Abstract
BACKGROUND
African Americans have higher rates of hypertension and worse blood pressure (BP) control than Whites, and poorer medication adherence may contribute to this phenomenon. We explored associations among patients’ race, self-reported experiences with clinicians, attitudes and beliefs about hypertension, and ultimately, medication adherence, among a sample with no racial disparities in BP control, to determine what lessons we could learn from patients and providers in this setting.
METHODS
We recruited 793 White and African-American (58%) patients previously diagnosed with hypertension from 3 VA medical centers to participate in survey assessments of each of the above dimensions, subsequent to a primary care clinic visit.
RESULTS
African-American patients’ providers were significantly more active in advising and counseling about hypertension care and medication adherence. African-American patients indicated greater knowledge or heightened awareness of the importance of controlling their BP, but there were no race differences on a summary adherence measure. In multivariate models modeling medication adherence, race was not significant, but having been told to split one’s pills, believing one’s BP continues to be high, and having one’s provider discuss things to do to make it easier to take BP medications were each significantly associated with worse adherence, whereas having more confidence in one’s ability to take BP medications as prescribed was associated with better adherence (all p’s ≤ .02).
CONCLUSION
When both physicians and patients take BP management seriously, disparities in BP adherence and control may be reduced.
KEY WORDS: physician–patient relations, patient compliance, attitude to health
BACKGROUND
Hypertension affects nearly 50 million Americans,1 and is more frequent among African Americans (www.americanheart.org., cited 2000 November 2), accounting for a significant portion of racial differences in mortality2. Many patients with established hypertension have poorly controlled blood pressure (BP), and African Americans are disproportionately represented among this group3.
Poor medication adherence is one of the most important barriers to blood pressure control1, but there is mixed evidence as to whether African Americans are less likely to adhere to prescribed therapies than Whites4,5. Provider–patient communication is an important determinant of adherence6, and poor communication is thought to contribute to worse care for African Americans and other ethnic minority individuals7,8. In addition, patients’ beliefs and attitudes about their blood pressure, and their experiences with providers regarding BP management, may ultimately affect adherence to treatment recommendations9,10. Yet little is known about how each of these dimensions varies by patient race. Such information is vital for the development of future clinical interventions to ultimately address disparities in blood pressure control.
Whereas most prior studies of race, medication adherence, and hypertension care have utilized samples with racial differences in BP control, we posit that the opposite approach might help identify factors associated with success in eliminating differences in BP care and outcomes. Thus, drawing from a multisite Department of Veterans Affairs (VA) sample with no racial disparities in BP control rates, we examined the links between patient race, experiences with clinicians, attitudes and beliefs about hypertension, and ultimately, adherence to antihypertensive medications. We first studied patterns of interactions with clinicians and patients’ beliefs about hypertension by race. Second, we examined patterns of antihypertensive medication adherence by race. Third, we evaluated whether any racial differences in interactions with clinicians or beliefs about blood pressure were related to observed differences in adherence.
METHODS
Sample
Initially, we identified all White and African-American patients with outpatient diagnoses of hypertension on at least 2 separate occasions in 2001 at 3 urban tertiary care Department of Veterans Affairs (VA) Medical Centers (ICD9 diagnosis codes: 401—401.0, 401.1, 401.9; 405—405.11, 405.19, 405.9, 405.91, 405.99). The study was approved by the Institutional Review Boards of all participating facilities, and patients provided informed consent.
Using this “universe” of 11,731 hypertensive patients from the 3 medical centers, study staff tracked patients’ primary care visits over a 14-month period, and as they presented for care, approached 1,210 of them to request participation in the study. A total of 203 were excluded owing to their race not being African American or White (n = 18), poor mental status (n = 41), denying hypertension (n = 59), participation in another hypertension study (n = 6), or miscellaneous other reasons (n = 79), leaving 1,007 eligible patients. Two hundred and fourteen patients (18% of the 1,210 approached) refused to participate. Thus, 793 patients were included in the final cohort (78.7% response rate).
Measures
Overview
We assessed 3 primary domains of interest: 1. Patient experiences with providers, 2. Patient characteristics, including sociodemographic factors and health beliefs, and 3. Antihypertensive medication adherence. In addition, we assessed numerous covariates that we thought were relevant to either the independent or dependent variables. Our selection of covariates was informed by the Health Decision Model (HDM;11). Figure 1 presents our expanded conceptualization of the factors that affect individuals’ health decisions (e.g., medication adherence), to include patient personality, preferences and knowledge, prior experiences, and social interactions (such as with physicians and family), in addition to health beliefs.
-
Experiences with providers
Using questions adapted from Ockene12, we assessed the content of the doctor–patient interaction focusing on hypertension and antihypertensive medication adherence, through an exit interview with each patient after his/her visit. Such “Patient Exit Interviews” (PEIs; see Table 2 for items [all yes/no responses]) have been demonstrated to accurately measure the actual content of clinic visits, through comparisons of audiotapes of such interactions to patient reports13. The question answers were summed to create 1 PEI scale score, with a range from 1 to 12 (higher scores indicate greater frequency of counseling).
-
Patient sociodemographic characteristics, and health beliefs
Patients completed an interview including questions about sociodemographic characteristics: date of birth, highest grade in school completed, employment, marital status, income, and race. We also obtained information about comorbid diagnoses and BP measurements from the medical record.
Following the Health Belief Model (HBM), which posits that patients’ appraisals of disease risk (susceptibility) and severity influence the practice of health-related behaviors14, we assessed patients’ perceptions of the seriousness of blood pressure, and consequences resulting from not taking BP medications (answer categories ranged from “extremely serious—a threat to one’s life’, to “not at all serious”). The HBM posits that an individual’s considerations of the perceived barriers and incentives for performing specific behaviors are important to consider. Thus, we asked patients if they thought BP medications would make them feel worse, or better, help them live longer, improve their quality of life, or prevent BP-related illnesses (all yes/no responses). Finally, the HBM considers cues to action, which prompt individuals to act by reminding them of the need to change their behaviors. We assessed 1 particular set of cues by asking patients if their family or friends help them to remember to take their BP medication.
-
Covariates
There is evidence that trust in one’s physician, experiences of racial discrimination in the health care setting, self-efficacy (e.g., knowledge about one’s BP, and confidence in one’s ability to take BP medications), complexity of one’s medical regimen, patient personality (both negative affect and optimism), and functional status might affect adherence. Thus, we assessed each dimension, as follows.
To assess trust in one’s physician, we included the 11-item Trust in Physician scale15, which assesses the extent to which patients feel their doctor cares about him/her, is considerate of his/her needs, tells the truth, and makes good judgments. The patients were asked to respond to each statement on a 5-point scale (1 = totally agree; 5 = totally disagree). Appropriate items were reverse coded and the answers to these questions were summed and converted to a 100-point scale, so higher scores represented greater trust. To assess patients’ experiences of racial discrimination in the health care setting, we included the “Experiences of Discrimination” scale. Item responses were summed and converted to a 100-point scale so that higher scores indicate less discrimination16. To assess self-efficacy, we asked patients how confident they were about their knowledge about BP and how to deal with it, and in their ability to take their BP medication as prescribed (0 = not confident at all; 10 = totally confident)6. To assess the complexity of a patient’s medication regimen17, we asked patients how many different types of BP pills they take, how many times each day they take it, and whether they were told to split their pills. Negative Affectivity (NA) was measured with the EPI-Q18. Optimism was assessed with the Life Orientation Test19. We included a broad generic measure of functional status, the VR-12 (the SF-12 adapted for veterans;20), which provides a mental component summary scale (MCS) and a physical component summary scale (PCS).
Figure 1.
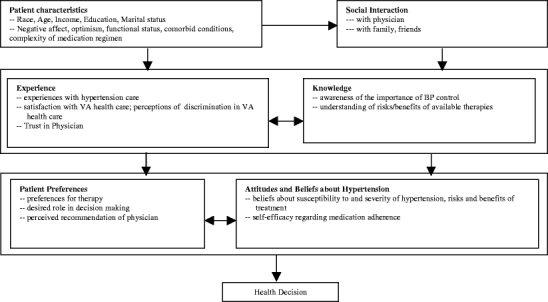
The health decision model, adapted from Eraker, Kirscht, and Becker, 1984 12.
Table 2.
Bivariate Results—Racial Differences in Experiences with Providers, and Beliefs and Attitudes Regarding High Blood Pressure (BP)
| Item text | African American (AA) | White | p value |
|---|---|---|---|
| Experiences with BP care/Patient Exit Interview items | |||
| PEI overall score | 6.6 | 5.8 | .01 |
| Did your primary care provider... | |||
| – talk to you about your BP and medications for BP during your appointment? (% yes) | 86.6 | 83.4 | .23 |
| – ask if you take your BP medication as prescribed? | 88.2 | 82.4 | .04 |
| – discuss how important your BP medication is for controlling your BP? | 84.6 | 78.0 | .03 |
| – discuss other health problems that might develop if someone does not take their BP medication? | 67.8 | 52.6 | <.001 |
| – advise you to take your BP medication as prescribed? | 90.3 | 88.8 | .54 |
| – discuss your efforts to manage your BP medication? | 77.4 | 73.6 | .28 |
| – discuss things that get in the way of taking your BP medication? | 34.6 | 31.0 | .35 |
| Did you and your provider... | |||
| – discuss things you can do to make it easier to take your BP medication? | 39.2 | 27.8 | .004 |
| – discuss any specific goals to help you take your BP medication as prescribed? | 37.4 | 34.4 | .46 |
| – agree on any specific goals for taking your BP medication? | 57.3 | 54.8 | .53 |
| Did your provider ask you to make another appointment to discuss your BP? | 59.5 | 67.2 | .05 |
| Did your provider give you any written materials about BP during your appointment? | 12.4 | 6.7 | .02 |
| Beliefs about BP and BP medications | |||
| Do you believe that taking BP medication...(% yes) | |||
| will make you feel worse? | 5.1 | 3.9 | .46 |
| will make you feel better? | 96.3 | 91.7 | .008 |
| will help you live longer? | 98.5 | 97.4 | .27 |
| will improve the quality of your life? | 95.4 | 93.4 | .25 |
| will prevent future high BP related illnesses? | 96.0 | 94.6 | .38 |
| How serious do you think high BP is, in general? | Extr. serious = 73.0% | Extr. serious = 59.9% | .003 |
| Quite serious = 17.2 | Quite serious = 25.1 | ||
| Mod. serious = 6.4 | Mod. serious = 11.4 | ||
| Little serious = 2.2 | Little serious = 2.6 | ||
| Not serious = 1.2 | Not serious = 1.0 | ||
| How serious do you think your high BP is, given your current use of medication? | Extr. serious = 31.8% | Extr. serious = 18.3% | <.001 |
| Quite serious = 19.9 | Quite serious = 17.3 | ||
| Mod. serious = 28.7 | Mod. serious = 37.3 | ||
| Little serious = 10.3 | Little serious = 11.1 | ||
| Not serious = 9.3 | Not serious = 16.0 | ||
| If you did not take your BP medication, how likely do you think it would be that you would develop other health problems over the next year? | Very likely = 71.3% | Very likely = 64.8% | .63 |
| Likely = 11.6 | Likely = 19.1 | ||
| 50–50 = 12.6 | 50–50 = 12.4 | ||
| Unlikely = 2.4 | Unlikely = 2.7 | ||
| Very unlikely = 2.2 | Very unlikely = 1.0 | ||
| If you did not take your BP medication, how likely do you think it would be that your BP would get worse over the next year? | Very likely = 75.9% | Very likely = 79.2% | .09 |
| Likely = 8.7 | Likely = 9.9 | ||
| 50–50 = 12.1 | 50–50 = 8.9 | ||
| Unlikely = 0.7 | Unlikely = 1.0 | ||
| Very unlikely = 2.7 | Very unlikely = 1.0 | ||
| How would you describe your BP currently? | Good control = 78.8% | Good control = 81.1% | .69 |
| High = 20.2 | High = 14.4 | ||
| No longer a prob = 0.9 | No longer a prob = 4.6 | ||
| BP medication adherence | |||
| Did you ever take less medicine because you felt you needed less? (% yes) | 12.6 | 8.8 | .11 |
| Sometimes if you feel worse when you take the medicine, do you stop taking it? (% yes) | 10.2 | 5.5 | .02 |
| How many days in the past week did you forget to take your BP medication? | 0 days = 78.9% | 0 days = 86.4% | .01 |
| 1 day = 10.7 | 1 day = 7.5 | ||
| 2+ days = 10.4 | 2+ days = 6.2 | ||
| How many days in the past week did you not take your medication on purpose? | 0 days = 90.7% | 0 days = 95.5% | .04 |
| 1 day = 4.3 | 1 day = 1.6 | ||
| 2+ days = 5.0 | 2+ days = 2.9 | ||
| How many days in the past week did you add an extra pill? | 0 days = 95.7% | 0 days = 97.1% | .54 |
| 1 day = 3.1 | 1 day = 1.6 | ||
| 2+ days = 1.2 | 2+ days = 1.3 | ||
| Some people have difficulty taking BP medication as prescribed. Do you have difficulty with this? (% yes) | 6.9 | 5.5 | .45 |
| Summary adherence measure (% adherent) | 74.2 | 79.8 | .10 |
| Covariates | |||
| Optimism scale (higher = more optimistic; mean scores) | 14.9 | 14.9 | .89 |
| Negative affectivity (higher = more negative affect; mean scores) | 3.3 | 3.4 | .53 |
| VR-12 Physical component (higher score is better) (mean score) | 40.1 | 38.0 | .02 |
| VR-12 Mental component (higher score is better) (mean score) | 48.8 | 50.7 | .03 |
| Trust in Physician (higher = more trust) | 78.2 | 82.5 | <.001 |
| Racial discrimination (lower = more discriminated against) | 57.5 | 91.6 | <.001 |
| Medication Regimen complexity | |||
| Split pills | 33.1 | 29.7 | .33 |
| # types of medications | 2.2 | 1.9 | .002 |
| # times/day medications taken | 1.4 | 1.5 | .30 |
| Family help taking medications (% yes) | 36.6 | 30.5 | .09 |
| Self-efficacy | |||
| Ability to take medications as prescribed? | 9.5 | 9.6 | .34 |
| Knowledge about BP and how to deal with it? | 8.8 | 8.4 | .01 |
Outcome Assessment – Antihypertensive Medication Adherence
We asked patients to self-report their medication adherence, using items from 2 well-validated measures from the literature to assess multiple dimensions of medication adherence. Following Choo et al.21, we assessed how many days in the past week patients forgot to take their blood pressure medication (0, 1, 2 or more days), how many days they did not take their medication on purpose (0, 1, 2, or more days), how many days they added an extra pill (0, 1, 2, or more days), whether they ever took less medicine because they felt they needed less (yes or no), and following Morisky et al.22 we asked, “sometimes if you feel worse when you take the medicine, do you stop taking it?” (yes or no). Finally, we asked, “Some people have difficulty taking blood pressure medication as prescribed. Do you have difficulty with this?” (yes or no).
We evaluated several different methods for combining these items, assessing the validity of each possible summary measure by examining its association with blood pressure control, choosing the measure with the strongest association. Thus, our final measure of adherence included the items assessing forgetting to take medications, not taking medications on purpose, taking less medications because of perceptions that one needed less, and having difficulties taking medications as prescribed. We specified that the patient must answer positively to at least 1 of the items to be considered as having adherence problems. We calculated this variable only for those who answered all of these questions. For the variables with 3 responses, a person was considered adherent if he/she indicated adherence problems for 0 day or 1 day each week, and nonadherent if he/she indicated adherence problems for 2 or more days; the other questions had yes/no responses (adherence problems or not).
Statistical Analyses
We first examined whether there were racial differences in interactions with clinicians, in patients’ beliefs and attitudes regarding hypertension, or in medication adherence, using bivariate analyses of each variable by race (chi square or t tests, as appropriate). Next, we performed bivariate analyses to determine which sociodemographic variables, health beliefs, and PEI items and other covariate scales were associated with the dichotomous adherence summary outcome. We then conducted stepwise analyses including all significant independent variables from the bivariate analyses, as well as race and site of care, retaining items significant at the p < .05 level. In the final step, using PROC LOGISTIC for the binary adherence outcome, we included all significant variables from the prior stepwise analysis, into the multivariate regression model (race and site of care were included in the final model regardless of their significance in prior analyses). All analyses were conducting using SAS 9.1.3 (SAS Institute, Cary, NC).
RESULTS
White patients were older (67.3 vs 64.4,) and more likely to be married (54.5 vs 37.4, both p’s < .0001; (Table 1)). African Americans had a lower frequency of coronary artery disease diagnoses (43% vs 53%), but nearly twice the rate of renal disease (31% vs 17%), and higher rates of tobacco use (21% vs 15%; all p’s < .05). African-American and White patients were equally likely to have a blood pressure greater than 140/90 mmHg (54% vs 57%, p = .41). Race was differentially distributed across sites, with the proportion of African Americans ranging from 42% (St. Louis), to 56% (Philadelphia), to 77% (Chicago; 58% overall). To account for these differences across sites, site was included as a covariate in all models. Adherent patients were 1.5 times more likely to have controlled BP than nonadherent patients, after controlling for comorbid conditions, BMI, age, and site of care (p = .0433; results not shown).
Table 1.
Sociodemographic and Clinical Characteristics of the Cohort, by Race
| African Americans N = 460 | Whites N = 333 | p value | |
|---|---|---|---|
| Sociodemographic variables | |||
| Age (mean) | 64.4 | 67.3 | <.001 |
| Education (%≥12 years) | 72.4 | 75.0 | .42 |
| Income (% ≥$20,000) | 45.5 | 47.9 | .53 |
| Employed | 17.7 | 13.6 | .12 |
| Married | 37.4 | 54.5 | <.001 |
| Blood pressure (% ≥140/90) | 53.6 | 56.6 | .41 |
| Blood pressure (% ≥160/100) | 19.4 | 14.5 | .07 |
| Benign prostatic hypertrophy | 33.5 | 30.6 | .40 |
| Coronary artery disease | 43.0 | 52.9 | .006 |
| Congestive heart failure | 20.4 | 24.3 | .19 |
| Cerebrovascular disease | 20.0 | 22.5 | .39 |
| Diabetes | 51.5 | 48.7 | .42 |
| Hyperlipidemia | 64.4 | 69.1 | .17 |
| Peripheral vascular disease | 26.3 | 23.4 | .36 |
| Renal disease | 31.3 | 16.5 | <.001 |
| Tobacco use (% yes) | 21.3 | 14.7 | .02 |
| Body mass index (mean) | 30.1 | 30.9 | .08 |
There were important bivariate racial differences on each of the 3 primary dimensions assessed (Table 2).
Patient–provider interactions African Americans (AA) reported that their providers were more active in counseling and advising them about BP, with a higher total patient exit interview score than Whites (6.6 vs 5.8, p < .01), indicating that AAs’ providers asked about 1 more question on average regarding BP. However, Whites’ (W) providers were more likely to request a follow-up appointment for BP care (67% vs 60%, p = .05). Whereas relatively high rates of patients of both races (∼80%) reported that doctors discussed BP and its management with them, only about a third of patients reported that providers explicitly discussed barriers to BP medication adherence, and only about 10% of patients reported that their providers provided them with written materials about BP (although AA patients more often reported that their doctors had done so: 12% vs 7%). African Americans reported that their doctors more often discussed other health problems that might result from high BP (68% vs 53%), whether they take their medications as prescribed (88% vs 82%), how important medications are for controlling BP (85% vs 78%), and discussed things to do to make it easier to take BP medications (39% vs 28%; all p’s < .05).
Patients’ beliefs about BP and BP medications Whereas there were some similarities in perceptions about BP medications, AAs were more likely to report that BP medications would make them feel better, and to rate high BP as a more serious health concern (p’s ≤ .01; Table 2). There were no significant racial differences in patients’ perceptions of whether their BP is under good control.
Medication adherence African Americans were less adherent on 3 of the 6 single items assessing adherence (more likely to stop taking medications if one feels worse; not taking medication on purpose, and forgetting to take medications [all p’s < .05]; Table 2). However, such differences remained only at the trend level on the summary adherence variable (74% vs 80%, p = .10).
Covariates With regard to medication regimen complexity, there were no racial differences in patients being told to split pills (on average, approximately 30% of both groups were told to do so) or in the number of times per day BP medications were taken. However, African Americans were taking 2.2 types of medications versus Whites’ 1.9 (p = .002). African Americans felt more knowledgeable about their BP and how to deal with it, and had better physical and mental functioning. Finally, African Americans were more likely to have experienced racial discrimination and White patients indicated greater trust in their physicians (p’s < .05).Last, we calculated a multivariate logistic regression model for self-reported adherence (Table 3). Confidence in one’s ability to take medications as prescribed was associated with better adherence (p < .0001). However, patient perception that one’s BP continues to be high was associated with worse adherence (p = .006), as were having the provider discuss things the patient can do to make it easier to take BP medications (p = .006) and being told to split one’s pills (p = .016).
Table 3.
Multivariate Logistic Regression Modeling Self-reported Medication Adherence
| Independent variables | Odds ratio | 95% CI | p value |
|---|---|---|---|
| White race vs. Black race | 1.24 | 0.80–1.92 | .33 |
| How confident about ability to take BP meds as prescribed | 1.41 | 1.20–1.67 | <.001 |
| Did you and provider discuss things you can do to make it easier to take your BP meds? | 0.56 | 0.37–0.85 | .006 |
| Told to split any BP pills by MD or pharmacist? | 0.58 | 0.37–0.90 | .02 |
| How would you describe your BP currently? | |||
| Continues to be high vs. under good control | 0.51 | 0.32–0.82 | .006 |
| No longer a problem vs. under good control | 0.41 | 0.07–2.32 | .32 |
| Site of care | |||
| Chicago vs. St. Louis | 1.00 | 0.61–1.65 | .99 |
| Philadelphia vs. St. Louis | 1.28 | 0.75–2.19 | .37 |
DISCUSSION
This study is among the first to simultaneously examine racial differences in patients’ experiences with physicians, attitudes and beliefs about hypertension and antihypertensive medication, and the association of each of these dimensions with patients’ antihypertensive medication adherence. In our sample with similar BP control among Whites and African Americans, we found that African Americans believed BP to be a more serious health threat, suggesting that public health, VA system-wide, and clinician-provided messages about the significance of high BP, especially among African Americans, seem to be reaching their target. These results also suggest that African Americans are receiving enhanced BP care—their physicians counseled them more about blood pressure and prescribed more medications for their BP. Thus, these VA providers seem to have received and acted upon the message regarding poorer outcomes for African-American patients with hypertension. We conclude that such methods and strategies, when used by clinicians, may positively influence patients’ beliefs about antihypertensive medications.
Our findings differ from previous reports about racial/ethnic differences in specific knowledge and beliefs about hypertension23,24, and suggest that in the VA setting, African Americans perceive BP to be a more serious threat to health than do White patients. In contrast, whereas earlier reports had noted that White patients were more likely to be counseled about hypertension by their providers25, our findings suggest the opposite dynamic is occurring in the VA.
Our study was limited in several ways. First, we only studied regular users of the VA care system, which may have biased our sample toward more adherent patients (e.g., appointment keepers). However, we still observed a range of adherence behaviors. Also, the VA system cares primarily for male patients, so our results may not be generalizable to women, or to patients in non-VA settings. Further, racial disparities in health care may be minimized in the VA setting26, which could limit our ability to generalize these findings.
These results suggest that several patient health beliefs and practices are associated with adherence, although we were unable to determine the causal direction of the associations. The fact that a patient’s understanding that his blood pressure was high was negatively associated with adherence, as were reports of providers counseling about medication taking suggests that providers may have been working harder with patients with harder-to-control BP, or with patients who did not seem to be adherent.
Notably, patients with greater perceived self-efficacy in medication taking had better adherence. Such beliefs can be fostered by primary care providers during clinic visits, using strategies developed for patient-centered counseling12. Clinicians can ask open-ended questions of their patients about medication adherence such as, “What kinds of problems are you having taking your blood pressure medications?” Then, using barriers identified by the patients, clinicians can help to strategize ways to address such barriers, thus enhancing patients’ self-efficacy, and adherence. Indeed, our prior work has demonstrated that there is room for improvement in primary care clinicians’ antihypertensive medication adherence counseling skills27.
African Americans are disproportionately affected by hypertension, with lower rates of blood pressure control in the general population, although not in this VA sample. Notably, less than half of this sample overall had controlled BP, indicating much room for improvement in BP care. Our findings suggest that patient beliefs are significantly associated with blood pressure medication adherence. Thus, we encourage providers to actively learn more about their patients’ beliefs about both hypertension and its therapies, to provide targeted counseling to help patients improve medication adherence, and ultimately, blood pressure control.
Acknowledgments
This research was presented as a poster at the American Heart Association Compliance Conference, May 2005 (NR Kressin, MB Orner, F Wang, J Long, W Kozak, C Clark, S Reddy, L Kroupa, B Bokhour, J Rothendler, D Berlowitz. Racial Differences in Antihypertensive Medication Adherence, Attitudes, Beliefs and Experiences with Blood Pressure Care). This research was supported by grants from the Department of Veterans Affairs (VA) Health Services Research and Development Service (TRH01-038, N. Kressin, P.I). Dr. Kressin is a Research Career Scientist, Department of Veterans Affairs, Health Services Research & Development (RCS 02-066-1); Dr. Long was an Associate in the Career Development Award Program of the VA HSR&D Service when this work was performed (CDA # 00-023).
Conflict of Interest No authors have any affiliation, financial agreement, or other involvement with any company whose product figured prominently in the submitted manuscript.The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
References
- 1.Joint National Committee. The sixth report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Arch Intern Med. 1997;157:2413–46. [DOI] [PubMed]
- 2.Wong M, Shapiro M, Boscardin W, et al. Contributions of major diseases to disparities in mortality. N Engl J Med. 2002;347:1585–92. [DOI] [PubMed]
- 3.Cushman WC, Ford CE, Cutler JA, et al. Success and predictors of blood pressure control in diverse North American settings: the antihypertensive and lipid-lowering treatment to prevent heart attack trial (ALLHAT). J Clin Hypertens (Greenwich). 2002;4(6):393–404. [DOI] [PubMed]
- 4.Monane M, Bohn RL, Gurwitz JH, Glynn RJ, Levin R, Avorn J. Compliance with antihypertensive therapy among elderly Medicaid enrollees: the roles of age, gender, and race. Am J Public Health. 1996;86(12):1805–8. [DOI] [PMC free article] [PubMed]
- 5.Sharkness CM, Snow DA. The patient’s view of hypertension and compliance. Am J Prev Med. 1992;8:141–6. [PubMed]
- 6.Dunbar-Jacob JM, Schlenk EA, Burke LE, Matthews JT. Predictors of patient adherence: patient characteristics. In: Shumaker SA, Schron EB, Ockene JK, McBee WL, eds. The Handbook of Health Behavior Change. 2nd ed. New York: Springer Publishing Company; 1998:491–512.
- 7.Kressin NR, Petersen LA. Racial variations in cardiac procedures: a review of the literature and prescription for future research. Ann Intern Med. 2001;135:352–66. [DOI] [PubMed]
- 8.Kleinman A, Eisenberg L, Good B. Culture, illness, and care: clinical lessons from anthropologic and cross-cultural research. Ann Intern Med. 1978;88:251–8. [DOI] [PubMed]
- 9.Taylor DW, Sackett DL, Johnson AL, Gibson ES, Roberts RS. Compliance with antihypertensive drug therapy. Ann NY Acad Sci. 1978:390–403. [DOI] [PubMed]
- 10.Norman SA, Marconi KM, Schezel GW, Schechter CF, Stolley PD. Beliefs, social normative influences, and compliance with antihypertensive medication. Am J Prev Med. 1985;1(3):10–7. [PubMed]
- 11.Eraker SA, Kirscht JP, Becker MH. Understanding and improving patient compliance. Ann Intern Med. 1984;100:258–68. [DOI] [PubMed]
- 12.Ockene IS, Hebert JR, Ockene JK, Merriam PA, Hurley TG, Saperia GM. Effect of training and a structured office practice on physician-delivered nutrition counseling: the Worcester-Area Trial for Counseling in Hyperlipidemia. Am J Prev Med. 1996;12(4):252–8. [PubMed]
- 13.Pbert L, Adams A, Quirk M, Hebert J, Ockene J, Luippold R. The Patient exit interview as an assessment of physician-delivered smoking intervention: a validation study. Health Psychol. 1999;18(2):183–8. [DOI] [PubMed]
- 14.Rosenstock I. Why people use health services. Milbank Mem Fund Q. 1966;44(94). [PubMed]
- 15.Thom D, Ribisl K, Stewart A, Luke D, and the Stanford Trust Study Physicians. Further validation and reliability testing of the Trust in Physician scale. Med Care. 1999;37(5):510–7. [DOI] [PubMed]
- 16.Krieger N. Racial and gender discrimination: risk factors for high blood pressure? Soc Sci Med. 1990;30(12):1273–81. [DOI] [PubMed]
- 17.Miller NH, Hill M, Kottke T, Ockene IS. The multilevel compliance challenge: recommendations for a call to action–a statement for healthcare professionals. Circulation. 1997;95:1085–90. [DOI] [PubMed]
- 18.Eysenck HJ, Eysenck SB. Manual of the Eysenck Personality Inventory. San Diego: Educational & Industrial Testing Service; 1968.
- 19.Scheier M, Carver C, Bridges M. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): a reevaluation of the life orientation test. J Pers Soc Psychol. 1994;67(6):1063–78. [DOI] [PubMed]
- 20.Kazis LE, Miller DR, Clark JA, et al. Improving the response choices on the veterans SF-36 health survey role functioning scales: results from the Veterans Health Study. J Ambul Care Manage. 2004;27(3):263–80. [DOI] [PubMed]
- 21.Choo PW, Rand CS, Inui TS, et al. Validation of patient reports, automated pharmacy records, and pill counts with electronic monitoring of adherence to antihypertensive therapy. Med Care. 1999;37(9):846–57. [DOI] [PubMed]
- 22.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67–74. [DOI] [PubMed]
- 23.Okonofua E, Cutler N, Lackland D, Egan B. Ethnic differences in older americans: awareness, knowledge, and beliefs about Hypertension. Am J Hypertens. 2005;18:972–9. [DOI] [PubMed]
- 24.Hertz R, Unger A, Cornell J, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005;165:2098–104. [DOI] [PubMed]
- 25.Tschann JM, Adamson TE, Coates TJ, Gullion DS. Behaviors of treated hypertensive patients and patient demographic characteristics. J Commun Health. 1988;13(1):19–32. [DOI] [PubMed]
- 26.Jha AK, Shlipak MG, Hosmer W, Frances CD, Browner WS. Racial differences in mortality among men hospitalized in the Veterans Affairs health care system. JAMA. 2001;285(3):297–303. [DOI] [PubMed]
- 27.Bokhour BG, Long JA, Berlowitz DR, Kressin NR. Assessing patient adherence in medical encounters: how do providers talk with patients about antihypertensive medication taking? J Gen Intern Med. 2006;21(6):577–83. [DOI] [PMC free article] [PubMed]


