Abstract
Aortic dissection masquerading as ischemic stroke is particularly challenging in the era of thrombolysis as a result of narrow diagnostic time window and severe hemorrhagic potential. We describe a case of a 77-year-old patient with a presumed ischemic cerebral infarct, in whom planned treatment with tissue plasminogen activator therapy (TPA) was withheld because of partial spontaneous improvement in his condition. Shortly afterwards, newly elicited clues in the medical history and physical examination led to timely diagnosis and treatment of ascending thoracic aorta dissection, which was the underlying disorder. Analysis of the features of this case and similar previously published cases illustrates the importance of using and mastering basic diagnostic skills.
KEY WORDS: aortic dissection, stroke, thrombolysis
Aortic dissection is an uncommon, life-threatening but treatable emergency that typically presents with tearing chest and back pain. The onset of pain is usually abrupt, and its maximal level is reached suddenly. Distal progression of the dissection process is suggested by extension of the pain to the abdomen, hips, and legs. A pain-free interval may follow the initial pain of aortic dissection, lasting from hours to days, and the subsequent return of pain usually heralds impending rupture. Nonetheless, 10% to 55% of patients will not experience any significant pain. Organ system involvement is present in more than one third of patients, mainly owing to the development of ischemia caused by the obstruction of branch arteries originating from the aorta. The organ system most commonly involved is the cardiovascular system with manifestations of aortic regurgitation, hypotension, and left ventricular regional wall abnormalities in 18–50%, 25% and 10–15% of cases, respectively; acute pericardial effusion, cardiac tamponade, and symptomatic ischemia of an extremity may also ensue. Various neurological deficits were described in 18–30% of cases of aortic dissection, most commonly cerebral ischemia in 5–10%. Cerebral hypoperfusion may result in symptoms ranging from altered mental status to syncope. Spinal cord syndromes may develop in up to 10% of cases, and peripheral neuropathies have also been described.1–4
Thrombolytic treatment with tissue plasminogen activator (TPA) is an established therapy for selected patients with ischemic stroke within a narrow time window of 3 hours from the onset of symptoms.5 However, severe complications and poor outcome are likely to ensue if a patient with acute aortic dissection is inadvertently treated with thrombolytic agents.6
We describe a patient presenting with a clinical picture of ischemic stroke who was eligible for thrombolytic treatment and in whom the underlying diagnosis of acute thoracic aortic dissection was made by a combination of chance and a high level of clinical suspicion. The early diagnosis led to a favorable outcome.
CASE REPORT
A 77-year-old White male was brought by his friend to the busy emergency department (ED) of a tertiary care center at 8 p.m. suffering from a decreased level of consciousness. The Internal Medicine resident who examined the patient was informed by the accompanying friend that while out walking with him an hour earlier, the patient had suddenly complained of general weakness eventually collapsing onto the seat of the friend’s car. From that moment, the patient was unresponsive. The patient was unmarried, lived alone, and had no close family or friends besides his present companion. To the best of the friend’s knowledge, the patient had no significant medical problems, but his blood pressure had been slightly elevated during the preceding weeks and he had been prescribed cilazapril (an angiotensin-converting enzyme inhibitor, not commercially available in the US). On examination in the ED, the patient was in stupor (Glasgow Coma Scale of 8–9), reacting only to pain. His blood pressure was 112/55 mmHg, pulse rate was 51 beats per minute and regular, rectal temperature was 38°C, and his oxygen saturation was 95% while breathing room air. There was no nuchal rigidity. Jugular venous pressure was 6 cm H2O. Heart auscultation revealed a regular rate and rhythm with no murmurs. The lungs were clear to auscultation bilaterally. The abdomen was soft and nontender without organomegaly. There was no pedal edema and no signs suggestive of deep vein thrombosis. Carotid pulses were normal bilaterally, and no bruits were heard. Radial, femoral, and distal pedal pulses were normal bilaterally. Neurologic examination revealed left hemiplegia, gaze deviation to the right, positive Babinski’s sign on the left, and normal reflexes bilaterally; the National Institutes of Health Stroke Scale (NIHSS) score was 15 at that point. Blood tests revealed a glucose level of 138 mg/dL, a BUN level of 15 mg/dL, a creatinine level of 0.95 mg/dL, and a white blood cell count of 14,410/μL. Blood coagulation tests were within normal limits. There was no evidence of pulmonary edema or mediastinal widening on chest x-ray. An electrocardiogram revealed normal sinus rhythm without ischemic features. Forty minutes after arriving in the ED (1 hour and 40 minutes after he had collapsed), the patient was examined by a consultant in neurology. Because of the clinical picture suggestive of stroke and a time interval of less than 3 hours from the onset of symptoms, the patient was considered for thrombolytic therapy. Head CT without contrast revealed no signs of ischemic infarction or brain hemorrhage. Immediately after the CT scan, there was spontaneous improvement in the patient’s condition. He looked more alert, although still suffering from dysarthria, and the left hemiplegia improved to hemiparesis with strength three of five (NIHSS score of 9). At that point, the neurologist decided to withhold thrombolytic therapy. The friend then recalled that during their walk, a few minutes before his collapse, the patient had complained of mild chest pain and slight breathlessness. The neurologist passed on this new information to the Internal Medicine resident who conducted a repeat physical examination. This now revealed the presence of bilaterally diminished pedal pulses. The new anamnestic detail, together with the new finding on physical examination, led the attending physicians to perform a CT scan of the chest with intravenous contrast. This revealed a Stanford type A dissection of the thoracic (Fig. 1a) and abdominal aorta with propagation and significant occlusion of the right external carotid artery (Fig. 1b). The dissection involved the superior mesenteric and left renal arteries. Mural thrombi were demonstrated in the left subclavian artery and the celiac trunk. Eight hours after the onset of symptoms, the patient was transferred to another hospital for emergency replacement of the aortic arch and repair of the aortic valve. He had a prolonged and complicated postoperative course but eventually recovered and was discharged to a rehabilitation center 49 days after his acute presentation. On follow-up 11 months post discharge, he was asymptomatic and without residual deficits.
Figure 1.
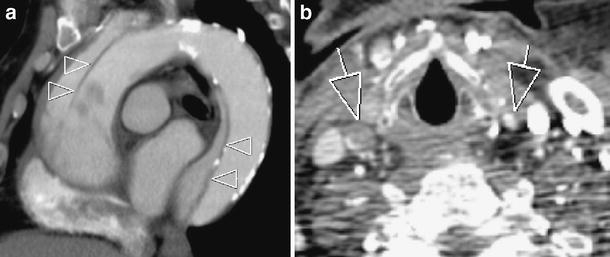
Post contrast sagital-oblique reformat (a) and axial (b) CT images of the present case. a CT image of type A aortic dissection with the intimal flap shown as an unopacified, partially calcified line within the aortic lumen (arrowheads), separating the true lumen from the false and extending from the ascending to the descending aorta. b An axial image at the level of the cricoid cartilage shows the two common carotid arteries (arrows). The left external carotid artery is fully opacified, whereas the right one shows only minimal rim enhancement as the dissection involves its origin
Discussion
Aortic dissection manifesting as cerebral infarction presents the clinician with a unique diagnostic problem in the era of thrombolysis. A Medline search of the English-language literature using the MeSH terms “dissecting aneurysm” and “thrombolytic therapy” or the terms “aortic dissection” and “thrombolysis” resulted in 6 reports of patients with acute aortic dissection presenting as ischemic cerebral infarction who were considered for thrombolytic therapy or inadvertently received such therapy (Table 1).7–12 Typical risk factors for ischemic infarction,13 including age and hypertension, were present in five of the six patients reported,7–11 as well as in the present case. Undoubtedly, the presence of these traditional risk factors made it difficult for the clinician to suspect the correct diagnosis in these cases.
Table 1.
Characteristics of Previously Reported Cases in which Patients were Considered for or Received TPA in the Setting of Acute Thoracic Aortic Dissection
| Ref. | Age/sex | Comorbidities | Source of medical history | Clue leading to diagnosis | TPA | Outcome |
|---|---|---|---|---|---|---|
| 7 | 72/F | Unknown | None | Chest x-ray revealing widened mediastinum | N | Dead |
| 8 | 54/M | Hypertension, smoker, diabetes mellitus | Wife | Thrombosed femoral artery 2 days after presentation | Y | Dead |
| 9 | 60/F | Hypertension, obesity | Husband | None antemortem | N | Dead |
| 10 | 64/M | Hypertension | Unknown, not patient | Report of hands grasping chest | N | Dead |
| Unequal blood pressure in left and right hands, nonpalpable unilateral pulses | ||||||
| 11 | 56/F | Hypertension | Patient | Chest pain as chief complaint | Y | Alive (GCS-3) |
| 12 | 44/M | Unremarkable | Patient | Back and flank pain after TPA administration | Y | Alive (residual hemiparesis) |
Basic clinical skills are invaluable in the scenario we describe. As in our presented case, no medical history could be elicited from the patients themselves in four of the six previously reported cases caused by decreased level of consciousness7 or aphasia.8–10 Because the most essential element in the diagnosis of acute aortic dissection is a high level of clinical suspicion and the most sensitive clue is the symptom of abrupt chest or abdominal pain, the inability of the patient to describe his symptoms is highly problematic.14 Clinical suspicion may also be aroused by the detection of a widened mediastinum on plain chest x-ray, but in up to 20% of cases the chest x-ray may be negative,15 as in the present case. Despite the lack of this important information, in four of seven cases including our presented case, valuable clues indicating the underlying diagnosis were to be found in a combination of collateral medical history, physical examination, and plain chest x-ray.7,10,11 Because the information regarding chest pain was elicited by chance in the current case, it would seem worthwhile to include direct questioning regarding that point for every patient presenting with symptoms of cerebral infarction.
Furthermore, as pulse deficits are present in only 20–30% of cases of acute aortic dissection and may well be only transient, the present case emphasizes the importance of serial physical examinations, which contributed substantially to the correct diagnosis.14 It should be noted that a comparison of blood pressure measurements in both arms was not conducted. This simple test might have led to an earlier diagnosis.
The favorable outcome in the present case is remarkable. Acute dissection of the ascending aorta is highly lethal with a cumulative mortality rate of 1% to 2% per hour early after the onset of symptoms. With medical management alone, the mortality rate peaks at nearly 20% and 50% after 24 hours and 1 month, respectively.16 This grim prognosis is well-demonstrated in the cases reported previously (Table 1); in two of three cases, the administration of TPA may have contributed to the poor outcome. Even after surgical treatment of acute type A aortic dissection, outcome has previously been reported to be poor.16 However, a recent larger, multicenter study has reported excellent 1- and 3-year survival rates of 96.1 ± 2.4% and 90.5 ± 3.9%, respectively.17 These figures, together with the present case, emphasize the importance of the early recognition and management of similar cases.
The present case also demonstrates the need for close cooperation between attending physicians and the sharing of information. The unfolding of events described in our report led to the correct diagnosis, the institution of the required life-saving procedures, and a favorable outcome.
In summary, a diagnosis of aortic dissection should be considered in any patient presenting with a clinical picture of ischemic stroke, especially when considering thrombolysis. It would obviously be incorrect and impractical to perform the diagnostic tests required to rule out aortic dissection in every such patient. Nevertheless, data from our case and those previously published suggest that basic clinical skills such as taking a full medical history, conducting a thorough physical examination, using simple diagnostic aids, maintaining a high level of clinical suspicion, and performing reevaluation in dynamic cases may disclose a considerable number of patients with this underlying diagnosis. In cases such as those reviewed here, a timely diagnosis may be life-saving.
Acknowledgements
We thank Israel Potasman, MD, whose mentoring was invaluable for the preparation of the manuscript and Richard Lincoln for proofreading of the manuscript.
Conflict of Interest None disclosed.
References
- 1.De Sanctis RW, Doroghazi RM, Austen WG, Buckley MJ. Aortic dissection. N Engl J Med. 1987;317:1060–67. [DOI] [PubMed]
- 2.Gerber O, Heyer EJ, Vieux U. Painless dissections of the aorta presenting as acute neurologic syndromes. Stroke. 1986;17:644–47. [DOI] [PubMed]
- 3.DeBakey ME, McCollum CH, Crawford ES, et al. Dissection and dissecting aneurysms of the aorta: twenty years follow-up of 527 patients treated surgically. Surgery. 1982;92:1118–34. [PubMed]
- 4.Khan IA, Nair CK. Clinical, diagnostic, and management perspectives of aortic dissection. Chest. 2002;122:311–28. [DOI] [PubMed]
- 5.The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–87. [DOI] [PubMed]
- 6.Kamp TJ, Golschmidt-Clermont PJ, Brinker JA, Resar JR. Myocardial infarction, aortic dissection, and thrombolytic therapy. Am Heart J. 1994;128:1234–37. [DOI] [PubMed]
- 7.Flemming KD, Brown RD Jr. Acute cerebral infarction caused by aortic dissection: caution in the thrombolytic era. Stroke. 1999;30:477–8. [DOI] [PubMed]
- 8.Fessler AJ, Alberts MJ. Stroke treatment with tissue plasminogen activator in the setting of aortic dissection. Neurology. 2000;54:1010. [DOI] [PubMed]
- 9.Villa A, Molgora M, Licari S, Omboni E. Acute ischemic stroke, aortic dissection, and thrombolytic therapy. Am J Emerg Med. 2003;21:159–60. [DOI] [PubMed]
- 10.Wright V, Horvath R, Baird AE. Aortic dissection presenting as acute ischemic stroke. Neurology. 2003;61:581–2. [DOI] [PubMed]
- 11.Uchino K, Estrera A, Calleja S, Alexandrov AV, Garami Z. Aortic dissection presenting as an acute ischemic stroke for thrombolysis. J Neuroimaging. 2005;15:281–3. [DOI] [PubMed]
- 12.Chua CH, Lien LM, Lin CH, Hung CR. Emergency surgical intervention in a patient with delayed diagnosis of aortic dissection presenting with acute ischemic stroke and undergoing thrombolytic therapy. J Thorac Cardiovasc Surg. 2005;130:1222–4. [DOI] [PubMed]
- 13.Elkind MS, Sacco RL. Stroke risk factors and stroke prevention. Semin Neurol. 1998;18:429–40. [DOI] [PubMed]
- 14.Nienaber CA, Eagle KA. Aortic dissection: new frontiers in diagnosis and management: Part I: from etiology to diagnostic strategies. Circulation. 2003;108:628–35. [DOI] [PubMed]
- 15.Earnest F 4th, Muhm JR, Sheedy PF 2nd. Roentgenographic findings in thoracic aortic dissection. Mayo Clin Proc. 1979;54:43–50. [PubMed]
- 16.Nienaber CA, Eagle KA. Aortic dissection: new frontiers in diagnosis and management: Part II: therapeutic management and follow-up. Circulation. 2003;108:772–8. [DOI] [PubMed]
- 17.Tsai TT, Evangelista A, Nienaber CA, et al. Long-term survival in patients presenting with type A acute aortic dissection: insights from the International Registry of Acute Aortic Dissection (IRAD). Circulation. 2006;114(1 Suppl):I350–6. [DOI] [PubMed]


