Abstract
Cannabis sativa is the source of a unique set of compounds known collectively as plant cannabinoids or phytocannabinoids. This review focuses on the manner with which three of these compounds, (−)-trans-Δ9-tetrahydrocannabinol (Δ9-THC), (−)-cannabidiol (CBD) and (−)-trans-Δ9-tetrahydrocannabivarin (Δ9-THCV), interact with cannabinoid CB1 and CB2 receptors. Δ9-THC, the main psychotropic constituent of cannabis, is a CB1 and CB2 receptor partial agonist and in line with classical pharmacology, the responses it elicits appear to be strongly influenced both by the expression level and signalling efficiency of cannabinoid receptors and by ongoing endogenous cannabinoid release. CBD displays unexpectedly high potency as an antagonist of CB1/CB2 receptor agonists in CB1- and CB2-expressing cells or tissues, the manner with which it interacts with CB2 receptors providing a possible explanation for its ability to inhibit evoked immune cell migration. Δ9-THCV behaves as a potent CB2 receptor partial agonist in vitro. In contrast, it antagonizes cannabinoid receptor agonists in CB1-expressing tissues. This it does with relatively high potency and in a manner that is both tissue and ligand dependent. Δ9-THCV also interacts with CB1 receptors when administered in vivo, behaving either as a CB1 antagonist or, at higher doses, as a CB1 receptor agonist. Brief mention is also made in this review, first of the production by Δ9-THC of pharmacodynamic tolerance, second of current knowledge about the extent to which Δ9-THC, CBD and Δ9-THCV interact with pharmacological targets other than CB1 or CB2 receptors, and third of actual and potential therapeutic applications for each of these cannabinoids.
Keywords: cannabis, Δ9-tetrahydrocannabinol, cannabidiol, Δ9-tetrahydrocannabivarin, CB1 receptors, CB2 receptors, cannabinoid receptor agonism, cannabinoid receptor antagonism, clinical applications, endocannabinoid system
Introduction
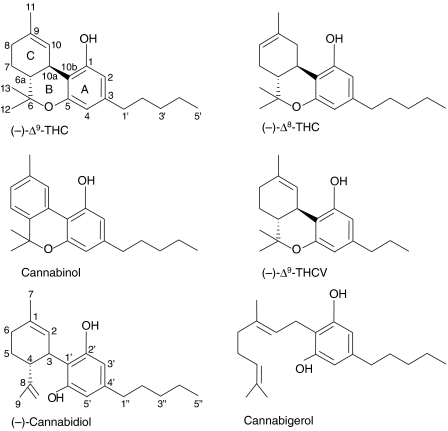
It was research in the 1960s and early 1970s that led to the discovery that the psychotropic effects of cannabis are produced mainly by (−)-trans-Δ9-tetrahydrocannabinol (Δ9-THC; Figure 1), to the pharmacological characterization of this plant cannabinoid (phytocannabinoid) and to the development of synthetic cannabinoids (reviewed in Pertwee, 2006). These advances led on to the introduction into the clinic in the 1980s of Δ9-THC (dronabinol, Marinol, Solvay Pharmaceuticals, Brussels, Belgium) and of one of its synthetic analogues, nabilone (Cesamet, Valeant Pharmaceuticals, Aliso Viejo, CA, USA), for the suppression of nausea and vomiting produced by chemotherapy and, in 1992, of Marinol for the stimulation of appetite in AIDS patients (reviewed in Robson, 2005; Pertwee and Thomas, 2007). Importantly, they also led on to the discovery that many of the effects produced by Δ9-THC and its synthetic cousins depend on the ability of these ligands to target a new family of receptors (reviewed in Howlett et al., 2002; Pertwee, 2005a, 2006). Two types of these cannabinoid receptors have so far been identified and both are members of the superfamily of G-protein-coupled receptors. These are the CB1 receptor, first cloned in 1990 (Matsuda et al., 1990), and the CB2 receptor, cloned in 1993 (Munro et al., 1993).
Figure 1.
The structures of the phytocannabinoids, (−)-Δ9-tetrahydrocannabinol (Δ9-THC), (−)-Δ8-tetrahydrocannabinol (Δ8-THC), cannabinol, (−)-Δ9-tetrahydrocannabivarin (Δ9-THCV), (−)-cannabidiol (CBD) and cannabigerol.
The cloning of the CB1 receptor was soon followed by the discovery that mammalian tissues can produce compounds that activate this receptor, and subsequently by the characterization of ligands such as Δ9-THC, (6aR)-trans-3-(1,1-dimethylheptyl)-6a,7,10,10a-tetrahydro-1-hydroxy-6,6-dimethyl-6H-dibenzo[b,d]pyran-9-methanol (HU-210), (−)-cis-3-[2-hydroxy-4-(1,1-dimethylheptyl)phenyl]-trans-4-(3-hydroxypropyl)cyclohexanol (CP55940) and (R)-(+)-[2,3-dihydro-5-methyl-3-(4-morpholinylmethyl)pyrrolo-[1,2,3-de]-1,4-benzoxazin-6-yl]-1-naphthalenylmethanone (R-(+)-WIN55212) as mixed CB1/CB2 receptor agonists and by the development of CB1- and CB2-selective agonists and antagonists (reviewed in Howlett et al., 2002; Pertwee, 2005a, 2006). It also soon became clear that CB1 receptors are located primarily in central and peripheral neurons and CB2 receptors predominantly in immune cells. CB1 receptors are also expressed by some non-neuronal cells, including immune cells, and CB2 receptors by some neurons both within and outside the brain (Skaper et al., 1996; Ross et al., 2001; Van Sickle et al., 2005; Wotherspoon et al., 2005; Beltramo et al., 2006; Gong et al., 2006). However, the role of neuronal CB2 receptors is currently unknown. The first endogenous cannabinoid receptor agonists (endocannabinoids) to be identified were N-arachidonoylethanolamine (anandamide) and 2-arachidonoylglycerol (Devane et al., 1992; Mechoulam et al., 1995; Sugiura et al., 1995), each of which can activate both CB1 and CB2 receptors and is synthesized on demand in response to elevations of intracellular calcium (Howlett et al., 2002; Di Marzo et al., 2005). Together with their receptors, these and other more recently discovered endocannabinoids (Pertwee, 2005b) constitute what is now usually referred to as the ‘endocannabinoid system'.
There are several reasons for believing that one important role of the neuronal CB1 component of the endocannabinoid system is to modulate neurotransmitter release in a manner that maintains homeostasis in health and disease by preventing the development of excessive neuronal activity in the central nervous system. First, neuronal CB1 receptors are found mainly at the terminals of central and peripheral neurons. Second, there is good evidence that these receptors can mediate inhibition of ongoing release of a number of different excitatory and inhibitory transmitters, for example acetylcholine, noradrenaline, dopamine, 5-hydroxytryptamine (5-HT), γ-aminobutyric acid (GABA), glutamate, D-aspartate and cholecystokinin (Howlett et al., 2002; Pertwee and Ross, 2002; Szabo and Schlicker, 2005). Finally, there is convincing evidence that endocannabinoids serve as retrograde synaptic messengers (Kreitzer, 2005; Vaughan and Christie, 2005). Thus, it is now generally accepted that postsynaptic increases in intracellular calcium induced by certain neurotransmitters can trigger the biosynthesis and release into the synapse of endocannabinoid molecules, which then act on presynaptic CB1 receptors to inhibit the release of neurotransmitters such as glutamate and GABA. CB2 receptor activation can also alter the release of chemical messengers, in this case the release of cytokines from immune cells and may, in addition, affect immune function by modulating immune cell migration both within and outside the central nervous system (reviewed in Walter and Stella, 2004; Cabral and Staab, 2005; Pertwee, 2005a).
This review focuses on the cannabinoid CB1 and CB2 receptor pharmacology of the phytocannabinoids Δ9-THC, (−)-cannabidiol (CBD) and (−)-trans-Δ9-tetrahydrocannabivarin (Δ9-THCV) (Figure 1), all three of which interact with these receptors at reasonably low concentrations. Whenever possible, previous review articles have been cited that provide more detailed information and list additional references.
The CB1 and CB2 receptor pharmacology of Δ9-THC
(−)-trans-Δ9-Tetrahydrocannabinol shares the ability of anandamide and 2-arachidonoylglycerol to activate both CB1 and CB2 receptors. More particularly, as discussed in greater detail elsewhere (Pertwee, 1997, 1999, 2005a; Howlett et al., 2002; Childers, 2006), it binds to cannabinoid CB1 and CB2 receptors with Ki values in the low nanomolar range (Table 1) that indicate it to have higher affinity for these receptors than its corresponding (+)-cis (6aS, 10aS) enantiomer ((+)-Δ9-THC), but lower CB1 and CB2 affinity than certain synthetic CB1/CB2 receptor agonists, for example HU-210, CP55940 and R-(+)-WIN55212. Δ9-THC also exhibits lower CB1 and CB2 efficacy than these synthetic agonists, indicating it to be a partial agonist for both these receptor types. In contrast, the affinity of Δ9-THC for CB1 and CB2 receptors does match or exceed that of the phytocannabinoids (−)-Δ8-THC, Δ9-THCV, CBD, cannabigerol and cannabinol (Table 1). It has also been found that Δ9-THC resembles anandamide in its CB1 affinity, in behaving as a partial agonist at CB1 receptors, albeit with less efficacy than anandamide, and in displaying even lower efficacy at CB2 than at CB1 receptors in vitro. Although 2-arachidonoylglycerol also possesses Δ9-THC-like CB1 affinity, it has been found in several investigations to display higher efficacy than anandamide and hence Δ9-THC at both CB1 and CB2 receptors.
Table 1.
Some Ki values of (−)-Δ9-THC and certain other phytocannabinoids for the in vitro displacement of [3H]CP55940 or [3H]HU-243 from CB1- and CB2-specific binding sites
| Phytocannabinoid | CB1 Ki (nM) | CB2 Ki (nM) | References |
|---|---|---|---|
| (−)-Δ9-THC | 5.05 | 3.13 | Iwamura et al. (2001) |
| 35.3a | 3.9a | Rinaldi-Carmona et al. (1994) | |
| 39.5b,c | 40c | Bayewitch et al. (1996) | |
| 21 | 36.4 | Showalter et al. (1996) | |
| 53.3 | 75.3 | Felder et al. (1995) | |
| 80.3b,c | 32.2c | Rhee et al. (1997) | |
| (−)-Δ8-THC | 44a | 44 | Huffman et al. (1999) |
| 47.6a | 39.3d | Busch-Petersen et al. (1996) | |
| (−)-Δ9-THCV | 75.4d | 62.8 | Thomas et al. (2005) |
| 46.6d | ND | Pertwee et al. (2007a) | |
| Cannabinol | 120.2 | 100 | MacLennan et al. (1998a, 1998b) |
| 211.2b,c | 126.4c | Rhee et al. (1997) | |
| 326 | 96.3 | Showalter et al. (1996) | |
| 1130 | 301 | Felder et al. (1995) | |
| CBD | 4350a | 2860 | Showalter et al. (1996) |
| 4900d | 4200 | Thomas et al. (2004, 2007) | |
| 27 542 | 2399 | MacLennan et al. (1998b) | |
| >10 000a,c | >10 000c | Bisogno et al. (2001) | |
| Cannabigerol | 440d | 337 | Gauson et al. (2007), Pertwee et al. (2007a) |
Abbreviations: CBD, cannabidiol; ND, not determined; THC, tetrahydrocannabinol; THCV, tetrahydrocannabivarin.
Experiments were performed with rat brain (CB1) or rat spleen (CB2) membranes.
Experiments were performed with membranes from cultured cells transfected with rat cannabinoid receptors.
Experiments were performed with [3H]HU243.
Experiments were performed with mouse brain (CB1) or mouse spleen (CB2) membranes.
All other data are from experiments performed with [3H]CP55940 and/or with membranes from cultured cells transfected with human cannabinoid receptors.
See Figure 1 for the structures of the compounds listed in this table.
Among the effects that Δ9-THC seems to produce in vivo in healthy animals by activating neuronal CB1 receptors are several that are frequently used as measured responses in bioassays for CB1 receptor agonists (reviewed in Howlett et al., 2002; Pertwee, 2006). For mice, these include a ‘tetrad' of effects, suppression of locomotor activity, hypothermia, immobility in the ring test and antinociception in the tail-flick or hot-plate test. That the production of these effects by Δ9-THC depends on CB1 receptor activation is supported by findings that this is readily antagonized by the selective CB1 receptor antagonist, N-(piperidin-1-yl)-5-(4-chlorophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazole-3-carboxamide hydrochloride (SR141716A), that most of the tetrad effects are not produced by Δ9-THC in mice from which the CB1 receptor has been genetically deleted, that Δ9-THC produces these effects with a potency (half-maximal effective dose=1–1.5 mg kg−1 intravenous (i.v.)) that is consistent with its CB1 receptor affinity and that they are also produced by a wide range of other established CB1 receptor agonists (Martin et al., 1991; Zimmer et al., 1999; Di Marzo et al., 2000; Wiley et al., 2001; Varvel et al., 2005). It is noteworthy, however, that deletion of the CB1 receptor from mice bred on a C57BL/6J background does not affect the ability of Δ9-THC to induce antinociception in the tail-flick test, though it does abolish HU-210-induced antinociception in this bioassay and also Δ9-THC-induced antinociception in the hot-plate test (Zimmer et al., 1999).
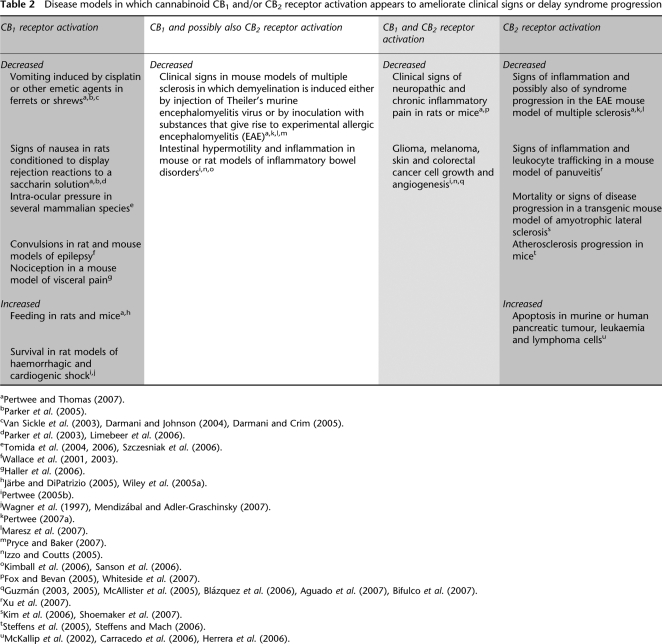
There is evidence that in addition to eliciting responses in healthy animals, cannabinoid receptor activation by Δ9-THC can also ameliorate clinical signs or delay syndrome progression in animal models of certain disorders (reviewed in Pertwee, 2005b, 2007a; Pertwee and Thomas, 2007). This it does in a manner that not only supports the established clinical applications of Δ9-THC and nabilone for appetite stimulation and antiemesis and of the Δ9-THC- and CBD-containing medicine, Sativex (GW Pharmaceuticals, Salisbury, Wiltshire, UK), for the symptomatic relief of neuropathic pain in patients with multiple sclerosis and of cancer pain, but has also identified potential additional therapeutic uses for Δ9-THC, nabilone or other cannabinoid receptor agonists (Table 2). Clinical evidence supporting the introduction of Δ9-THC or other cannabinoid receptor agonists into the clinic, for example for the management of disorders such as glaucoma and cancer, and for the relief of postoperative pain, spasms and spasticity caused by multiple sclerosis and painful spasticity triggered by spinal cord injury has also been obtained (Tomida et al., 2004, 2006; Robson, 2005; Guzmán et al., 2006; Pertwee, 2007a; Pertwee and Thomas, 2007).
Table 2.
Disease models in which cannabinoid CB1 and/or CB2 receptor activation appears to ameliorate clinical signs or delay syndrome progression
Δ9-THC and neurotransmission
Like endogenously released endocannabinoids, CB1 receptor agonists can act through neuronal presynaptic CB1 receptors to inhibit ongoing neurotransmitter release (reviewed in Pertwee and Ross, 2002; Szabo and Schlicker, 2005). Indeed, it is generally accepted that this action gives rise to many of the CB1-receptor-mediated effects that Δ9-THC produces when it is administered in vivo. It is likely, however, that neuronal CB1 receptors are targeted in a far less selective manner by exogenously administered Δ9-THC than by endocannabinoid molecules when these are released, for example during retrograde signalling (reviewed in Kreitzer, 2005; Vaughan and Christie, 2005).
Although CB1 receptors generally mediate an inhibitory effect on any ongoing transmitter release from the neurons on which they are expressed, activation of these receptors in vivo sometimes leads to increased transmitter release from other neurons. More specifically, there is evidence that in vivo administration of Δ9-THC produces CB1-mediated increases in the release of acetylcholine in rat hippocampus, of acetylcholine, glutamate and dopamine in rat prefrontal cortex, and of dopamine in mouse and rat nucleus accumbens (Pertwee and Ross, 2002; Pistis et al., 2002; Gardner, 2005; Nagai et al., 2006; Pisanu et al., 2006). At least some of these increases most probably occur because this cannabinoid is directly or indirectly inhibiting the release of an inhibitory transmitter onto acetylcholine-, glutamate- or dopamine-releasing neurons. Thus, for example, Δ9-THC may augment dopamine release in the nucleus accumbens by acting on CB1 receptors to inhibit the release of glutamate onto GABAergic neurons that project from the nucleus accumbens to the ventral tegmental area where they exert an inhibitory effect on the firing of dopaminergic neurons projecting back to the nucleus accumbens (reviewed in Pertwee and Ross, 2002). Similarly, since there is evidence that acetylcholine release in the prefrontal cortex is regulated by inhibitory GABAergic neurons that project from the nucleus accumbens, it is possible that Δ9-THC enhances cortical acetylcholine release through a ‘disinhibitory' process that involves a CB1-mediated suppression of GABA release onto cortical acetylcholine-releasing neurons (reviewed in Pertwee and Ross, 2002). It has also been proposed that it is the stimulatory effect of Δ9-THC on dopamine release in the nucleus accumbens that accounts for its ability to increase acetylcholine release in rat prefrontal cortex and hippocampus (Pisanu et al., 2006). This effect on dopamine release most likely explains why Δ9-THC can induce signs of reward in animals, for example a decrease in the reward threshold for in vivo electrical self-stimulation of rat neural reward circuits, the preference shown by rats and mice for a chamber paired with Δ9-THC in the conditioned place preference paradigm, and lever pressing by squirrel monkeys for i.v. injections of Δ9-THC, an effect that seems to be CB1 mediated as it can be blocked by the CB1-selective antagonist SR141716A (Braida et al., 2004; Gardner, 2005; Justinova et al., 2005). Δ9-THC-induced stimulation of dopamine release in the nucleus accumbens probably also accounts, at least in part, for the ability of this phytocannabinoid to increase food palatability/the incentive to eat and hence food intake (reviewed in Pertwee and Thomas, 2007).
The mixed stimulatory–inhibitory effect that Δ9-THC has on central neurotransmitter release when it is administered in vivo is one possible reason why this cannabinoid has been reported to exhibit both excitant and depressant effects in behavioural bioassays. Thus, for example, it has been found to display anticonvulsant activity in some in vivo models of epilepsy but proconvulsant activity in others (Chiu et al., 1979; Turkanis and Karler, 1981; Colasanti et al., 1982; Fish et al., 1983; Dewey, 1986; Wallace et al., 2003), and to induce signs of anxiolytic activity in some investigations with rats or mice but signs of anxiogenic activity in others (Berrendero and Maldonado, 2002; Patel and Hillard, 2006; Braida et al., 2007; Schramm-Sapyta et al., 2007). It is also possible that Δ9-THC augments as well as inhibits central neurotransmission because it can both activate and block CB1 receptors (see next section) and hence both mimic and block endocannabinoid-mediated retrograde signalling.
Δ9-THC can both activate and block cannabinoid receptors
Because Δ9-THC has relatively low cannabinoid receptor efficacy, classical pharmacology predicts that its ability to activate these receptors will be particularly influenced by the density and coupling efficiencies of these receptors. It is, for example, possible that there are some CB1- or CB2-expressing cells or tissues in which Δ9-THC does not share the ability of higher efficacy agonists to activate CB1 or CB2 receptors because the density and coupling efficiencies of these receptors are too low. These will be populations of cannabinoid receptors in which Δ9-THC might instead antagonize agonists that possess higher CB1 or CB2 efficacy when these are administered exogenously or released endogenously. It is noteworthy, therefore, that both the density and coupling efficiencies of CB1 receptors vary widely within the brain. For example, in rat, CB1 receptor density is much higher in substantia nigra pars reticulata, entopeduncular nucleus, globus pallidus and lateral caudate–putamen than in amygdala, thalamus, habenula, preoptic area, hypothalamus and brain stem and CB1 coupling to G proteins is markedly more efficient in hypothalamus than in frontal cortex, cerebellum or hippocampus (reviewed in Pertwee, 1997; Childers, 2006). Moreover, CB1 receptors in mouse hippocampus are more highly expressed by GABAergic interneurons than glutamatergic principal neurons (Monory et al., 2006). CB1 receptors are also distributed within the mammalian brain in a species-dependent manner. Thus for example, compared to rat brains, human brains express more CB1 receptors in the cerebral cortex and amygdala and less in the cerebellum, a finding that may explain why motor function seems to be affected more by CB1 receptor agonists in rats than humans (Herkenham et al., 1990). There is also evidence that a species difference in the relative sensitivities of GABA- and glutamate-releasing neurons to CB1 receptor agonism may explain why, following administration of the high-efficacy CB1 receptor agonist, R-(+)-WIN55212, signs of anxiety decrease in mice but increase in rats (Haller et al., 2007).
In view of the rather low-expression levels and/or coupling efficiencies of CB1 receptors in some central neurons, it is not altogether unexpected that Δ9-THC has been found to behave as a CB1 receptor antagonist in some experiments. For example, Patel and Hillard (2006) found that Δ9-THC shares the ability of the CB1-selective antagonists, SR141716A and N-(piperidin-1-yl)-5-(4-iodophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazole-3-carboxamide (AM251), to induce signs of anxiogenic activity in a mouse model in which CP55940 and R-(+)-WIN55212 each displayed anxiolytic-like activity. Evidence has also been obtained from one investigation that Δ9-THC can oppose R-(+)-WIN55212-induced stimulation of guanosine-5′-O-(3-thiotriphosphate) ([35S]GTPγS) binding to rat cerebellar membranes (Sim et al., 1996), and from others that it can attenuate inhibition of glutamatergic synaptic transmission induced in rat or mouse cultured hippocampal neurons by R-(+)-WIN55212 or 2-arachidonoylglycerol (Shen and Thayer, 1999; Kelley and Thayer, 2004; Straiker and Mackie, 2005). In one of these investigations, performed with mouse cultured ‘ataptic' hippocampal neurons (Straiker and Mackie, 2005), the results obtained also suggested that Δ9-THC can inhibit depolarization-induced suppression of excitation, and hence presumably that it may inhibit endocannabinoid-mediated retrograde signalling in at least some central neuronal pathways.
The extent to which and precise mechanisms through which the heterogeneity of the cannabinoid CB1 receptor population within the brain shapes the in vivo pharmacology of Δ9-THC and causes it to behave differently from agonists with higher CB1 or CB2 efficacy warrants further investigation. So too does the hypothesis that Δ9-THC may sometimes antagonize responses to endogenously released endocannabinoids, not least because there is evidence that such release can modulate the signs and symptoms of certain disorders and/or disease progression (reviewed in Pertwee, 2005b; Maldonado et al., 2006). Although this modulation often seems to be protective, there is evidence that it can sometimes produce harmful effects that, for example, give rise to obesity or contribute to the rewarding effects of drugs of dependence.
(−)-trans-Δ9-Tetrahydrocannabinol can also produce antagonism at the CB2 receptor. Thus, Bayewitch et al. (1996) have found Δ9-THC (0.01–1 μM) to exhibit only marginal agonist activity in COS-7 cells transfected with human CB2 (hCB2) receptors when the measured response was inhibition of cyclic AMP production stimulated by 1 μM forskolin. Instead, Δ9-THC behaved as a CB2 receptor antagonist in this bioassay at both 0.1 and 1 μM with an apparent KB value against HU-210 of 25.6 nM. More recently, Kishimoto et al. (2005) found that Δ9-THC (1 μM) shares the ability of the CB2-selective antagonist, N-[(1S)-endo-1,3,3-trimethyl bicyclo [2.2.1] heptan-2-yl]-5-(4-chloro-3-methylphenyl)-1-(4-methylbenzyl)-pyrazole-3-carboxamide (SR144528), to abolish 2-arachidonoylglycerol-induced migration of human leukaemic natural killer cells.
Clinical implications of the partial agonism displayed by Δ9-THC at CB1 and CB2 receptors
Whereas downregulation of cannabinoid receptors may cause Δ9-THC to produce antagonism rather than agonism, their upregulation is expected to enhance the ability of this partial agonist to activate cannabinoid receptors. It is noteworthy, therefore, that there are some disorders that appear to trigger an upregulation of cannabinoid receptors selectively in cells or tissues in which these receptors mediate symptom relief and/or inhibition of disease progression when activated by endogenously released or exogenously administered cannabinoids (Pertwee, 2005b). For example, there is evidence that in rat or mouse models of neuropathic pain there is increased expression of CB1 receptors in thalamic neurons, of CB1 and CB2 receptors in spinal cord, dorsal root ganglion/primary afferent neurons and paw skin and of CB2 receptors in activated microglia that have migrated into the spinal cord (Siegling et al., 2001; Lim et al., 2003; Zhang et al., 2003; Wotherspoon et al., 2005; Beltramo et al., 2006; Mitrirattanakul et al., 2006; Walczak et al., 2006). In addition, since the density or coupling efficiency of CB1 receptors is greater in some central neurons than in others (see above text), it is likely that the extent to which Δ9-THC activates or blocks central CB1 receptors will not be the same for all CB1-expressing neuronal pathways of the brain.
There is evidence too that both CB1 and CB2 receptors are more highly expressed in human hepatocellular carcinoma tumour samples than in matched non-tumorous tissues, that this increased expression may prolong survival (Xu et al., 2006) and that ‘protective' increases in the densities of both these receptor types occur in human prostate cancer cells (Sarfaraz et al., 2005). Increases that are apparently protective have also been detected in CB1 receptor expression within the brain in rodent models of stroke (Jin et al., 2000) and temporal-lobe epilepsy (Wallace et al., 2003) and in the density or expression of intestinal CB1 receptors in mouse models of intestinal inflammation, colitis and diarrhoea (Izzo et al., 2001, 2003; Massa et al., 2004; Kimball et al., 2006) and of CB2 receptors in colonic-infiltrated immune cells in mouse models of colitis (Kimball et al., 2006) and in macrophages and T lymphocytes located in human and murine atherosclerotic plaques (Steffens et al., 2005). It is noteworthy, however, that although CB1-receptor-coupling efficiency has been reported to increase in certain brain areas of rats with experimental autoimmune encephalomyelitis (EAE), this increase was accompanied by a decrease in CB1 receptor density in the same brain areas (Berrendero et al., 2001). Moreover in EAE mice, decreases have been detected in both central CB1 receptor density (cerebellum, globus pallidus and lateral caudate–putamen) and coupling efficiency (cerebellum) (Cabranes et al., 2006). In contrast, CB2 receptor expression levels have been reported to increase in regions of human post-mortem spinal cord affected by multiple sclerosis or amyotrophic lateral sclerosis (Yiangou et al., 2006) and in the central nervous systems of EAE mice (Maresz et al., 2005). These increases have been shown to result from an accumulation of microglial cells and peripheral macrophages and there is evidence from the mouse experiments that activation of the CB2 receptors expressed by these cells leads to an amelioration of EAE inflammation and possibly also to a slowing of EAE progression (Maresz et al., 2007).
Such upregulation of cannabinoid CB1 or CB2 receptors is expected to improve the selectivity and effectiveness of a cannabinoid receptor agonist as a therapeutic agent, especially when it is a partial agonist such as Δ9-THC. Thus, although an increase in receptor density will augment the potencies of both full and partial agonists, it will sometimes also increase the size of the maximal response to a partial agonist without affecting the maximal response to a full agonist. This difference between the pharmacology of full and partial agonists is well illustrated by results obtained with cannabinol, which is also a partial CB1 receptor agonist (reviewed in Pertwee, 1999), and with CP55940 in experiments in which an increase in the intestinal expression of CB1 receptors (and in intestinal inflammation) had been induced in mice by oral croton oil, the measured response being cannabinoid-induced CB1-receptor-mediated inhibition of upper gastrointestinal transit of a charcoal suspension (Izzo et al., 2001). It was found that this increase in CB1 expression level was accompanied not only by a leftward shift in the log dose–response curve of cannabinol but also by an increase in the size of its maximal effect. In contrast, CP55940, which has higher CB1 efficacy than cannabinol (reviewed in Pertwee, 1999), exhibited an increase in its potency but no change in its maximal effect. There has also been a recent report that in rats displaying signs of inflammatory thermal hyperalgesia in response to an intraplantar injection of complete Freund's adjuvant, CB1 expression in dorsal root ganglion neurons undergoes a transient elevation that is accompanied by a marked increase in the antinociceptive potency of the CB1-selective agonist, 2-arachidonyl-2-chloroethylamide, when this is injected directly into the inflamed paws (Amaya et al., 2006).
Tolerance to Δ9-THC
The density and coupling efficiencies of cannabinoid receptors can be affected not only by the location and nature of the cells that express them and by disease but also by exposure to a cannabinoid receptor ligand (reviewed in Sim-Selley, 2003; Lichtman and Martin, 2005; Childers, 2006). Thus, Δ9-THC, particularly when administered repeatedly, shares the ability of other CB1/CB2 receptor agonists to reduce CB1 receptor density and coupling efficiency in a manner that can give rise to tolerance to many of its in vivo effects, including memory disruption, decreased locomotion and antinociception. Interestingly, Δ9-THC appears to reduce CB1 receptor density and/or coupling efficiency more rapidly or to a greater extent in some rat and mouse brain areas (for example, hippocampus) than in others (for example, basal ganglia) (Breivogel et al., 1999; Sim-Selley and Martin, 2002). Moreover, compared to agonists with higher CB1 efficacy, it appears to be as effective in reducing CB1 receptor density, more effective at lowering CB1 coupling efficiency and much less effective at decreasing the number of CB1 receptors on the cell surface through internalization (Breivogel et al., 1999; Sim-Selley and Martin, 2002).
The production of tolerance by a cannabinoid receptor agonist when it is used as a medicine need not be disadvantageous since it may serve to widen the drug's therapeutic window. Thus there is evidence first, that tolerance develops less readily to some effects of a cannabinoid receptor agonist than to others (reviewed in Pertwee, 2004a; Lichtman and Martin, 2005) and second, that some sought-after therapeutic effects of a CB1 receptor agonist may be more resistant to tolerance development than some of its unwanted effects (De Vry et al., 2004). Since, in mice, Δ9-THC can induce tolerance to some (though not all) effects of exogenously administered anandamide (Wiley et al., 2005b), it may be that it has the capacity to render patients with certain disorders tolerant to this endocannabinoid when it is being released in a manner that is either protective or causing unwanted effects (reviewed in Pertwee, 2005b).
The CB1 and CB2 receptor pharmacology of CBD
The structure and stereochemistry of the phytocannabinoid, CBD, were first elucidated by Raphael Mechoulam in the 1960s who then went on to devise a method for its synthesis (reviewed in Pertwee, 2006). In contrast to Δ9-THC, CBD lacks detectable psychoactivity (reviewed in Pertwee, 2004b) and only displaces [3H]CP55940 from cannabinoid CB1 and CB2 receptors at concentrations in the micromolar range (Table 1). Since it displays such low affinity for these receptors, much pharmacological research with CBD has been directed at seeking out and characterizing CB1- and CB2-independent modes of action for this phytocannabinoid (Table 3). Recently, however, evidence has emerged that in spite of its low affinity for CB1 and CB2 receptors, CBD can interact with these receptors at reasonably low concentrations. This has come from the discovery that CBD is capable of antagonizing cannabinoid CB1/CB2 receptor agonists with apparent KB values in the low nanomolar range both in mouse whole-brain membranes and in membranes prepared from Chinese hamster ovary (CHO) cells transfected with hCB2 receptors (Thomas et al., 2007).
Table 3.
Some pharmacological actions of cannabidiol
| References | |
|---|---|
| Examples of actions induced by CBD at <1 μM | |
| The orphan receptor, GPR55 (B) | Pertwee (2007b), Ryberg et al. (2007) |
| Evoked human neutrophil migration (−) | McHugh and Ross (2005) |
| Basal microglial cell migration (+) | Walter et al. (2003) |
| Evoked microglial cell migration (−) | Walter et al. (2003) |
| Mitogen-induced release of interferon-γ (+) | a |
| Effects induced by CB1/CB2 receptor agonists (−) | b |
| Adenosine uptake by cultured microglia and macrophages (−) | Carrier et al. (2006) |
| Activation of the putative abnormal CBD receptor (±) | a |
| Ca2+ uptake by rat brain synaptosomes (−) | a |
| Delayed rectifier K+ and L-type Ca2+ currents (−) | a |
| Cytochrome P450 enzyme activity (−) | a |
| Membrane fluidity (+) | a |
| Examples of actions induced by CBD at 1–10 μM | |
| CB2 receptor constitutive activity (−) | b |
| TRPV1 receptor (A) | Bisogno et al. (2001) |
| Activation of α1-adrenoceptors and μ-opioid receptors (−) | Pertwee et al. (2002) |
| Cellular uptake of anandamide (−) | Rakhshan et al. (2000) |
| Cellular uptake of palmitoylethanolamide (−) | a |
| Synaptosomal uptake of noradrenaline, dopamine, 5-HT and γ-aminobutyric acid (−) | a |
| Ca2+ release from intracellular stores in rat hippocampal neurons and glia (+) | Drysdale et al. (2006) |
| Release of certain cytokines (±) | a |
| Cancer cell proliferation (−) | a |
| Human keratinocyte proliferation (−) | Wilkinson and Williamson (2007) |
| Signs of neuroprotection (+) | a |
| Oxidative stress (−) | a |
| Mg2+-ATPase activity (−) | a |
| Noradrenaline-induced melatonin biosynthesis (−) | Koch et al. (2006) |
| Lipoxygenase activity (−) | a |
| Phospholipase A2 activity (+) | a |
| Membrane stability (+) | a |
| Release of certain cytokines (±) | a |
| Examples of actions induced by CBD at >10 μM | |
| Choline uptake by rat hippocampal homogenates (−) | a |
| Cellular uptake and metabolism of anandamide (−) | Bisogno et al. (2001) |
| Release of certain cytokines (±) | a |
| Cyclooxygenase activity (−) | a |
| Allosteric modulation of μ- and δ-opioid receptors (−) | Kathmann et al. (2006) |
| 5-HT1A receptor (A) | Russo et al. (2005) |
Abbreviations: CBD, (−)-cannabidiol; 5-HT, 5-hydroxytryptamine; TRPV1, transient receptor potential vanilloid receptor 1; A, activation; B, antagonism; (+), increase induced; (−), decrease induced.
See reviews by Pertwee (2004b, 2005a) for references, further details and additional actions of CBD.
See text.
Turning first to the experiments performed in this investigation with brain membranes, these showed that the mean apparent KB values of CBD for antagonism of CP55940- and R-(+)-WIN55212-induced stimulation of [35S]GTPγS binding to these membranes are 79 and 138 nM, respectively, both well below the Ki value of CBD for its displacement of [3H]CP55940 from specific binding sites on these membranes (Table 1). In these experiments, CBD produced parallel dextral shifts in the log concentration–response curves of both agonists. Even so, the unexpectedly high potency with which these shifts were induced by CBD raises the possibility that this antagonism is non-competitive in nature. This hypothesis is supported by the finding that CBD can behave as a CB1 receptor ‘inverse agonist' at concentrations below those at which it undergoes significant binding to the CB1 orthosteric site. Thus, when administered by itself at a concentration (1 μM) at which it has been shown to antagonize CP559540 and R-(+)-WIN55212, CBD inhibits [35S]GTPγS binding to mouse brain membranes. CBD-induced inhibition of [35S]GTPγS binding has also been detected in hCB1-CHO cell membranes (MacLennan et al., 1998b; Thomas et al., 2007). No such inhibition was detected by Thomas et al. (2007) in untransfected CHO cell membranes, suggesting that the inverse effect of CBD in mouse brain tissue may be at least partly CB1 receptor mediated. It remains possible, however, that this inverse effect also has a CB1-receptor-independent component since CBD was found in the same investigation to be no less effective in inhibiting [35S]GTPγS binding to CB1−/− than to wild-type mouse brain membranes. Although the nature of this putative non-CB1 pharmacological target remains to be elucidated, there is already evidence that it is not present in all G-protein-coupled receptors as CBD does not reduce [35S]GTPγS binding to mouse brain membranes when this is being stimulated by the opioid receptor agonist, morphine (Thomas et al., 2007). The finding that CBD antagonizes CP55940 and R-(+)-WIN55212 in mouse brain and hCB1-CHO cell membrane experiments is consistent with previous reports first, that CBD at 10 μM antagonizes CP55940-induced stimulation of [35S]GTPγS binding to rat cerebellar membranes (Petitet et al., 1998) second, that it antagonizes CP55940 and R-(+)-WIN55212 in the mouse isolated vas deferens with apparent KB values in the low nanomolar range (Pertwee et al., 2002) and third, that it can block various in vivo responses to Δ9-THC in rabbits, rats, mice and human subjects (reviewed in Pertwee, 2004b).
Moving on to experiments performed with hCB2-CHO cell membranes, Thomas et al. (2007) found the mean apparent KB value of CBD for antagonism of CP55940 in the [35S]GTPγS-binding assay (65 nM) to be markedly less than its Ki value for displacing [3H]CP55940 from these membranes (Table 1). As in mouse brain membranes, so too in hCB2-CHO cell membranes CBD administered by itself inhibits [35S]GTPγS binding (MacLennan et al., 1998b; Thomas et al., 2007). Since it is inhibitory in this bioassay at 1 μM, the concentration at which it also antagonizes CP559540, it is possible that CBD produces this antagonism of CP55940 in a non-competitive manner by ‘physiologically' opposing the ability of this agonist to stimulate CB2 receptors. This hypothesis is supported by the findings first, that 1 μM CBD produces a marked downward displacement of the CP55940 log concentration–response curve in the [35S]GTPγS-binding assay and second, that this downward displacement appears to account entirely for this antagonism of CP55940 by CBD (Thomas et al., 2007). Further experiments are now required to establish whether CBD also behaves as an inverse agonist in a tissue in which CB2 receptors are expressed naturally and whether, as in brain experiments, there is any indication of an additional pharmacological target in such a tissue through which CBD can also act to produce signs of CB2 inverse agonism. If CBD does indeed interact with more than one target to produce its inverse effect in brain tissue and/or in a tissue that expresses CB2 receptors naturally, it will also be important to establish whether these interactions take place in an additive or synergistic manner.
That CBD can behave as a CB2 receptor inverse agonist may account, at least in part, for its well-documented anti-inflammatory properties (Pertwee, 2004b) as there is evidence that CB2 inverse agonism can inhibit immune cell migration and reduce clinical signs of inflammation (Lunn et al., 2006) and that CBD is a potent inhibitor of evoked migration in the Boyden chamber both of murine microglial cells and macrophages (Walter et al., 2003; Sacerdote et al., 2005) and of human neutrophils (McHugh and Ross, 2005). However, as indicated in Table 3 and elsewhere (Pertwee, 2004b), CBD has a number of other actions, some of which are also expected to reduce inflammation. Moreover, it has already been proposed that CBD modulates murine microglial cell migration by targeting the putative abnormal CBD receptor (Walter et al., 2003). Another possibility that CBD inhibits immune cell migration, at least in part, by activating CB2 receptors should also not be excluded at present, as CBD-induced inhibition of chemotaxis of murine macrophages can be prevented by SR144528 (Sacerdote et al., 2005) and CBD has been found to display high potency though low efficacy as an inhibitor of forskolin-stimulated cyclic AMP production by hCB2-expressing CHO cells (Gauson et al., 2007). Clearly, additional research is needed to establish which of the many actions of CBD contribute most to its anti-inflammatory effects. Also urgently required is further research directed at identifying the mechanisms that underlie some of the other potentially beneficial effects of CBD, for example its anticonvulsant, antipsychotic, anxiolytic, antiemetic, neuroprotective, anticancer and sleep-promoting effects (Pertwee, 2004b, 2005c; Parker et al., 2005).
The CB1 receptor pharmacology of Δ9-THCV
The discovery that the n-propyl analogue of Δ9-THC is a phytocannabinoid was made in 1970 by Edward Gill (Gill et al., 1970) who detected it in tincture of cannabis BPC, then a licensed medicine in the UK. This compound was subsequently named Δ9-THCV (Merkus, 1971). Initial pharmacological experiments with Δ9-THCV showed first, that it shares the ability of Δ9-THC to produce signs of catalepsy in the mouse ring test (Gill et al., 1970) and second, that it can induce Δ9-THC-like effects in humans (Hollister, 1974), albeit with a potency in mouse and human four or five times less than that of Δ9-THC. Much more recently, experiments with mice have confirmed that synthetic Δ9-THCV (O-4394) resembles Δ9-THC not only in producing cataleptic behaviour in the ring test but also in producing antinociception in the tail-flick test (Pertwee et al., 2007b). As in the earlier experiments with Δ9-THCV extracted from cannabis (eΔ9-THCV), O-4394 exhibits less potency than Δ9-THC in these bioassays. Pertwee et al. (2007b) also found that the antinociceptive effect of O-4394 could be attenuated by SR141716A at a dose (3 mg kg−1 intraperitoneal) at which this antagonist is expected to target CB1 receptors in a selective manner and at which it also opposes Δ9-THC-induced antinociception. It seems likely, therefore, that Δ9-THCV can activate CB1 receptors in vivo, albeit with less potency than Δ9-THC. This hypothesis is consistent with structure–activity data indicating that the potency/efficacy of Δ9-THC as a CB1 receptor agonist can be greatly influenced by the length and conformation of its C-3 side chain (Howlett et al., 2002). It is also supported by findings that both eΔ9-THCV and O-4394 can displace [3H]CP55940 from specific sites on mouse brain membranes and that their CB1 Ki values are slightly greater than some reported CB1 Ki values of Δ9-THC (Table 1).
Although Δ9-THCV seems to be capable of eliciting CB1-receptor-mediated responses in vivo, there is also evidence that it can behave as a CB1 receptor antagonist both in vivo and in vitro. Thus, when administered to mice in vivo at doses below those at which it produces signs of CB1 receptor agonism, O-4394 has been found to block effects of Δ9-THC that are thought to be CB1 receptor mediated. Moreover, when administered in vitro, both O-4394 and eΔ9-THCV antagonize established CB1/CB2 receptor agonists in a surmountable manner (Thomas et al., 2005; Pertwee et al., 2007b). More specifically, O-4394 has been found to attenuate Δ9-THC-induced hypothermia at 0.3 and 3 mg kg−1 i.v. and Δ9-THC-induced antinociception in the tail-flick test at 3 mg kg−1 i.v., and both O-4394 and eΔ9-THCV antagonize CP55940-induced stimulation of [35S]GTPγS binding to mouse whole-brain membranes with mean apparent KB values (82 and 93 nM, respectively) that do not deviate significantly from their CB1 Ki values for displacement of [3H]CP55940 from these membranes (Table 1; Thomas et al., 2005; Pertwee et al., 2007b). In contrast to SR141716A and CBD (Thomas et al., 2007), Δ9-THCV (O-4394) lacks detectable inverse agonist activity in the [35S]GTPγS-binding assay performed with mouse whole-brain membranes and also fails to produce any detectable stimulation of [35S]GTPγS binding to such membranes (Pertwee et al., 2007b). Even so, it would be premature to conclude that Δ9-THCV lacks significant efficacy as a CB1 receptor inverse or partial agonist until its actions have been investigated in other in vitro bioassays that display greater sensitivity than the [35S]GTPγS-binding assay to ligands of this kind.
Why O-4394 behaves in vivo as a CB1 receptor antagonist at doses of 3 mg kg−1 i.v. or less but as a CB1 receptor agonist at doses of 10 mg kg−1 i.v. or more remains to be established. Since it does not display detectable CB1 receptor efficacy in vitro, at least in the [35S]GTPγS-binding assay, one possibility is that O-4394 is metabolized in vivo to a compound that possesses significant efficacy as a cannabinoid receptor agonist and that the parent compound itself lacks such efficacy. Given the structural similarities between Δ9-THC and Δ9-THCV (Figure 1), this hypothesis is supported by evidence first, that Δ9-THC exhibits markedly less potency in vivo as a CB1 receptor agonist than its 11-hydroxy metabolite (Lemberger et al., 1973; Wilson and May, 1975; Watanabe et al., 1990) and second, that Δ9-THCV can undergo metabolism to an 11-hydroxy metabolite (Brown and Harvey, 1988).
There is evidence that like established CB1 receptor antagonists such as SR141716A and AM251 (reviewed in Pertwee, 2005b), Δ9-THCV can block CB1-mediated effects of endogenously released endocannabinoids when administered in vivo. This evidence has come from recent experiments showing that eΔ9-THCV shares the ability of AM251 to reduce the food intake and body weight of non-fasted and fasted ‘non-obese' mice when administered once (Robinson et al., 2007) and of dietary-induced obese mice when given repeatedly over 28 days (Cawthorne et al., 2007). It has also been found that like AM251, eΔ9-THCV can reduce the body fat content and plasma leptin concentration and increase the 24-h energy expenditure and thermic response to food of dietary-induced obese mice (Cawthorne et al., 2007), the data obtained suggesting that eΔ9-THCV produces its antiobesity effects more by increasing energy expenditure than by reducing food intake. In addition, both eΔ9-THCV and AM251 have been shown to reduce the time that ‘non-obese' mice spend close to a food hopper (Robinson et al., 2007). These experiments were prompted by conclusive evidence that established CB1 receptor antagonists suppress feeding and body weight in animals and humans (reviewed in Matias and Di Marzo, 2007) and by the introduction into the clinic of SR141716A (rimonabant; Acomplia, Sanofi-Aventis, Paris, France) in 2006 as an antiobesity agent. Further research is now required to determine whether Δ9-THCV would also be effective as a medicine for the management of obesity, and indeed for drug-dependence therapy, experiments with drug-dependent animals and human subjects having shown that CB1 receptor blockade can reduce signs of drug dependence and the incidence of relapse after drug withdrawal (reviewed in Le Foll and Goldberg, 2005).
Additional in vitro evidence that Δ9-THCV can block the activation of neuronal CB1 receptors has come recently from experiments with murine cerebellar slices (Ma et al., 2006). The results obtained suggest first, that eΔ9-THCV can block CB1-mediated inhibition of GABA release from basket-cell interneurons caused by R-(+)-WIN55212 and second, that by itself eΔ9-THCV shares the ability of the CB1 receptor antagonist/inverse agonist, AM251, to increase GABA release from these neurons. These effects were observed at a concentration (5.8 μM) below any at which eΔ9-THCV has been found to induce signs of inverse agonism in the [35S]GTPγS-binding assay when this is performed with murine cerebellar membranes (Dennis et al., 2007). It will now be important to establish whether eΔ9-THCV is increasing GABA release by opposing activation of basket-cell CB1 receptors by endogenously released endocannabinoid molecules, not least because such an effect could explain why eΔ9-THCV has also been found to disrupt the spread of epileptiform activity induced in rat piriform cortical slices by Mg2+-free Krebs medium (Weston et al., 2006), an observation that does of course raise the possibility that Δ9-THCV may display anticonvulsant activity in vivo.
The discovery that Δ9-THCV can antagonize cannabinoid receptor agonists was made in experiments with the mouse isolated vas deferens (Thomas et al., 2005), a tissue in which such agonists are thought to inhibit electrically evoked contractions by acting on prejunctional neuronal CB1 receptors to inhibit contractile transmitter release (Howlett et al., 2002). These experiments showed eΔ9-THCV to behave as a competitive surmountable antagonist of CP55940 and other established cannabinoid receptor agonists at a concentration (100 nM) at which it did not affect clonidine- or capsaicin-induced inhibition of evoked contractions of the vas deferens or produce any sign of CB1 receptor activation or inverse agonism. Unexpectedly, the antagonism displayed by eΔ9-THCV in the vas deferens was found to be ligand dependent. Thus, the mean apparent KB values of eΔ9-THCV for its antagonism of anandamide, R-(+)-WIN55212, methanandamide, CP55940 and Δ9-THC were 1.2, 1.5, 4.6, 10.3 and 96.7 nM, respectively. The mean apparent KB values of eΔ9-THCV for its antagonism of anandamide, R-(+)-WIN55212, methanandamide and CP55940 in this tissue preparation are significantly less than the Ki values of eΔ9-THCV for its displacement of [3H]CP55940 from mouse brain membranes (Thomas et al., 2005). So too is the apparent KB value of O-4394 against R-(+)-WIN55212 in the vas deferens (4.8 nM) (Pertwee et al., 2007b). The questions of why Δ9-THCV exhibits such potency as an antagonist of these cannabinoid receptor agonists in the vas deferens and of why it produces antagonism in this tissue that is ligand-dependent have yet to be answered.
The finding that Δ9-THCV exhibits less potency against CP55940 or R-(+)-WIN55212 in mouse whole-brain membranes than in the vas deferens (Thomas et al., 2005; Pertwee et al., 2007b) indicates that it displays not only agonist dependence as an antagonist, but also tissue dependence. Further evidence for such tissue dependence was recently obtained by Dennis et al. (2007), who found that eΔ9-THCV antagonizes R-(+)-WIN55212-induced stimulation of [35S]GTPγS binding more potently in mouse cerebellar membranes (apparent KB=7 nM) than in mouse piriform cortical membranes (apparent KB=54 nM). Clearly, further experiments are now required to establish why eΔ9-THCV does not display the same potency against CP55940 or R-(+)-WIN55212 in all CB1-expressing tissues and brain areas. It will also be important to investigate why, according to Schild analysis, Δ9-THCV appears to antagonize R-(+)-WIN55212 competitively in the mouse isolated vas deferens (Thomas et al., 2005) but non-competitively in both mouse cerebellar and piriform cortical membranes (Dennis et al., 2007).
The CB2 receptor pharmacology of Δ9-THCV
(−)-trans-Δ9-Tetrahydrocannabivarin targets not only CB1 but also CB2 receptors, and indeed, like Δ9-THC, appears to bind equally well to both these receptor types (Table 1). Moreover, as in experiments performed with mouse brain membranes, so too in experiments with hCB2-CHO cell membranes, eΔ9-THCV has been found to antagonize CP55940 in the [35S]GTPγS-binding assay in a surmountable manner (Thomas et al., 2005). In contrast to the brain membrane data, however, results obtained from the experiments performed with hCB2-CHO cell membranes indicate that the mean apparent KB value of eΔ9-THCV for its antagonism of CP55940 (10.1 nM) is significantly less than its hCB2 Ki value for displacement of [3H]CP55940 from these membranes (Table 1). At the concentration at which it produces this antagonism (1 μM), or indeed at 10 μM, eΔ9-THCV administered by itself does not affect [35S]GTPγS binding to the hCB2-CHO cell membranes (RG Pertwee and A Thomas, unpublished), suggesting that in contrast to CBD (Thomas et al., 2007), the unexpectedly high potency that eΔ9-THCV displays as a CB2 receptor antagonist in vitro does not stem from any ability to counteract CP55940-induced stimulation of [35S]GTPγS binding non-competitively through a direct inhibitory effect on CB2 receptor signalling.
Although Δ9-THCV may not be a CB2 receptor inverse agonist, evidence has emerged recently that it is a CB2 receptor partial agonist. This came from experiments with eΔ9-THCV in which the measured response used to indicate CB2 receptor activation was inhibition of forskolin-induced stimulation of cyclic AMP production by hCB2-CHO cells (Gauson et al., 2007). This is a bioassay that detects cannabinoid receptor activation with greater sensitivity than the [35S]GTPγS-binding assay, probably because adenylate cyclase is located further along the cannabinoid receptor signalling cascade than G protein (reviewed in Pertwee, 1999; Howlett et al., 2002). Additional experiments are now required to establish whether Δ9-THCV also activates CB2 receptors in vivo. If it does, then it will be important to determine whether Δ9-THCV is effective against chronic liver diseases, there being evidence that one effective strategy for managing these disorders in the clinic may be to administer a medicine that simultaneously blocks CB1 receptors and activates CB2 receptors (Mallat et al., 2007).
Non-CB1, non-CB2 pharmacological targets for Δ9-THC, CBD and Δ9-THCV
Although there is no doubt that Δ9-THC and CBD can target both CB1 and CB2 receptors, there is also general agreement that they have a number of additional pharmacological actions (Tables 3 and 4). These include several actions that can be elicited by these cannabinoids at submicromolar concentrations and are, therefore, expected to reduce the selectivity of these compounds as CB1 and CB2 receptor ligands. One finding of particular interest is that the orphan receptor, GPR55 is activated by Δ9-THC and blocked by CBD (Tables 3 and 4). It will now be important to seek out effects that are mediated by GPR55 in both health and disease and to identify any potential therapeutic benefits of activating or blocking this receptor with Δ9-THC, CBD or other ligands. The extent to which Δ9-THCV can induce CB1- and CB2-receptor-independent effects remains to be established.
Table 4.
Some CB1- and CB2-receptor-independent actions of Δ9-THC
| References | |
|---|---|
| Examples of actions induced by Δ9-THC at <1 μM | |
| The orphan receptor, GPR55 (A) | Pertwee (2007b), Ryberg et al. (2007) |
| Conductance in ligand-gated ion channels of 5-HT3 receptors (−) | a |
| Conductance in ligand-gated ion channels of glycine receptors (P) | Hejazi et al. (2006) |
| Peroxisome proliferator-activated receptor gamma (A) | O'Sullivan et al. (2005) |
| Putative non-CB1, non-CB2, non-TRPV1 receptors on capsaicin-sensitive perivascular sensory neurons mediating CGRP release (+) | Zygmunt et al. (2002) |
| Adenosine uptake by cultured microglia and macrophages (−) | Carrier et al. (2006) |
| Synaptosomal uptake of noradrenaline (+) | b |
| Synaptosomal uptake of dopamine (±) | b |
| Synaptosomal uptake of 5-HT (−) | b |
| Examples of actions induced by Δ9-THC at 1–10 μM | |
| Conductance in voltage-gated Na+ channels (−) | a |
| Conductance in Kv1.2 K+ voltage-gated channels (−) | a |
| Conductance in gap junctions between cells (−) | a |
| Oxidative stress (−) | a |
| Na+-K+-ATPase activity (−) | b |
| Mg2+-ATPase activity (±) | b |
| Noradrenaline-induced melatonin biosynthesis (−) | Koch et al. (2006) |
| Human keratinocyte proliferation (−) | Wilkinson and Williamson (2007) |
| Cellular uptake of anandamide (−) | Rakhshan et al. (2000) |
| Synaptosomal uptake of 5-HT (+) | b |
| Synaptosomal uptake of noradrenaline, γ-aminobutyric acid and choline (−) | b |
| Synaptic conversion of tyrosine to noradrenaline and dopamine (+) | b |
| Fluidity of synaptic plasma membranes (+) | b |
| Monoamine oxidase activity (−) | b |
| Examples of actions induced by Δ9-THC at >10 μM | |
| TRPA1 receptors (A) | a |
| Allosteric modulation of μ- and δ-opioid receptors (−) | Kathmann et al. (2006) |
Abbreviations: CGRP, calcitonin gene-related peptide; 5-HT, 5-hydroxytryptamine; Δ9-THC, (−)-trans-Δ9-tetrahydrocannabinol; TRPV1, transient receptor potential vanilloid receptor 1; A, activation; P, potentiation; (+), increase induced; (−), decrease induced.
See review by Oz (2006) for references and further details.
See review by Pertwee (1988) for references, further details and additional actions of Δ9-THC.
Some non-CB1, non-CB2 actions of Δ9-THC can also be produced by certain other cannabinoid receptor agonists at concentrations of 1 μM or less. For example, like Δ9-THC, both anandamide and 2-arachidonoylglycerol can activate GPR55 (Ryberg et al., 2007) and modulate conductance in ligand-gated ion channels of glycine receptors (reviewed in Oz, 2006), and the phytocannabinoid, cannabinol, can activate putative non-CB1, non-CB2, non-transient receptor potential vanilloid receptor 1 (non-TRPV1) peripheral neuronal receptors, though 11-hydroxy-Δ9-THC, Δ9-THC-11-oic acid, HU-210 and CP55940 cannot (Zygmunt et al., 2002). Some cannabinoids have been found to share the ability of Δ9-THC to reduce conductance in ligand-gated ion channels of human 5-HT3A receptors at submicromolar concentrations (Barann et al., 2002). Importantly, Δ9-THC is the most potent of these cannabinoids as an inhibitor of these ion channels, the rank order of potency being Δ9-THC>R-(+)-WIN55212>anandamide>(2-methyl-1-propyl-1H-indol-3-yl)-1-naphthalenylmethanone>CP55940, and consequently quite unlike that for CB1 or CB2 receptor agonism. It is also known that Δ9-THC-like antioxidant activity is exhibited by several other phenolic cannabinoids, for example CBD (Table 3) and HU-210 (reviewed in Pertwee, 2005a).
In addition, there is the possibility that Δ9-THC may share actions that have so far only been shown to be exhibited by other CB1/CB2 receptor agonists (reviewed in Pertwee, 2004c, 2005a). These include the ability of
HU-210 to increase 5-HT binding to the 5-HT2 receptor (Cheer et al., 1999);
CP55940 and R-(+)-WIN55212 to activate central putative non-CB1, non-CB2, TRPV1-like receptors (Hájos and Freund, 2002);
CP55940, R-(+)-WIN55212 and anandamide to activate putative non-I1, non-I2 imidazoline neuronal receptors (Göthert et al., 1999; Molderings et al., 2002);
anandamide to activate putative non-CB1, non-CB2, non-TRPV1 neuronal receptors in guinea-pig small intestine (Mang et al., 2001);
anandamide and R-(+)-methanandamide to bind to sites on muscarinic M1 and M4 receptors (Christopoulos and Wilson, 2001) and
R-(+)-WIN55212, anandamide and/or 2-arachidonoylglycerol to modulate ion currents in various voltage-gated or ligand-gated ion channels (reviewed in Oz, 2006).
There is already evidence, however, that Δ9-THC does not share the ability of anandamide to activate TRPV1 receptors (Lam et al., 2005) or the putative abnormal CBD receptor (reviewed in Pertwee, 2004c, 2005a). Nor does it seem to share the ability of R-(+)-WIN55212 and anandamide to activate non-CB1, non-CB2 G-protein-coupled receptors that appear to be expressed in the brains of CB1 receptor knockout mice (Breivogel et al., 2001; Monory et al., 2002).
Future directions
It is now well established that Δ9-THC is a cannabinoid CB1 and CB2 receptor partial agonist and that depending on the expression level and coupling efficiency of these receptors it will either activate them or block their activation by other cannabinoids. Further research is now required to establish in greater detail the extent to which the in vivo pharmacology of Δ9-THC is shaped by these opposing actions both in healthy organisms, for example following a decrease in cannabinoid receptor density or signalling caused by prior cannabinoid administration, and in animal disease models or human disorders in which upward or downward changes in CB1/CB2 receptor expression, CB1/CB2-receptor-coupling efficiency and/or in endocannabinoid release onto CB1 or CB2 receptors have occurred in cells or tissues that mediate unwanted effects or determine syndrome/disease progression. The extent to which the balance between cannabinoid receptor agonism and antagonism following in vivo administration of Δ9-THC is influenced by the conversion of this cannabinoid into the more potent cannabinoid receptor agonist, 11-OH-Δ9-THC, also merits investigation.
Turning now to CBD, an important recent finding is that this cannabinoid displays unexpectedly high potency as a CB2 receptor antagonist and that this antagonism stems mainly from its ability to induce inverse agonism at this receptor and is, therefore, essentially non-competitive in nature. Evidence that CB2 receptor inverse agonism can ameliorate inflammation through inhibition of immune cell migration and that CBD can potently inhibit evoked immune cell migration in the Boyden chamber raises the possibility that CBD is a lead compound from which a selective and more potent CB2 receptor inverse agonist might be developed as a new class of anti-inflammatory agent. When exploring this possibility it will be important to establish the extent to which CBD modulates immune cell migration through other pharmacological mechanisms. There is also a need for further research directed at identifying the mechanisms by which CBD induces signs of inverse agonism not only in CB2-expressing cells but also in brain membranes and in the mouse isolated vas deferens.
Important recent findings with Δ9-THCV have been that it can induce both CB1 receptor antagonism in vivo and in vitro and signs of CB2 receptor activation in vitro at concentrations in the low nanomolar range. Further research is now required to establish whether this phytocannabinoid also behaves as a potent CB2 receptor agonist in vivo. Thus, a medicine that blocks CB1 receptors but activates CB2 receptors has potential for the management of certain disorders that include chronic liver disease and also obesity when this is associated with inflammation. The bases for the ligand and tissue dependency that Δ9-THCV displays as an antagonist of CB1/CB2 receptor agonists in vitro also warrant further research. In addition, in view of the structural similarity of Δ9-THCV to Δ9-THC, it will be important to determine the extent to which Δ9-THCV shares the ability of Δ9-THC, and indeed of CBD, to interact with pharmacological targets other than CB1 or CB2 receptors at concentrations in the nanomolar or low micromolar range. It will also be important to establish the extent to which CB1- and CB2-receptor-independent actions contribute to the overall in vivo pharmacology of each of these phytocannabinoids and give rise to differences between the in vivo pharmacology of Δ9-THC or Δ9-THCV and other cannabinoid receptor ligands such as CP55940, R-(+)-WIN55212 and SR141716A.
Finally, cannabis is a source not only of Δ9-THC, CBD and Δ9-THCV but also of at least 67 other phytocannabinoids and as such can be regarded as a natural library of unique compounds. The therapeutic potential of many of these ligands still remains largely unexplored prompting a need for further preclinical and clinical research directed at establishing whether phytocannabinoids are indeed ‘a neglected pharmacological treasure trove' (Mechoulam, 2005). As well as leading to a more complete exploitation of Δ9-THC and CBD as therapeutic agents and establishing the clinical potential of Δ9-THCV more clearly, such research should help to identify any other phytocannabinoids that have therapeutic applications per se or that constitute either prodrugs from which semisynthetic medicines might be manufactured or lead compounds from which wholly synthetic medicines might be developed.
Acknowledgments
The writing of this review was supported by grants from the National Institute on Drug Abuse (NIDA) (DA-09789), the Biotechnology and Biological Sciences Research Council (BBSRC) and GW Pharmaceuticals.
Abbreviations
- AM251
N-(piperidin-1-yl)-5-(4-iodophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazole-3-carboxamide
- CBD
(−)-cannabidiol
- CHO
Chinese hamster ovary
- CP55940
(−)-cis-3-[2-hydroxy-4-(1,1-dimethylheptyl)phenyl]-trans-4-(3-hydroxypropyl)cyclohexanol
- EAE
experimental autoimmune encephalomyelitis
- GABA
γ-aminobutyric acid
- GTPγS
guanosine-5′-O-(3-thiotriphosphate)
- HU-210
(6aR)-trans-3-(1,1-dimethylheptyl)-6a,7,10,10a-tetrahydro-1-hydroxy-6,6-dimethyl-6H-dibenzo[b,d]pyran-9-methanol
- O-4394
synthetic Δ9-tetrahydrocannabivarin
- R-(+)-WIN55212
(R)-(+)-[2,3-dihydro-5-methyl-3-(4-morpholinylmethyl)pyrrolo-[1,2,3-de]-1,4-benzoxazin-6-yl]-1-naphthalenylmethanone
- SR141716A
N-(piperidin-1-yl)-5-(4-chlorophenyl)-1-(2,4-dichlorophenyl)-4-methyl-1H-pyrazole-3-carboxamide hydrochloride
- SR144528
N-[(1S)-endo-1,3,3-trimethyl bicyclo [2.2.1] heptan-2-yl]-5-(4-chloro-3-methylphenyl)-1-(4-methylbenzyl)-pyrazole-3-carboxamide
- THC
tetrahydrocannabinol
- THCV
tetrahydrocannabivarin
- TRPV1
transient receptor potential vanilloid receptor 1
Conflict of interest
The author states no conflict of interest.
References
- Aguado T, Carracedo A, Julien B, Velasco G, Milman G, Mechoulam R, et al. Cannabinoids induce glioma stem-like cell differentiation and inhibit gliomagenesis. J Biol Chem. 2007;282:6854–6862. doi: 10.1074/jbc.M608900200. [DOI] [PubMed] [Google Scholar]
- Amaya F, Shimosato G, Kawasaki Y, Hashimoto S, Tanaka Y, Ji R-R, et al. Induction of CB1 cannabinoid receptor by inflammation in primary afferent neurons facilitates antihyperalgesic effect of peripheral CB1 agonist. Pain. 2006;124:175–183. doi: 10.1016/j.pain.2006.04.001. [DOI] [PubMed] [Google Scholar]
- Barann M, Molderings G, Brüss M, Bönisch H, Urban BW, Göthert M. Direct inhibition by cannabinoids of human 5-HT3A receptors: probable involvement of an allosteric modulatory site. Br J Pharmacol. 2002;137:589–596. doi: 10.1038/sj.bjp.0704829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayewitch M, Rhee M-H, Avidor-Reiss T, Breuer A, Mechoulam R, Vogel Z. Δ9-Tetrahydrocannabinol antagonizes the peripheral cannabinoid receptor-mediated inhibition of adenylyl cyclase. J Biol Chem. 1996;271:9902–9905. doi: 10.1074/jbc.271.17.9902. [DOI] [PubMed] [Google Scholar]
- Beltramo M, Bernardini N, Bertorelli R, Campanella M, Nicolussi E, Fredduzzi S, et al. CB2 receptor-mediated antihyperalgesia: possible direct involvement of neural mechanisms. Eur J Neurosci. 2006;23:1530–1538. doi: 10.1111/j.1460-9568.2006.04684.x. [DOI] [PubMed] [Google Scholar]
- Berrendero F, Maldonado R. Involvement of the opioid system in the anxiolytic-like effects induced by Δ9-tetrahydrocannabinol. Psychopharmacology. 2002;163:111–117. doi: 10.1007/s00213-002-1144-9. [DOI] [PubMed] [Google Scholar]
- Berrendero F, Sánchez A, Cabranes A, Puerta C, Ramos JA, García-Merino A, et al. Changes in cannabinoid CB1 receptors in striatal and cortical regions of rats with experimental allergic encephalomyelitis, an animal model of multiple sclerosis. Synapse. 2001;41:195–202. doi: 10.1002/syn.1075. [DOI] [PubMed] [Google Scholar]
- Bifulco M, Laezza C, Gazzerro P, Pentimalli F. Endocannabinoids as emerging suppressors of angiogenesis and tumor invasion (review) Oncol Rep. 2007;17:813–816. [PubMed] [Google Scholar]
- Bisogno T, Hanus L, De Petrocellis L, Tchilibon S, Ponde DE, Brandi I, et al. Molecular targets for cannabidiol and its synthetic analogues: effect on vanilloid VR1 receptors and on the cellular uptake and enzymatic hydrolysis of anandamide. Br J Pharmacol. 2001;134:845–852. doi: 10.1038/sj.bjp.0704327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blázquez C, Carracedo A, Barrado L, Real PJ, Fernández-Luna JL, Velasco G, et al. Cannabinoid receptors as novel targets for the treatment of melanoma. FASEB J. 2006;20:2633–2635. doi: 10.1096/fj.06-6638fje. [DOI] [PubMed] [Google Scholar]
- Braida D, Iosuè S, Pegorini S, Sala M. Δ9-Tetrahydrocannabinol-induced conditioned place preference and intracerebroventricular self-administration in rats. Eur J Pharmacol. 2004;506:63–69. doi: 10.1016/j.ejphar.2004.10.043. [DOI] [PubMed] [Google Scholar]
- Braida D, Limonta V, Malabarba L, Zani A, Sala M. 5-HT1A receptors are involved in the anxiolytic effect of Δ9-tetrahydrocannabinol and AM 404, the anandamide transport inhibitor, in Sprague–Dawley rats. Eur J Pharmacol. 2007;555:156–163. doi: 10.1016/j.ejphar.2006.10.038. [DOI] [PubMed] [Google Scholar]
- Breivogel CS, Childers SR, Deadwyler SA, Hampson RE, Vogt LJ, Sim Selley LJ. Chronic Δ9-tetrahydrocannabinol treatment produces a time-dependent loss of cannabinoid receptors and cannabinoid receptor-activated G proteins in rat brain. J Neurochem. 1999;73:2447–2459. doi: 10.1046/j.1471-4159.1999.0732447.x. [DOI] [PubMed] [Google Scholar]
- Breivogel CS, Griffin G, Di Marzo V, Martin BR. Evidence for a new G protein-coupled cannabinoid receptor in mouse brain. Mol Pharmacol. 2001;60:155–163. [PubMed] [Google Scholar]
- Brown N, Harvey D. In vivo metabolism of the n-propyl homologues of delta-8- and delta-9-tetrahydrocannabinol in the mouse. Biomed Environ Mass Spectrom. 1988;15:403–410. doi: 10.1002/bms.1200150708. [DOI] [PubMed] [Google Scholar]
- Busch-Petersen J, Hill WA, Fan P, Khanolkar A, Xie X-Q, Tius MA, et al. Unsaturated side chain β-11-hydroxyhexahydrocannabinol analogs. J Med Chem. 1996;39:3790–3796. doi: 10.1021/jm950934b. [DOI] [PubMed] [Google Scholar]
- Cabral GA, Staab A.Effects on the immune system Cannabinoids. Handbook of Experimental Pharmacology 2005Springer-Verlag: Heidelberg; 385–423.In: Pertwee RG (ed).vol. 168. [DOI] [PubMed] [Google Scholar]
- Cabranes A, Pryce G, Baker D, Fernández-Ruiz J. Changes in CB1 receptors in motor-related brain structures of chronic relapsing experimental allergic encephalomyelitis mice. Brain Res. 2006;1107:199–205. doi: 10.1016/j.brainres.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Carracedo A, Gironella M, Lorente M, Garcia S, Guzmán M, Velasco G, et al. Cannabinoids induce apoptosis of pancreatic tumor cells via endoplasmic reticulum stress-related genes. Cancer Res. 2006;66:6748–6755. doi: 10.1158/0008-5472.CAN-06-0169. [DOI] [PubMed] [Google Scholar]
- Carrier EJ, Auchampach JA, Hillard CJ. Inhibition of an equilibrative nucleoside transporter by cannabidiol: a mechanism of cannabinoid immunosuppression. Proc Natl Acad Sci USA. 2006;103:7895–7900. doi: 10.1073/pnas.0511232103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cawthorne MA, Wargent E, Zaibi M, Stott C, Wright S.The CB-1 antagonist, delta-9-tetrahydrocannabivarin (THCV) has anti-obesity activity in dietary-induced obese (DIO) mice Symposium on the Cannabinoids 2007Burlington, Vermont, USA; International Cannabinoid Research Society, p 141 [Google Scholar]
- Cheer JF, Cadogan A-K, Marsden CA, Fone KCF, Kendall DA. Modification of 5-HT2 receptor mediated behaviour in the rat by oleamide and the role of cannabinoid receptors. Neuropharmacology. 1999;38:533–541. doi: 10.1016/s0028-3908(98)00208-1. [DOI] [PubMed] [Google Scholar]
- Childers SR. Activation of G-proteins in brain by endogenous and exogenous cannabinoids. AAPS J. 2006;8:E112–E117. doi: 10.1208/aapsj080113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu P, Olsen DM, Borys HK, Karler R, Turkanis SA. The influence of cannabidiol and Δ9-tetrahydrocannabinol on cobalt epilepsy in rats. Epilepsia. 1979;20:365–375. doi: 10.1111/j.1528-1157.1979.tb04816.x. [DOI] [PubMed] [Google Scholar]
- Christopoulos A, Wilson K. Interaction of anandamide with the M1 and M4 muscarinic acetylcholine receptors. Brain Res. 2001;915:70–78. doi: 10.1016/s0006-8993(01)02825-6. [DOI] [PubMed] [Google Scholar]
- Colasanti BK, Lindamood C, Craig CR. Effects of marihuana cannabinoids on seizure in cobalt-epileptic rats. Pharmacol Biochem Behav. 1982;16:573–578. doi: 10.1016/0091-3057(82)90418-x. [DOI] [PubMed] [Google Scholar]
- Darmani NA, Crim JL. Delta-9-tetrahydrocannabinol differentially suppresses emesis versus enhanced locomotor activity produced by chemically diverse dopamine D2/D3 receptor agonists in the least shrew (Cryptotis parva) Pharmacol Biochem Behav. 2005;80:35–44. doi: 10.1016/j.pbb.2004.10.019. [DOI] [PubMed] [Google Scholar]
- Darmani NA, Johnson JC. Central and peripheral mechanisms contribute to the antiemetic actions of delta-9-tetrahydrocannabinol against 5-hydroxytryptophan-induced emesis. Eur J Pharmacol. 2004;488:201–212. doi: 10.1016/j.ejphar.2004.02.018. [DOI] [PubMed] [Google Scholar]
- De Vry J, Jentzsch KR, Kuhl E, Eckel G. Behavioral effects of cannabinoids show differential sensitivity to cannabinoid receptor blockade and tolerance development. Behav Pharmacol. 2004;15:1–12. doi: 10.1097/00008877-200402000-00001. [DOI] [PubMed] [Google Scholar]
- Dennis I, Whalley B, Stephens G.Effects of cannabinoids on [35S]GTPγS binding in specific regions of the mouse brain 2007. Poster P041 at the Joint Focused Meeting/3rd European Workshop on Cannabinoid Research, University of Nottingham, UK, 20 and 21 April 2007. Focused Meeting of the British Pharmacological Society
- Devane WA, Hanus L, Breuer A, Pertwee RG, Stevenson LA, Griffin G, et al. Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science. 1992;258:1946–1949. doi: 10.1126/science.1470919. [DOI] [PubMed] [Google Scholar]
- Dewey WL. Cannabinoid pharmacology. Pharmacol Rev. 1986;38:151–178. [PubMed] [Google Scholar]
- Di Marzo V, Breivogel CS, Tao Q, Bridgen DT, Razdan RK, Zimmer AM, et al. Levels, metabolism, and pharmacological activity of anandamide in CB1 cannabinoid receptor knockout mice: evidence for non-CB1, non-CB2 receptor-mediated actions of anandamide in mouse brain. J Neurochem. 2000;75:2434–2444. doi: 10.1046/j.1471-4159.2000.0752434.x. [DOI] [PubMed] [Google Scholar]
- Di Marzo V, De Petrocellis L, Bisogno T.The biosynthesis, fate and pharmacological properties of endocannabinoids Cannabinoids. Handbook of Experimental Pharmacology 2005Springer-Verlag: Heidelberg; 147–185.In: Pertwee RG (ed).Vol 168. [DOI] [PubMed] [Google Scholar]
- Drysdale AJ, Ryan D, Pertwee RG, Platt B. Cannabidiol-induced intracellular Ca2+ elevations in hippocampal cells. Neuropharmacology. 2006;50:621–631. doi: 10.1016/j.neuropharm.2005.11.008. [DOI] [PubMed] [Google Scholar]
- Felder CC, Joyce KE, Briley EM, Mansouri J, Mackie K, Blond O, et al. Comparison of the pharmacology and signal transduction of the human cannabinoid CB1 and CB2 receptors. Mol Pharmacol. 1995;48:443–450. [PubMed] [Google Scholar]
- Fish BS, Consroe P, Fox RR. Convulsant–anticonvulsant properties of delta-9-tetrahydrocannabinol in rabbits. Behav Genet. 1983;13:205–211. doi: 10.1007/BF01065669. [DOI] [PubMed] [Google Scholar]
- Fox A, Bevan S. Therapeutic potential of cannabinoid receptor agonists as analgesic agents. Expert Opin Investig Drugs. 2005;14:695–703. doi: 10.1517/13543784.14.6.695. [DOI] [PubMed] [Google Scholar]
- Gardner EL. Endocannabinoid signaling system and brain reward: emphasis on dopamine. Pharmacol Biochem Behav. 2005;81:263–284. doi: 10.1016/j.pbb.2005.01.032. [DOI] [PubMed] [Google Scholar]
- Gauson LA, Stevenson LA, Thomas A, Baillie GL, Ross RA, Pertwee RG.Cannabigerol behaves as a partial agonist at both CB1 and CB2 receptors Symposium on the Cannabinoids 2007Burlington, Vermont, USA; International Cannabinoid Research Society, p 206 [Google Scholar]
- Gill EW, Paton WDM, Pertwee RG. Preliminary experiments on the chemistry and pharmacology of cannabis. Nature. 1970;228:134–136. doi: 10.1038/228134a0. [DOI] [PubMed] [Google Scholar]
- Gong J-P, Onaivi ES, Ishiguro H, Liu Q-R, Tagliaferro PA, Brusco A, et al. Cannabinoid CB2 receptors: immunohistochemical localization in rat brain. Brain Res. 2006;1071:10–23. doi: 10.1016/j.brainres.2005.11.035. [DOI] [PubMed] [Google Scholar]
- Göthert M, Brüss M, Bönisch H, Molderings GJ. Presynaptic imidazoline receptors: new developments in characterization and classification. Ann NY Acad Sci. 1999;881:171–184. doi: 10.1111/j.1749-6632.1999.tb09356.x. [DOI] [PubMed] [Google Scholar]
- Guzmán M. Cannabinoids: potential anticancer agents. Nat Rev Cancer. 2003;3:745–755. doi: 10.1038/nrc1188. [DOI] [PubMed] [Google Scholar]
- Guzmán M.Effects on cell viability Cannabinoids. Handbook of Experimental Pharmacology 2005Springer-Verlag: Heidelberg; 627–642.In: Pertwee RG (ed).vol. 168. [DOI] [PubMed] [Google Scholar]
- Guzmán M, Duarte MJ, Blazquez C, Ravina J, Rosa MC, Galve-Roperh I, et al. A pilot clinical study of Δ9-tetrahydrocannabinol in patients with recurrent glioblastoma multiforme. Br J Cancer. 2006;95:197–203. doi: 10.1038/sj.bjc.6603236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hájos N, Freund TF. Pharmacological separation of cannabinoid sensitive receptors on hippocampal excitatory and inhibitory fibers. Neuropharmacology. 2002;43:503–510. doi: 10.1016/s0028-3908(02)00157-0. [DOI] [PubMed] [Google Scholar]
- Haller J, Mátyas F, Soproni K, Varga B, Barsy B, Németh B, et al. Correlated species differences in the effects of cannabinoid ligands on anxiety and on GABAergic and glutamatergic synaptic transmission. Eur J Neurosci. 2007;25:2445–2456. doi: 10.1111/j.1460-9568.2007.05476.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haller VL, Cichewicz DL, Welch SP. Non-cannabinoid CB1, non-cannabinoid CB2 antinociceptive effects of several novel compounds in the PPQ stretch test in mice. Eur J Pharmacol. 2006;546:60–68. doi: 10.1016/j.ejphar.2006.07.024. [DOI] [PubMed] [Google Scholar]
- Hejazi N, Zhou C, Oz M, Sun H, Ye JH, Zhang L. Δ9-Tetrahydrocannabinol and endogenous cannabinoid anandamide directly potentiate the function of glycine receptors. Mol Pharmacol. 2006;69:991–997. doi: 10.1124/mol.105.019174. [DOI] [PubMed] [Google Scholar]
- Herkenham M, Lynn AB, Little MD, Johnson MR, Melvin LS, de Costa BR, et al. Cannabinoid receptor localization in brain. Proc Natl Acad Sci USA. 1990;87:1932–1936. doi: 10.1073/pnas.87.5.1932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrera B, Carracedo A, Diez-Zaera M, del Pulgar TG, Guzmán M, Velasco G. The CB2 cannabinoid receptor signals apoptosis via ceramide-dependent activation of the mitochondrial intrinsic pathway. Exp Cell Res. 2006;312:2121–2131. doi: 10.1016/j.yexcr.2006.03.009. [DOI] [PubMed] [Google Scholar]
- Hollister LE. Structure–activity relationships in man of cannabis constituents and homologs and metabolites of Δ9-tetrahydrocannabinol. Pharmacology. 1974;11:3–11. doi: 10.1159/000136462. [DOI] [PubMed] [Google Scholar]
- Howlett AC, Barth F, Bonner TI, Cabral G, Casellas P, Devane WA, et al. International Union of Pharmacology. XXVII. Classification of cannabinoid receptors. Pharmacol Rev. 2002;54:161–202. doi: 10.1124/pr.54.2.161. [DOI] [PubMed] [Google Scholar]
- Huffman JW, Liddle J, Yu S, Aung MM, Abood ME, Wiley JL, et al. 3-(1′,1′-Dimethylbutyl)-1-deoxy-Δ8-THC and related compounds: synthesis of selective ligands for the CB2 receptor. Bioorg Med Chem. 1999;7:2905–2914. doi: 10.1016/s0968-0896(99)00219-9. [DOI] [PubMed] [Google Scholar]
- Iwamura H, Suzuki H, Ueda Y, Kaya T, Inaba T. In vitro and in vivo pharmacological characterization of JTE-907, a novel selective ligand for cannabinoid CB2 receptor. J Pharmacol Exp Ther. 2001;296:420–425. [PubMed] [Google Scholar]
- Izzo AA, Capasso F, Costagliola A, Bisogno T, Marsicano G, Ligresti A, et al. An endogenous cannabinoid tone attenuates cholera toxin-induced fluid accumulation in mice. Gastroenterology. 2003;125:765–774. doi: 10.1016/s0016-5085(03)00892-8. [DOI] [PubMed] [Google Scholar]
- Izzo AA, Coutts AA.Cannabinoids and the digestive tract Cannabinoids. Handbook of Experimental Pharmacology 2005Springer-Verlag: Heidelberg; 573–598.In: Pertwee RG (ed).Vol 168. [DOI] [PubMed] [Google Scholar]
- Izzo AA, Fezza F, Capasso R, Bisogno T, Pinto L, Iuvone T, et al. Cannabinoid CB1-receptor mediated regulation of gastrointestinal motility in mice in a model of intestinal inflammation. Br J Pharmacol. 2001;134:563–570. doi: 10.1038/sj.bjp.0704293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Järbe TUC, DiPatrizio NV. Δ9-THC induced hyperphagia and tolerance assessment: interactions between the CB1 receptor agonist Δ9-THC and the CB1 receptor antagonist SR-141716 (rimonabant) in rats. Behav Pharmacol. 2005;16:373–380. doi: 10.1097/00008877-200509000-00009. [DOI] [PubMed] [Google Scholar]
- Jin KL, Mao XO, Goldsmith PC, Greenberg DA. CB1 cannabinoid receptor induction in experimental stroke. Ann Neurol. 2000;48:257–261. [PubMed] [Google Scholar]
- Justinova Z, Goldberga SR, Heishman SJ, Tanda G. Self-administration of cannabinoids by experimental animals and human marijuana smokers. Pharmacol Biochem Behav. 2005;81:285–299. doi: 10.1016/j.pbb.2005.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kathmann M, Flau K, Redmer A, Trankle C, Schlicker E. Cannabidiol is an allosteric modulator at mu- and delta-opioid receptors. Naunyn-Schmiedebergs Arch Pharmacol. 2006;372:354–361. doi: 10.1007/s00210-006-0033-x. [DOI] [PubMed] [Google Scholar]
- Kelley BG, Thayer SA. Δ9-Tetrahydrocannabinol antagonizes endocannabinoid modulation of synaptic transmission between hippocampal neurons in culture. Neuropharmacology. 2004;46:709–715. doi: 10.1016/j.neuropharm.2003.11.005. [DOI] [PubMed] [Google Scholar]
- Kim K, Moore DH, Makriyannis A, Abood ME. AM1241, a cannabinoid CB2 receptor selective compound, delays disease progression in a mouse model of amyotrophic lateral sclerosis. Eur J Pharmacol. 2006;542:100–105. doi: 10.1016/j.ejphar.2006.05.025. [DOI] [PubMed] [Google Scholar]
- Kimball ES, Schneider CR, Wallace NH, Hornby PJ. Agonists of cannabinoid receptor 1 and 2 inhibit experimental colitis induced by oil of mustard and by dextran sulfate sodium. Am J Physiol Gastrointest Liver Physiol. 2006;291:G364–G371. doi: 10.1152/ajpgi.00407.2005. [DOI] [PubMed] [Google Scholar]
- Kishimoto S, Muramatsu M, Gokoh M, Oka S, Waku K, Sugiura T. Endogenous cannabinoid receptor ligand induces the migration of human natural killer cells. J Biochem. 2005;137:217–223. doi: 10.1093/jb/mvi021. [DOI] [PubMed] [Google Scholar]
- Koch M, Dehghani F, Habazettl I, Schomerus C, Korf H-W. Cannabinoids attenuate norepinephrine-induced melatonin biosynthesis in the rat pineal gland by reducing arylalkylamine N-acetyltransferase activity without involvement of cannabinoid receptors. J Neurochem. 2006;98:267–278. doi: 10.1111/j.1471-4159.2006.03873.x. [DOI] [PubMed] [Google Scholar]
- Kreitzer AC. Neurotransmission: emerging roles of endocannabinoids. Curr Biol. 2005;15:R549–R551. doi: 10.1016/j.cub.2005.07.005. [DOI] [PubMed] [Google Scholar]
- Lam PMW, McDonald J, Lambert DG. Characterization and comparison of recombinant human and rat TRPV1 receptors: effects of exo- and endocannabinoids. Br J Anaesth. 2005;94:649–656. doi: 10.1093/bja/aei098. [DOI] [PubMed] [Google Scholar]
- Le Foll B, Goldberg SR. Cannabinoid CB1 receptor antagonists as promising new medications for drug dependence. J Pharmacol Exp Ther. 2005;312:875–883. doi: 10.1124/jpet.104.077974. [DOI] [PubMed] [Google Scholar]
- Lemberger L, Martz R, Rodda B, Forney R, Rowe H. Comparative pharmacology of Δ9-tetrahydrocannabinol and its metabolite, 11-hydroxy-Δ9-tetrahydrocannabinol. J Clin Invest. 1973;52:2411–2417. doi: 10.1172/JCI107431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtman AH, Martin BR.Cannabinoid tolerance and dependence Cannabinoids. Handbook of Experimental Pharmacology 2005Springer-Verlag: Heidelberg; 691–717.In: Pertwee RG (ed).Vol 168. [DOI] [PubMed] [Google Scholar]
- Lim G, Sung B, Ji R-R, Mao J. Upregulation of spinal cannabinoid-1-receptors following nerve injury enhances the effects of Win 55,212-2 on neuropathic pain behaviors in rats. Pain. 2003;105:275–283. doi: 10.1016/s0304-3959(03)00242-2. [DOI] [PubMed] [Google Scholar]
- Limebeer CL, Hall G, Parker LA. Exposure to a lithium-paired context elicits gaping in rats: a model of anticipatory nausea. Physiol Behav. 2006;88:398–403. doi: 10.1016/j.physbeh.2006.04.014. [DOI] [PubMed] [Google Scholar]
- Lunn CA, Fine JS, Rojas-Triana A, Jackson JV, Fan X, Kung TT, et al. A novel cannabinoid peripheral cannabinoid receptor-selective inverse agonist blocks leukocyte recruitment in vivo. J Pharmacol Exp Ther. 2006;316:780–788. doi: 10.1124/jpet.105.093500. [DOI] [PubMed] [Google Scholar]
- Ma Y-L, Whalley BJ, Stephens GJ.The phytocannabinoid Δ9-tetrahydrocannabivarin modulates synaptic transmission at central inhibitory synapses Proc Br Pharmacol Soc 2006. at
- MacLennan SJ, Reynen PH, Kwan J, Bonhaus DW. Evidence for inverse agonism of SR141716A at human recombinant cannabinoid CB1 and CB2 receptors. Br J Pharmacol. 1998a;124:619–622. doi: 10.1038/sj.bjp.0701915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacLennan SJ, Reynen PH, Kwan J, Bonhaus DW, Martin GR.[35S]GTPγS binding to assess inverse agonist actions of ligands at human recombinant CB1 and CB2 receptors Symposium on the Cannabinoids 1998bBurlington, Vermont, USA; International Cannabinoid Research Society. p 7 [Google Scholar]
- Maldonado R, Valverde O, Berrendero F. Involvement of the endocannabinoid system in drug addiction. Trends Neurosci. 2006;29:225–232. doi: 10.1016/j.tins.2006.01.008. [DOI] [PubMed] [Google Scholar]
- Mallat A, Teixeira-Clerc F, Deveaux V, Lotersztajn S. Cannabinoid receptors as new targets of antifibrosing strategies during chronic liver diseases. Expert Opin Ther Targets. 2007;11:403–409. doi: 10.1517/14728222.11.3.403. [DOI] [PubMed] [Google Scholar]
- Mang CF, Erbelding D, Kilbinger H. Differential effects of anandamide on acetylcholine release in the guinea-pig ileum mediated via vanilloid and non-CB1 cannabinoid receptors. Br J Pharmacol. 2001;134:161–167. doi: 10.1038/sj.bjp.0704220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maresz K, Carrier EJ, Ponomarev ED, Hillard CJ, Dittel BN. Modulation of the cannabinoid CB2 receptor in microglial cells in response to inflammatory stimuli. J Neurochem. 2005;95:437–445. doi: 10.1111/j.1471-4159.2005.03380.x. [DOI] [PubMed] [Google Scholar]
- Maresz K, Pryce G, Ponomarev ED, Marsicano G, Croxford JL, Shriver LP, et al. Direct suppression of CNS autoimmune inflammation via the cannabinoid receptor CB1 on neurons and CB2 on autoreactive T cells. Nat Med. 2007;13:492–497. doi: 10.1038/nm1561. [DOI] [PubMed] [Google Scholar]
- Martin BR, Compton DR, Thomas BF, Prescott WR, Little PJ, Razdan RK, et al. Behavioral, biochemical, and molecular modeling evaluations of cannabinoid analogs. Pharmacol Biochem Behav. 1991;40:471–478. doi: 10.1016/0091-3057(91)90349-7. [DOI] [PubMed] [Google Scholar]
- Massa F, Marsicano G, Hermann H, Cannich A, Monory K, Cravatt BF, et al. The endogenous cannabinoid system protects against colonic inflammation. J Clin Invest. 2004;113:1202–1209. doi: 10.1172/JCI19465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matias I, Di Marzo V. Endocannabinoids and the control of energy balance. Trends Endocrinol Metab. 2007;18:27–37. doi: 10.1016/j.tem.2006.11.006. [DOI] [PubMed] [Google Scholar]
- Matsuda LA, Lolait SJ, Brownstein MJ, Young AC, Bonner TI. Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature. 1990;346:561–564. doi: 10.1038/346561a0. [DOI] [PubMed] [Google Scholar]
- McAllister SD, Chan C, Taft RJ, Luu T, Abood ME, Moore DH, et al. Cannabinoids selectively inhibit proliferation and induce death of cultured human glioblastoma multiforme cells. J Neurooncol. 2005;74:31–40. doi: 10.1007/s11060-004-5950-2. [DOI] [PubMed] [Google Scholar]
- McHugh D, Ross RA.Endocannabinoids and phytocannabinoids inhibit human neutrophil migration Symposium on the Cannabinoids 2005Burlington, Vermont, USA; International Cannabinoid Research Society. p 38 [Google Scholar]
- McKallip RJ, Lombard C, Fisher M, Martin BR, Ryu SH, Grant S, et al. Targeting CB2 cannabinoid receptors as a novel therapy to treat malignant lymphoblastic disease. Blood. 2002;100:627–634. doi: 10.1182/blood-2002-01-0098. [DOI] [PubMed] [Google Scholar]
- Mechoulam R. Plant cannabinoids: a neglected pharmacological treasure trove. Br J Pharmacol. 2005;146:913–915. doi: 10.1038/sj.bjp.0706415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechoulam R, Ben-Shabat S, Hanus L, Ligumsky M, Kaminski NE, Schatz AR, et al. Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem Pharmacol. 1995;50:83–90. doi: 10.1016/0006-2952(95)00109-d. [DOI] [PubMed] [Google Scholar]
- Mendizábal VE, Adler-Graschinsky E. Cannabinoids as therapeutic agents in cardiovascular disease: a tale of passions and illusions. Br J Pharmacol. 2007;151:427–440. doi: 10.1038/sj.bjp.0707261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merkus FWHM. Cannabivarin and tetrahydrocannabivarin, two new constituents of hashish. Nature. 1971;232:579–580. doi: 10.1038/232579a0. [DOI] [PubMed] [Google Scholar]
- Mitrirattanakul S, Ramakul N, Guerrero AV, Matsuka Y, Ono T, Iwase H, et al. Site-specific increases in peripheral cannabinoid receptors and their endogenous ligands in a model of neuropathic pain. Pain. 2006;126:102–114. doi: 10.1016/j.pain.2006.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molderings GJ, Bönisch H, Hammermann R, Göthert M, Brüss M. Noradrenaline release-inhibiting receptors on PC12 cells devoid of α2- and CB1 receptors: similarities to presynaptic imidazoline and edg receptors. Neurochem Int. 2002;40:157–167. doi: 10.1016/s0197-0186(01)00076-6. [DOI] [PubMed] [Google Scholar]
- Monory K, Massa F, Egertová M, Eder M, Blaudzun H, Westenbroek R, et al. The endocannabinoid system controls key epileptogenic circuits in the hippocampus. Neuron. 2006;51:455–466. doi: 10.1016/j.neuron.2006.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monory K, Tzavara ET, Lexime J, Ledent C, Parmentier M, Borsodi A, et al. Novel, not adenylyl cyclase-coupled cannabinoid binding site in cerebellum of mice. Biochem Biophys Res Commun. 2002;292:231–235. doi: 10.1006/bbrc.2002.6635. [DOI] [PubMed] [Google Scholar]
- Munro S, Thomas KL, Abu-Shaar M. Molecular characterization of a peripheral receptor for cannabinoids. Nature. 1993;365:61–65. doi: 10.1038/365061a0. [DOI] [PubMed] [Google Scholar]
- Nagai H, Egashira N, Sano K, Ogata A, Mizuki A, Mishima K, et al. Antipsychotics improve Δ9-tetrahydrocannabinol-induced impairment of the prepulse inhibition of the startle reflex in mice. Pharmacol Biochem Behav. 2006;84:330–336. doi: 10.1016/j.pbb.2006.05.018. [DOI] [PubMed] [Google Scholar]
- O'Sullivan SE, Tarling EJ, Bennett AJ, Kendall DA, Randall MD. Novel time-dependent vascular actions of Δ9-tetrahydrocannabinol mediated by peroxisome proliferator-activated receptor gamma. Biochem Biophys Res Commun. 2005;337:824–831. doi: 10.1016/j.bbrc.2005.09.121. [DOI] [PubMed] [Google Scholar]
- Oz M. Receptor-independent actions of cannabinoids on cell membranes: focus on endocannabinoids. Pharmacol Ther. 2006;111:114–144. doi: 10.1016/j.pharmthera.2005.09.009. [DOI] [PubMed] [Google Scholar]
- Parker LA, Limebeer CL, Kwiatkowska M.Cannabinoids: effects on vomiting and nausea in animal models Cannabinoids as Therapeutics 2005Birkhaüser Verlag: Basel; 183–200.In: Mechoulam R (ed). [Google Scholar]
- Parker LA, Mechoulam R, Schlievert C, Abbott L, Fudge ML, Burton P. Effects of cannabinoids on lithium-induced conditioned rejection reactions in a rat model of nausea. Psychopharmacology. 2003;166:156–162. doi: 10.1007/s00213-002-1329-2. [DOI] [PubMed] [Google Scholar]
- Patel S, Hillard CJ. Pharmacological evaluation of cannabinoid receptor ligands in a mouse model of anxiety: further evidence for an anxiolytic role for endogenous cannabinoid signaling. J Pharmacol Exp Ther. 2006;318:304–311. doi: 10.1124/jpet.106.101287. [DOI] [PubMed] [Google Scholar]
- Pertwee RG. The central neuropharmacology of psychotropic cannabinoids. Pharmacol Ther. 1988;36:189–261. doi: 10.1016/0163-7258(88)90106-4. [DOI] [PubMed] [Google Scholar]
- Pertwee RG. Pharmacology of cannabinoid CB1 and CB2 receptors. Pharmacol Ther. 1997;74:129–180. doi: 10.1016/s0163-7258(97)82001-3. [DOI] [PubMed] [Google Scholar]
- Pertwee RG. Pharmacology of cannabinoid receptor ligands. Curr Med Chem. 1999;6:635–664. [PubMed] [Google Scholar]
- Pertwee RG. Pharmacological and therapeutic targets for Δ9-tetrahydrocannabinol and cannabidiol. Euphytica. 2004a;140:73–82. [Google Scholar]
- Pertwee RG.The pharmacology and therapeutic potential of cannabidiol Cannabinoids 2004bKluwer Academic/Plenum Publishers: New York; 32–83.In: Di Marzo V (ed). [Google Scholar]
- Pertwee RG. Novel pharmacological targets for cannabinoids. Curr Neuropharmacol. 2004c;2:9–29. [Google Scholar]
- Pertwee RG.Pharmacological actions of cannabinoids Cannabinoids. Handbook of Experimental Pharmacology 2005aSpringer-Verlag: Heidelberg; 1–51.In: Pertwee RG (ed).Vol. 168. [DOI] [PubMed] [Google Scholar]
- Pertwee RG. The therapeutic potential of drugs that target cannabinoid receptors or modulate the tissue levels or actions of endocannabinoids. AAPS J. 2005b;7:E625–E654. doi: 10.1208/aapsj070364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertwee RG.Cannabidiol as a potential medicine Cannabinoids as Therapeutics 2005cBirkhaüser Verlag: Basel; 47–65.In: Mechoulam R (ed). [Google Scholar]
- Pertwee RG. Cannabinoid pharmacology: the first 66 years. Br J Pharmacol. 2006;147:S163–S171. doi: 10.1038/sj.bjp.0706406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pertwee RG.Cannabinoids and multiple sclerosis Mol Neurobiol 2007a(in press) [DOI] [PubMed]
- Pertwee RG.GPR55: a new member of the cannabinoid receptor clan? Br J Pharmacol 2007b(in press) [DOI] [PMC free article] [PubMed]
- Pertwee RG, Ross RA. Cannabinoid receptors and their ligands. Prostaglandins Leukot Essent Fatty Acids. 2002;66:101–121. doi: 10.1054/plef.2001.0341. [DOI] [PubMed] [Google Scholar]
- Pertwee RG, Ross RA, Craib SJ, Thomas A. Cannabidiol antagonizes cannabinoid receptor agonists and noradrenaline in the mouse vas deferens. Eur J Pharmacol. 2002;456:99–106. doi: 10.1016/s0014-2999(02)02624-9. [DOI] [PubMed] [Google Scholar]
- Pertwee RG, Stevenson LA, Ross RA, Gauson LA, Thomas A.Signs of cannabinoid CB2 receptor activation by tetrahydrocannabivarin, cannabigerol and cannabidiol IACM Fourth Conference on Cannabinoids in Medicine 2007a(in press)
- Pertwee RG, Thomas A.Therapeutic applications for agents that act at CB1 and CB2 receptors The Cannabinoid Receptors 2007The Humana Press: Totowa, NJ; In: Reggio PH (ed).(in press) [Google Scholar]
- Pertwee RG, Thomas A, Stevenson LA, Ross RA, Varvel SA, Lichtman AH, et al. The psychoactive plant cannabinoid, Δ9-tetrahydrocannabinol, is antagonized by Δ8- and Δ9-tetrahydrocannabivarin in mice in vivo. Br J Pharmacol. 2007b;150:586–594. doi: 10.1038/sj.bjp.0707124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petitet F, Jeantaud B, Reibaud M, Imperato A, Dubroeucq M-C. Complex pharmacology of natural cannabinoids: evidence for partial agonist activity of Δ9-tetrahydrocannabinol and antagonist activity of cannabidiol on rat brain cannabinoid receptors. Life Sci. 1998;63:PL1–PL6. doi: 10.1016/s0024-3205(98)00238-0. [DOI] [PubMed] [Google Scholar]
- Pisanu A, Acquas E, Fenu S, Di Chiara G. Modulation of Δ9THC-induced increase of cortical and hippocampal acetylcholine release by mu opioid and D-1 dopamine receptors. Neuropharmacology. 2006;50:661–670. doi: 10.1016/j.neuropharm.2005.11.023. [DOI] [PubMed] [Google Scholar]
- Pistis M, Ferraro L, Pira L, Flore G, Tanganelli S, Gessa GL, et al. Δ9-Tetrahydrocannabinol decreases extracellular GABA and increases extracellular glutamate and dopamine levels in the rat prefrontal cortex: an in vivo microdialysis study. Brain Res. 2002;948:155–158. doi: 10.1016/s0006-8993(02)03055-x. [DOI] [PubMed] [Google Scholar]
- Pryce G, Baker D. Control of spasticity in a multiple sclerosis model is mediated by CB1, not CB2, cannabinoid receptors. Br J Pharmacol. 2007;150:519–525. doi: 10.1038/sj.bjp.0707003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rakhshan F, Day TA, Blakely RD, Barker EL. Carrier-mediated uptake of the endogenous cannabinoid anandamide in RBL-2H3 cells. J Pharmacol Exp Ther. 2000;292:960–967. [PubMed] [Google Scholar]
- Rhee M-H, Vogel Z, Barg J, Bayewitch M, Levy R, Hanus L, et al. Cannabinol derivatives: binding to cannabinoid receptors and inhibition of adenylylcyclase. J Med Chem. 1997;40:3228–3233. doi: 10.1021/jm970126f. [DOI] [PubMed] [Google Scholar]
- Rinaldi-Carmona M, Barth F, Héaulme M, Shire D, Calandra B, Congy C, et al. SR141716A, a potent and selective antagonist of the brain cannabinoid receptor. FEBS Lett. 1994;350:240–244. doi: 10.1016/0014-5793(94)00773-x. [DOI] [PubMed] [Google Scholar]
- Robinson L, Fadda P, McKillop-Smith S, Fratta W, Pertwee RG, Riedel G.Phytocannabinoid induced anorexic behaviour in fasted and non-fasted mice IACM Fourth Conference on Cannabinoids in Medicine 2007(in press)
- Robson P.Human studies of cannabinoids and medicinal cannabis Cannabinoids. Handbook of Experimental Pharmacology 2005Springer-Verlag: Heidelberg; 719–756.In: Pertwee RG (ed).vol. 168. [DOI] [PubMed] [Google Scholar]
- Ross RA, Coutts AA, McFarlane SM, Anavi-Goffer S, Irving AJ, Pertwee RG, et al. Actions of cannabinoid receptor ligands on rat cultured sensory neurones: implications for antinociception. Neuropharmacology. 2001;40:221–232. doi: 10.1016/s0028-3908(00)00135-0. [DOI] [PubMed] [Google Scholar]
- Russo EB, Burnett A, Hall B, Parker KK. Agonistic properties of cannabidiol at 5-HT1a receptors. Neurochem Res. 2005;30:1037–1043. doi: 10.1007/s11064-005-6978-1. [DOI] [PubMed] [Google Scholar]
- Ryberg E, Larsson N, Sjögren S, Hjorth S, Hermansson N-O, Leonova J, et al. The orphan receptor GPR55 is a novel cannabinoid receptor Br J Pharmacol 2007(in press) [DOI] [PMC free article] [PubMed]
- Sacerdote P, Martucci C, Vaccani A, Bariselli F, Panerai AE, Colombo A, et al. The nonpsychoactive component of marijuana cannabidiol modulates chemotaxis and IL-10 and IL-12 production of murine macrophages both in vivo and in vitro. J Neuroimmunol. 2005;159:97–105. doi: 10.1016/j.jneuroim.2004.10.003. [DOI] [PubMed] [Google Scholar]
- Sanson M, Bueno L, Fioramonti J. Involvement of cannabinoid receptors in inflammatory hypersensitivity to colonic distension in rats. Neurogastroenterol Motil. 2006;18:949–956. doi: 10.1111/j.1365-2982.2006.00819.x. [DOI] [PubMed] [Google Scholar]
- Sarfaraz S, Afaq F, Adhami VM, Mukhtar H. Cannabinoid receptor as a novel target for the treatment of prostate cancer. Cancer Res. 2005;65:1635–1641. doi: 10.1158/0008-5472.CAN-04-3410. [DOI] [PubMed] [Google Scholar]
- Schramm-Sapyta NL, Cha YM, Chaudhry S, Wilson WA, Swartzwelder HS, Kuhn CM. Differential anxiogenic, aversive, and locomotor effects of THC in adolescent and adult rats. Psychopharmacology. 2007;191:867–877. doi: 10.1007/s00213-006-0676-9. [DOI] [PubMed] [Google Scholar]
- Shen M, Thayer SA. Δ9-Tetrahydrocannabinol acts as a partial agonist to modulate glutamatergic synaptic transmission between rat hippocampal neurons in culture. Mol Pharmacol. 1999;55:8–13. doi: 10.1124/mol.55.1.8. [DOI] [PubMed] [Google Scholar]
- Shoemaker JL, Seely KA, Reed RL, Crow JP, Prather PL. The CB2 cannabinoid agonist AM-1241 prolongs survival in a transgenic mouse model of amyotrophic lateral sclerosis when initiated at symptom onset. J Neurochem. 2007;101:87–98. doi: 10.1111/j.1471-4159.2006.04346.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Showalter VM, Compton DR, Martin BR, Abood ME. Evaluation of binding in a transfected cell line expressing a peripheral cannabinoid receptor (CB2): identification of cannabinoid receptor subtype selective ligands. J Pharmacol Exp Ther. 1996;278:989–999. [PubMed] [Google Scholar]
- Siegling A, Hofmann HA, Denzer D, Mauler F, De Vry J. Cannabinoid CB1 receptor upregulation in a rat model of chronic neuropathic pain. Eur J Pharmacol. 2001;415:R5–R7. doi: 10.1016/s0014-2999(01)00798-1. [DOI] [PubMed] [Google Scholar]
- Sim LJ, Hampson RE, Deadwyler SA, Childers SR. Effects of chronic treatment with Δ9-tetrahydrocannabinol on cannabinoid-stimulated [35S]GTPγS autoradiography in rat brain. J Neurosci. 1996;16:8057–8066. doi: 10.1523/JNEUROSCI.16-24-08057.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sim-Selley LJ. Regulation of cannabinoid CB1 receptors in the central nervous system by chronic cannabinoids. Crit Rev Neurobiol. 2003;15:91–119. doi: 10.1615/critrevneurobiol.v15.i2.10. [DOI] [PubMed] [Google Scholar]
- Sim-Selley LJ, Martin BR. Effect of chronic administration of R-(+)-[2,3-dihydro-5-methyl-3-[(morpholinyl)methyl]pyrrolo[1,2,3-de]-1,4-benzoxazinyl]-(1-naphthalenyl)methanone mesylate (WIN55,212-2) or Δ9-tetrahydrocannabinol on cannabinoid receptor adaptation in mice. J Pharmacol Exp Ther. 2002;303:36–44. doi: 10.1124/jpet.102.035618. [DOI] [PubMed] [Google Scholar]
- Skaper SD, Buriani A, Dal Toso R, Petrelli L, Romanello S, Facci L, et al. The ALIAmide palmitoylethanolamide and cannabinoids, but not anandamide, are protective in a delayed postglutamate paradigm of excitotoxic death in cerebellar granule neurons. Proc Natl Acad Sci USA. 1996;93:3984–3989. doi: 10.1073/pnas.93.9.3984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steffens S, Mach F. Cannabinoid receptors in atherosclerosis. Curr Opin Lipidol. 2006;17:519–526. doi: 10.1097/01.mol.0000245257.17764.b2. [DOI] [PubMed] [Google Scholar]
- Steffens S, Veillard NR, Arnaud C, Pelli G, Burger F, Staub C, et al. Low dose oral cannabinoid therapy reduces progression of atherosclerosis in mice. Nature. 2005;434:782–786. doi: 10.1038/nature03389. [DOI] [PubMed] [Google Scholar]
- Straiker A, Mackie K. Depolarization-induced suppression of excitation in murine autaptic hippocampal neurones. J Physiol. 2005;569:501–517. doi: 10.1113/jphysiol.2005.091918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugiura T, Kondo S, Sukagawa A, Nakane S, Shinoda A, Itoh K, et al. 2-Arachidonoylglycerol: a possible endogenous cannabinoid receptor ligand in brain. Biochem Biophys Res Comm. 1995;215:89–97. doi: 10.1006/bbrc.1995.2437. [DOI] [PubMed] [Google Scholar]
- Szabo B, Schlicker E.Effects of cannabinoids on neurotransmission Cannabinoids. Handbook of Experimental Pharmacology 2005Springer-Verlag: Heidelberg; 327–365.In: Pertwee RG (ed).Vol 168. [DOI] [PubMed] [Google Scholar]
- Szczesniak AM, Kelly MEM, Whynot S, Shek PN, Hung O. Ocular hypotensive effects of an intratracheally delivered liposomal delta-9-tetrahydrocannabinol preparation in rats. J Ocul Pharmacol Ther. 2006;22:160–167. doi: 10.1089/jop.2006.22.160. [DOI] [PubMed] [Google Scholar]
- Thomas A, Baillie GL, Phillips AM, Razdan RK, Ross RA, Pertwee RG. Cannabidiol displays unexpectedly high potency as an antagonist of CB1 and CB2 receptor agonists in vitro. Br J Pharmacol. 2007;150:613–623. doi: 10.1038/sj.bjp.0707133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas A, Ross RA, Saha B, Mahadevan A, Razdan RK, Pertwee RG. 6″-Azidohex-2″-yne-cannabidiol: a potential neutral, competitive cannabinoid CB1 receptor antagonist. Eur J Pharmacol. 2004;487:213–221. doi: 10.1016/j.ejphar.2004.01.023. [DOI] [PubMed] [Google Scholar]
- Thomas A, Stevenson LA, Wease KN, Price MR, Baillie G, Ross RA, et al. Evidence that the plant cannabinoid Δ9-tetrahydrocannabivarin is a cannabinoid CB1 and CB2 receptor antagonist. Br J Pharmacol. 2005;146:917–926. doi: 10.1038/sj.bjp.0706414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomida I, Azuara-Blanco A, House H, Flint M, Pertwee RG, Robson PJ. Effect of sublingual application of cannabinoids on intraocular pressure: a pilot study. J Glaucoma. 2006;15:349–353. doi: 10.1097/01.ijg.0000212260.04488.60. [DOI] [PubMed] [Google Scholar]
- Tomida I, Pertwee RG, Azuara-Blanco A. Cannabinoids and glaucoma. Br J Ophthalmol. 2004;88:708–713. doi: 10.1136/bjo.2003.032250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turkanis SA, Karler R. Electrophysiologic properties of the cannabinoids. J Clin Pharmacol. 1981;21:449S–463S. doi: 10.1002/j.1552-4604.1981.tb02625.x. [DOI] [PubMed] [Google Scholar]
- Van Sickle MD, Duncan M, Kingsley PJ, Mouihate A, Urbani P, Mackie K, et al. Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science. 2005;310:329–332. doi: 10.1126/science.1115740. [DOI] [PubMed] [Google Scholar]
- Van Sickle MD, Oland LD, Mackie K, Davison JS, Sharkey KA. Δ9-Tetrahydrocannabinol selectively acts on CB1 receptors in specific regions of dorsal vagal complex to inhibit emesis in ferrets. Am J Physiol Gastrointest Liver Physiol. 2003;285:G566–G576. doi: 10.1152/ajpgi.00113.2003. [DOI] [PubMed] [Google Scholar]
- Varvel SA, Bridgen DT, Tao Q, Thomas BF, Martin BR, Lichtman AH. Δ9-Tetrahydrocannbinol accounts for the antinociceptive, hypothermic, and cataleptic effects of marijuana in mice. J Pharmacol Exp Ther. 2005;314:329–337. doi: 10.1124/jpet.104.080739. [DOI] [PubMed] [Google Scholar]
- Vaughan CW, Christie MJ.Retrograde signalling by endocannabinoids Cannabinoids. Handbook of Experimental Pharmacology 2005Springer-Verlag: Heidelberg; 367–383.In: Pertwee RG (ed).Vol 168. [DOI] [PubMed] [Google Scholar]
- Wagner JA, Varga K, Ellis EF, Rzigalinski BA, Martin BR, Kunos G. Activation of peripheral CB1 cannabinoid receptors in haemorrhagic shock. Nature. 1997;390:518–521. doi: 10.1038/37371. [DOI] [PubMed] [Google Scholar]
- Walczak JS, Pichette V, Leblond F, Desbiens K, Beaulieu P. Characterization of chronic constriction of the saphenous nerve, a model of neuropathic pain in mice showing rapid molecular and electrophysiological changes. J Neurosci Res. 2006;83:1310–1322. doi: 10.1002/jnr.20821. [DOI] [PubMed] [Google Scholar]
- Wallace MJ, Blair RE, Falenski KW, Martin BR, DeLorenzo RJ. The endogenous cannabinoid system regulates seizure frequency and duration in a model of temporal lobe epilepsy. J Pharmacol Exp Ther. 2003;307:129–137. doi: 10.1124/jpet.103.051920. [DOI] [PubMed] [Google Scholar]
- Wallace MJ, Wiley JL, Martin BR, DeLorenzo RJ. Assessment of the role of CB1 receptors in cannabinoid anticonvulsant effects. Eur J Pharmacol. 2001;428:51–57. doi: 10.1016/s0014-2999(01)01243-2. [DOI] [PubMed] [Google Scholar]
- Walter L, Franklin A, Witting A, Wade C, Xie Y, Kunos G, et al. Nonpsychotropic cannabinoid receptors regulate microglial cell migration. J Neurosci. 2003;23:1398–1405. doi: 10.1523/JNEUROSCI.23-04-01398.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walter L, Stella N. Cannabinoids and neuroinflammation. Br J Pharmacol. 2004;141:775–785. doi: 10.1038/sj.bjp.0705667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe K, Kijima T, Narimatsu S, Nishikami J, Yamamoto I, Yoshimura H. Comparison of pharmacological effects of tetrahydrocannabinols and their 11-hydroxy-metabolites in mice. Chem Pharm Bull. 1990;38:2317–2319. doi: 10.1248/cpb.38.2317. [DOI] [PubMed] [Google Scholar]
- Weston S, Williamson EM, Constanti A, Stephens G, Whalley B.Tetrahydrocannabivarin exhibits anticonvulsant effects in a piriform cortical brain slice model of epileptiform activity Proc Br Pharmacol Soc 2006. at
- Whiteside GT, Lee GP, Valenzano KJ. The role of the cannabinoid CB2 receptor in pain transmission and therapeutic potential of small molecule CB2 receptor agonists. Curr Med Chem. 2007;14:917–936. doi: 10.2174/092986707780363023. [DOI] [PubMed] [Google Scholar]
- Wiley JL, Burston JJ, Leggett DC, Alekseeva OO, Razdan RK, Mahadevan A, et al. CB1 cannabinoid receptor-mediated modulation of food intake in mice. Br J Pharmacol. 2005a;145:293–300. doi: 10.1038/sj.bjp.0706157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiley JL, Jefferson RG, Grier MC, Mahadevan A, Razdan RK, Martin BR. Novel pyrazole cannabinoids: insights into CB1 receptor recognition and activation. J Pharmacol Exp Ther. 2001;296:1013–1022. [PubMed] [Google Scholar]
- Wiley JL, Smith FL, Razdan RK, Dewey WL. Task specificity of cross-tolerance between Δ9-tetrahydrocannabinol and anandamide analogs in mice. Eur J Pharmacol. 2005b;510:59–68. doi: 10.1016/j.ejphar.2005.01.006. [DOI] [PubMed] [Google Scholar]
- Wilkinson JD, Williamson EM. Cannabinoids inhibit human keratinocyte proliferation through a non-CB1/CB2 mechanism and have a potential therapeutic value in the treatment of psoriasis. J Dermatol Sci. 2007;45:87–92. doi: 10.1016/j.jdermsci.2006.10.009. [DOI] [PubMed] [Google Scholar]
- Wilson RS, May EL. Analgesic properties of the tetrahydrocannabinols, their metabolites and analogs. J Med Chem. 1975;18:700–703. doi: 10.1021/jm00241a012. [DOI] [PubMed] [Google Scholar]
- Wotherspoon G, Fox A, McIntyre P, Colley S, Bevan S, Winter J. Peripheral nerve injury induces cannabinoid receptor 2 protein expression in rat sensory neurons. Neuroscience. 2005;135:235–245. doi: 10.1016/j.neuroscience.2005.06.009. [DOI] [PubMed] [Google Scholar]
- Xu H, Cheng B, Manivannan A, Cabay L, Pertwee RG, Coutts A, et al. Anti-inflammatory property of the cannabinoid receptor-2 selective agonist JWH-133 in a rodent model of autoimmune uveoretinitis J Leukoc Biol 2007. 82 [e-pub ahead of print] [DOI] [PubMed]
- Xu X, Liu Y, Huang S, Liu G, Xie C, Zhou J, et al. Overexpression of cannabinoid receptors CB1 and CB2 correlates with improved prognosis of patients with hepatocellular carcinoma. Cancer Genet Cytogenet. 2006;171:31–38. doi: 10.1016/j.cancergencyto.2006.06.014. [DOI] [PubMed] [Google Scholar]
- Yiangou Y, Facer P, Durrenberger P, Chessell IP, Naylor A, Bountra C, et al. COX-2, CB2 and P2X7-immunoreactivities are increased in activated microglial cells/macrophages of multiple sclerosis and amyotrophic lateral sclerosis spinal cord BMC Neurol 20066at [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Hoffert C, Vu HK, Groblewski T, Ahmad S, O'Donnell D. Induction of CB2 receptor expression in the rat spinal cord of neuropathic but not inflammatory chronic pain models. Eur J Neurosci. 2003;17:2750–2754. doi: 10.1046/j.1460-9568.2003.02704.x. [DOI] [PubMed] [Google Scholar]
- Zimmer A, Zimmer AM, Hohmann AG, Herkenham M, Bonner TI. Increased mortality, hypoactivity, and hypoalgesia in cannabinoid CB1 receptor knockout mice. Proc Natl Acad Sci USA. 1999;96:5780–5785. doi: 10.1073/pnas.96.10.5780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zygmunt PM, Andersson DA, Högestätt ED. Δ9-Tetrahydrocannabinol and cannabinol activate capsaicin-sensitive sensory nerves via a CB1 and CB2 cannabinoid receptor-independent mechanism. J Neurosci. 2002;22:4720–4727. doi: 10.1523/JNEUROSCI.22-11-04720.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]