Abstract
Twenty patients with thoracolumbar burst fractures (type A3 in the classification of Magerl et al.) were studied prospectively for the evaluation of clinical, radiographic and functional results. The patients were submitted to surgical treatment by posterior arthrodesis, posterior fixation and autologous transpedicular graft. The patients were followed up for 2 years after surgery and assessed on the basis of clinical (pain, neurologic deficit, postoperative infection), radiographic (load sharing classification, Farcy´s sagittal index of the fractured segment, relation between traumatic vertebral body height and the adjacent vertebrae (compression percentage), height of the intervertebral disk proximal and distal to the fractured vertebra, rupture or loosening of the implants) and functional (return to work, SF-36) criteria. Two patients presented a marked loss of correction and required the placement of an anterior support graft. Pain assessment revealed that eight patients (44%) had no pain; four (22%) had occasional pain, three (17%) moderate pain, and three (17%) severe pain. According to the classification of Frankel et al., 17 patients persisted as Frankel E and one patient presented improvement of one degree, becoming Frankel D. The mean value of Farcy´s sagittal index of the injured vertebral segment was 20.67° ± 6.15° (range 8°–32°) during the preoperative period, 11.22° ± 8.09° (range −5° to 21°) during the immediate postoperative period, and 14.22° ± 7.37° (range 3°–25°) at late evaluation. There was a statistically significant difference between the immediate postoperative values and the preoperative and late postoperative values. The compression percentage of the fractured vertebral body ranged from 9.1 to 60 (mean 28.81 ± 11.51) during the preoperative period, from 0 to 60 (mean: 15.59 ± 14.49) during the immediate postoperative period, and from 8 to 60 (mean: 25.9 ± 13.02) at late evaluation. There was a statistically significant difference between the preoperative and postoperative values and between the postoperative and late postoperative values. The height of the proximal intervertebral disk ranged from 6 to 14 mm (mean 8.44 ± 2.66) during the preoperative period, from 6 to 15 mm (mean 10 ± 2.30) during the immediate postoperative period, and from 0 to 11 mm (mean 7.22 ± 2.55) during the late postoperative period. A significant difference was observed between the immediate postoperative values and the preoperative and late postoperative values. The height of the intervertebral disk distal to the fractured vertebra ranged from 7 to 16 mm (mean 9.94 ± 2.64) during the preoperative period, from 5 to 18 mm (mean 11.61 ± 3.29) during the immediate postoperative period, and from 2 to 14 mm (mean 9.72 ± 3.17) during the late postoperative period. There was a significant difference between the immediate postoperative values and the preoperative and late postoperative values. Except for the height of the intervertebral disk proximal to the fractured vertebra, no correlation was detected between the clinical, functional and radiologic results. The results observed in the present study indicate that other, still incompletely defined parameters influence the functional result of thoracolumbar burst fractures.
Keywords: Traumatic thoracolumbar fractures, Burst fractures, Surgical treatment, Functional outcomes
Introduction
Burst fractures represent about 10–20% of all spinal fractures [11] and their treatment continues to be a matter of controversy. Although a large number of papers have been published describing techniques for the reduction and stabilization of these fractures, as well as conservative treatment, no consensus exists about the ideal treatment [25].
The loss of immediate postoperative correction has been one of the parameters studied for the evaluation and comparison of the results. However, the correlation between the loss of reduction and the clinical/functional result has not been presented in all reports. The loss of reduction and the occurrence of faults in the fixation system have been correlated with the degree of comminution of the fractured vertebral body [9,11, 13, 16, 19]. McKomark et al. [16] introduced the concept of load sharing and proposed a classification for burst fractures based on the degree of comminution of the fractured vertebra in order to orient the reconstruction of the anterior spine.
The objective of the present study was to evaluate prospectively a group of patients with thoracolumbar burst fractures submitted to surgical treatment through a posterior approach considering the morphological parameters of the fractured vertebral body, the adjacent disks, the sagittal alignment, as well as clinical and functional parameters.
Materials and methods
A sequential group of 20 patients with thoracolumbar burst fractures were operated and studied prospectively with a 2-year follow-up. Patient age ranged from 19 to 60 years (mean 36.6 ± 10.6 years). Sixteen patients (80%) were males and four (20%) were females. Trauma was caused by a fall from a height in nine patients, by a traffic accident in nine, and by direct trauma in two. The fracture was located at the T10 level in one patient, at T12 in 4, at L1 in five, L2 in six, L3 in three, and L5 in one. According to the classification of Magerl et al. [15], all patients had a typeA3 burst fracture. Five patients (25%) had a type A3.1 fracture, ten patients (50%) a type A3.2 fracture, and five patients a type A3.3 fracture (25%). Neurologic deficit was assessed using the scale of Frankel et al. [6] with 17 patients being classified as Frankel E and one patient as Frankel C. Associated lesions were present in seven patients: two ankle fractures, two heel fractures, one diaphyseal fracture of the femur, one diaphyseal fracture of the humerus, and one distal fracture of the radius.
Twenty patients with type A3 fracture of the spine with an indication for surgical treatment were selected prospectively for the study.
All patients were submitted to arthrodesis and posterior fixation with an internal fixator (Synthes). The area of fixation and arthrodesis comprised the distal and proximal vertebrae to the fractured area. An autologous graft was used for posterolateral arthrodesis, associated with unilateral placement of an autologous transpedicular cancellous graft in the fractured vertebra. During the postoperative period, walking and rehabilitation were started based on the pain symptoms and associated lesions of the patients. The patients wore a corset for 12 weeks during the postoperative period.
A 2-year postoperative follow-up was established for the final evaluation of the patients. The patients were evaluated according to clinical, radiologic and functional parameters, with a preoperative and immediate postoperative evaluation and a final evaluation after 2 years of follow-up.
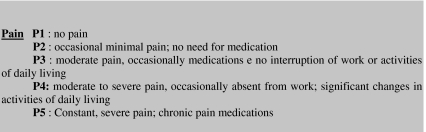
The clinical parameters evaluated were the neurological picture and pain according to the Denis scale [4] (Fig. 1). The parameters used for radiographic evaluation were the sagittal index of the fractured segment (Fracy’s sagittal index [5]); the relation between the traumatic vertebra body height and the adjacent vertebrae (compression percentage = 100 − (2 × F/A + B) × 100. F-height of fractured vertebra, A-height of the proximal vertebra, B-height of the distal vertebra) [21]; the height of the intervertebral disk above and below the fractured vertebra; classification of the fracture based on load sharing according to McCormack et al. [16]; loosening and rupture of the implants used for fixation.
Fig. 1.
Dennis pain scale
Vertebral body height was measured as the coefficient of the body height of the fractured vertebra divided by the sum of the heights of the vertebral body proximal and distal to the fractured vertebra.
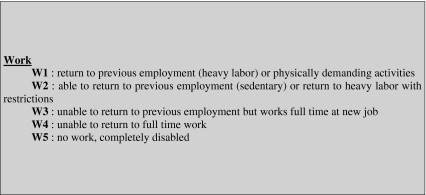
Functional evaluation was performed using the functional work scale of Denis [4] (Fig. 2) and the functional evaluation scale SF-36 [8].
Fig. 2.
Dennis work scale
The parameters of radiographic evaluation were analyzed by the paired t-test and the Wilcoxon test. The correlation between the clinical, functional and radiologic results was calculated by Spearman correlation and the level of significance was set at 95% in all analyses.
Results
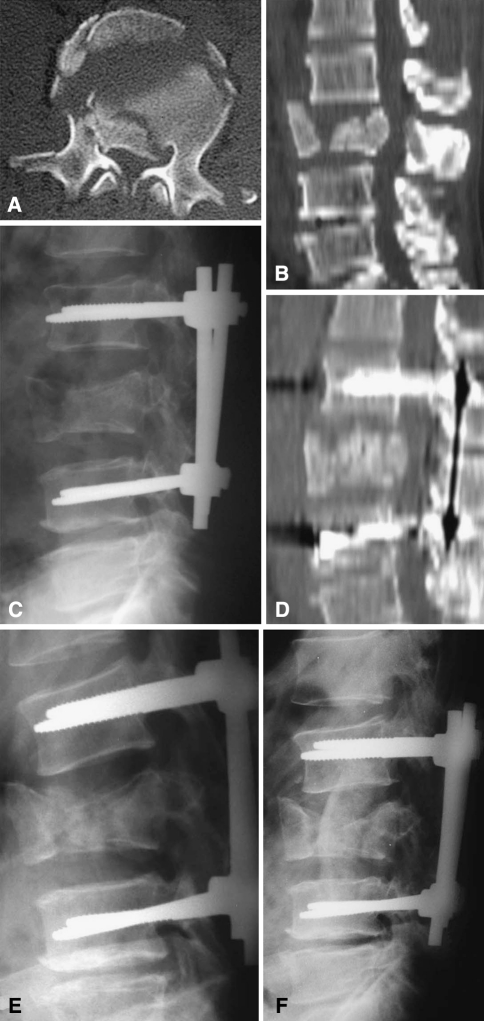
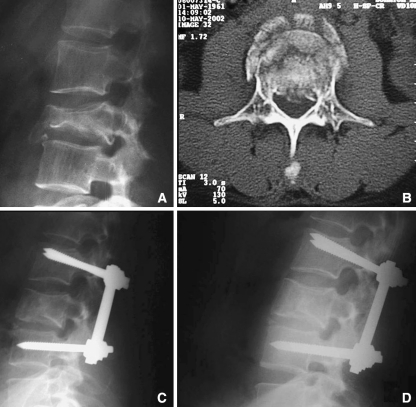
The patients were followed for a period of 2 years after surgery. Two patients were excluded from the final evaluation due to a marked loss of correction and to the need for an anterior approach for the reconstruction of the fractured vertebral body. These two patients presented an intense degree of comminution of the fractured vertebral body and reached nine points in the load-sharing classification [16] (Fig. 3). The general results for the 18 patients are listed in Table 1.
Fig. 3.
Fracture with intense degree of comminution and loss of reduction. a, b Preoperative CT. c, d Postoperative Rx and CT after posterior arthrodesis and fixation. E Loss of correction after 3 months. f Postoperative Rx after anterior support with iliac bone graft
Table 1.
Patients’ characteristics and details regarding the evaluation methods
| n | Level | Age | Type | Etiology | Frankel | Sagittal Index | Proximal disc height | Distal disc height | Compression percentage | Score Load Sharing | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| preop | postop | 2 years | Preop | Postop. | 2 years | Preop | Postop. | 2 years | preop | postop | 2 years | Classification | ||||||
| 1 | L3 | 41 | A3.2 | Fall from height | E | 20 | 15 | 15 | 12 | 15 | 8 | 7 | 11 | 7 | 33.4 | 16.66 | 33.33 | 9 |
| 2 | L1 | 25 | A3.2 | Fall from height | E | 20 | 10 | 20 | 6 | 10 | 7 | 12 | 15 | 10 | 23.1 | 0 | 23.07 | 6 |
| 3 | T12 | 36 | A3.2 | Traffic accident | E | 15 | -5 | 5 | 9 | 8 | 7 | 6 | 9 | 10 | 33.4 | 16.66 | 9.09 | 7 |
| 4 | L1 | 29 | A3.2 | Fall from height | E | 8 | 12 | 3 | 6 | 9 | 6 | 7 | 10 | 9 | 9.1 | 8 | 8 | 5 |
| 5 | L1 | 28 | A3.1 | Fall from height | E | 20 | 11 | 11 | 8 | 12 | 10 | 13 | 13 | 13 | 23.07 | 7.69 | 9.09 | 5 |
| 6 | L1 | 19 | A3.1 | Traffic accident | E | 32 | 20 | 20 | 6 | 10 | 11 | 16 | 15 | 13 | 33.4 | 28.57 | 23.07 | 6 |
| 7 | L2 | 46 | A3.2 | Traffic accident | E | 20 | 10 | 25 | 10 | 15 | 10 | 12 | 18 | 14 | 42.85 | 23.07 | 23.07 | 4 |
| 8 | L2 | 32 | A3.2 | Fall from height | E | 26 | 10 | 15 | 6 | 10 | 6 | 12 | 15 | 10 | 33.4 | 18.75 | 33.33 | 8 |
| 9 | T10 | 27 | A3.2 | Fall from height | E | 15 | -5 | 5 | 8 | 10 | 6 | 8 | 5 | 2 | 20 | 0 | 20 | 5 |
| 10 | T12 | 29 | A3.2 | Fall from height | E | 13 | 5 | 15 | 11 | 11 | 7 | 10 | 10 | 10 | 23.1 | 28.57 | 28 | 7 |
| 11 | L3 | 39 | A3.2 | Traffic accident | E | 18 | 18 | 22 | 5 | 7 | 7 | 8 | 8 | 8 | 20 | 14.28 | 33.33 | 5 |
| 12 | T12 | 47 | A3.3 | Fall from height | E | 25 | 5 | 5 | 12 | 10 | 10 | 10 | 11 | 11 | 60 | 60 | 60 | 7 |
| 13 | L5 | 34 | A3.3 | Fall from height | E | 15 | 20 | 15 | 10 | 10 | 8 | 9 | 10 | 7 | 12.5 | 0 | 42.85 | 9 |
| 14 | L2 | 55 | A3.2 | Traffic accident | E | 30 | 10 | 10 | 14 | 10 | 10 | 9 | 10 | 10 | 33.4 | 16.66 | 33.33 | 8 |
| 15 | L2 | 60 | A3.1 | Fall from height | E | 25 | 20 | 20 | 7 | 9 | 6 | 7 | 9 | 5 | 33.4 | 16.66 | 33.33 | 5 |
| 16 | L1 | 25 | A3.3 | Traffic accident | C | 20 | 20 | 20 | 6 | 6 | 5 | 10 | 10 | 11 | 23.7 | 23.07 | 16.66 | 7 |
| 17 | T12 | 39 | A3.1 | Fall from height | E | 25 | 5 | 5 | 6 | 8 | 0 | 10 | 15 | 10 | 33.4 | 0 | 16.66 | 7 |
| 18 | L1 | 49 | A3.1 | Traffic accident | E | 25 | 21 | 25 | 10 | 10 | 6 | 13 | 15 | 15 | 27.27 | 9.09 | 20 | 4 |
Evaluation of the neurological picture according to the classification of Frankel et al. [6] showed that the patient classified as Frankel C in the initial evaluation progressed to Frankel D and the remaining patients continued to be Frankel E.
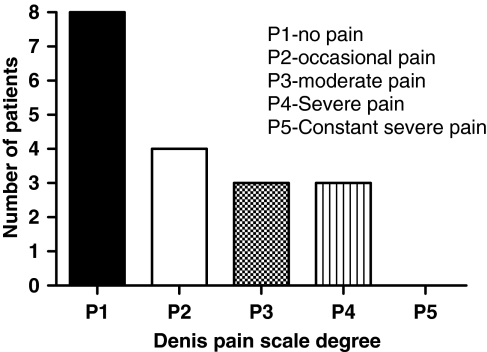
Evaluation of pain according to the Denis scale [4] showed that eight patients (44%) had no pain 2 years after surgery, four (22%) had minimal pain not requiring anti-inflammatory drugs, three (17%) had moderate pain requiring the occasional use of analgesics, and three (17%) had moderate to severe pain, with occasional loss of work days and significant changes in daily activities (Fig. 4).
Fig. 4.
Late evaluation of pain according to the Dennis scale
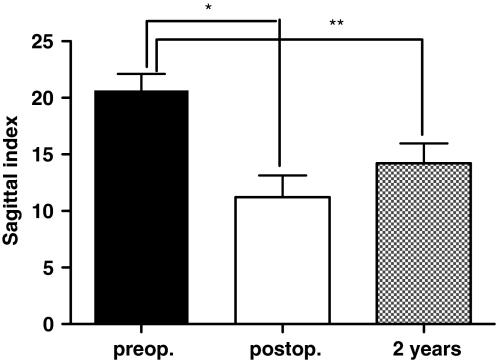
The sagittal index of the fractured vertebral segment ranged from 8° to 32° during the preoperative period (mean 20.67° ± 6.15°), from −5° to 21° during the immediate postoperative period (mean 11.22° ± 8.09) and from 3° to 25° (mean: 14.22° ± 7.37) at the final evaluation 2 years after surgery (Fig. 5). The values observed during the immediate postoperative period differed significantly from preoperative values (P = 0.0002—t test) and from late postoperative values (P = 0,0036—t test). There was no statistically significant difference between the postoperative and late postoperative values (P = 0.0512).
Fig. 5.
Evaluation of the sagittal index of the fractured vertebral segment during the preoperative period, immediate postoperative period, and late postoperative period. The asterisk (*) indicates a statistically significant difference (* P < 0.0002) and (** P < 0.0001)
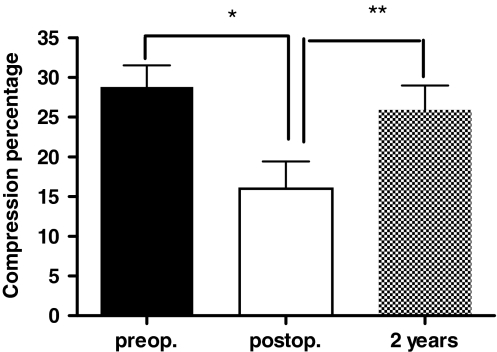
Compression percentage of the fractured vertebral body height was from 9.1 to 60 (mean 28.81 ± 11.51) during the preoperative period, the immediate postoperative values ranged from 0 to 0.60 (mean 15.59 ± 14.49) and the values measured 2 years after surgery ranged from 8 to 60 (mean 25.9 ± 13.02). There was a significant difference between preoperative and immediate postoperative values (P = 0.0006—Wilcoxon). There was no difference between preoperative and late postoperative values (P = 0.08—Wilcoxon). Immediate postoperative values differed significantly from late follow-up values (P = 0.0054—Wilcoxon). These results indicate that the correction of vertebral body height by the method used was significant but a significant loss of vertebral body height occurred during follow-up (Fig. 6).
Fig. 6.
Evaluation of the compression percentage of the vertebral body during the preoperative period, immediate postoperative period, and late postoperative period. The asterisk (*) indicates a statistically significant difference (* P < 0). * P = 0, ** P = 0.002 and *** P = 0.012
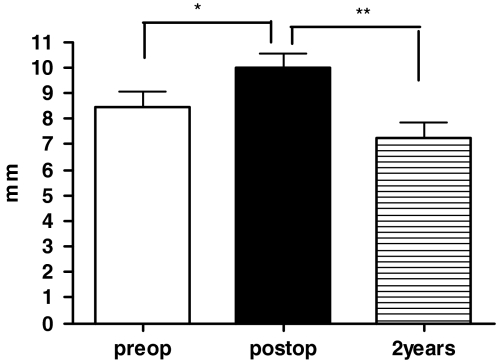
The height of the intervertebral disk proximal to the fractured vertebra ranged from 6 to 14 mm (mean 8.44 ± 2.66) during the preoperative period, from 6 to 15 mm (mean 10 ± 2.30) during the immediate postoperative period, and from 0 to 11 mm (mean 7.22 ± 2.55) 2 years after surgery. The immediate postoperative values differed significantly from the preoperative values (P = 0.021—Wilcoxon) and from the late postoperative values (P = 0.001—Wilcoxon). However, there was no significant difference between the preoperative and late postoperative values. These results indicate that there was a significant restoration of disk height, which, however, was not maintained, with the occurrence of loss of correction and with the values observed at final evaluation being equal to preoperative values (Fig. 7).
Fig. 7.
Height of the intervertebral disk proximal to the fractured vertebra during the preoperative period, immediate postoperative period, and late postoperative period. The asterisk (*) indicates a statistically significant difference (* P = 0.021) e (** P = 0.001)
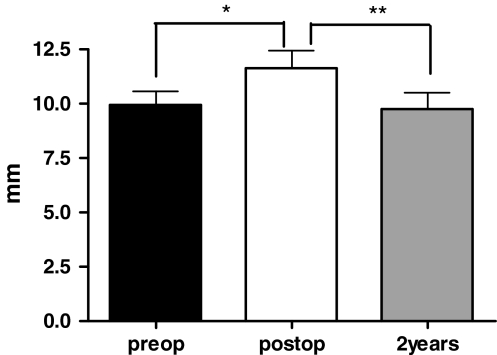
The height of the intervertebral disk distal to the fractured vertebra ranged from 7 to 16 mm (mean 9.94 ± 2.64) during the preoperative period, from 5 to 18 mm (mean 11.61 ± 3.29) during the immediate postoperative period, and from 2 to 14 mm (mean 9.72 ± 3.17) 2 years after surgery. The immediate postoperative values differed significantly from the preoperative ones (P = 0.009—Wilcoxon) and from the late postoperative ones (P = 0.006—Wilcoxon). However, no significant difference was observed between the preoperative values and those observed 2 years after surgery, demonstrating the same behavior as observed for the disk proximal to the fractured vertebra (Fig. 8).
Fig. 8.
Height of the intervertebral disk distal to the fractured vertebra during the preoperative period, immediate postoperative period, and late postoperative period. The asterisk (*) indicates a statistically significant difference (* P = 0.0009) and (** P = 0.006)
The values of the radiographic parameters (sagittal index, compression percentage of fractured vertebral body and intervertebral disk height) and the scores of the load-sharing classification are presented in Table 1. Comparison of the parameters with the scores of the load sharing classification did not reveal a significant correlation according to the Spearman test.
Evaluation of the ability to work by the Denis scale showed that nine patients (50%) returned to the job they held before the accident, four (22%) did not return to their previous job but are currently working full time on another job, two (11%) are working with limitations on a part time basis, and three (17%) are not working. Evaluation by the SF-36 functional scale is listed in Table 2.
Table 2.
Patients’ characteristics and SF-36 outcome
| Patient | Age | Gender | Physical function | Role limitations due to physical health | Role limitations due to emotional problems | Vitality index | Menthal health index | Social functioning index | Pain | General health perceptions index |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 41 | F | 60 | 0 | 0 | 60 | 24 | 25 | 22.5 | 12.5 |
| 2 | 25 | M | 95 | 100 | 100 | 100 | 96 | 100 | 77.5 | 90 |
| 3 | 36 | M | 100 | 100 | 100 | 35 | 68 | 62.5 | 55 | 85 |
| 4 | 29 | F | 65 | 0 | 0 | 35 | 44 | 25 | 22.5 | 35 |
| 5 | 28 | M | 100 | 100 | 100 | 90 | 96 | 100 | 100 | 90 |
| 6 | 19 | M | 80 | 100 | 100 | 95 | 88 | 80 | 90 | 96 |
| 7 | 46 | F | 95 | 100 | 100 | 80 | 84 | 100 | 100 | 80 |
| 8 | 32 | M | 95 | 100 | 100 | 90 | 84 | 75 | 77.5 | 90 |
| 9 | 26 | M | 35 | 0 | 0 | 50 | 76 | 50 | 22.5 | 0 |
| 10 | 29 | M | 95 | 100 | 100 | 100 | 100 | 100 | 100 | 90 |
| 11 | 39 | M | 95 | 75 | 66.5 | 70 | 84 | 100 | 90 | 100 |
| 12 | 47 | M | 95 | 100 | 100 | 90 | 92 | 100 | 100 | 100 |
| 13 | 34 | M | 100 | 100 | 100 | 85 | 88 | 100 | 90 | 95 |
| 14 | 55 | F | 95 | 100 | 100 | 100 | 100 | 100 | 100 | 90 |
| 15 | 60 | M | 65 | 100 | 100 | 75 | 80 | 87.5 | 77.5 | 70 |
| 16 | 25 | M | 40 | 25 | 66.7 | 75 | 32 | 50 | 75 | 75 |
| 17 | 45 | M | 40 | 0 | 0 | 35 | 44 | 22.5 | 35 | 5 |
| 18 | 44 | M | 20 | 0 | 0 | 40 | 64 | 25 | 35 | 30 |
Except for the height of the proximal intervertebral disk, no correlation was observed between the radiologic, clinical and functional results for the patients studied.
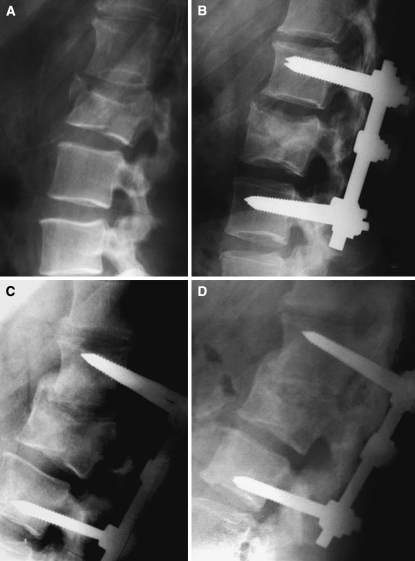
All the unsatisfactory results of the clinical and functional parameters evaluated were associated with a significant loss of proximal disk height. Sf 36 questionnaire (physical function—P = 0.01, role limitation due to physical health—P = 0.01, role limitations due to emotional problems—P = 0.013, vitality index—P = 0.013, mental health index—P = 0.006,social function index—P = 0.003, pain—P = 0.002, general health perception index—P = 0.006, Spearman test) (Figs. 9, 10). The complications observed in the 20 patients studied were: a significant loss of sagittal alignment in two requiring anterior reconstruction of the fractured vertebral segment, rupture of one of the inferior pins of the fixation system in two, superficial infection in one patient, and implant loosening in another. All four patients who presented complications related to infection or to implant rupture required implant removal.
Fig. 9.
Mounting of the case that had a good result. Preoperative radiograph (a) and computed tomography (b). Profile radiography during the immediate postoperative period (c) and at late evaluation (d). There was no loss of the correction obtained for this patient and the clinical, radiologic and functional results were good
Fig. 10.
Preoperative radiography (a), immediate postoperative period (b), with 2 (c) and with 4 years follow-up (d). Despite the kyphosis of the fractured vertebral segment, the patient presented a good clinical result. The good clinical results were associated with ankylosis of the fractured vertebra
Discussion
Evaluation and comparison of thoracolumbar fractures should consider specific types of fractures with similar morpho-pathological characteristics. Burst fractures vary widely in morphology, so that it is difficult to obtain a homogeneous group for study and comparison [19, 25]. The burst fracture is an injury characterized by anterior vertebral body height loss and retropulsion of the posterior aspect of the vertebral body into the spinal canal. The vertebral body injury frequently is associated with fractures through the neural arch. Using a three-column concept of instability the division of these fractures into stable and unstable injuries is difficult [19, 20]. Radiographic signs of instability include widening of the interspinous and interlaminar distance, translation of more than 2 mm, kyphosis of more than 20°, dislocations, height loss of more than 50%, and articular process fractures [20]. The assessment of instability in these fractures is still not straightforward; the definition of instability by White and Panjabi [27] is abstract and in clinical practice different classification systems are applied [24].
Different treatments have been proposed for thoracolumbar burst fractures, with controversial results having been reported by different authors [1, 3, 23, 28, 25]. It remains unclear if conservative or operative treatment is more effective [24].
The parameters used for the evaluation of the final result (radiologic, clinical and functional) have contributed to an increasing debate about the ideal method for the treatment of these fractures. Although some studies included clinical outcome measures such as pain and functioning, many studies focused on radiological outcome only. One could argue that radiological changes are only relevant if they are strongly associated with changes in clinical outcomes, which is not necessarily true [24]. Radiographic measurement of angulation on the sagittal plane of the fractured vertebral segment has been extensively used for the evaluation and postoperative follow-up of patients and most clinical studies have been unable to establish a relationship between the degree of kyphosis of the operated vertebral segment, lumbar pain and functional limitation [9, 13, 23, 28].
Regarding the measurement of kyphosis, loss of surgical correction has been observed with the different treatment methods used such as conservative treatment, posterior fixation, posterior fixation with a transpedicular graft and, to a lesser extent, combined posterior fixation and anterior arthrodesis [1, 3, 10, 11, 13, 25]. This fact has led several authors to conclude that no ideal treatment able to restore the morphology of the vertebral segment to normal physiological levels is currently available for thoracolumbar spine fractures [25].
This loss has been correlated, among other factors, with the degree of comminution of the vertebral body, a fact that led McCormack et al. [16] to propose the load-sharing classification, considering this parameter for the indication of anterior spinal reconstruction [19].
A correlation of the preoperative scores on the load-sharing classification [16] with the loss of correction of the fractured vertebral body was observed in our patients. However, the behavior of the loss of correction was not uniform for patients with a high score on the load-sharing classification [16]. This fact indicates that other still unidentified factors may influence the loss of correction of the fractured vertebral segment.
When we analyzed separately the height of the fractured vertebral body and of its adjacent disks in the final evaluation of sagittal alignment we observed that the main factor related to the loss of the correction obtained by surgery was the reduced height of the intervertebral disks adjacent to the fractured vertebra. The disk proximal to the fractured vertebra presented more frequently a more important reduction of height. In agreement with data reported by others [9,10, 13], in our patients there was no significant loss of vertebral body height.
The involvement of the proximal intervertebral disk in the loss of correction of the present patients must be correlated with the morphological pattern of the fractures studied, which presented comminution of their cephalic portion. In this type of fracture the adjacent disk is affected by the fracture of the terminal vertebral plate and its content may be introjected into the cephalic portion of the vertebral body. The fracture or fissure of the terminal vertebral plate may contribute to changes of the intervertebral disk even in the absence of an initial traumatic injury to the disk [7, 18]. Qualitative discomanometry showed disk lesion in experimentally produced burst fractures. A fractured vertebra is easy to recognize, but the associated disk injuries are less well known. The disk injury may be not be apparent in radiographic images of burst fractures [26].
Loss of correction was observed in all of our patients and was significant in two of them, requiring an anterior approach and the placement of a tricortical graft as an anterior support. This loss indicates the need to use a structural support in some patients with burst fractures [1, 2, 4, 11]. However, this significant loss did not occur in all patients with high scores on the load-sharing classification [16] and submitted to the same type of treatment, indicating that other, still incompletely defined factors in addition to the degree of comminution of the vertebral body influence this process [7, 25].
Except for height of the vertebral disk proximal to the fractured vertebra, in our patient series we observed no correlation between most of the radiographic values studied and the functional results.
Evaluation of pain by means of the Denis scale showed that 66% of the patients had no pain even though radiographic loss of correction was present [11, 23, 28].
The scores obtained for functional evaluation using the SF-36 questionnaire were lower than reference values [2]. The values observed in our patient group agree with the results observed in other series, with no correlation between this parameter and loss of correction of the fractured vertebral segment. High scores were observed even in patients with a significant loss of the fractured vertebral segment [11, 13].
Only 50% of the patients studied were able to return to their previous job. The evaluation of these patients is very complex and involves biopsychosocial factors beyond the scope of the present study. However, we observed patients with radiographic loss of the fractured vertebral segment who were able to return to their previous occupation, indicating that the loss of correction probably was not directly related to this parameter [10, 17, 23].
The degeneration of the disk proximal to the fractured vertebra may be related to the poor functional results observed. The loss of intervertebral disk height may produce a certain instability in the vertebral segment and a relaxation of the oblique fibers of the fibrous annulus, which may contribute to degeneration of the intervertebral disk [14].
However, this degeneration was not observed in the MR study for the evaluation of the disks adjacent to the burst fractured vertebra during the preoperative period and after the removal of the synthesis material, which occurred on average after 10 months of evolution [7].
Analysis of our group of patients with burst fractures showed that the clinical and functional result was not related to the loss of correction of the fractured vertebral segment. Despite the loss of correction, which was serious in two patients and required an anterior support, there is no scientific evidence linking posttraumatic kyphosis to clinical outcomes [12, 22, 25, 28].
No correlation between correction of fracture and functional results was observed in the patients studied here. Only the loss of height of the intervertebral disk adjacent to the fractured vertebra was related to unsatisfactory functional results. The results observed in the present group of patients suggest that other still undefined parameters influence the functional result of surgery for thoracolumbar spine fractures.
Conclusion
Arthrodesis and posterior fixation of burst fractures did not achieve maintenance of the intraoperative correction, with loss of correction of varying degrees occurring in all patients operated upon. Reconstruction of the anterior spine was necessary in two of the patients studied (20%). In the remaining patients the loss of radiologic correction showed no correlation with the functional results. The loss of height of the intervertebral disk adjacent to the fractured vertebra was the only radiologic parameter studied that showed correlation with the functional results obtained on the occasion of the evaluation performed two years after surgery.
References
- 1.Been HD, Bouma GJ. Comparison of two types of surgery for thoracolumbar burst fractures: Combined anterior and posterior stabilisation vs posterior instrumentation only. Acta Neurochir. 1999;1999:349–357. doi: 10.1007/s007010050310. [DOI] [PubMed] [Google Scholar]
- 2.Briem D, Linhart D, Lehmann W, Bullinger M, Schoder V, Meenen NM, Windolf J, Rueger JM. Investigation of the health-related quality of life after a dorso ventral stabilization of the thoracolumbar junction. Unfallchirurg. 2003;106:625–632. doi: 10.1007/s00113-003-0627-4. [DOI] [PubMed] [Google Scholar]
- 3.Defino HL, Rodriguez-Fuentes AE. Treatment of fractures of the thoracolumbar spine by combined anteroposterior fixation using the Harms method. Eur Spine J. 1998;7:187–194. doi: 10.1007/s005860050054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Defino HL, Scarparo P. Fractures of thoracolumbar spine: monosegmental fixation. Injury. 2005;36(Suppl 2):B90–B97. doi: 10.1016/j.injury.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 5.Farcy JP, Weidenbaunn M, Glassman SD. Sagittal index in management of thoracolumbar burst fractures. Spine. 1990;15:958–965. doi: 10.1097/00007632-199009000-00022. [DOI] [PubMed] [Google Scholar]
- 6.Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH, Vernon JD, Walsh JJ. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7:179–192. doi: 10.1038/sc.1969.30. [DOI] [PubMed] [Google Scholar]
- 7.Furderer S, Wenda K, Thiem N, Hachenberger R, Eysel P. Traumatic intervertebral disc lesion–magnetic resonance imaging as a criterion for or against intervertebral fusion. Eur Spine J. 2001;10:154–163. doi: 10.1007/s005860000238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gatchel RJ, Mayer T, Dersh J, Robinson R, Polatin P. The association of the SF-36 health status survey with 1-year socioeconomic outcomes in a chronically disabled spinal disorder population. Spine. 1999;24:2162–2170. doi: 10.1097/00007632-199910150-00017. [DOI] [PubMed] [Google Scholar]
- 9.Knop C, Fabian HF, Bastian L, Blauth M. Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine. 2001;26:88–99. doi: 10.1097/00007632-200101010-00016. [DOI] [PubMed] [Google Scholar]
- 10.Knop C, Fabian HF, Bastian L, Rosenthal H, Lange U, Zdichavsky M, Blauth M. Fate of the transpedicular intervertebral bone graft after posterior stabilisation of thoracolumbar fractures. Eur Spine J. 2002;11:251–257. doi: 10.1007/s00586-001-0360-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Korovessis P, Baikousis A, Zacharatos S, Petsinis G, Koureas G, Iliopoulos P. Combined anterior plus posterior stabilization versus posterior short-segment instrumentation and fusion for mid-lumbar (L2–L4) burst fractures. Spine. 2006;31:859–868. doi: 10.1097/01.brs.0000209251.65417.16. [DOI] [PubMed] [Google Scholar]
- 12.Kraemer WJ, Schemitsch EH, Lever J, McBroom RJ, McKee MD, Waddell JP. Functional outcome of thoracolumbar burst fractures without neurological deficit. J Orthop Trauma. 1996;10:541–544. doi: 10.1097/00005131-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Leferink VJ, Keizer HJ, Oosterhuis JK, Sluis CK, ten Duis HJ. Functional outcome in patients with thoracolumbar burst fractures treated with dorsal instrumentation and transpedicular cancellous bone grafting. Eur Spine J. 2003;12:261–267. doi: 10.1007/s00586-002-0518-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lu YM, Hutton WC, Gharpuray VM. Can variations in intervertebral disc height affect the mechanical function of the disc? Spine. 1996;21:2208–2216. doi: 10.1097/00007632-199610010-00006. [DOI] [PubMed] [Google Scholar]
- 15.Magerl F, Aebi M, Gertzbein SD, Harms J, Nazarian S. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184–201. doi: 10.1007/BF02221591. [DOI] [PubMed] [Google Scholar]
- 16.McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine. 1994;19:1741–1744. doi: 10.1097/00007632-199408000-00014. [DOI] [PubMed] [Google Scholar]
- 17.McLain RF. Functional outcomes after surgery for spinal fractures: return to work and activity. Spine. 2004;29:470–477. doi: 10.1097/01.BRS.0000092373.57039.FC. [DOI] [PubMed] [Google Scholar]
- 18.Natarajan RN, Ke JH, Andersson GB. A model to study the disc degeneration process. Spine. 1994;19:259–265. doi: 10.1097/00007632-199402000-00001. [DOI] [PubMed] [Google Scholar]
- 19.Parker JW, Lane JR, Karaikovic EE, Gaines RW. Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: a consecutive 41/2-year series. Spine. 2000;25:1157–1170. doi: 10.1097/00007632-200005010-00018. [DOI] [PubMed] [Google Scholar]
- 20.Petersilge CA, Emery SE. Thoracolumbar burst fracture: evaluating stability. Semin Ultrasound CT MR. 1996;17:105–113. doi: 10.1016/S0887-2171(96)90010-4. [DOI] [PubMed] [Google Scholar]
- 21.Steib JP, Aoui M, Mitulescu A, Bogosin I, Chiffolot X, Cognet JM. Thotacolumbar fractures surgically treated by “in situ” contouring. Eur Spine J. 2006;12:1823–1832. doi: 10.1007/s00586-006-0161-5. [DOI] [PubMed] [Google Scholar]
- 22.Thomas KC, Bailey CS, Dvorak MF, Kwon Fisher B. Comparison of operative and nonoperative treatment for thoracolumbar burst fractures in patients without neurological deficit: a systematic review. J Neurosurg Spine. 2006;4:351–358. doi: 10.3171/spi.2006.4.5.351. [DOI] [PubMed] [Google Scholar]
- 23.Tropiano P, Huang RC, Louis CA, Poitout DG, Louis RP. Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine. 2003;28:2459–2465. doi: 10.1097/01.BRS.0000090834.36061.DD. [DOI] [PubMed] [Google Scholar]
- 24.Roer N, Lange ES, Bakker FC, Vet HC, Tulder MW. Management of traumatic thoracolumbar fractures: a systematic review of the literature. Eur Spine J. 2005;14:527–534. doi: 10.1007/s00586-004-0847-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Verlaan JJ, Diekerhof CH, Buskens E, Tweel I, Verbout AJ, Dhert WJ, Oner FC. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine. 2004;29:803–814. doi: 10.1097/01.BRS.0000116990.31984.A9. [DOI] [PubMed] [Google Scholar]
- 26.Wang JL, Panjabi MM, Kato Y, Nguyen C. Radiography cannot examine disc injuries secondary to burst fracture: quantitative discomanometry validation. Spine. 2002;27:235–240. doi: 10.1097/00007632-200202010-00006. [DOI] [PubMed] [Google Scholar]
- 27.White AA, Panjabi MM. Clinical biomechanics of the spine. Philadelphia: J. B. Lippincoatt; 1978. p. 534. [Google Scholar]
- 28.Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V, Butterman G. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A:773–781. doi: 10.2106/00004623-200305000-00001. [DOI] [PubMed] [Google Scholar]