Abstract
The articular facets of the cervical spine have been well addressed; however, little information is available on the relationship of the superior facets of the cervical spine to traumatic dislocation in the literature. Morphometric analyses of the superior facets of 30 dried cervical spines from C3 to C7 were performed to determine any morphological differences. The angle of the superior facet with respect to the transverse plane was also measured on computed tomography (CT) scans of 30 patients having neck injury without fracture/dislocation. The vertical and surface lengths of the superior facet were significantly lower (P < 0.01) at C6–C7 levels than at C3–5 levels. The anteroposterior diameter of the superior facet was smaller (P < 0.05) at C6 and C7 levels compared to C3–5 levels. Although the superior facet joint surface is in a more coronal orientation in lower cervical vertebrae, the inclination of the superior facet is more horizontal relative to the transverse plane when measured in vivo. A combination of lower height, smaller anteroposterior diameter of the superior facet, and a more horizontally oriented superior facet at C6 and C7 levels in vivo may explain the predilection of translation relative to one another in the lower cervical spine.
Résumé
Les facettes articulaires de la colonne cervicale sont bien analysées cependant une meilleure connaissance des relations de l’articulaire supérieure lors des traumatismes avec luxations de la colonne dans la littérature est possible. L’analyse morphométrique de l’articulaire supérieure a été analysée sur 30 colonnes cervicales de cadavres, de C3 à C7, de façon à analyser les différences morphologiques. L’angle supérieur de l’articulaire a été mesuré sur le scanner de 30 patients ayant présenté un traumatisme cervical sans fracture, ni luxation. Les dimensions verticales et les surfaces de l’articulaire supérieure sont, significativement, moins importantes au niveau C6 et C7 qu’au niveau C3 à C5 (p < 0.01). Le diamètre antéropostérieur de l’articulaire supérieure est également plus petit au niveau de C6 C7 qu’au niveau de C3 C5 (p < 0.05). De la même façon, l’articulaire supérieure est dans un plan plus frontal dans la partie basse de la colonne. L’inclinaison de cette articulaire est, de même, plus horizontale par rapport au plan transversal, mesure in vivo. La combinaison de tous ces facteurs : dimensions moins importantes, petits diamètres, antéropostérieur et facettes supérieures de l’articulaire plus horizontale en C6 C7, expliquent la fréquence des translations relatives possibles des vertèbres dans la partie basse de la colonne et donc la fragilité de cette zone.
Introduction
Traumatic unilateral and bilateral cervical facet dislocations are not uncommon. Previous studies have focused on clinical and imaging studies [2, 8–10, 13, 14]. Hyperflexion/distraction with or without rotation have been implicated as the mechanism of injury for the bilateral and unilateral cervical facet dislocation, respectively. However, anatomical factors responsible for predilection of ventral translation of one vertebra relative to the adjacent one in the cervical spine are not clear. The dimensions and inclinations of the superior facet in the lower cervical vertebrae may be predisposing factors in development of traumatic slippage of superior vertebrae against inferior vertebrae. The current study investigates any predisposing anatomic and morphometric features of the superior facet from C3 to C7 levels which may provide the anatomic basis for higher frequency of dislocation or subluxation in the lower cervical spine.
Materials and methods
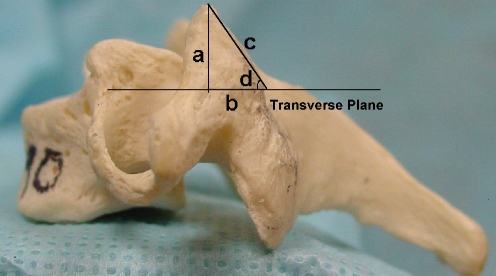
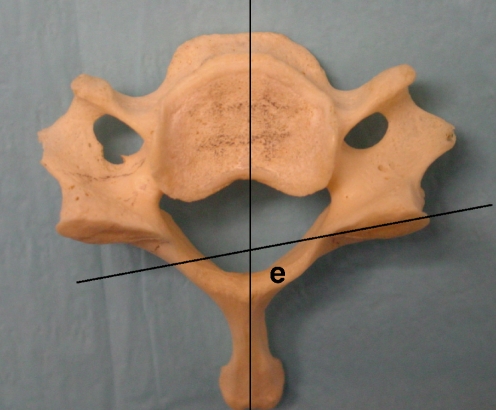
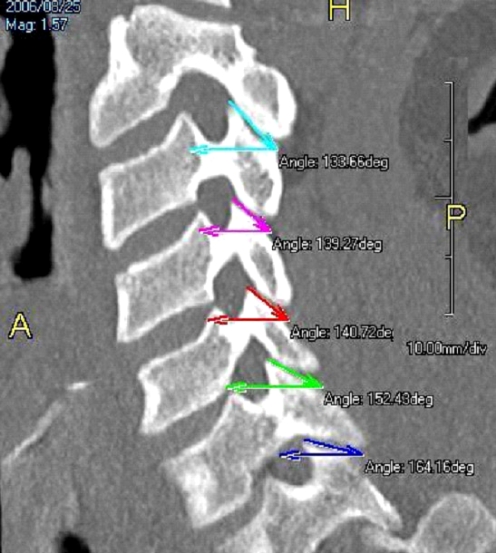
Thirty (18 male, 12 female, mean age: 56 years, range: 42–70) dried cervical spines from C3 to C7 (a total of 150 cervical vertebrae) were obtained from the Department of Anatomy. The specimens used were free from congenital anomaly. Three linear and two angular parameters were then bilaterally measured on the cervical superior facets. The three linear dimensions were measured by projecting a right-angled triangle on the lateral view of the cervical superior facet. This triangle was created by drawing a vertical line along the anterior edge of the superior facet as a reference line (vertical length, a) (Fig. 1). A perpendicular line to the above reference line was drawn starting from the most inferior margin of the superior facet (anteroposterior diameter, b). Finally, a line connecting the most superior and inferior edges of the superior facet surface was drawn to complete the triangle (surface length, c). The angles between the superior facet with the transverse plane (d in Fig. 1) and the sagittal plane (e in Fig. 2) were measured with the vertebrae placed on a flat table. As the vertebrae in normal persons are in a lordotic alignment, angles were also measured between the transverse plane and the superior facets on computed tomography (CT) scans of 30 people (15 men, 15 women, average: 39 years, range: 27–58) who had a CT scan for injury to the neck dislocation/dislocation(Fig. 3).
Fig. 1.
Schematic illustration of the measurements on the cervical superior facet: a vertical length, b anteroposterior diameter, c surface length, d facet angle with respect to transverse plane
Fig. 2.
e Facet angle with respect to sagittal plane
Fig. 3.
Illustration of facet angle with respect to transverse plane on reconstructed CT image
All measurements were performed using a caliper (Absolute Digimatic Solar Caliper, Mitutoyo, Japan with an accuracy of ± 0.02 mm) and goniometer with the vertebrae placed in a horizontal position. Computed tomography (CT) was performed with 1-mm slice thickness using Toshiba Aquilion 16 slice scanner (Toshiba Medical Systems Europe, Zoetermeer, Netherlands). Reconstructed CT was obtained in the plane passing through the center of C3, C4, C5, C6, and C7 pedicles on the right and left sides. The angles between the superior facet and the transverse plane were measured with Aquarius Image software (Microsoft Corp., Redmond, WA, USA) in the TeraRecon Aquarius workstation of CT.
All measurements were recorded three times by a single author and an average of the three observations was used for all statistical evaluations. The measured values were expressed as mean ± standard deviation. The difference in various parameters between cervical vertebral levels was analyzed with a single factor analysis of variance (ANOVA) and differences between the two sides and sexes with Student’s t-test.
Results
All linear measurements are shown in Table 1 and the angular parameters in Table 2 (dried specimens) and Table 3 (in vivo, CT scans). No statistical differences were found in any measurement for either side or sex. The vertical length of the superior facet decreased from C3 to C7 (from R 8.2 ± 0.6/L 8.4 ± 0.5 mm at C3 to R 6.6 ± 1.3/L 6.8 ± 1.0 mm at C7). The anteroposterior diameter of the superior facet decreased from C3 to C7 (from R 8.6 ± 0.5/L 8.7 ± 0.8 mm at C3 to R 6.9 ± 1.6/L 6.8 ± 1.2 mm at C7) and was significantly smaller at C6–7 than at C3–5 (P < 0.05). The surface length of the superior facet gradually decreased from C3 to C7 (from R 10.2 ± 1.1/L 10.5 ± 0.7 mm at C3 to R 8.1 ± 1.1/L 7.9 ± 0.8 mm at C7). Both the surface and vertical heights were significantly lower at C6–7 than at C3–5 (P < 0.0 l).
Table 1.
Linear parameters of superior facet of C3–7 measured on 30 dried cervical spines (mean ± standard deviation). All values are in millimeters. VL vertical length, AP anteroposterior diameter, SL surface length
| Level (N = 30) | VL | APD | SL | |||
|---|---|---|---|---|---|---|
| Right | Left | Right | Left | Right | Left | |
| C3 | 8.2 ± 0.6 | 8.4 ± 0.5 | 8.6 ± 0.5 | 8.7 ± 0.8 | 10.2 ± 1.1 | 10.5 ± 0.7 |
| C4 | 8.4 ± 0.8 | 8.3 ± 0.6 | 8.9 ± 0.6 | 8.7 ± 1.2 | 9.7 ± 1.1 | 9.8 ± 0.8 |
| C5 | 7.3 ± 0.9 | 7.5 ± 1.4 | 8.7 ± 1.2 | 8.6 ± 0.7 | 9.2 ± 1.3 | 9.4 ± 1.0 |
| C6 | 6.9 ± 1.3 | 7.1 ± 0.9 | 7.7 ± 0.6 | 7.6 ± 0.8 | 8.3 ± 0.9 | 8.2 ± 0.7 |
| C7 | 6.6 ± 1.3 | 6.8 ± 1.0 | 6.9 ± 1.6 | 6.8 ± 1.2 | 8.1 ± 1.1 | 7.9 ± 0.8 |
Table 2.
Inclination of superior facet of C3–7 measured on 30 dried cervical spines (mean ± standard deviation)
| Level | Transverse planea | Sagittal planeb | ||
|---|---|---|---|---|
| Right | Left | Right | Left | |
| C3 | 49.5 ± 4.1° | 51.7 ± 5.2° | 69.8 ± 11.1° | 70.9 ± 10.7° |
| C4 | 44.5 ± 6.2° | 45.3 ± 4.6° | 77.2 ± 9.3° | 79.8 ± 11.5° |
| C5 | 40.5 ± 5.1° | 39.8 ± 6.7° | 91.8 ± 10.9° | 90.7 ± 9.8° |
| C6 | 42.3 ± 4.4° | 43.2 ± 5.4° | 92.3 ± 11.5° | 93.5 ± 9.4° |
| C7 | 44.2 ± 4.6° | 45.8 ± 6.2° | 94.5 ± 7.7° | 94.3 ± 10.2° |
aAngulations of cervical superior facet with respect to transverse plane
bAngulations of cervical superior facet with respect to sagittal plane
Table 3.
Inclination of superior facet of C3–7 with respect to transverse plane as measured on the CT scan (mean ± standard deviation)
| Level | Transverse plane | |
|---|---|---|
| R | L | |
| C3 | 40.64 ± 6.38° | 39.47 ± 5.68° |
| C4 | 35.21 ± 6.34° | 36.13 ± 6.41° |
| C5 | 32.51 ± 6.54° | 33.18 ± 5.86° |
| C6 | 30.11 ± 5.56° | 29.35 ± 5.31° |
| C7 | 22.22 ± 5.84° | 21.28 ± 5.21° |
The angle of the superior facet with respect to the transverse plane in the dried bone specimens followed a U-shaped pattern with a highest inclination of R 49.5 ± 4.1°/L 51.7 ± 5.2° at C3 followed by a low of R 40.5 ± 5.1°/L 39.8 ± 6.7° at C5. This was followed by a gradual increase in the inclination angle to a high of R 44.2 ± 4.6°/L 45.8 ± 6.2° at C7. Similarly, the angle between the superior facet and the transverse plane as mreasured on the CT scan showed a gradual decrease in inclination from C3 to C7 (from R 40.64 ± 6.38°/L 39.47 ± 5.68° at C3 to R 22.22 ± 5.84°/L 21.28 ± 5.21° at C7). This decrease in angle was significantly smaller at C6–7 than at C3–5 (P < 0.05).
The angle of the superior facet with respect to the sagittal plane gradually increased from C3 to C7 (from R 69.8 ± 11.1°/L 70.9 ± 10.7° at C3 to R 94.5 ± 7.7°/L 94.3 ± 10.2° at C7) and was significantly greater at C6–7 than at C3–4 (P < 0.01).
Discussion
C5–6 and C6–7 levels are most commonly involved in uni- and bilateral facet dislocation of the cervical spine [3, 7–10, 13, 14]. O’Brien et al. [10] reported that unilateral facet dislocation occurred in 43% of patients and bilateral facet dislocation in 57% patients with cervical spine dislocations. Bilateral facet dislocation was most common at the C6–7 level and unilateral facet dislocation at the C5–6 level in their series. Axial rotation exists in unilateral facet dislocation [1]. Maiman et al. [9] described 28 patients with bilateral facet dislocation. The most common levels were C5–6 and C6–7, having ten each (total 71.4%). Bilateral facet dislocation is associated with significant soft tissue injury, including rupture of the posterior ligamentous complex, facet joint capsules, annulus fibrosus, and usually the anterior and posterior longitudinal ligaments [1, 2, 4, 16] with both facets remaining intact but dislocated. The inferior facet of the upper vertebra slides over the tip of the superior facet of the lower vertebra. The translational instability may be caused by abnormal forward (spondylolisthesis) or backward (retrospondylolisthesis) displacements. The dimensions and inclinations of the superior facet may decide the predilection of translation between the superior and inferior facets. Regardless of soft tissue restraints, the strength of bony constraint provided by superior facet joints of lower cervical vertebrae following rotatory and translatory forces is weakened because the joint plane is more horizontal. However, the upper cervical vertebrae are in more sagittal and vertical orientations, which may resist anteroposterior and rotatory forces.
Grobler et al. [6] correlated degenerative spondylolisthesis with increased sagittal orientation of facets in the lumbar spine. Although the current study indicated that the superior facet in lower cervical levels is oriented more coronally, smaller articular dimensions and a more horizontally oriented superio7r facet may result in compromise of its ability to resist forward translation or dislocation. Nonspondylolytic spondylolisthesis is defined as forward slipping of one vertebral body upon another, but with an intact vertebral arch [5]. Although degenerative slippage of the vertebral bodies is well described in the lumbar spine, the presence of these abnormalities in the cervical spine has received little attention. In degenerative spondylolisthesis, degenerated discs and facet joints with laxity of the annulus fibrosus and capsules sometimes increase the mobility and translational instability of facet joints, especially in lower cervical levels.
The superior facets in lower cervical vertebrae with less inclination relative to the transverse plane may weaken the effective check mechanism, preventing a vertebra from slipping forward on the vertebra below. However, this kind of slippage appears to be arrested in a limited distance with facet subluxation in the sagittal plane. The acute traumatic cervical facet dislocation is most likely to be complete translation of the inferior facet of the superior vertebra to the most anterior margin of the superior facet of the inferior vertebra in the sagittal plane. Sharma et al. [15] have demonstrated that the flexion moment of anterior shear loading moves the facets away from each other in the lumbar spine. More horizontally oriented superior facets in the lower cervical spine may predispose to facet translational or rotational instability if the hyperflexion/distraction motion and anterior shear forces are applied on the cervical spine. Therefore, there may be a tendency for the lower cervical vertebrae to dislocate ventrally because of more horizontally oriented superior facets.
Panjabi et al. [12] reported quantitative three-dimensional surface geometry in the form of linear, area, and angular dimensions of the articular facets of the spine. However, their relevance to traumatic facet dislocation has not been addressed in the literature. The present study demonstrated that the superior facet in the lower cervical vertebrae has lower vertical and surface lengths, smaller anteroposterior diameter, and a more horizontal orientation with respect to the transverse plane compared to the C3 and C4 vertebrae. The angles between the superior facet and the transverse plane were further reduced, when measured in vivo (CT scan). This increased horizontal orientation is due to the normal lordotic posture of the cervical spine which may place the lower cervical vertebrae at an increased risk for dislocation or subluxation. Though it is impossible to predict the position of the cervical spine at the time of an accident, still, a normal lordotic spine in neutral position at that time places the lower vertebrae at a higher risk of dislocation.
Panjabi et al. [12] also demonstrated that the area of the superior facet in lower cervical levels was less than that in upper cervical levels. According to them, the horizontal inclination of the superior facet follows a U-shaped pattern (R 48.8°/L 55.2° at C3 to R 59.4°/L 51.6° at C7, with the lowest at C5 measuring R 45.8°/L 45.3°). We had similar findings in the current study. On the other hand, Pal et al. [11] reported a progressively increasing horizontal inclination (R 44.80°/L 46.83° at C3 to R 65.26°/L 64.13° at C7) from a study involving 30 dry male cervical columns. Panjabi et al. [12] also reported posteromedial orientation of all the superior facets from C3 to C7, whereas there was posterolateral orientation from C5 in the present study and Pal et al.’s [11] study.
Anatomically, there is (1) a change from a lordotic to a kyphotic alignment, (2) a firmly stable thoracic cage below C7, (3) increased mobility in the lower cervical segment as compared with the thoracic spine, (4) smaller dimensions of superior facets, and (5) more horizontally oriented superior facets when measured in vivo. All the above anatomic features of the lower cervical levels may be predisposing factors in development of facet dislocation or subluxation. Therefore, it is not surprising that the majority of dislocations or subluxations occurred at the lower cervical levels as a result of the anatomic features of that region. However, we cannot exclude multiple other factors involved in the lower cervical dislocation including position of the neck, loading and directions of applied forces, action of muscles, rate and magnitude of loading, and patients’ factors such as generalized elasticity, bone density, etc.
In conclusion, our anatomic studies further elucidate the relationship of the superior facet to traumatic dislocation of the cervical spine.
References
- 1.Bauze RJ, Ardran GM (1978) Experimental production of forward dislocation of the human cervical spine. J Bone Joint Surg Br 60-B:239–245 [DOI] [PubMed]
- 2.Beatson TR (1963) Fractures and dislocations of the cervical spine. J Bone Joint Surg Br 45-B:21–35
- 3.Beyer CA, Cabanela ME, Berquist TH (1991) Unilateral facet dislocations and fracture-dislocations of the cervical spine. J Bone Joint Surg Br 73(6):977–981 [DOI] [PubMed]
- 4.Burke CD, Berryman D (1971) The place of closed manipulation in the management of flexion-rotation dislocations of the cervical spine. J Bone Joint Surg Br 53-B:165–182 [PubMed]
- 5.Gehweiler JA Jr, Osborne RL Jr, Becker RF (1980) The radiology of vertebral trauma. Saunders, Philadelphia, p 432
- 6.Grobler LJ, Robertson PA, Novotny JE, Pope MH (1993) Etiology of spondylolisthesis: assessment of the role played by lumbar facet joint morphology. Spine 18:80–91 [DOI] [PubMed]
- 7.Johnson MG, Fisher CG, Boyd M, Pitzen T, Oxland TR, Dvorak MF (2004) The radiographic failure of single segment anterior cervical plate fixation in traumatic cervical flexion distraction injuries. Spine 29(24):2815–2820 [DOI] [PubMed]
- 8.Mahale YJ, Silver JR (1992) Progressive paralysis after bilateral facet dislocation of the cervical spine. J Bone Joint Surg Br 74-B:219–223 [DOI] [PubMed]
- 9.Maiman DJ, Barolat G, Larson SJ (1986) Management of bilateral locked facets of the cervical spine. Neurosurgery 18:542–547 [DOI] [PubMed]
- 10.O’Brien PJ, Schweigel JF, Thompson WJ (1982) Dislocations of the lower cervical spine. J Trauma 22:710–714 [DOI] [PubMed]
- 11.Pal GP, Routal RV, Saggu SK (2001) The orientation of the articular facets of the zygapophyseal joints at the cervical and upper thoracic region. J Anat 198 (Pt 4):431–441 [DOI] [PMC free article] [PubMed]
- 12.Panjabi MM, Oxland T, Koichiro T, Goel V, Duranceau J, Krag M (1993) Articular facets of the human spine: quantitative three-dimensional anatomy. Spine 18:1298–1310 [DOI] [PubMed]
- 13.Rorabeck CH, Rock MG, Hawkins RJ, Bourne RB (1987) Unilateral facet dislocation of the cervical spine: an analysis of the results of treatment in 26 patients. Spine 12:23–27 [DOI] [PubMed]
- 14.Shapiro SA (1993) Management of unilateral locked facet of the cervical spine. Neurosurgery 33:832–837 [DOI] [PubMed]
- 15.Sharma M, Langrana NA, Rodriguez 1 (1995) Role of ligaments and facets in lumbar spinal stability. Spine 20:887–900 [DOI] [PubMed]
- 16.Sonntag VKH (1981) Management of bilateral locked facets of the cervical spine. Neurosurgery 8:150–152 [DOI] [PubMed]