Abstract
Since many years we routinely use diagnostic selective nerve root blocks (SNRB) at our department when evaluating patients with cervical radiculopathy. Frequently patients who also presented with headache reported that the headache disappeared when the nerve root responsible for the radicular pain was blocked with local anaesthetics. Headache has been described as a companioning symptom related to cervical radiculopathy but has never before been evaluated with SNRB performed in the lower cervical spine. For this reason we added to our routine an evaluation of the response from the SNRB on headache in patients with cervical radiculopathy. The aim was to describe the frequency of headache in patients with cervical radiculopathy and its response to a selective nerve root block of the nerve root/roots responsible for the radiculopathy. Can nerve root compression in the lower cervical spine produce headache? In this consecutive series of 275 patients with cervical radiculopathy, 161 patients reported that they also suffered from daily or recurrent headache located most often unilaterally on the same side as the radiculopathy. All patients underwent a careful clinical examination by a neurosurgeon and a MRI of the cervical spine. The significantly compressed root/roots, according to the MRI, underwent SNRB with a local anaesthetic. The effect of the nerve root block on the radiculopathy and the headache was carefully noted and evaluated by a physiotherapist using visual analogue scales (VAS) before and after the SNRB. All patients with headache had tender points in the neck/shoulder region on the affected side. Patients with headache graded significantly more limitations in daily activities and higher pain intensity in the neck/shoulder/arm than patients without headache. After selective nerve root block, 59% of the patients with headache reported 50% or more reduction of headache and of these 69% reported total relief. A significant correlation was seen between reduced headache intensity and reduced pain in the neck, shoulder and arm. The result indicates that cervical root compression from degenerative disease in the lower cervical spine producing radiculopathy might also induce headache.
Keywords: Cervical spine, Cervicogenic headache, Cervical radiculopathy, Selective nerve root block, International Headache Society classification
Introduction
The most common cause of cervical radiculopathy is degenerative disease in the cervical spine [11]. In 80–90% of patients with cervical radiculopathy, the C5/C6 or C6/C7 motion segments are affected by degenerative disease and the nearby C6 and/or C7 nerve roots are producing the symptoms [14]. Patients with cervical radiculopathy complain of neck pain and radiating pain in the arm sometimes combined with sensory and motor disturbances in the arm and/or hand. These symptoms are accepted as being caused by the nerve root compression [25]. Headache, if asked for, is frequently reported by patients with cervical radiculopathy but in general not discussed in terms of nerve root compression in the lower cervical spine. On the other hand, affection of nerve structures in the upper cervical spine, including the C2 and C3 nerve roots and the occipital major nerve, are accepted as a cause of occipital headache [8]. The term cervicogenic headache [34], is often mentioned in the literature. It is not related to nerve root compression, but described as being caused by musculoskeletal structures in the upper cervical spine and the pathogenic mechanism is unclear [4, 10].
The criteria for cervicogenic headache are recurrent and strictly unilateral headache without side shift. It starts in the neck and spreads to the fronto-ocular area and is elicited by certain movements or awkward position of the head. Clinical investigation reveals reduced mobility of the neck and external pressure tenderness is present [33]. Our own experience from many years of clinical research of patients with cervical radiculopathy is that headache often is present [3, 30] and that the headache sometimes is more disabling for the patient than the radicular pain in the shoulder/arm. We have also noticed that headache reduction might be achieved after conservative treatment of the neck pain or after surgery in patients with degenerative cervical radiculopathy [30]. We use selective diagnostic nerve root blocks when investigating patients with degenerative cervical radiculopathy and our experience is that both headache and radicular pain in the arm might be significantly reduced when the symptomatic nerve root is blocked with local anaesthetics [3]. This knowledge stimulated us to further investigate if nerve root compression in the lower cervical spine could cause headache.
Materials and methods
Patients
The present prospective study includes 275 consecutive patients, 125 women and 150 men, presenting with cervico-brachialgia for more than 3 months. All patients were referred to the Department of Neurosurgery for evaluation and, if necessary, surgical intervention. Mean age was 50.7 (SD 9.7) years, and mean symptom duration was 26 months (±22, 3–120) months (Table 1). Inclusion criteria were cervico-brachialgia with corresponding significant degenerative MRI pathology, on the same side as the brachialgia. To be classified as significant, the degenerative MRI pathology must have a close relation to the nerve roots. History and clinical findings have to indicate a cervical nerve root origin with pain radiating from the neck to the arm. Patients with spinal cord compression and/or myelopathy were excluded. Forty-nine patients had had previous surgery for similar symptoms and were now readmitted because of new symptoms.
Table 1.
Selected demographic and social data in all patients (n = 275) and patients who graded headache (n = 161) and without headache (n = 114) at the time before the nerve block
| All patients (n = 275) | With headache (n = 161) | Without headache (n = 114) | |
|---|---|---|---|
| Sex | |||
| Women | 125 (45%) | 72 (45%) | 53 (46%) |
| Men | 150 (55%) | 89 (55%) | 61 (54%) |
| Age, years | |||
| Mean (median) | 51 (51) | 50 (50) | 51 (52) |
| SD, range | ±9.7 (27–78) | ±9.7 (27–78) | ±9.7 (29–75) |
| Duration, months | |||
| Mean (median) | 26 (20) | 31 (24) | 21 (16) |
| SD (range) | ±22 (3–120) | ±26 (3–120) | ±16 (3–120) |
| Affected nerve root | |||
| C IV | 8 (3%) | 6 (4%) | 2 (2%) |
| C V | 31 (11%) | 21 (13%) | 10 (9%) |
| C VI | 142 (52%) | 84 (52%) | 58 (51%) |
| C VII | 81 (29%) | 46 (29%) | 35 (31%) |
| C VIII | 13 (5%) | 4 (2%) | 9 (8%) |
| Affected side | |||
| Right | 156 (57%) | 91 (57%) | 65 (57%) |
| Left | 119 (43%) | 70 (43%) | 49 (43%) |
| Onset | |||
| Suddenly | 114 (31%) | 65 (40%) | 49 (43%) |
| Gradually | 161 (59%) | 96 (60%) | 65 (57%) |
| Pain frequency (number) | |||
| Never pain-free | 177 (64%) | 113 (70%) | 64 (56%) |
| Pain-free some hours | 86 (31%) | 45 (28%) | 41 (36%) |
| Pain-free some days | 11 (4%) | 3 (2%) | 9 (8%) |
| Pain intensity | |||
| At rest | 33 (30) ± 23 (0–95) | 37 (33) ± 23 (0–95) | 28 (25) ± 22 (0–90) |
| At work | 77 (80) ± 19 (20–100) | 81 (80 ± 15 (30–100) | 72 (75) ± 18 (20–100) |
| Sickness benefit | |||
| Full time | 167 (61%) | 101 (63%) | 66 (58%) |
| Part time | 48 (17%) | 29 (18%) | 19 (17%) |
Methods
All referred patients had undergone a MRI investigation of the cervical spine. They were examined by a neurosurgeon at the outpatient clinic and were diagnosed to have cervical radiculopathy based on degenerative disease in the cervical spine. To further confirm the nerve root compression as a cause of the patients’ symptoms, selective nerve root blocks (SNRB) with local anaesthetics were performed on the nerve roots presenting with degenerative MRI pathology on the same side as the brachialgia. If two nerve roots showed significant MRI pathology on the same side as the brachialgia, both nerve roots underwent SNRB. The effect from the temporary nerve root block was assessed with a visual analogue scale (VAS) [12, 31] and compared with the pre-block assessment concerning pain in the neck, shoulder, arm and the headache.
The patients underwent a clinical examination by the same physiotherapist immediately before and 30 min after the nerve root block, according to a fixed protocol. The following variables were studied: Pain history, pain distribution, pain intensity in the neck, shoulder and arm, the occurrence of headache, muscle tenderness in the neck, paraesthesia and sensory loss. The occurrence of other symptoms such as sleep disturbances, neck stiffness,unsteadiness and hand weakness were noted. Neck disability index (NDI), a self-administrated questionnaire that had proved to be a reliable, valid and sensitive instrument, was used to measure neck related disability including pain intensity, personal care, lifting, reading, headaches, concentration, work, driving, sleep and recreation. [1, 17, 38]. The ten items are scored 0 (no activity limitation) to 5 (major activity limitations) and summed to a percentage score.
Muscle tenderness evaluation
Four selected muscles were palpated for grading muscle tenderness. They were located on each side of the head according to Travell’s and Simons trigger-point manual [37]. The muscles were chosen because they corresponded to the location of the neck pain and the headache [37]. The muscles chosen were M trapezius upper portion at the suboccipital attachment, M trapezius medial portion at the C7 level 10 cm from the lateral spinal process and M levator scapulae at the insertion at the superior angle of the scapulae. The degree of tenderness was assessed according to Langemark and Olesen on a four-point scale from no pain to severe pain with “jump up sign” [23]. The patients were sitting relaxed in front of a mirror. If the patients reported painful or severe tenderness with visual reaction, the tender-point was marked on the pain figure.
Headache classification
A headache intensity of >15 on the VAS (i.e. 0–100) was estimated as current headache. If a patient described headache, a classification of the headache took place according to International Classification of Headache Disorders [18]. The patients were asked about the location of the headache on a pain-figure and whether the headache was precipitated or aggravated by factors such as special neck movements or a sustained neck position. The patients were also asked if the headache had appeared for the first time in relation to the neck–shoulder–arm pain or if it had been present before. The patients’experience of neck stiffness was noted.
Pain assessment
A pain drawing was used to describe the location and quality of pain and other sensations as well as the location of possible headache. Different symbols describing pain types, such as aches, burns, cuts and other sensations as numbness, tingling and cramps could be used [29]. The current pain intensity in the neck, shoulder, and arm and the headache were noted immediately before the nerve block using VAS. Neck provocation including active motions by the patients was added and manoeuvres causing pain were noted.
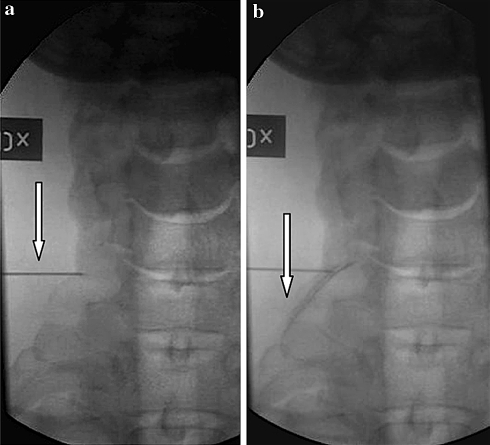
Nerve root block technique
The nerve root blocks were performed in an X-ray suite by a specially trained neuroradiologist. The technique used was basically similar to the lateral approach described by Kikuchi [22] but performed with the use of fluoroscopy [3]. A 0.7 mm needle, 40 or 75 mm long, was used. No local anaesthetics were given on the skin. The needle position was confirmed in all patients with the use of contrast media. Then 1/2 ml of Mepivacaine (Carbocain, Astra. Södertälje. Sweden) 10 mg/ml was injected for blocking the nerve (Fig. 1a, b). The effect from the nerve root block is estimated not to last more than 2 h.
Fig. 1.
a Shows needle in position, and b distribution of contrast enhanced injection of local anaesthetics along the nerve root
Evaluation of SNRB
No analgesics were allowed from 12 h before the block occasion until the examinations were finished. Immediately before and 30 min after the nerve root block, the patient underwent pain intensity assessment of the headache as well as the neck-, shoulder- and arm-pain by a specially trained physiotherapist. Pain increase by provocative active motion in the cervical spine was also noted on the VAS. If two nerve roots were blocked in the same patient, 4 h were allowed to elapse between the two blocks.
If the patient reported an arm-pain reduction with a corresponding VAS reduction of 50% or more, the root was classified as significant for mediating the radicular pain. If the patient reported a headache reduction, with a corresponding VAS reduction of 50% or more, the root was classified as significant for causing the headache.
Statistical methods
A non-parametric test was chosen. For comparison between patients with and without headache comparison with Mann–Whitney's U test was used. For comparison within groups before and after SNRB the Wilcoxon's matched-pairs signed-ranks test were used. Correlation between reduction of pain-intensity and reduction of headache-intensity was measured. A difference with P < 0.05 was considered statistically significant.
The study was approved by the ethics committee of the university Hospital of Lund, Sweden.
Results
Characteristics of the evaluated headache
Of the 275 patients with cervical radiculopathy, 161 reported headache. The MRI investigation of their cervical spines verified significant nerve root affection from degenerative disease at one or two levels in the lower cervical spine. Six patients had migraine in their history, but reported that that they could distinguish the evaluated headache from migraine. Immediately before the nerve root blocks 161 (59%) patients experienced headache exceeding a score of 15 on a VAS. The evaluated headache was predominantly unilateral at the same side as the radiculopathy (Table 1). The headache was aching, tightening and in most cases localised at the back of the head. Often the headache was radiating to the forehead. When investigating the patients with headache all had external pressure tenderness, most frequently in the M trapezius medial part and in the interscapular region, on the same side as the headache and the radiculopathy.
There was no difference in sex distribution or age when comparing patients with or without headache. However, symptom duration and pain frequency tended to be greater in patients with headache (Table 1). Patients with headache graded significantly higher pain intensity in the neck, shoulder and arm than the patients without headache (Table 2).
Table 2.
The pain intensity in the neck, shoulder, arm pain and headache, measured by Visual Analogue Scale, in patients with and without headache at the time before nerve root block (n = 275)
| Patients with headache (n = 161) | Patients without headache (n = 114) | P-value | |
|---|---|---|---|
| Neck | 61 (67) ± 24 (0–100) | 47 (50) ± 27 (0–100) | <0.000 |
| Shoulder | 58 (62) ± 26 (0–100) | 52 (53) ± 25 (0–100) | 0.042 |
| Arm | 55 (57) ± 28 (0–100) | 46 (50) ± 29 (0–100) | 0.009 |
| Headache | 54 (50) ± 26 (1–100) | ||
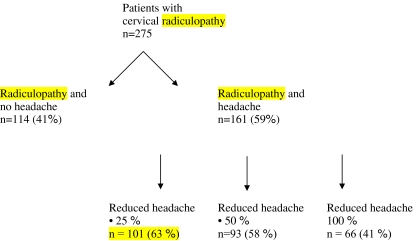
Results from nerve root blocks on headache
At the evaluation, 30 min after the SNRB, 101 of the 161 (63%) patients with headache experienced headache reduction on VAS, of 25% or more and 93 patients (58%) experienced a reduction of more than 50%. Of these 93 patients, 66 (70%) reported a total relief of headache during the nerve root block (Fig. 2).
Fig. 2.
This figure shows the reduction of headache 30 min after nerve block. The remaining 60 patients experienced no or less than 10% reduction of headache after the nerve root block
The pain in the neck, shoulder, arm and headache intensity after the SNRB are shown in Table 3. A significant correlation (P < 0.0001) was seen between headache reduction and the pain intensity in the neck, shoulder and arm after SNRB (Table 3). A significant correlation was also seen between the groups of patients with reduction of headache more than 25 and 50% and the groups of patients with reduced neck, shoulder and arm pain more than 25 and 50%. In patients with headache, a significantly higher limitation in daily activities was reported in comparison with patients without headache (Table 4).
Table 3.
The table shows the pain intensity according to VAS and the correlation confidence between the intensity of headache and neck-, shoulder-, arm-pain after the nerve block
| Headache 28 (29) ± 32 (0–100) | |
|---|---|
| Neck pain 33 (25) ± 29 (0–100) | 0.645*** |
| Shoulder pain 32 (32) ± 28 (0–100) | 0.530*** |
| Arm pain 29 (20) ± 27 ( 0–95) | 0.438*** |
Mean (median) SD and range are given
***P < 0.0001
Table 4.
Neck disability index (NDI) scores in patients with headache and without headache (n = 270)
| NDI score | Patients with headache | Patients without headache | P-value |
|---|---|---|---|
| Items (0–5) | n = 159 | n = 111 | |
| Mean (SD) | Median (min–max) mean (SD) | Median (min–max) | |
| Pain intensity | 3 (0–5) 2.7 ± 1.1 |
2 (0–5) 2.4 ± 1.04 |
0.0025 |
| Personal care | 1 (0–5) 1.4 ± 1.0 |
1 (0–3) 1.0 ± 0.8 |
0.0028 |
| Lifting | 3 (0–5) 2.7 ± 1.2 |
2 (0–4) 2.3 ± 1.2 |
0.0040 |
| Reading | 3 (0–5) 2.4 ± 1.2 |
2 (0–5) 1.8 ± 1.2 |
0.0001 |
| Headache | 3 (1–5) 3.4 ± 1.3 |
1 (0–5) 1.2 ± 1.3 |
0.0001 |
| Concentration | 2 (0–5) 1.7 ± 1.3 |
1 (0–4) 1.03 ± 1.1 |
0.0001 |
| Work | 4. (0–5) 3.6 ± 1.3 |
3 (0–5) 3.11 ± 1.5 |
0.0101 |
| Driving | 2 (0–5) 3.6 ± 1.3 |
2 (0–5) 1.8 ± 1.25 |
0.0110 |
| Sleep | 3 (0–5) 3.1 ± 1.5 |
2 (0–5) 2.36 ± 1.45 |
0.0001 |
| Recreation | 3 (0–5) 3.1 ± 1.5 |
2 (0–5) 2.5 ± 1.2 |
0.0001 |
| Total score | 26 (11–45) 26.6 ± 7.5 |
19 (3–34) 19 ± 6.9 |
0.0001 |
Discussion
This present study shows that daily or recurrent headache is common in patients with cervical radiculopathy. It was also found that patients with cervical radiculopathy and headache had higher NDI and higher pain intensity in the neck–shoulder–arm than patients without headache. Most important, 58% of the patients with cervical radiculopathy presented a significant (more than 50% reduction) or a total relief of headache after blocking the nerve root responsible for the patients’ radiculopathy. This is strong evidence that headache can be caused by nerve root compression in the lower cervical spine. Patients with cervical radiculopathy reported headache distributed most often unilaterally on the same side as the radiculopathy. We have previously reported that the headache is reduced or disappears after successful conservative or surgical intervention in the lower cervical spine [2, 30]. Other studies have reported the same findings [15, 27, 36] and will further support that nerve root compression in the lower cervical spine might induce headache. The similarity between the effect of the nerve root block on both headache and neck–arm pain suggests a common pathophysiology of these two symptoms.
The primary aim of the SNRB was to secure and select the nerve root which causes the raduculopathy. A careful neck/shoulder/arm pain and headache history was taken and a great weight was put on the pain assessment. Careful information how to fill in the VAS was given. From the classification of headache in patients with neck pain it can be difficult to distinguish between cervicogenic headache, tension type headache and migraine without aura [9, 20, 26]. The prevalence of earlier classified migraine in this population was low compared to the prevalence in the literature. But still it remains that the majority of patients had a temporal effect of the headache in connection with the diagnostic nerve root block in the cervical spine. In patients with cervical radiculopathy and headache, we found in an earlier study that almost all patients could be classified according to IHS and Sjaastad critera for cervicogen headache [30]. In the revised classification of cervigogenic headache in IHS, lesion within the upper cervical spine or soft tissues of the neck are valid causes of cervicogenic headache, while cervical spondolosis with or without nerve root compression in the lower cervical spine are not accepted as a valid cause [18]. When myofascial tender spots are present, the headache should be coded under tension type headache [18]. In the present study all patients with headache had tender points in neck/shoulder or interscapular muscles at the symptomatic side. The same experience was reported by Letchuman et al. in patients with cervical radiculopathy and in that study they found increased tender spots on the same side as the radiculopathy [24]. Jaeger found myofascial trigger and tender points on the symptomatic side in patients with cervicogenic headache [19].
At our department we have extensive experience of evaluating cervical radiculopaty with selective nerve root blocks. Especially in patients with multilevel degenerative disease on the MRI of the cervical spine, SNRB was proven to be useful when selecting nerve roots for treatment [2, 3].
The pathophysiology of the headache described in the present study is unclear. Headache might be induced with signals from nerve endings in spinal structures like the disc capsule, ligaments or neck muscles [5, 7, 10, 13, 16, 21, 32]. Thus, affection of nerve structures transforming pain signal of sclerotomal origin might be involved. Tender muscles in the neck, occiput and interscapulare are revealed by the clinical investigation. These muscles might furthermore produce headache.
The occurrence of headache in patients with radiculopathy is seldom described in the literature or used as an outcome variable. Maybe it is because many patients do not spontaneously complain of headache because the main symptom is the neck/shoulder/arm pain together with other symptoms such as neck stiffness, motor deficit and sensory disturbances. The headache seems to restrict the patients’ active daily living and more attention should be taken to help these patients with different varieties of physiotherapy [28, 35].
For this reason we recommend that headache classification and assessment together with muscle palpation should be a part of the neck examination in patients with cervical radiculopahty.
In the present study diagnostic short term effects on headache was evaluated. In future studies it will be important to evaluate long term effects on headache from treatment in patients with nerve root compression in the lower cervical spine. However, headache as the only symptom is not an indication for surgical treatment of degenerative disease in the cervical spine, it is the radicular symptom caused by the nerve root compression that is the indication for such treatment.
Conclusions
According to the results in the present study, nerve root compression from degenerative disease in the lower cervical spine producing radiculopathy might also induce headache. Patients with cervical radiculopathy and headache have greater limitations in daily activities and more severe radicular pain in comparison to patients with cervical radiculopathy without headache.
Acknowledgment
The study was supported by grants from the Region Skane, Medical Faculty, University in Lund, and the Department of Neurosurgery, University Hospital of Lund, Sweden.
References
- 1.Ackelman BH, Lindgren U. Validity and reliability of a modified version of the neck disability index. J Rehabil Med. 2002;34(6):284–287. doi: 10.1080/165019702760390383. [DOI] [PubMed] [Google Scholar]
- 2.Anderberg L, Annertz M, Brandt L, Säveland H. Selective diagnostic nerve root blocks: correlation with clinical symptoms and MRI-pathology. Acta Neurochir. 2004;146(6):559–565. doi: 10.1007/s00701-004-0241-4. [DOI] [PubMed] [Google Scholar]
- 3.Anderberg L, Annertz M, Rydholm U, Brandt L, Säveland H. Selective diagnostic nerve root block for the evaluation of radicular pain in the multilevel degenerated cervical spine. Eur Spine J. 2006;15(6):794–798. doi: 10.1007/s00586-005-0931-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Biondi DM (2005) Cervicogenic headache: a review of diagnostic and treatment strategies. JADA (suppl. 2);05(4):6–22 [PubMed]
- 5.Bogduk N. The clinical anatomy of the cervical dorsal rami. Spine. 1987;4:319–330. doi: 10.1097/00007632-198207000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Bogduk N. Cervicogenic headache: anatomic basis and pathophysiologic mechanism. Curr Pain and Headache Rep. 2001;5(4):382–386. doi: 10.1007/s11916-001-0029-7. [DOI] [PubMed] [Google Scholar]
- 7.Bogduk N. The neck and headaches. Neurol Clin. 2004;22(1):151–171. doi: 10.1016/S0733-8619(03)00100-2. [DOI] [PubMed] [Google Scholar]
- 8.Bogduk N. Distinguishing primary headache disorders from cervicogenic headache: clinical and therapeutic implications. Headache Currents. 2005;2:27–36. doi: 10.1111/j.1743-5013.2005.20204.x. [DOI] [Google Scholar]
- 9.Bogduk N, Marsland A. The cervical zygapophyseal joints as source of neck pain. Spine. 1988;13(6):610–617. doi: 10.1097/00007632-198813060-00003. [DOI] [PubMed] [Google Scholar]
- 10.Bogduk N, Windsor M, Inglis A. The innervation of the cervical intervertebral discs. Spine. 1988;13(1):2–8. doi: 10.1097/00007632-198801000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Carette Fehling MG (2005) Clinical practice. Cervical radiculopathy. N Engl J Med 28 353(4):392–399 [DOI] [PubMed]
- 12.Carlsson AM. Assessment of chronic pain: aspects of the reliability and validity of the visual analoque scale. Pain. 1983;16:87–101. doi: 10.1016/0304-3959(83)90088-X. [DOI] [PubMed] [Google Scholar]
- 13.Davidoff RA. Trigger points and myofascial pain: toward understanding how they affect headaches. Cephalalgia. 1998;18(7):436–448. doi: 10.1046/j.1468-2982.1998.1807436.x. [DOI] [PubMed] [Google Scholar]
- 14.Espersen JO, Buhl EF, Fode K, Lindeberg KH, Madsen CB, Strange P, Wohlert L. Treatment of cervical disc disease using Cloward technique. General results, effect of different operative methods and complications in 1106 patients. Acta Neurochir. 1984;70:97–114. doi: 10.1007/BF01406047. [DOI] [PubMed] [Google Scholar]
- 15.Fredriksen TA, Salvesen R, Stolt-Nielsen A, Sjaastad O. Cervicogen headache: long-term postoperative follow-up. Cephalagia. 1999;39:21–27. doi: 10.1046/j.1468-2982.1999.1910897.x. [DOI] [PubMed] [Google Scholar]
- 16.Haldeman S, Dagenais S. Cervicogenic headaches; a critical review. Spine J. 2001;1(1):31–46. doi: 10.1016/S1529-9430(01)00024-9. [DOI] [PubMed] [Google Scholar]
- 17.Hoving JL, O´Leary EF, Niere KR, Green S, Buchbinder R. Validity of the neck disability index, Northwick park neck pain questionnaire and problem elicitation technique for measuring disability associated with whiplash-associated disorders. Pain. 2003;102:273–281. doi: 10.1016/S0304-3959(02)00406-2. [DOI] [PubMed] [Google Scholar]
- 18.International Classification of headache disorders (2004). Headache classification subcommittee of the International Headache Sociality, 2nd edn. Cephalalgia, 24 (suppl 1)
- 19.Jaeger B. Are cervicogenic headache due to myofascial pain and cervical spine dysfunction? Cephalalgia. 1989;9:157–164. doi: 10.1046/j.1468-2982.1989.0903157.x. [DOI] [PubMed] [Google Scholar]
- 20.Jensen R. Peripheral and central mechanism in tension-type headache: an update. Cephalalgia. 2003;23(suppl.1):49–52. doi: 10.1046/j.1468-2982.2003.00574.x. [DOI] [PubMed] [Google Scholar]
- 21.Jensen S. Neck related causes of headache. Aust fam Phys. 2005;34(8):635–639. [PubMed] [Google Scholar]
- 22.Kikuchi S, Macnab P, Moreu P. Localization of the level of symptomatic cervical disc degeneration. J Bone Joint Surg. 1981;2:272–277. doi: 10.1302/0301-620X.63B2.7217155. [DOI] [PubMed] [Google Scholar]
- 23.Langemark M, Olesen J. Pericranial tenderness in tension headache. A blind controlled study. Cephalalgia. 1987;7:249–255. doi: 10.1046/j.1468-2982.1987.0704249.x. [DOI] [PubMed] [Google Scholar]
- 24.Letchuman R, Gay RE, Shelerud RA, VanOstrand LA. Are tender points associated with cervical radiculopathy? Arch Phys Med Rehabil. 2005;86(7):1333–1337. doi: 10.1016/j.apmr.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 25.Lunsford LD, Bissonette DJ, Jannetta PJ, Sheptak PE, Zorub DS. Anterior surgery for cervical disc disease. Part 1: treatment of lateral disc herniation in 253 cases. J Neurosurg. 1980;53(1):1–11. doi: 10.3171/jns.1980.53.1.0001. [DOI] [PubMed] [Google Scholar]
- 26.Marcus D, Scharff L, Mercer MA, Turk DC. Musculoskeletal abnormalities in chronic headache; a controlled comparison of headache diagnostic groups. Headache. 1999;39:21–27. doi: 10.1046/j.1526-4610.1999.3901021.x. [DOI] [PubMed] [Google Scholar]
- 27.Michler RP, Bovim G, Sjaastad O. Disorders in the lower cervical spine. A cause of unilateral headache. Headache. 1991;31:550–551. doi: 10.1111/j.1526-4610.1991.hed3108550.x. [DOI] [PubMed] [Google Scholar]
- 28.O`Leary S, Falla D, Jull G. Recent advances in therapeutic exercise for the neck; implications for patients with head and neck pain. Aust Endod J. 2003;239(3):138–142. doi: 10.1111/j.1747-4477.2003.tb00540.x. [DOI] [PubMed] [Google Scholar]
- 29.Persson L, Moritz U (1994) Pain-drawing: a quantitative and qualitative model for pain assessment in cervico-brachial pain syndrome. 1993 The pain clinic 1:13–22
- 30.Persson LC, Carlsson JY Headache in patients with neck–shoulder–arm pain of cervical radicular origin. Headache. 1999;39(3):218–224. doi: 10.1046/j.1526-4610.1999.3903218.x. [DOI] [PubMed] [Google Scholar]
- 31.Persson LCG, Carlsson CA, Carlsson JY. Long lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar. A prospective, randomized study. Spine. 1997;22:751–758. doi: 10.1097/00007632-199704010-00007. [DOI] [PubMed] [Google Scholar]
- 32.Pfaffenrath V, Dankekar R, Pöllmann W. Cervicogenic headache. The clinical picture, radiological findings and hypothesese on its pathophysiology. Headache. 1987;27:495–499. doi: 10.1111/j.1526-4610.1987.hed2709495.x. [DOI] [PubMed] [Google Scholar]
- 33.Sjaastad O, Saunte C, Hovdahl H, Breivik H, Grønbæk E. “Cervicogenic” headache. An hypothesis. Cephalalgia. 1983;3:249–256. doi: 10.1046/j.1468-2982.1983.0304249.x. [DOI] [PubMed] [Google Scholar]
- 34.Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. The Cervicogenic Headache International Study Group. Headache. 1998;38:442–445. doi: 10.1046/j.1526-4610.1998.3806442.x. [DOI] [PubMed] [Google Scholar]
- 35.Tan JC, Nordin M. Role of physical therapy in the treatment of cervical disk disease. Orthop Clin North Am. 1992;23(3):435–449. [PubMed] [Google Scholar]
- 36.Torbjorn AF, Stolt-Nielsen A, Skaanes KO, Sjaastad O. Headache and the lower cervical spine: long-term postoperative follow up after decompressive neck surgery. Funct Neurol. 2003;18(1):17–28. [PubMed] [Google Scholar]
- 37.Travell JG, Simons DG. Myofascial pain and dysfunction. Trigger point manual. 1st edn. Baltimore: Willams and Wilkins; 1983. [Google Scholar]
- 38.Vernon H, Mior S. The neck disability index: a study of validity and reliability. J Manipulative Physiol Ther. 1991;14:409–415. [PubMed] [Google Scholar]