Abstract
This study presents findings from a quasiexperimental, nonequivalent, group-design study with repeated measures that explored the effects of integrated trauma-informed services on the severity of substance abuse, mental health, posttraumatic stress disorder (PTSD) symptomatology among women with histories of trauma in urban, community-based substance abuse treatment. The study also explored if the model of integrated services was equally beneficial for women of various racial/ethnic groups. Participants in the study were 342 women receiving substance abuse treatment in intervention and comparison sites. Results indicated that at 6 and 12 month follow-ups, those in the trauma-informed intervention group, in contrast to the comparison group, had significantly better outcomes in drug abstinence rates in the past 30 days as well as in mental health and PTSD symptomatology. Results also showed that, overall, integrated services were beneficial for women across the different racial/ethnic groups in substance abuse treatment, although some differences appear to exist across racial/ethnic groups in improving addiction severity and mental health and PTSD symptomatology.
Keywords: Co-occurring disorders, Race/Ethnic differences, Substance abuse treatment, Trauma, Women.
INTRODUCTION
Studies have documented the impact of contextual factors on posttraumatic stress disorder (PTSD). Posttraumatic stress disorder is a commonly occurring disorder associated with exposure to multiple traumas, such as assaultive violence,1 repetitive childhood physical or sexual assault,2 partner violence, and, most recently, community violence,3 especially among low-income and urban residents.
Especially worrisome is the fact that rates of exposure to at least one traumatic lifetime event (using DSM-III-R criteria) have been reported at 60.7 and 51.2% for men and women, respectively,4 by respondents of the U.S. National Comorbidity Survey and as high as 90% (using DSM-IV criteria) among a community sample of respondents.1 Furthermore, in the U.S. National Comorbidity Survey sample, the average number of lifetime traumatic events experienced was 3.3.
Among women with substance abuse disorders the rates are significantly higher. In a detailed review of PTSD among women with substance use disorders, Najavits et al.2 reported estimated rates of lifetime history of trauma that ranged from 55 to 99%. In addition, high prevalence rates of comorbid PTSD and substance abuse disorders have been documented among women, especially those with a history of repetitive childhood physical or sexual assault. For this group the rates of lifetime history of trauma ranged from 32 to 66%. Moreover, among both men and women with substance abuse problems, and women residing in an inner-city neighborhood, studies have documented an average of five lifetime traumas experienced.2 Thus, integrated substance abuse treatment approaches that incorporate treatment of trauma are especially relevant for urban populations.
Posttraumatic Stress Disorders and Substance Use Disorders
Exposure to traumatic events and PTSD can have a severe impact on an individual’s health, health care utilization, general functioning, and other aspects of quality of life.5,6 For example, according to the U.S. National Comorbidity Survey, respondents with PTSD at the time of the interview had higher odds of high school and college failure, teenage childbearing, marital instability, and current unemployment (40, 30, 60, and 150%, respectively) compared to respondents without PTSD.1
Individuals with PTSD may have high rates of substance use disorders and other comorbid mental illness. Women with acute levels of traumatic stress show higher levels of substance use, mental and physical health problems, and greater HIV risk behaviors, compared to men and women with lower traumatic symptomatology.7 Moreover, for those persons receiving treatment for mental health disorders and/or posttraumatic stress/substance use disorders, higher drop-out rates are reported for persons with a history of physical or sexual abuse or a history of child abuse/neglect.8 Amaro et al.9 also reported that Latina women with a history of childhood abuse receiving services in a residential substance abuse program were more likely to drop out in the early stages of treatment than those without such history. In another study, Thompson and Kingree10 reported that treatment completion in a residential substance abuse treatment program for low-income pregnant women was related to PTSD.
Integrated Treatment Approach
There is growing agreement that an integrated treatment approach is a more appropriate model9–14 than treatments that address each disorder separately. Previous studies have also shown strong preference among women with a dual diagnosis for integrated treatment.13,15 Some components for successful integrated treatment models include stages of change components, motivational interviewing, and cognitive-behavioral interventions,11,12,16,17 plus screening for trauma and health problems as well as an approach that builds on safety and empowerment in the community.18 For women with a substance abuse or dependence disorder, especially PTSD, it has been suggested that comprehensive treatments should address substance use and directly intervene with PTSD symptoms and quality of life concerns such as vocational issues and social support.12,19,20 Integrated treatment has shown promising results, especially among disadvantaged minority populations.21
Given the higher risk of drop-out among minority women in substance abuse treatment20,22–25 combined with high rates of histories of trauma among urban populations1,4 and the lack of integrated substance abuse services,21,26 the present study sought to test a model of integrated treatment for women with cooccurring disorders living in urban communities. The treatment approach in this intervention was based on a growing research and clinical consensus about the diversity and complexity of long-term adaptations to traumatic events, especially those involving interpersonal violence.27,28 As noted above, increased risk of drug abuse is a well-established consequence of trauma exposure. Other areas of functioning may be negatively affected as well, leading to affective dysregulation,29 emotional numbness and dissociation,30 interpersonal relationship difficulties,31 and depression.32 Consistent with a broadly conceived recovery or rehabilitative approach appropriate for people with multiple problems,33 the present intervention approach integrated emphases on symptom reduction and skill development using cognitive-behavioral and skill-building approaches.34 Specifically, the intervention aimed to decrease symptomatology and negative coping such as drug use through development of skills fundamental to trauma recovery.35 It emphasized the use of active coping skills such as self-soothing, emotional modulation, and the development of safe, supportive, and mutual interpersonal relationships as key elements in psychosocial well-being.
The study sought to answer the following questions: (1) Compared to services as usual, does integrated trauma and substance abuse treatment result in better outcomes as measured by alcohol and drug use severity, mental health symptomatology, and PTSD symptoms? (2) Is the integrated care model equally efficacious for women of various racial/ethnic groups?
METHODS
Design and Procedures
The study used a quasiexperimental, nonequivalent group design with repeated measures comparing clients in the intervention group (receiving trauma-informed services) with a services-as-usual comparison group. Data in this paper came from participants in the Women, Co-occurring Disorders and Violence Study (WCDVS) Boston study site (Boston Consortium of Services for Families in Recovery, hereafter referred to as BCSFR). For a full description of the WCDVS study design, see McHugo et al.;36 for a full description of the BCSFR model, see Amaro et al.37
Study participants were enrolled from March 2001 to February 2002 and data were collected using structured in-person interviews from participants in the Boston study site, including baseline 6- and 12-month postbaseline in-person interviews conducted in the participant’s preferred language (English or Spanish) by trained interviewers who reflected the racial/ethnic composition of the study sample. Participants were recruited from consecutive admissions to the comparison and intervention program sites if they were determined to meet the following criteria by their primary counselor: Women were eligible to participate if they were at least 18 years of age and had experienced physical or sexual abuse. Women also had to meet criteria for a DSM-IV Axis I Substance Abuse Disorder, and an Axis I Mental Disorder or Axis II Personality Disorder. Based on clinician advice, those excluded were women in an especially sensitive state, that is, those who may not have been able to give reasonable answers to the interview and those for whom the interview could have triggered the reexperience of traumatic events.
Research staff approached eligible clients, explained the study, and obtained informed consent according to the protocol approved by the Institutional Review Boards of the Northeastern University, New England Research Institutes, and Boston University Medical Center. Participants were compensated $20, $40, and $40 for the baseline, 6 months, and 12 months interviews, respectively.
The present study used an intent-to-treat design, which requires that all participants (including those who dropped from the intervention or from the assessment) be included in the analyses.
Sample
At baseline, the sample for this study consisted of 342 women (181 in the intervention group and 161 in the comparison group) enrolled in the Boston site of the WCDVS funded by the Substance Abuse and Mental Health Services Administration (SAMHSA). The sample follow-up rates were 77% at 6 months and 76% at 12 months, with similar retention rates across intervention and comparison groups.
The mean age of the sample was 37.32 years (SD = 8.03). The majority was unemployed (92%) and had received less than a high school education (54%). The sample was comprised of 35% non-Hispanic white, 35% Hispanic, 26% non-Hispanic African American, and 5% American Indian and Asian combined. Hispanic women were primarily Puerto Ricans (90%) or Dominicans (2%).
Measures
The measures reported in this study were part of a larger assessment battery administered to participants based on the WCDVS protocol (for details on these measures, see McHugo et al.36). The average completion time for the larger assessment battery ranged from 70 to 85 min.
Measures That Characterize the Population
The measures that characterize the population were participants’ social demographic information (i.e., age, race, ethnicity, educational attainment, employment status, if treatment was court-ordered, and history of being arrested 30 days before entering treatment), treatment modality (outpatient or residential), and living in a restricted environment most of the time in the past 30 days before admission and at follow-up (i.e., psychiatric hospital/unit, crisis/respite program, jail, prison, other correctional facility, detoxification facility, and residential substance abuse treatment program).
Outcome Measures
Alcohol and drug addiction severity was measured using the Addiction Severity Index composite scores for alcohol and drug use.38 These scores range from 0 (no symptoms) to 1.0 (highest severity). For the present sample, the Cronbach’s α for the Addiction Severity Index Alcohol and Addiction Severity Index Drug subscales were 0.86 and 0.70, respectively. Mental health symptomatology was measured using the Brief Symptom Inventory (BSI).39 The BSI asks participants to rate how much they have been bothered by each of 53 symptoms in the past 7 days from 0 (not at all) to 4 (extremely). The Global Severity Index, a sum of the 53 items, was used. Higher scores in the Global Severity Index indicate more severe mental health symptoms. For the present sample, Cronbach’s α for the Global Severity Index was 0.97. Posttraumatic symptom severity was assessed using the Posttraumatic Symptom Scale.40,41 The Posttraumatic Symptom Scale is comprised of 17 items for which respondents rate how often each of the symptoms have bothered them in a scale from 0 (not at all or only one time) to 3 (almost always or more than five times a week). For the present sample, Cronbach’s α for the Posttraumatic Symptom Scale was 0.90.
Intervention and Comparison Conditions
Intervention Group
Programs in the intervention group were required to provide an integrated, comprehensive range of services with a particular emphasis on mental health, substance abuse, and trauma services, as well as to involve consumers in their efforts.36 The intervention group was comprised of clients receiving services in one of five substance abuse treatment programs in Boston’s poorest inner city communities. These included three residential programs, one outpatient program, and one methadone program. The intervention was known in the community as the BCSFR, a partnership of substance abuse, mental health, and other social service agencies and stakeholders that shaped the model of trauma-informed services. The BCSFR trauma-informed model37 had the following components: (1) trauma and mental health diagnostic assessment, treatment planning, and case management; (2) a 25-session modified version of the Trauma Recovery and Empowerment Model42 group; and (3) four manualized trauma-informed skills-building groups developed by the BCSFR37 that focused on leadership, economics, family reunification, and parenting skills. For a detailed description of the BCSFR trauma-informed model, see Amaro et al.37 Degree of exposure to intervention groups was as follows: The average number of Trauma Recovery and Empowerment Model sessions that participants attended was 10 with an overall 44% completion rate (completed ≥12 sessions out of 25 sessions).
Comparison Group
Programs in the comparison condition provided usual care. They were selected to represent similar programs, with similar length of treatment, serving similar populations in nearby geographical areas. Women in the comparison group were recruited from four treatment programs located in the Boston and Springfield, Massachusetts, USA, metropolitan areas in the following modalities: one outpatient, one methadone, and two residential programs. Unlike the intervention sites, they did not receive any additional support from SAMHSA under the grant to provide more comprehensive and integrated services that were trauma-informed and involved consumers. Rather their programs and services reflected what was available in communities under usual conditions. Services in the comparison group included the usual treatment services and intensity: for outpatients, one group or individual session per week; for methadone patients, daily dosing and weekly individual or group sessions; and for residential patients, typically weekly individual sessions and daily group sessions related to substance abuse treatment and relapse prevention.
Statistical Analysis
For each of the four outcome variables (i.e., alcohol use severity, drug use severity, mental health symptomatology, and PTSD symptoms), two mixed models for repeated measures were conducted. The first set of mixed models tested for differences in trajectories over time by intervention condition for each of the four dependent variables. For each of these models, the focus was on the condition × time interaction. The second set of mixed models tested whether racial/ethnic group moderated the effects of the intervention on each of the outcomes. Thus, for these models, the focus was on the condition × time × ethnicity interaction.
RESULTS
Comparability of Conditions
Pearson chi-square tests (for categorical data) and analysis of variance (for continuous data) indicated that there were significant differences in several of the demographic characteristics at baseline between the intervention and control group. As can be seen from Table 1, significant differences between intervention and control were observed for age, race/ethnicity, court-ordered participation in substance abuse or mental health services, arrested in past 30 days before admission, treatment modality, and percentage of women living in a restricted environment in the 30 days before the baseline interview. These variables were controlled for in the mixed models for repeated measures. In addition, Table 2 indicates that there was a significant difference between intervention and control in drug use severity at baseline. At baseline, women in the control group indicated higher drug use severity than women in the intervention. Thus, drug use severity was also controlled for in the mixed models for repeated measures.
TABLE 1.
Baseline characteristics of women in the intervention and services as usual comparison group who completed the 6-month follow-up (N = 342)
| Characteristics | Intervention (N = 181) | Comparison (N = 161) | p values |
|---|---|---|---|
| Age (years), mean (SD) | 35.9 (7.5) | 39.0 (8.3) | 0.0003 |
| Race/Ethnicity, frequency (%) | |||
| Hispanic | 57 (31.5) | 61 (37.9) | <0.0001 |
| Non-Hispanic black | 68 (37.6) | 22 (13.7) | |
| Non-Hispanic white | 48 (26.5) | 70 (43.5) | |
| Other non-Hispanic | 8 (4.4) | 8 (5.0) | |
| Education, frequency (%) | |||
| High school or above | 78 (43.1) | 78 (48.5) | 0.3211 |
| Less than high school | 103 (56.9) | 83 (51.5) | |
| Employment status upon admission, frequency (%) | |||
| Employed | 11 (6.1) | 16 (9.9) | 0.1863 |
| Unemployed | 170 (93.9) | 145 (90.1) | |
| Court-ordered to participate in substance abuse or mental health services, frequency (%) | |||
| Yes | 60 (33.3) | 35 (21.7) | 0.0171 |
| No | 120 (66.7) | 126 (78.3) | |
| Arrested in past 30 days before admission, frequency (%) | |||
| Yes | 8 (4.4) | 1 (0.6) | 0.0285 |
| No | 173 (95.6) | 160 (99.4) | |
| Modality, frequency (%) | |||
| Residential programs | 51 (28.2) | 71 (44.1) | 0.0010 |
| Outpatient programs | 71 (39.2) | 36 (22.4) | |
| Methadone treatments | 59 (32.6) | 54 (33.5) | |
| Living in controlled environment in past 30 days, frequency (%) | 53 (29.3) | 61 (37.9) | 0.0919 |
| Follow-up rate, % (no. of subjects) | |||
| 6 months | 77 (140) | 75 (120) | Ns |
| 12 months | 77 (140) | 78 (125) | Ns |
| Both 6 and 12 months | 69 (124) | 68 (109) | Ns |
TABLE 2.
Drug use severity at baseline between intervention and control groups (N=342)
| Outcome variables at baseline | Adjusted meansa (SE) | Adjusted means (SE) | Differences of adjusted meansb (SE) |
|---|---|---|---|
| Addiction severity | |||
| Addiction Severity Index: Alcohol (Higher score = more severity in alcohol addiction) | 0.09 (0.02) | 0.09 (0.02) | 0.00 (0.02) |
| Abstinence in past 30 days (%) | 63 | 68 | Ns |
| Addiction Severity Index: Drug use (Higher score = more severity in drug addiction) | 0.12 (0.01) | 0.15 (0.01) | 0.03 (0.01)* |
| Abstinence in past 30 days (%) | 41 | 32 | Ns |
| Mental health symptoms | |||
| Global Severity Index (Higher score = high severity of overall mental health problems) | 1.52 (0.08) | 1.47 (0.09) | −0.05 (0.09) |
| Posttraumatic Symptom Scale (Higher score = more PTSD symptoms) | 25.31 (1.22) | 23.88 (1.47) | −1.43 (1.46) |
SE Standard error
aAdjusted means are least-squares means at baseline controlling for age, racial/ethnic groups, court-ordered participation of substance abuse or mental health services, modality, and living in restricted environment most of the time in past 30 days. The mixed model was used for this analysis
bComparison group vs intervention group
*p < 0.05
Description of Services Received and Drop Out by Condition
No participants in the comparison condition received the trauma-informed groups offered in the intervention condition. Comparison group participants also did not receive any form of an integrated, comprehensive range of services with a particular emphasis on mental health, substance abuse, and trauma services.
Among 181 participants in the intervention condition, 120 (66%) participated in one or more of the trauma-informed groups offered as part of the intervention condition. Of these, 84 (70%) completed one or more of the intervention groups (defined as half or more of each of the sessions). With regard to the Trauma Recovery and Empowerment Model intervention, 102 (56%) participated and 41 subjects (40%) attended 12 sessions or more, which we consider to be a clinically significant dose of the treatment. There was a significant positive association between baseline drug addiction severity and the number of sessions in which intervention group subjects participated (Pearson correlation coefficients = 0.28, p = 0.004). No significant association was found between the intervention participation and baseline alcohol addiction, trauma, and mental health severity.
As expected, length of stay in substance abuse treatment varied by type of program: residential treatment (mean = 175.7 days, SD = 102.2 for comparison group; and mean = 188.4 days, SD = 123.5 for intervention group; p = 0.56); outpatient (mean = 315.4 days, SD = 77.4 for comparison group; and mean = 244.1 days, SD = 98.8 for intervention group; p = 0.06); and methadone (mean = 365.0 days, SD = 0 for comparison group; and mean = 331.0 days, SD = 60.7 for intervention group; p = 0.06).
Satisfaction and Experience with Treatment Programs
In general, at 6 months follow-up participants in the intervention group reported more satisfaction with services provided. Of those in the intervention group, 86% agreed or strongly agreed that “I was able to get all of the services I thought I needed” compared to 76% of women in the comparison group (p = 0.06). In addition, 95% of those in the intervention group agreed or strongly agreed that “Treatment was provided in a way that respected my values and beliefs” compared to 88% of those in the comparison group (p = 0.03). Furthermore, 90% of subjects in the intervention group agreed or strongly agreed that “The services I receive treat me as a whole person rather than pulling me apart into separate problems” in contrast to 81% in the comparison group (p = 0.07).
AIM 1: Compared to Services as Usual, Does Integrated Trauma and Substance Abuse Treatment Result in Better Outcomes as Measured by Alcohol and Drug Use Severity, Mental Health Symptomatology, and PTSD Symptoms?
Alcohol Addiction Severity
The analysis for alcohol addiction severity revealed a nonsignificant condition × time interaction [F(2, 559) = 0.33, p = 0.72 (d1 = 0.09)], indicating that the trajectories of alcohol addiction severity did not differ between the intervention and control groups. However, the main effect of time was significant [F(2, 569) = 12.25, p < 0.0001], indicating that both the intervention and control groups had a significant reduction in alcohol addiction severity over time. A post hoc analysis was conducted to compare the abstinence rate in past 30 days between the two groups. Results indicated that the intervention group did not report significantly higher abstinence rates than the comparison group at neither the 6- or 12-month follow-up.
Drug Addiction Severity
The analysis for drug addiction severity revealed a nonsignificant condition × time interaction [F(2, 555) = 0.37, p = 0.69 (d = 0.32)], indicating that the trajectories of drug addiction severity did not differ between the intervention and control groups. Moreover, the main effect of time was significant [F(2, 565) = 29.27, p < 0.001], indicating that both the intervention and control groups had a significant reduction in drug use severity over time. A post hoc chi-square test was conducted to compare the abstinence rate in past 30 days between the two groups. Results indicated that the intervention group reported significantly higher drug abstinence rates than the comparison group at both 6- and 12-month follow-ups (6-month 67 vs 38%; 12-month 75 vs 40%; all p values <0.0001).
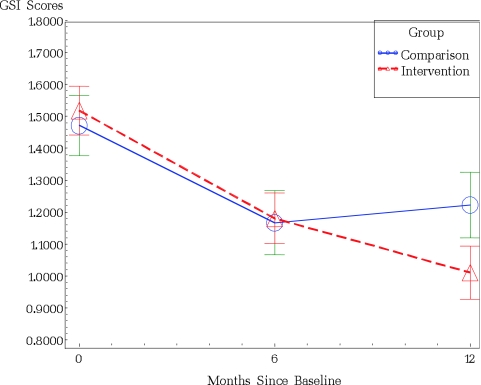
Mental Health Symptomatology
The analysis for mental health symptomatology revealed a significant condition × time interaction [F(2, 556) = 4.55, p = 0.01 (d = 0.32)], indicating that the trajectories of mental health symptomatology differed between the intervention and control groups. Examination of the error bars in Figure 1 demonstrates that at the 6- and 12-month assessments, the estimated mean for mental health symptomatology was lower in the intervention condition than in the control condition.
FIGURE 1.
Time path of global severity index scores by group.
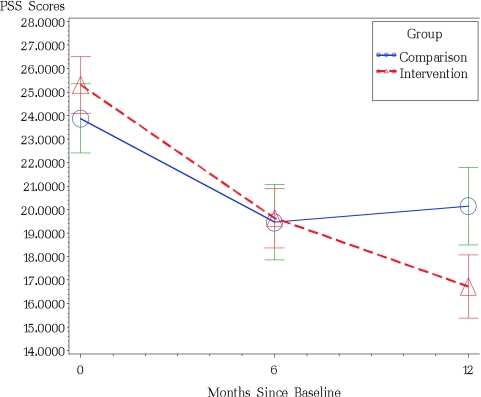
PTSD Symptoms
The analysis for PTSD symptoms revealed a significant condition × time interaction [F(2, 553) = 4.49, p = 0.01 (d = 0.35)], indicating that the trajectories of PTSD symptoms differed between the intervention and control groups. Examination of the error bars in Figure 2 demonstrates that at the 6- and 12-month assessments, the estimated mean for PTSD symptoms was lower in the intervention condition than in the control condition
FIGURE 2.
Time path of perceived stress scale scores by group.
AIM 2: Is the Integrated Care Model Equally Efficacious for Women of Various Racial/ethnic Groups?
The analyses to determine if racial/ethnic group moderated the effects of intervention on each of the four outcomes indicated that there was no significant condition × time × ethnicity interaction for alcohol addiction severity, drug use severity, mental health symptomatology, or PTSD symptoms, all p values >0.05, thus indicating that the integrated model was equally efficacious for women across all ethnic groups. However, because of the relatively small sample of women in each of the ethnic groups, especially for the other non-Hispanic racial group, effect sizes were computed for each outcome at both 6 and 12 months. As can be seen from Table 3 the effect size for alcohol use severity among the other non-Hispanic women group was large at 12 months postbaseline (d = 0.53), but small for women of all other ethnic races.43 On the contrary, the effect size for drug use severity among non-Hispanic white women was large at 12 months postbaseline but small or small to moderate at 12 months postbaseline for women of other ethnic groups. Thus, it appears that the effects of the intervention on drug use severity were strongest for non-Hispanic white and weakest for other non-Hispanic group. For mental health symptomatology, the effects of the intervention at 12 months postbaseline were strongest for non-Hispanic white and other non-Hispanic group. Finally, for PTSD symptoms, the effect sizes were small to moderate for black, Hispanic, and non-Hispanic white groups and largest for other non-Hispanic group.
TABLE 3.
Effect sizes by ethnic group for treatment outcomes
| Outcome | Ethnic group comparisons | Effect size for 6-month follow up | Effect size for 12-month follow up |
|---|---|---|---|
| Alcohol severity | Black | 0.18 | 0.19 |
| Hispanic | 0.11 | 0.11 | |
| Other non-Hispanic | 0.01 | 0.53 | |
| Non-Hispanic White | 0.01 | 0.14 | |
| Drug use severity | Black | 0.17 | 0.18 |
| Hispanic | 0.29 | 0.20 | |
| Other non-Hispanic | 0.47 | 0.05 | |
| Non-Hispanic White | 0.31 | 0.51 | |
| Mental health | Black | 0.28 | 0.18 |
| Symptomatology | Hispanic | 0.09 | 0.13 |
| Other non-Hispanic | 0.61 | 0.54 | |
| Non-Hispanic White | 0.01 | 0.45 | |
| PTSD symptoms | Black | 0.20 | 0.21 |
| Hispanic | 0.08 | 0.25 | |
| Other non-Hispanic | 0.24 | 0.85 | |
| Non-Hispanic White | 0.30 | 0.28 |
DISCUSSION
The present study considered the effects of integrated trauma-informed services on the severity of alcohol and drug use, mental health, and PTSD symptomatology among women with histories of trauma receiving substance abuse treatment in urban settings. The study also examined the outcomes by race/ethnicity to test if the model of integrated services was equally beneficial for women of different racial/ethnic groups.
Comparison Between the Treatment Conditions
Statistically significant differences in improvements in drug abstinence rates and mental health, and PTSD symptoms were found between the intervention and comparison groups. In contrast to the comparison group, the intervention group showed significantly greater improvement in drug use at both 6- and 12-month follow-ups. This finding suggests that the integrated services may lead to a favorable outcome in drug use in the short-term and that the improvement can be maintained over time. In addition, greater significant changes in improvements of severity of mental health problems were found at 12 months among women in the intervention group than among women in the comparison group. Furthermore, the intervention group showed significant change in improvement of PTSD symptomatology at 12 months compared to the comparison group. These findings suggest the long-term positive effect of the integrated services on both mental health and PTSD symptoms. These results are consistent with previous studies44–49 that have documented the importance of addressing trauma and substance abuse in an integrated manner to obtain significant positive outcomes among women with cooccurring disorders. The results also reflect strong associations among severity of substance use, mental health problems, and PTSD symptoms. It may be of importance for future studies to investigate pathways among those variables to identify underlying mechanisms.
Our results indicating a lack of an intervention effect on alcohol use severity are similar to those of previous studies examining the impact of trauma-informed services.44–46
Intervention Effect in Each Racial/Ethnic Group and Across Groups
In addition to the effectiveness of the trauma-informed integrated services, we evaluated the outcomes of black, Hispanic, and white women in the intervention and comparison groups to examine whether integrated services are equally beneficial for women from different racial/ethnic groups. Our results from the mixed models showed that the intervention effects in reducing drug addiction severity, mental health symptoms, and PTSD symptomatology were not different for women in each racial/ethnic group.
Our conclusions, however, must be carefully tempered by the limitations of the study. Because of the small number of participants in each ethnic group, the present study had limited statistical power to detect significant differences by racial/ethnic group. In fact, based on the effect sizes, the effects of the intervention on each of the outcomes appear to be stronger for some ethnic groups than for others. In addition, the overall findings on the effectiveness of the integrated model of treatment need to be viewed in the context of the lack of randomization and baseline differences in the treatment conditions. Although these differences were controlled for in statistical analyses, there may have been other unmeasured baseline differences that could have affected the results. The lack of a biological measure of drug use is another limitation that may have resulted in underidentification of drug use. In addition, the present study was not designed to tease out the effect of single components of the intervention package provided for women in both treatment conditions. Finally, the study lacked an end of treatment measure. Whereas most of the treatment interventions were conducted within the first 6 months, some of the intervention participants were still receiving services at that time.
The present study demonstrated the effectiveness of trauma-informed integrated services for women in urban communities with histories of trauma in substance abuse treatment settings. Our results suggested that integrating trauma-related services in substance abuse treatment settings may be a critical factor leading to better outcomes not only in abstinence from drug use, but also in mental health and PTSD symptomatology. Our results also indicated that the trauma-informed integrated services model was overall beneficial for all three groups of women. Future replications of these findings will contribute to building firm evidence on the effectiveness of integrated trauma-informed substance abuse services for women with cooccurring disorders living in urban settings.
Acknowledgements
This study (Hortensia Amaro, Principal Investigator) was funded under Guidance for Applicants no. TI 00-003 entitled Cooperative Agreement to Study Women with Alcohol, Drug Abuse and Mental Health (ADM) Disorders Who Have Histories of Violence: Phase II (grant no. 1 UD1 TI-11397) from the Department of Health and Human Services, Public Health Service, SAMHSA’s three centers: Center for Substance Abuse Treatment, Center for Mental Health Services, and Center for Substance Abuse Prevention (U.S. Health and Human Services, March 2000). The assistance of project staff and clients at the participating sites is gratefully acknowledged.
Footnotes
Effect sizes reported are for the 12-month postbaseline assessment (unless otherwise noted).
References
- 1.Kessler R. Posttraumatic stress disorder: the burden to the individual and to society. J Clin Psychiatry. 2000;61(Suppl 5):4–12. [PubMed]
- 2.Najavits LM, Weiss RD, Shaw SR. The link between substance abuse and posttraumatic stress disorder in women: a research review. Am J Addict. 1997;6:273–283. [PubMed]
- 3.Brown JR, Hill HM, Lambert SF. Traumatic stress symptoms in women exposed to community and partner violence. J Interpers Violence. 2005;20:1478–1494. [DOI] [PubMed]
- 4.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–1060. [DOI] [PubMed]
- 5.Hidalgo RB, Davidson JR. Posttraumatic stress disorder: epidemiology and health-related considerations. J Clin Psychiatry. 2000;61:5–13. [PubMed]
- 6.Davidson JR. Trauma: the impact of post-traumatic stress disorder. J Psychopharmacol. 2000;14:S5–S12. [DOI] [PubMed]
- 7.Stevens SJ, Murphy BS, McKnight K. Traumatic stress and gender differences in relationship to substance abuse, mental health, physical health, and HIV risk behavior in a sample of adolescents enrolled in drug treatment. Child Maltreat. 2003;8:46–57. [DOI] [PubMed]
- 8.Claus RE, Kindleberger LR. Engaging substance abusers after centralized assessment: predictors of treatment entry and dropout. J Psychoactive Drugs. 2002;34:25–31. [DOI] [PubMed]
- 9.Amaro H, Nieves R, Johannes SW, Cabeza NML. Substance abuse treatment: critical issues and challenges in the treatment of Latina women. Hisp J Behav Sci. 1999;21:266–282. [DOI]
- 10.Thompson MP, Kingree JB. The frequency and impact of violent trauma among pregnant substance abusers. Addict Behav. 1998;23:257–262. [DOI] [PubMed]
- 11.Barrowclough C, Haddock G, Tarrier N, et al. Randomized controlled trial of motivational interviewing, cognitive behavior therapy, and family intervention for patients with comorbid schizophrenia and substance use disorders. Am J Psych. 2001;158:1706–1713. [DOI] [PubMed]
- 12.Ouimette PC, Brown PJ, Najavits LM. Course and treatment of patients with both substance use and posttraumatic stress disorders. Addic Behav. 1998;23:785–795. [DOI] [PubMed]
- 13.Brown PJ, Stout RL, Gannon-Rowley J. Substance use disorders-PTSD comorbidity: patient’s perceptions of symptom interplay and treatment issues. J Subst Abuse Treat. 1998;15:445–448. [DOI] [PubMed]
- 14.Ouimette P, Brown PJ. Trauma and Substance Abuse: Causes, Consequences, and Treatment of Comorbid Disorders. Washington, D.C.: American Psychological Association; 2002.
- 15.Najavits LM, Sullivan TP, Schmitz M, Weiss RD, Catherine SN, Lee BA. Treatment utilization by women with PTSD and substance dependence. Am J Addict. 2004;13:215–224. [DOI] [PubMed]
- 16.Hellerstein DJ, Rosenthal RN, Miner CR. Integrating services for schizophrenia and substance abuse. Psychiatr Q. 2001;72:291–306. [DOI] [PubMed]
- 17.Najavits L, Weiss R, Shaw S, Muenz L. “Seeking safety”: outcome of a new cognitive-behavioral psychotherapy for women with post-traumatic stress disorder and substance dependence. J Trauma Stress. 1998;22:437–456. [DOI] [PubMed]
- 18.Rach Beisel J, Scott J, Dixon L. Co-occurring severe mental illness and substance use disorders: a review of recent research. Psychiatr Serv. 1999;50:1427–1434. [DOI] [PubMed]
- 19.McCaul ME, Svikis DS, Moore RD. Predictors of outpatient treatment retention: patient versus substance use characteristics. Drug Alcohol Depend. 2001;62:9–17. [DOI] [PubMed]
- 20.Ziedonis DM, Stern R. Dual recovery therapy for schizophrenia and substance abuse. Psychiatr Ann. 2001;31:255–264.
- 21.Drake RE, Yovetich NA, Rebout RR, Harris M, McHugo GJ. Integrated treatment for dually diagnosed homeless adults. J Nerv Ment Dis. 1997;185:298–304. [DOI] [PubMed]
- 22.Amaro H, Larson MJ, Gampel J, Richardson E, Savage A, Wagler D. Racial/ethnic differences in social vulnerability among women with co-occurring mental health and substance abuse disorders: implications for treatment services. J Community Psychol. 2005;33:495–511. [DOI]
- 23.Hser YI, Anglin MD, Chou C. Evaluation of drug abuse treatment. Repeated measures design assessing methadone maintenance. Eval Rev. 1998;12:547–570. [DOI]
- 24.Hohman MM, Galt DH. Latinas in treatment: comparisons of residents in a culturally specific recovery home with residents in non-specific recovery homes. J Ethn Cult Divers Soc Work. 2001;9(3/4):93–109. [DOI]
- 25.Mora J. Latinas in cultural transition: addiction, treatment and recovery. In: SLA Straussner, S Brown, eds, The Handbook of Addiction Treatment for Women: Theory and Practice. San Francisco, CA: Jossey Bass; 2002:323–347.
- 26.Ashley OS, Marsden ME, Brady TM. Effectiveness of substance abuse treatment programming for women: a review. Am J Drug Alcohol Abuse. 2003;29:19–53. [DOI] [PubMed]
- 27.Herman JL. Trauma and Recovery. New York: Basic Books; 1992.
- 28.van der Kolk BA, Pelcovitz D, Roth S, Mandel FS, McFarlane A, Herman JL. Dissociation, somatization, and affect dysregulation: the complexity of adaptation to trauma. Am J Psychiatry. 1996;153(Suppl 7):83–93. [DOI] [PubMed]
- 29.van der Kolk BA, Hostetler A, Herron N, Fisler RE. Trauma and the development of borderline personality disorder. Psychiatr Clin North Am. 1994;17:715–730. [PubMed]
- 30.Briere JN. Child Abuse Trauma: Theory and Treatment of the Lasting Effects. Newbury Park, CA: Sage Publications; 1992.
- 31.Malinowsky-Rummell R, Hansen DJ. Long-term consequences of childhood physical abuse. Psychol Bull. 1993;114:68–79. [DOI] [PubMed]
- 32.Levitan RD, Parkh SV, Lesage AD, et al. Major depression in individuals with a history of childhood physical or sexual abuse: relationship to vegetative features, mania, and gender. Am J Psychiatry. 1998;155:1746–1752. [DOI] [PubMed]
- 33.Shalev AY. Discussion: treatment of prolonged posttraumatic stress disorder—learning from experience. J Trauma Stress. 1997;10:415–423. [DOI] [PubMed]
- 34.Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. J Consult Clin Psychol. 1992;60:748–756. [DOI] [PubMed]
- 35.Fallot R, Harris M. Trauma Recovery and Empowerment Model (TREM): conceptual and practical issues in a group intervention for women. Community Ment Health J. 2002;38:475–485. [DOI] [PubMed]
- 36.McHugo GJ, Kammerer N, Jackson EW, et al. Women, Co-occurring Disorders, and Violence Study: evaluation design and study population. J Subst Abuse Treat. 2005;28:91–107. [DOI] [PubMed]
- 37.Amaro H, McGraw S, Larson MJ, Lopez L, Nieves R, Marshall B. Boston Consortium of Services for Families in Recovery: a trauma-informed intervention model for women’s alcohol and drug addiction treatment. Alcohol Treat Q. 2004;22:95–119. [DOI]
- 38.McLellan AT, Kushner H, Metzger D, et al. The fifth edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9:199–213. [DOI] [PubMed]
- 39.Derogatis LR. BSI: Brief Symptom Inventory (BSI): Administration, Scoring and Procedures Manual (4th edn.). Minneapolis: National Computer Systems, Inc; 1993.
- 40.Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: the Posttraumatic Diagnostic Scale. Psychol Assess. 1997;9:445–451. [DOI]
- 41.Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing post-traumatic stress disorder. J Trauma Stress. 1993; 6:459–473.
- 42.Harris M. Trauma Recovery and Empowerment: a Clinician’s Guide for Working with Women in Groups. New York: The Free Press; 1998.
- 43.Cohen J. Statistical Power Analysis for the Behavioral Sciences (2nd edn.). Hillsdale, NJ: Lawrence Earlbaum Associates; 1988.
- 44.Morrissey JP, Ellis AR, Gatz M, et al. Outcomes for women with co-occurring disorders and trauma: program and person-level effects. J Subst Abuse Treat. 2005a; 28:121–133. [DOI] [PubMed]
- 45.Morrissey JP, Jackson EW, Ellis AR, Amaro H, Brown VB, Najavits LM. 12-month outcomes of trauma-informed interventions for women with co-occurring disorders. Psychiatr Serv. 2005b;56:1213–1222. [DOI] [PubMed]
- 46.Cocozza J, Jackson E, Hennigan K, et al. Outcomes for women with co-occurring disorders and trauma: program-level effects. J Subst Abuse Treat. 2005;28:109–119. [DOI] [PubMed]
- 47.Dumain M. Meta-analysis of interventions with co-occurring disorders of severe mental illness and substance abuse: implications for social work practice. Res Soc Work Pract. 2003;13:142–165. [DOI]
- 48.Messman-Moore TL, Long PJ. Alcohol and substance use disorders as predictors of child to adult sexual revictimization in a sample of community women. Violence Vict. 2002;17:319–340. [DOI] [PubMed]
- 49.Ouimette PC, Moos RH, Finney JW. Two-year mental health service use and course of remission in patients with substance use and posttraumatic stress disorders. Addict Behav. 2000;23:785–795. [DOI] [PubMed]