Abstract
The functional results of prostheses and osteoarticular grafts for osteosarcoma around the knee joint are not satisfactory because of poor durability and gross distortion of the normal anatomy. We have investigated the functional outcome of intentional marginal excision for osteosarcoma around the knee joint in conjunction with caffeine-potentiated chemotherapy. Twenty-one patients with AJCC stage IIB high-grade osteosarcoma around the knee joint were given three to five preoperative courses of intra-arterial cisplatin and caffeine with or without doxorubicin. The histological response in these 21 patients to preoperative chemotherapy was grade IV (no viable cells) in 19 patients and grade III (only scattered foci of viable cells) in 2. The patients were separated into three groups on the basis of patterns of tumour excision. The first group underwent marginal excision of the proximal fibula, the second underwent epiphysis preservation followed by distraction osteogenesis, and the third underwent joint resection and reconstruction. The mean functional evaluations were 100, 95, and 88%, respectively. No local tumour recurrence was seen at mean follow-up of 97 months. Marginal excision of the proximal fibula resulted in excellent function. Preservation of the epiphysis leads to better function than joint resection.
Résumé
Les résultats fonctionnels des prothèses et des greffes ostéo-articulaires réalisées pour ostéosarcome autour du genou, ne sont pas satisfaisants du fait de leur courte durée de vie, des gros troubles de torsion et de l’importante remise en cause de l’anatomie normale. Nous avons voulu étudier le devenir fonctionnel d’une chirurgie comportant une résection d’ostéosarcome à la limite des marges tumorales au niveau de l’articulation du genou en association avec une chimiothérapie à base de caféine potentialisée. 21 patients présentant un ostéosarcome de stade IIB de haut grade autour du genou ont bénéficié en préopératoire de 3 à 5 cures de cisplatine intra artérielle avec caféine avec ou sans doxorubicine. La réponse histologique chez ces 21 patients à la chimiothérapie préopératoire a été de grade IV (pas de cellules vivantes) chez 19 patients et de grade III avec seulement quelques foyers de cellules vivantes (cellules viables) chez 2 patients. Les patients ont été séparés en trois groupes à partir du type d’excision fémorale. Le premier groupe a bénéficié d’une excision marginale de l’extrémité supérieure du péroné, le second groupe a bénéficié d’une conservation de l’épiphyse, suivi d’un allongement et, le troisième groupe a bénéficié d’une résection de l’articulation avec reconstruction. Le résultat fonctionnel moyen a été respectivement de 100%, 95% et 88%. Il n’y a pas eu de récidive de la tumeur après un suivi moyen de 97 mois. L’excision marginale de l’extrémité supérieure du péroné permet un excellent résultat fonctionnel. La préservation de l’épiphyse permet également d’améliorer la fonction de l’articulation comparée à une résection de celle-ci.
Introduction
Osteosarcoma usually occurs in young patients and most commonly around the knee joint. The five-year survival rate of patients with osteosarcoma treated with chemotherapy and proper surgery can be more than 70% [3, 9, 10]. The most common surgical techniques used to treat osteosarcoma around the knee include resection of the epiphysis and reconstruction with prosthesis, osteoarticular allograft, autoclaved autograft, or a combination. The functional results of prostheses and osteoarticular grafts are not satisfactory because of poor durability, joint instability, incongruity, and gross distortion of the normal anatomy. Most surgeons would not consider preserving the epiphysis when treating osteosarcoma around the knee joint because of the difficulties in reconstruction and the risk of contaminating the tumour site. For this reason, osteosarcoma around the knee joint presents a surgical challenge. No joint replacement can function as well as the normal knee. Recently, a few series in which the epiphysis has been salvaged have been reported [7–9].
Since 1987 the authors have published reports on the possibility of marginal excision for osteosarcoma along with the use of caffeine-assisted chemotherapy [11, 12]. Caffeine can enhance the cytocidal effects of anticancer drugs safely through its deoxyribonucleic acid repair-inhibiting effect [13]. We have demonstrated that caffeine-assisted chemotherapy induced a high rate of complete response in patients with osteosarcoma [12]. Because of the good response achieved with caffeine-potentiated chemotherapy, we have treated a limited number of cases with intra-epiphyseal resection followed by reconstruction using distraction osteogenesis. It is also important to confirm the effectiveness of chemotherapy and accuracy of the preoperative assessment of the extent of intramedullary tumour when a smaller resection margin is being considered. When a good response is documented by at least two of four radiological methods, including plain radiography, MRI, angiography, and 201Tl scintigram, more than 90% tumour necrosis can be expected and minimised excision can be performed [6].
The minimised excision can be expected to result in superior function compared with wide excision such as joint resection. The purpose of this study was to investigate the long-term functional outcome of intentional marginal excision with the focus of osteosarcoma around the knee joint.
Patients and methods
Between 1987 and 2004, 22 patients with AJCC stage IIB high-grade osteosarcoma around the knee joint were treated in our institute. They were routinely investigated by using whole-body scintigraphy, CT of the thorax and affected limb, MRI and angiography of the affected limb, followed by an open biopsy. For the sake of minimised surgery, caffeine was introduced to all patients to increase the efficacy of chemotherapy. They were given three to five preoperative courses of intra-arterial cisplatin (120 mg/m2) and caffeine (1.5 g m−2 day−1 × 3 days) with or without doxorubicin (30 mg m−2 day−1 × 2 days) according to our chemotherapy regimen.
Before the surgery, chemotherapeutic effects were evaluated clinically by plain radiography, MRI, angiography, and thallium-201 (201Tl) scintigraphy. Evidence of a good chemotherapeutic response consisted of sclerotic changes or good delineation of the tumour (observed on plain radiographs), marked shrinkage of any extension of the tumour into soft tissue (demonstrated on MRI), the disappearance of “tumour” vessels (on angiography), or the disappearance of the abnormal accumulation on 201Tl scintigrams. Postoperative chemotherapy was performed on a neoadjuvant basis. One patient was excluded from this study because of poor chemotherapeutic response, and the tumour was excised with wide margin, leaving 21 patients for this study (Table 1).
Table 1.
Clinical characteristics, treatment, and outcomes of 21 patients with osteosarcoma around the knee joint
| Case | Age (years) | Gender | Site | Histologic response | Pattern of excision | Reconstruction method | Outcome | Functional score (%) | Follow up (months) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 15 | M | Fibula | IV | Marginal excision of fibula head | – | CDF | 100 | 128 |
| 2 | 17 | M | Fibula | IV | Marginal excision of fibula head | – | CDF | 100 | 123 |
| 3 | 11 | M | Fibula | IV | Marginal excision of fibula head | – | CDF | 100 | 81 |
| 4 | 14 | F | Fibula | IV | Marginal excision of fibula head | – | CDF | 100 | 27 |
| 5 | 16 | M | Tibia | IV | Epiphysial preservation | DO | Death from hepatitis | 100 | 48 |
| 6 | 42 | F | Tibia | IV | Epiphysial preservation | DO | CDF | 100 | 112 |
| 7 | 14 | M | Tibia | IV | Epiphysial preservation | DO | CDF | 100 | 98 |
| 8 | 17 | M | Tibia | IV | Epiphysial preservation | DO | CDF | 100 | 16 |
| 9 | 17 | M | Tibia | IV | Joint resection | Allograft | NED | 90 | 129 |
| 10 | 14 | Tibia | IV | Joint resection | Prosthesis | CDF | 90 | 72 | |
| 11 | 16 | M | Tibia | III | Joint resection | Prosthesis | NED | 83 | 86 |
| 12 | 9 | F | Femur | IV | Epiphysial preservation | DO | CDF | 100 | 93 |
| 13 | 20 | M | Femur | IV | Joint resection | Prosthesis | CDF | 93 | 163 |
| 14 | 11 | M | Femur | IV | Joint resection | Prosthesis | CDF | 93 | 161 |
| 15 | 13 | F | Femur | IV | Joint resection | Prosthesis | CDF | 93 | 161 |
| 16 | 9 | M | Femur | IV | Epiphysial preservation | DO | CDF | 90 | 54 |
| 17 | 19 | M | Femur | III | Joint resection | Liquid nitrogen-treated bone+prosthesis | CDF | 90 | 6 |
| 18 | 13 | F | Femur | IV | Epiphysial preservation | DO | CDF | 87 | 140 |
| 19 | 21 | M | Femur | IV | Epiphysial preservation | DO | CDF | 87 | 118 |
| 20 | 17 | F | Femur | IV | Joint resection | Autoclaved bone+prosthesis | CDF | 83 | 159 |
| 21 | 13 | F | Femur | IV | Joint resection | Liquid nitrogen-treated bone | NED | 77 | 65 |
DO Distraction osteogenesis, CDF continuous disease free, NED no evidence of disease
Limb-salvaging surgery was conducted by means of intentional marginal excision, which led to the preservation of important structures such as major neurovascular bundles, tendons, ligaments, muscles, and the epiphysis. Tumours were located in the distal femur in ten patients, the proximal tibia in seven, and the proximal fibula in four. The patients were informed that the data from their cases would be submitted for publication, and gave their consent.
The functional evaluation of the patients was performed with use of the revised 30-point functional classification system established by the International Society of Limb Salvage and the Musculoskeletal Tumour Society [1]. This functional score measured six parameters: pain, function, emotional acceptance, use of walking supports, walking ability, and gait. Each parameter is given a value ranging from 0 to 5, according to specific criteria. The individual scores are added together to obtain an overall functional score, with a maximum of 30 points, which then is expressed as a percentage of normal.
The Kaplan-Meier method was used for survival analysis. Event-free survival was defined as the time from a patient’s entry into this study until his or her death with the disease in remission, local recurrence of disease after definitive surgery, development of distant metastases, development of a second malignancy, or last contact. Survival was defined as the time from study entry until death or last contact.
Results
The histological response in the 21 patients to preoperative chemotherapy was grade IV (no viable cells) in 19 patients and grade III (only scattered foci of viable cells) in two. All patients were treated by means of intentional marginal excision. Four cases of the proximal fibula were treated by marginal excision of the fibula head, which preserved the common peroneal nerve, lateral collateral ligament, and biceps femoris tendon. The collateral ligament and biceps tendon were reattached to the tibia. In the distal femur and proximal tibia, the possibility for preservation of the epiphysis was compatible with MRI findings. The epiphysis was preserved in eight patients, and the bone defect was reconstructed by distraction osteogenesis. Joint resection (resection of one or both epiphysis) was performed in nine patients. As for reconstruction, liquid nitrogen-treated or autoclaved bone graft and prosthesis composites were used in two, liquid nitrogen-treated bone graft in one, osteochondral allograft in one, and megaprostheses in five [14].
The patients were separated into three groups on the basis of patterns of tumour excision to compare each functional result. The first group underwent marginal excision of the proximal fibula, the second underwent epiphysis preservation followed by distraction osteogenesis, and the third underwent joint resection and reconstruction. The mean functional evaluations were 100, 95, and 88%, respectively. The overall average functional evaluation of the 21 patients treated with the minimum procedure was 93% of normal. No local tumour recurrence was seen. Complications accompanying this minimised surgery consisted of deep infection, skin necrosis and fracture in two patients each. No revision surgery was performed in this series. Pulmonary metastases developed in four patients at a mean follow-up of 35.8 months. Three patients had no evidence of disease and 17 patients remained disease-free at mean follow-up of 97 months. One patient died from hepatitis. The overall cumulative survival rate was 100% and the event-free survival rate, 78%.
Case presentation
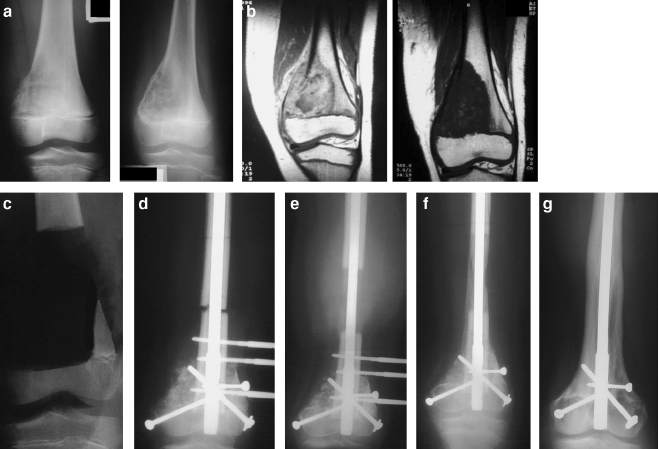
A nine-year-old girl with osteosarcoma in the distal femur underwent neoadjuvant chemotherapy. Tumour decreased markedly on MRI and the tumour stains disappeared on the angiogram. No tumour extension into the epiphysis was observed in the T2-weighted MR image after chemotherapy. The epiphysis of the distal femur was preserved by intentional marginal excision. Total tumour necrosis was observed histologically. After tumour resection, the bone was shortened by 7 cm and the femur was distracted by 9 cm at the diaphysis with an intramedullary nail. The affected limb was overextended by 2 cm to compensate for anticipated limb length discrepancy. The patient has had normal knee joint function and no evidence of disease for 93 months (Fig. 1).
Fig. 1a–g.
A nine-year-old girl. a The tumour of the distal femur shows lytic features on the initial radiograph. After chemotherapy, good margination of the tumour is observed. b Tumour has decreased markedly, and no tumor extension into the epiphysis is observed in the MR image after chemotherapy. c The epiphysis of the distal femur is preserved by intentional marginal excision. d The bone after tumour resection was shortened by 7 cm, and e the femur was distracted by 9 cm at the diaphysis with an intramedullary nail. The affected limb has been overextended by 2 cm to compensate for anticipated limb length discrepancy. f Transfixation. g Remodelling of the juxta-articular bone to its normal shape
Discussion
The natural history of osteosarcoma, which includes development of metastasis and death in spite of amputation, has been dramatically improved by the introduction of chemotherapy. Adjuvant chemotherapy has permitted limb-salvaging which otherwise would not have been possible. One randomised study showed no survival benefit for amputation because limb-salvaging surgery did not increase mortality [10]. In fact, limb-salvaging surgery for osteosarcoma is currently quite a common procedure [3]. The next aim should be to improve survival rate and preserve good limb function. However, more systemic and local control is needed to achieve that goal. We believe that the chemotherapeutic effect is a more important justification than the surgical margin for use of limb-salvaging procedures. Efficient chemotherapy alone improves prognosis and minimises the surgical margin.
The most potent agents in chemotherapy for osteosarcoma are high-dose methotrexate, cisplatin, doxorubicin, and ifosfamide. They are widely used in combination regimens to achieve a synergistic effect. On the other hand, dose escalation of drugs in a dose-intensive chemotherapy regimen did not improve the results of osteosarcoma treatment. Thus, new treatment approaches are needed and many interesting new biological approaches to therapy are being investigated. Most new treatment regimens involve adding new therapies (such as peripheral blood stem-cell support) to existing chemotherapy [2]. However, drugs for efficient treatment of osteosarcoma are still being sought. Caffeine can enhance the cytocidal effects of anticancer drugs, and we have demonstrated that caffeine-potentiated chemotherapy induced a high rate of complete response in patients with osteosarcoma.
Preserving the epiphysis is a surgical challenge and is needed to achieve the best possible functional result [7, 8]. We have little or no way to regenerate the epiphysis adequately. If an osteoarticular allograft or tumour-sterilised autograft is used, the grafted epiphysis never functions as a living one, and eventually it will break down. If a prosthesis is used, both epiphyses are excised, leading to gross distortion of the normal anatomy and questionable durability for young patients. Excision of ligaments and muscles with epiphyses is also a problem because it may cause joint instability and decline of muscle strength.
Previous reports about reconstructive procedures after preserving the epiphysis for osteosarcoma around the knee have included physeal distraction before removing the tumour, the use of frozen allografts, or the use of autoclaved autografts with or without vascularised fibular autografts after tumour resection [4, 5, 9]. Reconstruction with autoclaved autografts and frozen allografts requires prolonged immobilization of the knee. Vascularised bone transfer is limited by length and strength. The well-recognised high incidence of infection or fracture after the use of autoclaved autografts and allografts is a serious concern. Distraction osteogenesis is well known to regenerate living bone of sufficient strength, and osteogenesis, being a biological process, can be expected to form permanent bone [11]. In our series, one patient had a deep infection but did not require amputation. Leg-length discrepancy is not a major problem in children and is managed by subsequent lengthening manoeuvres. Timing affects the outcome of this technique to stretch bone and cause it to hypertrophy. It is necessary to use an intramedullary nail at the appropriate time combined with an external fixator to optimise the outcome.
The functional results in this study confirmed that more preservation of structures leads to better function. Marginal excision of the proximal fibula resulted in excellent function. Preservation of the epiphysis leads to better function than joint resection. If the epiphysis of the distal femur or proximal tibia is not involved with the tumour, the patient may regain normal limb function. As for the next step, reconstruction after resection of the epiphysis is a substantial challenge. Extendable prostheses have been developed and those with internal springs or small motors to elongate the implant without surgery are now available. The ultimate goal is biological reconstruction. Osteochondral grafting techniques that keep cartilage alive or regenerate cartilage in some way will need to be invented. Alternatively, development of an extremely effective therapy without the need for osteosarcoma surgery might be achieved.
Contributor Information
K. Hayashi, Phone: +1-858-4577921, FAX: +1-858-4577921, Email: hayashikatsu830@aol.com
H. Tsuchiya, Phone: +81-76-2652374, FAX: +81-76-2344261, Email: tsuchi@med.kanazawa-u.ac.jp
References
- 1.Amitani A, Yamazaki T, Sonoda J et al (1998) Preservation of the knee joint in limb salvage of osteosarcoma in the proximal tibia. Case report. Int Orthop 22:330–334 [DOI] [PMC free article] [PubMed]
- 2.Arpaci F, Ataergin S, Ozet A et al (2005) The feasibility of neoadjuvant high-dose chemotherapy and autologous peripheral blood stem cell transplantation in patients with nonmetastatic high grade localized osteosarcoma: results of a phase II study. Cancer 104:1058–1065 [DOI] [PubMed]
- 3.Bacci G, Ferrari S, Lari S et al (2002) Osteosarcoma of the limb. Amputation or limb salvage in patients treated by neoadjuvant chemotherapy. J Bone Joint Surg Br 84:88–92 [DOI] [PubMed]
- 4.Canadell J, Forriol F, Cara JA (1994) Removal of metaphyseal bone tumours with preservation of the epiphysis. Physeal distraction before excision. J Bone Joint Surg Br 76:127–132 [PubMed]
- 5.Enneking WF, Dunham W, Gebhardt MC et al (1993) A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop 286:241–246 [PubMed]
- 6.Hoffer FA, Nikanorov AY, Reddick WE et al (2000) Accuracy of MR imaging for detecting epiphyseal extension of osteosarcoma. Pediatr Radiol 30:289–298 [DOI] [PubMed]
- 7.Kumta SM, Chow TC, Griffith J (1999) Classifying the location of osteosarcoma with reference to the epiphyseal plate helps determine the optimal skeletal resection in limb salvage procedures. Arch Orthop Trauma Surg 119:327–331 [DOI] [PubMed]
- 8.Manfrini M, Gasbarrini A, Malaguti C et al (1999) Intraepiphyseal resection of the proximal tibia and its impact on lower limb growth. Clin Orthop 358:111–119 [PubMed]
- 9.Muscolo DL, Ayerza MA, Aponte-Tinao LA et al (2004) Partial epiphyseal preservation and intercalary allograft reconstruction in high-grade metaphyseal osteosarcoma of the knee. J Bone Joint Surg Am 86:2686–2693 [DOI] [PubMed]
- 10.Simon MA, Aschliman MA, Thomas N et al (1986) Limb salvage treatment versus amputation for osteosarcoma of the distal end of the femur. J Bone Joint Surg Am 68:1331–1337 [PubMed]
- 11.Tsuchiya H, Abdel-Wanis ME, Sakurakichi K et al (2002) Osteosarcoma around the knee. Intraepiphyseal excision and biological reconstruction with distraction osteogenesis. J Bone Joint Surg Br 84:1162–1166 [DOI] [PubMed]
- 12.Tsuchiya H, Tomita K, Mori Y et al (1999) Marginal excision for osteosarcoma with caffeine assisted chemotherapy. Clin Orthop Relat Res 358:27–35 [DOI] [PubMed]
- 13.Tsuchiya H, Tomita K, Yasutake H et al (1994) Intraarterial cisplatin and caffeine with/without doxorubicin for musculoskeletal high-grade spindle cell sarcoma. Oncology Reports 1:27–36 [DOI] [PubMed]
- 14.Yamamoto N, Tsuchiya H, Tomita K (2003) Effects of liquid nitrogen treatment on the proliferation of osteosarcoma and the biomechanical properties of normal bone. J Orthop Sci 8:374–380 [DOI] [PubMed]