Abstract
Atherosclerosis is a chronic inflammatory disease that is the primary cause of myocardial infarction and stroke, which occur after sudden thrombotic occlusion of an artery. A growing body of evidence suggests that cannabinoid signalling plays a fundamental role in atherosclerosis development and its clinical manifestations. Thus, CB2 receptors are protective in myocardial ischaemia/reperfusion and implicated in the modulation of chemotaxis, which is crucial for the recruitment of leukocytes during inflammation. Delta-9-Tetrahydrocannabinol (THC)-mediated activation has been shown to inhibit atherosclerotic plaque progression in a CB2 dependent manner. Although CB1 and CB2 expression has been reported on platelets, their involvement in thrombus formation is still controversial. While several reports suggest that CB1 receptors may have a relevant role in neuroprotection after ischaemic stroke, recent studies show the protective effects in various forms of neuroprotection are not related to CB1 stimulation, and a protective role of CB1 blockade has also been reported. In addition, vascular and myocardial CB1 receptors contribute to the modulation of blood pressure and heart rate. It is tempting to suggest that pharmacological modulation of the endocannabinoid system is a potential novel therapeutic strategy in the treatment of atherosclerosis. For these purposes, it is important to better understand the complex mechanisms of endocannabinoid signalling and potential consequences of its pharmacological modulation, as it may have both pro- and anti-atherosclerotic effects.
Keywords: atherosclerosis, inflammation, myocardial infarction, stroke, post-ischaemic heart failure, remodelling, cannabinoid receptors, cannabinoids
Introduction
Atherosclerosis is an inflammatory disease characterized by arterial lesions containing cholesterol, immune infiltrates and connective-tissue elements (Libby, 2002; Osterud and Bjorklid, 2003; Hansson, 2005; Hansson and Libby, 2006). It is responsible for major mortality causes, that is, ischaemic heart disease and cerebrovascular disease. Prevention and current treatments for atherosclerosis are mainly based on drugs that lower plasma cholesterol concentration and high blood pressure. In particular, statins have proven to reduce cardiovascular events significantly, not only by their cholesterol-lowering properties but also by their more recently identified anti-inflammatory and immunomodulatory effects (Mach, 2004). Nevertheless, atherosclerosis remains the primary cause of heart disease and stroke, accounting for up to 50% of deaths in the Western countries. The identification and development of potential promising novel anti-inflammatory therapies is thus of great interest for the medical community.
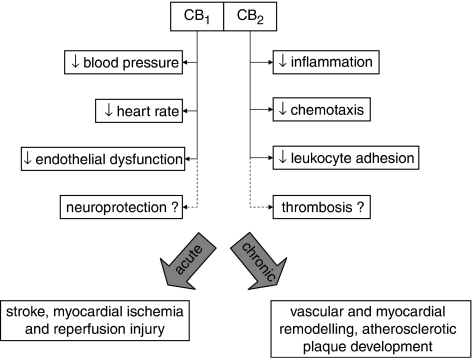
Cannabinoids such as delta-9-tetrahydrocannabinol (THC) modulate immune functions and therefore have a therapeutic potential for the treatment of inflammatory diseases (Klein, 2003, 2005). It is thought that the immunomodulatory effects of cannabinoids are mediated by CB2 receptors expressed on immune cells. A growing body of evidence suggests that endocannabinoid signalling plays a critical role in the pathogenesis of atherogenesis and its clinical manifestations (Figure 1). We have recently provided the first experimental evidence for a possible role of CB2 receptors in atherosclerosis progression (Steffens et al., 2005). Using an experimental mouse model of atherosclerosis, oral administration of THC resulted in significant inhibition of plaque development, an effect that could be reversed by the CB2 antagonist SR144528. In addition, cannabinoids are known to exhibit complex cardiovascular actions, although the findings are in part controversial due to different species and methodologies. The predominant experimental evidence indicates that CB2 receptor activation via endocannabinoids is protective in myocardial ischaemia/reperfusion (I/R), an acute complication of atherosclerosis (Lagneux and Lamontagne, 2001; Joyeux et al., 2002; Lépicier et al., 2003; Di Filippo et al., 2004). On the other hand, CB1 receptors contribute to the modulation of blood pressure and heart rate, thus representing an attractive target for therapeutic intervention to reduce cardiovascular risk factors such as hypertension (Bátkai et al., 2004; Pacher et al., 2005a, 2005b; Mendizábal and Adler-Graschinsky, 2007).
Figure 1.
Cannabinoid signalling via CB1 and CB2 receptors mediates differential cardiovascular effects, suggesting their implication in acute and chronic complications of atherosclerosis.
Atherosclerosis and inflammation
Early atherosclerosis is characterized by endothelial dysfunction enhanced by many risk factors. Beyond genetic risk factors, hyperlipidaemia, diabetes, hypertension, obesity and smoking are the main cardiovascular risk factors, which enhance endothelial injury (Lusis, 2000; Glass and Witztum, 2001). Under normal conditions, endothelial cells inhibit platelet and leukocyte adhesion to the vascular surface. In the setting of unfavourable risk factors, an inflammatory response is initiated in the artery wall. The endothelial inflammatory response induces the surface expression of several types of leukocyte adhesion molecules and secretion of chemoattractant molecules (Braunersreuther and Mach, 2006; Hansson and Libby, 2006). For example, the chemokine monocyte chemoattractant protein-1 /CCL2 was found at high expression levels within atherosclerotic lesions, and thus considered as a key player in monocyte recruitment into the arterial wall (Nelken et al., 1991; Ylä-Herttuala et al., 1991; Yu et al., 1992). Other CC family chemokines such as macrophage inflammatory protein-1α /CCL3, macrophage inflammatory protein-1β/CCL4, regulated on activated normal T-cell expressed and secreted/CCL5, as well as a number of more recently discovered chemokines have also been detected in atherosclerotic lesions (Schecter et al., 2000; von Hundelshausen et al., 2001; Veillard et al., 2004).
The local production of chemokines, chemokine receptors and adhesion molecules from activated endothelial cells and inflammatory cells causes leukocyte rolling along the vascular surface and cell adhesion at the site of activation (Braunersreuther and Mach, 2006). Endothelial dysfunction occurs preferentially at the sites of haemodynamic strain. Leukocytes recruited to the subendothelial space secrete chemokines and cytokines, thus promoting the ongoing chronic inflammatory process. This results in the presence of a large number of inflammatory and immune cells within atherosclerotic lesions.
Besides the regulation of leukocyte trafficking during inflammation, chemokines are also involved in the activation of platelets (Abi-Younes et al., 2000; Kowalska et al., 2000). Platelets are anucleated cellular fragments that circulate in the blood. In addition to their well-recognized role in haemostasis and acute thrombus formation, platelets are also thought to have proinflammatory and growth-regulatory properties that contribute to progression of atherosclerosis (Gawaz et al., 2005; Nieswandt et al., 2005; Weber, 2005). Platelet activation releases multiple growth factors and inflammatory mediators, including chemokines, such as platelet factor 4/CXCL4) and regulated on activated normal T cell expressed and secreted into the microenvironment (Scheuerer et al., 2000; Weber et al., 2004; Weber, 2005).
At more advanced stages of atherosclerosis, the release of proinflammatory cytokines and chemokines promotes the proliferation and migration of smooth-muscle cells from the media to the intima. Within the intima, smooth-muscle cells secrete extracellular matrix components, leading to the accumulation of collagen and proteoglycans, key factors implicated in plaque stability (Newby, 2005). Conversely, the secretion of matrix metalloproteinases by vascular and inflammatory cells degrades matrix components such as collagen, gelatin or elastin within atherosclerotic lesions. Depending on the stability of the lesion, the plaque may rupture and induce thrombosis, leading to acute vascular events such as myocardial infarction or stroke.
Role of cannabinoids in acute complications of atherosclerosis
Generally, the acute complications of atherosclerosis are due to the sudden thrombotic occlusion of an artery (Libby and Aikawa, 2002). Physical disruption of the plaque is the most frequent cause of thrombotic occlusion (Libby and Aikawa, 2002). The pathophysiology of this process is mainly regulated by endothelial cells, macrophages, T cells, mast cells and platelets, which produce cytokines and proteases, responsible for conferring to the plaque the susceptibility to rupture and consequent thrombosis (Hansson and Libby, 2006). In areas without collateral vessels (mainly heart and brain), thrombi arising from ruptured plaque can cause infarction of the tissues, with devastating clinical consequences (Hansson and Libby, 2006).
Synthetic and endogenous cannabinoids are known to exhibit complex cardiovascular actions as described in a vast number of in vitro and in vivo studies, with both increases and decreases in blood pressure being reported (Pacher et al., 2006). Clearly, the cardiovascular cannabinoid effects strongly depend on the pharmacology of the compound, the way and frequency of administration, the vehicle, use of anaesthesia, as well as the experimental in vitro model or species used. Given these investigative limitations, it is difficult to draw firm conclusions for a therapeutic use in humans. Nevertheless, synthetic and endogenous cannabinoids may represent an emerging target for pharmacotherapy for reducing acute cardiovascular complications such as stroke and acute myocardial infarction in multiple risk factor patients (Pacher et al., 2006).
Cardiovascular effects of cannabinoids
The acute administration of cannabinoids in humans is typically associated with tachycardia (Beaconsfield, 1974; Kanakis et al., 1979; Hollister, 1986) and increased supine blood pressure (Jones, 2002), but also marked orthostatic hypotension were observed (Mathew et al., 1992; Jones, 2002; Sidney, 2002). In contrast, acute administration of cannabinoids in laboratory animals is accompanied by bradycardia and hypotension (Fredericks et al., 1981; Dewey, 1986). Prevention of endocannabinoid anandamide degradation by an inhibitor of fatty-acid amide hydrolase was shown to lower blood pressure and heart rate in hypertensive rodents through reductions in both cardiac contractility and vascular resistance (Bátkai et al., 2004). These effects were prevented by CB1 antagonists. Fatty acid amide hydrolase-knockout mice, however, have normal blood pressure and cardiac function, indicating that under normal conditions anandamide does not play a major role in cardiovascular regulation (Pacher et al., 2005c). Consistent with these observations, THC inhalation was found to result in a greater and longer lasting decrease of arterial blood pressure in hypertensive as compared with normotensive individuals (Crawford and Merritt, 1979). These findings suggest that the endocannabinoid system represents a therapeutic target for treatment of hypertension (Pacher et al., 2005a).
The differences between humans and animals may be due to at least three different reasons. First, methodological differences in drug administration do not allow a direct comparison of human and animal data. The data on cardiovascular effects in humans mostly refer to marijuana smokers, whereas cannabinoid administration to animals is performed systemically or orally. Second, human populations are usually limited to only young men who represent the predominant population of marijuana smokers, while there are only a few data on older people or women (Mittleman et al., 2001; Jones, 2002). Similarly, animal experiments are usually performed with young male populations. Third, the doses of THC or cannabinoid given in the animal experiences are probably too high and do not reflect the concentrations found in humans after drug exposure (Dewey, 1986; Jones, 2002).
Stroke
Ischaemic stroke is caused by a transient interruption of blood flow to the brain, due to a thrombotic acute occlusion of the blood vessels. It represents one of the most important causes of death and disability in the industrialized countries (Klijn and Hankey, 2003; Pinto et al., 2004). Several in vitro and in vivo models of cerebral ischaemia have been developed to identify effective agents against atherosclerotic plaque rupture, the consequent thrombus formation and neurodegeneration.
There is a general consensus on considering cannabinoids as neuroprotective agents. (R+)-WIN 55,212-2, anandamide and 2-AG were found capable of protecting in vitro cultured rat neurons against hypoxia and glucose deprivation (Nagayama et al., 1999; Sinor et al., 2000). CB1, which is more highly expressed in the brain compared to CB2, is thought to be crucial for neuroprotection (Galve-Roperh et al., 2007). Indeed, alterations of CB1 receptor expression levels were found to be associated with neuroprotection (Galve-Roperh et al., 2007; Hayakawa et al., 2007). In different animal models of brain injury and neurodegenerative diseases, endocannabinoid signalling was implicated in the regulation of microglial cell and neuron proliferation and differentiation. After stroke, CB1 receptor agonists increase the production of neurotrophic factors in mouse neural progenitors (Aguado et al., 2007). In order to investigate the underlying molecular mechanisms of CB1-dependent neuroprotection, Panikashvili et al. (2005) showed the involvement of nuclear factor-kappa B inhibition, key regulator of the inflammatory response after brain injury. In this interesting study, the authors showed that activation of nuclear factor-kappa B in injured CB1-knockout mouse brain was three to fourfolds higher than in the respective non-injured CB1 knockout mice. Exogenous 2-AG treatment significantly improved neurobehavioral function in wild-type mice after brain injury, whereas no improvement was observed in CB1 knockout mice. While one study suggested a comparable role for endogenous and exogenous cannabinoids in neuroprotection (Parmentier-Batteur et al., 2002), the study by Panikashvili and co-workers showed that only the exogenous compound was neuroprotective. As mentioned previously, the dose and route of cannabinoid administration might strongly affect the results obtained in various experimental designs and explain the discrepant findings.
In addition, the neuroprotective effects of other cannabinoids, such as dexanabinol (HU-211; 4–4.5 mg kg−1) (Bar-Joseph et al., 1994; Leker et al., 1999; Lavie et al., 2001), WIN 55,212-2 (0.03–1 mg kg−1) (Nagayama et al., 1999), BAY38-7271 (0.1 μg kg−1) (Mauler et al., 2003), HU-210 (45 μg kg−1) (Leker et al., 2003), as well as 2-AG (1 mg kg−1) administered together with 2-palmitoyl-glycerol (5 mg kg−1) and 2-linoeoyl-glycerol (10 mg kg−1) (Panikashvili et al., 2001), have been demonstrated in various animal models of ischaemic, traumatic or compressive brain injuries. Finally, it should be noted that several studies contradict the neuroprotective role of CB1 receptor activation, but support the protective role of CB1 blockade (Berger et al., 2004; Muthian et al., 2004; Sommer et al., 2006).
Besides the controversially discussed role of CB1 in neuroprotection, CB2 activation was recently shown as being crucial in microglial cell proliferation and migration in ischaemic brain areas (Carrier et al., 2004; Ashton et al., 2007). The reactivity of these phagocytozing and antigen-presenting cells in the central nervous system is decreased by CB2 activation, which may help to reduce neuronal death in response to microglial macrophage infiltration.
On the other hand, the role of cannabinoids on intra-arterial thrombus formation is still controversial, although both CB1 and CB2 are known to be expressed on human platelets (Deusch et al., 2004). One study reported an inhibiting effect of high concentrations of THC (⩾10−5 M) on agonist-induced human and rabbit platelet aggregation (Formukong et al., 1989). Other studies found increased spontaneous aggregate formation in the presence of THC at similar concentrations, suggesting a procoagulatory role (Levy et al., 1976; Deusch et al., 2004). It is also important to note that the function of other cell types involved in thrombus formation (mainly leukocytes and endothelial cells) is modulated by cannabinoids. It is well known that cannabinoids modulate inflammatory cytokine secretion and chemotaxis of immune cells, such as macrophages, microglial cells and T lymphocytes (Sacerdote et al., 2000; Klein et al., 2003; Sacerdote et al., 2005; Ghosh et al., 2006; Coopman et al., 2007). The implication of CB2 receptors in leukocyte/endothelial interaction and their expression on platelets strongly suggests their crucial role in thrombus formation.
Acute myocardial infarction
Ischaemic heart disease is the leading cause of death among patients in the United States, Europe and the world (Murray and Lopez, 1997). Therefore, the acute coronary syndrome burden has to be considered as a central field for medical research. Acute myocardial infarction is caused by the coronary microvascular obstruction after plaque rupture, with the interruption of blood flow and the consequent ischaemia and necrosis of myocardium. The mechanisms underlying this acute event and the subsequent reperfusion injury, caused by the treatment of coronary artery occlusion (coronary interventions, focused to re-establish the blood flow to the myocardium), are subject of ongoing research. Various reports have highlighted a role for the endocannabinoid system in the physiopathology of I/R myocardial injury. However, a substantial difference between humans and animals has been reported. Several reports indicate an association of chronic THC intake and elevated risk of myocardial infarction in humans (Mittleman et al., 2001). Marijuana smoking in people with cardiovascular disease poses increased health risks (Jones, 2002) due to the increased cardiac work, catecholamine levels, carboxyhemoglobin and postural hypotension (Jones, 2002). To date, no studies investigating the role of cannabinoids in post-ischaemic reperfusion injury in humans are reported.
Conversely, in animals, cannabinoids have been shown to reduce I/R injuries. The endocannabinoid system was found to be implicated in the mechanisms by which lipopolysaccharide limits infarct size, mortality and preconditioning against myocardial I/R injury (Lagneux and Lamontagne, 2001). In this study, the authors showed that pretreatment with the CB2 antagonist SR144528 abolished the lipopolysaccharide-mediated cardioprotective effects. In support of these findings, a different study performed with isolated rat hearts obtained similar results (Joyeux et al., 2002). In addition, Di Filippo et al. (2004) showed that WIN55,212-2 significantly reduced the extent of infarct size in a mouse model of myocardial I/R. This effect was abolished by the CB2 antagonist AM630. In another study, anandamide and HU-210 both decreased the incidence of ventricular arrhythmias and reduced the infarct size through activation of CB2 receptors (Krylatov et al., 2001). In conclusion, numerous animal studies suggest that cannabinoids are cardioprotective in experimental models by activation of CB2 receptors. If similar mechanisms of cannabinoid actions might apply to acute myocardial ischaemia in humans needs to be investigated.
Only few studies have shown a possible role of CB1 receptors in I/R injuries. In ischaemic preconditioning, which mediated preservation of endothelium dependent vasodilation in isolated rat hearts, either CB1 or CB2 receptor blockade abolished the protective effect of preconditioning (Bouchard et al., 2003). In the same model, the selective CB1 agonist ACEA and the CB2 agonist JWH-015 both reduced the infarct size after I/R (Lépicier et al., 2003). Another study reported that the anandamide-induced reduction of infarct size in isolated perfused rat hearts was equally antagonized by CB1 and CB2 antagonists (Underdown et al., 2005).
The various studies suggest distinct roles for CB1 and CB2 receptors in the I/R syndrome. CB1 receptors are probably involved in coronary vasodilation (Bátkai et al., 2004), while CB2 receptors orchestrate leukocyte recruitment, responsible for the reperfusion injury in the infarcted myocardium (Sacerdote et al., 2000, 2005; Di Filippo et al., 2004; Ni et al., 2004; Ghosh et al., 2006; Lunn et al., 2006; Coopman et al., 2007). In conclusion, a broad body of evidence indicates that cannabinoids (mainly endocannabinoids) protect against myocardial I/R injury in animal models, predominantly via activating CB2 receptors.
Role of cannabinoid receptors in chronic complications of atherosclerosis
A growing body of evidence suggests that endocannabinoid signalling plays a critical role in the pathogenesis of atherogenesis and its clinical manifestations. We have recently provided a first experimental evidence for a possible role of CB2 receptors in atherosclerotic plaque progression (Steffens et al., 2005). Moreover, an increasing number of studies reported the modulation of endocannabinoid levels, receptors and related enzymes of biosynthesis and degradation in different inflammatory conditions. This knowledge evolved the concept of blocking endocannabinoid signalling with selective receptor antagonists for therapeutic use. Rimonabant is the first CB1 antagonist studied and approved as anti-obesity drug in Europe and is under review in the United States. Large randomized trials with rimonabant have demonstrated efficacy in treatment of obesity (Després et al., 2005; Van Gaal et al., 2005). In addition, multiple other cardiometabolic parameters were improved in the treatment groups, including increased levels of high-density lipoprotein cholesterol and reduced triglycerides, as well as improved glycemic control in prediabetic patients and in type 2 diabetic patients (Gelfand and Cannon, 2006). This novel medication may become an important therapeutic option to reduce cardiovascular risk factors; however, long-term clinical trials (which are ongoing) are warranted to determine if the improvement in metabolic parameters translates into improved morbidity and mortality and to reveal the rates of potential adverse effects.
Involvement of the endocannabinoid system in pathophysiological conditions
The first study to implicate the endocannabinoid system in a pathophysiological disorder was performed in a rat model of haemorrhagic shock (Wagner et al., 1997). In a more recent study, the levels of anandamide and 2-AG were found to increase in sera of patients with endotoxic shock (Wang et al., 2001). Activation of CB1 receptors by endocannabinoids secreted from platelets and/or macrophages appear to be responsible for the hypotension accompanying haemorrhagic or endotoxic shock (Varga et al., 1998; Liu et al., 2003). Consistently, endocannabinoid signalling via vascular CB1 receptors has been implicated in the vasodilated state in advanced liver cirrhosis (Bátkai et al., 2001), while activation of cardiac CB1 receptors by endogenous anandamide contributes to the reduced cardiac contractility associated with this condition (Bátkai et al., 2007a). In a mouse model of liver I/R injury, hepatic anandamide and 2-AG levels are significantly increased, and CB2 has a protective role (Bátkai et al., 2007b). Moreover, both CB1 and CB2 receptors have been implicated in liver fibrosis, promoting both pro- and antifibrogenic effects (Julien et al., 2005; Teixeira-Clerc et al., 2006). Endocannabinoid signalling has also been reported in periodontal inflammation, as both cannabinoid receptors CB1 and CB2 as well as anandamide were upregulated under pathological conditions (Nakajima et al., 2006). In a mouse model of colonic inflammation, blocking of endocannabinoid signalling with selective receptor antagonists revealed that CB1 receptors mediate intrinsic protective signals that counteract proinflammatory responses (Massa et al., 2004). A very recent report demonstrates a crucial role of the endocannabinoid system in controlling cutaneous contact hypersensitivity (Karsak et al., 2007). Various experimental studies have targeted the endocannabinoid system for the treatment of multiple sclerosis. Using the experimental autoimmune encephalomyelitis model, Maresz et al. (2007) recently demonstrated a differential role of CB1 and CB2 in the central nervous system autoimmune inflammation. While CB1 on neurons was responsible for THC-mediated suppression of neuronal symptoms, endocannabinoid activation of CB2 on effector T cells was crucial for controlling inflammation. Very recent findings further support the protective role of endocannabinoids in inflammatory disorders such as atherosclerosis. Enhanced anandamide levels in mice lacking fatty acid amide hydrolase were protective against age-associated decline in cardiac function, inflammation, oxidative/nitrative stress and apoptosis (Bátkai et al., 2007c).
Modulation of leukocyte/endothelial cell interaction
The recruitment of inflammatory cells (mainly monocytes and T lymphocytes) in the intima is an essential step in the development and progression of atherosclerosis. The tethering, rolling, adhesion and transendothelial migration of leukocytes are triggered by local production of chemokines and chemokine receptors as well as adhesion molecules (Braunersreuther and Mach, 2006). It has been reported that treatment of rat macrophages with CP55,940 reduced both spontaneous and formyl–methionyl–leucine–phenylalanine-induced chemotaxis (Sacerdote et al., 2000). The non-psychoactive marijuana component cannabidiol was shown to inhibit murine macrophage chemotaxis in vitro and in vivo in a CB2 receptor-dependent manner (Sacerdote et al., 2005). In a different study, cannabidiol attenuated the high glucose-induced transendothelial migration of THP-1 monocytes, and monocyte-endothelial adhesion in human coronary artery endothelial cells, as well as the disruption of the endothelial barrier function (Rajesh et al., 2007a). Moreover, cannabidiol attenuated the high glucose-induced mitochondrial superoxide generation, nuclear factor-kappa B activation, nitrotyrosine formation as well as upregulation of inducible nitric oxide synthase and adhesion molecules intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule. The attenuation of all these high glucose-induced effects via cannabidiol was independent of CB1 and CB2 receptors. These data are particularly relevant to atherosclerosis, since endothelial dysfunction is a crucial event in the initiation and progression of this pathogenesis.
Both endogenous as well as synthetic agonists 2-AG, CP55,940 and WIN55,212-2, as well as the CB2-selective agonists JWH-015 and JWH-133, caused a significant inhibition of the chemokine CXCL12-induced and CXCR4-mediated chemotaxis of Jurkat or primary human T cells (Ghosh et al., 2006; Coopman et al., 2007). In addition, in an experimental autoimmune encephalomyelitis mouse model, WIN 55,212-2 attenuated leukocyte rolling and adhesion on endothelial cells through the activation of CB2 receptors (Ni et al., 2004). Furthermore, the novel CB2-selective inverse agonist Sch.336 potently inhibited leukocyte chemotaxis to 2-AG, HU-210 or monocyte chemoattractant protein-11/CCL2 in vitro and in vivo (Lunn et al., 2006). In a mouse model of liver I/R injury, the CB2-selective agonist JWH-133 protected against I/R damage by decreasing inflammatory cell infiltration, tissue and serum tumour necrosis factor-α, macrophage inflammatory protein-1α/CCL3 and macrophage inflammatory protein-2/CXCL2 levels, and expression of ICAM-1 (Bátkai et al., 2007b). In vitro, JWH-133 was shown to attenuate the tumour necrosis factor-α-induced ICAM-1 and vascular cell adhesion molecule expression in human liver sinusoidal endothelial cells and the adhesion of human neutrophils to human liver sinusoidal endothelial cells. Similar results were obtained with the CB2-selective agonist HU-308 (Rajesh et al., 2007c). In a different study, anandamide dose dependently attenuated the tumour necrosis factor-α-induced ICAM-1 and vascular cell adhesion molecule expression in human coronary artery endothelial cells, and the adhesion of THP-1 monocytes to human coronary artery endothelial cells in a CB1- and CB2-dependent manner (Bátkai et al., 2007b). Likewise, the two CB2-selective agonists JWH-133 and HU-308 inhibited the tumour necrosis factor-α-induced nuclear factor-kappa B and RhoA activation, upregulation of adhesion molecules ICAM-1 and vascular cell adhesion molecule, increased expression of monocyte chemoattractant protein-11, enhanced transendothelial migration of THP-1 monocytes and augmented monocyte–endothelial adhesion (Rajesh et al., 2007b). Finally, we have shown that THC inhibited murine peritoneal macrophage chemotaxis in response to monocyte chemoattractant protein-11/CCL2 and reduced the expression of the chemokine receptor CCR2 on splenocytes (Steffens et al., 2005). These effects were blocked by the CB2 receptor antagonist SR144528 or when cells from CB2-knockout mice were used.
CB2-dependent effects of THC on atherosclerotic lesion progression
Based on the well-known immunomodulatory properties of cannabinoids, we tested the anti-atherosclerotic potential of THC in a murine model and found that THC inhibited progression of established atherosclerotic lesions (Steffens et al., 2005). The anti-atherosclerotic effect was associated with reduced proliferation and interferon-γ secretion of lymphoid cells, as well as reduced macrophage infiltration into atherosclerotic lesions. Moreover, we detected CB2 receptor expression on macrophages and T lymphocytes within human and mouse atherosclerotic lesions. These findings are promising; however, it is not possible to draw firm conclusions about the potential therapeutic effects in humans. Additional in vitro experiments with human vascular cells and clinical data are required to examine the underlying mechanisms of cannabinoid actions in humans.
Post-ischaemic heart failure
Heart failure occurs when the heart is unable to supply sufficient blood flow and thus oxygen delivery to the periphery. Besides coronary artery disease, a major cause of heart failure is myocardial infarction. Non-infarcted regions of the myocardium must compensate the lacking activity of the infarcted tissue, which can lead to changes in the morphology and size of the heart. This process known as remodelling may, over time, cause functional changes leading to cardiac failure.
In an attempt to study the long-term effects of endogenous and exogenous cannabinoids on cardiac remodelling and vascular function, Wagner et al. (2003) subjected rats to left coronary artery occlusion without reperfusion, followed by a 12-week CB1 antagonist (AM-251) or HU-210 treatment. Chronic CB1 antagonism had a deleterious effect on cardiac performance volume in rats, with large myocardial infarction (necrotic area>40% of left ventricle), suggesting that endocannabinoids prevent cardiac remodelling in this model. This study is in conflict with recently published findings, demonstrating that treatment with the CB1 antagonist rimonabant or AM-281 markedly improved cardiac dysfunction in doxorubicin-induced cardiotoxicity (Mukhopadhyay et al., 2007). A possible explanation for this discrepancy might be the use of low doses of the CB1 antagonist AM-251 (0.5 mg kg−1) in the previously mentioned study (Wagner et al., 2003), as well as the different species and methodologies used. In the long-term study, the non-selective cannabinoid agonist HU-210 increased the left ventricular end-diastolic pressure, but prevented hypotension (Wagner et al., 2003). In addition, HU-210 reduced endothelial dysfunction, as determined by vasodilator response of isolated aortic rings. Myocardial CB1 expression was not altered during remodelling. Remarkably, HU-210 appeared to be of benefit after small infarcts (⩽40%), since cardiac index and stroke volume index were increased, while the total peripheral resistance was decreased. This suggests that the benefit of exogenous cannabinoid intervention might be limited by infarct size. In a different report, the same authors show that the cannabinoids anandamide, R-methanandamide and HU-210 decrease contractile performance in human atrial muscle via CB1 receptors (Bonz et al., 2003). Maslov and co-workers studied the effect of HU-210 or cannabinoid receptor antagonist pretreatment on contractility in the isolated Langendorff-perfused rat heart model of I/R. They found that HU-210 transiently increased the degree of reperfusion-induced cardiac contractile dysfunction, whereas endogenous cannabinoids seem not involved in this process (Maslov et al., 2006).
Apart from this limited number of studies, little is known about the cannabinoid-mediated effects on cardiac performance. Therefore, further investigations with particular regard to long-term effects are needed to clarify this important aspect.
Concluding remarks
Synthetic and endogenous cannabinoids are known to exhibit complex cardiovascular actions, although the findings in humans and animal models are in part controversial, likely due to methodological and species differences. Over the centuries, the medical use of cannabinoids has been very limited, mainly due to the psychotropic effects associated with marijuana use. Now, synthetic non-psychotropic cannabinoids or pharmacological modulation of the endocannabinoid system may represent an emerging target for reducing acute and chronic cardiovascular complications in multiple risk factor patients. A future challenge for the scientific community is to overcome these experimental limitations in order to better understand the complex cardiovascular effects of cannabinoids in humans. This may allow the precise modulation of the endocannabinoid system via pharmacological intervention, without triggering detrimental cardiovascular side effects.
Acknowledgments
This work was supported by grants from the Swiss National Science Foundation to Dr Mach and Dr Steffens. The authors belong to the European Vascular Genomics Network (http://www.evgn.org) a Network of Excellence supported by the European Community.
Abbreviations
- ICAM-1
intercellular adhesion molecule-1
- I/R
ischaemia/reperfusion
- THC
delta-9-tetrahydrocannabinol
Conflict of interest
The authors state no conflict of interest.
References
- Abi-Younes S, Sauty A, Mach F, Sukhova GK, Libby P, Luster AD. The stromal cell-derived factor-1 chemokine is a potent platelet agonist highly expressed in atherosclerotic plaques. Circ Res. 2000;86:131–138. doi: 10.1161/01.res.86.2.131. [DOI] [PubMed] [Google Scholar]
- Aguado T, Romero E, Monory K, Palazuelos J, Sendtner M, Marsicano G, et al. The CB1 cannabinoid receptor mediates excitotoxicity-induced neural progenitor proliferation and neurogenesis. J Biol Chem. 2007;282:23892–23898. doi: 10.1074/jbc.M700678200. [DOI] [PubMed] [Google Scholar]
- Ashton JC, Rahman RM, Nair SM, Sutherland BA, Glass M, Appleton I. Cerebral hypoxia–ischemia and middle cerebral artery occlusion induce expression of the cannabinoid CB2 receptor in the brain. Neurosci Lett. 2007;412:114–117. doi: 10.1016/j.neulet.2006.10.053. [DOI] [PubMed] [Google Scholar]
- Bar-Joseph A, Berkovitch Y, Adamchik J, Biegon A. Neuroprotective activity of HU-211, a novel NMDA antagonist, in global ischemia in gerbils. Mol Chem Neuropathol. 1994;23:125–135. doi: 10.1007/BF02815406. [DOI] [PubMed] [Google Scholar]
- Bátkai S, Járai Z, Wagner JA, Goparaju SK, Varga K, Liu J, et al. Endocannabinoids acting at vascular CB1 receptors mediate the vasodilated state in advanced liver cirrhosis. Nat Med. 2001;7:827–832. doi: 10.1038/89953. [DOI] [PubMed] [Google Scholar]
- Bátkai S, Mukhopadhyay P, Harvey-White J, Kechrid R, Pacher P, Kunos G. Endocannabinoids acting at CB1 receptors mediate the cardiac contractile dysfunction in vivo in cirrhotic rats. Am J Physiol Heart Circ Physiol. 2007a;293:H1689–H1695. doi: 10.1152/ajpheart.00538.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bátkai S, Osei-Hyiaman D, Pan H, El-Assal O, Rajesh M, Mukhopadhyay P, et al. Cannabinoid-2 receptor mediates protection against hepatic ischemia/reperfusion injury. FASEB J. 2007b;21:1788–1800. doi: 10.1096/fj.06-7451com. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bátkai S, Pacher P, Osei-Hyiaman D, Radaeva S, Liu J, Harvey-White J, et al. Endocannabinoids acting at cannabinoid-1 receptors regulate cardiovascular function in hypertension. Circulation. 2004;110:1996–2002. doi: 10.1161/01.CIR.0000143230.23252.D2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bátkai S, Rajesh M, Mukhopadhyay P, Haskó G, Liaudet L, Cravatt BF, et al. Decreased age-related cardiac dysfunction, myocardial nitrative stress, inflammatory gene expression and apoptosis in mice lacking fatty acid amide hydrolase. Am J Physiol Heart Circ Physiol. 2007c;293:H909–H918. doi: 10.1152/ajpheart.00373.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beaconsfield P. Some cardiovascular effects of cannabis. Am Heart J. 1974;87:143–146. doi: 10.1016/0002-8703(74)90033-7. [DOI] [PubMed] [Google Scholar]
- Berger C, Schmid PC, Schabitz WR, Wolf M, Schwab S, Schmid HH. Massive accumulation of N-acylethanolamines after stroke. Cell signalling in acute cerebral ischemia? J Neurochem. 2004;88:1159–1167. doi: 10.1046/j.1471-4159.2003.02244.x. [DOI] [PubMed] [Google Scholar]
- Bonz A, Laser M, Küllmer S, Kniesch S, Babin-Ebell J, Popp V, et al. Cannabinoids acting on CB1 receptors decrease contractile performance in human atrial muscle. J Cardiovasc Pharmacol. 2003;41:657–664. doi: 10.1097/00005344-200304000-00020. [DOI] [PubMed] [Google Scholar]
- Bouchard JF, Lépicier P, Lamontagne D. Contribution of endocannabinoids in the endothelial protection afforded by ischemic preconditioning in the isolated rat heart. Life Sci. 2003;72:1859–1870. doi: 10.1016/s0024-3205(02)02474-8. [DOI] [PubMed] [Google Scholar]
- Braunersreuther V, Mach F. Leukocyte recruitment in atherosclerosis: potential targets for therapeutic approaches? Cell Mol Life Sci. 2006;63:2079–2088. doi: 10.1007/s00018-006-6127-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carrier EJ, Kearn CS, Barkmeier AJ, Breese NM, Yang W, Nithipatikom K, et al. Cultured rat microglial cells synthesize the endocannabinoid 2-arachidonylglycerol, which increases proliferation via a CB2 receptor-dependent mechanism. Mol Pharmacol. 2004;65:999–1007. doi: 10.1124/mol.65.4.999. [DOI] [PubMed] [Google Scholar]
- Coopman K, Smith LD, Wright KL, Ward SG. Temporal variation in CB2R levels following T lymphocyte activation: evidence that cannabinoids modulate CXCL12-induced chemotaxis. Int Immunopharmacol. 2007;7:360–371. doi: 10.1016/j.intimp.2006.11.008. [DOI] [PubMed] [Google Scholar]
- Crawford WJ, Merritt JC. Effects of tetrahydrocannabinol on arterial and intraocular hypertension. Int J Clin Pharmacol Biopharm. 1979;17:191–196. [PubMed] [Google Scholar]
- Després JP, Golay A, Sjöström L, Rimonabant in Obesity-Lipids Study Group Effects of rimonabant on metabolic risk factors in overweight patients with dyslipidemia. N Engl J Med. 2005;353:2121–2134. doi: 10.1056/NEJMoa044537. [DOI] [PubMed] [Google Scholar]
- Deusch E, Kress HG, Kraft B, Kozek-Langenecker SA.The procoagulatory effects of delta-9-tetrahydrocannabinol in human platelets Anesth Analg 2004991127–1130.table of contents [DOI] [PubMed] [Google Scholar]
- Dewey WL. Cannabinoid pharmacology. Pharmacol Rev. 1986;38:151–178. [PubMed] [Google Scholar]
- Di Filippo C, Rossi F, Rossi S, D'Amico M. Cannabinoid CB2 receptor activation reduces mouse myocardial ischemia–reperfusion injury: involvement of cytokine/chemokines and PMN. J Leukoc Biol. 2004;75:453–459. doi: 10.1189/jlb.0703303. [DOI] [PubMed] [Google Scholar]
- Formukong EA, Evans AT, Evans FJ. The inhibitory effects of cannabinoids, the active constituents of Cannabis sativa L. on human and rabbit platelet aggregation. J Pharm Pharmacol. 1989;41:705–709. doi: 10.1111/j.2042-7158.1989.tb06345.x. [DOI] [PubMed] [Google Scholar]
- Fredericks AB, Benowitz NL, Savanapridi CY. The cardiovascular and autonomic effects of repeated administration of delta-9-tetrahydrocannabinol to Rhesus monkeys. J Pharmacol Exp Ther. 1981;216:247–253. [PubMed] [Google Scholar]
- Galve-Roperh I, Aguado T, Palazuelos J, Guzmán M. The endocannabinoid system and neurogenesis in health and disease. Neuroscientist. 2007;13:109–114. doi: 10.1177/1073858406296407. [DOI] [PubMed] [Google Scholar]
- Gawaz M, Langer H, May AE. Platelets in inflammation and atherogenesis. J Clin Invest. 2005;115:3378–3384. doi: 10.1172/JCI27196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gelfand EV, Cannon CP. Rimonabant: a cannabinoid receptor type 1 blocker for management of multiple cardiometabolic risk factors. J Am Coll Cardiol. 2006;47:1919–1926. doi: 10.1016/j.jacc.2005.12.067. [DOI] [PubMed] [Google Scholar]
- Ghosh S, Preet A, Groopman JE, Ganju RK. Cannabinoid receptor CB(2) modulates the CXCL12/CXCR4-mediated chemotaxis of T lymphocytes. Mol Immunol. 2006;43:2169–2179. doi: 10.1016/j.molimm.2006.01.005. [DOI] [PubMed] [Google Scholar]
- Glass CK, Witztum JL. Atherosclerosis. The road ahead. Cell. 2001;104:503–516. doi: 10.1016/s0092-8674(01)00238-0. [DOI] [PubMed] [Google Scholar]
- Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–1695. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- Hansson GK, Libby P. The immune response in atherosclerosis: a double-edged sword. Nat Rev Immunol. 2006;6:508–519. doi: 10.1038/nri1882. [DOI] [PubMed] [Google Scholar]
- Hayakawa K, Mishima K, Nozako M, Hazekawa M, Aoyama Y, Ogata A, et al. High-cholesterol feeding aggravates cerebral infarction via decreasing the CB1 receptor. Neurosci Lett. 2007;414:183–187. doi: 10.1016/j.neulet.2006.12.022. [DOI] [PubMed] [Google Scholar]
- Hollister LE. Health aspects of cannabis. Pharmacol Rev. 1986;38:1–20. [PubMed] [Google Scholar]
- Jones RT. Cardiovascular system effects of marijuana. J Clin Pharmacol. 2002;42:58S–63S. doi: 10.1002/j.1552-4604.2002.tb06004.x. [DOI] [PubMed] [Google Scholar]
- Joyeux M, Arnaud C, Godin-Ribuot D, Demenge P, Lamontagne D, Ribuot C. Endocannabinoids are implicated in the infarct size-reducing effect conferred by heat stress preconditioning in isolated rat hearts. Cardiovasc Res. 2002;55:619–625. doi: 10.1016/s0008-6363(02)00268-7. [DOI] [PubMed] [Google Scholar]
- Julien B, Grenard P, Teixeira-Clerc F, Van Nhieu JT, Li L, Karsak M, et al. Antifibrogenic role of the cannabinoid receptor CB2 in the liver. Gastroenterology. 2005;128:742–755. doi: 10.1053/j.gastro.2004.12.050. [DOI] [PubMed] [Google Scholar]
- Kanakis C, Pouget M, Rosen KM. Lack of cardiovascular effects of delta-9-tetrahydrocannabinol in chemically denervated men. Ann Intern Med. 1979;91:571–574. doi: 10.7326/0003-4819-91-4-571. [DOI] [PubMed] [Google Scholar]
- Karsak M, Gaffal E, Date R, Wang-Eckhardt L, Rehnelt J, Petrosino S, et al. Attenuation of allergic contact dermatitis through the endocannabinoid system. Science. 2007;316:1494–1497. doi: 10.1126/science.1142265. [DOI] [PubMed] [Google Scholar]
- Klein TW. Cannabinoid-based drugs as anti-inflammatory therapeutics. Nat Rev Immunol. 2005;5:400–411. doi: 10.1038/nri1602. [DOI] [PubMed] [Google Scholar]
- Klein TW, Newton C, Larsen K, Lu L, Perkins I, Nong L, et al. The cannabinoid system and immune modulation. J Leukoc Biol. 2003;74:486–496. doi: 10.1189/jlb.0303101. [DOI] [PubMed] [Google Scholar]
- Klijn CJ, Hankey GJ, American Stroke Association and European Stroke Initiative Management of acute ischaemic stroke: new guidelines from the American Stroke Association and European Stroke Initiative. Lancet Neurol. 2003;2:698–701. doi: 10.1016/s1474-4422(03)00558-1. [DOI] [PubMed] [Google Scholar]
- Kowalska MA, Ratajczak MZ, Majka M, Jin J, Kunapuli S, Brass L, et al. Stromal cell-derived factor-1 and macrophage-derived chemokine: 2 chemokines that activate platelets. Blood. 2000;96:50–57. [PubMed] [Google Scholar]
- Krylatov AV, Ugdyzhekova DS, Bernatskaya NA, Maslov LN, Mekhoulam R, Pertwee RG, et al. Activation of type II cannabinoid receptors improves myocardial tolerance to arrhythmogenic effects of coronary occlusion and reperfusion. Bull Exp Biol Med. 2001;131:523–525. doi: 10.1023/a:1012381914518. [DOI] [PubMed] [Google Scholar]
- Lagneux C, Lamontagne D. Involvement of cannabinoids in the cardioprotection induced by lipopolysaccharide. Br J Pharmacol. 2001;132:793–796. doi: 10.1038/sj.bjp.0703902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavie G, Teichner A, Shohami E, Ovadia H, Leker RR. Long term cerebroprotective effects of dexanabinol in a model of focal cerebral ischemia. Brain Res. 2001;901:195–201. doi: 10.1016/s0006-8993(01)02356-3. [DOI] [PubMed] [Google Scholar]
- Leker RR, Gai N, Mechoulam R, Ovadia H. Drug-induced hypothermia reduces ischemic damage: effects of the cannabinoid HU-210. Stroke. 2003;34:2000–2006. doi: 10.1161/01.STR.0000079817.68944.1E. [DOI] [PubMed] [Google Scholar]
- Leker RR, Shohami E, Abramsky O, Ovadia H. Dexanabinol: a novel neuroprotective drug in experimental focal cerebral ischemia. J Neurol Sci. 1999;162:114–119. doi: 10.1016/s0022-510x(98)00301-3. [DOI] [PubMed] [Google Scholar]
- Lépicier P, Bouchard JF, Lagneux C, Lamontagne D. Endocannabinoids protect the rat isolated heart against ischaemia. Br J Pharmacol. 2003;139:805–815. doi: 10.1038/sj.bjp.0705313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy R, Schurr A, Nathan I, Dvilanski A, Livne A. Impairment of ADP-induced platelet aggregation by hashish components. Thromb Haemost. 1976;36:634–640. [PubMed] [Google Scholar]
- Libby P. Inflammation in atherosclerosis. Nature. 2002;420:868–874. doi: 10.1038/nature01323. [DOI] [PubMed] [Google Scholar]
- Libby P, Aikawa M. Stabilization of atherosclerotic plaques: new mechanisms and clinical targets. Nat Med. 2002;8:1257–1262. doi: 10.1038/nm1102-1257. [DOI] [PubMed] [Google Scholar]
- Liu J, Batkai S, Pacher P, Harvey-White J, Wagner JA, Cravatt BF, et al. Lipopolysaccharide induces anandamide synthesis in macrophages via CD14/MAPK/phosphoinositide 3-kinase/NF-kappaB independently of platelet-activating factor. J Biol Chem. 2003;278:45034–45039. doi: 10.1074/jbc.M306062200. [DOI] [PubMed] [Google Scholar]
- Lunn CA, Fine JS, Rojas-Triana A, Jackson JV, Fan X, Kung TT, et al. A novel cannabinoid peripheral cannabinoid receptor-selective inverse agonist blocks leukocyte recruitment in vivo. J Pharmacol Exp Ther. 2006;316:780–788. doi: 10.1124/jpet.105.093500. [DOI] [PubMed] [Google Scholar]
- Lusis AJ. Atherosclerosis. Nature. 2000;407:233–241. doi: 10.1038/35025203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mach F. Statins as immunomodulatory agents. Circulation. 2004;109:II15–II17. doi: 10.1161/01.CIR.0000129502.10459.fe. [DOI] [PubMed] [Google Scholar]
- Maresz K, Pryce G, Ponomarev ED, Marsicano G, Croxford JL, Shriver LP, et al. Direct suppression of CNS autoimmune inflammation via the cannabinoid receptor CB1 on neurons and CB2 on autoreactive T cells. Nat Med. 2007;13:492–497. doi: 10.1038/nm1561. [DOI] [PubMed] [Google Scholar]
- Maslov LN, Lasukova OV, Krylatov AV, Hanus LO, Pertwee R, Ivanchuk II, et al. Role of cannabinoid receptors in the regulation of cardiac contractility during ischemia/reperfusion. Bull Exp Biol Med. 2006;142:557–561. doi: 10.1007/s10517-006-0417-4. [DOI] [PubMed] [Google Scholar]
- Massa F, Marsicano G, Hermann H, Cannich A, Monory K, Cravatt BF, et al. The endogenous cannabinoid system protects against colonic inflammation. J Clin Invest. 2004;113:1202–1209. doi: 10.1172/JCI19465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathew RJ, Wilson WH, Humphreys D, Lowe JV, Wiethe KE. Middle cerebral artery velocity during upright posture after marijuana smoking. Acta Psychiatr Scand. 1992;86:173–178. doi: 10.1111/j.1600-0447.1992.tb03247.x. [DOI] [PubMed] [Google Scholar]
- Mauler F, Horváth E, De Vry J, Jäger R, Schwarz T, Sandmann S, et al. BAY 38–7271: a novel highly selective and highly potent cannabinoid receptor agonist for the treatment of traumatic brain injury. CNS Drug Rev. 2003;9:343–358. doi: 10.1111/j.1527-3458.2003.tb00259.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendizábal VE, Adler-Graschinsky E. Cannabinoids as therapeutic agents in cardiovascular disease: a tale of passions and illusions. Br J Pharmacol. 2007;151:427–440. doi: 10.1038/sj.bjp.0707261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mittleman MA, Lewis RA, Maclure M, Sherwood JB, Muller JE. Triggering myocardial infarction by marijuana. Circulation. 2001;103:2805–2809. doi: 10.1161/01.cir.103.23.2805. [DOI] [PubMed] [Google Scholar]
- Mukhopadhyay P, Bátkai S, Rajesh M, Czifra N, Harvey-White J, Haskó G, et al. Pharmacological inhibition of CB1 cannabinoid receptor protects against doxorubicin-induced cardiotoxicity. J Am Coll Cardiol. 2007;50:528–536. doi: 10.1016/j.jacc.2007.03.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269–1276. doi: 10.1016/S0140-6736(96)07493-4. [DOI] [PubMed] [Google Scholar]
- Muthian S, Rademacher DJ, Roelke CT, Gross GJ, Hillard CJ. Anandamide content is increased and CB1 cannabinoid receptor blockade is protective during transient, focal cerebral ischemia. Neuroscience. 2004;129:743–750. doi: 10.1016/j.neuroscience.2004.08.044. [DOI] [PubMed] [Google Scholar]
- Nagayama T, Sinor AD, Simon RP, Chen J, Graham SH, Jin K, et al. Cannabinoids and neuroprotection in global and focal cerebral ischemia and in neuronal cultures. J Neurosci. 1999;19:2987–2995. doi: 10.1523/JNEUROSCI.19-08-02987.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakajima Y, Furuichi Y, Biswas KK, Hashiguchi T, Kawahara K, Yamaji K, et al. Endocannabinoid, anandamide in gingival tissue regulates the periodontal inflammation through NF-kappaB pathway inhibition. FEBS Lett. 2006;580:613–619. doi: 10.1016/j.febslet.2005.12.079. [DOI] [PubMed] [Google Scholar]
- Nelken NA, Coughlin SR, Gordon D, Wilcox JN. Monocyte chemoattractant protein-1 in human atheromatous plaques. J Clin Invest. 1991;88:1121–1127. doi: 10.1172/JCI115411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby AC. Dual role of matrix metalloproteinases (matrixins) in intimal thickening and atherosclerotic plaque rupture. Physiol Rev. 2005;85:1–31. doi: 10.1152/physrev.00048.2003. [DOI] [PubMed] [Google Scholar]
- Ni X, Geller EB, Eppihimer MJ, Eisenstein TK, Adler MW, Tuma RF. Win 55212-2, a cannabinoid receptor agonist, attenuates leukocyte/endothelial interactions in an experimental autoimmune encephalomyelitis model. Mult Scler. 2004;10:158–164. doi: 10.1191/1352458504ms1009oa. [DOI] [PubMed] [Google Scholar]
- Nieswandt B, Aktas B, Moers A, Sachs UJ. Platelets in atherothrombosis: lessons from mouse models. J Thromb Haemost. 2005;3:1725–1736. doi: 10.1111/j.1538-7836.2005.01488.x. [DOI] [PubMed] [Google Scholar]
- Osterud B, Bjorklid E. Role of monocytes in atherogenesis. Physiol Rev. 2003;83:1069–1112. doi: 10.1152/physrev.00005.2003. [DOI] [PubMed] [Google Scholar]
- Pacher P, Bátkai S, Kunos G. Blood pressure regulation by endocannabinoids and their receptors. Neuropharmacology. 2005a;48:1130–1138. doi: 10.1016/j.neuropharm.2004.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacher P, Bátkai S, Kunos G. Cardiovascular pharmacology of cannabinoids. Handb Exp Pharmacol. 2005b;168:599–625. doi: 10.1007/3-540-26573-2_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacher P, Bátkai S, Kunos G. The endocannabinoid system as an emerging target of pharmacotherapy. Pharmacol Rev. 2006;58:389–462. doi: 10.1124/pr.58.3.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacher P, Bátkai S, Osei-Hyiaman D, Offertáler L, Liu J, Harvey-White J, et al. Hemodynamic profile, responsiveness to anandamide, and baroreflex sensitivity of mice lacking fatty acid amide hydrolase. Am J Physiol Heart Circ Physiol. 2005c;289:H533–H541. doi: 10.1152/ajpheart.00107.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panikashvili D, Mechoulam R, Beni SM, Alexandrovich A, Shohami E. CB1 cannabinoid receptors are involved in neuroprotection via NF-kappa B inhibition. J Cereb Blood Flow Metab. 2005;25:477–484. doi: 10.1038/sj.jcbfm.9600047. [DOI] [PubMed] [Google Scholar]
- Panikashvili D, Simeonidou C, Ben-Shabat S, Hanus L, Breuer A, Mechoulam R, et al. An endogenous cannabinoid (2-AG) is neuroprotective after brain injury. Nature. 2001;413:527–531. doi: 10.1038/35097089. [DOI] [PubMed] [Google Scholar]
- Parmentier-Batteur S, Jin K, Mao XO, Xie L, Greenberg DA. Increased severity of stroke in CB1 cannabinoid receptor knockout mice. J Neurosci. 2002;22:9771–9775. doi: 10.1523/JNEUROSCI.22-22-09771.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinto A, Tuttolomondo A, Di Raimondo D, Fernandez P, Licata G. Cerebrovascular risk factors and clinical classification of strokes. Semin Vasc Med. 2004;4:287–303. doi: 10.1055/s-2004-861497. [DOI] [PubMed] [Google Scholar]
- Rajesh M, Mukhopadhyay P, Bátkai S, Haskó G, Liaudet L, Drel VR, et al. Cannabidiol attenuates high glucose-induced endothelial cell inflammatory response and barrier disruption. Am J Physiol Heart Circ Physiol. 2007a;293:H610–H619. doi: 10.1152/ajpheart.00236.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajesh M, Mukhopadhyay P, Batkai S, Hasko G, Liaudet L, Huffman JW, et al. Cannabinoid-2 receptor stimulation attenuates TNF{alpha}-induced human endothelial cell activation, transendothelial migration of monocytes, and monocyte-endothelial adhesion. Am J Physiol Heart Circ Physiol. 2007b;293:2210–2218. doi: 10.1152/ajpheart.00688.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajesh M, Pan H, Mukhopadhyay P, Bátkai S, Osei-Hyiaman D, Haskó G, et al. Pivotal Advance: cannabinoid-2 receptor agonist HU-308 protects against hepatic ischemia/reperfusion injury by attenuating oxidative stress, inflammatory response, and apoptosis J Leukoc Biol 2007c. 82:(in press) [DOI] [PMC free article] [PubMed]
- Sacerdote P, Martucci C, Vaccani A, Bariselli F, Panerai AE, Colombo A, et al. The nonpsychoactive component of marijuana cannabidiol modulates chemotaxis and IL-10 and IL-12 production of murine macrophages both in vivo and in vitro. J Neuroimmunol. 2005;159:97–105. doi: 10.1016/j.jneuroim.2004.10.003. [DOI] [PubMed] [Google Scholar]
- Sacerdote P, Massi P, Panerai AE, Parolaro D. In vivo and in vitro treatment with the synthetic cannabinoid CP55, 940 decreases the in vitro migration of macrophages in the rat: involvement of both CB1 and CB2 receptors. J Neuroimmunol. 2000;109:155–163. doi: 10.1016/s0165-5728(00)00307-6. [DOI] [PubMed] [Google Scholar]
- Schecter AD, Calderon TM, Berman AB, McManus CM, Fallon JT, Rossikhina M, et al. Human vascular smooth muscle cells possess functional CCR5. J Biol Chem. 2000;275:5466–5471. doi: 10.1074/jbc.275.8.5466. [DOI] [PubMed] [Google Scholar]
- Scheuerer B, Ernst M, Dürrbaum-Landmann I, Fleischer J, Grage-Griebenow E, Brandt E, et al. The CXC–chemokine platelet factor 4 promotes monocyte survival and induces monocyte differentiation into macrophages. Blood. 2000;95:1158–1166. [PubMed] [Google Scholar]
- Sidney S. Cardiovascular consequences of marijuana use. J Clin Pharmacol. 2002;42:64S–70S. doi: 10.1002/j.1552-4604.2002.tb06005.x. [DOI] [PubMed] [Google Scholar]
- Sinor AD, Irvin SM, Greenberg DA. Endocannabinoids protect cerebral cortical neurons from in vitro ischemia in rats. Neurosci Lett. 2000;278:157–160. doi: 10.1016/s0304-3940(99)00922-2. [DOI] [PubMed] [Google Scholar]
- Sommer C, Schomacher M, Berger C, Kuhnert K, Müller HD, Schwab S, et al. Neuroprotective cannabinoid receptor antagonist SR141716A prevents downregulation of excitotoxic NMDA receptors in the ischemic penumbra. Acta Neuropathol (Berlin) 2006;112:277–286. doi: 10.1007/s00401-006-0110-8. [DOI] [PubMed] [Google Scholar]
- Steffens S, Veillard NR, Arnaud C, Pelli G, Burger F, Staub C, et al. Low dose oral cannabinoid therapy reduces progression of atherosclerosis in mice. Nature. 2005;434:782–786. doi: 10.1038/nature03389. [DOI] [PubMed] [Google Scholar]
- Teixeira-Clerc F, Julien B, Grenard P, Tran Van Nhieu J, Deveaux V, Li L, et al. CB1 cannabinoid receptor antagonism: a new strategy for the treatment of liver fibrosis. Nat Med. 2006;12:671–676. doi: 10.1038/nm1421. [DOI] [PubMed] [Google Scholar]
- Underdown NJ, Hiley CR, Ford WR. Anandamide reduces infarct size in rat isolated hearts subjected to ischaemia–reperfusion by a novel cannabinoid mechanism. Br J Pharmacol. 2005;146:809–816. doi: 10.1038/sj.bjp.0706391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Gaal LF, Rissanen AM, Scheen AJ, Ziegler O, Rössner S, RIO-Europe Study Group AN Effects of the cannabinoid-1 receptor blocker rimonabant on weight reduction and cardiovascular risk factors in overweight patients: 1-year experience from the RIO-Europe study. Lancet. 2005;365:1389–1397. doi: 10.1016/S0140-6736(05)66374-X. [DOI] [PubMed] [Google Scholar]
- Varga K, Wagner JA, Bridgen DT, Kunos G. Platelet- and macrophage-derived endogenous cannabinoids are involved in endotoxin-induced hypotension. FASEB J. 1998;12:1035–1044. doi: 10.1096/fasebj.12.11.1035. [DOI] [PubMed] [Google Scholar]
- Veillard NR, Steffens S, Burger F, Pelli G, Mach F. Differential expression patterns of proinflammatory and antiinflammatory mediators during atherogenesis in mice. Arterioscler Thromb Vasc Biol. 2004;24:2339–2344. doi: 10.1161/01.ATV.0000146532.98235.e6. [DOI] [PubMed] [Google Scholar]
- von Hundelshausen P, Weber KS, Huo Y, Proudfoot AE, Nelson PJ, Ley K, et al. RANTES deposition by platelets triggers monocyte arrest on inflamed and atherosclerotic endothelium. Circulation. 2001;103:1772–1777. doi: 10.1161/01.cir.103.13.1772. [DOI] [PubMed] [Google Scholar]
- Wagner JA, Hu K, Karcher J, Bauersachs J, Schäfer A, Laser M, et al. CB(1) cannabinoid receptor antagonism promotes remodeling and cannabinoid treatment prevents endothelial dysfunction and hypotension in rats with myocardial infarction. Br J Pharmacol. 2003;138:1251–1258. doi: 10.1038/sj.bjp.0705156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner JA, Varga K, Ellis EF, Rzigalinski BA, Martin BR, Kunos G. Activation of peripheral CB1 cannabinoid receptors in haemorrhagic shock. Nature. 1997;390:518–521. doi: 10.1038/37371. [DOI] [PubMed] [Google Scholar]
- Wang Y, Liu Y, Ito Y, Hashiguchi T, Kitajima I, Yamakuchi M, et al. Simultaneous measurement of anandamide and 2-arachidonoylglycerol by polymyxin B-selective adsorption and subsequent high-performance liquid chromatography analysis: increase in endogenous cannabinoids in the sera of patients with endotoxic shock. Anal Biochem. 2001;294:73–82. doi: 10.1006/abio.2001.5015. [DOI] [PubMed] [Google Scholar]
- Weber C. Platelets and chemokines in atherosclerosis: partners in crime. Circ Res. 2005;96:612–616. doi: 10.1161/01.RES.0000160077.17427.57. [DOI] [PubMed] [Google Scholar]
- Weber C, Schober A, Zernecke A. Chemokines: key regulators of mononuclear cell recruitment in atherosclerotic vascular disease. Arterioscler Thromb Vasc Biol. 2004;24:1997–2008. doi: 10.1161/01.ATV.0000142812.03840.6f. [DOI] [PubMed] [Google Scholar]
- Ylä-Herttuala S, Lipton BA, Rosenfeld ME, Särkioja T, Yoshimura T, Leonard EJ, et al. Expression of monocyte chemoattractant protein 1 in macrophage-rich areas of human and rabbit atherosclerotic lesions. Proc Natl Acad Sci USA. 1991;88:5252–5256. doi: 10.1073/pnas.88.12.5252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu X, Dluz S, Graves DT, Zhang L, Antoniades HN, Hollander W, et al. Elevated expression of monocyte chemoattractant protein 1 by vascular smooth muscle cells in hypercholesterolemic primates. Proc Natl Acad Sci USA. 1992;89:6953–6957. doi: 10.1073/pnas.89.15.6953. [DOI] [PMC free article] [PubMed] [Google Scholar]