Abstract
BACKGROUND
In January 2003, people covered by Oregon’s Medically Needy program lost benefits owing to state budget shortfalls. The Medically Needy program is a federally matched optional Medicaid program. In Oregon, this program mainly provided prescription drug benefits.
OBJECTIVE
To describe the Medically Needy population and determine how benefit loss affected this population’s health and prescription use.
DESIGN
A 49-question telephone survey instrument created by the research team and administered by a research contractor.
PARTICIPANTS
A random sample of 1,269 eligible enrollees in Oregon’s Medically Needy Program. Response rate was 35% with 439 individuals, ages 21–91 and 64% women, completing the survey.
MEASUREMENTS
Demographics, health information, and medicatication use at the time of the survey obtained from the interview. Medication use during the program obtained from administrative data.
RESULTS
In the 6 months after the Medically Needy program ended, 75% had skipped or stopped medications. Sixty percent of the respondents had cut back on their food budget, 47% had borrowed money, and 49% had skipped paying other bills to pay for medications. By self-report, there was no significant difference in emergency department visits, but a significant decrease in hospitalizations comparing 6 months before and after losing the program. Two-thirds of respondents rated their current health as poor or fair.
CONCLUSIONS
The Medically Needy program provided coverage for a low-income, chronically ill population. Since its termination, enrollees have decreased prescription drug use and increased financial burden. As states make program changes and Medicare Part D evolves, effects on vulnerable populations must be considered.
KEY WORDS: prescription drugs, vulnerable populations, survey research
INTRODUCTION
Previous studies have documented decreased medication use and financial burden of increasing copayments for prescription drugs.1–6 Losing health insurance coverage also has been shown to result in decreased drug use and worse health.7,8 Low-income people with high medical costs and without health insurance are at particularly high risk of cost-related medication noncompliance with even small amounts of cost-sharing.9–13 In 1 large survey, 35% of all seniors without prescription drug coverage and 42% of seniors with incomes less than 200% of the federal poverty level reported discontinuing a prescription; 21% of low-income seniors reported spending less on rent or food to pay for their prescriptions.4
People who are covered by Medically Needy programs are not well characterized nationally or on a local level, and little is known about their health care needs.14 The Medically Needy program is a federally matched optional program in which states may choose to provide Medicaid coverage or Medicare premium assistance, or both, to certain groups not otherwise eligible for Medicaid but who have significant health care needs.14 Thirty-five states currently offer Medically Needy programs, and most offer access to full Medicaid benefits in that state. For most Medicaid categories, having income above a specified level automatically disqualifies an individual from Medicaid, but in Medically Needy programs individuals can qualify for state assistance through a mechanism called “spending-down.” Each state has its own predetermined level of “spending-down” and income limits.14
In Oregon from 1991–2003, eligibility for the Medically Needy program was determined prospectively on a monthly basis. An individual subtracted his or her qualifying medical expenses for a given month from countable income for that same month. If the difference was at or below the Medically Needy income limit of $413, the individual then qualified for program benefits for that month.15 Oregon’s Medically Needy coverage was limited to prescription drugs, some medical transportation, and partial mental health and chemical dependency coverage. There were no copays, cost-sharing, formularies, or other restrictions on drug type, and many enrollees were consistently enrolled in the program because of recurring medical expenses, like prescriptions.15 As of January 2003, 8,750 people were covered under Oregon’s Medically Needy program.15 Prescription drug coverage accounted for 88% of program expenditures. On January 31, 2003, people covered by Oregon’s program lost their health benefits owing to state budget financial shortfalls. This change, decided by the legislature at the beginning of January, was unexpected, and occurred 2 years before Medicare Part D benefits began.16 Temporary coverage programs were created for people with transplants and HIV/AIDS.
The Office of Medical Assistance Programs (OMAP) and the Office for Oregon Health Plan Policy and Research (OHPPR) wanted to learn more about the Medically Needy population to inform policy decisions for this population’s future health benefits. Because the program was primarily a prescription drug benefit and most beneficiaries were covered by Medicare, its termination was seen as an opportunity to examine the impact of losing prescription drug coverage and to consider new prescription benefit changes, particularly because this was before Medicare Part D. Our primary objective was to describe the Medically Needy population and determine how the loss of benefits affected this population’s health care use. Secondary objectives included investigating how patients changed medication use and their finances after prescription benefits loss. We hypothesized benefit loss would result in prescription use changes that would adversely affect health status and lead to an increase in health care use.
METHODS
A telephone survey of a statewide, random sample of people enrolled in the Medically Needy program in January 2003 and without subsequently acquired Medicaid benefits was conducted in August 2003, 6 months after the program’s termination. We created the 49-question survey instrument with the assistance of OMAP and OHPPR, using primarily standardized and validated questions from the National Health Interview Survey and the Behavioral Risk Factor Surveillance Survey.17–20 The instrument included questions about demographic information, insurance coverage, health conditions, access to care, prescription drug use, and health care use. For adequate power to detect a 10% change in health care use after the program’s end, 400 completed surveys were needed. OMAP drew a random sample of 1,269 people from the 7,550 program participants in January 2003 meeting the following criteria: over age 18, without current Medicaid benefits, a phone number on record before the program’s end, and English-speaking. This study was approved by OHSU’s institutional review board and all respondents gave informed consent.
We obtained data about study participants’ medication use during the Medically Needy program from OMAP administrative data for January 2003 to represent use during the program. We examined medication fills and expected some early refills by people anticipating the program’s end. These duplicate fills, which represented 12–16% of prescriptions, were deleted. Medication use at the time of the survey was obtained from the interview. OMAP benefits at the time of the survey were obtained from OMAP administrative data. We used t tests and χ2 analyses to compare the sample to the total Medically Needy population, and to compare changes in medications and utilization.
RESULTS
Respondent Demographics
From the sample of 1269, 279 (22%) had incorrect phone numbers, 444 (35%) were noncontacts after 10 attempts (including attempts during nights and weekends), and 105 (8%) refused, giving a response rate of 35% (439 people). In our surveyed population, the average age was 58, 64% were women; the sample was predominately White, and 95% unemployed. Nineteen percent completed less than high school, slightly lower than average Oregonians (26%). Sixty percent of the surveyed population reported gross household incomes of less than $10,000 per year. We estimated 70–75% of this population was under 135% of the Federal Poverty Level (FPL). Comparing the sample to the total population, the surveyed population consisted of significantly more women, was older with lower incomes, and other differences were not significant (Table 1).
Table 1.
Survey Respondent and Oregon Medically Needy Population Comparative Demographics
| Demographics | Medically Needy population (n = 8,750) | Survey responders (n = 439) | P value |
|---|---|---|---|
| Female | 56% | 64% | <.01 |
| Age | 56 | 58 (range 22–91) | <.01 |
| Under 65 | 70% | 65% | |
| 65 or over | 30% | 34% | |
| Education | n/a | ||
| Less than high school | n/a | 19% | |
| High school diploma or GED | n/a | 31% | |
| More than high school | n/a | 48% | |
| Race | .74 | ||
| White | 92% | 92% | |
| American Indian/Alaskan Native | 1% | 3% | |
| Black or African American | 3% | 2% | |
| Hispanic, Spanish or Latino | 2% | 2% | |
| Employed | n/a | 5% | n/a |
| Gross household income | Ave. Income 9,494 | <.01 | |
| Under $5,000 | 2% | 7% | |
| $5,000–$9,999 | 59% | 53% | |
| $10,00–14,999 | 25% | 24% | |
| $15,000–19,999 | 13% | 4% | |
| Over $20,000 | 2% | 3% | |
| Covered by Medicare | 95% | 92% | .17 |
Health Insurance Coverage
Ninety-two percent of the surveyed population had Medicare coverage owing to age or permanent disability, similar to the total Medically Needy population.15 Twenty-one percent reported coverage by another type of health insurance, but only 33 people (7.5%) reported having prescription drug coverage after the Medically Needy program ended.
Depending on insurance coverage, there can be many medically related out-of-pocket costs including copayments, deductibles, and medical equipment. Respondents were asked how much they had spent in the last 6 months on medical care not including prescriptions or dental costs. Twenty-seven percent spent nothing on medical care in the last 6 months, 39% spent up to $500, and the remaining 34% spent more than $500. Thirty-nine percent of those surveyed currently owed outstanding health care bills—13% with less than $100 unpaid, 30% owed $101–$500, 36% owed $501–$5,000, and 21% owed more than $5,000. Of those sampled, 12% had filed for bankruptcy in the past because of medical bills.
Chronic Medical Conditions/Medical Care
Respondents were asked about their perception of their overall health status and how it compared to their status 1 year before. Over two-thirds of people rated their current health as poor (32%) or fair (36%), whereas only 2% rated it excellent and 5% very good. Compared to the prior year, 44% rated their health as worse, 39% as about the same, and 17% as better.
Questions about health problems and medical care were asked to assess disease burden and usual medical care; all health conditions were self-reported. The majority of respondents reported having hypertension (59%); asthma (31%) and diabetes (28%) were also common. Respondents had an average of 3.5 chronic diseases with a range of 0 to 25 chronic conditions; only 2% reported no chronic diseases. Self-reported medical conditions were grouped by system with the exception of hypertension, the most common disease in this population. The second most prevalent category was mental health conditions (54%), including depression, schizophrenia, bipolar disorder, posttraumatic stress disorder, and panic disorder. The prevalence of pulmonary diseases was 43% and rheumatologic disease 25%. Twenty percent reported other conditions categorized as pain disorders. Coronary disease, the most common cause of hospitalizations in this population, affected 17%, whereas congestive heart failure was present in 2%.
Prescription Drugs
The major benefit this population lost with the Medically Needy program’s end was prescription drug coverage. The number of people taking prescriptions and the average number of prescriptions per person increased after the program ended, but not significantly (Table 2). Medications were grouped both by class and by disease category. By self-report, the most frequently used categories of medications were mental health drugs (21% of all prescriptions), antihypertensives (19%), and pain medications (10%).
Table 2.
Changes after Medically Needy Program’s End
| N = 439 | With Medically Needy | After Medically Needy | P value |
|---|---|---|---|
| Number of medications | 5.6 (range 0–27) | 5.8 (range 0–20) | .59 |
| Location of medical care | <.01 | ||
| Private office/clinic | 87% (382) | 84% (369) | |
| County/community/migrant clinic | 12% (52) | 9% (40) | |
| Emergency department/Urgent care | 1%(5) | 5% (21) | |
| Number of ED visits | 422 | 430 | .46 |
| Number of hospitalizations | 227 | 179 | .04 |
| Reasons hospitalized | .64 | ||
| Heart disease | 21% (48) | 22% (39) | |
| Mental health | 9% (20) | 11% (20) | |
| Pneumonia | 9% (20) | 10% (18) | |
| Out-of-pocket costs for prescriptions per month | <.01 | ||
| Nothing | 100% | 8% | |
| $1–50 | 0% | 20% | |
| $51–100 | 0% | 20% | |
| $101–200 | 0% | 17% | |
| Over $200 | 0% | 27% | |
Survey respondents were asked about how loss of prescription coverage changed their medication use or impacted their daily lives. Seventy-five percent of respondents reported not taking 1 or more prescriptions because of cost. These individuals reported specific drugs they had skipped or stopped; however, many said they could not list all the prescriptions they had skipped, or had skipped all medications for some period. The types of skipped medications were primarily mental health (17.2%), pain-related (12.5%), and cardiovascular (8.3%) medications, but skipped medications existed in every category. Thirty-six percent reported switching to a similar, lower-cost medication, such as a generic drug. Only a third of those who switched drugs obtained advice from someone to help guide their decision, most often from a health care provider. Besides changing to a lower cost medication, 77% reported some financial burden to pay for their prescription drugs: 60% of all respondents cut back on their food budget, 49% skipped other bills or paid them late, 47% borrowed money from family or friends, and 20% added credit card debt to pay for their medications. As there were no major changes to other social programs, these changes are likely solely because of the Medically Needy program’s loss.
Respondents were asked to estimate their monthly out-of-pocket prescription drugs costs in the last 6 months (Table 2). Because this population’s annual gross income was low, out-of-pocket expenditures often represented a significant proportion of their income. Even the lowest levels of prescription drug spending ($0–50) had impact on food budgets, inability to pay other bills, borrowing money, and incurring credit card debt. The percent of people reporting these impacts increased with more out-of-pocket spending (Fig. 1).
Figure 1.
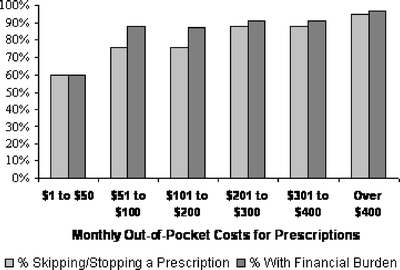
Percentage skipping/stopping a prescription and percentage reporting financial burden by monthly out-of-pocket prescription expense levels.
Healthcare Utilization
Eighty-four percent of this population received their usual medical care through a private doctor’s office or clinic. Thirteen percent reported changing their usual place of care after losing their Medically Needy benefits, mostly moving from a private doctor’s office to a county, community, or migrant clinic, but a few shifted care to an emergency department or urgent care clinic (Table 2).
Respondents were asked to self-report the number of emergency department (ED) visits and the number of hospitalizations for the 6 months before and after the Medically Needy program ended (Table 2). There were 422 total ED visits in the 6 months before the program ended and 430 during the next 6 months, not a significant difference. A subgroup analysis of each of the 3 most common diseases—hypertension, asthma and diabetes—had no difference in ED visits in the 6 months before and after the program’s end. There were 227 total hospitalizations reported in the 6 months before the program ended and 179 after, a statistically significant decrease, but again, no difference was found for subgroups. The most common reasons for hospitalization both before and after the Medically Needy program ended were heart disease, pneumonia, and mental health.
DISCUSSION
Participants in Oregon’s Medically Needy program were vulnerable, very low income people with multiple medical problems. The loss of this program resulted in decreased medication use and increased financial burden, but rates of hospitalizations and ED visits did not increase over 6 months.
This survey was conducted to determine whether there was an early health impact from this benefit’s loss; health status decreased, but use of services did not increase. The finding of similar numbers of ED visits and fewer hospitalizations after the program’s end were surprising in this adequately powered study. There could be many contributing factors to these findings: selection bias if the poorest or sickest people were unable to be contacted, some people had more medications because they obtained multiple refills of their medications in January, people spread out medication use by skipping doses, and 6 months was too short to see an effect on chronic illnesses such as hypertension and diabetes. Finally, as this population was already financially burdened, they may have wanted to avoid additional financial losses by avoiding care in the ED or hospital.7,8
The Medically Needy population in Oregon does not qualify for Medicaid coverage because they do not meet the income threshold (<100% FPL), resource requirement (<$2,000), or Medicaid was capped. In other population surveys of people dually eligible for Medicare and Medicaid with similar ages, income, and educational status, 21% of dual-eligibles report poor health and 17% excellent or very good; this Medically Needy population was more ill with worse reported health status.5,19,21
Survey respondents had average prescription out-of-pocket costs in the range of $100–199 per month so estimated annual average drug costs were $1,200–2,388. Using the average yearly gross income for this population, this translates into 25–50% of their income spent on prescription drugs. It is not surprising many people reported skipping or stopping prescriptions. In this survey, 75% of people reported discontinuing prescriptions owing to cost, whereas other surveys of cost-related noncompliance have reported much lower levels from 18 to 42%.4,22–25 This Medically Needy population reported a large financial burden, whereas in other surveys of low-income seniors, 21–24% reported a prescription-related financial burden, considerably less than the percentage found in this survey.4,25
The Medically Needy population is a group previously not well-defined. Medicare Part D is important for providing drug benefits for this population who does not qualify for Medicaid. Whereas the Medicare Modernization Act (MMA) probably mitigates the impact of this type of program cut, it does not provide the level of prior coverage under the Medically Needy program and has cost-sharing in copayments, premiums, and coverage gaps. Whereas there is greater coverage for individuals under 135% FPL, Part D does not have a “spend down” design to assist the “near poor” chronically ill with large medical and prescription costs, such as those found in Medically Needy programs. This survey and previous studies have shown that increased cost-sharing leads to discontinuing prescriptions, which in turn leads to worsening chronic disease and higher health-related expenditures.13,26–31 The cost-sharing involved with the MMA should be adjusted for income impact or be needs-based because it adversely affects these “near poor” with low incomes and high medical costs.
Limitations
There are several limitations of this survey. This study describes 1 population in 1 state, but it is a population not well described. The sample was limited to English-speaking individuals. There was a 35% response rate, and there were many incorrect telephone numbers, both frequently encountered problems in this type of population. There was potential selection bias if the poorest or sickest were not contacted; however, reported income from the sampled Medically Needy population is lower than that of the total Medically Needy population. Most information about prescription drugs and health care utilization was self-reported and thus could have substantial recall bias. However, past studies have shown for low-income older adults there is a high degree of congruence between self-report and pharmacy data.32–34 Most people read their current medications to the interviewer from a list or the bottles and were able to give strength and frequency for each medicine, so medications at the time of the survey may be reliable. Determining medicines discontinued is less accurate. Regarding self-reporting of ED visits and hospitalizations, all respondents were aware of the date of the program’s cessation. There is potential for bias both in under- or overreporting events as this is based on recollection of past events.
Conclusion
This study suggests the Medically Needy in Oregon were a vulnerable population with worse perceived health status than people dually eligible for Medicare and Medicaid, an otherwise similar demographic population. Losing prescription coverage had immediate impact on prescription use and finances in this population. It may be too early to determine the impact of these changes on health outcomes such as ED visits and hospitalizations. Owing to state budget crises, Medically Needy and Medicaid programs are being changed or cut in many states.35,36 As this study shows, an arbitrary and unexpected cut in benefits for state budgetary reasons can cause unintended adverse health consequences. As the safety net erodes, this vulnerable population is in jeopardy of further health deterioration, and a short-term cost saving for the state likely leads to much higher costs in health care over time for this population. This socioeconomically vulnerable population is likely disproportionally affected by gaps in Medicare Part D coverage and may have further deterioration in health. Further study should examine changes in health and prescription drug use over time, including the impact of the MMA, and provide further information about this frail, chronically ill population.
Acknowledgments
Funding is from the VA HSR&D, RWJ State Coverage Initiatives Grant, RWJ Clinical Scholars Program. This research was supported by the Veteran’s Administration and the Robert Wood Johnson Clinical Scholars Program. The views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs or the Robert Wood Johnson Foundation. The authors would like to acknowledge the assistance of Bruce Goldberg, MD and Rick Deyo, MD. Parts of this paper have been presented at the SGIM national meeting 2004 and Academy Health’s annual meeting 2004.
Conflicts of interest None disclosed
References
- 1.Soumerai SB, Ross-Degnan D. Inadequate prescription-drug coverage for Medicare enrollees—a call to action. N Engl J Med. 1999;340:722–8. [DOI] [PubMed]
- 2.Stuart B, Zacker C. Who bears the burden of Medicaid drug copayment policies? Health Aff (Project Hope). 1999;18:201–12. [DOI] [PubMed]
- 3.Piette JD, Heisler M, Wagner TH. Problems paying out-of-pocket medication costs among older adults with diabetes. Diabetes Care. 2004;27:384–91. [DOI] [PubMed]
- 4.Safran DG. Seniors and prescription drugs: findings from a 2001 survey of seniors in eight states. The Commonwealth Fund/Kaiser Family Foundation/Tufts-New England Medical Center; July 2002.
- 5.Xu KT. Financial disparities in prescription drug use between elderly and nonelderly Americans. Health Aff (Project Hope). 2003;22:210–21. [DOI] [PubMed]
- 6.Tseng CW, Brook RH, Keeler E, Steers WN, Waitzfelder BE, Mangione CM. Effect of generic-only drug benefits on seniors’ medication use and financial burden. Am J Manag Care. 2006;12:525–32. [PubMed]
- 7.Lurie N, Ward NB, Shapiro MF, Brook RH. Termination from Medi-Cal—does it affect health? N Engl J Med. 1984;311:480–4. [DOI] [PubMed]
- 8.Lurie N, Ward NB, Shapiro MF, Gallego C, Vaghaiwalla R, Brook RH. Termination of Medi-Cal benefits. A follow-up study one year later. N Engl J Med. 1986;314:1266–8. [DOI] [PubMed]
- 9.Saver BG, Doescher MP, Jackson JE, Fishman P. Seniors with chronic health conditions and prescription drugs: benefits, wealth, and health. Value Health. 2004;7:133–43. [DOI] [PubMed]
- 10.Kleinke JD. The price of progress: prescription drugs in the health care market. Health Aff (Project Hope). 2001;20:43–60. [DOI] [PubMed]
- 11.Tseng CW, Brook RH, Keeler E, Mangione CM. Impact of an annual dollar limit or “cap” on prescription drug benefits for Medicare patients. JAMA. 2003;290:222–7. [DOI] [PubMed]
- 12.Harris BL, Stergachis A, Ried LD. The effect of drug co-payments on utilization and cost of pharmaceuticals in a health maintenance organization. Med Care. 1990;28:907–17. [DOI] [PubMed]
- 13.Johnson RE, Goodman MJ, Hornbrook MC, Eldredge MB. The effect of increased prescription drug cost-sharing on medical care utilization and expenses of elderly health maintenance organization members. Med Care. 1997;35:1119–31. [DOI] [PubMed]
- 14.Crowley JS, Ashner D, Elam L. Medicaid outpatient prescription drug benefits: findings from a national survey. 2003. Available at: http://www.kff.org/medicaid/4164.cfm. Accessed October 18, 2006.
- 15.Oregon Department of Human Services Memo. Oregon Department of Human Services, State of Oregon; June 2003.
- 16.CMS. Prescription drug coverage: General information 2006. Centers for Medicaid and Medicare Services. Available at: http://www.cms.hhs.gov/PrescriptionDrugCovGenIn/. Accessed October 18, 2006.
- 17.Brodie M, Blendon R. National survey on prescription drugs. Health Desk: A Partnership of the Kaiser Family Foundation and the Newshour with Jim Lehrer; 2000.
- 18.Berk ML, Schur CL, Mohr P. Using survey data to estimate prescription drug costs. Health Aff (Project Hope). 1990;9:146–56. [DOI] [PubMed]
- 19.Barnes PM, Adams PF, Schiller JS. Summary of health statistics for the US population: National Health Interview Survey, 2001. National Center for Health Statistics. Vital Health Stat. 2003;27. [PubMed]
- 20.CDC Behavioral Risk Factor Surveillance System, Centers for Disease Control and Prevention National Center for Chronic Disease Prevention and Health Promotion. 2004. Available at: http://www.cdc.gov/brfss/. Accessed October 18, 2006.
- 21.MedPAC. Dual eligible beneficiaries: an overview. Report to the Congress: New approaches in Medicare, section 3. 2004:71–91.Available at: http://www.medpac.gov/publications/congressional_reports/Jun06DataBookSec3.pdf. Accessed October 18, 2006.
- 22.Cunningham PJ. Medicaid cost containment and access to prescription drugs. Health Aff (Project Hope). 2005;24:780–9. [DOI] [PubMed]
- 23.Piette JD, Heisler M. Problems due to medication costs among VA and non-VA patients with chronic illnesses. Am J Manag Care. 2004;10:861–8. [PubMed]
- 24.Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically ill adults: the treatments people forgo, how often, and who is at risk. Am J Pub Health. 2004;94:1782–7. [DOI] [PMC free article] [PubMed]
- 25.Tseng CW, Brook RH, Keeler E, Steers WN, Mangione CM. Cost-lowering strategies used by Medicare beneficiaries who exceed drug benefit caps and have a gap in drug coverage. JAMA. 2004;292:952–60. [DOI] [PubMed]
- 26.Soumerai SB, Avorn J, Ross-Degnan D, Gortmaker S. Payment restrictions for prescription drugs under Medicaid: effects on therapy, cost, and equity. N Engl J Med. 1987;317:550–6. [DOI] [PubMed]
- 27.Soumerai SB, Ross-Degnan D, Avorn J, McLaughlin T, Choodnovskiy I. Effects of Medicaid drug-payment limits on admission to hospitals and nursing homes. N Engl J Med. 1991;325:1072–7. [DOI] [PubMed]
- 28.Motheral B, Fairman KA. Effect of a three-tier prescription copay on pharmaceutical and other medical utilization. Med Care. 2001;39:1293–304. [DOI] [PubMed]
- 29.Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. JAMA. 2001;285:421–9. [DOI] [PubMed]
- 30.Rector TS, Venus PJ. Do drug benefits help Medicare beneficiaries afford prescribed drugs? Health Aff (Project Hope). 2004;23:213. [DOI] [PubMed]
- 31.Mojtabai R, Olfson M. Medication costs, adherence, and health outcomes among Medicare beneficiaries. Health Aff (Project Hope). 2003;22:220–9. [DOI] [PubMed]
- 32.Caskie GI, Willis SL. Congruence of self-reported medications with pharmacy prescription records in low-income older adults. Gerontologist. 2004;44:176–85. [DOI] [PMC free article] [PubMed]
- 33.Boudreau DM, Daling JR, Malone KE, Gardner JS, Blough DK, Heckbert SR. A validation study of patient interview data and pharmacy records for antihypertensive, statin, and antidepressant medication use among older women. Am J Epidemiol. 2004;159:308–17. [DOI] [PubMed]
- 34.Boudreau DM, Doescher MP, Saver BG, Jackson JE, Fishman PA. Reliability of Group Health Cooperative automated pharmacy data by drug benefit status. Pharmacoepidemiol Drug Saf. 2005;14:877–84. [DOI] [PubMed]
- 35.Iglehart JK. The dilemma of Medicaid. N Engl J Med. 2003;348:2140–8. [DOI] [PubMed]
- 36.Baugh DK, Pine PL, Blackwell S, Ciborowski G. Medicaid prescription drug spending in the 1990s: a decade of change. Health Care Financ Rev. 2004;25:5–23. [PMC free article] [PubMed]


