Abstract
Background
The World Health Organization encourages the development of youth friendly services, yet little is known on how youth currently present in general practice.
Objective
To describe the perspectives, expectations, and service receipt of young people presenting to family doctors to inform the development of youth friendly services.
Design
Cross-sectional survey.
Participants and measurements
Consecutive young people attending 26 randomly selected practices were recruited in the waiting rooms. Standardized instruments were used to interview them before their consultation.
Results
Of 501 young people who were approached, 450 participated (91% participation rate). Most had respiratory (26%) or dermatological complaints (18%). When asked to assess their health status, 59% perceived they had neither a physical nor a mental illness. However, 43% stated they had fears about their health problem and 1 in 5 feared it could be life-threatening. Although only 10% presented with psychological complaints, 24% perceived they currently had a mental illness. The most common expectations were treatment (50%) and good communication (42%). Most youth were prescribed medication (60%), but 40% of those who received a prescription had not expected to receive a treatment. A follow-up appointment was offered to 57% of participants.
Conclusions
This study identifies a gap between young people’s perception of illness and their presentations to family doctors. It also highlights unexpected fears, and a mismatch between expectations and service receipt. These findings have implications for family medicine training and for clinical practice. They should inform the development of youth friendly services.
KEY WORDS: family practice, adolescent health services, health knowledge, attitudes, practice
BACKGROUND
The World Health Organization (WHO) recently emphasized the need to develop youth-friendly health services to improve the care provided to young people throughout the world.1 In countries with established economies, psychosocial problems represent the greatest burden of disease for young people including mental disorders; tobacco, alcohol, and other substance use; accidents and injury; sexually transmitted diseases; and unwanted pregnancies.2–4 Youth (defined by WHO as young people between 15 and 24 years) are in particular need of developmentally appropriate services to address this largely preventable disease burden as many do not receive professional help for the problems that affect them.5
Most young people visit a family doctor at least once a year.6–11 . Hence, family doctors are ideally placed to identify and respond to the common psychosocial burdens of youth. Studies indicate that despite the burden of disease attributable to mental and behavioral disorders, the majority of consultations to family doctors are for somatic health problems (respiratory and dermatological).4, 12, 13 Although many of them would welcome a discussion on these themes, few receive counseling about health-related behaviors in the consultation.14–16 In the US, about 8% of all ambulatory care encounters (specialist and primary care) are with patients in the age group 15 to 24 years.17 In Australia, approximately 10% of primary care encounters are with youth, yet little is known about the characteristics of this group of primary care patients.18 To date, much of the research on the relationship between youth and primary care has focused on the barriers young people encounter to accessing care.4, 11, 19, 20 However, we know little of why young people who do go to see family doctors actually present, what they expect from the consultation, and the types of services provided to them.20 This baseline knowledge is important for highlighting ways in which primary care can become more responsive to the needs of youth. The aim of the present study was to describe this profile of youth visiting family doctors.
PARTICIPANTS, DESIGN, AND MEASUREMENT
Subjects, Design, and Recruitment
We undertook a cross-sectional study in 26 randomly selected general practices throughout the state of Victoria, Australia. The sample was stratified so that the number of participating practices reflected the proportion of the Victorian population living in Rural, Remote, and Metropolitan Areas (RRMA). Consecutive patients aged 16 to 24 years (an average of 20 per practice) were recruited (DMH) in the waiting rooms and invited to participate in an interview before their medical consultation. Exclusion criteria were an acute medical condition requiring immediate attention by the doctor, and any other condition that could impair the young person’s ability to consent.
Measures
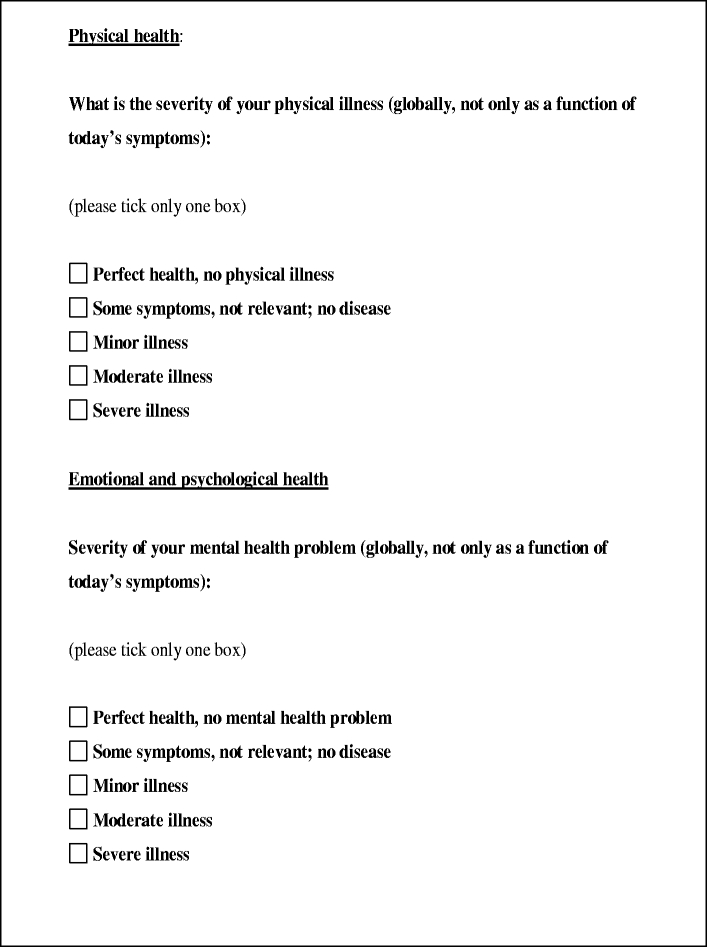
The questions used to interview participants about the health problem for which they had come to see the doctor and their expectations from the consultation, were taken from a standardized measure.21 Patients were asked to describe their reason for the consultation, whether they had any fears in relation to this health problem and what they hoped to gain from the consultation. Responses to these open-ended questions were written down in full and subsequently coded (see analysis). In addition, they completed a scale of emotional distress (K-10)22 and self-rated the severity of their physical and mental health problems (see Box 1).23 The K-10 is a 10-item scale developed with the US National Center for Health Statistics and designed to indicate significant levels of emotional distress (mostly anxiety or depressive states).
For each participant, the doctor completed a short questionnaire summarizing the outcomes of the consultation (health problems identified in the consultation, proposed treatment, followup or referral or both). Practitioners’ and young people’s sociodemographic characteristics were also recorded.
All measures were piloted with 56 young people (16 to 24 years), none of whom described any difficulties in understanding the questions.
Analysis
Participants’ answers to open-ended questions were written down in full then coded according to a standardized code book. For example, responses to the question “do you have any fears in relation to this [health] problem?” were coded into 1 of 17 types of fears such as “fear of cancer,” “fear of effect on work or studies,” etc. As the original code book came from studies involving adults, a pilot study was run to assess the range of answers from Australian youth. The code book was revised accordingly. For example, the category “fear of marital breakdown” was removed from the code book, as it did not emerge from young people’s answers in the pilot study. Several categories were, however, added, such as “fear of inappropriate diagnosis,” for example. Quality of coding (interrater reliability) was confirmed by having 2 investigators code a random selection of 45 participant questionnaires (all kappas >0.86). Reasons for encounter were coded using the International Classification for Primary Care (ICPC-2).24, 25 Analyses were conducted using Stata.26 Categorical variables were summarized using frequencies. All confidence intervals were adjusted for clustering within practices. Numeric data were described using means and standard deviations (SD). Logistic regression adjusting for confounders (patients’ age, gender, place of birth, student status, GPs’ age and gender, and socioeconomic index for the location of the practice) and clustering was used to study the association between patient or GP factors (patient expectations, fears, level of emotional distress, perception of having a physical or a mental illness, GP identification of a physical or mental illness) and the prescription of medication and nonpharmacological treatments.
Scores for the K-10 were computed following the method proposed by Andrews et al.27 A Bayesian approach (which takes into account the pretest probability, here the expected prevalence in our population, when defining the cutoff score) was then used to interpret these scores.28 A score of 20 or above was thus considered indicative of high probability of a common mental disorder (78% probability or higher).
Ethics
The study was approved by the ethics committees of the Royal Children’s Hospital in Melbourne and of The University of Melbourne. In wishing to explore the views of young people, it was important to obtain an opinion that was independent of their parents’. Despite being “youth” according to WHO definitions, patients aged 15 years were not included in the study as these ethics committees only approved inclusion of minors aged 16 to 18 years without parental consent.
RESULTS
Respondent Characteristics
One hundred six family doctors were involved in the study. Out of 501 youth, approached, 450 agreed to participate (90% participation rate; 3% excluded, 6% declined). Overall, the stratification of the sample was equivalent to that of the population of Victoria although, owing to the limitations related to the fixed cluster size of 20, a slightly higher proportion of participants were sampled in the capital city (77% compared to 74% of the Victorian population), and consequently a slightly lower proportion from rural areas (18% compared to 21% in the Victorian population).
Participants’ sociodemographic characteristics by gender are described in Table 1. Most participants were female (66.0%) and born in Australia. The majority of those born overseas were born in Asia (7.8%). The proportion of indigenous participants paralleled known proportions for the State. Most young people, and in particular males, still lived with their parents. The majority of youth were students and most of those who were not students were involved in full- or part-time paid work. However, 8.4% of participants neither worked nor studied. About a third had a low yearly income, hence were eligible for a health care concession card.
Table 1.
Sociodemographic Characteristics of Study Participants, by Gender (n = 450)
| Characteristic | Male (N = 153) | Female (N = 297) | Total (N = 450) | ||||
|---|---|---|---|---|---|---|---|
| N | Years | N | Years | N | Years | SD | |
| Mean age (yrs) | 153 | 19.6 | 297 | 20.1 | 450 | 20.0 | 2.5 |
| % | % | % | 95%CI | ||||
| Born overseas | 22 | 14.4 | 49 | 16.5 | 71 | 15.8 | 7.9–23.7 |
| Indigenous | 1 | 0.7 | 2 | 0.7 | 3 | 0.7 | 0–1.4 |
| Living with both parents | 103 | 69.1 | 173 | 58.8 | 276 | 62.3 | 52.9–71.8 |
| Student | 88 | 59.1 | 172 | 58.2 | 260 | 58.5 | 49.5–67.3 |
| Employed full-time | 57 | 38.3 | 81 | 27.7 | 138 | 31.3 | 24.2–37.8 |
| Neither employed nor student | 9 | 6.0 | 29 | 9.8 | 38 | 8.4 | 5.2–11.9 |
| Healthcare card holder | 51 | 33.0 | 111 | 38.0 | 162 | 36.3 | 29.3–43.3 |
Consulting Pattern
Only half of the participants (N = 227, 50.4%) said they had come to their usual practice. Fifty-six percent of participants aged under 18 years came with a parent, whereas a parent accompanied only 9% of those aged 18 years and older. Most participants (55.6%) stated that they alone had made the decision to come to see the doctor. Those who had been encouraged by someone else had most commonly followed the advice of their mother (44.7%), another health professional (23.6%), their partner (9.0%), or a nonmedical professional such as a sports coach (9.0%). Minors were not significantly more likely to have followed someone’s advice when deciding to come.
Young People’s Stated Reason for the Encounter
The most common presenting problems for both males and females were respiratory and skin disorders, followed by general problems (Table 2). For females, problems related to childbearing and contraception were frequent, and for males, musculoskeletal complaints. Males born outside Australia presented significantly more frequently for respiratory complaints than males born in Australia (59%; 95% CI: 37–81% compared to 29%; 95% CI: 21–37%), and were less likely to come for general complaints (0%, compared to 16%; 95% CI: 10–22%). Foreign-born females presented significantly more frequently for skin problems (29%; 95% CI: 15.5–42% compared to 16%; 95% CI: 12–21%) and significantly less frequently for family planning reasons (4%; 95% CI: 0–10% compared to 23%; 95% CI: 17–28%) than Australian-born females.
Table 2.
Most Common Reasons for the Medical Encounter in 450 Primary Care Attendees Aged 16–24 Years, Using lcpc-2 Classification, with a Comparison of Data for All Age Groups in Australia
| Major ICPC-2 category (typical examples) | Rate per 100 participants in %* (95%CI) | Percent encounter, Australian general practice # | ||
|---|---|---|---|---|
| Male n = 153 | Female n = 297 | Total n = 450 | ||
| R: Respiratory(asthma, URTI) | 33.3 (24.1–42.5) | 21.9 (16.2–27.3) | 25.8 (21.5–30) | 13.8 |
| S: Skin (acne,dermatitis) | 18.3 (11.2–25.4) | 18.2 (13.4–23.0) | 18.2 (14.6–21.8) | 10.4 |
| A: General or unspecified (feeling unwell, travel advice, medical check-up) | 13.7 (7.4–20.1) | 12.5 (8.5–16.4) | 12.9 (9.4–16.3) | 24.4 |
| W: Pregnancy, childbearing, family planning (contraceptive pill) | – | 19.5 (14.5–24.6) | 12.9 (9.4–16.4) | 2.3 |
| D: Digestive (nausea, diarrhea) | 11.8 (69–16.6) | 9.4 (5.5–13.4) | 10.2 (7.3–13.2) | 6.6 |
| P: Psychological (depression, sleep disturbance) | 8.5 (3.6–13.4) | 11.1 (7.7–14.5) | 10.2 (7.3–13.2) | 5.1 |
| X: Female genital system (thrush) | – | 14.8 (9.0–20.7) | 9.8 (5.9–13.6) | 3.3 |
| L: Musculoskeletal (back pain) | 13.7 (7.6–19.9) | 6.1 (2.9–9.2) | 8.7 (5.1–12.2) | 11.1 |
*Patient-reported complaints; several participants had more than 1 category of presenting complaint.
†Patient complaints as reported by GPs
The use of the ICPC-2 classification allowed comparison with the distribution of Australian patients’ reasons for encounter.18 Circulatory and musculoskeletal reasons for encounter were less frequent in our study population than in the general Australian primary care population (all age groups). Conversely, respiratory, skin, family planning, and psychological reasons for encounter were more commonly seen among the young people in this study than for all age groups in Australia.
Youth’s Perceptions of their Health Problem
Although only 10% of participants presented with a psychological complaint, 24% considered they currently had a mental illness and 36% had K-10 scores suggesting the presence of a common mental disorder.
Although the majority presented with a physical complaint, 69% participants did not perceive they had a physical illness. Indeed, most participants (59.0%) considered they had neither a mental nor a physical illness. However, nearly half the participants declared they had some level of fear in relation to their health problem. One in 5 (19.6%) reported a fear of having a life-threatening or serious illness (fear of death, cancer, another serious illness or incurable illness, or of committing suicide or self-harm). These perceptions were similar in Australian and foreign-born participants.
The relationship between high K-10 scores, presentation and perceptions of having a mental illness are presented in Table 3
Table 3.
Proportion of Young People with Each Level of K-10 Scores Who Presented with a Psychological Complaint or Not, and Who Perceived to Have a Mental Illness and Those Who Did Not
| High probability of common mental disorder according to the K-10 | Low probability of common mental disorder according to the K-10 | |
|---|---|---|
| Presented only with a physical complaint | 117 (72%; 95% CI: 64–80%) | 275 (98%; 95% CI: 96–100%) |
| Presentation included a psychological complaint | 45 (28%; 95% CI: 20–36%) | 5 (2%; 95% CI: 0–3%) |
| Young person perceives to have a mental illness | 89 (55%; 95% CI: 46–64%) | 17 (6%; 95% CI 3–9%) |
| Young person does not perceive to have a mental illness | 73 (45%; 95% CI: 36–54%) | 268 (94%; 95% CI: 92–97%) |
Young People’s Expectations
The most common expectations from the consultation were treatment (50%) and good communication (42% expected advice, reassurance, or that the doctor would listen to them; Table 4). Other common expectations were that the doctor would make a diagnosis, would propose some tests, or would complete a medical certificate or referral letter. There were no differences between the expectations of foreign and Australian-born participants.
Table 4.
Expectations from the Consultation in 450 Primary Care Attendees Aged 16–24 Years (Presented in Rank Order of Frequency)
| Expectation | N* | Percent* | 95% CI |
|---|---|---|---|
| Treatment | 223 | 49.9 | 45.2–54.6 |
| Medical prescription, Surgery, procedure | 170 | 38 | – |
| Cure | 36 | 8 | – |
| Change in current treatment | 22 | 4.9 | – |
| Communication | 186 | 41.6 | 36.9–46.4 |
| Advice, explanation | 139 | 31 | – |
| Reassurance | 41 | 9.2 | – |
| Listening, understanding | 14 | 3.1 | – |
| Diagnosis | 97 | 21.7 | 18.1–25.3 |
| Know what it is | 78 | 17.4 | – |
| Know the cause | 22 | 4.9 | – |
| Further examination/tests | 50 | 11.2 | 8.0–14.3 |
| Administrative task | 44 | 9.8 | 7.4–12.3 |
| Medical certificate | 27 | 6 | – |
| Referral letter | 17 | 3.8 | – |
| Other | 24 | 5.4 | 3.4–7.8 |
*N and Percent for the subcategories add up to more than the N and Percent for the main categories of expectations because a few YP named more than 1 expectation related to a main category. Similarly, total N and Percent add up to more than 450 and 100% because some YP named more than 1 category of expectation.
Consultation Outcomes
A summary of the major outcomes of the consultation, by gender, is presented in Table 5. Most patients (60.0%) were prescribed a pharmacological treatment. Antibiotics were by far the most frequently prescribed type of medication. Contraception and dermatological preparations were also frequently prescribed. The only factor associated with doctors’ prescription of medication was participants’ expectation that the doctor would prescribe a treatment (odds ratio [OR]: 2.2; 95% CI adjusted for clustering: 1.0–4.6). However, 40% of those who received a prescription had not reported this expectation before the consultation.
Table 5.
Outcomes of the Consultation with 450 Young Primary Care Attendees Aged 16-24 Years, by Gender
| Outcome | Male | Female | Total | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | 95% CI * | |
| Prescription of medication | 96 (62.8) | 173 (58.6) | 269 (60.0) | 55.9–64.2 |
| Nonpharmacological treatment | 71 (46.7) | 145 (49.3) | 216 (48.4) | 42.9–53.9 |
| Follow-up | 83 (54.3) | 171 (58.0) | 254 (56.7) | 50.7–62.7 |
| Referral | 17 (11.1) | 43 (14.6) | 60 (13.4) | 10.1–16.7 |
| Investigations | 12 (8.0%) | 20 (6.9%) | 32 (7.2%) | 4.2–10.3 |
*Adjusted for clustering within practices
Doctors proposed nonpharmacological treatments to nearly half of the participants (48.4%). Most commonly, this consisted of lifestyle advice such as a change of diet or an increase in physical activity. Rest and counseling were also often proposed. The multivariate analysis showed that the doctors were significantly more likely to prescribe nonpharmacological treatments to young people in whom they identified a mental illness (OR: 1.8; 95% CI: 1.0–3.4). Male practitioners were less likely to propose nonpharmacological treatments than female practitioners (OR: 0.58; 95% CI: 0.36–0.92)
Doctors offered a follow-up appointment in more than half of the cases (57%), and organized referrals for 13.4% of young people seen. Referrals were most commonly made to dermatologists and mental health specialists. Further investigations (blood test or x-ray, or both) were proposed for less than 10% of participants.
DISCUSSION
This study provides the first detailed description of young people’s perspectives on illness, expectations, and service receipt in primary care. A striking finding was that most young people did not actually perceive they had any illness at all. Yet many participants expressed fears in relation to their current health problem, and a substantial proportion of young people even had fears that their health problem was severe or life-threatening. We found no comparative data in relation to adults that would help us assess whether this is a usual occurrence in primary care or whether these findings are specific to youth.
Our findings confirm results from previous studies indicating that youth consult family doctors mostly for somatic complaints.4, 12, 13 Only 10% of young people presented with psychological complaints. Despite not presenting for such reasons, a quarter of participants perceived they had a mental illness when asked to evaluate their mental health status. This suggests that a substantial proportion of youth may be aware of their mental health problems, but not of the potential role that a family doctor can play in addressing them.29–32 Young people also often lack knowledge of what constitutes a treatable mental health problem.29 Fear of stigma and low awareness of the treatment options are other common barriers to seeking mental health services.33 Alternatively, young people may not expose their mental health problems to the family doctor because they do not trust the doctor to be competent in helping them with such issues or may be embarrassed to bring up this theme in the consultation.31, 32, 34 Either negative previous experiences or lack of trust in the current management options, or both, have been shown to affect young people’s willingness to seek help for their mental health problems.33 Despite not presenting for these, many young people had mental health symptoms that they recognized to be significant. Family doctors should therefore continue to be encouraged to routinely inquire about common symptoms of emotional distress in young people.
Half the participants did not attend their usual practice. This finding has important implications, as continuity of care favors recognition of psychosocial problems in primary care.35 Conversely, the fact that most young people were offered a follow-up appointment indicates that the family doctors are creating opportunities for improved assessment. The finding that close to half of those who were minors came without a parent is in line with previous findings and emphasizes the trend toward autonomy, which characterizes this age group.11
An important proportion of participants hoped the doctor would provide them with reassurance or advice. Similar findings emerge from studies involving adult primary care patients.36
Although most did not perceive they had an illness, half of the participants expected the doctor to prescribe medication and a majority of youth were prescribed such treatment. Although expecting a prescription was significantly associated with receiving one, it is of note that nearly half of those who were prescribed medication had not hoped to gain this from the consultation. Rather, many were seeking guidance and reassurance from the doctor. Although studies of adults suggest similar trends, we are not aware of any previous study highlighting such a gap between young people’s expectations from the consultation in relation to their health problem and the care they receive.37 These findings provide important guidance for doctors who wish to improve the way they respond to young people’s needs in the consultation. Dealing with health problems, and attending the doctor on their own, is yet another challenge young people face on their developmental path toward adulthood. In addition to the usual care they provide, family doctors can play an important role in providing guidance and advice to young people who seek help in facing unexpected symptoms and the fears related to them. These findings suggest young people’s views, expectations, and fears should be assessed in the consultation to appropriately respond to them. Communicating with young people in the consultation requires specific skills, which we recommend doctors acquire in their training.38
A high participation rate and the use of standardized measures are factors that increase the internal validity of the present findings. The potential bias related to coding participants’ answers in the interview was minimized by the use of clearly defined coding rules, as demonstrated by the high level of agreement in the interrater agreement study. A closed question was used to assess young people’s perception of their physical and mental health. Participants’ answers may reflect their understanding of the word illness rather than the concept illness. The use of an open question may have broadened the spectrum of responses and avoided such a bias, but was not possible within the time frame given for interviews before the consultation. External validity was optimized by recruiting patients from randomly selected practices throughout the entire State. The sample was stratified so that it reflected the same distribution as the population living in the Australian state of Victoria, with the majority of participants living in metropolitan areas. This sample can thus be said to be representative of youth living mainly in urban areas in countries with established economies. The external validity of the findings could have been further enhanced if patients themselves, rather than practices, had been randomly selected. However, technical limitations in relation to data collection precluded the implementation of such a recruitment strategy. Finally, as recruitment did not take place over the entire year, our findings regarding the prevalence of youth reasons for encounter may have been biased toward health problems that are more common in the Australian winter, spring and summer. However, though there were some seasonal variations in the frequency of some reasons for encounter, the most common presenting complaints (as presented in Table 2) remained the same throughout all seasons of the study.
CONCLUSIONS
This study identifies a gap between young people’s perception of illness and their presentations to family doctors. It also uncovers unexpected fears, and a mismatch between expectations and service receipt. Finally, it highlights that many young people, although perceiving to have a mental illness, do not request help for this when attending primary care. These results have important implications for clinical practice and medical training. They highlight the role for doctors in assessing young people’s fears, expectations, and perceptions of their mental and their physical health to provide appropriate guidance. Future research examining the relationship between youth presentations, expectations, and consultation outcomes (including satisfaction) will inform new interventions to improve the care offered to youth in primary care. Above all, these findings should inform the development of youth friendly primary care services.
Acknowledgments
We wish to thank the young people and the GPs for their kind participation. We are also grateful to Emeritus Professor Anthony Mann and Dr. Athula Sumathipala for providing us with the interview instrument and its original code book.
Conflict of Interest D. Haller’s fellowship in Melbourne was supported by Geneva University Hospital, Geneva Academic Society and the Swiss National Science Foundation. She was awarded an International Postgraduate Research Scholarship from The University of Melbourne and a publication grant (Fonds Tremplin) from Geneva University. L. Sanci was in receipt of an Australian National Health and Medical Research Council Public Health Postdoctoral Fellowship. None of these funding sources had any control or influence over the research project or the decision to submit the final article for publication.
APPENDIX
Box 1
Questions used to assess young people’s perception of their physical and mental health (derived from the GP questionnaire used in a WHO collaborative study in primary care23)
Footnotes
This study was presented as an abstract at the 2006 General Practice and Primary Care Research Conference in Perth, Australia, in July 2006.
References
- 1.WHO. Adolescent friendly health services: an agenda for change. Geneva: WHO; 2002. Report No.: WHO/FCH/CAH/02/14.
- 2.WHO. The World Health Report 2001. Mental health: new understanding, new hope. Geneva: World Health Organisation Publications; 2001.
- 3.Mathers C, Vos T, Stevenson C. The burden of disease and injury in Australia. Canberra: Australian Institute of Health and Welfare; 1999. Report No.: AIHW cat no PHE17.
- 4.Ozer EM, Macdonald T, Irwin CE, Jr. Health Care in the United States: implications and projections for the new millennium. In: Mortimer JT, Larson RW, eds. The Changing Adolescent Experience: Societal Trends and the Transition to Adulthood. England: Cambridge University Press; 2002.
- 5.Elster AB, Kuznets NJ. Guidelines for adolescent preventive services (GAPS): recommendations and rationale. Baltimore: Williams & Wilkins; 1994.
- 6.McPherson A. Adolescents in primary care. BMJ. 2005;330(7489):465–7. [DOI] [PMC free article] [PubMed]
- 7.Murdoch JC, Silva PA. The use of general practice services by 18 year olds in New Zealand. N Z Med J. 1996;109(1019):113–5. [PubMed]
- 8.Elliott BA, Larson JT. Adolescents in mid-sized and rural communities: foregone care, perceived barriers, and risk factors. J Adolesc Health. 2004;35(4):303–9. [DOI] [PubMed]
- 9.Jeannin A, Narring F, Tschumper A, et al. Self-reported health needs and use of primary health care services by adolescents enrolled in post-mandatory schools or vocational training programmes in Switzerland. Swiss Med Wkly. 2005;135:11–8. [DOI] [PubMed]
- 10.Irwin CE, Jr. Adolescent health at the crossroads: where do we go from here? J Adolesc Health. 2003;33(1):51–6. [DOI] [PubMed]
- 11.Donovan C, Mellanby AR, Jacobson LD, Taylor B, Tripp JH. Teenagers’ views on the general practice consultation and provision of contraception. The Adolescent Working Group. Br J Gen Pract. 1997;47(424):715–8. [PMC free article] [PubMed]
- 12.Australian Institute of Health and Welfare. Australia’s young people: their health and wellbeing 2003. Canberra: AIHW; 2003.
- 13.Potts Y, Gillies ML, Wood SF. Lack of mental well-being in 15-year-olds: an undisclosed iceberg? Fam Pract. 2001;18(1):95–100. [DOI] [PubMed]
- 14.Joffe A, Radius S, Gall M. Health counseling for adolescents: what they want, what they get, and who gives it. Pediatrics. 1988;82(3 Pt 2):481–5 [PubMed]
- 15.Blum RW, Beuhring T, Wunderlich M, Resnick MD. Don’t ask, they won’t tell: the quality of adolescent health screening in five practice settings. Am J Public Health. 1996;86(12):1767–72. [DOI] [PMC free article] [PubMed]
- 16.Lustig JL, Ozer EM, Adams SH, et al. Improving the delivery of adolescent clinical preventive services through skills-based training. Pediatrics. 2001;107(5):1100–7. [DOI] [PubMed]
- 17.Hing E, Cherry D, Woodwell D. National Ambulatory Medical Care Survey: 2004 Summary. Advance Data from Vital and Health Statistics; No. 374. Hyattsville, Maryland: National Center for Health Statistics; 2006. [PubMed]
- 18.Britt H, Miller GC, Knox S, et al. General Practice Activity in Australia 2004–2005. Canberra: Australian Institute of Health and Well-being; 2005.
- 19.Gleeson C, Robinson M, Neal R. A review of teenager’s perceived needs and access to primary health care: implications for health services. Primary Health Care Research and Development. 2002;3:184–93. [DOI]
- 20.Sanci LA, Kang MSL, Ferguson BJ. Improving adolescents’ access to primary health care. Med J Aust. 2005;183(8):416–7. [DOI] [PubMed]
- 21.Lloyd KR, Jacob KS, Patel V, St Louis L, Bhugra D, Mann AH. The development of the Short Explanatory Model Interview (SEMI) and its use among primary-care attenders with common mental disorders. Psychol Med. 1998;28(5):1231–7. [DOI] [PubMed]
- 22.Kessler RC, Andrews G, Colpe LJ, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol Med. 2002;32(6):959–76. [DOI] [PubMed]
- 23.Ustun TB, Sartorius N. Mental illness in General Health Care: an International Study. Chichester Wiley; 1995.
- 24.International Classification Committee of Wonca. ICPC-2 International Classification of Primary care, 2nd edn. Oxford: Oxford University Press; 1998.
- 25.Okkes IM, Becker HW, Bernstein RM, Lamberts H. The March 2002 update of the electronic version of ICPC-2: a step forward to the use of ICD-10 as a nomenclature and a terminology for ICPC-2. Fam Pract. 2002;19(5):543–6. [DOI] [PubMed]
- 26.Intercooled Stata 9.0 for Windows. College Station, Texas: StataCorp LP; 2005.
- 27.Andrews G, Slade T. Interpreting scores on the Kessler Psychological Distress Scale (K10). Aust N Z J Public Health. 2001;25(6):494–7. [DOI] [PubMed]
- 28.Furukawa TA, Kessler RC, Slade T, Andrews G. The performance of the K6 and K10 screening scales for psychological distress in the Australian National Survey of Mental Health and Well-Being. Psychol Med. 2003;33(2):357–62. [DOI] [PubMed]
- 29.Wissow LS, Platt RE. Promoting adolescents’ use of medical services. Patient Educ Couns. 2006;62(2):159–60. [DOI] [PubMed]
- 30.National Mental Health Strategy, (Keys Young). Research and Consultation among young people on mental health issues: final report: Commonwealth Department of Health and Family; 1997.
- 31.Booth ML, Bernard D, Quine S, et al. Access to health care among Australian adolescents young people’s perspectives and their sociodemographic distribution. J Adolesc Health. 2004;34(1):97–103. [DOI] [PubMed]
- 32.Biddle L, Donovan JL, Gunnell D, Sharp D. Young adults’ perceptions of GPs as a help source for mental distress: a qualitative study. Br J Gen Pract. 2006;56(533):924–31. [PMC free article] [PubMed]
- 33.Van Voorhees BW, Fogel J, Houston TK, Cooper LA, Wang NY, Ford DE. Attitudes and illness factors associated with low perceived need for depression treatment among young adults. Soc Psychiatry Psychiatr Epidemiol. 2006;41(9):746–54. [DOI] [PubMed]
- 34.McGee R, Feehan M, Williams S, Verhulst FC, Koot HM. Long-term follow-up of a birth cohort. The Epidemiology of Child and Adolescent Psychopathology. Oxford: Oxford University Press, 1995. pp. 366–84.
- 35.The MaGPIe Research Group. The effectiveness of case-finding for mental health problems in primary care. Br J Gen Pract. 2005;55:665–9. [PMC free article] [PubMed]
- 36.Rao JK, Weinberger M, Kroenke K. Visit-specific expectations and patient-centered outcomes: a literature review. Arch Fam Med. 2000;9(10):1148–55. [DOI] [PubMed]
- 37.Sanchez-Menegay C, Stalder H. Do physicians take into account patients’ expectations? J Gen Intern Med. 1994;9(7):404–6. [DOI] [PubMed]
- 38.Sanci L, Glover S, Coffey C. Adolescent health education programmes: theoretical principles in design and delivery. Ann Acad Med Singap. 2003;32(1):78–85. [PubMed]


