Abstract
Aims
We extend the literature on the association of early onset of drug use and estimated risk for developing a substance use disorder (SUD) by investigating the risk that recent-onset of alcohol and cannabis use confers for developing a substance use disorder at each chronological age of adolescence and young adulthood (12 – 21-years-old).
Design
Using 2003 data from the National Survey on Drug Use and Health (SAMHSA, 2004), we computed separate risk indices for developing an alcohol and cannabis use disorder for recent (prior 2 years) alcohol and cannabis users, respectively, at each age from 12- to 21-years of age, and compared estimated risk to recent–onsets users among respondents age 22-26.
Findings
The results indicated that the teenage years were strongly linked to an elevated risk status. The odds ratio (OR) of having a prior year alcohol use disorder (AUD) among recent onset alcohol users was significantly elevated for youth at ages 14, 16, 17 and 18 (range of ORs = 2.0 – 2.1) compared to the estimated risk for AUD among recent onset users aged 22-26. For cannabis, we obtained significantly elevated ORs for a cannabis use disorder (CUD) at each of teenage years (ages 12 -18; range of ORs = 3.9 – 7.2), when compared to older recent onset users (aged 22-26).
Conclusions
These data provide further epidemiological support that adolescence is a particularly vulnerable period for developing a SUD.
Keywords: Early onset alcohol and cannabis use, Estimated risk for a substance use disorder
1. Introduction
Several population- and clinical-based studies have documented that drug use during youth contributes to an elevated risk for developing a substance use disorder (SUD), starting with the publication by Robins and Przybeck (1985), and followed by several more recent analyses of survey data (DeWit et al., 2000; Grant & Dawson, 1997; Grant et al., 2001; Hingson et al., 2006; Nelson & Wittchen, 1998; Substance Abuse and Mental Health Administration, SAMHSA, 2005), and several prospective studies have also highlighted the reliable association of early onset of use and later drug use problems, including a substance use disorder (e.g., Brook et al., 2002; Lynskey et al., 2003; McGue et al., 2001).
The observed link between early onset of drug taking and increased risk of a SUD is important to the drug abuse literature for several reasons (Chen et al., 2005): the association between early onset and estimated SUD risk held up for over two decades of research and across diverse demographic groups (e.g., Grant & Dawson, 1998) and in other countries (e.g., Nelson & Wittchen, 1998; SAMHSA, 2005); the onset of use variable is relatively easy to measure, especially in the context of other more complex risk factors that represent the wide range of individual, peer, family and community risk factors reported in a vast literature (Hawkins et al., 1992); and this risk factor readily accommodates prevention programs that need to target their efforts toward a reliable and relatively universal factor (Winters et al., in press).
The link between early onset use and estimated risk for SUDs may surely be influenced by the fact that early onset users accumulate more exposure to the drug and thus are at higher risk to develop a drug problem, compared to late onset users who have less exposure to drug involvement. But mechanisms other than duration of drug use are emerging as also important to consider. Two reports by Anthony and colleagues have analyzed national survey data to show that the risk afforded to early onset use is not just an artifact of exposure time (Anthony & Petronis, 1995; Chen et al., 2005). The recent report is particularly relevant to the present paper. They examined findings from the National Household Survey on Drug Abuse conducted during 2000-2001 of a representative sample of U.S. residents ages 12 and older (SAMHSA 2001, 2002). The analysis estimated the risk of becoming cannabis dependent among those whose first use of cannabis occurred within twenty-four months prior to taking the survey. Excess risk of cannabis dependence was the highest in the early to late adolescent age groups (age 12-18-years-old), with the highest rate at around the 14-15-year-old range. In addition, family incomes less than US$ 20,000 and those that used three or more drugs before the first use of cannabis was also associated with elevated risk.
The extant literature provides a basis to view both chronological age and age of onset as vital risk factors. Despite the fact that the association of early onset of drug use, age and progression to abuse or dependence has been studied in some detail, there is room to extend this work. To date, this body of work provides only a general picture of how chronological age and early onset use contribute to risk for SUD. Our research question is this: To what extent is there an elevated risk of developing alcohol and cannabis use disorders at each chronological age of youth among those who are recent-onset users? There are no published reports that have examined this research question at each chronological age. Specifically, we explored the likelihood among recent (within the prior 2 years) onset users of alcohol and recent onset users of cannabis of having a current (prior year) DSM-IV-defined (American Psychiatric Association, 1994) substance use disorder as a function of age of the respondent, based on responses to the 2003 NSDUH (SAMHSA, 2004). It is our expectation that the younger years will continue to reveal a strong link to drug use vulnerability when chronological age is more closely examined. A better understanding of the association of recent use, chronological age and estimated risk for developing drug problems will help further clarify the risk pathways toward SUDs for young people.
2. Method
2.1 Participants
The study sample (N = 55,230) represents the public use file from the full 2003 NSDUH data set of representative individuals in the United States (N = 67,784) (SAMHSA, 2004). The target sample for the study are youth respondents (n = 27,708), which we define as the 12-21-year-old range. We wanted to capture both the core teenage years (12-18-years-old), as well as young adulthood (19-21-years-old). The older sample (age 22-26 and older) is included as a comparison (reference) group.
The demographic breakdowns among recent-onset alcohol and recent-onset cannabis users, as well as those that met a DSM-IV-defined alcohol use disorder (AUD) and cannabis use disorder (CUD), are shown in Tables 1 and 2, respectively. Weighted and unweighted percentages are presented. For alcohol, 4074 individuals were identified as recent alcohol users (unweighted 7.3% of total sample) and 334 met criteria for a current AUD (unweighted 0.06% of total sample). For cannabis, 2176 individuals were identified as recent cannabis users (unweighted 3.9 % of total sample) and 266 met criteria for a current CUD (unweighted 0.05% of total sample).
Table 1.
Demographic characteristics among recent-onset alcohol users (prior 2 years) and those meeting criteria for alcohol abuse or dependence disorder (prior year)
| Recent-Onset Alcohol Users | Alcohol Abuse or Dependence | |||||
|---|---|---|---|---|---|---|
| n | % uwta | % wtb | n | % uwt | % wt | |
| All study sample | 4074 | 100 | 100 | 334 | 100 | 100 |
| Sex | ||||||
| Male | 1829 | 44.9 | 44.6 | 143 | 42.8 | 45.5 |
| Female | 2245 | 55.1 | 55.4 | 191 | 57.2 | 54.5 |
| Age of respondent | ||||||
| 22-26 | 243 | 6.0 | 8.8 | 9 | 2.7 | 5.2 |
| 21 | 185 | 4.5 | 6.2 | 11 | 3.3 | 3.8 |
| 20 | 147 | 3.6 | 4.5 | 6 | 1.8 | 2.6 |
| 19 | 282 | 6.9 | 7.7 | 19 | 5.7 | 7.4 |
| 18 | 405 | 9.9 | 11.0 | 40 | 12.0 | 11.2 |
| 17 | 554 | 13.6 | 12.3 | 51 | 15.3 | 13.4 |
| 16 | 653 | 16.0 | 14.5 | 62 | 18.6 | 18.4 |
| 15 | 662 | 16.2 | 14.7 | 55 | 16.5 | 15.0 |
| 14 | 489 | 12.0 | 10.5 | 45 | 13.5 | 12.4 |
| 13 | 316 | 7.8 | 6.9 | 26 | 7.8 | 7.4 |
| 12 | 138 | 3.4 | 2.9 | 10 | 3.0 | 3.2 |
| Race/ethnicity | ||||||
| White | 2498 | 61.3 | 59.2 | 200 | 59.9 | 63.0 |
| African American | 584 | 14.3 | 15.8 | 41 | 12.3 | 13.9 |
| Hispanic | 675 | 16.6 | 18.9 | 53 | 15.9 | 15.7 |
| Family income | ||||||
| 0-US$ 19,999 | 969 | 23.8 | 22.5 | 81 | 24.3 | 21.5 |
| US$ 20,000-US$ 49,999 | 1466 | 36.0 | 36.0 | 118 | 35.3 | 31.8 |
| US$ 50,000-US$ 74,999 | 710 | 17.4 | 16.7 | 62 | 18.6 | 17.9 |
| US$ 75,000 or above | 929 | 22.8 | 24.8 | 73 | 21.9 | 28.8 |
| Population density | ||||||
| MSAc of 1 million plus | 1440 | 35.3 | 46.1 | 104 | 31.1 | 44.0 |
| MSA < 1 million | 1523 | 37.4 | 33.5 | 119 | 35.6 | 31.0 |
| Residence not in a MSA | 1111 | 27.3 | 20.4 | 111 | 33.2 | 25.0 |
| Used cannabis prior to starting use of alcohol | ||||||
| Yes | 203 | 5.0 | 4.3 | 18 | 5.4 | 7.0 |
| No | 3871 | 95.0 | 95.7 | 316 | 94.6 | 93.0 |
unweighted.
weighted.
metropolitan statistical area of residence.
Table 2.
Demographic characteristics among recent-onset cannabis users (prior 2 years) and those meeting criteria for cannabis abuse or dependence disorder (prior year)
| Recent-Onset Cannabis Users | Cannabis Abuse or Dependence | |||||
|---|---|---|---|---|---|---|
| n | % uwta | % wtb | n | % uwa | % wtb | |
| All study sample | 2176 | 100 | 100 | 266 | 100 | 100 |
| Sex | ||||||
| Male | 1030 | 47.3 | 48.3 | 128 | 48.1 | 47.7 |
| Female | 1146 | 52.7 | 51.7 | 138 | 51.9 | 52.3 |
| Age of respondent | ||||||
| 22-26 | 135 | 6.3 | 11.8 | 4 | 1.5 | 1.4 |
| 21 | 68 | 3.1 | 3.5 | 3 | 1.1 | 1.4 |
| 20 | 102 | 4.7 | 5.3 | 7 | 2.6 | 2.3 |
| 19 | 162 | 7.4 | 9.1 | 13 | 4.9 | 8.0 |
| 18 | 235 | 10.8 | 11.5 | 30 | 11.3 | 13.6 |
| 17 | 358 | 16.5 | 14.7 | 38 | 14.3 | 16.1 |
| 16 | 384 | 17.6 | 15.9 | 59 | 22.2 | 17.7 |
| 15 | 342 | 15.7 | 13.7 | 56 | 21.1 | 21.9 |
| 14 | 248 | 11.4 | 9.7 | 35 | 13.2 | 11.8 |
| 13 | 109 | 5.0 | 3.6 | 19 | 7.1 | 5.2 |
| 12 | 33 | 1.5 | 1.2 | 2 | 0.8 | 0.5 |
| Race/ethnicity | ||||||
| White | 1406 | 64.6 | 65.1 | 168 | 63.2 | 64.9 |
| African American | 289 | 13.3 | 13.8 | 33 | 12.4 | 11.1 |
| Hispanic | 313 | 14.4 | 15.6 | 46 | 17.3 | 17.0 |
| Family income | ||||||
| 0-US$ 19,999 | 559 | 25.7 | 23.6 | 55 | 20.7 | 17.9 |
| US$ 20,000-US$ 49,999 | 786 | 36.1 | 35.4 | 102 | 38.3 | 37.4 |
| US$ 50,000-US$ 74,999 | 341 | 15.7 | 15.5 | 44 | 16.5 | 15.7 |
| US$ 75,000 or above | 490 | 22.5 | 25.6 | 65 | 24.4 | 29.0 |
| Population density | ||||||
| MSA of 1 million plus | 712 | 32.7 | 42.8 | 92 | 34.6 | 44.5 |
| MSA < 1 million | 849 | 39.0 | 35.1 | 103 | 38.7 | 36.3 |
| Residence not in a MSA | 615 | 28.3 | 22.1 | 71 | 26.7 | 19.2 |
| Used alcohol prior to starting use of cannabis | ||||||
| Yes | 317 | 14.6 | 14.6 | 41 | 15.4 | 17.7 |
| No | 1859 | 85.4 | 85.4 | 225 | 84.6 | 82.3 |
unweighted.
weighted.
2.2 Survey Assessment
Sponsored by SAMHSA, the NSDUH (and its predecessor, National Household Survey on Drug Abuse) has been conducted since 1971 in order to provide a national estimate of the prevalence and incidence of illegal drug, alcohol, and tobacco use in the civilian, noninstitutionalized population aged 12 or older in the United States. The survey also includes information about formal diagnostic criteria for substance abuse and dependence, as well as about mental health problems and receipt of substance abuse and mental health services.
A full description of the sampling design and data collection procedures can be found at http://www.oas.samhsa.gov/2k3/NSDUH/nsduh.htm. Briefly, NSDUH collects information from residents of households, noninstitutional group quarters (e.g., shelters, rooming houses, dormitories), and civilians living on military bases. The sample employs a 50–State design with an independent, multistage area probability sample for each State and the District of Columbia. The design over-samples youths and young adults, so that each State's sample is distributed equally among three age groups (12 to 17 years, 18 to 25 years, and 26 years or older). The data collection method is in–person interviews conducted with a sample of individuals at their place of residence. Prior to 1999, the NSDUH used a paper–and–pencil interviewing (PAPI) methodology. Since 1999, the interview has been carried out with year using a combination of computer–assisted personal–interviewing (CAPI) conducted by the interviewer for some basic demographic information and audio computer–assisted self–interviewing (ACASI) for most of the questions. ACASI provides a highly private and confidential means of responding to questions to increase the level of honest reporting of illegal drug use and other sensitive behavior.
Information for the 2003 NSDUH (SAMHSA, 2004) was collected continuously from January 1 through December 31. The weighted screening response rate was 91 percent and the weighted interview response rate was 77 percent (based on the original sample, N = 67,784).
2.3 Variables
Illegal drug, alcohol and tobacco use is asked in terms of lifetime, past year, and past month. Questions pertaining to the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM–IV) (American Psychiatric Association, 1994) criteria for substance abuse and dependence disorders refer to the past year. Nine specific classes of drugs are surveyed: cannabis/hashish, cocaine (including crack), inhalants, hallucinogens, heroin, and prescription–type drugs used for nonmedical purposes (pain relievers, tranquilizers, stimulants, and sedatives). Also, a number of demographic and geographic characteristics are included in the survey.
Recent onset users were identified as respondents who had a non-missing value for the variable “calendar year of first use” with a range of 2002-2003 for the calendar year 2003. Because of variation in the calendar timing of dates of birth and the dates of the interview, the interval between age of first use and age of interview can be as great as 23 months (just under 24 months) or as small as one week. Whereas we could have chosen a narrower time frame, we chose procedures for identifying recent onset users that are identical as those used elsewhere (Chen et al., 2005), and that would not create sample sizes prohibitively small. First alcohol use is assessed as the first time the respondent had a drink of an alcoholic beverage, excluding times when the individual had a sip or two from a drink; first use of cannabis is the first time the respondent used marijuana or hashish.
Two aspects of the NSDUH are noteworthy. First, underage participants (age 17 or younger) may have received the interview in the presence of a parent. Because this administration feature was not recorded in the national dataset, it is impossible to compare endorsement rates between youth who did and did not have a parent present during their interview. Teenagers' willingness to disclose illegal drug use may be impacted by the presence of a parent during the interview. Thus, it is logical to argue that the rates of drug use and substance use disorders may be lower among underage youth. Another survey administration issue pertains to the approach used in NSDUH in which the assessment of abuse and dependence symptoms only occurs unless the respondent has indicated six or more days of use of the particular drug. The logic of this commonly-used strategy in large scale epidemiological surveys is to reduce the interview duration and respondent burden. Yet this approach may fail to identify drug abusers who have a rapid onset and extremely rapid offset of a substance use disorder; such individuals would not receive the abuse and dependence questions even though symptoms may be present (Chen et al., 2005). Unfortunately there is no study in the literature that provides an estimate of the prevalence of rapid onset and offset users (Chen et al., 2005).
2.4 Statistical analysis
Multiple logistic regression was used to examine the likelihood of developing an AUD and CUD among recent onset users of the respective drug at each chronological age from ages 12 to 21, with the group of respondents aged 22-26 as the reference group (there were so few cases of recent onset users older than 26, we limited the size of reference group to avoid unwanted heterogeneity in the reference group). Given that the data from SAMHSA were collected according to a complex survey design, sampling weights and a variance estimation approach using Taylor series linearization were used to acquire unbiased standard errors, significance tests, p-value, and 95% confidence interval (SAMHSA, 2004; StataCorp, 2005). Because several demographic characteristics other than age have been found to be associated with estimated risk for alcohol or drug use disorder (Chen et al., 2005), analyses were first conducted without controlling for demographic variables, and subsequently including them as covariates. Demographic variables used as covariates were sex (male as reference), race/ethnicity (white as reference), and family income (low-middle, $20,000-$49,999 as reference). The race/ethnicity analysis was limited to the white, African American and Hispanic groups because of sample size considerations. We also added to the covariate list prior drug use involvement variable in the interest of exploring whether the order of drug use onset affected estimated risk status. For the alcohol analyses, we controlled for use of cannabis prior to alcohol (no prior cannabis as the reference); for the cannabis analyses, we controlled for use of alcohol prior to cannabis (no prior alcohol as the reference).
3. Results
3.1 Descriptive findings
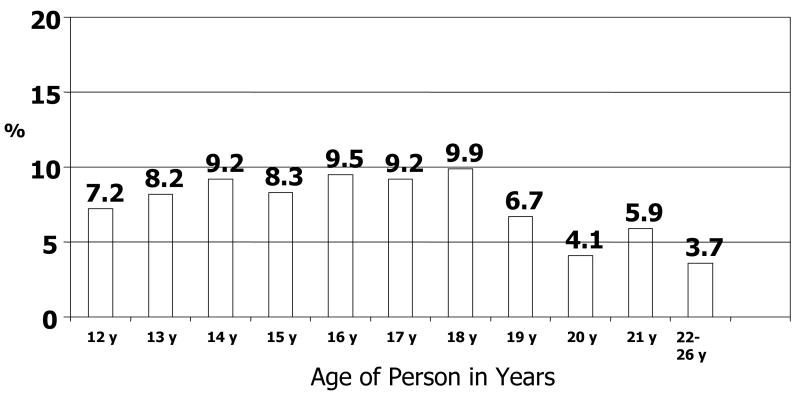
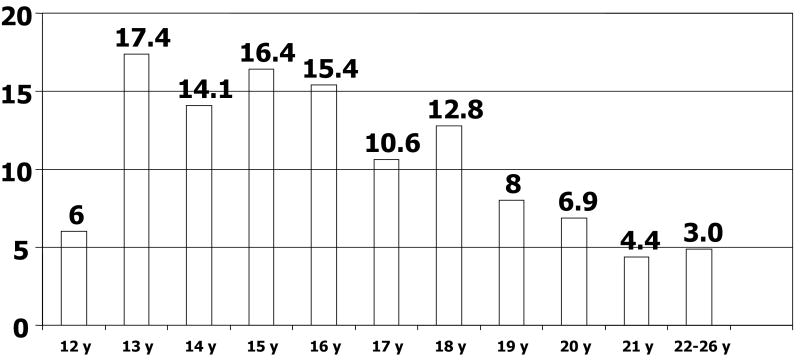
Within the recent-onset users, we computed at each chronological age the percentage of those that met the respective diagnostic criteria for an AUD and CUD. For alcohol, there was a general trend of an increase in the AUD rate during the 12-18-year-old range (from 7.2% to 9.9%), although a slight dip occurred at age 15 (see Figure 1). At age 19, the rate dropped to 6.7% and stayed at a relatively lower rate for the remaining young adult age groups (4.1%, 5.9%, and 3.7%). For cannabis, the pattern of CUD also showed a general trend upward from ages 12 to 18 years (see Figure 2). At age 12 the rate of CUD was 6.1%; the rate increased quite dramatically to 17.4% at age 13, and it stayed relatively high until age 18 (12.8%). Again at age 19, the rate dropped considerably to 8%, and showed a steady decline across the young adult age groups (6.9%, 4.4%, and 3.0%).
Fig. 1.
Percentages of past year alcohol use disorder by age among recent alcohol onset users (prior 2 years; n = 4074)
Fig. 2.
Percentages of past year cannabis use disorder by age among recent cannabis onset users (prior 2 years; n = 2176)
We also computed the rates of abuse vs. dependence within substance use disorder cases. For the total group of individuals in the 12-21 age range, 69% of AUD cases were alcohol abuse and 31 % of AUD cases were alcohol dependence. For CUD in this age group, 60% cases were abuse and 40% cases were dependence. For the aggregate of individuals in the 22-26 group, the breakdowns were as follows: AUD, 77.8% abuse, 22.2% dependence; CUD, 75% abuse, 25% dependence. In general, this relative predominance of abuse vs. dependence as the case at each age group.
Next we contrasted type of recency of onset, that is, very recent onset (0-12 months) vs. distant recent onset (13-24 months), in order to address the possibility that the youngest users only had 0-12 months for a disorder to emerge, whereas the older-onset users might have been more likely to have 13-24 months for a disorder to emerge. For alcohol and marijuana, only one age showed a significant difference (p < .01) in estimated risk as a function of age and type of recency (age 17 and age 16, respectively). In both cases, the significantly lower percentage of a substance use disorder was among the very recent onset cases compared to the distant recent onset cases. Nonetheless, we did not find that younger recent-onset users, who may have had less time for exposure to substances and thus a shorter period for the disorder to emerge, revealed a differential rate of a substance use disorder as a function of type of recency compared to the older recent-onset users.
3.2 Predictors of AUD
Table 3 shows the odds ratios (ORs) for the 4,074 recent onset alcohol users that also reported an AUD, with and without statistical adjustments. We did not observe significant results with respect to sex, race, family income, and if cannabis onset preceded alcohol onset. We did observe an effect for population density; those not residing in a metropolitan region had a significant elevated estimated risk for an AUD compared to the reference group (residing in a metropolitan region < than a pollution of 1 million; OR = 1.4, p < .05). Also, we did observe significant ORs with respect to several age groups. Both non-adjusted and adjusted analyses revealed that individuals at ages 14, 16, 17, and 18 who reported recent alcohol onset were significantly more likely to meet criteria for an AUD compared to those at ages 22-26 with recent alcohol onset (range of ORs = 2.0 - 2.1, all p ≤ .05).
Table 3.
Odd ratios (ORs) for meeting criteria for alcohol abuse or dependence among recent-onset alcohol users (prior 2 years) without and with statistical adjustments (N = 4074)
| OR | 95% CI | OR | 95% CI | |
|---|---|---|---|---|
| Without Statistical Adjustment | With Statistical Adjustment | |||
| Sex | ||||
| Male | 1.0 | — | 1.0 | — |
| Female | 1.1 | 0.9-1.5 | 1.2 | 0.9-1.6 |
| Age | ||||
| 22-26 | 1.0 | — | 1.0 | — |
| 21 | 1.2 | 0.5-2.8 | 1.2 | 0.5-2.8 |
| 20 | 0.9 | 0.3-2.7 | 0.8 | 0.3-2.5 |
| 19 | 1.7 | 0.8-3.9 | 1.8 | 0.8-4.0 |
| 18 | 2.1* | 1.0-4.5 | 2.3* | 1.1-4.8 |
| 17 | 2.0‡ | 1.0-4.2 | 2.1* | 1.0-4.4 |
| 16 | 2.1* | 1.1-4.0 | 2.2* | 1.1-4.2 |
| 15 | 1.7 | 0.9-3.5 | 1.8 | 0.9-3.6 |
| 14 | 2.1‡ | 0.9-4.4 | 2.1‡ | 1.0-4.6 |
| 13 | 1.8 | 0.9-3.6 | 1.8 | 0.9-3.7 |
| 12 | 1.5 | 0.5-4.4 | 1.6 | 0.5-4.5 |
| Race/ethnicity | ||||
| White | 1.0 | — | 1.0 | — |
| African American | 1.0 | 0.7-1.6 | 1.1 | 0.7-1.6 |
| Hispanic | 1.0 | 0.7-1.5 | 1.1 | 0.8-1.5 |
| Family income | ||||
| 0-US$ 19,999 | 1.2 | 0.9-1.7 | 1.3 | 0.9-1.8 |
| US$ 20,000-US$ 49,999 | 1.0 | — | 1.0 | — |
| US$ 50,000-US$ 74,999 | 1.2 | 0.8-1.7 | 1.1 | 0.8-1.6 |
| US$ 75,000 or above | 1.0 | 0.7-1.4 | 0.9 | 0.7-1.3 |
| Population density | ||||
| MSA of 1 million plus | 1.0 | 0.7-1.3 | 1.0 | 0.7-1.4 |
| MSA < 1 million | 1.0 | — | 1.0 | — |
| Residence not in a MSA | 1.4* | 1.1-1.9 | 1.4* | 1.0-1.9 |
| Using cannabis prior to alcohol onset | ||||
| No | 1.0 | — | 1.0 | — |
| Yes | 1.1 | 0.6-1.9 | 1.0 | 0.6-1.8 |
Results based on logistic regression with weighted data and Taylor series linearization for variance estimation to estimate 95% confidence interval (CI) and associated p values.
p = .05.
p < .05.
3.3 Predictors of CUD
Table 4 represents the findings for the ORs of CUD among the 2,176 recent onset cannabis users with and without statistical adjustments. We did not observe significant results with respect to sex, race, family income, population density and if the other drug (in this case, alcohol) preceded the target drug (cannabis). We did observe a more pronounced effect of age on the risk for cannabis compared to alcohol. Significant ORs, regardless of statistical adjustment, were found for each of the teenage years. Respondents at ages 12 – 18 who reported recent cannabis onset were significantly more likely to report a current CUD compared to those at ages 22-26 with recent cannabis onset (range of ORs = 3.9 - 7.2, all p ≤ .05). The largest ORs were for those aged 15 and 16 (OR = 7.2 and 6.8, respectively).
Table 4.
Odd ratios (ORs) for meeting criteria for cannabis abuse or dependence among recent-onset alcohol users (prior 2 years) without and with statistical adjustments (N = 2176)
| OR | 95% CI | OR | 95% CI | |
|---|---|---|---|---|
| Without Statistical Adjustment | With Statistical Adjustment | |||
| Sex | ||||
| Male | 1.0 | — | 1.0 | — |
| Female | 0.9 | 0.6-1.2 | 0.9 | 0.6-1.2 |
| Age | ||||
| 22-26 | 1.0 | — | 1.0 | — |
| 21 | 1.5 | 0.1-27.3 | 1.5 | 0.1-27.0 |
| 20 | 3.1 | 1.0-10.1 | 3.1 | 1.0-10.2 |
| 19 | 2.6 | 0.7-9.4 | 2.7 | 0.7-9.8 |
| 18 | 4.7** | 1.7-13.4 | 4.8** | 1.7-13.5 |
| 17 | 5.2* | 1.4-18.7 | 5.3* | 1.5-19.2 |
| 16 | 6.8** | 2.3-20.0 | 7.0*** | 2.4-20.6 |
| 15 | 7.2*** | 2.6-19.8 | 7.4*** | 2.7-20.4 |
| 14 | 5.6** | 1.7-18.7 | 5.8** | 1.7-19.5 |
| 13 | 5.6** | 1.8-17.7 | 5.7** | 1.8-18.0 |
| 12 | 3.9‡ | 0.6-23.8 | 3.9‡ | 0.6-23.7 |
| Race/ethnicity | ||||
| White | 1.0 | — | 1.0 | — |
| Black | 0.9 | 0.6-1.3 | 0.9 | 0.6-1.4 |
| Hispanic | 1.2 | 0.9-1.7 | 1.2 | 0.9-1.6 |
| Family income | ||||
| 0-US$ 19,999 | 0.8 | 0.6-1.1 | 0.9 | 0.6-1.4 |
| US$ 20,000-US$ 49,999 | 1.0 | — | 1.0 | — |
| US$ 50,000-US$ 74,999 | 1.2 | 0.9-1.7 | 1.2 | 0.8-1.7 |
| US$ 75,000 or above | 1.3 | 0.9-1.8 | 1.3 | 0.9-1.8 |
| Population density | ||||
| MSA of 1 million plus | 1.2 | 0.8-1.8 | 1.2 | 0.8-1.7 |
| MSA < 1 million | 1.0 | — | 1.0 | — |
| Residence not in a MSA | 1.0 | 0.7-1.4 | 1.0 | 0.7-1.4 |
| Using alcohol prior to cannabis onset | ||||
| No | 1.0 | — | 1.0 | — |
| Yes | 1.2 | 0.8-1.7 | 1.3 | 0.9-1.9 |
Results based on logistic regression with weighted data and Taylor series linearization for variance estimation to estimate 95% confidence interval (CI) and associated p values.
p = .05.
p < .05.
p < .01.
p < .001.
4. Discussion
Our data confirm cross-sectional (e.g., Anthony & Petronis, 1995) and prospective (e.g., Grant et al., 2001) research supporting the view that youth is a developmental period of high risk for becoming either abusive of or dependent on substances. Specifically, our study provides three major findings. First, we observed that among the recent onset users, the only demographic variable that was reliably related to AUD and CUD was chronological age. Both the analyses with and without statistical adjustments indicated that alcohol onset and cannabis onset during youth is related to a significant increased estimated risk for being abusive of or dependent on these substances soon after onset. Race, sex, family income and order of drug use onset were not associated with elevated risk. Whereas population density (residing in a non-metropolitan area) was associated with an elevated estimated risk for AUD, it was not linked to an elevated estimated risk for CUD.
The second major finding was that among those who were recent onset users, youth in the teenage years (12 – 18), for the most part, conferred the greatest estimated risk for developing an AUD and CUD. We observed a general steady increase of the rate of a substance use disorder for alcohol and cannabis from age 12 to age 18. Then the rate dropped quite dramatically at age 19, and stayed relatively lower throughout the remaining years of late adolescence and young adulthood. The logistic regression analysis confirmed this pattern. For alcohol, the significant risk years were recent users aged 13, 14, 16, 17 and 18; for cannabis the significant risk years were recent users for all of the teenage years. Youth aged 19, 20 and 21 who were recent users did not reveal a greater estimated risk for an AUD and CUD compared to those aged 22-26. This finding of a conditional risk for SUD as a function of recent onset and youth is consistent with recent analyses indicating that drug problems can emerge among recent onset users (Chen et al., 2005; Hingson et al., 2006). This growing body of research challenges the notion that the risk for developing a SUD requires a lengthy period of drug involvement (Anthony & Petronis, 1995), and provides further confirmation of the association between early use and risk for developing a substance use disorder (Tarter & Mezzich, 1992).
The third core finding was that the conditional risk conferred by the teenage age years was more pronounced for the illegal drug, cannabis, compared to alcohol. We found that among recent users, all of the teenage years were associated with elevated estimated risk for CUD. Yet estimated risk for AUD was not associated with ages 12 and 15 (although the OR for age 15 approached significance, p > .07). Also, the magnitude of the significant ORs was generally 2 – 3 times greater for the estimated risk for CUD compared to the ORs for the estimated risk for AUD. The teenage years associated with a significant risk for AUD (13, 14, 16, 17 and 18 years of age) yielded findings that indicated about twice the risk compared to recent alcohol onset users aged 22-26. Yet the teenage years associated with a significant estimated risk for CUD (12 – 18 years of age) yielded results that indicated in the range of 4 to 7 times the estimated risk compared to recent cannabis onset users aged 22-26. The heightened risk for cannabis may reflect the markedly increased THC concentrations in smoked cannabis since the 1980s (Compton et al., 2004), or reflect a differential prominence of risk factors that aggregated more among cannabis users than alcohol users.
Our findings support the view that age of onset is one of the most significant predictors of developing an SUD (Flory et al., 2004; McGue et al., 2001). Moreover, the study's results further reinforce the importance of targeting early onset drug use in intervention and prevention programs. Delaying of the age of onset is associated with a reduced likelihood of a young person developing later a substance use disorder (August et al., 2004), and early intervention of drug abusing youth has the potential to reduce their likelihood of developing a dependence disorder.
The study's general finding of a conditional risk of SUD linked to youth may have been influenced by several factors and variables that we did not measure. Youth that waited until late adolescence to begin drug use may have possessed more protective factors during the teenage years compared to youth that started their drug use earlier. The late-starters may have been more involved in healthier recreational activities, had more non-drug using friends, and had parents that were more intolerant of drug use – all factors that have been linked to reduced drug use during adolescence (Clark & Winters, 2002; Hawkins et al., 1992). Another explanatory factor that we did not examine (due to statistical power limitations) is the accumulation of prior drug experiences as a risk for developing a SUD. This factor has emerged from prospective studies of adolescents and young adults (Coffey et al., 2003) and from cross-sectional epidemiological studies (e.g., Chen et al., 2005; Grucza & Bierut, 2006).
Not only is youth a time of exposure to several psychosocial risk factors, recent science indicates that the human brain is still developing into the middle twenties (Spear, 2002; Giedd et al., 1999), and there indications that the developing brain is vulnerable to the effects of drugs, particularly alcohol (Spear, 2002; Nagel et al., 2005). Exposure to drugs at a young age, as the brain is going though significant neurological development may cause a heightened susceptibility to abuse and dependence disorders. On the other hand, the older youth who waits and uses drugs for the first time when the brain is more mature may be more resilient to neurobiological processes that contribute to abuse and dependence.
It is noteworthy that our conditional risk analyses did not find an effect of family income on conditional risk. In the Chen study (Chen et al., 2005), lower income families had about a double likelihood of developing a cannabis dependence disorder among recent onset cannabis users compared to those with a higher family income. It is important to note that our data analytic strategy differed somewhat from the Chen report (e.g., the younger ages were collapsed into small subgroups; conditional risk focused on dependence rather than abuse and dependence). A post-hoc analysis of the present data set in which we replicate the Chen analytic strategy produced the same general finding that recent onset cannabis users with a lower family income were about twice as likely to develop cannabis dependence disorder compared to those with higher income families.
4.1 Limitations
Several research design issues need to be considered in interpreting the study results. First, the survey data incorporates the recall of drug use from individuals across a wide span of age. It is not clear that developmentally, individuals provide comparable recall abilities. This is particularly relevant for this study given that the very young respondents (e.g., 12 and 13-year-olds) were expected to provide accurate recall data. Also, social desirability tendencies and the extent to which an adult was present during the interview, which may contribute to under-reporting of drug involvement and substance use disorder symptoms, may vary with age. Thus, the effect of social desirability and context effects on the data may not be equivalent across the various age groups in the survey. Also, measurement bias may have resulted from concerns by respondents to self-disclose use of illegal substances, and individuals with a current substance use disorder to be more likely to remember when they started to use the respective substance because of consequences experienced later in life. This tendency would contribute to an artificially elevated relationship between age of substance use onset and a current SUD (Hingson et al., 2006).
There are several other measurement issues to consider. Our findings may have been affected by differential accuracy in retrospectively reporting onset of first use, given that older individuals tend to report later age of first use (Parra et al., 2003). The meaning of many abuse and dependence criteria may differ between adults and adolescents. For example, increased tolerance during adolescence may be a normal developmental phenomenon (Martin & Winters, 1998), and social influences may be more related to several dependence criteria among adolescents compared to adults (e.g., the criteria of “using more than intended”) (Chung & Martin, 2002). A consideration for future research is to examine the prevalence of symptom frequencies across recent onset users as a function of age to see if there developmental trends in symptom onset. The NSDUH may underestimate the incidence of SUD given that abuse and dependence questions were only asked of individuals who reported using six or more occasions of the respective drug within twelve months prior to assessment, which would miss those with a rapid-onset and rapid-offset pattern of use that also develop a SUD. Also, the recent onset variable spans a considerable interval, that is, from zero months to just under twenty-four months after the first use of the respective drug. Such a variable interval period creates a considerable variability of exposure to risk experiences across individuals. Naturally, an analysis based on a recent onset variable with a smaller interval period would have been more desirable. Moreover, our estimates of the prevalence of substance-related problems may be low because we did not consider as positive cases those subthreshold dependence cases that also did not meet abuse criteria (or termed “diagnostic orphans”).
A final limitation is that the NSDUH is a cross-sectional study, and thus longitudinal studies are required to verify these findings. However, the study results are generally consistent with several longitudinal studies indicating a link between early onset of drug use and development of a SUD (August et al., 2006; Ferguson & Horwood, 2000; Lynskey et al., 2003).
Acknowledgments
This research was supported by NIDA award K02DA15347 (Winters). NIDA had no role in the study design, data analysis, interpretation of the data, or in the decision to submit the paper for publication.
Data reported herein acquired from national survey data collected under the direction of the Office of Applied Studies, Substance Abuse and Mental Health Services Administration.
This research was supported by NIDA award K02DA15347 (Winters). Data reported herein acquired from national survey data collected under the direction of the Office of Applied Studies, Substance Abuse and Mental Health Services Administration.
Footnotes
Author Winters designed the study. Winters took the lead on preparing the Introduction and Discussion; Lee took the lead in analyzing the data, and preparing the Methods and Results. Both authors approved the final manuscript.
Conflict of Interest: There are no conflicts of interest to report for both authors.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- APA. Diagnostic and Statistical Manual of the Mental D-IV. The American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Anthony JC, Petronis KR. Early-onset drug use and risk of later drug problems. Drug Alcohol Depend. 1995;40:9–15. doi: 10.1016/0376-8716(95)01194-3. [DOI] [PubMed] [Google Scholar]
- August GJ, Winters KC, Realmuto G, Fahnhorst T, Botzet A, Lee S. Prospective study of adolescent drug abuse among community samples of ADHD and non-ADHD participants. J Am Acad Child Adol Psychiatry. 2006;45:824–832. doi: 10.1097/01.chi.0000219831.16226.f8. [DOI] [PubMed] [Google Scholar]
- August GJ, Winters KC, Tarter R, Perry C, Hektner JM. Moving evidence-based drug abuse prevention programs from basic science to practice: ‘Bridging the efficacy-effectiveness interface’. Subst Use Misuse. 2004;39:2037–2053. doi: 10.1081/ja-200033240. [DOI] [PubMed] [Google Scholar]
- Brook JS, Adams RE, Balka EB, Johnson E. Early adolescent marijuana use: risks for the transition to young adulthood. Psychol Med. 2002;32:79–91. doi: 10.1017/s0033291701004809. [DOI] [PubMed] [Google Scholar]
- Chen C, O'Brien MS, Anthony JC. Who becomes cannabis dependent soon after onset of use? Epidemiological evidence from the United States: 2000-2001. Drug Alcohol Depend. 2005;79:11–22. doi: 10.1016/j.drugalcdep.2004.11.014. [DOI] [PubMed] [Google Scholar]
- Chung T, Martin CS. Concurrent and discriminant validity of DSM-IV symptoms of impaired control over alcohol consumption in adolescents. Alcohol: Clin Exp Res. 2002;26:485–492. [PubMed] [Google Scholar]
- Clark D, Winters KC. Measuring risks and outcomes in substance use disorders prevention research. J Consul Clin Psychol. 2002;70:1207–1223. doi: 10.1037//0022-006x.70.6.1207. [DOI] [PubMed] [Google Scholar]
- Coffey C, Carlin JC, Lynskey M, Li N, Patton GC. Adolescent precursors of cannabis dependence: Findings from the Victorian Adolescent Health Cohort Study. Brit J Psychiatry. 2003;182:330–336. doi: 10.1192/bjp.182.4.330. [DOI] [PubMed] [Google Scholar]
- Compton WM, Grant BF, Colliver JD, Glantz MD, Stinson FS. Prevalence of marijuana use disorders in the United States: 1991-1992 and 2001-2002. J Am Med Assoc. 2004;291:2114–2121. doi: 10.1001/jama.291.17.2114. [DOI] [PubMed] [Google Scholar]
- DeWit DJ, Adlaf EW, Offord DR, Ogborne AC. Age of first alcohol use : A risk factor for the development of alcohol disorders. Am J Psychiatry. 2000;157:745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ. Cannabis use and dependence in a New Zealand birth cohort. New Zealand Med J. 2000;113:156–158. [PubMed] [Google Scholar]
- Flory K, Lynam D, Milich R, Leukefeld C, Clayton R. Early adolescent through adult alcohol and marijuana use trajectories: early predictors, young adult outcomes, and predictive utility. Develop Psychopathology. 2004;16:193–213. doi: 10.1017/s0954579404044475. [DOI] [PubMed] [Google Scholar]
- Giedd JN, Blumenthal J, Jeffries NO, Castellanos FX, Liu H, Zijdenbos A, Paus T, Evans AC, Rapoport JL. Brain development during childhood and adolescence: A longitudinal MRI study. Nature Neuro. 1999;2:861–863. doi: 10.1038/13158. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset of alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiological Survey. J Subst Abuse. 1998;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Grant BF, Stinson FS, Harford TC. Age of onset of alcohol use and DSM-IV alcohol abuse and dependence. J Subst Abuse. 2001;13:493–504. doi: 10.1016/s0899-3289(01)00096-7. [DOI] [PubMed] [Google Scholar]
- Grucza RA, Bierut LJ. Cigarette smoking and risk for alcohol use disorders among adolescent drinkers. Alcohol: Clin Exp Res. 2006;30:2046–2054. doi: 10.1111/j.1530-0277.2006.00255.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins J, Catalano R, Miller J. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychol Bulletin. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence. Arch Ped Med. 2006;60:739–746. doi: 10.1001/archpedi.160.7.739. [DOI] [PubMed] [Google Scholar]
- Kaminer Y. Adolescent Substance Abuse. New York: Plenum Publishing Corporation; 1994. [Google Scholar]
- Krueger RF, Hickks BM, Patrick CJ, Carlson SR, Iacono WG, McGue M. Biologic connections among substance dependence, antisocial behavior, and personality: Modeling the externalizing spectrum. J Abnorm Psychol. 2002;111:411–424. [PubMed] [Google Scholar]
- Lynskey MT, Heath AC, Bucholz KK, Slutske WS, Madden PA, Nelson EC, Statham DJ, Martin NG. Escalation of drug use in early-onset cannabis users vs co-twin control. JAMA. 2003;289:427–433. doi: 10.1001/jama.289.4.427. [DOI] [PubMed] [Google Scholar]
- Martin CS, Winters KC. Diagnosis and assessment of alcohol use disorders among adolescents. Alcohol Health Res World. 1998;22:95–105. [PMC free article] [PubMed] [Google Scholar]
- McGue M, Iacono W, Legrand N, Elkins I. Origins and consequences of age at first drink, II: Familial risk and heritability. Alcohol Clin Exp Res. 2001;25:1166–1173. [PubMed] [Google Scholar]
- Nagel BJ, Schweinsburg AD, Phan V, Tapert SF. Reduced hippocampal volume among adolescents with alcohol use disorders without psychiatric comorbidity. Psychiatry Res Neuroimaging. 2005;139:181–190. doi: 10.1016/j.pscychresns.2005.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson CB, Wittchen HU. DSM-IV alcohol disorders in a general population sample of adolescents and young adults. Addict. 1998;93:1065–1077. doi: 10.1046/j.1360-0443.1998.937106511.x. [DOI] [PubMed] [Google Scholar]
- Parra G, O'Neill SE, Sher K. Reliability of self-reported age of substance involvement onset. Psychology Addictive Behav. 2003;17:211–218. doi: 10.1037/0893-164X.17.3.211. [DOI] [PubMed] [Google Scholar]
- Robins LN, Przybeck TR. Age of onset of drug use as a factor in drug and other disorders. In: Jones CL, Battjes RL, editors. Etiology of Drug Abuse: Implications for Prevention. NIDA Research Monograph 56. Rockville, MD: National Institute of Drug Abuse; 1985. pp. 178–192. [PubMed] [Google Scholar]
- Spear LP. The adolescent brain and age-related behavioral manifestations. Neuroscience Biobehavioral Rev. 2002;24:417–463. doi: 10.1016/s0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 9. College Station, TX: StataCorp; 2005. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Summary of Findings from the 2000 National Household Survey on Drug Abuse. NHSDA Series H-13, DHHS Publication No (SMA) 01-3549. Rockville, MD: Office of Applied Studies; 2001. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) Results from the 2001 National Household Survey on Drug Abuse: Summary of National Findings. NHSDA Series H-17, DHHS Publication No (SMA) 02-3758. Vol. 1. Rockville, MD: Office of Applied Studies; 2002. [Google Scholar]
- Substance Abuse Mental Health Service Administration (SAMHSA) Overview of Findings from the 2003 National Survey on Drug Use and Health. NSDUH Series H-24, DHHS Publication No SMA-04-3963. Rockville, MD: Office of Applied Studies; 2004. [Google Scholar]
- Substance Abuse Mental Health Service Administration (SAMHSA) Results from the 2004 National Survey on Drug Use and Health: National Findings. NSDUH Series H-28, DHHS Publication No SMA-05-4062. Rockville, MD: Office of Applied Studies; 2005. [Google Scholar]
- Tarter RE, Mezzich AC. Ontogeny of substance abuse: Perspectives and findings. In: Glantz M, Pickens R, editors. Vulnerability to Drug Abuse. Washington, D.C.: American Psychological Association; 1992. pp. 149–178. [Google Scholar]
- Winters KC, Fawkes T, Fahnhorst T, Botzet A, August GJ. A synthesis review of exemplary drug abuse prevention programs in the United States. J Subst Abuse Treat. doi: 10.1016/j.jsat.2006.10.002. in press. [DOI] [PubMed] [Google Scholar]