Abstract
Fractures of the thoracolumbar spine rank among the severest injuries of the human skeleton. Especially in younger patients they often result from high-energy accidents. Recently, a shift in paradigm towards more aggressive treatment strategies including anterior procedures could be observed. However, so far only few data exist reflecting the quality of life (QoL) after such injuries. The aim of this study was to evaluate medium-term QoL and further to identify factors that influence the clinical outcome in patients with fractures of the thoracolumbar spine. Data of 906 patients who were treated during a 10-year period in our institution were evaluated retrospectively. Only patients with single-level traumatic injuries aged between 18 and 65 years without neurological deficits, concomitant injuries of other locations and internal comorbidities were included into the investigation (n = 204). Three different treatment groups (i.e. non-operative, dorsal and dorsoventral stabilisation) were compared to healthy controls as well as different pain populations. The QoL was assessed using established questionnaires (SF-36, HFAQ, VAS-Spinescore, PRQ, and PTSD). Sixty-five percent of the included patients (n = 133) were studied at an average follow-up of 5.3 ± 1.7 years after injury. All treatment groups revealed an identical gender and age distribution. More severe and unstable injuries were found in the surgical groups associated with higher treatment costs and a longer inability to work. Compared to healthy controls, QoL was compromised to the same extent in all groups. Furthermore, all patients treated in this study did significantly better than low back pain individuals with regard to QoL and pain regulation parameters. In our study, patients with thoracolumbar spine fractures showed a reduced QoL compared to healthy controls. Thus, patients do not seem to regain their former QoL. However, the level of discomfort was comparably low in all groups, even in patients with more severe injuries requiring extensive surgery. Overall, outcome and QoL after traumatic fractures of the thoracolumbar spine rather seem to be determined by the severity of injury than by pain regulation or other psychosocial factors which is likely the case in low back pain disorders.
Keywords: Spine, Fracture, Surgery, Outcome, Quality of life
Introduction
Fractures of the thoracolumbar spine rank among the severest injuries of the human skeleton. Especially in younger patients, they often result from high-energy trauma, like MVA or falls from great height [33]. While stable fractures without neurological injury are often successfully treated conservatively, unstable injuries commonly require surgical intervention and stabilisation [4, 13, 21, 53].
If treated surgically, fractures are predominantly stabilised with a multitude of fixateur interne systems [14, 34]. However, it is a well-known phenomena that the dorsal stabilisation may fail to maintain intraoperative reduction leading to painful kyphotic deformity [31, 42, 58]. Therefore, the combined anterior and posterior stabilisation has been introduced as a suitable procedure to overcome the inadequate long-term stability of the dorsal stabilisation [1, 11, 22, 29, 37, 57, 61].
Beside such traditional parameters like long-term stability, feasibility of implants and approaches as well as cost effectiveness surgeons have recently begun to evaluate treatment success in a more patient-oriented way [15, 19, 27]. This includes to reflect the patient’s subjective perception and health-related quality of life (QoL). For this a variety of general and disease specific tools, most of them questionnaires, have been introduced [5, 6, 46].
Although vertebral fractures may be associated with adverse health effects such as back pain and disability, little is yet known about the impact of vertebral fracture on the QoL [30, 39]. One further problem is to define parameters that sufficiently represent health-related QoL in patients with thoracolumbar spine fractures and to identify suitable tools that allow for a reliable measurement of them [43].
The aim of our study was to evaluate the medium-term QoL and to identify factors with impact on the clinical outcome in patients after traumatic injuries of the thoracolumbar spine.
Methods
The charts of 906 patients with fractures of the thoracolumbar spine admitted to our institution in a 10-year period were reviewed retrospectively. Exclusion criteria were defined as followed: age > 65 years, neurological deficit, other major organ system or musculoskeletal injuries, occurrence of low back pain or other spinal disorders in the patient’s medical history requiring a specific medical treatment, serious mental disorders leading to medical intervention, pathological fractures, and insufficient knowledge of the German language.
Depending on the patterns of injury the patients of our study population were either treated non-operatively or surgically via posterior approach using a fixateur interne or else by means of a combined anterior and posterior two-stage procedure including ventral fusion with an autogenous bone graft taken from the left iliac crest and a fixed-angle implant (Table 1). Postoperatively the remobilisation of the patient was initialized in our hospital, and continued in the outpatient clinic or in a rehabilitation centre.
Table 1.
Indication and procedure of non-operative treatment as well as solely dorsal or combined anterior and posterior surgery for fractures of the thoracolumbar spine
| Treatment | Indication | Procedure | Implant |
|---|---|---|---|
| Non-operative | Stable fractures (type A1 and A2.1/2.2) | Short bedrest (Mobilization with brace) | – |
| Solely dorsal surgery | Posterior instability with minor anterior injury Minor vertebral height loss |
Open posterior approach Laminectomy if necessary |
USS®, Synthes |
| Combined stabilisation | Pincers injury Communition or complete burst of vertebra Severe vertebral height loss |
Open anterior approach (n = 10) Endoscopically since 2000 (n = 21) |
VentroFix®, Synthes (open surgery) MACS®, Aesculap (minimal-invasive) |
At the time of follow-up, the functional outcome was evaluated in cooperation with two independent research institutes using several standardised questionnaires (Table 2): Short Form-36 health survey (SF-36), Hannover Functional Ability Questionnaire (HFAQ), Pain Regulation Questionnaire (PRQ), 10-cm visual-analoge scale (VAS), and Posttraumatic Stress Disorders (PTSD) screening instrument by Stieglitz [12, 20, 32, 35, 51, 55]. In addition, the current social as well as the demographic status of the patient was determined and compared to the data obtained at primary admission.
Table 2.
Characteristics and parameters of the questionnaires used in this investigation in order to evaluate functional outcome and quality of life
| Questionnaire | Objective | Items | Interpretation |
|---|---|---|---|
| Short form-36 (SF-36) | Quality of life (QoL) | Physical functioning Role physical Bodily pain General health perception Vitality Social functioning Role emotional Mental health |
Scores 0–100 Higher Scores = Better results |
| Hannover functional ability score (HFAQ) | Activities of daily living (ADL) | 18 items as responses to ADL | Cumulative score 0–100 Higher Score = Better result |
| Pain regulation questionnaire (PRQ) | Ability to compensate pain | Pain competence Pain intensity Pain depression Pain anxiety Pain avoidance Pain withdrawal Pain distraction |
Scores 0–100 Higher Scores = Better results |
| Visual-analogue scale (VAS) | Back-related problems | 19 items | Cumulative scale 0–10 Higher Scale = Better result |
| Posttraumatic stress screening (PTSD) | Incidence of PTSD | 10 Posttraumatic stress symptoms | Score 10–70 Higher Score = Higher stress |
All data were given as mean values ± standard deviation (SD). The different treatment groups were compared by using a student’s t test. If the parameters were not normally distributed, a non-parametric assay was run instead (Mann-Whitney Rank Sum test). Frequency distributions were compared by using the Chi-square test. The sample size was confirmed as being sufficient by a power analysis. For this, the standard deviation was estimated to be ≤75% of the expected difference in means between the groups.
The clinical data were correlated with the parameters of the outcome measurement tools using Spearmans Rank Order Correlation test. Finally, multiple regression analyses were performed in order to assess the predictive value of social and demographic criteria on the different outcome parameters. All tests were calculated with a desired power of β = 0.8. A statistical level of α = 0.05 was considered significant. Statistical analyses were performed with the software program Sigma Stat/Sigma Plot.
Results
Two hundred and four patients who met the inclusion criteria were included into this investigation (Table 3). Sixty-five percent of these patients were examined (n = 133, 65 male, 68 female, average age 48.4 ± 14.2 years, range 21–65). Forty-two patients could not be located, 22 persons did not respond, six patients had died in the meantime of injury unrelated causes, and one patient refused to take part. Patients were assigned to three different treatment groups including non-operative treatment (n = 85), dorsal (n = 17) and combined stabilization (n = 31). Age as well as sex distribution did not statistically differ between the treatment groups (Table 4).
Table 3.
Incidence of criteria leading to exclusion of patients from the study
| Reason of exclusion | Non-operative | Dorsal | Dorsoventral |
|---|---|---|---|
| Neurologic deficit | 3 | 12 | 55 |
| Cerebral trauma | 2 | 23 | 12 |
| Blunt chest or abdominal trauma | 4 | 11 | 18 |
| Pelvic injury | 1 | 9 | 13 |
| Additional/multilevel spinal trauma | 6 | 10 | 19 |
| Severe trauma of the limbs (f.e. disabling joint injury) | 2 | 33 | 26 |
| Concomitant internal disease | 28 | 5 | 10 |
| Mental disorders | 26 | 8 | 4 |
| Age < 18 or > 65 years | 361 | 2 | 1 |
Table 4.
Age and sex distribution of patients included in the study; incidence of occupational accidents (O.A.) and posttraumatic stress disorders in the study population
| Patient characteristics | Non-operative | Dorsal | Dorsoventral |
|---|---|---|---|
| Sex distribution (f/m) | 41/44 | 7/10 | 17/14 |
| Age (years) | 47.8 ± 12.8 (Range 25–65) | 40.0 ± 14.4 (Range 21–65) | 47.7 ± 13.2 (Range 22–65) |
| Incidence of O.A. (n) | 16% (14/85, KI 9–26) | 52% (9/17, KI 27–77)* | 38% (12/31, KI 21–57) |
| Incidence of PTSD (n) | 11% (10/85, KI 5–20) | 41% (7/17, KI 18–67)* | 38% (12/31, KI 21–57)* |
*P < 0.05 versus non-operative
However, the patterns of injury widely differed between the groups, and a higher incidence of more unstable and severe fractures in the surgical groups precludes a direct comparison of outcome in the different treatment groups (Table 5). The higher severity of injuries in the surgical groups is further emphasized by the fact, that more patients of the surgical groups showed signs of posttraumatic stress disorders. A further difference was seen with regard to the incidence of occupational accidents, which was highest in the dorsal group (Table 4).
Table 5.
Fracture localization and classification in patients treated either non-operatively or surgically for fractures of the thoracolumbar spine
| Fracture pattern | Non-operative | Dorsal | Dorsoventral |
|---|---|---|---|
| Localization | |||
| Thoracic (Th1–Th10) | 14 | 2 | 3 |
| Transition (Th11–L2) | 62 | 14 | 24 |
| Lumbar (L3–L5) | 9 | 1 | 4 |
| Classification | |||
| A1, A 2.1, A2.2 | 80 | – | – |
| A2.3 | – | – | 6 |
| A3.1 | 5 | 13 | 7 |
| A3.2 | – | 1 | 7 |
| A3.3 | – | 6 | |
| B | – | 3 | 2 |
| C | – | – | 3 |
According to the more extensive surgical procedure the combined stabilisation was associated with a longer hospital stay and higher treatment costs as compared to patients either treated conservatively or stabilised via a dorsal approach only (Table 6). For the economic evaluation, treatment costs for daily medical care were calculated with a daily rate of 430 €. The costs of surgical treatment were calculated with a rate of 3.16 € per min. for anaesthesia and 2.76 € for the operating team.
Table 6.
Treatment cost of primary hospital stay in patients with thoracolumbar spine fractures after non-operative treatment, dorsal stabilization and dorsoventral surgery (data does not include costs of radiological examination, physiotherapy and consultation of departments other than traumatology)
| Treatment costs (€) | Non-operative | Dorsal | Dorsoventral |
|---|---|---|---|
| Metal implants | – | 2060.34 | 4165.10 |
| Surgery | – | 623.47 ± 124.88 | 1024.18 ± 252.71 |
| Primary hospital stay | 4469.18 ± 1935.57 | 5044.12 ± 1945.02 | 7282.26 ± 1435.77 |
| Primary costs overall | 4469.18 ± 1935.57 | 7727.93 ± 2069.90** | 12471.54 ± 1688.48**,## |
| DRG-revenues | 1850 | 4928 | 12156 |
**P < 0.001 versus non-operative; ##P < 0.001 versus dorsal
Assessment of the SF-36 performed at an average follow-up of 5.3 ± 1.7 years (range 3–8) showed an impaired QoL in all treatment groups compared to healthy controls (Table 7). The further analysis of the functional outcome by means of the HFAQ and the VAS showed similar results in all treatment groups (Figs. 1, 2). Overall working inabilty rate was 9%, again without differences between the treatment groups.
Table 7.
Medium-term quality of life according to the SF-36 questionnaire in patients with thoracolumbar spine fractures after non-operative treatment, dorsal stabilization and dorsoventral surgery compared to a healthy control group [12]
| Parameters SF-36 | Non-operative | Dorsal | Dorsoventral | Control |
|---|---|---|---|---|
| Physical functioning index (Pfi) | 74.93 ± 2.68* | 71.76 ± 6.30* | 75.96 ± 3.36* | 88.95 ± 5.57 |
| Role physical index (Rolph) | 68.83 ± 4.54* | 60.29 ± 8.31* | 77.41 ± 5.95** | 87.49 ± 8.75 |
| Bodily pain index (Pain) | 65.78 ± 2.87* | 56.47 ± 6.90* | 59.80 ± 3.85* | 78.90 ± 8.87 |
| General health perceptions index (Ghp) | 63.45 ± 2.41* | 54.17 ± 5.50* | 64.19 ± 4.09* | 68.00 ± 5.97 |
| Vitality index (Vital) | 53.56 ± 2.28* | 45.58 ± 3.58* | 58.38 ± 2.33 | 64.13 ± 5.21 |
| Social functioning index (Social) | 83.73 ± 2.49* | 64.70 ± 4.82* | 81.85 ± 4.05** | 89.36 ± 5.48 |
| Role emotional index (Rolem) | 77.16 ± 4.49* | 58.82 ± 10.89* | 83.87 ± 5.75* | 91.51 ± 7.19 |
| Mental health index (Mhi) | 66.35 ± 2.17* | 53.64 ± 3.25* | 69.54 ± 2.62 | 73.66 ± 4.91 |
*P < 0.05 versus control;**P < 0.001 versus control
Fig. 1.
Results of the VAS-Spinescore in patients after non-operative treatment, dorsal stabilization or dorsoventral surgery
Fig. 2.
Results of the HFAQ in patients after non-operative treatment, dorsal stabilization or dorsoventral surgery
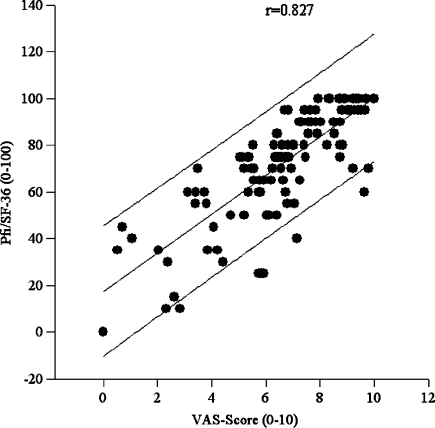
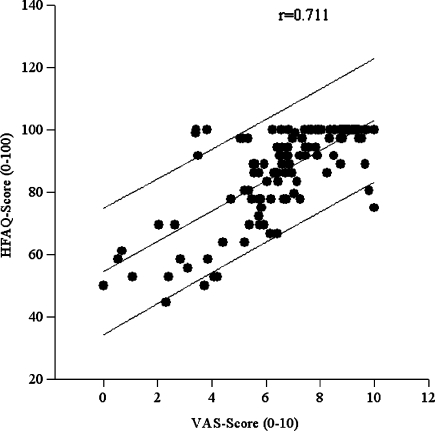
Analysis of the PRQ revealed significant better results in all study groups compared to low back pain individuals (Table 8). Patient-specific parameters (i.e. age, pain regulation) did neither correlate with nor predict hospital stay, working inability, treatment duration and QoL parameters, respectively (Table 9). A strong correlation was found between SF-36 subscales and the VAS on the one hand and between the VAS and the HFAQ on the other hand indicating that both, VAS and HFAQ are appropriate tools in QoL assessment (Figs. 3, 4).
Table 8.
Medium-term pain regulation according to the PRQ in patients with thoracolumbar spine fractures after non-operative treatment, dorsal stabilization and dorsoventral surgery compared to a low back pain control group [50]
| Parameters PRQ | Non-operative | Dorsal | Dorsoventral | Control |
|---|---|---|---|---|
| Pain competence | 41.40 ± 1.12** | 39.31 ± 1.82 | 40.66 ± 1.84* | 36.98 ± 8.41 |
| Pain intensity | 23.84 ± 1.30** | 26.29 ± 1.77 | 24.26 ± 1.94** | 29.55 ± 8.62 |
| Pain anxiety | 26.63 ± 11.59** | 25.00 ± 2.86** | 25.73 ± 2.07** | 31.90 ± 8.58 |
| Pain depression | 21.15 ± 1.27** | 21.76 ± 2.09 | 21.03 ± 1.88* | 25.33 ± 9.60 |
| Pain avoidance | 25.718 ± 0.94 | 26.62 ± 1.6 | 26.46 ± 1.67 | 25.38 ± 8.10 |
| Pain withdrawal | 24.93 ± 1.23** | 28.82 ± 2.26 | 23.40 ± 1.95 | 28.90 ± 10.90 |
| Pain distraction | 33.29 ± 1.03 | 34.17 ± 2.19 | 35.09 ± 1.60 | 32.37 ± 8.21 |
*P < 0.05 versus control;**P < 0.001 versus control
Table 9.
Spearman’s rank order correlation of several pairs of parameters
| Age | Hospital stay | Inability to work | VAS | HFAQ | Pfi | Pain | Comp | Intens | Depr | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age | 1.0 | 0.07 | −0.03 | −0.04 | −0.258 | −0.24 | −0.15 | 0.04 | −0.02 | 0.003 |
| Hospital stay | 1.0 | 0.47 | −0.002 | −0.1 | −0.18 | −0.2 | 0.004 | 0.05 | 0.11 | |
| Inability to work | 1.0 | −0.19 | −0.1 | −0.24 | −0.24 | 0.04 | 0.1 | 0.02 | ||
| VAS | 1.0 | 0.711 | 0.83 | 0.78 | 0.1 | −0.15 | −0.19 | |||
| HFAQ | 1.0 | 0.768 | 0.664 | 0.05 | −0.12 | −0.12 | ||||
| Physicalfunctioning index (Pfi) | 1.0 | 0.87 | 0.05 | −0.15 | −0.17 | |||||
| Bodily pain index (Pain) | 1.0 | 0.04 | −0.12 | −0.12 | ||||||
| Pain competence (Comp) | 1.0 | −0.63 | −0.74 | |||||||
| Pain intensity (Intens) | 1.0 | 0.69 | ||||||||
| Pain depression (Depr) | 1.0 |
Fig. 3.
Significant positive correlation between single components of the SF-36 (Physical functioning index, Pfi) and the VAS spine score
Fig. 4.
Significant positive correlation between the Hannover functional ability questionnaire (HFAQ) and the VAS spine score
Discussion
Quality of life assessment
Assessment of general health-related QoL has nowadays become an important integral part in evaluating the success of a specific medical treatment. For the latter well-defined questionnaires, such as SF-12, SF-36, Nottingham Health Profile, or Sickness Impact Profile have been established reflecting the patient’s subjective complaints and contentedness [3, 28, 59, 60]. In addition so called preference-based health profile instruments like the EQ-5D or the SF-6D can be used for outcome studies [8, 16].
The short form questionnaire with 36 questions, referred to as SF-36, has been widely used in several areas of medicine including a variety of spinal disorders [7, 18, 20, 39, 62]. It delivers normative data and provides a documented reliability and validity enabling the user to compare different treatment groups between each other and with regard to the age-referenced norm populations [46]. Furthermore, the SF-36 correlates with socioeconomic outcomes in spinal disorder populations [17]. After German translation and validation, the SF-36 has been used been used at our institution for QoL studies regularly [9–12].
Studies should preferably consist of a controlled randomized investigation where assessment is carried out at baseline and two years after trauma. However, baseline data in trauma patients will usually not be available and trauma populations often include a variety of fracture patterns requiring differentiated decision making and application of different treatment protocols. For example, thoracolumbar spine fractures of Magerl’s type B or C often require surgical stabilization and thus, are treated operatively in most of the cases. This explains the paucity of data from controlled randomized studies.
In our study QoL was assessed by psychometric testing with the SF-36, which represents a reliable and powerful tool for this purpose. The results indicate that a slightly impaired QoL has to be expected in patients with fractures of the thoracolumbar spine compared to healthy controls. In line with this observation several other study groups have previously described quite similar results with regard to the SF-36 [7, 39, 41, 49, 62].
The impact of radiological data on functional outcomes has been controversially discussed in the past. We have already demonstrated that radiological outcome (i.e. kyphotic deformation) does not seem to influence QoL after injuries of the thoracolumbar spine and, therefore, not omitted this parameter in our current study [9, 10]. These findings are in line with the data published by other investigators [39, 41, 49].
Functional Outcome
Back-related symptoms can be measured with a variety of scoring systems, such as the oswestry disability index (ODI), the Roland Morris disability questionnaire (RMDQ), the low back outcome score (LBOS), the NASS lumbar spine outcome (NASS LSO), and the Quebec back pain disability scale (QBPDS). Of the latter, the ODI, RMDQ, and QBPDS have recently been validated and approved for the application in German [45].
At our institution, we preferably use the HFAQ and VAS spinal score, both approved for the use in German [32, 35]. We could demonstrate that the HFAQ as well as the VAS strongly correlate with established questionnaires (i.e. SF-36) and, thus can be recommended as suitable tools to measure functional outcome and severity of back specific symptoms in patients with traumatic fractures of the thoracolumbar spine [23].
The data of both questionnaires indicate that back-specific symptoms can occur even several years after injury independently of its severity. Working inability rates did not differ between the different treatment groups in our current study and were relatively low as compared to the findings of other study groups [39–41, 48, 53]. Overall these findings confirm that functional outcome and working ability after fractures of the thoracolumbar spine may persistently be affected.
Cost analysis
Economic evaluation has recently been introduced in spinal disorders [50]. More specifically, cost-effectiveness analyses were performed in LBP patients in order to evaluate the effectiveness of different treatment methods with regard to the patient’s QoL [6, 38]. To our knowledge, no studies have been performed on this topic in trauma patients.
In our study, we found that unstable and severe injuries of the thoracolumbar spine that require extensive combined anterior and posterior approaches are associated with long hospital stays and high treatment costs. For this evaluation, costs of surgery were calculated with rates per min for anaesthesia and trauma care specifically introduced by our department of administration. Other German study groups considered that costs of surgery would be markedly higher [26,47].
It has further to be considered that our data did not include the costs for physiotherapy, radiological examinations and treatment by other specialities. With regard to that it becomes clear that the revenues from the German DRG will not match the treatment costs of any procedure applied in our study, neither non-operative nor surgical.
Pain regulation
The individual’s ability to regulate and compensate pain seems to potentially contribute to the outcome after non-operative and surgical treatment of patients with low back pain [44]. The construct of pain regulation can be measured in those patients using a variety of psychometric questionnaires [24]. One of these is the PRQ, which is currently validated and available only in German [51]. Recently, it has been successfully applied in patients with back-related symptoms and trauma patients as well [49, 51].
The PRQ contains seven different subscales such as pain intensity and depression. Amongst these, pain competence is believed as determinant that significantly influences the patient’s ability to cope with acute and chronic pain symptoms [51]. In our study, we observed that independent of the applied treatment the patient’s pain competence was significantly better compared to LBP individuals. Thus, in contrast to LBP, patients with traumatic injuries of the thoracolumbar spine seem to be able to sufficiently cope with the pain stimulus caused by their injuries.
Predictors of outcome
Predictors of outcome are yet predominantly studied in patients undergoing a specific medical treatment for clearly defined pre-existing problems. In patients with low back pain (LBP), the identification of predictors of outcome is of major interest in order to better select those patients who would rather benefit from surgery and thus, to avoid failed back surgery.
Up to now sex, age, pre-existing receipt of disability benefits, long duration of pre-surgical back-related complaints, life style factors such as smoking representing a negative health behaviour, and low social as well as low education and working status are thought as being risk factors for a low outcome in LBP [18, 25, 43, 52, 54].
Further, a variety of psychological factors that determine the patient’s coping strategies such as hypochondriasis, hysteria, fear-avoidance, pain drawing, psychological distress, general satisfaction, etc. are being discussed as potential predictive factors in LBP [43]. In contrast to low back pain individuals, predictive factors have so far not been identified in trauma patients.
In our study, patient-specific characteristics (i.e. age, sex, working status, social status) did not seem to influence QoL and functional outcome. As psychological factors such as pain acceptance or pain depression may substantially influence pain perception in patients with chronic spinal disorders and thus influence surgical outcome [24] both parameters were addressed in our study.
We did not find any evidence that the diminished QoL observed in our patients was caused by a pathological pain regulation or other psychosocial factors indicating that results from LBP research are not transferable to patients with traumatic lesions. Thus, in contrast to low back pain disorders, pain regulation does not seem to crucially contribute to QoL in patients suffering from traumatic injuries of the thoracolumbar spine.
The data obtained from our study rather suggest, that severity of injury determines the kind of treatment and by this, prognosis and outcome regarding hospital stay, inability to work and costs. This suggestion is in line with the findings of a recent study on patients after combined or posterior stabilisation for traumatic burst fractures of the lumbar spine [36].
In a further study, Tropiano et al. reported on patients treated non-operatively after burst fractures of the thoracolumbar spine [56]. They found an increased pain intensity in those patients featuring a more severe injury with regard to traumatic kyphosis at the time of injury. This indicates that unfavourable results regarding outcome and QoL have to be expected after conservative treatment or limited surgery for more severe and unstable injuries of the thoracolumbar spine.
Conclusion
In summary, patients with traumatic injuries of the thoracolumbar spine studied in this investigation suffered from a reduced QoL compared to healthy controls. However, these results indicated only a comparably low level of discomfort. Most of the patients were rather able to return to their previous jobs even after severe and unstable injuries requiring extensive combined posterior and anterior surgery.
Overall, severity of injury determined the kind of treatment in our study and by this, prognosis and outcome. One important point is that the expenses of the surgical treatment are barely covered by the German DRG-system. Finally, we could demonstrate that the diminished QoL observed in our trauma patients can not be related to an inadequate pain regulation or other psychosocial factors, which is in sharp contrast to low back pain individuals.
References
- 1.Been HD, Poolman RW, Ubags LH. Clinical outcome and radiographic results after surgical treatment of post-traumatic thoracolumbar kyphosis following simple type A fractures. Eur Spine J. 2004;13(2):101–107. doi: 10.1007/s00586-003-0576-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Been HD, Bouma GJ. Comparison of two types of surgery for thoraco-lumbar burst fractures: combined anterior and posterior stabilisation vs. posterior instrumentation only. Acta Neurochir. 1999;141:349–357. doi: 10.1007/s007010050310. [DOI] [PubMed] [Google Scholar]
- 3.Bergner M, Bobbit RA, Carter WB, Gilson BS. The sickness impact profile: development and final revision of health status measure. Med Care. 1981;19:787–805. doi: 10.1097/00005650-198108000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Blauth M, Tscherne H, Gotzen L, Haas N. Results of different surgical procedures in the treatment of fresh injuries of the thoracic and lumbar spine. Unfallchirurg. 1987;90(6):260–273. [PubMed] [Google Scholar]
- 5.Boden SD. Outcome assessment after spinal fusion: why and how ? Orthop Clin North Am. 1998;29(4):717–728. doi: 10.1016/S0030-5898(05)70043-2. [DOI] [PubMed] [Google Scholar]
- 6.Bombardier C. Outcome assessments in the evaluation of treatment of spinal disorders: summary and general recommendations. Spine. 2000;25:3100–3103. doi: 10.1097/00007632-200012150-00003. [DOI] [PubMed] [Google Scholar]
- 7.Boucher M, Bhandari M, Kwok D. Health-related quality of life after short segment instrumentation of lumbar burst fractures. J Spinal Disord. 2001;14:417–426. doi: 10.1097/00002517-200110000-00008. [DOI] [PubMed] [Google Scholar]
- 8.Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. J Health Econ. 2002;21:271–292. doi: 10.1016/S0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- 9.Briem D, Lehmann W, Ruecker AH, Windolf J, Rueger JM, Linhart W. Factors influencing the quality of life after burst fractures of the thoracolumbar transition. Arch Orthop Trauma Surg. 2004;124:461–468. doi: 10.1007/s00402-004-0710-5. [DOI] [PubMed] [Google Scholar]
- 10.Briem D, Linhart W, Lehmann W, Bullinger M, Schoder V, Meenen NM, Windolf J, Rueger JM. Investigation of the health-related quality of life after a dorso ventral stabilization of the thoracolumbar junction. Unfallchirurg. 2003;106:625–632. doi: 10.1007/s00113-003-0627-4. [DOI] [PubMed] [Google Scholar]
- 11.Briem D, Rueger JM, Linhart W. Osseous integration of autogenous bone grafts following combined dorso-ventral instrumentation of unstable thoracolumbar spine fractures. Unfallchirurg. 2003;106:195–203. doi: 10.1007/s00113-002-0508-2. [DOI] [PubMed] [Google Scholar]
- 12.Bullinger M. German translation and psychometric testing of the SF-36 health survey: preliminary results from the IQOLA Project. International quality of life assessment. Soc Sci Med. 1995;41:1359–1366. doi: 10.1016/0277-9536(95)00115-N. [DOI] [PubMed] [Google Scholar]
- 13.Daniaux H, Wagner M, Kathrein A, Lang T. Fractures of the thoraco-lumbar junction. Conservative management. Orthopäde. 1999;28(8):682–691. doi: 10.1007/s001320050398. [DOI] [PubMed] [Google Scholar]
- 14.Dick W. The “fixateur interne” as a versatile implant for spine surgery. Spine. 1987;12(9):882–900. doi: 10.1097/00007632-198711000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Elfering A. Work-related outcome assessment instruments. Eur Spine J. 2006;15(Suppl 1):S32–S43. doi: 10.1007/s00586-005-1047-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.The EuroQol Group EuroQol—a new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy. 1990;16:199–208. doi: 10.1016/0168-8510(90)90421-9. [DOI] [PubMed] [Google Scholar]
- 17.Gatchel RJ, Mayer T, Dersh J, Robinson R, Polatin P. The association of the SF-36 health status survey with 1-year socioeconomic outcomes in a chronically disabled spinal disorder population. Spine. 1999;24:2162–2170. doi: 10.1097/00007632-199910150-00017. [DOI] [PubMed] [Google Scholar]
- 18.Glassman SD, Dimar JR, Johnson JR, Minkow R. Preoperative SF-36 responses as a predictor of reoperation following lumbar fusion. Orthopedics. 1998;21:1201–1203. doi: 10.3928/0147-7447-19981101-07. [DOI] [PubMed] [Google Scholar]
- 19.Greenough CG. Outcome assessment: recommendations for daily practice. Eur Spine J. 2006;15(Suppl 1):S118–S123. doi: 10.1007/s00586-005-1056-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grevitt M, Khazim R, Webb J, Mulholland R, Shepperd J. The short form-36 health survey questionnaire in spine surgery. J Bone Joint Surg Br. 1997;79:48–52. doi: 10.1302/0301-620X.79B1.1269. [DOI] [PubMed] [Google Scholar]
- 21.Gumppenberg S, Vieweg J, Claudi B, Harms J. Primary management of fresh injuries of the thoracic and lumbar vertebrae. Aktuelle Traumatol. 1991;21(6):265–273. [PubMed] [Google Scholar]
- 22.Haas N, Blauth M, Tscherne H. Anterior plating in thoracolumbar spine injuries. Indication, technique, and results. Spine. 1991;16(3 Suppl):S100–S111. doi: 10.1097/00007632-199103001-00015. [DOI] [PubMed] [Google Scholar]
- 23.Haase I, Schwarz A, Burger A, Kladny B. Comparison of Hannover functional ability questionnaire (FFbH) and the SF-36 subscale “Physical Functioning”. Rehabilitation. 2001;40(1):40–42. doi: 10.1055/s-2001-12127. [DOI] [PubMed] [Google Scholar]
- 24.Haefeli M, Elfering A. Pain assessment. Eur Spine J. 2006;15(Suppl 1):S17–S24. doi: 10.1007/s00586-005-1044-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hansson E, Hansson T, Jonsson T. Predictors for work ability and disability in men and women with low-back or neck problems. Eur Spine J. 2006;15(6):780–793. doi: 10.1007/s00586-004-0863-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hartwig E, Schultheiss M, Bischoff M. Flat rate reimbursement system for minimally invasive management of unstable vertebral fractures. An analysis of costs and benefits. Unfallchirurg. 2002;105(8):755–758. doi: 10.1007/s00113-002-0466-8. [DOI] [PubMed] [Google Scholar]
- 27.Hiebert R, Nordin M. Methodological aspects of outcomes research. Eur Spine J. 2006;15(Suppl 1):S4–S16. doi: 10.1007/s00586-005-1057-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hunt SM, McKenna SP, McEwen J, Williams J, Papp E. The Nottingham health profile: subjective health status and medical consultations. Soc Sci Med. 1981;15:221–229. doi: 10.1016/0271-7123(81)90005-5. [DOI] [PubMed] [Google Scholar]
- 29.Kaneda K, Taneichi H, Abumi K, Hashimoto T, Satoh S, Fujiya M. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am. 1997;79(1):69–83. doi: 10.2106/00004623-199701000-00008. [DOI] [PubMed] [Google Scholar]
- 30.Knop C, Blauth M, Bühren V, Arand M, Egbers HJ, Hax PM, Nothwang J, Oestern HJ, Pizanis A, Roth R, Weckbach A, Wentzensen A. Surgical treatment of injuries of the thoracolumbar transition-3: follow-up examination. Results of a prospective multi-center study by the “Spinal” study group of the German Society of Trauma Surgery. Unfallchirurg. 2001;104:583–600. doi: 10.1007/s001130170089. [DOI] [PubMed] [Google Scholar]
- 31.Knop C, Fabian HF, Bastian L, Blauth M. Late results of thoracolumbar fractures after posterior instrumentation and transpedicular bone grafting. Spine. 2001;26:88–99. doi: 10.1097/00007632-200101010-00016. [DOI] [PubMed] [Google Scholar]
- 32.Knop C, Oeser M, Bastian L, Lange U, Zdichavsky M, Blauth M. Development and validation of the visual analogue scale (VAS) spine score. Unfallchirurg. 2001;104:488–497. doi: 10.1007/s001130170111. [DOI] [PubMed] [Google Scholar]
- 33.Knop C, Blauth M, Bühren V, Hax PM, Kinzl L, Mutschler W, Pommer A, Ulrich C, Wagner S, Weckbach A, Wentzensen A, Wörsdorfer O. Surgical treatment of injuries of the thoracolumbar transition. 1: Epidemiology. Unfallchirurg. 1999;102(12):924–935. doi: 10.1007/s001130050507. [DOI] [PubMed] [Google Scholar]
- 34.Knop C, Blauth M, Bühren V, Hax PM, Kinzl L, Mutschler W, Pommer A, Ulrich C, Wagner S, Weckbach A, Wentzensen A, Wörsdorfer O. Surgical treatment of injuries of the thoracolumbar transition. 2: Operation and roentgenologic findings. Unfallchirurg. 2000;103(12):1032–1047. doi: 10.1007/s001130050667. [DOI] [PubMed] [Google Scholar]
- 35.Kohlmann T, Raspe H. Hannover functional questionnaire in ambulatory diagnosis of functional disability caused by backache. Rehabilitation. 1996;35(1):I–VIII. [PubMed] [Google Scholar]
- 36.Korovessis P, Baikousis A, Zacharatos S, Petsinis G, Koureas G, Iliopoulos P. Combined anterior plus posterior stabilization versus posterior short-segment instrumentation and fusion for mid-lumbar (L2-L4) burst fractures. Spine. 2006;31(8):859–868. doi: 10.1097/01.brs.0000209251.65417.16. [DOI] [PubMed] [Google Scholar]
- 37.Kossmann T, Ertel W, Platz A, Trentz O. Combined surgery for fractures of the thoraco-lumbar junction using the inlay-span method. Orthopäde. 1999;28(5):432–440. doi: 10.1007/s001320050368. [DOI] [PubMed] [Google Scholar]
- 38.Kovacs FM, Llobera J, Abraira V, Lazaro P, Pozo F, Kleinbaum D. Effectiveness and cost-effectiveness analysis of neuroreflexotherapy for subacute and chronic low back pain in routine general practice: a cluster randomized, controlled trial. Spine. 2002;27:1149–1159. doi: 10.1097/00007632-200206010-00004. [DOI] [PubMed] [Google Scholar]
- 39.Kraemer WJ, Schemitsch EH, Lever J, McBroom RJ, McKee MD, Waddell JP. Functional outcome of thoracolumbar burst fractures without neurological deficit. J Orthop Trauma. 1996;10:541–544. doi: 10.1097/00005131-199611000-00006. [DOI] [PubMed] [Google Scholar]
- 40.Krismer M, Auckenthaler T, Gruber R, Wimmer C, Sterzinger W, Ogon M. Lumbar fusion in adults-dorsal or combined ventral/dorsal approach ? Orthopäde. 1997;26(6):568–571. doi: 10.1007/s001320050125. [DOI] [PubMed] [Google Scholar]
- 41.Leferink VJ, Keizer HJ, Oosterhuis JK, Sluis CK, ten Duis HJ. Functional outcome in patients with thoracolumbar burst fractures treated with dorsal instrumentation and transpedicular cancellous bone grafting. Eur Spine J. 2003;12:261–267. doi: 10.1007/s00586-002-0518-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Leferink VJ, Zimmerman KW, Veldhuis EF, ten Vergert EM, ten Duis HJ. Thoracolumbar spinal fractures: radiological results of transpedicular fixation combined with transpedicular cancellous bone graft and posterior fusion in 183 patients. Eur Spine J. 2001;10(6):517–523. doi: 10.1007/s005860100319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mannion AF, Elfering A. Predictors of surgical outcome and their assessment. Eur Spine J. 2006;15(Suppl 1):S93–S108. doi: 10.1007/s00586-005-1045-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mercado AC, Carroll LJ, Cassidy JD, Cote P. Passive coping is a risk factor for disabling neck or low back pain. Pain. 2005;117:51–57. doi: 10.1016/j.pain.2005.05.014. [DOI] [PubMed] [Google Scholar]
- 45.Müller U, Roder C, Greenough CG. Back related outcome assessment instruments. Eur Spine J. 2006;15(Suppl 1):S25–S31. doi: 10.1007/s00586-005-1054-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Németh G. Health related quality of life outcome instruments. Eur Spine J. 2006;15(Suppl 1):S44–S51. doi: 10.1007/s00586-005-1046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pape HC, Mahlke L, Schaefer O, Krettek C. Thoughts on the economic aspects of management of severely injured patients with reference to “diagnostic related groups” (DRG). An initiative of the Specialized Committee of the German Health Care System. Unfallchirurg. 2003;106(10):869–873. doi: 10.1007/s00113-003-0671-0. [DOI] [PubMed] [Google Scholar]
- 48.Post RB, Keizer HJ, Leferink VJ, Sluis CK. Functional outcome 5 years after non-operative treatment of type A spinal fractures. Eur Spine J. 2005;15(4):472–478. doi: 10.1007/s00586-005-0887-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reinhold M, Knop C, Lange U, Bastian L, Blauth M. Non-operative treatment of thoracolumbar spinal fractures. Long-term clinical results over 16 years. Unfallchirurg. 2003;106(7):566–576. doi: 10.1007/s00113-003-0607-8. [DOI] [PubMed] [Google Scholar]
- 50.Roer N, Boos N, Tulder MW. Economic evaluations: a new avenue of outcome assessment in spinal disorders. Eur Spine J. 2006;15(Suppl 1):S109–S117. doi: 10.1007/s00586-005-1052-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schermelleh-Engel K, Moosbrugger H. Empirical validation of the “pain intensity” construct. Z Klin Psychol Psychopathol Psychother. 1991;39:369–381. [PubMed] [Google Scholar]
- 52.Schneider S, Lipinksi S, Schiltenwolf M. Occupations associated with a high risk of self-reported back pain: representative outcomes of a back pain prevalence study in the Federal Republic of Germany. Eur Spine J. 2006;15(6):821–833. doi: 10.1007/s00586-005-1015-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shen WJ, Shen YS. Nonsurgical treatment of three-column thoracolumbar junction burst fractures without neurologic deficit. Spine. 1999;24:412–415. doi: 10.1097/00007632-199902150-00024. [DOI] [PubMed] [Google Scholar]
- 54.Sjolie AN. Psychosocial correlates of low-back pain in adolescents. Eur Spine J. 2002;11:582–588. doi: 10.1007/s00586-002-0412-z. [DOI] [PubMed] [Google Scholar]
- 55.Stieglitz RD, Frommberger U, Foa EB, Berger M. Evaluation of the German version of the PTSD Symptom Scale (PSS) Psychopathology. 2001;34(3):128–133. doi: 10.1159/000049295. [DOI] [PubMed] [Google Scholar]
- 56.Tropiano P, Huang RC, Louis CA, Poitout DG, Louis RP. Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine. 2003;28(21):2459–2465. doi: 10.1097/01.BRS.0000090834.36061.DD. [DOI] [PubMed] [Google Scholar]
- 57.Verlaan JJ, Diekerhof CH, Buskens E, Tweel I, Verbout AJ, Dhert WJ, Oner FC. Surgical treatment of traumatic fractures of the thoracic and lumbar spine: a systematic review of the literature on techniques, complications, and outcome. Spine. 2004;29(7):803–814. doi: 10.1097/01.BRS.0000116990.31984.A9. [DOI] [PubMed] [Google Scholar]
- 58.Wälchli B, Heini P, Berlemann U. Loss of correction after dorsal stabilization of burst fractures of the thoracolumbar junction. The role of transpedicular spongiosa plasty. Unfallchirurg. 2001;104(8):742–747. doi: 10.1007/s001130170076. [DOI] [PubMed] [Google Scholar]
- 59.Ware J., Jr SF-36 health survey update. Spine. 2000;25:3130–3139. doi: 10.1097/00007632-200012150-00008. [DOI] [PubMed] [Google Scholar]
- 60.Ware J, Jr, Kosinski M, Keller SD. A 12-item short-form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34:220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 61.Wilke HJ, Kemmerich V, Claes LE, Arand M. Combined anteroposterior spinal fixation provides superior stabilisation to a single anterior or posterior procedure. J Bone Joint Surg Br. 2001;83(4):609–617. doi: 10.1302/0301-620X.83B4.9072. [DOI] [PubMed] [Google Scholar]
- 62.Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V, Butterman G. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003;85:773–781. doi: 10.1302/0301-620X.85B3.13849. [DOI] [PubMed] [Google Scholar]