Abstract
Returning to work after disc surgery appears to be more heavily influenced by psychological aspects of work than by MR-identified morphological alterations. It is still not known whether psychosocial factors of importance for outcome after disc surgery are present preoperatively or develop in the postoperative phase. The aim of this study was to investigate the presence of work-related stress, life satisfaction and demanding life events, among patients undergoing first-time surgery for lumbar disc herniation in comparison with patients scheduled for arthroscopic knee surgery. Sixty-nine patients with disc herniation and 162 patients awaiting arthroscopy were included in the study, during the time period March 2003 to May 2005. Sixty-two percent of the disc patients had been on sick leave for an average of 7.8 months and 14 percent of the knee patients had been on sick leave for an average of 4.2 months. The psychosocial factors were investigated preoperatively using a questionnaire, which was a combination of the questionnaire of quality of work competence (QWC), life satisfaction (LiSat9) and life events as a modification of the social readjustment scale. There were no significant differences between the two groups in terms of work-related stress or the occurrence of demanding life events. The disc patients were significantly less satisfied with functions highly inter-related to pain and discomfort, such as present work situation, leisure-time, activities of daily living (ADL) function and sleep. Patients with disc herniation on sick leave were significantly less satisfied with their present work situation than knee patients on sick leave; this sub-group of patients with disc herniation also reported significantly higher expectations in relation to future job satisfaction than knee patients. The results indicate that psychosocial stress is not more pronounced preoperatively in this selected group of disc patients, without co-morbidity waiting for first-time disc surgery, than among knee patients awaiting arthroscopy. It was notable that the disc patients had high expectations in terms of improved job satisfaction after treatment by surgery.
Keywords: Lumbar disc herniation, Disc surgery, Psychosocial factors, Job satisfaction, Stress
Introduction
Even if radicular pain in disc herniation is one of the few spinal pain syndromes in which there appears to be a close association between pathomorphological changes and pain [1–4], it has been suggested that the morphology-based understanding of the pain pathogenesis in this condition needs to be re-evaluated [5]. One reason for this suggestion is that previous studies have demonstrated a high proportion, 20–70%, of disc herniations in asymptomatic individuals [6–8].
Although high proportions of successful outcome after disc surgery are consistently reported, there are still a significant number of patients who do not benefit from this procedure [9–12]. The underlying reasons for the fact that some patients have an excellent outcome and others a poor outcome, after the same type of surgical procedure in patients with identical preoperative clinical and MRI findings, are still largely unknown. Identifying, and possibly eliminating or treating, factors leading to a poor outcome must be regarded as a substantial challenge for people treating patients with disc hernia.
Psychosocial factors can be described as individual characteristics, such as psychological, cognitive or behavioural traits, but they can also be related to social aspects of the individual’s life, including job satisfaction, family life and other social circumstances. These factors may contribute to the explanation of why discectomy has not been universally successful, even when the morphological problem has been correctly addressed by surgery. A large number of studies have demonstrated an association between psychosocial factors and musculoskeletal disorders [13–17]. Psychosocial aspects of work may play an important role in the perpetuation of back pain, even among patients with disc herniations. In previous studies, it has been shown that a return to work after disc surgery is more heavily influenced by psychological factors and psychological aspects of work than by MR-identified morphological alterations [5, 18, 19].
The influence of psychosocial factors may also be reflected in life satisfaction, which is purely subjective and refers to a person’s feelings of happiness with his or her life [20]. Studies of the relationship between life satisfaction and low back pain (LBP) and sciatica are still sparse. It has been suggested that pronounced problems within family life play a role in the modulation of pain, but the empirical support for this assumption is insufficient [15]. Klapow et al. [21] have demonstrated greater life adversity and less satisfaction with social support networks in chronic LBP patients, compared with patients with good pain control.
The impact of demanding life events on the development and onset of LBP is not yet fully understood. Originally, the influence of life events was developed for the study of cardiovascular diseases, but it has since been used in the field of musculoskeletal research [22, 23]. Adverse life events appear to apply in particular to the development of chronic idiopathic LBP [21, 24]. To our knowledge, the question of whether stressful life events are more often found in patients with disc herniations and radicular pain than in others has not previously been studied.
Little attention has also been paid to the question of whether the psychosocial factors of importance for outcome after disc surgery are present preoperatively or develop in the postoperative phase.
The aim of this study was to compare the presence of work-related stress, life satisfaction and demanding life events among patients undergoing surgery for lumbar disc herniation to patients waiting for arthroscopic knee surgery due to a suspected degenerative meniscus tear.
Knee patients were chosen as a comparative group since their disease to a large extent is degenerative and this patient group has the same age profile as patients with disc herniation. Furthermore, arthroscopic meniscal knee surgery is usually reported as a surgical treatment with excellent outcome [25, 26], and psychosocial factors has to the authors knowledge not been reported to have a decisive impact on the result of treatment at this patient group.
Methods
Participants
The patients were recruited from two neighbouring orthopaedic clinics between March 2003 and May 2005. All eligible disc patients and knee patients who fulfilled the criteria for participation during the current time period were consecutively asked to participate. The demographic data are presented in Table 1. There was a significant difference between the two groups in terms of age; the mean age in the disc patient group was 40 years (SD 8.9), while it was 44 years in the knee patient group (SD 10). When it came to gender, workload, occupation requiring advanced or special education versus occupation not requiring advanced or special education and leisure time activity levels, there were no significant differences between the two groups.
Table 1.
Demographic data for patients with disc herniation and knee patients and P-values for comparison between groups
| Patients with disc herniation | Knee patients | P-value | |||
|---|---|---|---|---|---|
| n = 69 | Percentage | n = 162 | Percentage | ||
| Men | 39 | 56.5 | 94 | 58.0 | |
| Women | 30 | 43.5 | 68 | 42.0 | 0.833 |
| Mean age, years | 40 | 44 | 0.007 | ||
| Work load | |||||
| Heavy | 19 | 27.5 | 37 | 22.8 | |
| Moderate | 27 | 39.1 | 82 | 50.6 | |
| Light | 18 | 26.1 | 41 | 25.3 | |
| Unemployed | 5 | 7.2 | 2 | 1.2 | 0.208 |
| Educational level | |||||
| Occupations requiring university or specialist education | 22 | 31.9 | 54 | 33.3 | |
| Occupations not requiring advanced education | 45 | 65.2 | 100 | 61.7 | |
| Studying | 2 | 2.9 | 8 | 4.9 | 0.842 |
| Physical activity | |||||
| Leisure time physical activity, yes | 52 | 75.4 | 125 | 77.2 | |
| No. leisure time physical activity | 17 | 24.6 | 36 | 22.2 | |
| No data | – | 1 | 0.6 | 0.708 | |
| Physical activity occasionally | 32 | 46.4 | 59 | 36.4 | |
| Physical activity once a week | 9 | 13.0 | 21 | 13.0 | |
| Physical activity 2–5 times a week | 25 | 36.2 | 71 | 43.8 | |
| No data | 3 | 4.3 | 11 | 6.8 | 0.270 |
| Mean time of complaints, months | 18 | 21 | 0.100 | ||
Disc patients
Patients diagnosed with lumbar disc herniation, verified by MRI and clinical examination by an orthopaedic surgeon, were included in the study. All these patients had radiating leg pain and were scheduled for disc surgery. In all patients, the surgeon had recommended treatment by surgery and the patient had given his/her consent.
Eligible patients were between 18 and 60 years of age, had not had any previous spinal surgery and disc herniation was the main indication for decompression surgery. Patients undergoing acute surgery, or who had any co-morbidity influencing daily activities or working capacity, or who were not fluent in the Swedish language were excluded.
During the recruitment period, 72 patients fulfilled the criteria to participate in the study. Sixty-nine disc patients agreed to participate in the study and were included, while three patients declined participation. One patient had a history of neck pain, but at the time for inclusion in this study she said the neck did not bother her, and that she was on sick leave only because of the disc herniation. She was included, but nevertheless she got sickness pension due to neck problems the year after treatment by surgery.
Forty-three patients were on sick leave at the time of the investigation (62.3%). The mean length of sick leave was 7.8 months (range 0.5–40.0).
Knee patients
The knee patients were between 18 and 60 years of age and were waiting for arthroscopic surgery due to a suspected meniscus tear. The medical records of the patients were screened by the investigator for possible candidates. Likely participants were contacted by telephone, to determine whether they fulfilled all the inclusion criteria. Patients with co-morbidity influencing daily activities and working capacity, and those who were not able to understand Swedish, were excluded. In all, 232 patients were contacted and they all agreed to participate. One hundred and sixty-two of these patients received and managed to return a completed questionnaire before the operation.
Twenty-two knee patients were on sick leave (13.6%); the mean length of sick leave was 4.2 months (range 1.0–13.0).
The study was approved by our regional ethics committee.
Measures
Demographics
Background variables, including age, gender, diagnosis, occupation, sick level and physical activity level, were recorded (Table 1). Classification of occupational status was based on the Swedish Standard Classification [27], which in turn is based on International Standard Classification of Occupation 1988 (ISCO-88). Originally, this classification had nine main job classes, but they were merged into two classes. One class represented occupations requiring advanced or specialist education (university or equivalent), while the other class represented occupations not requiring advanced or specialist education.
Assessment questionnaires
The psychosocial factors were assessed by a questionnaire 1–4 weeks before the disc hernia or the arthroscopic knee operation.
Psychosocial stress at work
Work-related stress was measured by a short form of the questionnaire of quality of work competence (QWC). These scales have been developed in a series of studies, based on samples totalling approximately 100,000 employees. The questionnaire has been shown to have acceptable validity and reliability [28]. The questionnaire contains three overall items about job satisfaction; current, during the last year and expectations about job satisfaction during the following year. The following questions cover the subsequent areas/indices: mental energy, work climate, work tempo, performance management, participatory management, skills development, organisational efficacy and leadership. Each enhancement index consists of 1 to 5 multi-point questions with standard Likert check-off scales. The percentage scores on the enhancement indices range from a possible low of 0% to a high of 100%.
Life satisfaction
Satisfaction with life as a whole and with an additional eight domains of life was assessed with a modified life satisfaction questionnaire (LiSat9), a nine-item self-administered checklist, with the aim of characterising life satisfaction, both global (one item) and domain specific (eight items) [29]. The items on LiSat-9 have been found to show acceptable test–retest reliability, specificity and sensitivity [30, 31]. We omitted one question relating to sexual life and added one question relating to satisfaction with sleep. The domains were vocation, economy, spare time, contact with friends, partner relationship, family life, sleep and activities of daily living (ADL).
The levels of life satisfaction were reported on a six-grade scale ranging from very dissatisfied to very satisfied.
Additionally, in the analyses, a dichotomy was used where grades 5 and 6 were classified as satisfied and grades 1–4 as not satisfied.
Life events
A modification of the social readjustment scale (SRSS) [32] was used retrospectively to assess stressful life events, during the last 2 years before planned surgery. This scale measures a cluster of social events requiring changes in ongoing life adjustment and identifies changes in family constellation, marriage, occupation, economics, residence, group and peer relations and health. The scale contains 18 questions with response alternatives yes or no. The total life events score was obtained by calculating the number of points according to the following scale: no = 0, yes = 1.
Statistics
A power analysis was carried out prior to the study. It was determined that a total of 70 disc patients and 70 knee patients were needed to detect a mean score difference of 15 points in the QWC subscale work related stress with a 80% power and at a 5% significant level. As we had access to 162 knee patients who were suitable for inclusion we included all these patients, to ensure proper power. The chosen level of significance was P < 0.05, two-tailed.
Demographics were compared between groups using the Mann–Whitney rank sum test. The questions belonging to the same dimension in the QWC questionnaire (psychosocial stress at work) were summarised and a median value was calculated for each dimension. The different dimensions were compared between groups using the Mann–Whitney rank sum test, as well as the three questions about overall job satisfaction.
Since the distributions of the variable present job satisfaction were not normally distributed, a non-parametric test for interactions, based on aligned ranks (program written in FORTRAN) [33] was also applied. Briefly, the test is based on the joint ranking of all observations after removing the effect of the factor group belonging (disc herniation or knee patient). Suitably normalised, the weighted sum of squared differences between the two sub-categories’ mean rank (each combination of group and sick leave) and the total mean rank will be approximately F-distributed. If the null hypothesis was rejected, a Kruskal–Wallis test was run with each group (disc herniation and controls) and sick-leave combination constituting a separate sub-category. A two-sided P-value of less than 0.05 was considered to be significant in all the analyses of main effects, while the P-value when testing for the presence of interactions was less than 0.1.
For each item on LiSat9, differences between groups were analysed using the Mann–Whitney rank sum test. A dichotomy was also used to separate those who were satisfied (grades 5 and 6) from those who were not satisfied (grades 1–4) according to Fugl-Mayer [34].
Differences in the proportions between groups regarding life events were tested using Chi-square statistics.
Results
Psychosocial stress at work
There were no significant differences between the two groups in terms of experience of work-related exhaustion, work climate, work tempo, performance management, participatory management, skills development, organisational efficacy and leadership (Table 2).
Table 2.
Median scores and interquartile range on the quality work competence (QWC) indices, for patients with disc herniation and knee patients respectively. Medians, q3–q1 and P-values
| QWC areas | Patients with disc herniation | Knee patients | P-value | ||
|---|---|---|---|---|---|
| Median | q3–q1 | Median | q3–q1 | ||
| Job satisfaction previous year | 70 | 90–50 | 70 | 80–50 | 0.817 |
| Job satisfaction now | 50 | 80–20 | 70 | 85–50 | 0.003 |
| Expectations of job satisfaction next year | 80 | 92.5–70 | 70 | 90–60 | 0.095 |
| Work climate | 65 | 81.25–33.75 | 65 | 80–50 | 0.471 |
| Work tempo | 58 | 71–44 | 56 | 74–39.5 | 0.912 |
| Work-related exhaustion | 47 | 58–34 | 44 | 58–34 | 0.641 |
| Performance feedback | 72 | 85–48.75 | 70 | 85–50 | 0.804 |
| Participatory management | 70 | 92.5–37.5 | 70 | 80–40 | 0.865 |
| Skills development | 80 | 100–70 | 80 | 100–70 | 0.910 |
| Efficiency | 80 | 100–70 | 80 | 100–70 | 0.970 |
| Leadership | 80 | 100–70 | 80 | 100–70 | 0.910 |
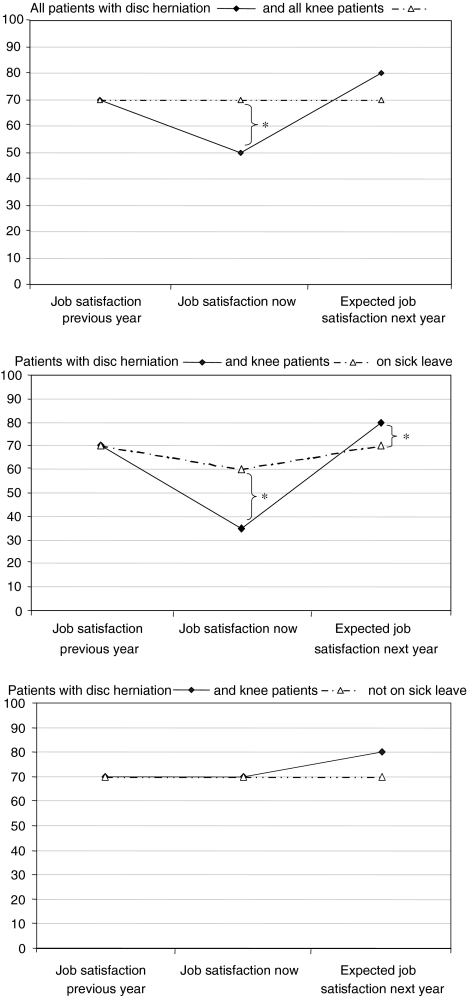
The disc patients were significantly less satisfied with their present work situation compared with the knee patients. The median score among disc patients was 50, whereas it was 70 for knee patients (Fig. 1).
Fig. 1.
Job satisfaction. Comparison of medians of job satisfaction between patients with disc herniation and knee patients. The brackets indicate a significant difference between the two groups, *P < 0.05. Both groups rated job satisfaction the previous year at a median of 70, irrespectively of whether or not they were on sick leave
Patients with disc herniation who were on sick leave rated their present work situation at a median of 35, compared with patients with disc herniation who were not on sick leave, who rated their current job satisfaction at a median of 70 (P = 0.001). This pattern was not seen among the knee patients.
Consequently, there was an interaction between the variables of group belonging, sick leave and current job satisfaction (Table 3; Fig. 1).
Table 3.
Job satisfaction now, a comparison between patients on sick leave/not on sick leave among patients with disc herniation and knee patients respectively. Medians and q3–q1
| Disc herniation on sick leave | Disc herniation not on sick leave | Knee patients on sick leave | Knee patients not on sick leave | |
|---|---|---|---|---|
| n = 36 | n = 25 | n = 20 | n = 132 | |
| Median | 35 | 70 | 60 | 70 |
| q3–q1 | 55 | 40 | 68 | 40 |
0 = very bad, 100 = very good
When patients with disc herniation on sick leave were compared with knee patients on sick leave in terms of the differences between current job satisfaction and expectations relating to job satisfaction next year, both groups expected significantly higher job satisfaction next year. The expected change in job satisfaction (job satisfaction previous year compared with expectations of job satisfaction next year) was significantly higher among patients with disc herniation compared with knee patients (P = 0.013) (Fig. 1).
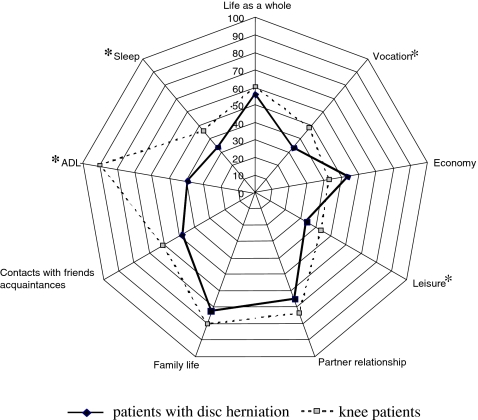
Life satisfaction
There was no significant difference when it came to life as a whole, economy, or contacts with partner or friends, between disc patients and knee patients (Fig. 2).
Fig. 2.
Life satisfaction. Proportions (%) of patients with disc herniation and knee patients respectively, who were satisfied or very satisfied (grades 5 or 6) according to LiSat9. Asterisk denotes P < 0.05 for comparison between groups
Only 33.3% of the patients with disc herniation were very satisfied or satisfied with their vocational situation, compared with 46.9% of the knee patients; this difference was significant. There was also a significant difference between the two groups in terms of leisure time, ADL and sleep (P < 0.05); 39.1% of the patients with disc herniation compared with 90% of the knee patients were very satisfied or satisfied with their ADL function.
When asked about “life as a whole”, 28.9% of the disc patients were rather to very dissatisfied, whereas only 6.9% of the knee patients were rather to very dissatisfied, but this difference did not reach a significant level. Nor did the dimensions relating to economy, partnership relations, family life and contacts with friends/acquaintances.
Life events
There was no difference between disc patients and knee patients in terms of the self-reported occurrence of demanding life events during the last 2 years before planned disc surgery (Table 4). The mean numbers of demanding life events during the last 2 years were 3.01 for disc patients and 2.93 for knee patients.
Table 4.
Occurrence of life events among patients with disc herniation and knee patients respectively, presented as the percentage of numbers of yes, and P-values for comparisons between groups
| Life events | Patients with disc herniation | Knee patients | P-value |
|---|---|---|---|
| Yes (%) | Yes (%) | ||
| Conflict with spouse | 21 | 20 | 0.938 |
| Conflict with relative/friends | 17 | 17 | 0.862 |
| Physical injury | 25 | 27 | 0.733 |
| Physical injury relative/close friend | 19 | 21 | 0.675 |
| Deaths of spouse/relative | 0 | 3 | 0.181 |
| Deaths of relative/close friend | 28 | 21 | 0.223 |
| Been object of harassment (bullying) at school or work | 7 | 5 | 0.522 |
| Strained financial position | 29 | 24 | 0.412 |
| Conflict at work | 19 | 21 | 0.708 |
| Low job control | 26 | 26 | 0.944 |
| Other important negative events | 21 | 18 | 0.642 |
| Divorce or separation | 7 | 14 | 0.149 |
| Entering into marriage or partnership | 7 | 14 | 0.154 |
| Forced to change domicile | 10 | 5 | 0.096 |
| Given birth to child or adoption | 15 | 8 | 0.101 |
| Forced to change work | 10 | 13 | 0.520 |
| Reduced job responsibility | 6 | 5 | 0.818 |
| Increased job responsibility | 37 | 45 | 0.295 |
Discussion
In this study, there was no difference between the presence of psychosocial stress factors among patients with disc herniation scheduled for disc surgery and knee patients waiting for arthroscopic knee surgery. Regarding perceived work-related stress, and demanding life events, there were no differences between the disc patients and knee patients.
There were, however, some differences between the two groups of patients in terms of satisfaction with their present work situation, leisure time, ADL function and sleep. The difference between patients with disc herniation and knee patients in terms of satisfaction with their present work situation could be partly explained by the fact that more of the disc patients were on sick leave (64% of the patients with disc herniation, compared with 14% of the knee patients). However, when the patients with disc herniation on sick leave were compared with the knee patients on sick leave, the patients with disc herniation were significantly less satisfied with their present work situation. This sub-group of patients also had significantly higher expectations of future job satisfaction. Since low job satisfaction previously has been reported to have a negative impact on return to work after disc surgery this result is noteworthy [5, 35].
In many ways, the study groups were comparable. They were approximately of the same age category, their disease was degenerative and they were waiting for orthopaedic surgery. They also had differences, such as more disabling pain and working incapacity among the disc patients.
Tools are needed to identify patients who are “at risk” of a poor outcome after disc surgery. It has been presumed that environmental stress plays a role in the development and preservation of pain [36].
In a previous study by Boos et al. [7] in which asymptomatic controls (without pain) were compared with patients with symptoms (with pain) of disc herniation, higher occupational mental stress and less job satisfaction were found among the symptomatic patients. In our study, we were not able to confirm that the psychosocial factors at work played such a prominent role preoperatively as they did in the study by Boos. This discrepancy in results could be due to differences in the patients chosen as controls. The controls in the study by Boos had no pain at all, as they had asymptomatic disc herniations, whereas our comparison group consisted of knee patients listed for arthroscopic surgery. Patients with a suspected meniscus tear treated by arthroscopic knee surgery constitute a group of patients who have been reported to have a successful outcome in 88–95.7% of cases [25, 26] in comparison to a reported successful outcome of 61–69% [37, 38] among patients treated by disc surgery. However, the symptomatic disc patients in the study by Boos had several similarities to our study group; a scheduled discectomy, no previous back surgery and no language deficiency.
The findings of Leino-Arjas et al., who studied the 1-year incidence of hospitalisation due to intervertebral disc disorders among Finns, are in line with the findings of Boos. They found that low job control was one important factor for an increase in the risk of hospitalisation [39]. However, all our patients were treated surgically compared with 52.3% of the patients in the study by Leino-Arjas et al. According to earlier studies, psychosocial factors might be more frequently present among patients who do not fulfil the criterion for surgery [22, 40]. It could be presumed that these patients were more frequently represented in the study by Leino-Arjas than in our study, which could be one explanation of the divergent results.
The natural history of individuals with asymptomatic disc abnormalities and predictors of future LBP were investigated in another study by Boos [41]. The only morphological abnormality exhibiting an impact on the outcome variables (=LBP-related medical consultation and work absence) was the extent of neural compromise. Other predictive factors were listlessness, physical job characteristics, adverse influence of work on private life and deficient social support by the closest co-worker. These factors explained 42% of the criterion variance. On the basis of this study, psychosocial factors could be expected to be more important than we demonstrated in our study. However, one important difference between the studies was the fact that none of the individuals in the study by Boos had radicular pain, even though 29.3% had minor neural compromise. In our study, all the disc patients had radicular pain. Another difference relating to the study population in our study compared with the study by Boos was the presence of co-morbidity, which was an exclusion criterion in our study but not in the study by Boos. Since co-morbidity is a factor influencing life in most aspects, it might be a confounding factor, which may contribute to perceived psychosocial stress [42].
The mean period of sciatic pain was 15 months (range 2–120) in our patients and 62% of the patients were on sick leave, with a mean duration of sick leave of 7.8 months (range 0–40), compared with the controls of whom 14% were on sick leave, with a mean duration of 4.2 months (range 1–13). It could be suspected that the sick-leave rate among the disc patients would contribute to the development of concurrent adverse psychosocial factors. The only significant difference we found was lower rates regarding present job satisfaction among patients with disc herniation on sick leave, compared to knee patients on sick leave. One explanation to this phenomenon could be that individuals with disc herniation and poor job satisfaction might seek sick leave more actively than individuals with high job satisfaction, something revealed already through the so called Boeing study [43].
Besides that, it is possible that sick leave has more influence on individual psychological factors such as depression and anxiety, which was not examined in this study. It is well known that sick leave due to LBP of unknown origin has an impact on social life. Our results indicate that this might not be the situation when there is a morphological origin for the diagnosis.
From previous studies, we know that disc patients have reduced quality of life/life satisfaction both before and after disc surgery [44, 45]. In this study, we found that disc patients were dissatisfied with aspects of life, which are highly influenced by pain and discomfort.
Life events have above all been shown to have an impact on chronic LBP of uncertain origin [24, 40]. We have only found one previous study in which stressful life events among patients with LBP with a definite organic origin were evaluated. In this study by Leavitt and co-workers, the occurrence of stressful life events was compared between LBP patients with pain of non-organic origin, probable organic origin and definite organic disease. The number of stressful events during the previous years did not differ between the groups with different levels of organic contribution to their symptoms. Those with demonstrable organic disease had the same number of stressful events as those without demonstrable organic disease [46]. Further, these groups of patients did not describe a higher occurrence of stressful life events than healthy controls reported elsewhere in the literature, which is in line with our results [47].
Although life events may be important when they occur, the events evaluated here occur only infrequently. As a result, the methodology may not be sensitive to this variable, even though the patients in this study were asked to describe life events, which had occurred during the last 2 years. Lack of sensitivity in the questionnaires we used may also explain why psychosocial factors were not reflected in our study group. On the other hand, we used standardised, reliable and preferably validated instruments, previously used to study these variables.
Another possible weakness in our study, which might have had an effect on the results, is our comparison group. We felt that the risk of other, uncontrolled confounding factors and the risk of drop-outs would have been immediate if we had chosen controls from the general population. To our knowledge, there are no studies indicating that psychosocial factors are more pronounced among patients with meniscus tears than among others, even if this not necessarily implies that such factors are non-existing among patients waiting for arthroscopic knee surgery. Despite that the knee patients probably had less pain than the disc patients, they had sufficient symptoms to merit a surgical procedure and had had their problems for a while. This circumstance could have an impact on psychosocial factors and job satisfaction also in this group. If anything, this would diminish the differences we found between the two groups. We therefore believe that the difference between the two groups is derived from real differences between the two groups, based on more disabling pain and discomfort among the patients with disc herniation.
The reason why the patients with disc herniations on sick leave were less satisfied with their present work situation than the controls on sick leave is unclear. Based on the assumption mentioned earlier, it could be due to the longer sick leave duration among the disc patients. Regarding job satisfaction previous year, there was no significant difference between patients with disc herniation on sick leave compared to those who were not on sick leave. Since the patients with disc herniation had been on sick leave on average 3.5 month longer than the knee patients, recall bias might have had influenced the answers among patients with disc herniation. The significantly higher expectations of future job satisfaction among the patients with disc herniation are also noteworthy. This phenomenon might also be explained by the longer sick-leave duration within this group.
Having high expectations of treatment are probably of advantages for the outcome of surgery, but it could also be a problem if the expectations are not fulfilled.
Another variable which might bias the report on other variables (e.g. life satisfaction) is pain intensity. It is reasonable to believe that the disc patients had higher pain levels than the knee patients. However, since pain not always is the main symptom among knee patients with a suspected meniscus tear, we decided not to compare this variable between the two groups.
The influence of psychosocial factors on patients with disc herniation needs to be further analysed, preferably in prospective studies. For this purpose, there is also a need for more sensitive examination forms, which can be easily handled in clinical settings. The identification of sub-groups of patients with different needs during the rehabilitation process is probably crucial when it comes to improving the outcome after disc herniation surgery.
Conclusion
Patients with disc herniation who were scheduled for first-time surgery without co-morbidity, did not have more work-related stress or demanding life events in the previous 2 years before surgery than a group of patients scheduled for knee arthroscopy. The disc patients were less satisfied with their present work situation and leisure time, ADL and sleep functions, factors highly inter-related with disabling pain and discomfort. The disc patients had higher expectations of improvements relating to job satisfaction compared with the knee patients.
References
- 1.Brisby H, Byrod G, Olmarker K, Miller VM, Aoki Y, Rydevik B. Nitric oxide as a mediator of nucleus pulposus-induced effects on spinal nerve roots. J Orthop Res. 2000;18:815–820. doi: 10.1002/jor.1100180520. [DOI] [PubMed] [Google Scholar]
- 2.Kawakami M, Tamaki T, Hayashi N, Hashizume H, Nishi H. Possible mechanism of painful radiculopathy in lumbar disc herniation. Clin Orthop Relat Res. 1998;351:241–251. doi: 10.1097/00003086-199806000-00029. [DOI] [PubMed] [Google Scholar]
- 3.Nachemson AL. Newest knowledge of low back pain. A critical look. Clin Orthop Relat Res. 1992;279:8–20. [PubMed] [Google Scholar]
- 4.Olmarker K, Larsson K. Tumor necrosis factor alpha and nucleus-pulposus-induced nerve root injury. Spine. 1998;23:2538–2544. doi: 10.1097/00007632-199812010-00008. [DOI] [PubMed] [Google Scholar]
- 5.Schade V, Semmer N, Main CJ, Hora J, Boos N. The impact of clinical, morphological, psychosocial and work-related factors on the outcome of lumbar discectomy. Pain. 1999;80:239–249. doi: 10.1016/S0304-3959(98)00210-3. [DOI] [PubMed] [Google Scholar]
- 6.Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. J Bone Joint Surg Am. 1990;72:403–408. [PubMed] [Google Scholar]
- 7.Boos N, Rieder R, Schade V, Spratt KF, Semmer N, Aebi M. 1995 Volvo Award in clinical sciences. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine. 1995;20:2613–2625. doi: 10.1097/00007632-199512150-00002. [DOI] [PubMed] [Google Scholar]
- 8.Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med. 1994;331:69–73. doi: 10.1056/NEJM199407143310201. [DOI] [PubMed] [Google Scholar]
- 9.Asch HL, Lewis PJ, Moreland DB, Egnatchik JG, Yu YJ, Clabeaux DE, Hyland AH. Prospective multiple outcomes study of outpatient lumbar microdiscectomy: should 75 to 80% success rates be the norm? J Neurosurg. 2002;96:34–44. doi: 10.3171/spi.2002.96.1.0034. [DOI] [PubMed] [Google Scholar]
- 10.Daneyemez M, Sali A, Kahraman S, Beduk A, Seber N. Outcome analyses in 1072 surgically treated lumbar disc herniations. Minim Invasive Neurosurg. 1999;42:63–68. doi: 10.1055/s-2008-1053372. [DOI] [PubMed] [Google Scholar]
- 11.Findlay GF, Hall BI, Musa BS, Oliveira MD, Fear SC. A 10-year follow-up of the outcome of lumbar microdiscectomy. Spine. 1998;23:1168–1171. doi: 10.1097/00007632-199805150-00019. [DOI] [PubMed] [Google Scholar]
- 12.Loupasis GA, Stamos K, Katonis PG, Sapkas G, Korres DS, Hartofilakidis G. Seven- to 20-year outcome of lumbar discectomy. Spine. 1999;24:2313–2317. doi: 10.1097/00007632-199911150-00005. [DOI] [PubMed] [Google Scholar]
- 13.Bigos SJ, Battie MC, Spengler DM, Fisher LD, Fordyce WE, Hansson TH, Nachemson AL, Wortley MD. A prospective study of work perceptions and psychosocial factors affecting the report of back injury. Spine. 1991;16:1–6. doi: 10.1097/00007632-199101000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Bongers PM, Winter CR, Kompier MA, Hildebrandt VH. Psychosocial factors at work and musculoskeletal disease. Scand J Work Environ Health. 1993;19:297–312. doi: 10.5271/sjweh.1470. [DOI] [PubMed] [Google Scholar]
- 15.Hoogendoorn WE, Poppel MN, Bongers PM, Koes BW, Bouter LM. Systematic review of psychosocial factors at work and private life as risk factors for back pain. Spine. 2000;25:2114–2125. doi: 10.1097/00007632-200008150-00017. [DOI] [PubMed] [Google Scholar]
- 16.Linton SJ. Occupational psychological factors increase the risk for back pain: a systematic review. J Occup Rehabil. 2001;11:53–66. doi: 10.1023/A:1016656225318. [DOI] [PubMed] [Google Scholar]
- 17.Moon S, Sauter S. Psychosocial aspects of musculoskeletal disorders in office work. London: Taylor and Francis; 1996. [Google Scholar]
- 18.Junge A, Frohlich M, Ahrens S, Hasenbring M, Sandler A, Grob D and Dvorak J (1996) Predictors of bad and good outcome of lumbar spine surgery. A prospective clinical study with 2 years’ follow up. Spine 21:1056–1064; discussion 1064–1065 [DOI] [PubMed]
- 19.Trief PM, Grant W, Fredrickson B. A prospective study of psychological predictors of lumbar surgery outcome. Spine. 2000;25:2616–2621. doi: 10.1097/00007632-200010150-00012. [DOI] [PubMed] [Google Scholar]
- 20.Melin R, Fugl-Meyer AR. On prediction of vocational rehabilitation outcome at a Swedish employability institute. J Rehabil Med. 2003;35:284–289. doi: 10.1080/16501970310012437. [DOI] [PubMed] [Google Scholar]
- 21.Klapow JC, Slater MA, Patterson TL, Atkinson JH, Weickgenant AL, Grant I, Garfin SR. Psychosocial factors discriminate multidimensional clinical groups of chronic low back pain patients. Pain. 1995;62:349–355. doi: 10.1016/0304-3959(94)00276-K. [DOI] [PubMed] [Google Scholar]
- 22.Kaila-Kangas L, Kivimaki M, Riihimaki H, Luukkonen R, Kirjonen J, Leino-Arjas P. Psychosocial factors at work as predictors of hospitalization for back disorders: a 28-year follow-up of industrial employees. Spine. 2004;29:1823–1830. doi: 10.1097/01.BRS.0000134572.46151.0A. [DOI] [PubMed] [Google Scholar]
- 23.Theorell T. Possible mechanisms behind relationship between the demand-control-support model and disorders of the locomotor system. In: Moon SD, Sauter SL, editors. Beyond biomechanics: psychosocial aspects of musculoskeletal disorders in office work. London: Taylor & Frances; 1996. pp. 65–73. [Google Scholar]
- 24.Lampe A, Sollner W, Krismer M, Rumpold G, Kantner-Rumplmair W, Ogon M, Rathner G. The impact of stressful life events on exacerbation of chronic low-back pain. J Psychosom Res. 1998;44:555–563. doi: 10.1016/S0022-3999(97)00231-6. [DOI] [PubMed] [Google Scholar]
- 25.Burks RT, Metcalf MH, Metcalf RW. Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy. 1997;13:673–679. doi: 10.1016/S0749-8063(97)90000-1. [DOI] [PubMed] [Google Scholar]
- 26.Chatain F, Robinson AH, Adeleine P, Chambat P, Neyret P. The natural history of the knee following arthroscopic medial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 2001;9:15–18. doi: 10.1007/s001670000146. [DOI] [PubMed] [Google Scholar]
- 27.Reports on Statistical Co-ordinations for the Official Statistics of Sweden (1998:3)
- 28.Arnetz JE, Arnetz BB. The development and application of a patient satisfaction measurement system for hospital-wide quality improvement. Int J Qual Health Care. 1996;8:555–566. doi: 10.1016/S1353-4505(96)00073-7. [DOI] [PubMed] [Google Scholar]
- 29.Fugl-Meyer AR, Eklund M, Fugl-Meyer KS. Vocational rehabilitation in northern Sweden. III. Aspects of life satisfaction. Scand J Rehabil Med. 1991;23:83–87. [PubMed] [Google Scholar]
- 30.Brännholm I-B, Lundmark P, Fugl-Mayer K, Fugl-Mayer A. On work and life satisfaction. J Rehabil Sci. 1991;4:29–34. [Google Scholar]
- 31.Gil A, Martinez E, Oyaguez I, Palacios G, Rejas J. Erectile dysfunction in a primary care setting: results of an observational, no-control-group, prospective study with sildenafil under routine conditions of use. Int J Impot Res. 2001;13:338–347. doi: 10.1038/sj.ijir.3900782. [DOI] [PubMed] [Google Scholar]
- 32.Holmes TH, Rahe RH. The social readjustment rating scale. J Psychosom Res. 1967;11:213–218. doi: 10.1016/0022-3999(67)90010-4. [DOI] [PubMed] [Google Scholar]
- 33.Ohrvik J. Nonparametric methods in the two-way layout. Chiang Mai J Sci. 2002;29:103–115. [Google Scholar]
- 34.Fugl-Meyer KS (1997) Health, sexual ability and life satisfaction. In: Lewin B (ed) Sexuality in Sweden. Folkhälsoinstitutet, Stockholm, pp 219–233
- 35.Mannion AF, Elfering A. Predictors of surgical outcome and their assessment. Eur Spine J. 2006;15:S93–S108. doi: 10.1007/s00586-005-1045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ferguson SA, Marras WS. A literature review of low back disorder surveillance measures and risk factors. Clin Biomech (Bristol, Avon) 1997;12:211–226. doi: 10.1016/S0268-0033(96)00073-3. [DOI] [PubMed] [Google Scholar]
- 37.Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the maine lumbar spine study. Spine. 2005;30:936–943. doi: 10.1097/01.brs.0000158953.57966.c0. [DOI] [PubMed] [Google Scholar]
- 38.Weber H. Lumbar disc herniation. A controlled, prospective study with ten years of observation. Spine. 1983;8:131–140. doi: 10.1097/00007632-198303000-00003. [DOI] [PubMed] [Google Scholar]
- 39.Leino-Arjas P, Kaila-Kangas L, Kauppinen T, Notkola V, Keskimaki I, Mutanen P. Occupational exposures and inpatient hospital care for lumbar intervertebral disc disorders among Finns. Am J Ind Med. 2004;46:513–520. doi: 10.1002/ajim.20084. [DOI] [PubMed] [Google Scholar]
- 40.Craufurd DI, Creed F, Jayson MI. Life events and psychological disturbance in patients with low-back pain. Spine. 1990;15:490–494. doi: 10.1097/00007632-199006000-00011. [DOI] [PubMed] [Google Scholar]
- 41.Boos N, Semmer N, Elfering A, Schade V, Gal I, Zanetti M, Kissling R, Buchegger N, Hodler J, Main CJ. Natural history of individuals with asymptomatic disc abnormalities in magnetic resonance imaging: predictors of low back pain-related medical consultation and work incapacity. Spine. 2000;25:1484–1492. doi: 10.1097/00007632-200006150-00006. [DOI] [PubMed] [Google Scholar]
- 42.Gijsen R, Hoeymans N, Schellevis FG, Ruwaard D, Satariano WA, Bos GA. Causes and consequences of comorbidity: a review. J Clin Epidemiol. 2001;54:661–674. doi: 10.1016/S0895-4356(00)00363-2. [DOI] [PubMed] [Google Scholar]
- 43.Bigos SJ, Battie MC, Spengler DM, Fisher LD, Fordyce WE, Hansson T, Nachemson AL, Zeh J. A longitudinal, prospective study of industrial back injury reporting. Clin Orthop Relat Res. 1992;279:21–34. [PubMed] [Google Scholar]
- 44.Jansson KA, Nemeth G, Granath F, Jonsson B, Blomqvist P. Health-related quality of life in patients before and after surgery for a herniated lumbar disc. J Bone Joint Surg Br. 2005;87:959–964. doi: 10.1302/0301-620X.87B7.16240. [DOI] [PubMed] [Google Scholar]
- 45.Zanoli Outcome assessment in lumbar spine surgery. Acta Orthop Suppl. 2005;76:5–47. [PubMed] [Google Scholar]
- 46.Leavitt F, Garron DC, Bieliauskas LA. Stressing life events and the experience of low back pain. J Psychosom Res. 1979;23:49–55. doi: 10.1016/0022-3999(79)90071-0. [DOI] [PubMed] [Google Scholar]
- 47.Bieliauskas Sample size characteristics and scores on the social readjustment rating scale. J Psychosom Res. 1976;20:201–205. doi: 10.1016/0022-3999(76)90021-0. [DOI] [PubMed] [Google Scholar]