Abstract
Current literature shows that intertrochanteric osteotomies can produce excellent results in selected hip disorders in specific groups of patients. However, it appears that this surgical option is considered an historical one that has no role to play in modern practice. In order to examine current awareness of and views on intertrochanteric osteotomies among international hip surgeons, an online survey was carried out. The survey consisted of a set of questions regarding current clinical practice and awareness of osteotomies. The second part of the survey consisted of five clinical cases and sought to elicit views on preoperative radiological investigations and preferred (surgical) treatments. The results of our survey showed that most of these experts believe that intertrochanteric osteotomies should still be performed in selected cases. Only 56% perform intertrochanteric osteotomies themselves and of those, only 11% perform more than five per year. The responses to the cases show that about 30–40% recommend intertrochanteric osteotomies in young symptomatic patients. This survey shows that the role of intertrochanteric osteotomies is declining in clinical practice.
Résumé
La littérature montre que les ostéotomies inter-trochantériennes peuvent donner de bons résultats dans des indications précises. Cependant il apparait que cette opération est considérée comme historique, sans rôle à jouer dans une pratique moderne. Pour apprécier les idées actuelles sur ces ostéotomies parmi les chirurgiens de la hanche, une enquête a été faite par courrier électronique. Cette étude comportait une série de questions concernant les pratiques cliniques et la connaissance des ostéotomies inter trochantériennes. Une seconde partie concernait 5 cas cliniques et il était demandé les investigations radiologiques et les traitements proposés. Les résultats de cette étude montraient que la plupart des experts pensait que ces ostéotomies pouvaient être faites dans des cas sélectionnés. Seulement 56% font des ostéotomies intertrochantériennes et parmi eux, seulement 11% en font plus de 5 par an. Les réponses aux cas cliniques montraient que 30 à 40% préconise ces ostéotomies chez des patients jeunes et symptomatiques. Cette étude montre que le rôle de l’ostéotomie intertrochantérienne est déclinant en pratique clinique.
Introduction
The use of intertrochanteric osteotomies appears to be declining in current clinical practice. It seems that many orthopaedic surgeons consider it an historical operation that has lost its place in current hip-disorder treatment. There are many retrospective studies showing overall unsatisfactory results (Table 1) [1, 2, 4, 6, 9–10, 13, 16–18, 20, 21, 23–28, 30]. However, many of these included elderly patients with advanced stages of primary osteoarthritis (OA). The same studies showed that the outcome in younger patients with early-onset secondary osteoarthritis was good. However, only a few of these studies showed survival rates identical or superior to those of total hip replacements and then only in selected patient groups. In a recent long-term follow-up study, we demonstrated that, for specific hip disorders, intertrochanteric osteotomies can achieve good to excellent long-term results [6]. Several recent reviews presented the same message, namely that intertrochanteric osteotomies should not be forgotten as a treatment option in these selected cases [19, 29]. Since we believed that this view was not shared universally, we initiated an online international survey to investigate current awareness among orthopaedic hip surgeons about these selected groups and to map the current clinical use of intertrochanteric osteotomies.
Table 1.
Review of the literature
| Authorsa | n | Indication | Type of osteotomy | Age (mean, range) | Grade of OA | Follow-up | Survival/conclusion |
|---|---|---|---|---|---|---|---|
| Haverkamp et al. 2006 [6] | 276 | All | All | 45 (16–79) | Mild to advanced | 15–29 years | Better results in young patients with mild OA |
| Haverkamp et al. 2006 [6] | 48 | Idiopathic | All | 57 (34–79) | Mild to advanced | 15–29 years | 10-year survival 50% and 15-year 32% |
| Haverkamp et al. 2006 [6] | 166 | Dysplasia | All | 46 (16–75) | Mild to advanced | 15–29 years | 10-year survival 72% and 15-year 56% |
| Haverkamp et al. 2006 [6] | 22 | Post-traumatic | All | 37 (17–68) | Mild to advanced | 15–29 years | 10-year survival 91% and 15-year 78% |
| Haverkamp et al. 2006 [6] | 14 | SCFE | All | 44 (25–55) | Mild to advanced | 15–29 years | 10-year survival 71% and 15-year 56% |
| Haverkamp et al. 2006 [6] | 20 | AVN | All | 38 (16–60) | Mild to advanced | 15–29 years | 10-year survival 60% and 15-year 30% |
| Pecasse et al. 2004 [21] | 15 | LCPD | All | 30 (19–55) | Mild to advanced | 4–25 years | 33% converted after an average of 15.4 years |
| D’Souza et al. 1998 [4] | 25 | All | All | 38 (18–53) | Mild to advanced | 2–12 years | 67% survival after an average of 12 years |
| Perlau et al. 1996 [23] | 16 | Idiopathic | All | 48 (38–75) | Mild to advanced | 5–10 years | 44% converted after an average of 6.1 years |
| Morssher et al. 1971 [20] | 2,251 | All | All | 20–80+ | Moderate to advanced | 2–14 years | Good indicationss are LCPD, SCFE and dysplasia |
| Schneider et al. 1966 [26] | 109 | All | All | 70 by follow up | Moderate to advanced | 12–15 years | 35% converted after an average of 8 years |
| Marti et al. 2001 [17] | 10 | OA after acetabular fractures | All | 29 (16–47) | Mild to advanced | 3–22 years | 80% survival after an average of 10 years |
| DePalma et al. 1970 [3] | 38 | All | All | 57 (15–81) | Moderate to advanced | 1–9 years | Pain relief in 87%, no long-term results |
| Perlau et al. 1996 [23] | 18 | Dysplasia | All | 33 (24–58) | Mild to advanced | 5–10 years | 79% survival after an average of 6.1 years |
| Toyama et al. 2000 [28] | 67 | Dysplasia | Valgus-extension | 44 (23–59) | Advanced | 5–16 years | 10-year survival 79% |
| Gotoh et al. 1997 [5] | 31 | Dysplasia | Valgus-extension | 43 (22–59) | Advanced | 12–18 years | 15-year survival 51% |
| Iwase et al. 1996 [9] | 42 | Dysplasia | Varus | 25 | Mild | 20 years | 10-year survival 89% and 15-year 87% |
| Jingushi et al. 2002 [10] | 70 | Dysplasia | Valgus | 44 (14–59) | Advanced | 2–15 years | 10-year survival 82% |
| Kubo et al. 2000 [12] | 17 | Dysplasia | Valgus-extension | 50 (34–58) | Advanced | 10–14 years | 18% good at last follow up |
| Pellicci et al. 1991 [22] | 56 | Dysplasia | Varus | 35 (17–62) | Mild to moderate | 2–21 years | 72% good to excellent after 9 years |
| Ito et al. 2005 [8] | 55 | Dysplasia | Varus | 32 (12–55) | Mild to moderate | 6–28 years | 10-year survival 81% |
| Iwase et al. 1996 [9] | 58 | Dysplasia | Valgus | 37 | Moderate to advanded | 20 years | 10-year survival 66% and 15-year 38% |
| Langlais et al. 1979 [13] | 150 | Idiopathic | Valgus | Moderate to advanded | 3–10 years | 68% good | |
| Maistrelli et al. 1990 [16] | 277 | All | Valgus-extension | 52 (26–66) | Mild to advanced | 11–15 years | 67% perfect to good, better results in young patients with secondary OA |
| Miegel et al. 1984 [18] | 77 | All | Medialisation | ? | Moderate to advanced | 12–15 years | 10-year survival 49% |
| Reigstad et al. 1984 [24] | 103 | All | All | 58 (24–74) | Moderate to advanced | 10-year survival 58% | |
| Santore et al. 1983 [25] | 45 | All | Valgus | 50 (32–69) | Moderate to advanced | 11 years | 75% good |
| Weisl et al. 1980 [30] | 757 | All | All | ? (incl. 70+) | Moderate to advanced | 10–22 years | 25% good at follow up, better results in young patients with secondary OA |
| Castaing et al. 1981 [1] | 141 | All | Varus | 51 (25–71) | Moderate to advanced | 13.5 years | 67% good |
| Collert et al. 1979 [2] | 94 | All | All | 60 (32–77) | Advanced | 5 years | 46% good after 5 years |
| Linde et al. 1985 [15] | 85 | All | All | <60 | Moderate to advanced | 1–15 years | 39% good after 5 years |
| Teinturier et al. 1982 [27] | 63 | All | Flexion | 55 (37–71) | Advanced | 10 years | 65% good |
| Zaoussis et al. 1984 [31] | 70 | All | Medialisation + rotation | 47 (21–68) | Mild to advanced | 6–15 years | 70% good |
aWhere possible, articles are subdivided as indicated
Methods
We developed a questionnaire consisting of two sections. The first section consisted of questions dealing with the use of intertrochanteric osteotomy in clinical orthopaedic practice. To assess orthopaedic surgeons’ awareness, the second part of the questionnaire consisted of questions related to five clinical cases. These cases were taken from our own long-term follow-up series and the long-term outcome of the performed intertrochanteric osteotomy was known in each case [6]. The responders were unaware of the treatment these patients received. Table 2 shows the full questionnaire (cases excluded).
Table 2.
Questions from the survey
| Questions |
|---|
| Occupation: Orthopaedic Surgeon/Orthopaedic Resident/Other |
| Age: <30 years/30–50 years/>50 years |
| Question 1: |
| Is there still a place for intertrochanteric osteotomies (ITO) in the treatment of primary or secondary osteoarthritis? No/Yes/Yes, but only in young patients/Yes, but only in some special cases |
| Question 2: |
| Do you perform intertrochanteric osteotomies yourself? Yes/No |
| If Yes, how many per year? |
| Question 3a: |
| Do you investigate the possibility of performing an ITO in (selected) patients with osteoarthritis of the hip? Yes/No |
| Question 3b: |
| If Yes, for which types of osteoarthritis do you consider an osteotomy? |
| Idiopathic OA |
| OA secondary to acetabular dysplasia |
| OA secondary to coxa valga |
| OA secondary to Legg-Calvé-Perthes disease |
| OA secondary to slipped capital femoral epiphysis |
| Post-traumatic OA |
| Question 4: |
| Is 3-D CT scanning necessary for the planning of an ITO? Yes/No |
| Question 5: |
| Which kind of radiological investigation is necessary to plan an ITO in your opinion? (several options are possible) |
| Plain pelvic X-ray |
| Abduction and/or adduction correction views |
| X-ray according to Dunn |
| False profile |
| Lateral hip X-ray |
| CT scan |
| CT scan with 3-D reconstruction |
| MRI |
| Arthro-MRI |
| Question 6: |
| Do you consider a total hip replacement after a previous osteotomy to be a more challenging operation? Yes/No |
| Question 7: |
| Do you think that the long-term results of total hip replacement after a previous osteotomy are worse than the results of a primary THR? Yes, worse than the long-term results of a primary THR/No, both long-term results are comparable |
| Question 8: |
| Is there, in your opinion, an age limit for performing an ITO? Yes/No |
An invitation to respond online to the questionnaire was sent to all members of the American Association of Hip and Knee Surgeons, all members of the British Hip Society and members of the Dutch Orthopaedic Society.
In order to identify factors that influenced surgeons to opt for an intertrochanteric osteotomy, a statistical analysis of the required data was carried out using a Pearson correlation analysis in which P<0.05 was considered as significant.
Results
One thousand invitations were sent by mail with an online return of 162 questionnaires. Since all responses were anonymous, no reminders or second invitations could be sent to non-responders. There were 69 responders from the United States and 93 from Europe.
From the content of the responses, we assume that all responders are orthopaedic surgeons with a special interest in hip surgery. Of all respondents, 96% believe that there is still a place for intertrochanteric osteotomy in current clinical practice with 56% still performing these. Only 11% perform more than five osteotomies per year.
The indications that are considered valid for performing intertrochanteric osteotomies are given in Table 3.
Table 3.
Indications for which intertrochanteric osteotomies are still considered
| Indication | % of respondents |
|---|---|
| Idiopathic OA | 23 |
| Dysplasia | 51 |
| Coxa valga | 65 |
| Legg-Calvé-Perthes disease | 40 |
| Slipped capital femoral epiphysis | 53 |
| Post-traumatic deformities | 31 |
In the workup of hip disorders, 87% of surgeons ask for an AP pelvic radiograph and 85% a lateral radiograph. False profile views instead of lateral views are added only by 62%. A CT scan is routinely requested by 29% and an additional MRI by 17%. Only 3% requested an MR arthrography.
When the issue of performing a THR after a previous intertrochanteric osteotomy was raised, 83% regarded this as a more challenging operation. Thirty-four percent believed that the long-term results of THR after a previous osteotomy would be impaired. This view appeared to have no bearing on the decision whether osteotomies should still be performed. Of the surgeons who perform osteotomies themselves, 46% think that the long-term outcome of a subsequent THR is impaired. In the case of surgeons who did not perform osteotomies, this figure increased to 68% (chi-square not significant).
When a sub-analysis was performed comparing responses from orthopaedic surgeons from the United States with those from Europe, the only significant differences were found in the performance and indication. In Europe, 69% of the questioned surgeons perform intertrochanteric osteotomies; in the United States only 39% (chi-square P<0.01). In Europe, 33% believed that selected patients with idiopathic OA could benefit from an ITO; in the USA, this was only 9% (chi-square P<0.01). Also for post-Perthes deformities (Europe 50%, USA 27%) and post-traumatic deformities (Europe 41%, USA 16%), significant differences were present (chi-square both P<0.01). No significant regional differences were present in preoperative screening.
Although it is not possible to show all X-rays from the cases in this article, we attempt to give an impression by presenting the neck-shaft angle (CCD) as an indicator of coxa valga, the Sharp angle as an indication of the steepness of the acetabulum, and the CE angle according to Wiberg and the acetabular head index (AHI) as indicators of dysplasia and lateralisation.
The severity of osteoarthritis was graded according to Tönnis. Complaints were scored using the Merle d’Aubigne score.
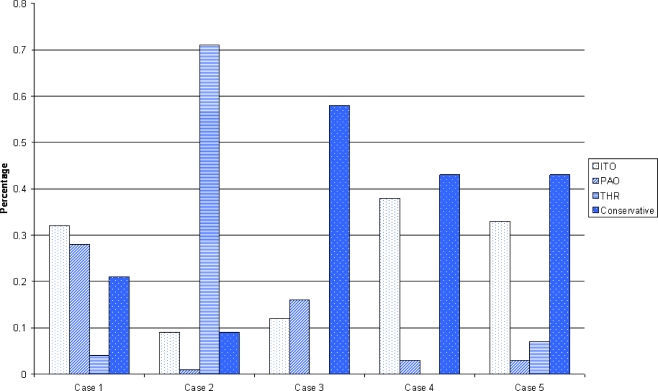
In case 1, we presented a 34-year-old female with a coxa valga (CCD 140°) and mild dysplasia (Sharp angle 50°, CE 22° and AHI 0.7) with mild OA (Tönnis grade 1) and a Merle d’Aubigne score of 13. In addition to a pelvic X-ray and an abduction correction view, 64% requested additional investigations. These were mainly false profiles (35%), lateral X-rays (32%) and CT scans (30%). As a treatment option, an intertrochanteric osteotomy was mentioned by 32%, an acetabular realigning osteotomy (also known as periacetabular osteotomy, PAO) by 28% and a THR by 4% (Fig. 1). We performed a 15° varus osteotomy, which was converted to a THA after 21 years.
Fig. 1.
Suggested interventions per case. Case 1 A 34-year-old female with symptomatic mild OA due to mild dysplasia and coxa valga. Case 2 A 55-year-old female with symptomatic moderate OA due to mild dysplasia and coxa valga. Case 3 A 31-year-old female with mild OA without significant complaints due to mild dysplasia and coxa valga. Case 4 An 18-year-old female with symptomatic excessive femoral anteversion without OA changes. Case 5 A 28-year-old male with a symptomatic post-Perthes deformity without OA changes. ITO Intertrochanteric osteotomy, PAO periacetabular osteotomy, THR total hip replacement
In case 2, we presented a 55-year-old female with a coxa valga (CCD 139°) and minimal dysplasia (Sharp angle 43°, CE 24°) with moderate OA (Tönnis grade 2) and a Merle d’Aubigne score of 9. In addition to a pelvic X-ray and an abduction/adduction correction view as shown, 28% requested additional investigations. As a treatment option, an intertrochanteric osteotomy was mentioned by 9%, an acetabular realigning osteotomy by 1% and a THR by 70%. We performed a 10° valgus osteotomy, which was converted to a THA after 9.4 years.
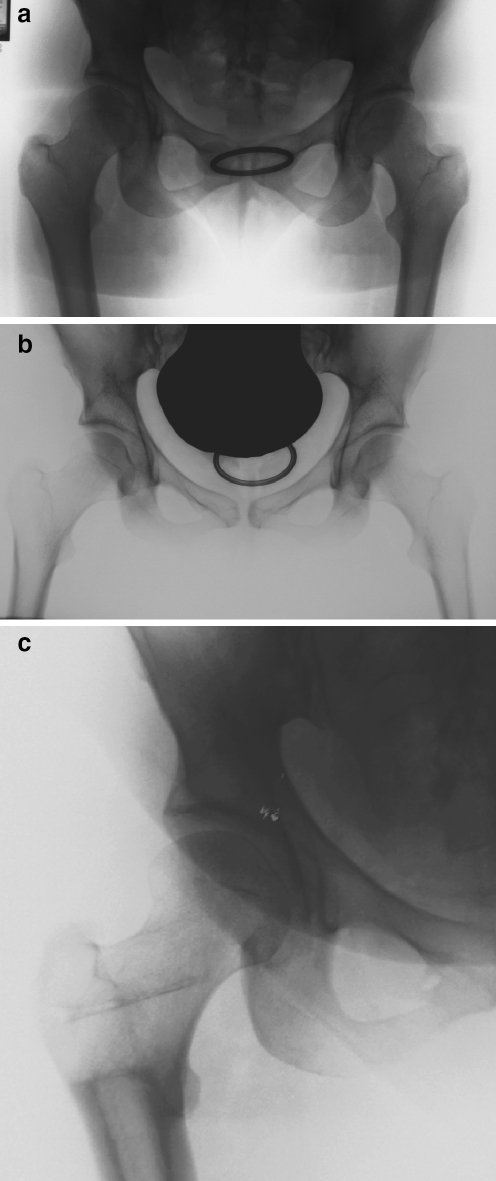
In case 3, we presented a young female (31 years of age) with minimal complaints and mild dysplasia (sharp angle 50° and CE angle of 14°) without significant osteoarthritic changes (Fig. 1). The majority advised conservative treatment (58%). In this case, 21% requested additional MRI scanning and 22% requested additional false profile X-rays. We performed a 15° varus osteotomy. After 19 years the patient had a Merle d’Aubigne score of 13.
In case 4, we described an 18-year-old female with a symptomatic (Merle d’Aubigne 16) excessive femoral anteversion (CCD 140° anteversion 38°) with a normal acetabulum (Sharp angle 38° and CE angle 36°). In addition to a pelvic X-ray and a Dunn X-ray, 49% requested additional investigations and 50% of these requested an MRI. The suggested treatment consisted of conservative treatment in 43% and an intertrochanteric osteotomy in 41%. We performed a slight varus and 20° derotation osteotomy (at both hips) and after 20 years, the patient had a Merle d’Aubigne score of 15 (and 18 for the contra lateral hip).
In case 5, a typical post-Perthes deformity was shown in a 28-year-old male with progressive complaints. In addition to the presented pelvic X-ray and adduction correction view, 44% requested additional investigations, mainly lateral views and CT scans. The suggested treatment consisted of conservative treatment in 43% and an intertrochanteric osteotomy in 33%. We performed a valgus osteotomy; after 14 years, the patient had a Merle d’Aubigne score of 17.
Figure 2 shows a summary of suggestions made in the five cases. Overall, intertrochanteric osteotomies were advised by 30–40% in symptomatic young patients. One case consisted of an older female patient (case 2) with a symptomatic OA secondary to dysplasia, in which mainly THR was advised.
Fig. 2a–c.
Example of a case (case 3). a A 31-year-old female, with minor complaints of the right hip (Merle d’Aubigne score 16). ROM was full. Radiological measurements for right hip: Sharp angle 50°, CE angle 14°, CCD 140°. b Abduction correction view. c Long-term follow up after 18 years
In the cases concerning younger patients, 44–63% of the respondents requested additional radiological investigations. In cases 1 and 5, these were mainly false profile views and CT scans; in case 3, mainly false profile views and MRIs; and in case 4, mainly CT scans and MRIs.
Responders were divided into two age groups: younger and older than 50. Apart from their responses in cases of post-traumatic deformities (young 40%, older 22%, chi-square P<0.05), no significant differences were present.
The Pearson correlation analysis showed a significant correlation between THR and age (R=0.91) and clinical complaints (R=0.91). Conservative treatment showed a significant correlation with clinical complaints (R=0.93).
Discussion
The aim of this survey was to show the role of the intertrochanteric osteotomy in current practice. Although almost all responders believe that intertrochanteric osteotomies should still play a role in modern medicine, only a few are performed nowadays. One should take into account that we primarily surveyed hip experts and not many general orthopaedic surgeons. Thus, the responses do not necessarily reflect common orthopaedic practice; however, we can assume that the use of intertrochanteric osteotomy by the non-specialised hip surgeon is probably even lower. This indicates that less reconstructive osteotomy surgery is performed nowadays and that the surgical know-how is in danger of being lost.
Of course, it is difficult to give accurate advice based on limited information and without seeing the patient; however it is possible to state a general opinion. The cases presented were selected in order to analyse the type of patients and hip deformities for which intertrochanteric osteotomies are considered and also to assess what type of radiological investigations are used in this decision-making process.
We believe that the cases presented are representative; however 45 (29%) of the surgeons who indicated that there was a place for intertrochanteric osteotomies in clinical practice did not recommend an intertrochanteric osteotomy in any of the cases.
There was a clear consensus that osteotomies should be reserved for younger patients and that THR was indicated in the older patient. This is consistent with the results from the literature [6, 19, 29].
The results of the survey showed a significant correlation between the level of symptoms and the choice for conservative treatment. One case consisted of a 31-year-old patient with minimal complaints (Merle d’Aubigne score 16 out of 18) with a mild dysplasia (Sharp angle 50°, CE angle 14°) and coxa valga (CCD 140°). In this case, 58% advised conservative therapy.
In patients already suffering from hip complaints (although only minor), it is thought that the development of OA is inevitable [11, 14]. Several authors have mentioned that, in these patients especially, early intervention could be rewarding [6, 9, 19, 23]. This view is clearly not shared commonly.
In hips where the main deformity is on the acetabular side, an acetabular realigning procedure is the preferred surgical choice. In hips where the problem on the acetabular side is mild and where there is also a problem on the femoral side, a femoral osteotomy could be just as effective. In our cases, two of these types of patients were included (cases 1 and 3). Those who chose joint-saving surgery were equally divided among PAO and ITO supporters. The available literature shows that good long-term results can be obtained with intertrochanteric osteotomies in these patients [6].
The declining role of osteotomies could also be caused by patient preferences. Modern patients mostly wish to have a quick result, which is easier to obtain with a THR than with an osteotomy. A second patient preference could be that patients are no longer satisfied with the good results that can be obtained with an osteotomy, but want the excellent results that a THR could probably provide. It is important for us to inform patients of the long-term effects that this decision could have and to advise osteotomies in those patients who could benefit from it.
Many orthopaedic surgeons believe that the long-term outcome of a subsequent THR is impaired after a previous osteotomy. This view does not seem to influence the decision as to whether to perform or recommend intertrochanteric osteotomies. In the literature, several reports on THR after osteotomies are available but with conflicting views. However, it appears that the long-term outcome of the THR is not impaired after a previous osteotomy [7].
Our survey shows that, even among experts, the role of intertrochanteric osteotomies is declining. Only a few are performed each year although most surgeons believe they should still be performed today. The current use of intertrochanteric osteotomy is limited to a select group of young and active patients. By identifying the right indications, we should preserve intertrochanteric osteotomies from complete extinction.
References
- 1.Castaing J, Marcillaud G (1981) Varus osteotomy in severe arthrosis of the hip-a long-term study [author’s translation]. Rev Chir Orthop Reparatrice Appar Mot 67:267–277 [PubMed]
- 2.Collert S, Gillstrom P (1979) Osteotomy in osteoarthritis of the hip. A prospective study. Acta Orthop Scand 50:555–561 [DOI] [PubMed]
- 3.DePalma AF, Rothman RH, Klemek JS (1970) Osteotomy of the proximal femur in degenerative arthritis. Clin Orthop Relat Res 73:109–115 [DOI] [PubMed]
- 4.D’Souza SR, Sadiq S, New AM, Northmore-Ball MD (1998) Proximal femoral osteotomy as the primary operation for young adults who have osteoarthrosis of the hip. J Bone Joint Surg Am 80:1428–1438 [DOI] [PubMed]
- 5.Gotoh E, Inao S, Okamoto T, Ando M (1997) Valgus-extension osteotomy for advanced osteoarthritis in dysplastic hips. Results at 12 to 18 years. J Bone Joint Surg Br 79(4):609–615 [DOI] [PubMed]
- 6.Haverkamp D, Eijer H, Patt TW, Marti RK (2006) Multi directional intertrochanteric osteotomy for primary and secondary osteoarthritis-results after 15 to 29 years. Int Orthop 30(1):615–620 [DOI] [PMC free article] [PubMed]
- 7.Haverkamp D, de Jong PT, Marti RK (2006) Intertrochanteric osteotomies do not impair long-term outcome of subsequent cemented total hip arthroplasties. Clin Orthop Relat Res 444:154–160 [DOI] [PubMed]
- 8.Ito K, Matsuno T, Minami A (2005) Intertrochanteric varus osteotomy for osteoarthritis in patients with hip dysplasia: 6-28 years follow up. Clin Orthop Relat Res 433:124–128 [DOI] [PubMed]
- 9.Iwase T, Hasegawa Y, Kawamoto K, Iwasada S, Yamada K, Iwata H (1996) Twenty years’ followup of intertrochanteric osteotomy for treatment of the dysplastic hip. Clin Orthop Relat Res 331:245–255 [DOI] [PubMed]
- 10.Jingushi S, Sugioka Y, Noguchi Y, Miura H, Iwamoto Y (2002) Transtrochanteric valgus osteotomy for the treatment of osteoarthritis of the hip secondary to acetabular dysplasia. J Bone Joint Surg Br 84:535–539 [DOI] [PubMed]
- 11.Klaue K, Durnin CW, Ganz R (1991) The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br 73:423–429 [DOI] [PubMed]
- 12.Kubo T, Horii M, Yamaguchi J, et al (2000) Acetabular labrum in hip dysplasia evaluated by radial MRI. J Rheumatol 27:1955–1961 [PubMed]
- 13.Langlais F, Roure JL, Maquet P (1979) Valgus osteotomy in severe osteoarthritis of the hip. J Bone Joint Surg Br 61-B:424–431 [DOI] [PubMed]
- 14.Leunig M, Beck M, Dora C, Ganz R (2006) Femoroacetabular impingement: trigger for the development of osteoarthritis. Orthopade 35:77–84 [DOI] [PubMed]
- 15.Linde F, Pallesen R (1985) Osteoarthritis of the hip in patients under 60 years of age. A study of the importance of pain at rest as an indication for intertrochanteric osteotomy. Arch Orthop Trauma Surg 104(5):267–270 [DOI] [PubMed]
- 16.Maistrelli GL, Gerundini M, Fusco U, Bombelli R, Bombelli M, Avai A (1990) Valgus-extension osteotomy for osteoarthritis of the hip. Indications and long-term results. J Bone Joint Surg Br 72:653–657 [DOI] [PubMed]
- 17.Marti RK, Chaldecott LR, Kloen P (2001) Intertrochanteric osteotomy for posttraumatic arthritis after acetabular fractures. J Orthop Trauma 15:384–393 [DOI] [PubMed]
- 18.Miegel RE, Harris WH (1984) Medial-displacement intertrochanteric osteotomy in the treatment of osteoarthritis of the hip. A long-term follow-up study. J Bone Joint Surg Am 66:878–887 [DOI] [PubMed]
- 19.Millis MB, Kim YJ (2002) Rationale of osteotomy and related procedures for hip preservation: a review. Clin Orthop 405:108–121 [DOI] [PubMed]
- 20.Morsscher E (1971) Die intertrochantere Osteotomie bei Coxarthrose. Verlag Hans Huber, Bern
- 21.Pecasse GA, Eijer H, Haverkamp D, Marti RK (2004) Intertrochanteric osteotomy in young adults for sequelae of Legg-Calve-Perthes’ disease-a long term follow-up. Int Orthop 28:44–47 [DOI] [PMC free article] [PubMed]
- 22.Pellicci P, Hu S, Garvin K, Salvati E, Wilson PJ (1991) Varus rotational femoral osteotomies in adults th hip dysplasia. Clin Orthop Relat Res 272:162–166 [PubMed]
- 23.Perlau R, Wilson MG, Poss R (1996) Isolated proximal femoral osteotomy for treatment of residua of congenital dysplasia or idiopathic osteoarthrosis of the hip. Five to ten-year results. J Bone Joint Surg Am 78:1462–1467 [DOI] [PubMed]
- 24.Reigstad A, Gronmark T (1984) Osteoarthritis of the hip treated by intertrochanteric osteotomy. A long-term follow-up. J Bone Joint Surg Am 66:1–6 [PubMed]
- 25.Santore RF, Bombelli R (1983) Long-term follow-up of the Bombelli experience with osteotomy for osteoarthritis: results at 11 years. Hip 1983:106–128 [PubMed]
- 26.Schneider R (1966) Mehrjahreresultate eines Kollektivs von 100 intertrochanteren Osteotomien bei Coxarthrose. Helv Chir Acta 33:185–205 [PubMed]
- 27.Teinturier P, Levai JP, Collin JP, Terver S (1982) Intertrochanteric flexion osteotomy as an only alternative to total hip arthroplasty in advanced osteoarthritis. A ten-year follow-up. Clin Orthop Relat Res 166:158–161 [PubMed]
- 28.Toyama H, Endo N, Sofue M, Dohmae Y, Takahashi HE (2000) Relief from pain after Bombelli’s valgus-extension osteotomy, and effectiveness of the combined shelf operation. J Orthop Sci 5:114–123 [DOI] [PubMed]
- 29.Turgeon TR, Phillips W, Kantor SR, Santore RF (2005) The role of acetabular and femoral osteotomies in reconstructive surgery of the hip: 2005 and beyond. Clin Orthop Relat Res 441:188–199 [DOI] [PubMed]
- 30.Weisl H (1980) Intertrochanteric osteotomy for osteoarthritis. A long-term follow-up. J Bone Joint Surg Br 62-B:37–42 [DOI] [PubMed]
- 31.Zaoussis AL, Adamopoulos G, Geraris G, Manoloudis M, Galanis I (1984) Osteotomy for osteoarthritis of the hip. A clinical and radiological survey. Int Orthop 7(4):223–228 [DOI] [PubMed]