, there was not a significant interaction at the third level of the model (see Table 2).
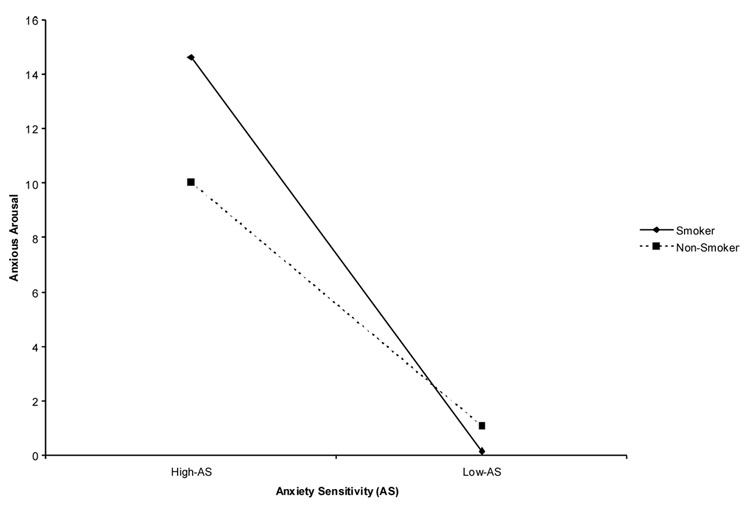
Significant interactions were examined in regard to hypothesized moderation both graphically (see Cohen & Cohen, 1983; for a review) and analytically (Holmbeck, 2002) to determine direction and significance. First, based on recommendations of Cohen and Cohen (1983; pp. 323, 419), the form of these interactions was examined by inserting specific values for each predictor variable into the regression equations associated with the described analysis. As can be seen in Figure 1–Figure 3, the form of the interactions supported hypotheses. Specifically, having a positive smoking status combined with higher levels of AS were associated with increased anxiety symptoms (Figure 1), agoraphobic cognitions (Figure 2), and depressive symptoms (Figure 3) compared to being high on only one or neither of these factors. Furthermore, based on recommendations of Holmbeck (2002), post-hoc probing analyses were conducted on the data to examine moderation. Results indicated that moderation does indeed occur in all three significant interactions. In all three cases, the relation between smoking status and the outcome variables (i.e. anxious arousal, anhedonic depression, or agoraphobic cognitions) was moderated when AS was high (t = 2.94, β = .19, p <.01, t = 2.02, β =.15, p <.05 and t = 4.16, β = .27, p < .01, respectively).
Figure 1.
Interaction between anxiety sensitivity and smoking status predicting anxious arousal. On the X-axis, “high” levels of AS refers to 1 standard deviation above the mean ASI level in the entire sample; similarly, “low” AS levels refers to1 standard deviation below the mean AS level in the entire sample.
Figure 3.
Interaction between anxiety sensitivity and smoking status predicting anhedonic depression. On the X-axis, “high” levels of AS refers to 1 standard deviation above the mean ASI level in the entire sample; similarly, “low” AS levels refers to1 standard deviation below the mean AS level in the entire sample.
Figure 2.
Interaction between anxiety sensitivity and smoking status predicting agoraphobic cognitions. On the X-axis, “high” levels of AS refers to 1 standard deviation above the mean ASI level in the entire sample; similarly, “low” AS levels refers to1 standard deviation below the mean AS level in the entire sample.
Discussion
There is a growing recognition that smoking may interplay in a clinically meaningful manner with AS in terms of panic-related problems (Zvolensky & Bernstein, 2005). Building from such work, the present study sought to replicate and extend past work documenting an interactive relationship between AS and smoking status in regard to a number of panic-related variables among a representative sample from Russia.
Consistent with prediction, there was convergent evidence for a significant interactive effect between AS and smoking status in regard to anxious arousal symptoms, catastrophic thinking related to bodily events, and depressed affect. These effects were small in effect size, but apparent after controlling for the variance attributable to gender, alcohol use problems, environmental stress (past month) as well as the respective main effects. Inspection of the form of these interactions indicated that, as expected, high AS smokers reported the highest levels of anxiety and depressive symptoms and catastrophic thinking related to bodily events (see Figure 1). Also as expected, there was no interactive effect apparent for negative emotional symptoms in general, providing evidence of explanatory specificity with respect to the studied panic and depressive symptoms. Thus, the interactive effect for AS and smoking status provides evidence for anxiety and depressive vulnerability but not negative affect in general. This finding is expected given extant work on smoking and panic factors wherein there is an expected theoretically-relevant learning process occurring that is not apparent for simply any negative emotional state (Zvolensky & Bernstein, 2005). These data uniquely extend past laboratory data among youth (Leen-Feldner, Zvolensky et al., in press). Thus, there is increased confidence in past work and an extension of it to a novel population. Future work could continue to refine and test this model by exploring whether particular AS lower-order factors are especially important in this relationship. Overall, the present findings demonstrate that AS is an important behavioral factor that qualifies the association between smoking status and panic-related symptoms as well as depressed affect. Indeed, such data indicate that smokers with high AS are at risk relative to their low AS non-smoking counterparts in regard to a range of problems with panic-related as well as depressive symptoms. Although the cross-sectional design does not permit explication of the causal relations between these vulnerability factors, it provides an empirical basis for future work to build upon the present work and related findings (Leen-Feldner, Zvolensky et al., in press) and conduct larger-scale prospective examinations. Future study in this domain can focus on biological (e.g., increased risk of physical disease) as well as behavioral (e.g., coping-based motivation for tobacco use) potential mechanisms of action.
Though not the primary study objective, it is noteworthy that AS and smoking status shared no variance with one another (see Table 1). This finding is important because it indicates that these two panic-related risk factors are tapping different types of vulnerability processes. This finding, in conjunction with the documented interaction, suggests that it may be fruitful to target high AS smokers as an at risk population for developing future panic psychopathology. For example, by employing integrated smoking-panic intervention protocols among high AS smokers before they have developed panic psychopathology, it may be possible to prevent the future development of such problems (see Zvolensky, Schmidt et al., 2006, for an expanded discussion).
An implication of the present findings is that individuals may be at greater risk for panic-related problems by virtue of individual differences in AS and smoking status. The identification of such moderating relations is theoretically important, as it helps to refine understanding of complex associations between a specific drug behavior (i.e., cigarette smoking) and panic psychopathology. It also facilitates understanding subpopulations with potentially different causal mechanisms or course of illness (Kraemer et al., 2002). Clinical intervention strategies can be adapted to better meet the needs of the population with this type of information. For example, rather than implementing prevention programs for panic disorder among individuals with only a single known risk factor, it may be more efficacious and cost-efficient to work towards developing prevention programs that focus on particularly high-risk segments of a specific population such as smokers with high AS. In this way, moderators can potentially help guide intervention decision-making to target high-risk groups.
There are a number of important interpretative caveats to the present study. First, the present cross-sectional correlational design does not permit causal-oriented hypothesis testing. It is nonetheless noteworthy that previous studies have typically found the panic-smoking relationship to be unidirectional (from smoking to panic psychopathology rather than vice versa; e.g., Bernstein et al., in press; Breslau & Klein, 1999). Although we did not have age of onset data for the present sample, future work could focus on such data to better gauge the patterning between smoking and panic vulnerability in addition to using prospective designs. Second, as with most large-scale population based studies, self-report methods were utilized to index the core constructs of interest. The challenge to the data pertains to the possibility of method variance contributing, at least in part, to the study results. To help remedy this concern, future studies should utilize a multimethod assessment approach. Third, although co-varying for alcohol use problems did not affect the pattern of findings in the present sample, empirical research indicates smoking is correlated with other types of drug/alcohol use and problems (Amos et al., 2004) and individuals with panic-related problems may use multiple types of psychoactive substances (Zvolensky, Bernstein et al., 2006). Thus, a key issue to address in future research is whether and how other types of substances (e.g., marijuana) affect the AS-panic association, and how polysubstance use relates to panic vulnerability.
Fourth, we used a measure that indexes exposure to aversive life conditions in the past month. We used this measure because it was constructed with an explicit a priori recognition of the specific types of socio-environmental stressors that currently characterize life in Russia (Yastrebov, 2001) as well as precedent of past work (Adams et al. 2002). Future work could utilize measures that provide an even more precise operationalization of specific stress constructs relevant to panic and/or smoking problems. Fifth, the present hypotheses were contextualized theoretically in terms of panic-related processes (Zvolensky & Bernstein, 2005). Future work could therefore extend the present study by including other assessments of panic-relevant processes, including unexpected panic attacks, severity of anticipatory anxiety, and so on. Sixth, there were no significant main effects observed for either AS or smoking status in regard to depressed affect, but there was the expected significant interaction. This finding suggests that only the combination of these two factors is related to depressive symptoms, a position that would be expected by extant theory pertaining to smoking and panic (Zvolensky & Bernstein, 2005). Nonetheless, as we utilized a measure that taps only the anhedonic features of depressed affect, it would be useful for future work to use other indices of depressive problems to better understand the nature of this interactive process. Finally, we utilized sampling methods that help to ensure a representative sample from the general community. Nonetheless, our sampling procedures were limited to adult residents of Moscow and therefore the present findings may not necessarily be representative of all Russians (e.g., individuals residing in rural areas). Future studies could address this potential limitation by targeting individuals from a larger geographic distribution in order to further enhance the generalizability of the present results.
Overall, the present study represents a novel, clinically-relevant test of the AS-smoking relationship as it applies to panic-related problems across diverse populations. To better understand the processes that contribute to panic psychopathology, it will be an important, albeit challenging, task to continue efforts to link the study of AS within the context of substance use behavior.
Acknowledgment
This paper was supported by National Institute on Drug Abuse research grants (1 R01 DA018734-01A1, R03 DA16307-01, and 1 R21 DA016227-01) awarded to the first author, a Graduate International Research Fellowship in Global Health from Center for International Rural and Environmental Health awarded to the second author, and an OSU-OIS Faculty International Travel Grant awarded to the fourth author.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Michael J. Zvolensky, The University of Vermont
Roman Kotov, State University of New York at Stony Brook.
Marcel O. Bonn-Miller, The University of Vermont
Norman B. Schmidt, Florida State University
Anna V. Antipova, Institute of Psychology, Russian Academy of Science
References
- Adams RE, Brome EJ, Panina N, Golovakha E, Goldgaber D, Gluzman S. Stress and well-being in mothers of young children 11 years after the Chornobyl nuclear power plant accident. Psychological Medicine. 2002;32:143–156. doi: 10.1017/s0033291701004676. [DOI] [PubMed] [Google Scholar]
- Amos A, Wiltshire S, Bostock Y, Haw S, McNeill A. You can’t go without a fag…you need it for your hash- a qualitative exploration of smoking, cannabis, and young people. Addiction. 2004;99:77–81. doi: 10.1111/j.1360-0443.2004.00531.x. [DOI] [PubMed] [Google Scholar]
- Arrindell WA. The fear of fear concept: Stability, retest artifact, and predictive power. Behaviour Research and Therapy. 1993;31:139–148. doi: 10.1016/0005-7967(93)90065-3. [DOI] [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, Grant M. The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care. WHO Publication No. 92.4. Geneva: World Health Organization. 1992
- Baker-Morissette SL, Brown TA, Wolfsdorf-Kamholz B, Gulliver SB. Differences between smokers and nonsmokers with anxiety disorders. Journal of Anxiety Disorders. doi: 10.1016/j.janxdis.2005.08.003. in press. [DOI] [PubMed] [Google Scholar]
- Barlow DH. The nature and treatment of anxiety and panic. 2nd ed. Vol. 2002 The Guilford Press: New York; 2002. Anxiety and its disorders. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Beckham J, Zvolensky MJ, Breslau N. Report on Tobacco use and cessation in psychiatric disorders; Paper presented at the 12th annual meeting of the Society for Research on Nicotine and Tobacco; February; Orlando, Florida. 2006. [Google Scholar]
- Bernstein A, Zvolensky MJ, Schmidt NB, Sachs-Ericcson N. Developmental course(s) of lifetime cigarette use and panic attack comorbidity: An equifinal phenomenon? Behavior Modification. doi: 10.1177/0145445506295056. in press. [DOI] [PubMed] [Google Scholar]
- Breslau N, Klein DF. Smoking and panic attacks: An epidemiologic investigation. Archives of General Psychiatry. 1999;56:1141–1147. doi: 10.1001/archpsyc.56.12.1141. [DOI] [PubMed] [Google Scholar]
- Breslau N, Novak SP, Kessler RC. Daily smoking and the subsequent onset of psychiatric disorders. Psychological Medicine. 2004;34:323–333. doi: 10.1017/s0033291703008869. [DOI] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Zvolensky MJ, Lejuez CW, Ramsey SE. Anxiety sensitivity: Relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addictive Behaviors. 2001;26:887–899. doi: 10.1016/s0306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Cigarette smoking among adults - United States, 1997. Morbidity and Mortality Weekly Report. 1999;48:993–996. [PubMed] [Google Scholar]
- Chambless DL, Caputo GC, Bright P, Gallagher R. Assessment of fear of fear in agoraphobics: The Body Sensations Questionnaire and the Agoraphobic Cognitions Questionnaire. Journal of Consulting and Clinical Psychology. 1984;54:1090–1097. doi: 10.1037//0022-006x.52.6.1090. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum. 1983 [Google Scholar]
- Comeau N, Stewart SH, Loba P. The relations of trait anxiety, anxiety sensitivity, and sensation seeking to adolescents' motivations for alcohol, cigarette, and marijuana use. Addictive Behaviors. 2001;26:803–825. doi: 10.1016/s0306-4603(01)00238-6. [DOI] [PubMed] [Google Scholar]
- Cox BJ, Taylor S, Enns MW. Fear of cognitive dyscontrol in relation to depression symptoms: comparisons between original and alternative measures of anxiety sensitivity. Journal of Behavior Therapy and Experimental Psychiatry. 1999;30:301–311. doi: 10.1016/s0005-7916(99)00026-9. [DOI] [PubMed] [Google Scholar]
- Folkman S, Moskowitz JT. Positive affect and the other side of coping. American Psychologist. 2000;55:647–654. doi: 10.1037//0003-066x.55.6.647. [DOI] [PubMed] [Google Scholar]
- Hayward C, Killen JD, Kraemer HC, Taylor CB. Predictors of panic attacks in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:207–214. doi: 10.1097/00004583-200002000-00021. [DOI] [PubMed] [Google Scholar]
- Hayward C, Killen JD, Taylor CB. Panic attacks in young adolescents. American Journal of Psychiatry. 1989;146:1061–1062. doi: 10.1176/ajp.146.8.1061. [DOI] [PubMed] [Google Scholar]
- Himle J, Thyer BA, Fischer DJ. Prevalence of smoking among anxious outpatients. Phobia Practice and Research Journal. 1988;1:25–31. [Google Scholar]
- Holmbeck GN. Post-hoc probing of significant moderational and mediational effects in studies of pediatric populations. Journal of Pediatric Psychology. 2002;27:87–96. doi: 10.1093/jpepsy/27.1.87. [DOI] [PubMed] [Google Scholar]
- Isensee B, Wittchen H, Stein MB, Höfler M, Lieb R. Smoking increases the risk of panic: Findings from a prospective community study. Archives of General Psychiatry. 2003;60:692–700. doi: 10.1001/archpsyc.60.7.692. [DOI] [PubMed] [Google Scholar]
- Ising M. Moderating factors in psychiatric disorders – essential to understanding the diversity of phenotypes. Journal of Psychiatric Research. 2006;40:381–382. [Google Scholar]
- Johnson JG, Cohen P, Pine DS, Klein DF, Kasen S, Brook JS. Association between cigarette smoking and anxiety disorders during adolescence and early adulthood. Journal of the American Medical Association . 2000;284:2348–2351. doi: 10.1001/jama.284.18.2348. [DOI] [PubMed] [Google Scholar]
- Kotov R, Schmidt NB, Zvolensky MJ, Vinogradov A, Antipova AV. Adaptation of panic-related psychopathology measures to Russian. Psychological Assessment. 2005;17(2):242–246. doi: 10.1037/1040-3590.17.2.242. [DOI] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras W. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Lasser K, Boyd JW, Woolhandler S, Himmelstein DU, McCormick D, Bor DH. Smoking and mental illness. Journal of the American Medical Association. 2000;284:2606–2610. doi: 10.1001/jama.284.20.2606. [DOI] [PubMed] [Google Scholar]
- Leen-Feldner EW, Zvolensky MJ, van Lent J, Vujanovic AA, Bleau T, Bernstein A, Bielawski-Branch A, Feldner MT. Anxiety sensitivity moderates tobacco smoking in regard to panic attack symptoms and bodily complaints: A concurrent test among adolescents. Journal of Psychopathology and Behavioral Assessment. in press. [Google Scholar]
- Maller RG, Reiss S. Anxiety sensitivity in 1984 and panic attacks in 1987. Journal of Anxiety Disorders. 1992;6:241–247. [Google Scholar]
- McCabe RE, Chudzik SM, Antony MM, Young L, Swinson RP, Zvolensky MJ. Smoking behaviors across anxiety disorders. Journal of Anxiety Disorders. 2004;18(1):7–18. doi: 10.1016/j.janxdis.2003.07.003. [DOI] [PubMed] [Google Scholar]
- McLeish AC, Zvolensky MJ, Bonn-Miller MO, Bernstein A. Perceived health moderates the association between smoking rate and panic vulnerability variables among daily smokers. Depression and Anxiety. 2006;23:257–265. doi: 10.1002/da.20170. [DOI] [PubMed] [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;52:938–946. doi: 10.1016/s0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- Moscow City Commission of State Statistics. Natural movement of residents of Moscow in 1999. Moscow, Russia: 2000. Author. [Google Scholar]
- Novak A, Burgess ES, Clark M, Zvolensky MJ, Brown RA. Anxiety sensitivity, self-reported motives for alcohol and nicotine use, and level of consumption. Journal of Anxiety Disorders. 2003;17:165–180. doi: 10.1016/s0887-6185(02)00175-5. [DOI] [PubMed] [Google Scholar]
- Otto MW, Pollack MH, Fava M, Uccello R, Rosenbaum JF. Elevated Anxiety Sensitivity Index scores in patients with major depression: correlates and changes with antidepressant treatment. Journal of Anxiety Disorders. 1995;9:117–123. [Google Scholar]
- Peterson RA, Reiss S. Anxiety Sensitivity Index Manual. 2nd ed. Worthington, OH: International Diagnostic Systems; 1992. [Google Scholar]
- Pohl R, Yeragani VK, Balon R, Lycaki H, McBride R. Smoking in patients with panic disorder. Psychiatry Research. 1992;43:253–262. doi: 10.1016/0165-1781(92)90058-b. [DOI] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. In: Theoretical Issues in Behavior Therapy. Reiss S, Bootzin RR, editors. San Diego: Academic Press; 1985. pp. 107–121. [Google Scholar]
- Reiss S, Peterson RA, Gursky M, McNally RJ. Anxiety, sensitivity, anxiety frequency, and the prediction of fearfulness. Behaviour Research and Therapy. 1986;24:1–8. doi: 10.1016/0005-7967(86)90143-9. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant T. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. The role of anxiety sensitivity in the pathogenesis of panic: Prospective evaluation of spontaneous panic attacks during acute stress. Journal of Abnormal Psychology. 1997;106:355–364. doi: 10.1037//0021-843x.106.3.355. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson DR. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: Replication and extension. Journal of Abnormal Psychology. 1999;108:532–537. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Joiner TE. Anxiety sensitivity and the pathogenesis of anxiety and depression: evidence for symptom specificity. Behaviour Research and Therapy. 1998;36:165–177. doi: 10.1016/s0005-7967(98)00011-4. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ, Maner JK. Journal of Psychiatric Research. Anxiety sensitivity: Prospective prediction of panic attacks and Axis I pathology. in press. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Karp J, Pihl RO, Peterson RA. Anxiety sensitivity and self-reported reasons for drug use. Journal of Substance Abuse. 1997;9:223–240. doi: 10.1016/s0899-3289(97)90018-3. [DOI] [PubMed] [Google Scholar]
- Taylor S. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Mahwah, NJ: Erlbaum; 1999. [Google Scholar]
- Warren R, Zgourides G, Englert M. Relationships between catastrophic cognitions and body sensations in anxiety disordered, mixed diagnosis, and normal subjects. Behaviour Research and Therapy. 1990;28:355–357. doi: 10.1016/0005-7967(90)90090-6. [DOI] [PubMed] [Google Scholar]
- Warren R, Zgourides G, Jones A. Cognitive bias and irrational belief as predictors of avoidance. Behaviour Research and Therapy. 1989;27:181–188. doi: 10.1016/0005-7967(89)90077-6. [DOI] [PubMed] [Google Scholar]
- Watson D. Basic problems in positive mood regulation. Psychological Inquiry. 2000;11:205–209. [Google Scholar]
- Watson D, Clark LA, Tellegen L. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, McCormick RA. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of Abnormal Psychology. 1995;104:3–14. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]
- Weems CF, Hayward C, Killen J, Taylor CB. A longitudinal investigation of anxiety sensitivity in adolescence. Journal of Abnormal Psychology. 2002;111:471–477. [PubMed] [Google Scholar]
- Yartz AR, Zvolensky MJ, Gregor K, Feldner MT, Leen-Feldner E. Health perception is a unique predictor of anxiety symptoms in nonclinical participants. Cognitive Behaviour Therapy. doi: 10.1080/16506070510010611. in press. [DOI] [PubMed] [Google Scholar]
- Yastrebov VS. Psychological health of the population on the threshold of third millennium. Psihiatria. 2001;1:3–8. [Google Scholar]
- Zinbarg RE, Barlow DH, Brown TA. Hierarchical structure and general factor structure saturation of the Anxiety Sensitivity Index: Evidence and implications. Psychological Assessment. 1997;9:277–284. [Google Scholar]
- Zvolensky MJ, Baker KM, Leen-Feldner EW, Bonn-Miller MO, Feldner MT, Brown RA. Anxiety sensitivity: Association with intensity of retrospectively-rated smoking-related withdrawal symptoms and motivation to quit. Cognitive Behaviour Therapy. 2004;33:114–125. doi: 10.1080/16506070310016969. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A. Cigarette smoking and panic psychopathology. Current Directions in Psychological Science. 2005;14:301–305. [Google Scholar]
- Zvolensky MJ, Bernstein A, Cardenas SJ, Colotla VA, Marshall EC, Feldner MT. Anxiety sensitivity and early relapse to smoking: A test among Mexican daily, low-level smokers. Nicotine and Tobacco and Research. doi: 10.1080/14622200701239621. in press. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Marshall EC, Feldner MT. Panic attacks, panic disorder, and agoraphobia: Associations with substance use, abuse, and dependence. Current Psychiatry Reports. 2006;8:279–285. doi: 10.1007/s11920-006-0063-6. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Bernstein A, Yartz AR, McLeish A, Feldner MT. Cognitive-behavioral treatment of comorbid panic psychopathology and tobacco use and dependence. In: Stewart SH, Conrad P, editors. Comorbidity of anxiety and substance use disorders. New York: Springer; in press. [Google Scholar]
- Zvolensky MJ, Bonn-Miller MO, Bernstein A, Marshall EC. Anxiety sensitivity and abstinence duration to smoking. Journal of Mental Health. in press. [Google Scholar]
- Zvolensky MJ, Bonn-Miller MO, Feldner MT, Leen-Feldner E, McLeish AC, Gregor K. Anxiety sensitivity: Concurrent association with negative affect smoking motives and abstinence self-confidence among young adult smokers. Addictive Behaviors. 2006;31:429–439. doi: 10.1016/j.addbeh.2005.05.027. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner E, Bonn-Miller MO, McLeish AC, Gregor K. Evaluating the role of anxiety sensitivity in smoking outcome expectancies among regular smokers. Cognitive Therapy and Research. 2004;28:473–486. [Google Scholar]
- Zvolensky MJ, Feldner MT, Leen-Feldner EW, McLeish AC. Smoking and panic attacks, panic disorder, and agoraphobia: A review of the empirical literature. Clinical Psychology Review. 2005;25(6):761–789. doi: 10.1016/j.cpr.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Forsyth JP. Anxiety sensitivity dimensions in the prediction of body vigilance and emotional avoidance. Cognitive Therapy and Research. 2002;26:449–460. [Google Scholar]
- Zvolensky MJ, Forsyth JP, Fuse T, Feldner MT, Leen-Feldner E. Panic attacks and smoking: An initial investigation of panic-relevant cognitive processes. Cognitive Behaviour Therapy. 2002;31:170–182. [Google Scholar]
- Zvolensky MJ, Lejuez CW, Kahler CW, Brown RA. Integrating an interoceptive exposure-based smoking cessation program into the cognitive-behavioral treatment of panic disorder: Theoretical relevance and clinical demonstration. Cognitive and Behavioral Practice. 2003;10:348–358. [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Cross-cultural evaluation of smokers risk for panic and anxiety pathology: A test in a Russian epidemiological sample. Behaviour Research and Therapy. 2003;41:1199–1215. doi: 10.1016/s0005-7967(03)00031-7. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Diathesis stress model for panic-related distress: A test in a Russian epidemiological sample. Behaviour Research and Therapy. 2005;43(4):521–532. doi: 10.1016/j.brat.2004.09.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Leen-Feldner EW, Feldner MT, Bonn-Miller MO, Lejuez CW, Kahler C, Stuart G. Emotional responding to biological challenge as a function of panic disorder and smoking. Journal of Anxiety Disorders. 2004;18:19–32. doi: 10.1016/j.janxdis.2003.07.004. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Schmidt NB, Bernstein A, Keough ME. Risk factor research and prevention programs for anxiety disorders: A translational research framework. Behaviour Research and Therapy. 2006;44:1219–1239. doi: 10.1016/j.brat.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Schmidt NB, McCreary BT. The impact of smoking on panic disorder: An initial investigation of a pathoplastic relationship. Journal of Anxiety Disorders. 2003;17:447–460. doi: 10.1016/s0887-6185(02)00222-0. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Schmidt MB, Stewart SH. Panic disorder and smoking. Clinical Psychology: Science and Practice. 2003;10:29–51. [Google Scholar]