Abstract
BACKGROUND
Nonadherence to prescription drugs results in poorer control of chronic health conditions. Because of significant racial/ethnic disparities in the control of many chronic diseases, differences in the rates of and reasons for medication nonadherence should be studied.
OBJECTIVES
1) To determine whether rates of and reasons for medication nonadherence vary by race/ethnicity among seniors; and 2) to evaluate whether any association between race/ethnicity and nonadherence is moderated by prescription coverage and income.
DESIGN/SETTING
Cross-sectional national survey, 2003.
PATIENTS
Medicare beneficiaries ≥65 years of age, who reported their race/ethnicity as white, black, or Hispanic, and who reported taking at least 1 medication (n = 14,829).
MAIN OUTCOME MEASURES
Self-reported nonadherence (caused by cost, self-assessed need, or experiences/side effects) during the last 12 months.
RESULTS
Blacks and Hispanics were more likely than whites to report cost-related nonadherence (35.1%, 36.5%, and 26.7%, respectively, p < .001). There were no racial/ethnic differences in nonadherence caused by experiences or self-assessed need. In analyses controlling for age, gender, number of chronic conditions and medications, education, and presence and type of prescription drug coverage, blacks (odds ratio [OR] 1.38; 95% confidence interval [CI] 1.08–1.78) and Hispanics (1.35; 1.02–1.78) remained more likely to report cost-related nonadherence compared to whites. When income was added to the model, the relationship between cost-related nonadherence and race/ethnicity was no longer statistically significant (p = .12).
CONCLUSIONS
Racial/ethnic disparities in medication nonadherence exist among seniors, and are related to cost concerns, and not to differences in experiences or self-assessed need. Considering the importance of medication adherence in controlling chronic diseases, affordability of prescriptions should be explicitly addressed to reduce racial/ethnic disparities.
KEY WORDS: medication adherence, drug therapy/economics, health disparities
INTRODUCTION
Prescription drug coverage for seniors remains an issue at the center of public discussion in health care. The start of the Medicare Part D prescription benefit in January 1, 2006 brought the hope that seniors, more than ever, would have fewer financial barriers to prescription drugs. Whereas access to affordable clinical care and prescription coverage are essential, prescription drugs are only useful if they are taken. In 2003, a national survey of Medicare beneficiaries found that 40% of seniors reported some form of medication nonadherence.1 Vulnerable seniors, who either had no prescription coverage, low incomes, or high disease burden, had even higher rates of nonadherence.1,2
Prior work on medication adherence has focused on cost-related adherence and has shown, for the most part, an association between increased cost-sharing and out-of-pocket costs, and decreased adherence to medications.3–9 Several studies have linked this cost-related restriction of medication use to adverse events and decreased health status.10–15
The connection between medication adherence and control of chronic diseases is particularly relevant to racial/ethnic minorities. Disparities in the management and outcomes of chronic diseases between whites and racial/ethnic minorities are well documented; blacks are more likely to die from heart disease than any other U.S. racial/ethnic group, and Hispanic Americans are reported to have twice the mortality from diabetes as whites.16 There are continuing racial (white vs black) disparities in glucose control among patients with diabetes, and in cholesterol control among patients with cardiovascular disease.17 It is not entirely clear what role medication adherence might play in health disparities, and whether adherence could be a target for intervention. Prior observational research in diabetes has shown a relationship between medication nonadherence and poor outcomes in racial/ethnic minorities.18
Data on the relationship between medication adherence and race/ethnicity is mixed, and again focuses almost exclusively on nonadherence because of cost.2,8,19–22 In a review of the topic of adherence to medication, Osterberg and Blaschke write that race has not been consistently associated with levels of adherence.23 Whether the new Medicare Part D drug benefit will be effective in improving adherence and addressing racial/ethnic disparities in chronic disease remains to be seen. Clarifying current rates of medication adherence and disparity is an important first step.
We report here on a national survey of seniors in 2003, which focused on prescription use and adherence, and evaluated both cost-related and noncost-related prescription nonadherence. We aimed to answer the following questions: 1) Does adherence to medications vary by race/ethnicity among seniors, and if so, 2) Do the types of nonadherence vary as well, specifically looking at nonadherence caused by cost, nonadherence as a result of experiences, and nonadherence caused by self-assessed need, and finally, 3) What effect do prescription drug coverage and income have on any association between race/ethnicity and nonadherence?
METHODS
Study Sample and Design
The study sample was obtained from a 2003 national survey of seniors, administered by the Health Institute at Tufts-New England Medical Center. Details of the survey instrument and survey protocol have been published elsewhere.1,24 The Centers for Medicare and Medicaid Services (CMS) provided a 1% probability sample of noninstitutionalized Medicare beneficiaries aged 65 or older from each state and the District of Columbia. Medicaid enrollees and seniors residing in low-income neighborhoods were oversampled. A random sample of 36,901 Medicare beneficiaries was drawn in 2003. The survey was administered in English and Spanish by mail, with follow up of nonrespondents by telephone, between July 15 and October 7, 2003. After accounting for beneficiaries excluded as a result of death, institutionalization, relocation, non-English/Spanish language, or severe cognitive or physical impairment, the response rate was 51% (n = 17,569). Nonrespondents were slightly older, and disproportionately of minority race/ethnicity and lower socioeconomic status.1 For this analysis, we included individuals who self-identified as white, black, or Hispanic, and reported taking at least 1 prescription medicine over the past year (n = 14,829).
Questionnaire
The study questionnaire focused on current prescription drug coverage, use, and spending, and included questions on health status, income, and other sociodemographic characteristics, drawing from instruments that have been extensively tested and validated.1,2,24 Both cognitive testing and extensive psychometric testing of the survey items and composite measures support the reliability and validity of the information it yields. In particular, the measures of nonadherence, which are the focus of these analyses, are supported by both face validity and by considerable evidence of criterion validity across several studies.1,2,24 For example, rates of cost-related nonadherence are higher among those in whom it would be expected based on theory and prior evidence (e.g., low income, prescription coverage absent or limited), whereas rates of the other (non-economic) forms of nonadherence (e.g., because of experiences and of self-assessed need), are not associated with income, coverage, or other economic variables.1,2,24
Nonadherence The survey included a series of questions concerning nonadherence to prescription regimens, and included questions on cost-related nonadherence that have subsequently been incorporated into the Medicare Current Beneficiary Survey (MCBS).1,2 All adherence questions referenced experiences over the past 12 months. Factor analysis confirmed the conceptual model of 3 types of nonadherence, based on the individual survey questions: (1) cost-related nonadherence, (2) nonadherence because of medication experiences (e.g., side effects); and (3) nonadherence because of self-assessed need for particular medications. A summary indicator of “any nonadherence” was defined to denote nonadherence in 1 or more of these areas.Cost-related nonadherence was evaluated with questions about the following 3 behaviors: (1) not filling a prescription because of cost, (2) skipping doses to make a prescription last longer, and (3) taking smaller doses than prescribed to make a prescription last longer. The Cronbach’s alpha for cost-related nonadherence was 0.69. Respondents who reported using a prescription medicine for 1 or more named chronic conditions also indicated whether they had failed to fill any of these because of cost. Respondents also reported whether they had spent less on “food, heat or other basic needs” over the past 12 months to afford their prescriptions.Experience-related nonadherence was assessed by asking whether the respondent had skipped doses or stopped taking a medicine because: (1) it was making them feel worse; and/or (2) they did not think the medicine was helping them. Nonadherence because of self-assessed need was assessed by asking whether respondents had failed to fill a prescription because: (1) they felt they were taking too many medicines; and/or (2) they did not think they needed the medicine. There was overlap among the different causes of nonadherence, such that an individual could answer yes to more than 1 reason. The Cronbach’s alpha for nonadherence because of experiences and self-assessed need were 0.74 and 0.72, respectively.
Covariates
Covariates for analysis included the presence and type of prescription coverage (Medicaid, employer, other private/HMO, state, other public, none), age, gender, the number of self-reported chronic conditions (including hypertension, myocardial infarction, congestive heart failure, asthma or COPD, diabetes, rheumatoid arthritis or osteoarthritis, cancer, and depression), number of medications (1–2, 3–4, or more than 5), education (less than high school, high school, at least 1 year of college), and income (poor, near-poor, non-poor).
Prescription Coverage For beneficiaries reporting more than 1 source of prescription coverage, a primary coverage source was assigned based on the following hierarchy: Medicaid, employer-sponsored, HMO, Medigap, state prescription program, Veteran’s Administration/Department of Defense, and others. In this hierarchy, the leading sources of prescription coverage supercede more minor sources, and sources offering more comprehensive coverage supercede those offering less.1 For individuals with multiple drug coverage sources, this approach attributes their experiences and out-of-pocket costs to the source that has the largest influence. Beneficiaries whom CMS indicated to have full Medicaid coverage were classified as having Medicaid prescription coverage (n = 2,657), even if the individual did not self-report Medicaid (n = 564).
Poverty Using the 2003 federal poverty thresholds ($8,988 single; $12,120 married), together with self-reported income and marital status, we classified seniors as poor (≤100% poverty), near-poor (101–200% poverty) or non-poor (>200% poverty). For approximately 10% of respondents with missing income data, income was imputed based on Buck’s Method, which puts respondents into the single most likely category, which has an advantage for ease of understanding over other imputation methods that may classify respondents into multiple categories based on a probability distribution.25
Data Analysis
The analytic sample excluded those who did not take any medicine (n = 2,037) or were classified as Asian, Native Hawaiian/Pacific Islander, American Indian/Native Alaskan, or other race/ ethnicity (n = 615) as well as missing race/ ethnicity (n = 93). Data analysis was cross-sectional, and focused on 2 issues: 1) comparing the frequencies of each of the causes of nonadherence among the racial/ ethnic groups using Chi-Square tests, and 2) using multivariate logistic regression to model the relationship between nonadherence caused by cost and race/ethnicity (comparing those who were nonadherent because of cost with those who were not), accounting for other variables that we hypothesized might confound the relationship between race/ethnicity and nonadherence. Regression using the same covariates was also performed for those types of adherence for which there were no racial/ethnic differences, adding nonadherence caused by cost as a covariate. The analytic sample included all respondents, using dummy variables to account for missing data, and had 99% power at the p = .05 significance level to detect a 5% difference in adherence rates for blacks compared to whites, and 81% power for Hispanics. Probability sampling weights were applied to all analyses to correct for unequal sampling probabilities across states and strata. Analyses were carried out using SAS version 9.1 and SUDAAN version 9.0.
The funding source for this paper played no role in this analysis, although the original funding source for the 2003 survey on which these analyses are based did participate in the design of the original survey.
RESULTS
Description of the Sample
The analytic sample included 14,829 seniors, 10.8% of whom self-identified as black, and 6.2% of whom were Hispanic (Table 1). The racial/ethnic groups were similar in their number of chronic conditions and number of medications. Whites were slightly older than the other groups, and had higher income and education levels, and more private and employer-sponsored insurance (p < .001).
Table 1.
Description of the Sample
| N = 14,829 | White (n = 12,313) | Black (n = 1,603) | Hispanic (n = 913) |
|---|---|---|---|
| Age, mean (range) * | 75.1 (65–109) | 74.2 (65–101) | 73.2 (65–100) |
| Median number of chronic conditions (range) | 2 (0–8) | 2 (0–7) | 2 (0–8) |
| Gender * | |||
| Female | 58.9% | 68.4% | 59.6% |
| Number of current prescription medications: | |||
| 1–2 | 25.5% | 26.1% | 23.1% |
| 3–4 | 28.5 | 27.6 | 28.3 |
| 5+ | 46.1 | 46.3 | 48.6 |
| Education: * | |||
| Less than high school | 22.7% | 46.0% | 58.8% |
| High school | 37.2 | 28.9 | 23.4 |
| Some/All college | 40.0 | 25.1 | 17.8 |
| Income:* | |||
| <100% FPL | 9.7% | 34.7% | 35.9% |
| 101–200% FPL | 27.4 | 26.3 | 36.9 |
| >200% FPL | 62.9 | 39.0 | 27.2 |
| Insurance coverage:* | |||
| Medicaid | 4.7% | 22.8% | 28.3% |
| Employer | 31.7 | 21.9 | 18.6 |
| Other private/ HMO | 30.5 | 22.4 | 28.4 |
| State | 2.5 | 2.7 | 1.0 |
| Other public | 7.0 | 6.2 | 3.4 |
| None | 23.6 | 24.0 | 20.4 |
Frequencies shown are weighted. Data for education was missing on 668 respondents, and missing for number of medications on 305 respondents.
*The differences between racial/ ethnic groups are statistically significant (p < .001).
Rates of Nonadherence
Overall, 41.6% of the sample reported 1 or more forms of nonadherence. The rates of nonadherence differed significantly among the racial/ethnic groups, with blacks (45.3%) and Hispanics (48.8%) reporting higher rates of nonadherence than whites (41.1%) (p = .017) (Table 2). Blacks and Hispanics were significantly more likely to report nonadherence because of cost for every measure of cost-related nonadherence. For example, 24.0% of blacks reported skipping doses to make prescription last longer, compared to 19.9% of Hispanics, and 16.2% of whites (p = .003). Blacks and Hispanics were also significantly more likely to report spending less on food, heat, or other basic needs to afford their prescription (p < .001).
Table 2.
Rates of Nonadherence because of Cost, Experiences, and Self-Assessed Need
| Any nonadherence | Total | White | Black | Hispanic | P value |
|---|---|---|---|---|---|
| 41.6 % | 41.1 % | 45.3 % | 48.8 % | .017* | |
| Nonadherence because of cost | 27.6 | 26.7 | 35.1 | 36.5 | <.001* |
| Did not fill prescription because of cost | |||||
| One or more times | 19.0 | 18.3 | 26.1 | 27.2 | .0001* |
| Three or more times | 5.9 | 5.5 | 10.6 | 9.3 | .001* |
| Skipped doses to make prescription last longer | 16.8 | 16.2 | 24.0 | 19.9 | .003* |
| Took smaller doses to make Rx last longer | 13.3 | 13.0 | 15.1 | 18.1 | .089 |
| Spent less on food, heat, or other basic needs to afford prescription† | 12.6 | 11.3 | 26.6 | 23.9 | <.001* |
| Nonadherence because of experiences | 25.3 | 25.4 | 23.4 | 24.9 | .673 |
| Skipped doses or stopped prescription because it was making feel worse | 19.3 | 19.3 | 18.0 | 20.9 | .618 |
| Skipped dose or stopped prescription because did not think it was helping | 18.3 | 18.4 | 15.9 | 18.3 | .386 |
| Nonadherence because of self-assessed need | 14.8 | 14.7 | 15.8 | 16.3 | .713 |
| Did not fill prescription because did not think needed the medicine | 12.5 | 12.5 | 13.0 | 13.5 | .875 |
| Did not fill prescription because felt were taking too many medicines | 9.2 | 9.1 | 9.8 | 10.7 | .608 |
* Indicates statistical significance at level indicated
†Related to prescription affordability, although not a specific measure of nonadherence because of cost
Rates of reported nonadherence because of experiences, and nonadherence because of self-assessed need did not differ by race/ethnicity. Nonadherence because of experiences was reported by one-quarter of the seniors, whereas nonadherence because of self-assessed need was reported by almost 15% of the sample.
Types of Nonadherence
To illustrate the relationship between race/ethnicity and the specific types of nonadherence, the subsample of seniors who reported at least 1 form of nonadherence was further examined (Fig. 1). Among respondents who reported any nonadherence, there was a significant relationship between race/ethnicity and the type of nonadherence reported (P < .001). Of those respondents who reported some form of medication nonadherence, blacks and Hispanics were more likely to report cost as the only reason for nonadherence, compared to whites (38.9%, 41.4%, and 28.4%, respectively). Conversely, blacks and Hispanics who were nonadherent were less likely to be nonadherent only because of experiences compared to whites.
Figure 1.
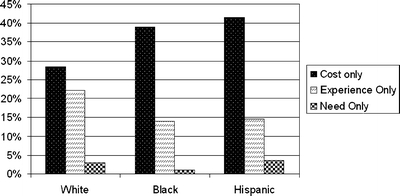
Rates of nonadherence as a result of one cause only among the sample of patients who were nonadherent (n = 6,196)
Multivariate Analysis
Blacks had 1.48 times the odds of reporting cost-related nonadherence (95% CI 1.19, 1.86) compared to Whites, and Hispanics had an odds ratio of 1.58 (95% CI 1.22, 2.04), in unadjusted analysis. Table 3 shows the results of this bivariate regression, and the 2 subsequent models. In models controlling for age, gender, number of chronic conditions and medications, presence and type of prescription drug coverage, and education, race/ethnicity remained a significant predictor of nonadherence caused by cost with the odds of cost-related nonadherence 1.38 times higher among blacks compared to Whites (95% CI 1.08,1.78), and 1.35 times higher in Hispanics (95% CI 1.02, 1.78). When income was added to model, race/ethnicity was no longer a significant predictor of nonadherence caused by cost. Table 4 shows the odds ratios from this fully adjusted multivariate model.
Table 3.
Effect of Race/Ethnicity on Nonadherence because of Cost, From Multivariate Logistic Regressions
| Variables in model | Blacks | Hispanic | P value |
|---|---|---|---|
| Odds Ratio (95% confidence interval) | Odds Ratio (95% confidence interval) | ||
| Race/Ethnicity | 1.48 (1.19,1.86) | 1.58 (1.22,2.04) | <.0001 |
| Race/Ethnicity, age, gender, number of prescriptions, number of chronic conditions, drug coverage, education | 1.38 (1.08,1.78) | 1.35 (1.02,1.78) | .009 |
| Race/Ethnicity, age, gender, number of prescriptions, number of chronic conditions, drug coverage, education, income | 1.28 (0.99,1.66) | 1.19 (0.90,1.56) | .12 |
Three models are shown, starting with univariate relationship between adherence and race/ethnicity, then adding covariates except for income, and finally adding income. Odds ratios are reported for blacks and Hispanics compared to whites. P values shown are for race/ethnicity as a categorical predictor.
Table 4.
Results of Fully Adjusted Multivariate Logistic Regression, Modeling Nonadherence because of Cost
| Variable | Odds Ratio (95% confidence interval) | P value |
|---|---|---|
| Race/Ethnicity | .12 | |
| White | Reference | |
| Black | 1.28 (0.99,1.66) | |
| Hispanic | 1.19 (0.90,1.56) | |
| Age (continuous) | 0.96 (0.95,0.97) | <.001 |
| Gender | .34 | |
| Female | 0.93 (0.80,1.08) | |
| Number of prescriptions | <.001 | |
| 1–2 | Reference | |
| 3–4 | 1.23 (1.01,1.50) | |
| 5+ | 1.58 (1.29, 1.93) | |
| Number of chronic conditions (continuous) | 1.20 (1.14,1.27) | <.001 |
| Prescription drug coverage | <.001 | |
| Medicaid | 0.28 (0.21,0.36) | |
| Employer | 0.25 (0.21,0.31) | |
| Private/HMO | 0.59 (0.49,0.71) | |
| State | 0.74 (0.49, 1.11) | |
| Other public | 0.22 (0.15, 0.32) | |
| None | Reference | |
| Education | .89 | |
| Less than high school | Reference | |
| High school | 1.02 (0.85,1.22) | |
| At least 1 year of college | 1.06 (0.87,1.30) | |
| Income | <.001 | |
| ≤100% FPL | 2.26 (1.81,2.83) | |
| 100–200% FPL | 1.86 (1.57, 2.20) | |
| >200%FPL | Reference |
*Model goodness of fit assessed using the Satterthwaite adjusted F test, with a p value of 0.27.
There continued to be no racial/ethnic differences in nonadherence caused by experiences (p = .30) and nonadherence because of self-assessed need (p = .95) in the fully adjusted models using similar covariates as above. However, when the presence of nonadherence because of cost was added as a covariate, Blacks were less likely to be nonadherent as a result of experiences compared to whites (odds ratio 0.74, 95% CI 0.57–0.96), and Hispanic ethnicity remained nonsignificant (OR 0.82, 95% CI 0.62, 1.09).
DISCUSSION
This study of racial and ethnic differences in medication adherence among seniors holds important insights relevant to clinicians, and to those responsible for the continued implementation of the Medicare Part D drug benefit. This national survey suggests that racial/ethnic disparities in nonadherence to medications exist and are largely related to cost concerns, and not to self-assessed need or differences in experiences with medications. The racial/ethnic disparities in adherence are worthy of concern, considering the importance of medication adherence in controlling chronic diseases, and the known disparities in outcomes from chronic disease by race/ethnicity. Our data suggest that 1 key target of intervention to address racial/ ethnic disparities might be reducing cost barriers to medication adherence.
The disparity in cost-related nonadherence persisted even when accounting for the presence and type of drug coverage. However, a significant portion of the effect of race/ethnicity was explained by income. This finding suggests that the provision of prescription coverage alone may not be enough to address these disparities. Patients’ ability to pay is paramount, and copayments, deductibles, benefit caps, and drug prices all need to be addressed. The fact that about 1 in 4 black and Hispanic seniors reported spending less on food, heat, or other basic needs to afford their prescriptions (and 1 in 9 whites), should be a stark reminder that the issue of prescription affordability should be a priority for policy makers, and for health care providers managing chronic health conditions. Prior research has shown that approximately one-third of seniors who have cost-related nonadherence do not discuss their problems with medication cost with their clinicians.26,27
The effect of the Medicare Part D drug benefit on cost-related nonadherence will not be known for some time. The benefit provides generous subsidies to low-income seniors who enroll in the subsidy program and choose a part D plan. This almost certainly will address the affordability of drugs in the context of insurance coverage and may help to address the disparities in cost-related nonadherence. However, only about half of low-income subsidy-eligible seniors who are not dually enrolled in Medicaid have signed up for these subsidies according to 1 report, with approximately 3.3 million eligible beneficiaries who are not receiving this important assistance.28 The racial/ethnic and sociodemographic characteristics of these low-income seniors who are not receiving subsidies are not known. Most seniors will not be eligible for low-income subsidies, and there are a number of “near-poor” seniors who, despite saving by joining the Part D plans, will still have significant out-of-pocket costs.29 A recent survey of enrollment status in Part D plans shows that of those with household yearly income less than $20,000, 12.4% will have no creditable prescription coverage and are not enrolled in any drug plans.30
Our overall rates of cost-related nonadherence are similar to other recent reports.1,20,31 Soumerai et al.2 recently reported on data from the 2004 Medicare Current Beneficiary Survey, showing a 13% rate of cost-related nonadherence among the elderly. The incorporation of the measures of cost-related nonadherence used in this survey into MCBS lends strength to their validity. The lower rate observed in this MCBS study may in part reflect the fact that 8% of their study sample took no medications, and 1 of the questions relating to cost-related nonadherence was asked only of respondents who reported not obtaining 1 or more of their prescribed medications during the year. Older studies have found slightly lower rates of cost-related nonadherence among seniors, although they tend to ask only 1 question on the topic, rather than a group of questions, which may explain the lower rates.12,19,21
Of note, the paper by Soumerai and colleagues found that black race was an independent predictor of cost-related nonadherence, after adjusting for confounders including income. Whereas that study was not carried out to look at racial differences, and no information is available in the final analysis for Hispanics, the somewhat conflicting reports add to the ongoing discussion on the important topic. Previous research on the association between adherence and race/ethnicity is mixed: some studies have found no significant differences, both adjusted and unadjusted, by race/ethnicity in cost-related medication skipping.8,19,20 There are other reports, however, including both surveys and claims-based studies, that do identify race/ethnicity as an independent predictor for nonadherence among elderly patients.2,21,22 The strengths of our analysis include its large sample size and adequate power, recent data source, and our ability to specifically examine Hispanic ethnicity and move beyond the white versus nonwhite paradigm, which many prior studies in medication adherence have used.
Also important is our juxtaposition of noncost-related nonadherence, which provides an important insight into other reasons for nonadherence that are significant and important but do not appear to be a large contributor to health disparities. Rates of nonadherence as a result of experiences and self-assessed need have not previously been extensively studied. There do not seem to be any racial/ethnic differences among seniors in the self-reported rates of stopping medications because they experience side effects, or felt they did not need the medicine, or felt they were taking too many medicines. The lack of differences here points to the fact that there are no inherent effects of race/ethnicity on nonadherence, but it is the practical barriers of income and cost that are the real drivers of the disparity. In fact, the black race was a predictor of being less nonadherent because of experiences, once cost-related nonadherence was accounted for. Whereas racial/ethnic disparities may not exist in these measures of nonadherence, the rates are not insignificant. Almost 1 in 5 seniors reported skipping doses or stopping their prescription because it was making them feel worse; 14.9% of seniors reported not filling a prescription either because they did not think they needed the medicine, or because they felt they were taking too many medicines. Clinicians should be aware of these barriers to medication use, which seem to affect seniors regardless of race or ethnicity, which have important relevance for patient safety, and which may be addressed in part by better communication between provider and patient.32,33
Limitations
The results of this study must be interpreted in the context of the study design. First, the survey achieved only a modest response rate, and we were not able to examine other reasons for nonadherence, such as poor literacy, and forgetfulness, because these questions were not included in the survey, and we were also not able to specify what medications were being skipped. Nonetheless, the questions asked in the survey are important and clinically relevant, and the cost-related nonadherence questions have been subsequently included in the Medicare Current Beneficiary Survey (MCBS). Note that we were also not able to examine other ethnic groups included in the survey, such as Asians or Native Hawaiian/Pacific Islanders, because of a more limited sample size. Second, the study is cross-sectional, and cannot directly address how to reduce nonadherence. However, these results suggest that coverage may attenuate disparities in adherence, but that income differentials will remain a driver of disparities. Finally, whereas data shown are self-reported, questionnaires using self-reported adherence have strong concordance with other nonself-reported measures of medication adherence.34
Conclusion
Racial/ethnic disparities in nonadherence to medications exist among seniors and are related to cost concerns, and not to self-assessed need or differences in experiences. Prescription coverage alone that does not effectively control out-of-pocket costs or deductibles for patients, is not likely to be sufficient in addressing these disparities. Reducing racial/ethnic disparities in chronic diseases requires that prescription affordability issues be explicitly and aggressively addressed, both in the clinic and in health policy, especially for the poor. This is particularly important as efforts are made to continue to encourage low-income Medicare beneficiaries to sign up for subsidies for the new drug benefit and decisions are made about cost-sharing for future years.
Acknowledgements
Preparation and production of this manuscript was supported by a National Research Service Award (T32HP11001-18). The design and conduct of the 2003 survey on which these analyses are based was supported by funding from the Commonwealth Fund and the Henry J. Kaiser Family Foundation (KFF) under the direction of Dr. Safran at Tufts-New England Medical Center. Dr. Safran and her team gratefully acknowledge the technical expertise and support provided by Lawrence (Spike) Duzor, Dural Suite, Robyn Thomas of the Centers for Medicare and Medicaid Services (CMS), and Kelly Merriman of ResDAC, without whom the conduct of the survey would not have been possible; and Tricia Neuman and Michelle Kitchman (KFF) and Cathy Schoen (Commonwealth Fund), whose partnership contributed immeasurably to the richness of the survey content and study design. The contents of this paper are the sole responsibility of the authors and do not necessarily represent the views of the Harvard Medical School, Brigham and Women’s Hospital, Tufts-New England Medical Center, or Tufts Medical School.
Conflict of Interest None disclosed.
References
- 1.Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: findings from a 2003 national survey. Health Aff (Millwood) 2005; Suppl Web Exclusives: W5-152-W155-166. [DOI] [PubMed]
- 2.Soumerai SB, Pierre-Jacques M, Zhang F, et al. Cost-related medication nonadherence among elderly and disabled Medicare beneficiaries: a national survey 1 year before the Medicare drug benefit. Arch Intern Med. 2006;166(17):1829–35. [DOI] [PubMed]
- 3.Tseng CW, Brook RH, Keeler E, Steers WN, Mangione CM. Cost-lowering strategies used by Medicare beneficiaries who exceed drug benefit caps and have a gap in drug coverage. JAMA. 2004;292(8):952–60. [DOI] [PubMed]
- 4.Gibson TB, Ozminkowski RJ, Goetzel RZ. The effects of prescription drug cost sharing: a review of the evidence. Am J Manag Care. 2005;11(11):730–40. [PubMed]
- 5.Gibson TB, Mark TL, McGuigan KA, Axelsen K, Wang S. The effects of prescription drug copayments on statin adherence. Am J Manag Care. 2006;12(9):509–17. [PubMed]
- 6.Goldman DP, Joyce GF, Escarce JJ, et al. Pharmacy benefits and the use of drugs by the chronically ill. JAMA. 2004;291(19):2344–50. [DOI] [PubMed]
- 7.Adams AS, Soumerai SB, Ross-Degnan D. The case for a Medicare drug coverage benefit: a critical review of the empirical evidence. Annu Rev Public Health. 2001;22:49–61. [DOI] [PubMed]
- 8.Piette JD, Heisler M, Wagner TH. Problems paying out-of-pocket medication costs among older adults with diabetes. Diabetes Care. 2004;27(2):384–91. [DOI] [PubMed]
- 9.Piette JD, Wagner TH, Potter MB, Schillinger D. Health insurance status, cost-related medication underuse, and outcomes among diabetes patients in three systems of care. Med Care. 2004;42(2):102–9. [DOI] [PubMed]
- 10.Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001;285(4):421–9. [DOI] [PubMed]
- 11.Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The health effects of restricting prescription medication use because of cost. Med Care. 2004;42(7):626–34. [DOI] [PubMed]
- 12.Mojtabai R. Medication Costs, Adherence, and Health Outcomes Among Medicare Beneficiaries. Health Aff (Millwood). 2003;22(4):220–9. [DOI] [PubMed]
- 13.Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166(17):1836–41. [DOI] [PubMed]
- 14.Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298(1):61–9. [DOI] [PMC free article] [PubMed]
- 15.Hsu J, Price M, Huang J, et al. Unintended consequences of caps on Medicare drug benefits. N Engl J Med. 2006;354(22):2349–59. [DOI] [PubMed]
- 16.Smedley BD, Stith AY, Nelson AR, eds. Unequal treatment: confronting racial and ethnic disparities in health care. Washington, D.C.: National Academy Press; 2003. [PubMed]
- 17.Trivedi AN, Zaslavsky AM, Schneider EC, Ayanian JZ. Trends in the quality of care and racial disparities in Medicare managed care. N Engl J Med. 2005;353(7):692–700. [DOI] [PubMed]
- 18.Schectman JM, Nadkarni MM, Voss JD. The association between diabetes metabolic control and drug adherence in an indigent population. Diabetes Care. 2002;25(6):1015–21. [DOI] [PubMed]
- 19.Wilson IB, Rogers WH, Chang H, Safran DG. Cost-related skipping of medications and other treatments among Medicare beneficiaries between 1998 and 2000. Results of a national study. J Gen Intern Med. 2005;20(8):715–20. [DOI] [PMC free article] [PubMed]
- 20.Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically ill adults: the treatments people forgo, how often, and who is at risk. Am J Public Health. 2004;94(10):1782–7. [DOI] [PMC free article] [PubMed]
- 21.Steinman MA, Sands LP, Covinsky KE. Self-restriction of medications due to cost in seniors without prescription coverage. J Gen Intern Med. 2001;16(12):793–9. [DOI] [PMC free article] [PubMed]
- 22.Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Levin R, Avorn J. Compliance with antihypertensive therapy among elderly Medicaid enrollees: the roles of age, gender, and race. Am J Public Health. 1996;86(12):1805–8. [DOI] [PMC free article] [PubMed]
- 23.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(5):487–97. [DOI] [PubMed]
- 24.Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: how well are states closing the gap? Health Aff (Millwood). 2002;Suppl Web Exclusives:W253–68. [DOI] [PubMed]
- 25.Buck SF. A method of estimation of missing values in multivariate data suitable for use with an electronic computer. J R Stat Soc. 1960;B22:302–6.
- 26.Piette JD, Heisler M, Wagner TH. Cost-related medication underuse: do patients with chronic illnesses tell their doctors? Arch Intern Med. 2004;164(16):1749–55. [DOI] [PubMed]
- 27.Wilson IB, Schoen C, Neuman P, et al. Physician–patient communication about prescription medication nonadherence: a 50-state study of America’s seniors. J Gen Intern Med. 2007;22(1):6–12. [DOI] [PMC free article] [PubMed]
- 28.Prescription Drug Coverage Among Medicare Beneficiaries. Menlo Park, CA: The Henry J. Kaiser Family Foundation; June 2006.
- 29.Gellad WF, Huskamp HA, Phillips KA, Haas JS. How the new Medicare drug benefit could affect vulnerable populations. Health Aff (Millwood). 2006;25(1):248–55. [DOI] [PMC free article] [PubMed]
- 30.Heiss F, McFadden D, Winter J. Who failed to enroll in Medicare part d, and why? Early results. Health Aff (Millwood). 2006;25(5):w344–54. [DOI] [PubMed]
- 31.Rector TS, Venus PJ. Do drug benefits help medicare beneficiaries afford prescribed drugs. Health Aff. 2004;23(4):213–22. [DOI] [PubMed]
- 32.Weingart SN, Gandhi TK, Seger AC, et al. Patient-reported medication symptoms in primary care. Arch Intern Med. 2005;165(2):234–40. [DOI] [PubMed]
- 33.Gandhi TK, Weingart SN, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348(16):1556–64. [DOI] [PubMed]
- 34.Garber MC, Nau DP, Erickson SR, Aikens JE, Lawrence JB. The concordance of self-report with other measures of medication adherence: a summary of the literature. Med Care. 2004;42(7):649–52. [DOI] [PubMed]


