Abstract
BACKGROUND
Posttraumatic stress disorder (PTSD) is associated with medical and psychological morbidity. The prevalence of PTSD in urban primary care has not been well described.
OBJECTIVE
To measure the prevalence of PTSD in primary care patients overall and among those with selected conditions (chronic pain, depression, anxiety, heavy drinking, substance dependence (SD), irritable bowel syndrome (IBS), and immigrant status).
DESIGN
Cross-sectional study.
PARTICIPANTS
English-speaking patients aged 18–65 years old, awaiting primary care appointments in an urban academic medical center, were eligible for enrollment to determine PTSD prevalence (N = 509). Additional eligible participants (n = 98) with IBS or SD were subsequently enrolled.
MEASUREMENTS
PTSD (past year) and trauma exposure were measured with Composite International Diagnostic Interview. We calculated the prevalence of PTSD associated with depression, anxiety, heavy drinking, SD, IBS, and chronic pain. Only the analyses on heavy drinking, SD, and IBS used all 607 participants.
RESULTS
Among the 509 adults in primary care, 23% (95% CI, 19–26%) had PTSD, of whom 11% had it noted in the medical record. The prevalence of PTSD, adjusted for age, gender, race, and marital and socioeconomic statuses, was higher in participants with, compared to those without, the following conditions: chronic pain (23 vs 12%, p = .003), major depression (35 vs 11%, p < .0001), anxiety disorders (42 vs 14%, p < .0001), and IBS (34 vs 18%, p = .01) and lower in immigrants (13 vs 21%, p = .05).
CONCLUSIONS
The prevalence of PTSD in the urban primary care setting, and particularly among certain high-risk conditions, compels a critical examination of optimal approaches for screening, intervention, and referral to PTSD treatment.
KEY WORDS: underserved populations, PTSD, prevalence
INTRODUCTION
Media coverage of the 2001 World Trade Center attacks increased American awareness of posttraumatic stress disorder (PTSD) as an important psychiatric diagnosis.1,2 Recent documentation of the burden of mental disorders, including PTSD, among US soldiers returning from Iraq3,4 and people affected by Hurricane Katrina5–7 further increased awareness of PTSD risk after exposure to trauma. Posttraumatic stress disorder is characterized by disabling symptoms of reexperiencing, avoidance, and numbing after a significant traumatic event.8 The World Health Organization and others have substantiated the major impact of posttraumatic mental disturbance on social and health functioning.9,10
In primary care settings, the prevalence of PTSD depends upon the features of the population studied and the methods for participant recruitment and assessment. In a nationally representative US sample, Kessler et al.11 found a lifetime PTSD prevalence of 6.8%; 61% of males and 51% of females reported trauma exposure.12 Breslau et al.13 reported 90% lifetime prevalence of trauma and 9% probability of developing PTSD after trauma in an urban sample in Detroit. Stein and colleagues14 found a 2% prevalence of current PTSD in a middle-class, university-affiliated primary care practice in San Diego. In a representative sample of national health clinics in Israel, 9% of patients had current PTSD.15 One-third of African-American primary care patients in an urban setting met PTSD diagnostic criteria.16 Prevalence at veterans affairs (VA) health facilities ranges from 11.5% (current) to 27% (lifetime) PTSD.17,18 Female gender, being divorced or widowed, other psychiatric or substance-use disorders, and exposure to certain traumas increase PTSD risk.12,13,19
However, these studies may not accurately estimate PTSD prevalence because of selective recruitment, nondiagnostic assessments, and low study participation.14,16,19–21 Only one of these studies was conducted in a primary care practice in an urban, impoverished, and under represented minority population, a group at risk for PTSD because of high trauma exposure and low levels of social support.22 PTSD is clinically under-recognized; of patients with PTSD, primary care providers recognized 2% in Israel and 47% in a VA setting.15,17 These findings are consistent with extensive literature on clinician under-recognition of other mental disorders.23
Accurate determination of PTSD prevalence in primary care settings serving patients at high risk is important for several reasons. First, PTSD is associated with increased health-care utilization.4,24–26 Second, PTSD and trauma exposure have been associated with conditions commonly treated by primary care clinicians: somatization functional impairment, depression, anxiety, chronic pain, irritable bowel syndrome (IBS) and substance-use disorders.15,18,20,27–42 Apart from depression,16 these associations have not been evaluated in primary care. Additionally, immigrant and refugee populations have high exposure to violence and merit further evaluation.43 If PTSD is sufficiently prevalent in urban primary care patients or in those with certain common conditions, then it fulfills a key criterion for a clinical screening recommendation.44 Determining if primary care patients with specific comorbid conditions have particularly high prevalence of current PTSD strengthens the case and may even suggest an approach for targeted screening in primary care.
We conducted a cross-sectional study to evaluate the prevalence of and risk factors for PTSD in primary care patients at an urban hospital-based outpatient department. We assessed the prevalence of PTSD among those with immigrant status, depression, generalized anxiety or panic disorder, chronic pain, IBS, heavy drinking, and substance dependence (SD), and we determined also whether PTSD was identified by physicians caring for these patients. We hypothesized that PTSD prevalence would be high, especially in patients with selected characteristics, and under-recognized by clinicians. We also hypothesized that clinicians might identify PTSD as depression, a more familiar mental illness.
METHODS
Study Design
We interviewed a consecutive sample of primary care patients at the outpatient department of an urban university-affiliated hospital to examine overall prevalence of PTSD and its prevalence among patients with seven selected conditions: being an immigrant to the United States, major or other depression, generalized anxiety or panic disorder, heavy drinking, SD, IBS, and chronic pain. We also reviewed medical records for documentation of PTSD and depression.
Participants
Patients visiting the Internal Medicine and Family Medicine clinics were eligible if they spoke English, were 18–65 years old, and had a scheduled appointment with a primary care clinician. Patients were excluded if they could not be interviewed alone or did not appear to understand study procedures. After a planned minimum study enrollment of 100 participants per selected condition was met for depression, anxiety, pain, and immigrant status with the first 509 enrolled participants (“consecutive sample”), enrollment was limited to eligible patients with heavy drinking, drug use or IBS, or none of the selected conditions (control group) to permit planned subgroup analyses (“oversampled group”, n = 98). Enrollment occurred from February 2003 to September 2004.
Recruitment and Enrollment
Interviewers approached consecutive patients upon arrival for appointments and screened them for eligibility. Eligible patients were asked to participate in an interview about stress and health. Each participant gave written informed consent. Study participants were compensated with $10, and they received safety referrals upon interview completion. Interviews not completed before clinician visit were completed immediately afterward. Boston University Medical Center’s Institutional Review and HIPAA Privacy Review Boards approved the study. A Certificate of Confidentiality was obtained from the National Institutes of Health.
Data Collection
Screening
The self-administered screening tool contained 19 questions about the following: demographics, symptoms of depression and anxiety (2 questions from the PRIME-MD screener),45 IBS (4 definition questions from the ROME II Integrative questionnaire),46 quantity and frequency of alcohol use in the past 30 days,47 use of heroin or cocaine in the past month, and chronic pain in the past 3 months.48
Interview
Interview included demographic questions, the Composite International Diagnostic Interview (CIDI) version 2.1 PTSD module,8,49 the Chronic Pain Definitional Questionnaire,48 the Patient Health Questionnaire (PHQ)45 modules measuring depression diagnoses (major and other depression in the past 2 weeks) and anxiety disorder (generalized anxiety and/or panic disorder in the past 4 weeks), and the CIDI-Short Form (CIDI-SF) substance-use disorder modules.49 The interview lasted for approximately 30 min.
Medical Record Review
Using standardized data-collection forms, researchers trained in chart abstraction reviewed patient electronic medical records (EMRs), including all outpatient and emergency department records and inpatient discharge summaries for the 12 months before and including the date of interview, to identify documentation of ICD-9 coded PTSD or depression in the problem list or in the visit assessment. All clinical encounters used EMR documentation.
Dependent Variables: Trauma Exposure, PTSD, Medical Record Documentation
Current (past 12 months) and lifetime PTSD were diagnosed using CIDI version 2.1.49 The CIDI includes 9 questions about specific traumatic events and 2 open-ended questions. The research team classified open-ended responses as traumatic or nontraumatic according to DSM-IV guidelines for qualifying trauma.8 We defined trauma exposure as self-reported experience of any category of qualifying trauma. Multiple experiences of a single category of trauma (e.g., rape or physical assault) were counted as one trauma exposure. Clinician recognition of PTSD and depression was defined as documentation of this diagnosis (PTSD or depression, respectively) in the active problem list or in the free text of a note in the medical record.
Independent Variables and Covariates
Independent variables included immigrant status, IBS, chronic pain, anxiety, depression, heavy drinking, and SD. Immigrants were participants born outside the US or Puerto Rico. Irritable bowel syndrome was present if participants endorsed diagnostic criteria from the Rome II Integrative Questionnaire.46 Chronic pain was present if participants endorsed pain for 3 months or more on the Chronic Pain Definitional Questionnaire.48 Current anxiety disorder was present if participants met diagnostic criteria for generalized anxiety and/or panic disorder in the past month according to the PHQ.45 Current depressive disorder was classified into major or other depression in the past 2 weeks according to the PHQ.45 Heavy drinking in the past month was defined using the National Institute of Alcohol Abuse and Alcoholism guidelines.47 Substance dependence included alcohol dependence and/or drug dependence in the past 6 months as determined by the CIDI-SF.50 Covariates were age, gender, income, employment, marital status, and race.
Analyses
We used descriptive analyses to determine the prevalence of current and lifetime PTSD and trauma exposure. Bivariate analyses compared the prevalence of PTSD and trauma exposure in people with and without 7 selected conditions. We employed multivariable logistic regression to adjust for covariates. Adjusted proportions were calculated using the mean values of background covariates; P values comparing adjusted proportions are based on the regression coefficients for the group variable. Bivariate analyses compared PTSD or depression EMR documentation with research interview diagnoses. We used the consecutive sample (N = 509) for most analyses. Analyses examining heavy drinking, SD, and IBS utilized the enhanced sample (the consecutive sample plus the oversampled group, n = 98) of 607 participants.
RESULTS
Participant Demographic and Clinical Characteristics
Of 627 eligible patients, 509 (81%) were enrolled in the consecutive sample (Fig. 1). See Table 1 for the demographic and clinical characteristics of the sample. Gender differences were notable for race, immigrant status, income, other depression, anxiety, and SD. Compared to US-born people, immigrants were more likely to be employed (63 vs 47%) and to be married or living with a partner (37 vs 23%).
Figure 1.
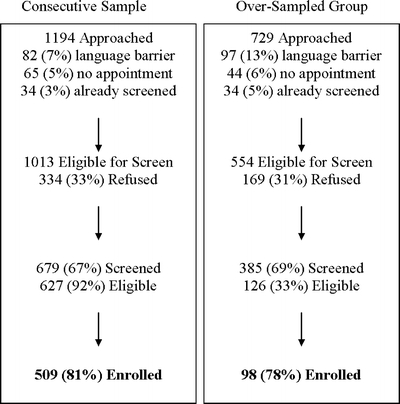
Study enrollment of patients in primary care. Consecutive sample: patients approached consecutively after registering for appointment. Oversampled group: consecutive sample criteria plus positive screen for irritable bowel symptoms, heavy drinking in past month, use of drugs in past month, or none of 6 select conditions (see text for details).
Table 1.
Demographic and Clinical Characteristics of Participants Recruited in Primary Care (Consecutive Sample)
| Variable | Total (N = 509) | Male (n = 251) | Female (n = 258) |
|---|---|---|---|
| N (%) | |||
| Mean age in years (SD) | 42 (11.3) | 42 (11.1) | 41 (11.5) |
| Race/Ethnicity | |||
| Black/African American | 300 (59) | 137 (55) | 163 (63) |
| White | 98 (19) | 60 (24) | 38 (15) |
| Hispanic/Latino | 40 (8) | 25 (10) | 15 (6) |
| Other | 71 (14) | 29 (12) | 42 (16) |
| Immigrant status | |||
| USA- or Puerto Rico-born | 365 (72) | 194 (77) | 171 (66) |
| Marital Status | |||
| Married/Living with partner | 137 (27) | 67 (27) | 70 (27) |
| Separated/Divorced | 110 (22) | 55 (22) | 55 (21) |
| Widowed | 19 (4) | 5 (2) | 14 (5) |
| Never married/not living with a partner | 243 (48) | 124 (49) | 119 (46) |
| Employment status | |||
| Full-/Part-time | 234 (46) | 118 (47) | 116 (45) |
| Student | 28 (6) | 11 (4) | 17 (7) |
| Unemployed or disabled | 247 (49) | 122 (49) | 125 (48) |
| Annual income | |||
| <*$20,000 | 254 (52) | 109 (44) | 145 (59) |
| Irritable bowel syndrome | 27 (5) | 12 (5) | 15 (6) |
| Chronic pain* | 324 (64) | 156 (62) | 168 (65) |
| Major depression* | 109 (21) | 46 (18) | 63 (24) |
| Other depressive disorder* | 110 (22) | 45 (18) | 65 (25) |
| Anxiety disorder† | 109 (22) | 44 (18) | 65 (25) |
| Heavy drinking | 48 (9) | 24 (10) | 24 (9) |
| Substance dependence‡ | 73 (15) | 52 (21) | 21 (8) |
*N = 508
†Generalized anxiety and/or panic disorders (N = 500)
‡N = 502
PTSD and Trauma Prevalence
Thirty-four percent (95% CI, 30–38%) of the consecutive sample met the diagnostic criteria for lifetime PTSD and 23% (CI 19–26%) for current PTSD. Median duration of PTSD symptoms was 6 years (range 1 month–44 years). Twenty-six percent (CI 21–32%) of women and 19% (CI 14–24%) of men met the criteria for current PTSD (p = .04). Trauma exposure was very common (79%), with 65% reporting exposure to more than one trauma category. See Appendix for details of trauma exposure.
Current PTSD was more common in participants with incomes <$20,000 (30 vs 14%, p < .0001), unemployed or disabled (30 vs 16%, p = .0001), or separated/divorced (31 vs 15% for married, p = .009; or 31 vs 22% for never married, p = .009).
Comorbid Conditions
PTSD was significantly more common among participants with at least one comorbid condition (depression, pain, IBS, anxiety, and/or SD) than among those with none of these conditions (27 vs 8%, p < .0001). Ninety-one percent of participants with current PTSD had at least one comorbid condition compared to 71% of those without PTSD. Of note, 75% of the entire consecutive sample (including those with PTSD) met the diagnostic criteria for at least one comorbid condition. In those with a comorbid condition, 28% had PTSD, whereas in those without a comorbid condition, 91% did not have PTSD.
Relationship of Comorbid Conditions with PTSD Prevalence: Adjusted Analyses
In the consecutive sample, current PTSD was less common among immigrants compared to nonimmigrants. Current PTSD was more common among participants with chronic pain, anxiety disorders, and both major and other depression. Adjusted analyses of lifetime PTSD prevalence in people with comorbid conditions echoed the current PTSD findings (Table 2).
Table 2.
PTSD Prevalence Among Participants with Selected Conditions (Consecutive Sample, N = 509)
| Current PTSD | Lifetime PTSD | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Condition | N | Unadjusted prevalence (%) | p value | Adjusted prevalence‡ (95% CI) | p value§ | Unadjusted prevalence (%) | p value | Adjusted prevalence‡ (95% CI) | p value§ | |
| Immigrant* | Yes | 140 | 17 | 0.06 | 13% (8–20) | 0.046 | 24 | 0.004 | 22% (15–30) | 0.006 |
| No | 359 | 25 | 21% (17–26) | 38 | 36% (31–42) | |||||
| Chronic pain* | Yes | 319 | 27 | 0.0009 | 23% (18–29) | 0.003 | 40 | <0.0001 | 38% (33–44) | 0.0003 |
| No | 180 | 14 | 12% (8–18) | 23 | 21% (15–28) | |||||
| Anxiety† | Yes | 104 | 50 | <0.0001 | 42% (31–53) | <0.0001 | 68 | <0.0001 | 64% (53–74) | <0.0001 |
| No | 389 | 16 | 14% (11–18) | 25 | 25% (21–30) | |||||
| Major depression* | Yes | 104 | 43 | <0.0001 | 35% (25–45) | <0.0001 | 60 | <0.0001 | 54% (44–65) | <0.0001 |
| Other depression | Yes | 109 | 31 | 26% (18–36) | 41 | 38% (29–48) | ||||
| No depression | 286 | 12 | 11% (8–16) | 22 | 22% (17–28) | |||||
*N = 499
†Generalized anxiety disorder and/or panic disorder (N = 493)
‡Models are adjusted for age, gender, race, income, employment, and marital status. Adjusted proportions were calculated using the mean values on background covariates.
§p values comparing adjusted proportions are based on the regression coefficients for the group variable.
Adjusted analyses in the enhanced sample revealed that current, but not lifetime, PTSD was significantly more common in participants with IBS. Current PTSD prevalence was not significantly higher among heavy drinkers or those with SD, whereas lifetime PTSD was (Table 3).
Table 3.
PTSD Prevalence Among Participants with Comorbid Conditions (Enhanced Sample, N = 607)
| Current PTSD | Lifetime PTSD | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Condition | N | Unadjusted prevalence (%) | p value | Adjusted prevalence‡ (95% CI) | p value§ | Unadjusted prevalence (%) | p value | Adjusted prevalence‡ (95% CI) | p value§ | |
| IBS* | Yes | 47 | 45 | 0.0002 | 34% (22–49) | 0.012 | 53 | 0.007 | 45% (31–60) | 0.104 |
| No | 550 | 21 | 18% (15–22) | 34 | 32% (28–37) | |||||
| Heavy† | Yes | 73 | 32 | 0.05 | 26% (16–38) | 0.174 | 53 | 0.0005 | 49% (37–62) | 0.007 |
| Drinking | No | 524 | 21 | 19% (15–23) | 33 | 31% (27–36) | ||||
| Substance | Yes | 105 | 30 | 0.056 | 26% (18–36) | 0.069 | 52 | <0.0001 | 52% (41–62) | <0.0001 |
| Dependence† | No | 488 | 21 | 18% (14–22) | 31 | 29% (25–34) | ||||
*N = 597
†N = 593
‡Models are adjusted for age, gender, race, income, employment, and marital status. Adjusted proportions were calculated using the mean values on background covariates.
§p values comparing adjusted proportions are based on the regression coefficients for the group variable.
Clinician Recognition: Medical Record Documentation
Based on EMRs of the participants in the consecutive sample, 11% of patients with CIDI-determined current PTSD had a PTSD diagnosis documented in the medical record. Of participants with current PTSD, 51% had depression noted in the medical record. Depression was noted in the EMR of 55% of those with both PTSD and depression (major and other), 43% of those with PTSD alone, 32% of those with depression but not PTSD, and 18% of those with neither PTSD nor depression (p < .0001 for differences between groups).
DISCUSSION
Among the patients attending an urban hospital-based primary care practice, PTSD is an exceptionally common diagnosis.51 Almost one-quarter of patients met the criteria for current PTSD and one-third met the criteria for lifetime PTSD. Importantly, documentation of this diagnosis was exceedingly uncommon. Only 11% of those with current PTSD were correctly identified in the medical record. In patients with certain conditions (chronic pain, IBS, depression, anxiety disorder, and SD), PTSD prevalence was two to three times as high; patients with these conditions accounted for over 90% of all cases of PTSD. While over a quarter of those with a co-occurring condition had PTSD, not having a co-occurring condition made the diagnosis of PTSD very unlikely.
Our findings are consistent with the published studies of people with PTSD reporting more physical symptoms.52–58 Multiple factors may contribute to the association between PTSD and physical symptoms including organic illnesses,31,57,59–61 altered physiology,62–64 and psychological mechanisms.30
In this study, lifetime PTSD was present in half of patients with current heavy drinking and SD. These findings are similar to those from substance-abuse treatment settings and primary care.38,39,65 Surprisingly, current SD and heavy drinking were strongly associated with lifetime PTSD but only weakly with current PTSD. One explanation may be that substance use dampens PTSD symptoms, an assertion supported by reports of PTSD patient self-medication in other studies.66–68 Another explanation may be that patterns of substance use are initiated in a period of current PTSD but persist beyond its resolution.
The higher PTSD prevalence in those with a diagnosis of depression and anxiety was not unexpected based on the literature detailing the psychiatric conditions comorbid with PTSD.12,69 While primary care clinicians have become relatively more comfortable with identifying and managing depression in the past 10 years, more work remains to optimize screening and treatment for other psychiatric disorders.70–73 More than half of our participants with EMR documentation of depression met the diagnostic criteria for PTSD, suggesting that clinicians may have labeled psychological distress as the more familiar diagnosis of depression.
Unlike depression, for which medication alone can be effective, evidence-based care for PTSD includes psychotherapy with or without medication.74 Trauma-focused psychotherapies can result in significant improvement of symptoms in more than half of patients.75 Thus, treatment by primary care clinicians may require new strategies beyond psychoactive medication prescription. In particular, the close relationship between physical problems and PTSD suggests an avenue to develop new interventions, better coordinating the care of general medicine and mental-health clinicians. Such coordination of care to address mental-health conditions in the primary care setting has been encouraged by a recent Institute of Medicine report.76 Based on this study’s findings, clinicians should consider evaluating patients who present with more than 3 months of physical pain or IBS for PTSD and referring those with PTSD for care. In addition, effective PTSD treatment may improve pain. Extensive literature suggests that treating depressive symptoms can improve pain and disability.77–81
An unexpected finding was the lower PTSD prevalence among immigrants. The study eligibility requirement to speak English likely selected acculturated immigrants, producing a “healthy immigrant effect”.82 Immigrants in this study had more social support as well. Other studies suggest lower psychiatric morbidity among some immigrant groups, depending on home country, socioeconomic status and subsequent adjustment to their adopted land.83 Additionally, it is likely that immigrants with PTSD would have had substantial barriers to learning English fluently enough to participate in this study.84 Future studies should examine both English and non-English speaking immigrants for PTSD to better understand its prevalence.
The prevalence of PTSD in these urban primary care patients was markedly higher than that found in most other studies of primary care settings, including those involving veterans, where PTSD prevalence is expected to be high.14,15,18,19,21,31,37,85 Possible explanations for this population’s high PTSD prevalence are rooted in its socioeconomic profile with high exposure to trauma and low levels of social support. In a recent study of high school students in Boston, 71% witnessed violence and 44% were directly victimized in the prior year.86 Social support is an important source of protection from the development of PTSD after trauma exposure,87–90 and several demographic characteristics can serve as proxies for social support in this study. For example, half of our participants earned less than $20,000 per year. Likewise, half of the participants, all of whom were of working age, were unemployed or disabled. In addition, only 27% were married or living with a partner.91,92
There were limitations to this study. As a diagnostic instrument, the CIDI PTSD module only assessed for symptoms after one trauma selected as most stressful by the participant, whereas other diagnostic interviews assessed for symptoms after multiple traumas, offering more opportunities for PTSD diagnosis. However, the instrument used in this study is the same or very similar to those instruments used in national PTSD studies.12,13 Our sample was drawn from a single hospital care system whose mission is to serve vulnerable populations and may not represent settings with a broader range of patients. However, our sample is similar to other urban medical settings serving low-income populations in demographic characteristics as well as prevalence of: depression, trauma exposure, substance-use disorders, and co-occurring chronic conditions.16,93–97 Further research in primary care settings serving other populations is warranted. Lastly, the prevalence would only apply to patients aged 18–65 years old presenting for care, not to a population of all primary care patients.
Despite these limitations, the study had numerous strengths. We enrolled a large primary care sample of patients, oversampled for less prevalent comorbid conditions of interest, utilized a well-regarded structured diagnostic interview for PTSD, and analyzed data with multivariable approaches. These methodological features address some of the concerns with prior studies of PTSD prevalence in primary care.
Our results underscore the need to focus on the identification and treatment of PTSD in urban primary care settings as well as to explore the relationship between PTSD and certain conditions (chronic pain, IBS, SD, heavy drinking, depression, anxiety, and immigrant status) in varied settings with lower baseline PTSD prevalence. Before recommending broad screening for PTSD, screening tools and interventions in the primary care setting need to be developed and tested. In the meantime, it is appropriate for primary care clinicians treating patients in high-risk areas, particularly those with the conditions identified in this study, to assess for PTSD and refer those identified to effective care.
Acknowledgments
This work was supported by a Generalist Physician Faculty Scholar Award from the Robert Wood Johnson Foundation, Princeton, New Jersey (RWJF #045452) and by a career development award from the National Institute on Drug Abuse, National Institutes of Health (K23 DA016665).
We thank Jessica Geier, Minga Claggett-Borne, Lauren Kelly, Michael Rosas, Mary Reyes, Pavan Sekhar, Jen Tran, Eric Holder, and Mary Benitta Schickel for their aid in data collection, and Joann Elmore (MD MPH), Roger Weiss (MD), and Larry Culpepper (MD) for their comments on research design and analysis.
Conflict of Interest Summary None disclosed.
Appendix
Table 4.
Trauma exposure of participants recruited in primary care (consecutive sample)
| Traumatic event | Total (N = 509) | Male (N = 251) | Female (N = 258) |
|---|---|---|---|
| N (%) | |||
| Witness someone being badly injured or killed* | 233 (46) | 150 (60) | 83 (32) |
| Seriously physically attacked or assaulted† | 209 (41) | 120 (48) | 89 (35) |
| Threatened with a weapon, held captive, kidnapped* | 191 (38) | 127 (51) | 64 (25) |
| Life-threatening accident* | 163 (32) | 98 (39) | 65 (25) |
| Fire, flood, other natural disaster* | 112 (22) | 61 (24) | 51 (20) |
| Sexually molested* | 104 (20) | 31 (12) | 73 (28) |
| Raped† | 80 (16) | 11 (4) | 69 (27) |
| Violent death of family/friend** | 66 (13) | 30 (12) | 36 (14) |
| Violent acts to family/friend** | 60 (12) | 29 (12) | 31 (12) |
| Non-violent death of family/friend** | 57 (11) | 31 (12) | 26 (10) |
| Sexual violence to family/friend** | 41 (8) | 15 (6) | 26 (10) |
| Tortured or victim of terrorism* | 23 (5) | 12 (5) | 11 (4) |
| Direct combat experience in a war* | 17 (3) | 9 (4) | 8 (3) |
| Health complications/illness | 16 (3) | 9 (4) | 7 (3) |
| Accident (non-life-threatening) | 17 (3) | 11 (4) | 6 (2) |
| Natural disaster to family/friend** | 10 (2) | 4 (2) | 6 (2) |
All traumas met the DSM-IV criterion A for PTSD: sudden, violent, or unexpected with corresponding horror, helplessness, or fear for one’s life. Some included events occurring to a person close to the participant as per DSM-IV. Only trauma exposures reported by >2% participants are listed.
*N = 508
†N = 507
**Event occurred to person close to participant.
Footnotes
Portions of this work were presented at the annual meeting of the Society of General Internal Medicine, May 2005, New Orleans, LA, at the annual meeting of the College on Problems of Drug Dependence, June 2005, Orlando, FL, and at the annual meeting of the American Public Health Association, November 2004, Washington, DC.
References
- 1.Yehuda R. Post-traumatic stress disorder. N Engl J Med. 2002;346(2):108–14 (Jan 10). [DOI] [PubMed]
- 2.Goode E. A nation challenged: psychological trauma. The New York Times. September 18, 2001;B:1.
- 3.Mishra R. Mental toll on troops detailed. The Boston Globe. July 1, 2004:A1.
- 4.Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023–32 (Mar 1). [DOI] [PubMed]
- 5.Weisler RH, Barbee JG, Townsend MH. Mental health and recovery in the Gulf Coast after Hurricanes Katrina and Rita. JAMA. 2006;296(5):585–8. [DOI] [PubMed]
- 6.Centers for Disease Control and Prevention. Health hazard evaluation of police officers and firefighters after Hurricane Katrina, New Orleans, Louisiana, October 17–28 and November 30–December 5, 2005: Centers for Disease Control and Prevention; 2006. [PubMed]
- 7.Lamberg L. Katrina survivors strive to reclaim their lives. JAMA. 2006;296(5):499–502. [DOI] [PubMed]
- 8.American Psychiatric Association, ed. Diagnostic and Statistical Manual of Mental Disorders Fourth Edition. Washington, DC: American Psychiatric Association; 1994.
- 9.Mollica RF, Cardozo BL, Osofsky HJ, Raphael B, Ager A, Salama P. Mental health in complex emergencies. Lancet. 2004;364(9450):2058–67 (Dec 4–10). [DOI] [PubMed]
- 10.Murray CJ, Lopez AD, eds. The global burden of disease: a comprehensive assessment of mortality and disability from diseases, injuries and risk factors in 1990 and projected to 2020. Cambridge, MA: Harvard University Press; 1996; No. 1.
- 11.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. [DOI] [PubMed]
- 12.Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048–60. [DOI] [PubMed]
- 13.Breslau N, Kessler R, Chilcoat H, Schultz L, Davis G, Andreski P. Trauma and posttraumatic stress disorder in the community: The 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998; 55:626–32. [DOI] [PubMed]
- 14.Stein M, McQuaid J, Pedrelli P, Lenox R, McCahill M. Posttraumatic stress disorder in the primary care medical setting. Gen Hosp Psychiatry. 2000;22:261–9. [DOI] [PubMed]
- 15.Taubman-Ben-Ari O, Rabinowitz J, Feldman D, Vaturi R. Post-traumatic stress disorder in primary care settings: prevalence and physicians’ detection. Psychol Med. 2001;31:555–60. [DOI] [PubMed]
- 16.Alim TN, Graves E, Mellman TA, Aigbogun N. Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. J Natl Med Assoc. 2006;98(10):1630–6. [PMC free article] [PubMed]
- 17.Magruder KM, Frueh BC, Knapp RG, et al. Prevalence of posttraumatic stress disorder in Veterans Affairs primary care clinics [see comment]. Gen Hosp Psychiatry. 2005;27(3):169–79. [DOI] [PubMed]
- 18.Escalona R, Achilles G, Waitzkin H, Yager J. PTSD and somatization in women treated at a VA primary care clinic. Psychosomatics. 2004;45(4):291–6 (Jul–Aug). [DOI] [PubMed]
- 19.Zlotnick C, Rodriguez BF, Weisberg RB, et al. Chronicity in posttraumatic stress disorder and predictors of the course of posttraumatic stress disorder among primary care patients. J Nerv Ment Dis. 2004;192(2):153–9 (Feb). [DOI] [PubMed]
- 20.Weisberg RB, Bruce SE, Machan JT, Kessler RC, Culpepper L, Keller MB. Nonpsychiatric illness among primary care patients with trauma histories and posttraumatic stress disorder. Psychiatr Serv. 2002;53(7):848–54 (Jul). [DOI] [PubMed]
- 21.Samson AY, Bensen S, Beck A, Price D, Nimmer C. Posttraumatic stress disorder in primary care. J Fam Pract. 1999;48(3):222–7. [PubMed]
- 22.Breslau N, Davis GC, Andreski P. Risk factors for PTSD-related traumatic events: a prospective analysis. Am J Psychiatry. 1995;152(4):529–35. [DOI] [PubMed]
- 23.Edlund MJ, Unutzer J, Wells KB. Clinician screening and treatment of alcohol, drug, and mental problems in primary care: results from healthcare for communities. Med Care. 2004;42(12):1158–66 (Dec). [DOI] [PubMed]
- 24.Walker EA, Katon W, Russo J, Ciechanowski P, Newman E, Wagner AW. Health care costs associated with posttraumatic stress disorder symptoms in women. Arch Gen Psychiatry. 2003;60(4):369–74. [DOI] [PubMed]
- 25.Calhoun PS, Bosworth HB, Grambow SC, Dudley TK, Beckham JC. Medical service utilization by veterans seeking help for posttraumatic stress disorder. Am J Psychiatry. 2002;159(12):2081–6 (Dec). [DOI] [PubMed]
- 26.Spertus IL, Yehuda R, Wong CM, Halligan S, Seremetis SV. Childhood emotional abuse and neglect as predictors of psychological and physical symptoms in women presenting to a primary care practice. Child Abuse Negl. 2003;27(11):1247–58 (Nov). [DOI] [PubMed]
- 27.Andreski P, Chilcoat H, Breslau N. Post-traumatic stress disorder and somatization symptoms: a prospective study. Psychiatry Res. 1998;79(2):131–8 (Jun 15). [DOI] [PubMed]
- 28.Asmundson GJ, Coons MJ, Taylor S, Katz J. PTSD and the experience of pain: research and clinical implications of shared vulnerability and mutual maintenance models. Can J Psychiatry. 2002;47(10):930–7. [DOI] [PubMed]
- 29.Bryant RA, Marosszeky JE, Crooks J, Baguley IJ, Gurka JA. Interaction of posttraumatic stress disorder and chronic pain following traumatic brain injury. J Head Trauma Rehabil. 1999;14(6):588–94. [DOI] [PubMed]
- 30.Otis JD, Keane TM, Kerns RD. An examination of the relationship between chronic pain and post-traumatic stress disorder. J Rehabil Res Dev. 2003;40(5):397–405. [DOI] [PubMed]
- 31.Frayne SM, Seaver MR, Loveland S, et al. Burden of medical illness in women with depression and posttraumatic stress disorder. Arch Intern Med. 2004;164(12):1306–12. [DOI] [PubMed]
- 32.Bonin MF, Norton GR, Asmundson GJ, Dicurzio S, Pidlubney S. Drinking away the hurt: the nature and prevalence of PTSD in substance abuse patients attending a community-based treatment program. J Behav Ther Exp Psychiatry. 2000;31(1):55–66 (Mar). [DOI] [PubMed]
- 33.Rodriguez BF, Weisberg RB, Pagano ME, Machan JT, Culpepper L, Keller MB. Mental health treatment received by primary care patients with posttraumatic stress disorder. J Clin Psychiatry. 2003;64(10):1230–6. [DOI] [PMC free article] [PubMed]
- 34.Smith MV, Rosenheck RA, Cavaleri MA, Howell HB, Poschman K, Yonkers KA. Screening for and detection of depression, panic disorder, and PTSD in public-sector obstetric clinics. Psychiatr Serv. 2004;55(4):407–14 (Apr). [DOI] [PubMed]
- 35.Hankin CS, Spiro A, 3rd, Miller DR, Kazis L. Mental disorders and mental health treatment among U.S. Department of Veterans Affairs outpatients: the Veterans Health Study. Am J Psychiatry. 1999;156(12):1924–30 (Dec). [DOI] [PubMed]
- 36.Kubany ES, McKenzie WF, Owens JA, Leisen MB, Kaplan AS, Pavich E. PTSD among women survivors of domestic violence in Hawaii. Hawaii Med J. 1996;55(9):164–5 (Sep). [PubMed]
- 37.Davis TM, Wood PS. Substance abuse and sexual trauma in a female veteran population. J Subst Abuse Treat. 1999;16(2):123–7. [DOI] [PubMed]
- 38.Najavits LM, Weiss RD, Shaw SR. The link between substance abuse and posttraumatic stress disorder in women. A research review. Am J Addict. 1997;6(4):273–83. [PubMed]
- 39.Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug Alcohol Depend. 2005;77(3):251–8 (Mar 7). [DOI] [PubMed]
- 40.Brown PJ, Recupero PR, Stout R. PTSD substance abuse comorbidity and treatment utilization. Addict Behav. 1995;20(2):251–4 (Mar–Apr). [DOI] [PubMed]
- 41.Drossman DA, Leserman J, Nachman G, et al. Sexual and physical abuse in women with functional or organic gastrointestinal disorders. Ann Intern Med. 1990;113:828–33. [DOI] [PubMed]
- 42.Drossman DA, Talley NJ, Leserman J, Olden KW, Barreiro MA. Sexual and physical abuse and gastrointestinal illness: review and recommendations. Ann Intern Med. 1995;123:782–94. [DOI] [PubMed]
- 43.Holman EA, Silver RC, Waitzkin H. Traumatic life events in primary care patients: a study in an ethnically diverse sample. Arch Fam Med. 2000;9(9):802–10 (Sept/Oct). [DOI] [PubMed]
- 44.Force UPST. Guide to Clinical Preventive Services, 2nd Edition. Bethesda, MD; 1996.
- 45.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–44. [DOI] [PubMed]
- 46.Drossman DA, Corazziari E, Talley NJ, Thompson WG, Whitehead WE. Rome II. The Functional Gastrointestinal Disorders. Diagnosis, Pathophysiology and Treatment: A Multinational Consensus. McLean, VA: Degnon Associates; 2000.
- 47.NIAAA. Helping Patients Who Drink Too Much: A Clinician’s Guide. http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/clinicians_guide.htm; 2006.
- 48.Purves AM, Penny KI, Munro C, et al. Defining chronic pain for epidemiological research assessing a subjective definition. Pain Clinic. 1998;10(3):139–47.
- 49.World Health Organization. Composite International Diagnostic Interview (CIDI): Version 2.1. Geneva: World Health Organization; 1997.
- 50.Kessler R, Andrews G, Mroczek D, Ustun B, Wittchen HU. The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF). Int J Methods Psychiatr Res. 1998;7(4):171–85. [DOI]
- 51.Health, United States, 2004 With Chartbook on Trends in the Health of Americans. Hyattsville, MD: National Center for Health Statistics; 2004. [PubMed]
- 52.Dobie DJ, Kivlahan DR, Maynard C, Bush KR, Davis TM, Bradley KA. Posttraumatic stress disorder in female veterans: association with self-reported health problems and functional impairment. Arch Intern Med. 2004;164(4):394–400 (Feb 23). [DOI] [PubMed]
- 53.Sherman JJ, Turk DC, Okifuji A. Prevalence and impact of posttraumatic stress disorder-like symptoms on patients with fibromyalgia syndrome. Clin J Pain. 2000;16(2):127–34 (Jun). [DOI] [PubMed]
- 54.Engel CC, Jr., Liu X, McCarthy BD, Miller RF, Ursano R. Relationship of physical symptoms to posttraumatic stress disorder among veterans seeking care for gulf war-related health concerns. Psychosom Med. 2000;62(6):739–45 (Nov–Dec). [DOI] [PubMed]
- 55.Asmundson GJ, Wright KD, Stein MB. Pain and PTSD symptoms in female veterans. Eur J Pain. 2004;8(4):345–50 (Aug). [DOI] [PubMed]
- 56.Amir M, Kaplan Z, Neumann L, Sharabani R, Shani N, Buskila D. Posttraumatic stress disorder, tenderness and fibromyalgia. J Psychosom Res. 1997;42(6):607–13 (Jun). [DOI] [PubMed]
- 57.Lauterbach D, Vora R, Rakow M. The relationship between posttraumatic stress disorder and self-reported health problems. Psychosom Med. 2005;67(6):939–47 (Nov–Dec). [DOI] [PubMed]
- 58.Beckham J, Crawford A, Feldman ME, et al. Chronic posttraumatic stress disorder and chronic pain in Vietnam combat veterans. J Psychiatr Res. 1997;43(4):379–89. [DOI] [PubMed]
- 59.Frayne SM, Skinner KM, Sullivan LM, et al. Medical profile of women Veterans Administration outpatients who report a history of sexual assault occurring while in the military. J Womens Health Gend Based Med. 1999;8(6):835–45 (Jul–Aug). [DOI] [PubMed]
- 60.Liebschutz JM, Feinman G, Sullivan L, Stein MD, Samet J. Physical and sexual abuse in women infected with the human immunodeficiency virus: increased illness and health care utilization. Arch Intern Med. 2000;160:1659–64. [DOI] [PubMed]
- 61.Liebschutz JM, Mulvey KP, Samet JH. Victimization among substance-abusing women: worse health outcomes. Arch Intern Med. 1997;157:1093–97. [DOI] [PubMed]
- 62.Sharp TJ, Harvey AG. Chronic pain and posttraumatic stress disorder: mutual maintenance? Clin Psychol Rev. 2001;21(6):857–77 (Aug). [DOI] [PubMed]
- 63.Griffin MG, Resick PA, Yehuda R. Enhanced cortisol suppression following dexamethasone administration in domestic violence survivors. Am J Psychiatry. 2005;162(6):1192–9 (Jun). [DOI] [PMC free article] [PubMed]
- 64.Nixon RD, Bryant RA, Moulds ML, Felmingham KL, Mastrodomenico JA. Physiological arousal and dissociation in acute trauma victims during trauma narratives. J Trauma Stress. 2005;18(2):107–13 (Apr). [DOI] [PubMed]
- 65.Zlotnick C, Bruce SE, Weisberg RB, Shea MT, Machan JT, Keller MB. Social and health functioning in female primary care patients with post-traumatic stress disorder with and without comorbid substance abuse. Compr Psychiatry. 2003;44(3):177–83. [DOI] [PubMed]
- 66.Jacobsen LK, Southwick SM, Kosten TR. Substance use disorders in patients with posttraumatic stress disorder: a review of the literature. Am J Psychiatry. 2001;158(8):1184–90. [DOI] [PubMed]
- 67.Brady KT, Sinha R. Co-occurring mental and substance use disorders: the neurobiological effects of chronic stress. Am J Psychiatry. 2005;162(8):1483–93. [DOI] [PubMed]
- 68.Bremner JD, Southwick SM, Darnell A, Charney DS. Chronic PTSD in Vietnam combat veterans: course of illness and substance abuse. Am J Psychiatry. 1996;153(3):369–75. [DOI] [PubMed]
- 69.Bruce SE, Weisberg RB, Dolan RT, et al. Trauma and posttraumatic stress disorder in primary care patients. Prim Care Companion J Clin Psychiat. 2001;3(5):211–7 (Oct). [DOI] [PMC free article] [PubMed]
- 70.Kessler RC, Berglund P, Demler O, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289(23):3095–105 (Jun 18). [DOI] [PubMed]
- 71.Wang PS, Berglund P, Kessler RC. Recent care of common mental disorders in the United States: prevalence and conformance with evidence-based recommendations. J Gen Intern Med. 2000;15(5): 284–92. [DOI] [PMC free article] [PubMed]
- 72.Oquendo MA, Malone KM, Ellis SP, Sackeim HA, Mann JJ. Inadequacy of antidepressant treatment for patients with major depression who are at risk for suicidal behavior. Am J Psychiatry. 1999;156(2):190–4. [DOI] [PubMed]
- 73.Seong-Yi B, Bowers B, Oakley L, Susman J. The recognition of depression: the primary care clinician’s perspective. Ann Fam Med. 2005;3:31–7. [DOI] [PMC free article] [PubMed]
- 74.Foa EB, Davidson JRT, Frances A. The expert consensus guideline series: treatment of post-traumatic stress disorder. J Clin Psychiatry. 1999;60(suppl 16):1–76. [PubMed]
- 75.Bradley R, Greene J, Russ E, Dutra L, Westen D. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry. 2005;162(2):214–27 (Feb). [DOI] [PubMed]
- 76.Institute of Medicine, ed. Improving the Quality of Health Care for Mental and Substance Use Conditions: Quality Chasm Series. Washington, DC: The National Academies Press; 2006. [PubMed]
- 77.Katzelnick DJ, Simon GE, Pearson SD, et al. Randomized trial of a depression management program in high utilizers of medical care. Arch Fam Med. 2000;9(4):345–51 (Apr). [DOI] [PubMed]
- 78.Lin EH, Katon W, Von Korff M, et al. Effect of improving depression care on pain and functional outcomes among older adults with arthritis: a randomized controlled trial. JAMA. 2003;290(18):2428–29 (Nov 12). [DOI] [PubMed]
- 79.Simon GE, Katon W, Rutter C, et al. Impact of improved depression treatment in primary care on daily functioning and disability. Psychol Med. 1998;28(3):693–701 (May). [DOI] [PubMed]
- 80.Von Korff M, Balderson BH, Saunders K, et al. A trial of an activating intervention for chronic back pain in primary care and physical therapy settings. Pain. 2005;113(3):323–30 (Feb). [DOI] [PubMed]
- 81.Lin EH, VonKorff M, Russo J, et al. Can depression treatment in primary care reduce disability? A stepped care approach. Arch Fam Med. 2000;9(10):1052–8 (Nov–Dec). [DOI] [PubMed]
- 82.Newbold KB. Self-rated health within the Canadian immigrant population: risk and the healthy immigrant effect. Soc Sci Med. 2005;60(6):1359–70. [DOI] [PubMed]
- 83.Chen AW, Kazanjian A. Rate of mental health service utilization by Chinese immigrants in British Columbia. Can J Public Health. 2005;96(1):49–51. [DOI] [PMC free article] [PubMed]
- 84.Marshall GN, Schell TL, Elliott MN, Berthold SM, Chun CA. Mental health of Cambodian refugees 2 decades after resettlement in the United States. JAMA. 2005;294(5):571–9. [DOI] [PubMed]
- 85.Dobie DJ, Maynard C, Kivlahan DR, et al. Posttraumatic stress disorder screening status is associated with increased VA medical and surgical utilization in women. J Gen Intern Med. 2006;21(suppl 3):S58–S64 (Mar). [DOI] [PMC free article] [PubMed]
- 86.Hemenway D, Prothrow-Stith D, Browne A. Report of the 2004 Boston Youth Survey. Boston: City of Boston; 2005 (Aug).
- 87.Ahern J, Galea S, Fernandez WG, Koci B, Waldman R, Vlahov D. Gender, social support, and posttraumatic stress in postwar Kosovo. J Nerv Ment Dis. 2004;192(11):762–70. [DOI] [PubMed]
- 88.Glynn SM, Asarnow JR, Asarnow R, et al. The development of acute post-traumatic stress disorder after orofacial injury: a prospective study in a large urban hospital. J Oral Maxillofac Surg. 2003;61(7):785–92. [DOI] [PubMed]
- 89.Muller RT, Goebel-Fabbri AE, Diamond T, Dinklage D. Social support and the relationship between family and community violence exposure and psychopathology among high risk adolescents. Child Abuse Negl. 2000;24(4):449–64. [DOI] [PubMed]
- 90.Viinamaki H, Kontula O, Niskanen L, Koskela K. The association between economic and social factors and mental health in Finland. Acta Psychiatr Scand. 1995;92(3):208–13. [DOI] [PubMed]
- 91.Steptoe A, Marmot M. Burden of psychosocial adversity and vulnerability in middle age: associations with biobehavioral risk factors and quality of life. Psychosom Med. 2003;65(6):1029–37. [DOI] [PubMed]
- 92.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–14. [DOI] [PubMed]
- 93.Miller DK, Malmstrom TK, Joshi S, Andresen EM, Morley JE, Wolinsky FD. Clinically relevant levels of depressive symptoms in community-dwelling middle-aged African Americans. J Am Geriatr Soc. 2004;52(5):741–8. [DOI] [PubMed]
- 94.Matheson FI, Moineddin R, Dunn JR, Creatore MI, Gozdyra P, Glazier RH. Urban neighborhoods, chronic stress, gender and depression. Soc Sci Med. 2006;63(10):2604–16. [DOI] [PubMed]
- 95.O’Toole TP, Arbelaez JJ, Lawrence RS; Baltimore Community Health Consortium. Medical debt and aggressive debt restitution practices: predatory billing among the urban poor. J Gen Intern Med. 2004;19(7):772–8. [DOI] [PMC free article] [PubMed]
- 96.Gaskin DJ, Hadley J. Population characteristics of markets of safety-net and non-safety-net hospitals. J Urban Health. 1999;76(3):351–70. [DOI] [PMC free article] [PubMed]
- 97.Bassuk EL, Buckner JC, Perloff JN, Bassuk SS. Prevalence of mental health and substance use disorders among homeless and low-income housed mothers. Am J Psychiatry. 1998;155(11):1561–4. [DOI] [PubMed]


