Abstract
Pedicle screw fixation has achieved significant popularity amongst spinal surgeons for both single and multi-level spinal fusion. Misplacement and pedicle cortical violation occurs in over 20% of screw placement and can result in potential complications such as dysthesia, paraparesis or paraplegia. There have been many advances in techniques available for navigating through the pedicle; however, these techniques are not without drawbacks. A new electrical conductivity-measuring device, previously evaluated on the porcine model to detect the pedicle violation, was evaluated amongst nine European Hospitals to be used in conjunction with the methods currently used in that centre. This new device is based on two original principles; the device is integrated in the drilling or screwing tool. The technology allows real-time detection of perforation through two independent parameters, impedance variation and evoked muscle contractions. Data was collected twofold. Initially, the surgeon was given the device and a comparison was made between the devices ability to detect a breech and the surgeon’s ability to detect one using his traditional methods of pedicle preparation. In the second module of the study, the surgeon was limited to using the electrical conductivity detection device as their sole guide to detect pedicle breaches. A comparison was made between the detection ability of the device and the other detection possibilities. Post-operative fine cut CT scanning was used to detect the pedicle breaches. Overall, the 11 trial surgeons performed a total of 521 pedicle drillings on 97 patients. Initially there were 147 drillings with 23 breaches detected. The detection rate of these breaches were 22/23 for the device compared to 10/23 by the surgeon. Over both parts of the study 64 breaches (12.3%) were confirmed on post-operative CT imaging. The electrical conductivity detection device detected 63 of the 64 breaches (98.4%). There was one false negative and four false positives. This gives the device an overall sensitivity of 98% and specificity of 99% for detecting a pedicle breach. The negative predictive value was 99.8%, with a positive predictive value of 94%. No adverse event was noted with the use of the electrical conductivity device. Electrical conductivity monitoring may provide a simple, safe and sensitive method of detecting pedicle breech during routine perforation of the pedicle, in the course of pedicle screw placement.
Keywords: Pedicle screws, PediGuard, Electrical conductivity measuring device, Impedance measuring device, Spine
Introduction
Pedicle screw fixation has become one of the most widely practiced fusion operations [17, 21]. The incidence of misplaced pedicle screws using conventional techniques (surgeon’s feel, anatomic landmarks and fluoroscopy) ranges from 10 to 55% [7, 8, 22, 25]. The consequences of mis-directing screws are well documented and have led to increased interest for more accurate placement methods [7, 8, 14].
Several methods have been utilized to increase the accuracy of screw placement. somatosensory evoked potentials (SSEP), motor evoked potentials, compound muscle action potentials (CMAP), electromyography recordings (EMG), intra-operative fluoroscopy, computed tomography (CT) and most recently computer-aided frameless stereotaxis [2, 3, 5, 6, 11, 15, 16]. Although all of these tools offer varying degrees of benefit, they all have limitations.
Neurophysiological monitoring requires the presence of trained neurophysiology personnel in theatre during screw placement. Recording of sensory or motor evoked potentials rely on the detection of impingement on nervous tissue. At that stage a full cortical breech has occurred. In terms of a warning system these methods are flawed because the surgeon is alerted far too late in the whole process when the crisis of impaired nervous function has been detected.
All neurophysiological recordings are subject to interference by numerous intra-operative parameters including anaesthetic agents, body temperature, blood pressure, electrical interference, electrical contacts and blood chemistry [16, 20]. Beatty et al. [3] reported false-negative results as high as 23% with continuous EMG monitoring during pedicle screw placement. Both CMAP and EMG recordings require the use of subtotal neuromuscular blockade.
With advances in computer technology, image-guidance in the spine has become an interactive means of using a surgical pointer or tool at the time of surgery and visualizing a corresponding virtual tool on images on a computer workstation in the operating theatre. It offers the surgeon many benefits for the safe and accurate placement of spinal instrumentation [9, 10]. Computer-aided stereotactic navigation provides a three-dimensional guide for pedicle screw placement [5]. Image guidance can facilitate pre-operative planning and help determine the optimal trajectory for screw placement. Although computer image guidance remains a very useful tool in complex spinal cases it too has drawbacks. It remains an expensive tool, requiring pre-operative CT scanning, registration technique, requires a wide range of experience and formal training, and is relatively time consuming especially if more than one registration is necessary for multilevel problems. However, more recent spinal navigation systems using 3D reconstruction from initial fluoro C-Arm images without the need of pre-operative CT scanning or intra-operative registration has become available to the spinal surgeon, little information is available in current literature as to accuracy in navigation of the pedicles. Further these images are also obtained ‘pre-operatively’ all be it within the theatre and do not reflect real time activity.
The use of intra-operative fluoroscopy for placement of pedicle screws has resulted in prolonged fluoro time and radiation exposure to the surgical personnel and patient [18]. Finally, the use of computed tomography for the assessment of pedicle screw position after surgery is too late.
Because of the limitations of the current guidance aids, a new device was designed to help surgeons during pedicle drilling. This new device was based on two original principles. First, which the drilling tool would be similar to a current standard spinal tool. Second, that technology built into the tip would allow real time detection of pedicle breaches.
Initial studies carried out using a large animal model confirmed that the electrical conductivity variation detection capability of this device offers a potentially simple technique to detect pedicle perforations, prior to inserting the screw [4]. A multi-centre trial was undertaken for clinical validation. The aim of this study was to ascertain if this electrical conductivity-measuring device could detect the presence of pedicle cortical breaches and if the detection rate was superior to the surgeon’s traditional methods of detecting breaches.
Methods
A multi-centre clinical trial was undertaken from September 2002 to September 2004. Eleven senior surgeons in nine European centres were enrolled in the study (Table 1). Each centre obtained local ethics committee approval. Each surgeon was given the electrical conductivity detection device (PediGuard™, SpineVision) and asked to use the device in lieu of his regular pedicle-drilling instrument. Pedicle screws were then inserted using each surgeon’s usual protocol.
Table 1.
Number of enrolled patients per European centres
| Centre | Number of Patients |
|---|---|
| Dublin, Ireland | 22 |
| Paris, France | 17 |
| Geneva, Switzerland | 16 |
| Milan, Italy | 12 |
| Paris, France | 9 |
| Rome, Italy | 9 |
| Bordeaux, France | 6 |
| Barcelona, Spain | 3 |
| Madrid, Spain | 3 |
Data was collected twofold. Initially, the surgeon used the new instrument as a pedicle awl but was asked to rely on his usual traditional methods to detect pedicle breaches (i.e. the surgeons normal protocol for inserting pedicle screws). The output from the electrical conductivity device was also noted during each pedicle drilling. Post-operative fine-cut CT imaging was obtained through the pedicle to see if a breach had occurred.
CT scanning protocol
CT scanning was carried out on a 16 multislice scanner using 2 mm slices with a maximum Kernel resolution. The scan was orientated craniocaudal to include the vertebrae of interest with no angulations. These scans were then reconstructed in 1 mm slices with a 0.7 mm increment to allow for overlapping. All scans were reviewed by an independent radiologist to assess for the presence of breaches. The surgeon’s ability to detect a pedicle breach by his usual methods was compared to those detected by the device.
In the second module of the study, the surgeon was limited to using the electrical conductivity detection device as their sole guide to detect pedicle breaches. The accuracy of the tool was assessed for detecting a breach in isolation by obtaining post-operative CT.
Outcome measures
The primary outcome measure was the ability of the device to detect pedicle breaches against any other available possibility. Thus, a comparison was made between the devices ability to detect breaches and the methods each surgeon normally relied on prior to enrolling in the study (surgeon’s tactile feel, mechanical probing, fluoroscopy, CT scans, EMG, SEEP, computer assisted navigation; depending on their availability in each centre), versus the actual number of breaches that were visible on post-operative CT scanning.
The following parameters were computed for analysis purposes.
False positive: if device tells there is a breach through a rise in the auditory alert and after CT scanning there is none
False negative: if device tells there is a no breach, no rise in the auditory alert, and after CT scanning there is one
Positive predictive value: probability of a breach if detection occurred
Negative predictive value: probability of no breach if no detection occurred
Specificity: probability of no-detection if there is no breach
Sensitivity: probability of detection if there is a breach.
Statistical analysis was carried out using a standard statistical package (JMP, SAS Institute, USA), coupling the frequency of breaches, either detected by the device or the surgeon, using post-operative CT scanning. Using the Pearson’s non-parametric test, we evaluated the correlation between the detection of breaches by the device and the surgeon using pedicle probing.
The electrical conductivity device
The device was designed as a free hand drilling instrument that measures electrical conductivity at the tip. The measured conductivity is translated into a visual and an audio signal to inform in real time when a change occurs at the tip. It features bipolar electrodes that avoid any shunting effect and keep the measured conductivity independent of the insertion depth. In a uniform medium the electrical conductivity remains constant while the instrument is advanced into the vertebral pedicle. Variation of conductivity occurs when the instrument passes through a boundary between two different media (Fig. 2).
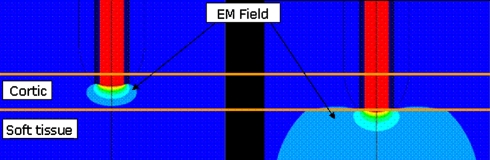
Fig. 2.
Electromagnetic field (EM) shape. Left in the cortical bone prior to a breach; Right immediately prior to the breach in soft tissue
The electrical conductivity device consists of an awl instrument with a hollow handle that accepts a built-in electronic printed circuit board (Fig. 1). The electronic components allow performing electrical conductivity measurement and translation to audible signal and coloured light emitting diodes (LEDs) to be used as feedback to the surgeon five times per seconds. In addition it also features a neurostimulator that can be used in conjunction with a standard EMG.
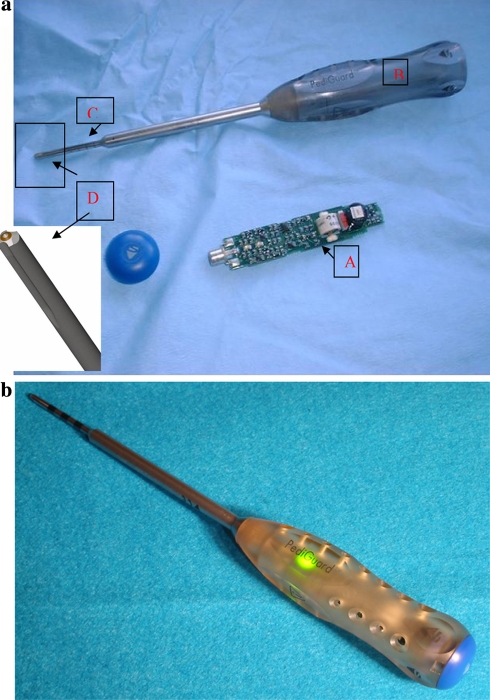
Fig. 1.
a
Picture of the device dissembled. The disposable circuit board (A) is placed into the hollow handle (B) of the device. The tip of the device (C) is a standard drilling tool for pedicle preparation with the electromagnetic field sensor at the tip (D) (inset enlarged picture of tip) b
Assembled device with the LED activated
Results
Of the 147 pedicle drillings on the first arm of the study there were a total of 23 (16%) breaches detected on post-operative CT scanning. The device detected 22 (96%) of these breaches during the actual pedicle drilling compared to 10 (43%) detected by the surgeon (Pearsons 74.242; P ≤ 0.001) (Table 2).
Table 2.
Table of results of breaches detected by either device or surgeon during pedicle preparation
| First arm of study | Second arm of Study | Total | |
|---|---|---|---|
| Detected by surgeon | 10/23 (43%) | N/A | 10/23 (43%) |
| Detected by device | 22/23 (96%) | 41/41 (100%) | 62/64 (97%) |
| Detected on CT scanning | 23 (16%) | 41 (11%) | 64 (12%) |
| Total drillings | 147 | 374 | 521 |
There was one breach which went undetected by the auditory alert mechanism of the device (false negative); however, there was a visible contraction of the patient’s leg caused by the neurostimulator component of the device. Considering this paper is focusing on the electrical conductivity component of the device this detection of the breach was classed as “not detected”. On one occasion the device gave an auditory alert indicating that a breach had occurred, but no such breach was detected on post-operative CT scanning (false positive). Therefore the device yielded a positive predictive value 96% and a negative predictive value of 99%. Combining these results the device sensitivity is 96% with a specificity of 99% (Table 3).
Table 3.
Statistical analysis of the device
| First arm of study (%) | Second arm of study (%) | Total (%) | |
|---|---|---|---|
| Positive predictive valuea | 96 | 93 | 94 |
| Negative predicative valueb | 99 | 100 | 100 |
| Specificityc | 96 | 100 | 98 |
| Sensitivityd | 99 | 99 | 99 |
aProbability of a breach if detection occurred
bProbability of no breach if no detection occurred
cProbability of no detection if there is no breach
d Probability of detection if there is a breach
In the second arm of the study there were 374 pedicle drillings performed on 69 patients with 41 (11%) confirmed breaches on post-operative CT scanning. The device detected all of these breaches (Pearsons 374.000; P ≤ 0.001). During this phase of the study there was no differentiation made between the surgeons pick-up of breaches (Table 2).
There were no false negative recorded with three false positives during this part of the study. This gives a positive predictive value of 93% with a negative predictive value of 100%, coupling these figures yields a sensitivity of 100% with a specificity of 99% (Table 3).
Combining these figures together there was a total of 521 drillings on 97 patients. In total there were 64 (12%) breaches confirmed on post-operative CT scanning. Overall the device detected 63 (98%) of these breaches (Table 2) with 4 false positives. This gives an overall positive predictive value of 94% with a negative predictive value of 99.8%. Coupling all these figures yields a 98% sensitivity and 99% specificity.
There were no adverse events noted with the use of this device. Although it was outside the scope of this paper to look at length of tine for screw placement, the trial surgeons reported no noticeable difference or even less time taken once familiar with the device.
Discussion
The popularity of spinal instrumentation has soared over the past decade [17]. With the increased usage of these techniques, the associated complications have become relatively more common [17]. The traditional methods of good anatomical knowledge, combined with an experienced surgeon’s feel during the pedicle drilling allows correct placement of the majority of pedicle screws. There is however a proportion of screws that end-up poorly positioned [13]. Some of these misplaced screws result in injury to the patient [7, 8]. As well as immediate complications, the development of late kyphotic complications have also been associated with poor screw positioning [1].
Numerous different aids have been used to try and decrease the frequency of wayward screws including fluoroscopy, neurophysiological monitoring [23] and more recently computer image guidance [19]. The shear numbers of different aids that have been tried, testify to the deficiencies that each one has. Up until now no user friendly device has been available that would allow instant feedback, and would achieve that primary end point of early detection of pedicle breaches.
The device used in this study is a wireless perforation instrument, (similar to a conventional pedicle awl), working on the principle of local tissue electrical conductivity, which is monitored at the tip of the instrument. When the electrical conductivity at the distal part of the instrument changes, it alerts the surgeon. It is novel in the fact that it allows detection of cortical breaches before the full breach has occurred. This is possible because changes in the electromagnetic field around the tip of the instrument allow detection of media that are of a different consistency to bone (Fig. 2).
The device is integrated in the drilling tool, and the technology allows real-time detection of perforation through two independent parameters, electrical conductivity variation and evoked muscular contractions. The device is therefore able to detect iatrogenic breaches in the vertebral pedicle wall prior to screw insertion and therefore allows the surgeon to redirect. The device’s in-built neuro-stimulator can warn of close approximation to nervous tissue either by causing visible twitching in the lower limbs or be detected by an EMG machine.
Measurements of absolute electrical conductivity values have previously been shown not to be useful in detecting pedicle breaches [6]. This is because there is a wide variation in pedicle electrical conductivity between subjects. Other problems identified by previous authors include inaccuracies with partial shunting when monopolar probes were used. Shunting or partial shunting can occur if a pilot hole is drilled prior to inserting the electrical conductivity measurement device [24]. Blood and tissue products that accumulate in the pilot hole can lead to inaccuracies of electrical conductivity detection. By incorporating the electronic detection into the perforation tool, as has been done in this device, this problem has been overcome. The device features bipolar electrodes that avoid any shunting effect and keep the measured electrical conductivity independent of the insertion depth.
The electrical conductivity measurement has a sensitivity of >98% in the detection of breaches. The electrical conductivity-measuring device detected 52% more breaches than the actual surgeon performing the surgeries. Therefore the tool is giving real-time feedback to the surgeon, without the surgeon having to change instruments and therefore not loosing momentum during pedicle preparation.
In this study there were four false positives. However, the surgeon was free to redirect the screw once a breech was detected by the device, it is therefore possible that screw re-direction rendered a true breech into a false positive on post-operative scanning. In relation to the single false negative, it should be noted that the breech was detected by the EMG component of the device and thus the surgeon was still alerted to the fact that a breech had occurred.
There is no need for pre-operative CT scanning or pre-operative planning, which time is saving for the surgical team. Because this tool does not require computer registration or vertebral tracking it can be used in all aspects of spinal fixation, inclusive of fractures and spondylolisthesis cases, regardless of the degree of pars fracture and dislocation.
This instrument offers the surgeon real-time monitoring with minimal effect to the standard surgical procedure.
Conclusion
Electrical conductivity measuring may provide a simple, safe and sensitive method of detecting pedicle breeches during routine perforation of the pedicle when placing pedicle screws.
References
- 1.Acikbas SC, Arslan FY, Turner MR. The effect of transarticular screw misplacement on late spinal stability. Acta Neurochir. 2003;145:949–954. doi: 10.1007/s00701-003-0116-0. [DOI] [PubMed] [Google Scholar]
- 2.Amiot L, Lang K, Zippel H. Comparison accuracy between conventional and computer-assisted pedicle screw installation. J Bone Joint Surg [Br] 1998;80:240. doi: 10.1302/0301-620X.80B2.8036. [DOI] [Google Scholar]
- 3.Beatty RM, McGuire P, Moroney JM. Continuous intraoperative electromyographic recording during spinal surgery. J Neurosurg. 1995;82:401–405. doi: 10.3171/jns.1995.82.3.0401. [DOI] [PubMed] [Google Scholar]
- 4.Bolger C, Carozzo C, Roger T, McEvoy L, Nagaria J, Vanacker G, Bourlion M. A preliminary study of reliability of impedance measurement to detect iatrogenic initial pedicle perforation (in the porcine model) Eur Spine J. 2005;15(3):316–320. doi: 10.1007/s00586-005-1024-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bolger C, Wigfield C. Image-guided surgery: applications to the cervical and thoracic spine and a review of the first 120 procedures. J Neurosurg. 2000;92:175–180. doi: 10.3171/spi.2000.92.2.0175. [DOI] [PubMed] [Google Scholar]
- 6.Darden BV, Wood KE, Hatley MK, Owen JH, Kostuik J. Evaluation of pedicle screw insertion monitored by intraoperative evoked electromyography. J Spinal Disord. 1996;9:8–16. [PubMed] [Google Scholar]
- 7.Davane SH, Myers DL. Complications of lumbar spine fusion with transpedicular instrumentation. Spine. 1992;17:362–367. doi: 10.1097/00007632-199203000-00021. [DOI] [PubMed] [Google Scholar]
- 8.Esses SI, Sachs BL, Dreyzin V. Complications associated with technique of pedicle screw fixation. Spine. 1993;18:2231–2239. doi: 10.1097/00007632-199311000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Foley K, Smith M. Image-guided spine surgery. Neurosurg Clin N Am. 1996;7:171–186. [PubMed] [Google Scholar]
- 10.Foley KT, Simon DA, Rampersaud YR. Virtual fluoroscopy: computer-assisted fluoroscopic navigation. Spine. 2001;26:347–351. doi: 10.1097/00007632-200102150-00009. [DOI] [PubMed] [Google Scholar]
- 11.Gundanna M, Eskenazi M, Bendo J, Spivak J, Moskovich R. Somatosensory evoked potential monitoring of lumbar pedicle screw placement for in situ posterior spinal fusion. Spine J. 2003;3:370–376. doi: 10.1016/S1529-9430(03)00144-X. [DOI] [PubMed] [Google Scholar]
- 12.Herdmann J, Deletis V, Edmonds HL, Morota N. Spinal cord and nerve root monitoring in spine surgery and related procedures. Spine. 1996;21:870–877. doi: 10.1097/00007632-199604010-00023. [DOI] [PubMed] [Google Scholar]
- 13.Kim YJ, Lenke LG, Bridwell KH, Cho YS, Riew KD. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine. 2004;29:333–342. doi: 10.1097/01.BRS.0000109983.12113.9B. [DOI] [PubMed] [Google Scholar]
- 14.Laine T. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutaive patients. Eur Spine J. 2005;9:235–240. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Laine T, Lund T, Ylikoski M, Lohikoski J, Schlenzka D. Accuracy of pedicle screw insertion with and without computer assistance: a randomised controlled clinical study in 100 consecutive patients. Eur Spine J. 2000;9:235–240. doi: 10.1007/s005860000146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lubicky J, Spadaro J, Yuan H, Fredrickson B, Henderson N. Variability of somatosensory cortical evoked potential monitoring during spinal surgery. Spine. 1989;14:790–798. doi: 10.1097/00007632-198908000-00003. [DOI] [PubMed] [Google Scholar]
- 17.Nohara Y, Taneichi H, Ueyama K, Kawahara N, Shiba K, Tokuhashi Y, Tani T, Nakahara S, Iida T. Nationwide survey on complications of spine surgery in Japan. J Orthop Sci. 2004;9:424–433. doi: 10.1007/s00776-004-0802-7. [DOI] [PubMed] [Google Scholar]
- 18.Rampersaud YR, Foley KT, Shen AC, et al. Radiation exposure to the spine surgeon during fluroscopically assissted pedicle insertion. Spine. 2000;25:2637–2645. doi: 10.1097/00007632-200010150-00016. [DOI] [PubMed] [Google Scholar]
- 19.Rampersaud YR, Pik JH, Salonen D, Farooq S. Clinical accuracy of fluoroscopic computer-assisted pedicle screw fixation: a CT analysis. Spine. 2005;30:E183–E190. doi: 10.1097/01.brs.0000157490.65706.38. [DOI] [PubMed] [Google Scholar]
- 20.Rappaport M, Lenord J, Portillo S. Effect of anaesthesia and stimulus intensity on posterior tibial nerve somatosensory evoked potentials. Clin Electroencephalogr. 1992;23:24–30. doi: 10.1177/155005949202300107. [DOI] [PubMed] [Google Scholar]
- 21.Roy-Camille R, Saillant G, Mazel C. Internal fixation of the lumbar spine with pedicle screw plating. Clin Orthop. 1986;203:7–17. [PubMed] [Google Scholar]
- 22.Sagi H, Manos R, Ordway NR, Connolly PJ. Electromagnetic field-based image-guided surgery part one: results of a cadaveric study evaluating lumbar pedicle screw placement. Spine. 2003;28:2013–2018. doi: 10.1097/01.BRS.0000087851.51547.00. [DOI] [PubMed] [Google Scholar]
- 23.Shi YB, Binette M, Martin WH, Pearson JM, Hart RA. Electrical stimulation for intraoperative evaluation of thoracic pedicle screw placement. Spine. 2003;28:595–601. doi: 10.1097/00007632-200303150-00015. [DOI] [PubMed] [Google Scholar]
- 24.Toleikis JR. Neurophysiological monitoring during pedicle screw placement. In: Deletis, editor. Neurophysiology in neurosurgery. New York: Academic; 2002. pp. 231–234. [Google Scholar]
- 25.Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, An HS. Placement of pedicle screws in the thoracic spine. Part II: an anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200–1206. doi: 10.2106/00004623-199508000-00009. [DOI] [PubMed] [Google Scholar]