Abstract
Objective
Up to 32% of older patients take less medication than prescribed to avoid costs, yet a comprehensive assessment of risk factors for cost-related nonadherence (CRN) is not available. This review examined the empirical literature to identify patient-, medication-, and provider-level factors that influence the relationship between medication adherence and medication costs.
Design
We conducted searches of four databases (MEDLINE, CINAHL, Sciences Citations Index Expanded, and EconLit) from 2001 to 2006 for English-language original studies. Articles were selected if the study included an explicit measure of CRN and reported results on covarying characteristics.
Main Results
We found 19 studies with empirical support for concluding that certain patients may be susceptible to CRN: research has established consistent links between medication nonadherence due to costs and financial burden, but also to symptoms of depression and heavy disease burden. Only a handful of studies with limited statistical methods provided evidence on whether patients understand the health risks of CRN or to what extent clinicians influence patients to keep taking medications when faced with cost pressures. No relationship emerged between CRN and polypharmacy.
Conclusion
Efforts to reduce cost-related medication nonadherence would benefit from greater study of factors besides the presence of prescription drug coverage. Older patients with chronic diseases and mood disorders are at-risk for CRN even if enrolled in Medicare’s new drug benefit.
KEY WORDS: medicare, cost sharing, patient compliance, prescriptions
INTRODUCTION
Cost-related medication nonadherence (CRN) is a common and critical problem for elderly patients in the outpatient setting who take, on average, 4 to 5 different medications each week.1 Recent surveys show that up to 32% of older adults take less medication than prescribed to avoid costs.2–4 Patients who reduce medical costs by taking their medications sporadically, splitting pills, or delaying refills do not achieve the full therapeutic benefits of therapy and may be at increased risk of declining health.3
Although several studies5,6 have reviewed the evidence for linking medication costs to medication adherence, information on which patients are at-risk for CRN is limited. Research shows that individuals with apparently similar financial resources respond differently to medication costs: some will decrease adherence after modest increases in out-of-pocket costs,7 others will cut back if the increase is large,8 and still, a third group will steadfastly adhere to therapy despite substantial cost increases.9 It is yet unclear why economic burden alone does not predict patient susceptibility to cost-related nonadherence. This oversight is particularly urgent, as most enrollees in the standard Medicare Part D drug plan will pay out-of-pocket between 42 and 69% of their total drug expenses each year, and the consequences on medication adherence are yet unknown.10
The objective of this study was to review the empirical literature on the risk factors for CRN. Previous reviews have not focused on the characteristics of patients who explicitly identify their nonadherence as motivated by cost concerns. This focus is necessary and potentially enlightening, as 2 recent national surveys found that up to 73% of the Medicare population is engaged in drug cost reduction strategies, and 40% report nonadherence, and yet, only 26% report that such nonadherence is related to medication costs.2,4
We organized this paper according to a conceptual model developed by Piette et al.11 specifically for cost-related nonadherence behaviors (see Fig. 1). In this model, decisions about CRN are driven by financial pressures and polypharmacy. Secondary effects include characteristics of the medication, mental/physical health, and patient demographics. Clinicians and the health system may mediate the main and secondary effects through such means as fostering patient trust, selecting medications with lower costs, or providing access to cost assistance programs.11 We applied this model to the empirical literature to assess the evidence for the proposed associations.
Figure 1.
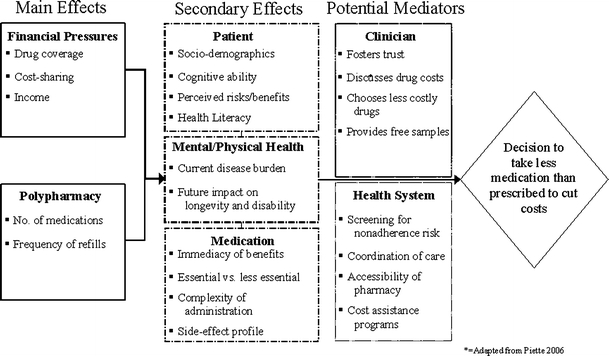
Conceptual model of cost-related nonadherence of medications.
METHODS
Search Strategy
We conducted searches of four electronic databases (MEDLINE, CINAHL, Sciences Citations Index Expanded, and EconLit) for English-language articles with empirical data related to medication costs and medication adherence. The review covered the last 5 years of literature (2001–October 2006) to coincide with improved measurement of the strategies patients use to avoid medication costs (See Figs. 1 and 2). Earlier surveys of CRN asked about only prescription filling problems and did not ask about such behaviors as skipping doses or splitting pills; thus, estimates of CRN were too low.12 For the MEDLINE search, we developed the search strategy, which included the subject heading prescription, drugs in combination with the cost terms personal financing, out-of-pocket costs, economics, ability to pay, deductible, coinsurance, copayment, or cost-sharing; we then applied the terms patient adherence, compliance, drug nonacquisition, or nonadherence. As primary or review articles were identified, we also manually reviewed the reference lists for additional sources and modified the search terms for the other three databases. Three investigators developed the search strategy, 1 (BAB) retrieved the articles and extracted the data, and 3 (BAB, JHG, SBS) made the final selection of studies.
Figure 2.
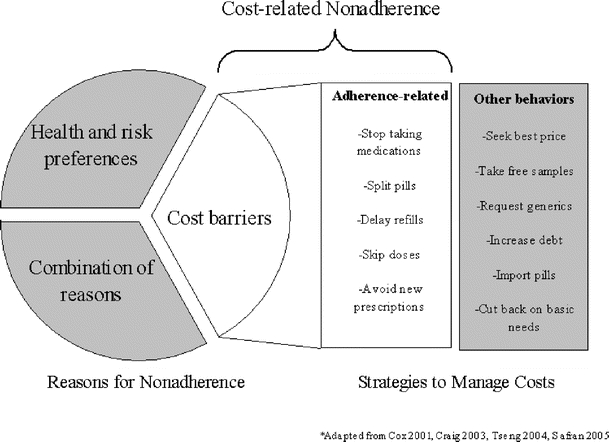
Relationship between medication nonadherence and cost-avoidance behaviors.
Study Selection
Articles were selected if they met three criteria: (1) reported original study results; (2) used an explicit measure for identifying cost-related nonadherence; and (3) provided results on potential risk factors. The measurement criterion excluded studies that combined all cost-management behaviors (related and unrelated to nonadherence) into a single measure of “cost burden”13–15 or derived CRN by estimating the proportion of all medication nonadherence attributable to insurance coverage or income.16–20 Those studies are less useful for identifying risk factors, as it is unclear how much of an overlap occurs in the characteristics of individuals who are nonadherent due to cost reasons rather than noncost reasons or who reduce drug costs without taking less medication. In addition, we excluded studies that reported no results on the covariates, as our objective was to assess risk factors.7,8,21–25 Finally, we limited the review to only studies conducted in the United States.
RESULTS
The electronic search identified 18,961 articles on medication adherence and 2,331 on medication costs, and the combination produced 203 for manual review. Of these, only 51 related to our study objective and 17 met the inclusion criteria.2–4,26–39 A manual review of the bibliographies of these papers produced another three articles.40–42 Papers generated from the same survey and sample were grouped together34,36,38 creating a total of 19 independent studies. Key characteristics of the final reviewed articles are summarized in the Table 1. All studies used survey data, and 3 also included administrative records; 5 were conducted by in-person/telephone interviews, 4 by Internet, and 10 by mail. Seven of the studies26,28,33,35,40,42,43 identified the samples through enrollment in health care plans or clinics, 82–4,29–32,41 from Medicare/Census eligibility files and 427,34,37,39 from lists of telephone numbers. Survey response rates ranged from 51 to 86%. All but one35 of the studies limited their samples to Medicare beneficiaries or adults aged 50 or older. With only one exception,3 all of the studies were cross-sectional, and all but one study26 used multivariate methods.
Table 1.
Risk factors for cost-related nonadherence of medications: a summary of the empirical evidence
| Risk factors and source | Number of studies | Populations studied | Range of sample sizes | Strength of evidence | Comments | Overall association |
|---|---|---|---|---|---|---|
| Financial pressures | ||||||
| Income 2–4, 26–32, 34–38, 40, 41, 43 | 15 | Medicare beneficiaries | 222–24,855 | Strong. 13 of 15 studies found statistically significant (P < .05) relationship, 12 in multivariate models | Income retains association in presence of drug coverage and cost-sharing | Higher income decreases risk |
| Medicare HMO enrollees | ||||||
| Homebound adults 60+ | ||||||
| Adults 50+ with chronic conditions | ||||||
| Diabetic persons 21+ | ||||||
| Drug coverage 2–4, 26–42 | 17 | Medicare beneficiaries | 222–24,855 | Strong. 16 of 17 studies found statistically significant (P < .05) relationship in multivariate models | Duration of coverage and type of coverage affect the magnitude of association | Coverage decreases risk |
| Medicare HMO enrollees | Knowledge about the benefit may be a factor | Inconsistent findings with benefit features | ||||
| Homebound adults 60+ | ||||||
| Adults 50+ with chronic conditions | ||||||
| Diabetic persons 21+ | ||||||
| Cost-sharing 26, 27, 29, 30, 32, 34, 36, 38, 40, 41, 43 | 9 | Medicare beneficiaries | 912–6,535 | Strong. 8 of 9 studies found statistically significant (P < .05) relationship in multivariate models | Cost-sharing retains association in presence of drug coverage | Higher cost-sharing increases risk |
| Medicare HMO enrollees | ||||||
| Homebound adults 60+ | ||||||
| Adults 50+ with chronic conditions | ||||||
| Polypharmacy 26, 27, 34, 36–38, 41 | 5 | Medicare beneficiaries | 222–4,630 | Moderate. 5 of 5 studies found no statistically significant relationship in multivariate models | Measured as number of medications | No association |
| Medicare HMO enrollees | ||||||
| Homebound adults 60+ | ||||||
| Adults 50+ with chronic conditions | ||||||
| Patient characteristics | ||||||
| Socio-demographics 3, 4, 26–29, 32, 34, 36-38, 40-43 | 13 | Medicare beneficiaries | 222–24,855 | Mixed. 11 of 13 studies found statistically significant (P < .05) relationships in multivariate models for age, 5 of 13 for gender, and 4 of 13 for race | Older age decreases risk; inconsistent or no relationship with other demographic measures | |
| Medicare HMO enrollees | ||||||
| Homebound adults 60+ | ||||||
| Adults 50+ with chronic conditions | ||||||
| Perceived risks/benefits 2, 26, 31, 33, 42, 43 | 6 | Medicare beneficiaries | 912–24,855 | Weak. Only bivariate tests of association | Most of the evidence comes from indirect measures | Decreasing perception of risk increases actual risk |
| Medicare HMO enrollees | ||||||
| Adults 50+ with chronic conditions | ||||||
| Mental/physical health | ||||||
| Current disease burden 2–4, 26, 28–31, 34–37, 40–43 | 16 | Medicare beneficiaries | 222–24,855 | Strong. 14 of 14 found statistically significant (P < .05) relationships in multivariate models for physical health | Physical health and mental health are independent risk factors | Increasing disease burden increases risk |
| Medicare HMO enrollees | Moderate. 6 of 7 found statistically significant (P < .05) relationships in multivariate models for mental health | |||||
| Homebound adults 60+ | ||||||
| Adults 50+ with chronic conditions | ||||||
| Medication characteristics | ||||||
| Essential vs less essential 27, 33, 34 | 3 | Weak. No statistical tests of relationship | Inconclusive relationship | |||
| Clinician characteristics | ||||||
| Physician–patient relationship 40, 42, 43 | 3 | Medicare beneficiaries | 912–24,855 | Mixed. 2 of 2 found statistically significant (P < .05) relationships in multivariate models for physician trust; 2 of 2 found no relationship with number of outpatient visits | High physician trust decreases risk | |
| Medicare HMO enrollees | ||||||
| Diabetic persons 21+ | ||||||
| Prescribed less costly agents or discussed costs 26, 33, 37, 42 | 3 | Medicare beneficiaries | 1,088–24,855 | Weak. Only bivariate tests of association | No assessment of physician-initiated discussions of cost | Inconclusive relationship |
| Medicare HMO enrollees | ||||||
The definitions of medication costs varied across the studies but were captured as having any drug coverage and monthly out-of-pocket payments for medications. In addition, 33,4,32 studies reported whether the drug coverage was full-year or part-year, 84,24,29–31,36,37,40 identified the type of coverage, and 326,28,33 described the elements of the benefit design. Three26,33,37 studies asked about the ease or difficulty of the out-of-pocket medication cost. The definitions of CRN also varied across studies. Some studies assessed nonadherence by asking 1 question about taking less medication than prescribed because of costs. Others asked about specific behaviors such as delaying or not filling prescriptions, skipping doses, or cutting pills4,28,31,33 Several studies also characterized the frequency of medication nonadherence and types of medications affected.27,33 Factors that were identified as influencing the effects of medication costs and medication nonadherence are summarized below.
Financial Pressures
Drug Coverage/Cost-Sharing Not having prescription drug coverage emerged as a significant and robust risk factor for cost-related nonadherence in all 17 reviewed studies with this measure; although, the protection afforded by drug coverage varied by the source, duration, design features, and patient cost-sharing. Just having any kind of prescription drug coverage consistently reduced the risk of CRN, and this association achieved a statistical significance (P < .05 or less) in 16 of the 17 studies. For instance, in a national survey of 17,685 Medicare beneficiaries, 26% reported any nonadherence due to costs, but 37% did so if without drug coverage (P < .001).2 However, when the source of coverage was measured in 7 studies,2,4,29,31,36,37,40 the risk-reduction of drug coverage varied considerably. For example, in a national study of 4,055 chronically ill individuals aged 50 or older, the rates of cost-related nonadherence of medications ranged from 12% with drug coverage from the Veterans Affairs to 15% with private insurance to 25% with Medicaid.36 Interestingly, that study and several others2,40 found cost-related nonadherence was high with Medicaid drug coverage even though such coverage is usually quite generous. In the 3 studies4,30,32 measuring duration of coverage, all found that the protective effect of drug coverage decreased by about half with anything less than full year coverage.Details about the drug benefit design beyond source and duration were studied far less, and the evidence was sometimes inconsistent. Drug plans with a low maximum drug benefit cap (e.g., $200 in total drug costs per quarter) were reexamined in 3 studies,26,28,44 and all three detected a significant risk for CRN with this drug benefit design. Only one study examined how CRN relates to patient knowledge of what the drug coverage actually covers, and it found an association with caps or limits on drug benefits but not with copays.39The evidence was strong in 8 of 9 reviewed studies for a substantial increase in the risk of CRN with increased medication costs, independent of having any drug coverage. For instance, among 912 persons with diabetes in the Veterans Affairs health system, those with monthly out-of-pocket drug costs exceeding $100 were substantially more likely (OR 9.8; CI 5.3–18.2) to reduce medication use due to costs compared to individuals with costs less than $50.43 In a survey of 4,055 chronically ill individuals, monthly out-of-pocket drug costs exceeding $100 increased the likelihood 5-fold for CRN (OR 5.5; CI 4.0–7.7) relative to costs under $50.38 In 6 of 7 studies with multivariate models, medication costs emerged as a significant predictor of CRN, even after controlling for drug insurance status. A comparison of multivariate models, both with and without out-of-pocket costs, found that medication costs, rather than insurance coverage, was the stronger predictor of cost-related nonadherence.36
Income Income was a strong risk factor for CRN and one of the most consistently tested. Thirteen of the 15 reviewed studies detected a statistically significant (P < .05) risk increase of CRN associated with low income. For instance, in a survey of 1,088 Medicare HMO plan enrollees who reached a benefit limit, the authors observed a 38% reduction in medication use for those with monthly incomes under $1,000 compared to 17% for those with incomes above $4,000 (P < .05).26 Among 15,998 Medicare beneficiaries, those with annual incomes below $20,000 were at a higher risk for CRN (OR 4.2; CI 2.2–7.8) relative to persons with incomes of $50,000 or higher.40 Income remained an independent and significant explanatory factor in 10 of 12 multivariate models, after adjustments for health insurance and medication costs.
Patient Characteristics
Socio-Demographics In the 13 reviewed studies, including demographic measures, most detected mixed or no associations between cost-related medication nonadherence and traditional indicators of vulnerability such as female gender, low education, and minority race, after controlling for income and insurance. The one exception was older age: in 11 of 13 studies, older adults were consistently less likely to engage in CRN than younger adults, after controlling for economic status.
Perceived Risks/Benefits of Therapy Direct evidence on how patients weigh the benefits of therapy against the risks of nonadherence was limited to one study; however, 5 studies provided indirect evidence suggesting that the risk of CRN increases when patients perceive a negligible consequence. Direct evidence is offered in a study of 1,088 Medicare enrollees where 32% reported cost-related nonadherence, yet only 9% thought their condition had worsened as a result.26 Indirect evidence may be provided by the finding in 4 of 5 studies that reducing the dose was a more common behavior than forgoing the prescription. It is intuitive that patients would save the most money by omitting entire prescriptions, yet most CRN patients instead tried to make the prescription last longer. This behavior indicates some level of risk-to-benefit decision making. For instance, in a survey of 1,088 Medicare enrollees, 24% skipped doses because of costs, while only 13% did not fill prescriptions.26
Mental/Physical Health
Current Disease Burden All of the 16 reviewed studies found that poor health status increased the risk of cost-related nonadherence, and this relationship achieved a statistical significance of P < .05 or less in all cases. The association appears to be robust across different measures of disease burden including self-reported health status, activities of daily living scale, and count of comorbidities. For instance, a nationally representative cohort study of 7,991 individuals found that those who took less medication due to costs reported more comorbidities at baseline (2.7 vs 2.0, P < .001) and more often rated their health as fair or poor (53.6 vs 27.1%, P < .001). Furthermore, cost-related nonadherence of medications was highly correlated with poor health care habits such as smoking (22.5 vs 11.2%, P < .001) and having a body mass index in the obese range (26.8 vs 19.5%, P < .001).3 In a national survey of Medicare beneficiaries, individuals reporting CRN were more likely to rate their health as poor (23 vs 10%) and to have recently been hospitalized (43 vs 33%).30 Two national studies of 12,100 and 13,835 Medicare beneficiaries, respectively, detected significant associations (P < .001) between multiple chronic conditions and CRN, even after statistically controlling for socio-demographics, drug coverage, and income.2,4In 6 of 7 reviewed studies, poor mental health emerged as a statistically significant (P < .05 or less) risk factor for cost-related nonadherence. For instance, in a study of 912 diabetic patients, individuals were more likely (OR 2.4; 95% CI 1.3–4.5) to report cost-related nonadherence if they also had symptoms of depression.43 Two large surveys of Medicare beneficiaries detected significant associations (P < .0004) between CRN and lower scores from the Mental Component Scale of the Short Form-12.40,41
Polypharmacy and Medication Characteristics
Contrary to the proposed association in the conceptual model, no relationship emerged between cost-related related medication nonadherence and polypharmacy, as measured by the number of medications prescribed. After multivariate adjustments for patients’ health and socioeconomic status, all 5 reviewed studies found no evidence that the risk of cost-related medication nonadherence increased with multidrug regimens.26,27,34,36–38,41
Limited information was available on the types of the medications that exacerbate or ameliorate cost-related nonadherence. Only 3 studies examined the kinds of medications affected by cost-related nonadherence, and none tested the association. For instance, a listing of the top 5 drug classes most affected by CRN showed a wide range of therapeutic importance: HMG Co-A reductase inhibitors, proton pump inhibitors, COX-2 inhibitors, diuretics, and non-sedating antihistamines.33 In contrast, in 4,055 older adults with chronic illnesses, those who took less medication to reduce costs said it was often the drug taken for medication-sensitive conditions such as asthma, chronic obstructive pulmonary disease, and depression.34 No clear pattern emerged in these studies of cost-related nonadherence occurring more for essential than for nonessential medications.
Clinician Characteristics
Physician–Patient Relationship Only 3 reviewed studies assessed the influence of the physician–patient relationship on CRN, and the results varied by measurement method. In the 2 studies using a measure of physician trust or quality, protective associations were detected with high trust at statistically significant levels (P < .05 or less) and in multivariate models. For example, a study of 15,998 Medicare beneficiaries found those who reported the lowest quality physician relationship were at higher risk (OR 2.1; 95% CI 1.4–3.2) of CRN relative to patients with higher quality physician relationships41 Similarly, in a survey of older patients with diabetes, high physician trust was associated with lower CRN, even after adjusting for high prescription costs and low income.43 In contrast, the two studies using the number of physician visits found no evidence of a relationship to cost-related nonadherence.41,42
Prescribed Less Costly Agents or Discussed Costs Only 3 studies assessed the association between CRN and the prescribing of less costly agents or discussing drug costs and all found increased risk or did not test the relationships for statistical significance. For example, in a cross-sectional survey of health plan members, those who asked their doctor or pharmacist for less costly medications were far more likely to be engaged in cost-related nonadherence of medications than individuals who did not make such requests (41 vs 15%, P < .001) Similarly, the reviewed studies provided only anecdotal evidence on the extent prescribers choosing less-expensive agents will prevent cost-related nonadherence. For instance, in a study of the medications affected by cost-related nonadherence in 1 health plan, 15 of the top 20 affected medications had generic or over-the-counter substitutes.33 The authors interpreted this finding as suggestive of missed opportunities to prescribe less costly agents.
DISCUSSION
The findings from a randomized trial45 and dozens of observational studies indicate that lack of drug coverage strongly inhibits the use of prescription drugs, but there is less information on the other risk factors, especially those unrelated to financial burden. Furthermore, there has been no assessment of whether the risk factors identified for all-cause nonadherence also predict cost-related nonadherence as indicated by patients. In our review, we found empirical support for concluding that certain patients may be more susceptible to cost-related medication nonadherence than others, regardless of financial burden. Nearly all of the studies were cross-sectional, which limits the interpretation to only associations. Nevertheless, some of the associations remained consistent across different patient groups and in numerous studies with large sample sizes.
As others have found, not having prescription drug coverage emerged as a significant and robust risk factor for cost-related nonadherence. However, the protection afforded by drug coverage varied by the source, duration, and to some extent, the benefit design features. Medication costs, rather than drug coverage, was the more influential economic factor on CRN decisions. These findings are supported by studies using only insurance claims, which have shown average medication use decreases after increases in copayments even among people with the same type of drug coverage.8,22,23
The reviewed studies also established consistent links among low levels of physical health, mental health deficits, and CRN, and these effects persisted after controlling for economic factors. Individuals who have symptoms of depression or a heavy disease burden appear to be more susceptible to cost-related nonadherence, and this tendency cannot be explained by lack of drug coverage, poverty status, or monthly out-of-pocket drug costs.
We did not find sufficient evidence that patients fully understand the potential consequences of CRN on their health. To the contrary, the limited evidence suggested that perceptions of low health risk may predict CRN. It remains to be determined why so many patients apparently believe that skipping doses to reduce costs will not compromise the effectiveness of their treatment.
Physician relationships rated by patients as high quality and trustworthy greatly decreased the likelihood of CRN. However, discussions about medication costs with doctors, pharmacists, or nurses appeared as a marker of high risk. This latter finding, though, is likely due to the cross-sectional study designs.
Several limitations of this review should be noted. The assessment of CRN was based on self-report. In general, patients tend to understate nonadherence so our study populations were probably a subset of the true population.46 Furthermore, we did not know whether the reported nonadherence conflicted with the advice of prescribers or was trivial (i.e., one skipped dose). The cross-sectional study designs also confounded some of the findings and interpretations. There are high correlations, for instance, among contemporaneous measures of health status, medication costs, and polypharmacy. Thus, it is unclear if medication costs lead to cost-related nonadherence, which then leads to lower health status or if the causality order begins with worsening health. Lastly, only 2 of the reviewed studies35,43 examined patients under the age of 50, thereby, limiting the generalizability of this review to younger populations.
Future studies are needed that model the patient response to medication costs using standard measures and accepted theories of health care decision making. One challenge of this review was the wide variety of CRN measures (some without tested reliability and validity). Furthermore, this body of research lacked robust models for explaining the behavior. Piette’s conceptual framework for understanding CRN suggests that the response may be modified by multiple contextual factors, but it has never been formally tested. As a result, the studies reviewed here provided uneven coverage of potentially important components of cost-related nonadherence. Also, research on CRN would be improved by more studies of both subjective patient assessments and objective data sources such as administrative insurance claims. It would be valuable to understand the gap between what the drug coverage actually covers and what patients believe it covers.
Lastly, longitudinal studies that track patient perception of risk and financial pressures before the nonadherence decisions are made would provide more valid methods for identifying the most important factors that prompt or prevent CRN. The body of longitudinal research drawn from prescription claims has provided unequivocal evidence of population-level decreases in drug utilization after increases in cost-sharing.7,8,47 The next step is to identify the factors that enabled some patients to maintain their prescription drug regimen despite the cost increases.
What are the implications of this review for the new Medicare Part D benefit? Projections of the average Part D cost-sharing under standard benefit (without income subsidies) are $1,095 in 2006, $1,325 in 2007, and $1,357 in 2008.10 Moreover, these out-of-pocket costs can vary, as beneficiaries spend through the plan’s deductible, coverage gap (“donut-hole”), and catastrophic threshold.10 Some plans offer alternative benefit designs; however, the majority of Part D enrollees will face substantial and unpredictable medication costs. To put these numbers in context, the median income of households headed by someone aged 65 or older in 2004 was $24,509.48 Understanding and measuring the risk factors that moderate or exacerbate the impact of medication costs on adherence will be critical for explaining patient responses to the new drug benefit.
Acknowledgements
This study was supported by grants RO1AG022362 and R01AG028745 from the National Institute on Aging (NIA). Drs. Briesacher, Soumerai, and Gurwitz are investigators in the HMO Research Network Center for Education and Research in Therapeutics, which receives funding from the US Agency for Healthcare Research and Quality (grant 2U18HS010391).
Conflict of Interest Dr. Briesacher reported that she has received unrestricted research grants from and has been a consultant for Novartis Pharmaceuticals Corporation within the last 3 years. The other authors reported no conflicts of interest.
References
- 1.Kaufman DW, Kelly JP, Rosenberg L, Anderson TE, Mitchell AA. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. J Am Med Assoc. 2002;287:337–44. [DOI] [PubMed]
- 2.Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: findings from a 2003 national survey. Health Aff (Millwood) 2005. [DOI] [PubMed]
- 3.Heisler M, Langa KM, Eby EL, Fendrick AM, Kabeto MU, Piette JD. The health effects of restricting prescription medication use because of cost. Med Care. 2004;42:626–34. [DOI] [PubMed]
- 4.Soumerai SB, Pierre-Jacques M, Zhang F, et al. Cost-related medication nonadherence among elderly and disabled medicare beneficiaries: a national survey 1 year before the medicare drug benefit. Arch Intern Med. 2006;166:1829–35. [DOI] [PubMed]
- 5.Gibson TB, Ozminkowski RJ, Goetzel RZ. The effects of prescription drug cost sharing: a review of the evidence. Am J Manag Care. 2005;11:730–40. [PubMed]
- 6.Rice T, Matsuoka KY. The impact of cost-sharing on appropriate utilization and health status: a review of the literature on seniors. Med Care Res Rev. 2004;61:415–52. [DOI] [PubMed]
- 7.Tamblyn R, Laprise R, Hanley JA, et al. Adverse events associated with prescription drug cost-sharing among poor and elderly persons. J Am Med Assoc. 2001;285:421–9. [DOI] [PubMed]
- 8.Roblin DW, Platt R, Goodman MJ, et al. Effect of increased cost-sharing on oral hypoglycemic use in five managed care organizations: how much is too much? Med Care. 2005;43:951–9. [DOI] [PubMed]
- 9.Motheral B, Fairman KA. Effect of a three-tier prescription copay on pharmaceutical and other medical utilization. Med Care. 2001;39:1293–304. [DOI] [PubMed]
- 10.Stuart B, Briesacher BA, Shea DG, Cooper B, Baysac FS, Limcangco MR. Riding the rollercoaster: the ups and downs in out-of-pocket spending under the standard Medicare drug benefit. Health Aff (Millwood). 2005;24:1022–31. [DOI] [PubMed]
- 11.Piette JD, Heisler M, Horne R, Caleb Alexander G. A conceptually based approach to understanding chronically ill patients’ responses to medication cost pressures. Soc Sci Med. 2006;62:846–57. [DOI] [PubMed]
- 12.Craig BM, Kreling DH, Mott DA. Do seniors get the medicines prescribed for them? Evidence from the 1996–1999 Medicare Current Beneficiary Survey. Health Aff (Millwood). 2003;22:175–82. [DOI] [PubMed]
- 13.Heisler M, Wagner TH, Piette JD. Clinician identification of chronically ill patients who have problems paying for prescription medications. Am J Med. 2004;116:753–8. [DOI] [PubMed]
- 14.Alexander GC, Casalino LP, Meltzer DO. Patient–physician communication about out-of-pocket costs. J Am Med Assoc. 2003;290:953–8. [DOI] [PubMed]
- 15.Mitchell J, Mathews HF, Hunt LM, Cobb KH, Watson RW. Mismanaging prescription medications among rural elders: the effects of socioeconomic status, health status, and medication profile indicators. Gerontologist. 2001;41:348–56. [DOI] [PubMed]
- 16.Kennedy J, Erb C. Prescription noncompliance due to cost among adults with disabilities in the United States. Am J Public Health. 2002;92:1120–4. [DOI] [PMC free article] [PubMed]
- 17.Kennedy J, Coyne J, Sclar D. Drug affordability and prescription noncompliance in the United States: 1997–2002. Clin Ther. 2004;26:607–14. [DOI] [PubMed]
- 18.Fortess EE, Soumerai SB, McLaughlin TJ, Ross-Degnan D. Utilization of essential medications by vulnerable older people after a drug benefit cap: importance of mental disorders, chronic pain, and practice setting. J Am Geriatr Soc. 2001;49:793–7. [DOI] [PubMed]
- 19.Piette JD, Heisler M, Wagner TH. Cost-related medication underuse: do patients with chronic illnesses tell their doctors? Arch Intern Med. 2004;164:1749–55. [DOI] [PubMed]
- 20.Schommer JC, Mott DA, Hansen RA, Cline RR. Selected characteristics of senior citizens prescription drug payment and procurement in 1998 and 2001. J Manag Care Pharm. 2003;9:408–15. [DOI] [PMC free article] [PubMed]
- 21.Landsman PB, Yu W, Liu X, Teutsch SM, Berger ML. Impact of 3-tier pharmacy benefit design and increased consumer cost-sharing on drug utilization. Am J Manag Care. 2005;11:621–8. [PubMed]
- 22.Huskamp HA, Deverka PA, Epstein AM, Epstein RS, McGuigan KA, Frank RG. The effect of incentive-based formularies on prescription-drug utilization and spending. N Engl J Med. 2003;349:2224–32. [DOI] [PubMed]
- 23.Goldman DP, Joyce GF, Escarce JJ, et al. Pharmacy benefits and the use of drugs by the chronically ill. J Am Med Assoc. 2004;291:2344–50. [DOI] [PubMed]
- 24.Balkrishnan R, Byerly WG, Camacho FT, Shrestha A, Anderson RT. Effect of prescription benefit changes on medical care utilization in a Medicare HMO population. Am J Manag Care. 2001;7:1093–100. [PubMed]
- 25.Love J. Filling the Rx: An Analysis of the Perceptions, Attitudes and Buying Habitts of Medicare Beneficiaries. Washington, DC: AARP; 2004:1–17.
- 26.Rector TS, Venus PJ. Do drug benefits help Medicare beneficiaries afford prescribed drugs? Health Aff (Millwood). 2004;23:213–22. [DOI] [PubMed]
- 27.Piette JD, Heisler M, Wagner TH. Problems paying out-of-pocket medication costs among older adults with diabetes. Diabetes Care. 2004;27:384–91. [DOI] [PubMed]
- 28.Cox ER, Jernigan C, Coons SJ, Draugalis JL. Medicare beneficiaries’ management of capped prescription benefits. Med Care. 2001;39:296–301. [DOI] [PubMed]
- 29.Klein D, Turvey C, Wallace R. Elders who delay medication because of cost: health insurance, demographic, health, and financial correlates. Gerontologist. 2004;44:779–87. [DOI] [PubMed]
- 30.Mojtabai R, Olfson M. Medication Costs, Adherence, And Health Outcomes Among Medicare Beneficiaries. Health Aff. 2003;22:220–9. [DOI] [PubMed]
- 31.Safran DG, Neuman P, Schoen C, et al. Prescription drug coverage and seniors: how well are states closing the gap? Health Aff (Millwood). 2002;Supp Web Exclusives: W253–68. [DOI] [PubMed]
- 32.Steinman MA, Sands LP, Covinsky KE. Self-restriction of medications due to cost in seniors without prescription coverage. J Gen Intern Med. 2001;16:793–9. [DOI] [PMC free article] [PubMed]
- 33.Tseng CW, Brook RH, Keeler E, Steers WN, Mangione CM. Cost-lowering strategies used by Medicare beneficiaries who exceed drug benefit caps and have a gap in drug coverage. J Am Med Assoc. 2004;292:952–60. [DOI] [PubMed]
- 34.Piette JD, Heisler M, Wagner TH. Cost-related medication underuse among chronically ill adults: the treatments people forgo, how often, and who is at risk. Am J Public Health. 2004;94:1782–7. [DOI] [PMC free article] [PubMed]
- 35.Piette JD, Wagner TH, Potter MB, Schillinger D. Health insurance status, cost-related medication underuse, and outcomes among diabetes patients in three systems of care. Med Care. 2004;42:102–9. [DOI] [PubMed]
- 36.Piette JD, Heisler M. Problems due to medication costs among va and non-va patients with chronic illnesses. Am J Manag Care. 2004;10 (part 2):861–868. [PubMed]
- 37.Sharkey JR, Ory MG, Browne BA. Determinants of self-management strategies to reduce out-of-pocket prescription medication expense in homebound older people. J Am Geriatr Soc. 2005;53:666–74. [DOI] [PubMed]
- 38.Heisler M, Wagner TH, Piette JD. Patient strategies to cope with high prescription medication costs: who is cutting back on necessities, increasing debt, or underusing medications? J Behav Med. 2005;28:43–51. [DOI] [PubMed]
- 39.Piette JD, Heisler M. The relationship between older adults’ knowledge of their drug coverage and medication cost problems. J Am Geriatr Soc. 2006;54:91–6. [DOI] [PubMed]
- 40.Saver B, Doescherm M, Jackson E, Fishman P. Seniors with chronic health conditions and prescription drugs: benefits, wealth, and health. Value Health. 2004;7:113–143. [DOI] [PubMed]
- 41.Wilson IB, Rogers WH, Chang H, Safran DG. Cost-related skipping of medications and other treatments among Medicare beneficiaries between 1998 and 2000. Results of a national study. J Gen Intern Med. 2005;20:715–20. [DOI] [PMC free article] [PubMed]
- 42.Taira DA, Iwane KA, Chung RS. Prescription drugs: elderly enrollee reports of financial access, receipt of free samples, and discussion of generic equivalents related to type of coverage. Am J Manag Care. 2003;9:305–12. [PubMed]
- 43.Piette JD, Heisler M, Krein S, Kerr EA. The role of patient–physician trust in moderating medication nonadherence due to cost pressures. Arch Intern Med. 2005;165:1749–55. [DOI] [PubMed]
- 44.Tseng CW, Brook RH, Keeler E, Mangione CM. Impact of an annual dollar limit or “cap” on prescription drug benefits for Medicare patients. JAMA. 2003;290:222–7. [DOI] [PubMed]
- 45.Newhouse JP, Manning WG, Duan N, et al. The findings of the Rand Health Insurance experiment—a response to Welch et al. Med Care. 1987;25:157–79. [DOI] [PubMed]
- 46.DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–9. [DOI] [PubMed]
- 47.Soumerai SB, Avorn J, Ross-Degnan D, Gortmaker S. Payment restrictions for prescription drugs under Medicaid. Effects on therapy, cost, and equity. N Engl J Med. 1987;317:550–6. [DOI] [PubMed]
- 48.DeNavas-Walt C, Proctor BD, Lee CH. Income, Poverty, and Health Insurance Coverage in the United States: 2004 Current Population Reports. Washington, DC: U.S. Census Bureau; 2005.


