Abstract
The botulinum neurotoxins (BoNT) are the most toxic proteins for humans and designated “Category A Select Agents.” The current vaccine against botulism is in limited supply, and there is a need to develop new vaccine strategies. A recombinant BoNT/A toxoid was produced in Clostridium botulinum that contained a double amino acid substitution, R363A Y365F (termed BoNT/ARYM). BoNT/ARYM was noncatalytic for SNAP25 and nontoxic for mice. Immunization with BoNT/ARYM protected mice from challenge at levels that were similar to chemically inactivated BoNT/A toxoid. BoNT/ARYM elicited an immune response against the light-chain and heavy-chain components of the toxin. Neutralizing anti-BoNT/ARYM sera blocked BoNT toxicity in primary cortical neurons and blocked ganglioside binding by the heavy chain. BoNT/ARYM represents a viable vaccine candidate for a holotoxoid against botulism.
The neurotoxins of Clostridium botulinum (BoNTs) are the most potent protein toxins for humans and are included in the list of “Category A Select Agents and Toxins” (16, 17, 24, 25). BoNTs comprise seven distinct neurotoxins designated A to G (BoNT/A to BoNT/G), which are differentiated serologically by specific neutralization. Polyclonal antibodies derived for a specific neurotoxin can neutralize the toxic effects of that toxin but will not cross-neutralize another toxin serotype (31).
BoNTs are produced as 150-kDa nontoxic single-chain proteins that are activated by proteolytic cleavage to a dichain molecule (16, 17, 24, 25). BoNTs comprise three functional domains, organized as an N-terminal catalytic domain (light chain [LC]), an internal translocation domain (heavy-chain translocation), and a C-terminal receptor-binding domain (heavy-chain receptor [HCR]) (20). BoNTs enter neurons via receptor-mediated endocytosis where neuronal tropism involves BoNT binding to unique host cell receptors. Fundamental studies by Chapman and coworkers demonstrated that luminal domain fragments of synaptic vesicle proteins synaptotagmin I and synaptotagmin II mediate the binding and entry of BoNT/B into cultured neuroendocrine cells (11). A similar approach demonstrated that synaptotagmin I and synaptotagmin II also mediate the binding and entry of BoNT/G, whereas isoforms of synaptic vesicle protein 2 (SV2) mediated the binding and entry of BoNT/A into cultured neurons (12, 27). Upon delivery into the cytosol, LC cleaves one or more of the neuronal SNARE proteins SNAP25, Syntaxin 1A, and Synaptobrevin 2 (16, 17, 24, 25).
The threat of bioterrorism has stimulated renewed efforts to generate vaccines and therapies against agents such as BoNTs. There are two available therapies against botulism, the human botulinum immune globulin product (BabyBIG) used in infant botulism cases against type A and B toxins and an equine-based antitoxin treatment and concurrent intubation and ventilation assistance for respiratory failure (1, 22). Immunization with chemically detoxified proteins has led to successful vaccines against several bacterial pathogens. This approach was also used for generation of the current vaccine against botulism (1, 8). However, at present, there are no licensed vaccines for preventing botulism. The U.S. Centers for Disease Control and Prevention currently distributes a pentavalent (ABCDE) toxoid under investigational new drug status to individuals at high risk of exposure (1). The vaccine is composed of formalin-inactivated crude isolates of BoNTs absorbed to aluminum phosphate and containing thimerosal as a preservative. This is a relatively impure preparation that is difficult to produce, which combined with the limited supply of this vaccine highlights the need to develop more efficient approaches for vaccine development against botulism.
There is a need to develop novel strategies for vaccine and therapies against botulism. Several studies have reported the immunogenic properties of bacterium- or yeast-derived HCRs directed against various BoNT serotypes (5, 9, 13, 21, 30, 32). The HCR component of BoNTs has several potential advantages over currently available C. botulinum-derived antigens. Production of HCR in a heterologous system facilitates large-scale production and removes the possibility of contamination with other neurotoxins and clostridial components. We recently reported the neutralizing capacities and immunogenic properties of Escherichia coli-derived HCRs directed against BoNT serotypes A and E. The immunogenic potency of the E. coli-derived HCRs demonstrated the suitability of this strategy for the development of the next generation of vaccines against botulism (5). However, recent studies demonstrated that the LC of BoNT/A alone can stimulate a protective immune response. These observations indicate the presence of neutralizing epitopes on the LC and suggest that a holotoxin-derived immunogen may constitute an optimal BoNT vaccine. Here we report the generation of a genetically engineered holotoxoid that elicits a protective immune response similar to chemically inactivated BoNT.
MATERIALS AND METHODS
Materials.
Unless otherwise stated, molecular biology-grade chemicals and reagents were obtained from Sigma-Aldrich Co. Restriction enzymes were from New England Biolabs. Bacterial culture media and components were purchased from Becton Dickinson and Thermo Fisher Scientific. Anti-SNAP25 monoclonal antibody clone MC-6053 was purchased from R&D Systems. Sprague-Dawley rat embryonic-day-18 cortices were from Brainbits LLC and handled as described by the supplier. BoNT/A was purified as described previously (23) and was below the maximum amounts excluded from regulation as defined by the Centers for Disease Control and Prevention Select Agent Program.
Construction and expression of recombinant HCR/A in E. coli.
The construction and expression of HCR/A in E. coli has been described in detail previously (5).
Construction and expression of recombinant BoNT/ARYM in C. botulinum.
In order to comply with the guidelines for research involving recombinant DNA molecules, specifically, cloning of toxin genes with a 50% lethal dose (LD50) of less than 100 ng/kg of body weight (according to National Institutes of Health guidelines), the gene for the expression of nontoxigenic BoNT/A holotoxin was constructed in several steps. First, the LC and HC regions of the neurotoxin gene were amplified by PCR in separate reactions using C. botulinum chromosomal DNA from strain ATCC 3502 as a template. Unique restriction sites for SacI (5′) and BglII (3′) were added to the LC/A gene fragment (coding for amino acid residues 1 to 450). The PCR fragment was inserted into a TA cloning vector pGEM-T (Promega), and the nucleotide sequence of the cloned fragment was verified. Next, site-directed mutagenesis was performed to introduce two mutations in the catalytic region of the LC/A, Arg362Ala and Tyr365Phe, using a QuikChange kit (Stratagene) according to the manufacturer's instructions. The HC/A gene region (coding for amino acid residues 451 to 1296) with added restriction sites for BamHI (5′) and SphI (3′) was inserted into a modified pCITE4a(+) vector (Novagen), and the HC/A nucleotide sequence was verified. The modifications of the pCITE4a(+) vector included insertion of additional restriction sites into the multicloning site and the histidine tag (C-terminal His6), followed by the stop codon. The next step was insertion of the altered LC/ARYM in front of the HC/A to form a recombinant BoNT/ARYM gene with a C-terminal His tag. During the last cloning step, six additional nucleotides were introduced in the junction site between the LC and HC regions (BglII/BamHI); thus, two additional amino acid residues, Arg and Ser, were added to the recombinant holotoxin. To remove these extra nucleotides from the junction site, the neurotoxin gene region between the Bsu361 and BstBI restriction sites (nucleotides1140 to 2317) was amplified by PCR using chromosomal DNA of C. botulinum strain ATCC 3502 as a template. The Bsu361 and BstBI fragment in the recombinant gene was then replaced with the same DNA fragment from the wild-type gene, and the nucleotide sequence of final gene construct was verified. Lastly, the recombinant BoNT/ARYM gene was inserted into a clostridial expression vector pMTL9361 (N. P. Minton, University of Nottingham, Nottingham, United Kingdom) between restriction sites SacI and NotI. The resulting plasmid, pMVP410 contained a recombinant nontoxigenic neurotoxin gene, which differs from the wild-type gene by two mutations (Arg362Ala and Tyr365Phe) in the catalytic region and a C-terminal His tag.
Introduction of the pMVP410 expression vector into nontoxigenic C. botulinum strain LNT01.
The expression vector pMVP410 was first transformed into E. coli donor strain CA434 and then transferred by conjugation to a nontoxigenic C. botulinum strain LNT01 as described previously (7).
Purification of pMVP410BoNT/ARYM.
The recombinant holotoxin (BoNT/ARYM) was purified from C. botulinum strain LNTO1 carrying expression vector pMVP410. Cultures were grown in an anaerobic chamber (ThermoForma), using an initial gas mixture comprised of 80% N2, 10% CO2, and 10% H2. Cultures were incubated at 37°C in 1 liter of TPM medium (2% casein hydrolysate [NZ Case TT], 1% yeast extract, and 0.5% glucose [pH 7.2]) supplemented with 10 mM EGTA and 50 μg of erythromycin/ml. When the culture reached an optical density at 600 nm of 0.3, toxin expression was induced by addition of 1 mM IPTG (isopropyl-β-d-thiogalactopyranoside), and then the culture was further incubated at 30°C for an additional 18 h. Bacterial cells were precipitated by centrifugation at 6,000 × g for 15 min at 4°C. The cell pellet was suspended in 50 ml of buffer (0.2 M KH2PO4, 0.2 M Na2HPO4 [pH 6.0]) and stirred gently for 2 h at room temperature, followed by centrifugation at 10,000 × g for 20 min at 20°C to clear the cell extract. BoNT/ARYM was purified from the clarified lysate using chromatography on Ni2+-nitrilotriacetic acid resin (5-ml bed volume; QIAGEN). Protein samples from the chromatography fractions were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) using a 12% NuPAGE gel (Invitrogen), followed by a semidry transfer to an Immobilon-P membrane (Millipore). A Western blot was performed using a His6-tagged monoclonal antibody (Covance) as a primary antibody and the His tag AP Western blot kit (Novagen). Protein concentrations were determined by using a BCA protein assay kit (Pierce).
Determination of BoNT/ARYM toxicity.
Recombinant BoNT/ARYM was tested for toxicity in both the single and dichain forms. The native single-chain recombinant BoNT/ARYM was converted to a dichain form by mild trypsinization in 0.1 M sodium acetate buffer (pH 6.0; 40:1 [wt/wt] BoNT/ARYM-trypsin, 37°C, 30 min). SDS-PAGE analysis of the trypsin-treateded BoNT/ARYM showed a single band of ∼150 kDa in the unreduced sample and two bands of ∼100 and ∼50 kDa in the reduced sample corresponding to the HC and LC domains, respectively. Female ICR mice (18 to 22 g) were injected intraperitoneally with up to 1 μg/mouse of either the single chain or dichain forms of the recombinant BoNT/ARYM and then monitored for 96 h, at which point survival was scored. All mice survived challenge with up to 1 μg of the single or dichain form of the recombinant BoNT/ARYM and showed no symptoms of botulinal intoxication.
Immunization of mice with recombinant HCR fragments and BoNTRYM.
Female ICR mice (18 to 22 g) were immunized intraperitoneally with either 1 or 0.1 μg of total protein (recombinant HCRs or BoNT/ARYM) in phosphate-buffered saline (PBS) mixed with an equal volume of Alhydrogel as adjuvant. Mice were vaccinated at 0, 14, and 28 days; the adjuvant was omitted for the final boost. At 7 days after the final boost, mice were challenged with the indicated amount of the native BoNT holotoxins and monitored for 96 h, at which point survival was scored.
ELISA.
Native BoNT/A was diluted to 0.5 μg/ml in coating buffer (50 mM Na2CO3 [pH 9.6]), and 100 μl was added to each well of an enhanced binding enzyme-linked immunosorbent assay (ELISA) plate (enzyme immunoassay/radioimmunoassay high binding plate; Corning) and allowed to adhere overnight at 4°C. Column 1 was incubated with coating buffer alone (no-antigen control). Plates were then washed four times with 400 μl of PBS and blocked for 1 h at 37°C with 200 μl per well of 2% (wt/vol) bovine serum albumin (BSA) in coating buffer. After a washing step as outlined above, plates were incubated for 1 h at 37°C with serial dilutions of the sera in binding buffer (1% [wt/vol] BSA in PBS, 100 μl per well). As controls, no antigen was incubated with the lowest dilution of the serum, while no primary antibody was incubated with binding buffer alone. After a washing step, plates were incubated for 1 h at 37°C with either donkey anti-mouse or donkey anti-mouse immunoglobulin G (IgG)-horseradish peroxidase (HRP) conjugate (1:12,000) in binding buffer. Plates were washed six times with 400 μl of PBS and then incubated with 100 μl per well of Ultra-TMB (tetramethyl benzidine; Pierce) as a substrate. The reaction was terminated by the addition of 100 μl of 0.2 M sulfuric acid per well, and the absorbance was read at 450 nm by using an ELISA plate reader (Victor 3V; Perkin-Elmer).
Ganglioside-binding assay.
Porcine brain gangliosides (Avanti-Polar Lipids) were dissolved in methanol and applied to high-affinity 96-well plates (0.2 μg of mixed gangliosides in 100 μl/well). The solvent was evaporated at room temperature, and wells were washed with PBS. Nonspecific binding sites were blocked by incubation for 1 h in sodium carbonate buffer (pH 9.6) supplemented with 1% (wt/vol) BSA. Binding assays were performed in binding buffer (10 mM Tris-HCl, 150 mM NaCl, 1% [wt/vol] BSA [pH 7.6]; 100 μl/well) for 1 h at room temperature containing wild-type or mutated HCR/A domains (150 nM final concentration) which had been preincubated for 30 min at 37°C with either control mouse serum or sera from mice immunized with antigens. Unbound protein was removed by three washes each with 400 μl of PBS. Bound HCR domains were detected by incubation with α-FLAG M2 monoclonal antibody-HRP for 15 min at 4°C. Ultra-TMB served as a substrate for HRP. The reaction was terminated by addition of 0.2 M H2SO4, and the absorbance at 450 nm was determined by using an ELISA plate reader (Victor 3V).
Neutralization of BoNT activity in rat cortical neurons.
Rat cortical neurons were cultured on laminin-coated glass coverslips in neurobasal medium supplemented with 2 mM glutamine, 55 μM β-mercaptoethanol, and B27 supplement for 10 to 14 days prior to use. Cells were treated with low-K+ solution (15 mM HEPES, 145 mM NaCl, 5.6 mM KCl, 2.2 mM CaCl2, 0.5 mM MgCl2, 5.6 mM glucose, 0.5 mM ascorbic acid, 0.1% BSA [pH 7.4]) or high-K+ solution (same as the control solution but adjusted to 95 mM NaCl and 56 mM KCl) for 15 min at 37°C, in the presence of 10 nM BoNT/A which had been preincubated for 30 min at 37°C with either control mouse serum or sera from mice immunized with antigens. Cells were washed with PBS and incubated for a further 48 h at 37°C in fresh neurobasal medium-conditioned neurobasal media (1:1). After treatment, cells were washed three times with PBS, fixed with 4% (wt/vol) paraformaldehyde in PBS (15 min at room temperature), permeabilized with 0.1% Triton X-100-4% formaldehyde in PBS (for 10 min at room temperature), and stained with mouse α-SNAP25-C (clone MC-6053). Staining was visualized by using goat anti-mouse IgG conjugated to Alexa Fluor 568 dye (Molecular Probes). Images were captured at room temperature by using a Nikon TE 2000 microscope equipped with a CFI Plan Apo VC 60× Oil, N.A. 1.4 type lens and a Photometrics CoolSnap EZ camera. Image acquisition and subsequent analysis was performed by using Metamorph version 7. Figures were compiled by using Photoshop CS2 (Adobe).
Cleavage of SNAP25bHA.
The endopeptidase activity of the recombinant LC proteins was assayed in a 40-μl reaction mixture containing 2 μg of GST-SNAP25b and the indicated concentrations of LC/A or LC/ARYM. After incubation for 5 min in reaction buffer A (20 mM K+-HEPES [pH 7.4]-150 mM potassium glutamate with or without 20 μM ZnCl2) at 37°C, the reactions were stopped by adding an equal volume of 2× SDS-PAGE sample buffer. The products were resolved by 10% SDS-PAGE and stained with Coomassie blue.
RESULTS
The crystal structure of LC/A containing a double mutation at Arg362 and Tyr365 was recently solved and observed to retain a three-dimensional structure that could be superimposed upon wild-type LC/A, indicating that these mutations did not perturb LC/A structure (14). Previous reports demonstrated that single mutations at Arg and Tyr did not influence substrate binding affinity but reduced the catalytic rate (6). rLC/A (residues 1 to 425) containing the double mutation R362A Y365F (hereafter referred to as LC/ARYM or BoNT/ARYM) failed to cleave human SNAP25b at all of the tested concentrations. The addition of exogenous Zn2+ to the reactions did not stimulate catalysis, a finding which is consistent with the proposed role of Arg362 and Tyr365 in facilitating the proper alignment of His222 and Glu261, respectively, for the Zn2+ coordination sphere. Thus, the lack of catalytic activity and the conservation of overall LC/ARYM structure validates BoNT/ARYM holotoxoid as a vaccine candidate.
BoNT/ARYM expression system.
Cloning and expression of BoNT/ARYM was facilitated with the use of a clostridial expression vector pMTL9361. In addition to the pCD6 replicon and erythromycin selection marker, the plasmid contained a Pfac promoter/operator and an oriT region to allow mobilization from E. coli donors. The recombinant BoNT/ARYM gene containing a C-terminal His tag was inserted into the vector, yielding the expression vector pMVP410. The BoNT/ARYM expression vector was introduced into the nontoxigenic C. botulinum strain LNT01 by conjugal transfer from E. coli donor strain CA434 as described previously (7). Plasmid pMVP410 was stably maintained in C. botulinum in the presence of erythromycin (50 μg/ml) and produced approximately 1.0 mg of BoNT/ARYM from a 1-liter batch culture that was purified by Ni2+-nitrilotriacetic acid chromatography.
Determination of BoNT/ARYM toxicity.
While mutation of Arg362 and Tyr365 resulted in a catalytically inactive LC in vitro, experiments were performed to determine residual LC/ARYM catalytic activity that could cause toxicity when introduced into the holo-BoNT. To address this concern, mice were challenged with 1 μg of purified BoNT/ARYM (∼3.3 × 104 mouse LD50) and monitored for 96 h. All mice survived challenge with 1 μg of single-chain or trypsin-nicked dichain BoNT/ARYM.
Immune protection of HCR/A, BoNT/A toxoid, or BoNT/ARYM against BoNT/A.
We demonstrated previously the efficacy of HCR/A and HCR/E as vaccine candidates against challenge with the homologous BoNT serotype (5). These observations prompted the subsequent studies that addressed the suitability of BoNT/ARYM as an alternate vaccine candidate.
Mice were immunized with either 0.1, 1, or 10 μg of HCR/A, BoNT/A toxoid, or BoNT/ARYM in aluminum hydroxide adjuvant (Alhydrogel) and challenged with either 1,000 or 10,000 mouse LD50 of BoNT/A. As reported previously, mice immunized with HCR/A were protected against subsequent challenge with BoNT/A (Table 1). Mice immunized with 1 or 10 μg of each of the three vaccines were protected against challenge by either 1,000 or 10,000 LD50 of BoNT/A, while vaccination with 0.1 μg of vaccine provided at least a partial protection against challenge with 1,000 LD50 of BoNT/A when immunized with BoNT/A toxoid or BoNT/ARYM; in one experiment mice were partially protected against challenge with 1,000 mouse LD50 of BoNT/A and completely protected in the second experiment. This indicated that 0.1 μg of these vaccines approximates a minimal protective dose at a 1,000 LD50 challenge of BoNT/A in this mouse model of intoxication.
TABLE 1.
Protection from BoNT/A intoxication by BoNT/A antigensa
| Antigen | Dose (μg of antigen) | Mouse survivalb
|
||
|---|---|---|---|---|
| Expt 1 (1,000 LD50) | Expt 2 (1,000 LD50) | Expt 3 (10,000 LD50) | ||
| Recombinant | 0.1 | 3/3 | 4/4c | NA |
| HCR/A | 1 | 3/3 | NA | 5/5 |
| 10 | 3/3 | NA | NA | |
| BoNT/ARYM | 0.1 | 2/3 | 5/5 | NA |
| 1 | 3/3 | NA | 5/5 | |
| 10 | 3/3 | NA | NA | |
| BoNT/A toxoid | 0.1 | 1/3 | 5/5 | NA |
| 1 | 3/3 | NA | 5/5 | |
| 10 | 3/3 | NA | NA | |
Mice were immunized with the indicated antigen and then challenged by the indicated amount of BoNT/A. Mice were observed for 96 h and scored for survival or death.
Each experiment is an independent replicate. Values indicate the number of mice surviving/the number of mice tested. NA, not applicable.
One mouse died of symptoms not consistent with botulinal intoxication.
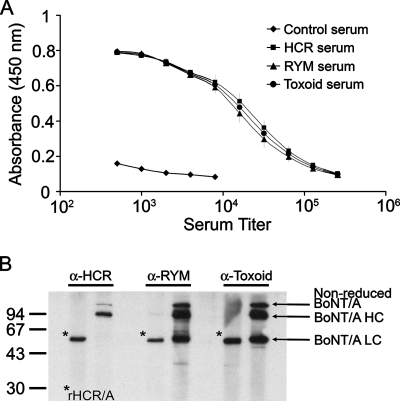
Immunoreactivity of mouse anti-HCR/A, BoNT/A toxoid, and BoNT/ARYM antibodies.
Pooled sera isolated from mice immunized with either 0.1 or 1 μg of antigens were analyzed by ELISA and Western blotting. ELISA analysis using native BoNT/A as antigen confirmed that sera of mice from three independent immunizations were immunoreactive and displayed similar titers (Fig. 1A). Sera from mice immunized with either HCR/A, BoNT/A toxoid, or BoNT/ARYM reacted against both the heavy chain of native BoNT/A and the recombinant HCR/A as determined by Western blotting (Fig. 1B). Sera from mice immunized with BoNT/A toxoid or BoNT/ARYM, but not HCR/A, also reacted with the LC of BoNT/A. This demonstrates the immunogenicity of the LC within BoNT/A toxoid or BoNT/ARYM and the specificity of the immune response to each immunogen.
FIG. 1.
Immunological characterization of mouse antisera to BoNT derivatives. (A) ELISA of mouse antisera to native BoNT/A (50 ng of toxin per well as capture antigen) was performed as described in Materials and Methods, using antisera generated against HCR/A (HCR serum, ▪), BoNT/ARYM (RYM serum, ▴) chemically inactivated BoNT/A (toxoid serum, •), or control serum (⧫). (B) Recombinant HCR/A (rHCR/A; 0.35 μg, left lanes) and BoNT/A (1 μg, right lanes) were separated by SDS-PAGE and visualized by Western blotting with mouse antisera raised against HCR/A (α-HCR), BoNT/ARYM (α-RYM), and chemically inactivated BoNT/A (α-toxoid). An asterisk indicates the position of recombinant HCR/A, and arrows indicate the positions of full-length BoNT/A (nonreduced BoNT/A), BoNT/A HC, and BoNT/A LC. The blot shown is a composite of three independent experiments with the indicated primary antisera.
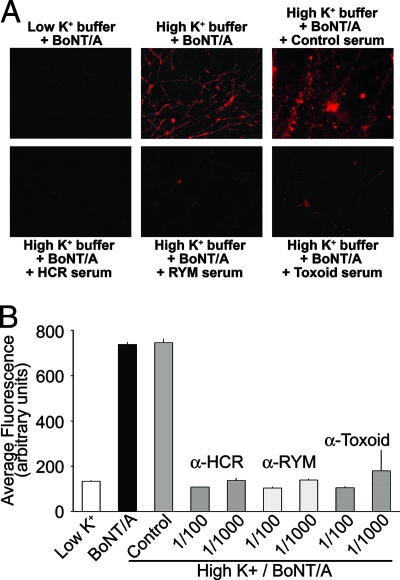
Inhibition of BoNT/A activity with antisera in cultured rat neurons.
At present, the mechanisms of serum neutralization remain largely unknown. To address this question, sera from mice resistant to BoNT intoxication were tested for the ability to neutralize BoNT/A toxicity of cortical neurons. Treatment of cortical neurons with BoNT/A alone or with BoNT/A incubated with control mouse serum resulted in cleavage of SNAP25, as visualized by staining with a monoclonal antibody that specifically recognizes only the cleaved form of SNAP25 (Fig. 2) (12). In contrast, incubation of sera from mice immunized with chemically inactivated BoNT toxoid, BoNT/ARYM, or HCR/A blocked the action of BoNT/A on the cultured neurons. The neutralizing capacity and unique serum reactivity of the mouse sera promoted subsequent studies to determine the mechanisms of antibody neutralization.
FIG. 2.
Neutralizing sera inhibit the uptake of BoNT/A into primary cortical neurons. BoNT/A (10 nM) was incubated for 30 min at 37°C in the buffer alone or in buffer with mouse antisera raised against HCR/A (α-HCR), BoNT/ARYM (α-RYM), and chemically inactivated BoNT/A (α-toxoid) at the indicated dilutions. After incubation, cortical neurons were exposed to each of the reaction mixtures for 15 min at 37°C. Cells were then rinsed and incubated for an additional 48 h at 37°C. (A) Cleavage of SNAP25 by BoNT/A was detected by using anti-SNAP25-C that recognizes the cleaved form of SNAP25. (B) SNAP25 cleavage by BoNT/A was reduced ∼80% by sera against HCR/A, BoNT/ARYM, and BoNT/A toxoid (P < 0.001 [Student t test]) but not by control serum (1/100 dilution, P > 0.05 [Student t test]).
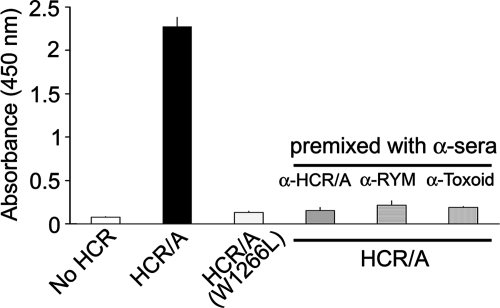
Inhibition of BoNT/A binding to mixed gangliosides by antisera.
The interaction of BoNT/A with gangliosides is well documented and is proposed as an initial step in BoNT/A intoxication of the neuromuscular junction (4). To further elucidate the mechanisms of BoNT immune serum inhibition, a solid-phase ganglioside binding assay was developed. Porcine brain gangliosides were immobilized on microtiter plates and incubated with either wild-type HCR/A or a mutated HCR/A (W1266L), which was previously shown to lack ganglioside binding (28). The amount of bound protein was quantified by using a monoclonal antibody against the N-terminal FLAG epitope of recombinant HCR/A. Wild-type HCR/A efficiently bound to porcine brain gangliosides in a dose-dependent manner, while HCR/AW1266L showed a reduction in ganglioside binding relative to wild-type HCR/A (Fig. 3). Control experiments showed that, in the absence of ganglioside coating, HCR/A binding was not detected above blank wells (data not shown). Preincubation of HCR/A with antisera against chemically inactivated BoNT toxoid, BoNT/ARYM, or HCR/A, but not control mouse sera, inhibited ganglioside binding by HCR/A (Fig. 3). Thus, serum neutralization of BoNT is mediated, at least in part, by inhibition of ganglioside binding. To our knowledge this is the first demonstration that neutralizing sera block the interaction of BoNTs with their cognate ganglioside receptors.
FIG. 3.
BoNT/A neutralizing sera block BoNT/A binding to gangliosides. HCR/A (150 nM) was incubated for 30 min at room temperature in buffer alone or in buffer with mouse antisera raised against HCR/A (HCR), BoNT/ARYM (RYM), and chemically inactivated BoNT/A (Toxoid) as indicated. After incubation, reaction mixtures were incubated with mixed gangliosides for 2 h at 4°C, and binding was determined with a FLAG-specific antibody-HRP conjugate, using Ultra-TMB as a substrate. The data represent mean values ± the standard deviation of three to four independent experiments performed in triplicate.
DISCUSSION
Effective vaccines and therapies against botulinum neurotoxins are limited. A pentavalent vaccine that protects against BoNT/A to BoNT/E and a separate monovalent vaccine that protects against BoNT serotype F are available but have several limitations including cost, efficacy, and accessibility. The use of recombinant-derived HCRs and the recombinant holotoxin-derived vaccine described here constitute BoNT vaccines that can be produced in large quantities and under low biocontainment. In the present study, the development of a recombinant catalytically inactive holotoxin based upon a previously described mutated LC/A is described. In agreement with previous observations, mutation of Arg362 and Tyr365 to alanine and phenylalanine, respectively, reduced the catalytic rate of LC/A to undetectable levels (6). The recently solved crystal structure of LC/A R362A/Y365F (hereafter referred to as LC/ARYM) revealed conservation of overall structure relative to the wild-type LC/A, further validating BoNT/ARYM as a potential vaccine candidate (5).
Recombinant BoNT/ARYM holotoxin gene was inserted into a clostridial expression vector pMTL9361, yielding pMVP410, and the recombinant holotoxin was expressed in C. botulinum strain LNT01 (7, 26). The nontoxigenic C. botulinum type A strain (LNT01) was chosen as the expression strain because it is a native host for botulinum neurotoxins and it does not produce any neurotoxin to interfere with the purification of modified BoNT derivatives. The purified holotoxin was nontoxic in vivo and did not cleave SNAP25 in vitro. Aside from the loss of toxicity, the other major difference between the recombinant and native BoNT/A toxins was that the former was not nicked. C. botulinum strain LNT01 is a transposon Tn916 mutant of 62A (18). Upon transposon insertion, this strain loses a 32.5-kb region containing the entire neurotoxin gene cluster and regions flanking the cluster (unpublished data). A gene encoding a protease responsible for the cleavage of the neurotoxin may be located within the region deleted from this strain. Our previous studies have shown that BoNT gene clusters and their flanking regions are highly homologous between 62A and the genome strain ATCC 3502. Based on descriptions of the putative open reading frames (ORFs) in the region deleted from LNT01, the most likely candidate for nicking the neurotoxin gene is an ORF (CBO0812), a putative amidohydrolase (29). This ORF is located 4 kb downstream of the toxin gene; its close proximity to the cluster suggests a possible role in toxin formation and activation. However, more studies are necessary to determine the role and functions of the CBO0812 ORF. Since the BoNT/ARYM could be readily nicked by trypsin treatment, this was not expected to have a major influence on neurotoxin properties because all serotypes of BoNTs are initially produced as single-chain polypeptides that are subsequently cleaved by proteases to yield fully active double-chain molecules. The single-chain form of serotype E is associated with human disease where gut proteases nick and activate the toxin (19).
The ability of BoNT/ARYM to stimulate protective immunity was tested after intraperitoneal injection of antigen and compared to recombinant HCR/A and formalin-inactivated BoNT/A toxoid. Mice immunized with ≥1 μg of HCR/A, BoNT/ARYM, or BoNT/A toxoid were resistant to challenge with at least 10,000 mouse LD50. The loss of protection occasionally observed when the BoNT/ARYM dose was lowered to 0.1 μg could be overcome by pretreatment of the protein with formalin (data not shown), suggesting the native antigen may be less stable than the recombinant HCR protein. Alternatively, formalin treatment may increase the immunogenicity of the antigen through cross-linking protein molecules. ELISA and Western blot analysis demonstrated the production of antibodies against native BoNT/A toxin. Sera from mice immunized with BoNT/ARYM or chemically inactivated BoNT/A toxoid—but not HCR/A—was reactive against LC/A, demonstrating both the antigenicity of LC/A and the specificity of the observed antibody response. The three immunogens stimulated a strong antibody response against HC/A, with similar titers supporting earlier observations that the HCR domain contains immunodominant epitopes (2). Moreover, antibodies to HCR/A, BoNT/ARYM, or BoNT/A toxoid were able to neutralize the activity of the toxin in a cultured neuron model (Fig. 2).
Despite the widely reported neutralizing epitopes within the HCR subunit, the role of anti-HCR antibodies in toxin neutralization remains largely unknown. Based on the longstanding double receptor model described in previous studies (3, 25), BoNT is proposed to interact initially with lipid- and/or protein-linked oligosaccharides such as ganglioside GT1b, concentrating the toxin on the presynaptic membrane. Subsequent to initial capture, calcium influx resulting from an action potential stimulates synaptic vesicle membrane fusion. This exposes synaptic protein complexes to the extracellular milieu, allowing neurotoxin binding and subsequent uptake through clathrin-mediated endocytosis. Two independent studies on the interaction of BoNT/B with its cognate protein receptor, synaptotagmin II, have provided the first physical evidence for this model (4, 10, 15).
The observation that the synaptotagmin-binding domain is adjacent to the ganglioside-binding site raises the possibility that neutralizing antibodies against the HCR domain may block one or both of the binding sites. In support of this model, antibodies to HCR/A, BoNT/ARYM, or BoNT/A toxoid were demonstrated to inhibit the interaction of HCR/A with immobilized porcine gangliosides (Fig. 3). Neutralizing BoNT/A antisera also blocked the intoxication of primary cortical neurons by BoNT/A, implicating the ability of the antisera to block the interaction of BoNT/A with receptors. However, this interpretation is complicated by the need to perform the binding component of the experiment at 37°C, since the exposure of the BoNT receptor requires synaptic vesicle fusion to the plasma membrane (12). While the interaction of SV2 with BoNT/A can occur independent of gangliosides (12), the possibility remains that inhibition of BoNT/A intoxication of primary neurons is due to steric hindrance due to the presence of antibody bound to the ganglioside-binding pocket.
We describe here the development of an expression and purification strategy for a catalytically inactive BoNT/A holotoxin. The immunogenic potency of the BoNTRYM protein we observed represents a tool that allows genetic manipulation to develop the next generation of vaccines and therapies against botulism, as well as reagents to elucidate the mechanisms of serum neutralization and the cell biology of BoNT intoxication of neurons.
Acknowledgments
This study was sponsored by the NIH/NIAID Regional Center of Excellence for Bio-defense and Emerging Infectious Diseases Research (RCE) Program. We acknowledge membership in and support from the Region V “Great Lakes” RCE (NIH award 1-U54-AI-057153).
We thank Nigel Minton (University of Nottingham, Nottingham, United Kingdom) for providing clostridial expression vector pMTL9361 and the E. coli donor strain CA434. The assistance of Amanda Hill at the Medical College of Wisconsin in the preparation of HCR/A is also acknowledged.
Editor: V. J. DiRita
Footnotes
Published ahead of print on 29 October 2007.
REFERENCES
- 1.Arnon, S. S., R. Schechter, T. V. Inglesby, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, J. Hauer, M. Layton, S. Lillibridge, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, D. L. Swerdlow, and K. Tonat. 2001. Botulinum toxin as a biological weapon: medical and public health management. JAMA 2851059-1070. [DOI] [PubMed] [Google Scholar]
- 2.Atassi, M. Z. 2004. Basic immunological aspects of botulinum toxin therapy. Mov. Disord. 19(Suppl. 8)S68-S84. [DOI] [PubMed] [Google Scholar]
- 3.Baldwin, M. R., and J. T. Barbieri. 2007. Association of botulinum neurotoxin serotypes a and B with synaptic vesicle protein complexes. Biochemistry 463200-3210. [DOI] [PubMed] [Google Scholar]
- 4.Baldwin, M. R., J. J. Kim, and J. T. Barbieri. 2007. Botulinum neurotoxin B-host receptor recognition: it takes two receptors to tango. Nat. Struct. Mol. Biol. 149-10. [DOI] [PubMed] [Google Scholar]
- 5.Baldwin, M. R., W. H. Tepp, C. L. Pier, M. Bradshaw, M. Ho, B. A. Wilson, R. B. Fritz, E. A. Johnson, and J. T. Barbieri. 2005. Characterization of the antibody response to the receptor binding domain of botulinum neurotoxin serotypes A and E. Infect. Immun. 736998-7005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Binz, T., S. Bade, A. Rummel, A. Kollewe, and J. Alves. 2002. Arg(362) and Tyr(365) of the botulinum neurotoxin type a light chain are involved in transition state stabilization. Biochemistry 411717-1723. [DOI] [PubMed] [Google Scholar]
- 7.Bradshaw, M., M. C. Goodnough, and E. A. Johnson. 1998. Conjugative transfer of the Escherichia coli-Clostridium perfringens shuttle vector pJIR1457 to Clostridium botulinum type A strains. Plasmid 40233-237. [DOI] [PubMed] [Google Scholar]
- 8.Byrne, M. P., and L. A. Smith. 2000. Development of vaccines for prevention of botulism. Biochimie 82955-966. [DOI] [PubMed] [Google Scholar]
- 9.Byrne, M. P., R. W. Titball, J. Holley, and L. A. Smith. 2000. Fermentation, purification, and efficacy of a recombinant vaccine candidate against botulinum neurotoxin type F from Pichia pastoris. Protein Expr. Purif. 18327-337. [DOI] [PubMed] [Google Scholar]
- 10.Chai, Q., J. W. Arndt, M. Dong, W. H. Tepp, E. A. Johnson, E. R. Chapman, and R. C. Stevens. 2006. Structural basis of cell surface receptor recognition by botulinum neurotoxin B. Nature 4441096-1100. [DOI] [PubMed] [Google Scholar]
- 11.Dong, M., D. A. Richards, M. C. Goodnough, W. H. Tepp, E. A. Johnson, and E. R. Chapman. 2003. Synaptotagmins I and II mediate entry of botulinum neurotoxin B into cells. J. Cell Biol. 1621293-1303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dong, M., F. Yeh, W. H. Tepp, C. Dean, E. A. Johnson, R. Janz, and E. R. Chapman. 2006. SV2 is the protein receptor for botulinum neurotoxin A. Science 312592-596. [DOI] [PubMed] [Google Scholar]
- 13.Dux, M. P., R. Barent, J. Sinha, M. Gouthro, T. Swanson, A. Barthuli, M. Inan, J. T. Ross, L. A. Smith, T. J. Smith, R. Webb, B. Loveless, I. Henderson, and M. M. Meagher. 2006. Purification and scale-up of a recombinant heavy chain fragment C of botulinum neurotoxin serotype E in Pichia pastoris GS115. Protein Expr. Purif. 45359-367. [DOI] [PubMed] [Google Scholar]
- 14.Fu, Z., S. Chen, M. R. Baldwin, G. E. Boldt, A. Crawford, K. D. Janda, J. T. Barbieri, and J. J. Kim. 2006. Light chain of botulinum neurotoxin serotype A: structural resolution of a catalytic intermediate. Biochemistry 458903-8911. [DOI] [PubMed] [Google Scholar]
- 15.Jin, R., A. Rummel, T. Binz, and A. T. Brunger. 2006. Botulinum neurotoxin B recognizes its protein receptor with high affinity and specificity. Nature 4441092-1095. [DOI] [PubMed] [Google Scholar]
- 16.Johnson, E. A. 1999. Clostridial toxins as therapeutic agents: benefits of nature's most toxic proteins. Annu. Rev. Microbiol. 53551-575. [DOI] [PubMed] [Google Scholar]
- 17.Johnson, E. A., and M. Bradshaw. 2001. Clostridium botulinum and its neurotoxins: a metabolic and cellular perspective. Toxicon 391703-1722. [DOI] [PubMed] [Google Scholar]
- 18.Johnson, E. A., W. J. Lin, Y. T. Zhou, and M. Bradshaw. 1997. Characterization of neurotoxin mutants in Clostridium botulinum type A. Clin. Infect. Dis. 25(Suppl. 2)S168-S170. [DOI] [PubMed] [Google Scholar]
- 19.Kiyatkin, N., A. B. Maksymowych, and L. L. Simpson. 1997. Induction of an immune response by oral administration of recombinant botulinum toxin. Infect. Immun. 654586-4591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lacy, D. B., W. Tepp, A. C. Cohen, B. R. DasGupta, and R. C. Stevens. 1998. Crystal structure of botulinum neurotoxin type A and implications for toxicity. Nat. Struct. Biol. 5898-902. [DOI] [PubMed] [Google Scholar]
- 21.Lee, J. S., P. Pushko, M. D. Parker, M. T. Dertzbaugh, L. A. Smith, and J. F. Smith. 2001. Candidate vaccine against botulinum neurotoxin serotype A derived from a Venezuelan equine encephalitis virus vector system. Infect. Immun. 695709-5715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Long, S. S. 2007. Infant botulism and treatment with BIG-IV (BabyBIG). Pediatr. Infect. Dis. J. 26261-262. [DOI] [PubMed] [Google Scholar]
- 23.Malizio, C. J., M. C. Goodnough, and E. A. Johnson. 2000. Purification of Clostridium botulinum type A neurotoxin. Methods Mol. Biol. 14527-39. [DOI] [PubMed] [Google Scholar]
- 24.Montecucco, C. 1995. Clostridial neurotoxins: the molecular pathogenesis of tetanus and botulism. Springer-Verlag, Berlin, Germany.
- 25.Montecucco, C., O. Rossetto, and G. Schiavo. 2004. Presynaptic receptor arrays for clostridial neurotoxins. Trends Microbiol. 12442-446. [DOI] [PubMed] [Google Scholar]
- 26.Purdy, D., T. A. O'Keeffe, M. Elmore, M. Herbert, A. McLeod, M. Bokori-Brown, A. Ostrowski, and N. P. Minton. 2002. Conjugative transfer of clostridial shuttle vectors from Escherichia coli to Clostridium difficile through circumvention of the restriction barrier. Mol. Microbiol. 46439-452. [DOI] [PubMed] [Google Scholar]
- 27.Rummel, A., T. Karnath, T. Henke, H. Bigalke, and T. Binz. 2004. Synaptotagmins I and II act as nerve cell receptors for botulinum neurotoxin G. J. Biol. Chem. 27930865-30870. [DOI] [PubMed] [Google Scholar]
- 28.Rummel, A., S. Mahrhold, H. Bigalke, and T. Binz. 2004. The HCC-domain of botulinum neurotoxins A and B exhibits a singular ganglioside binding site displaying serotype specific carbohydrate interaction. Mol. Microbiol. 51631-643. [DOI] [PubMed] [Google Scholar]
- 29.Sebaihia, M., M. W. Peck, N. P. Minton, N. R. Thomson, M. T. Holden, W. J. Mitchell, A. T. Carter, S. D. Bentley, D. R. Mason, L. Crossman, C. J. Paul, A. Ivens, M. H. Wells-Bennik, I. J. Davis, A. M. Cerdeno-Tarraga, C. Churcher, M. A. Quail, T. Chillingworth, T. Feltwell, A. Fraser, I. Goodhead, Z. Hance, K. Jagels, N. Larke, M. Maddison, S. Moule, K. Mungall, H. Norbertczak, E. Rabbinowitsch, M. Sanders, M. Simmonds, B. White, S. Whithead, and J. Parkhill. 2007. Genome sequence of a proteolytic (group I) Clostridium botulinum strain Hall A and comparative analysis of the clostridial genomes. Genome Res. 171082-1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith, L. A. 1998. Development of recombinant vaccines for botulinum neurotoxin. Toxicon 361539-1548. [DOI] [PubMed] [Google Scholar]
- 31.Smith, T. J., J. Lou, I. N. Geren, C. M. Forsyth, R. Tsai, S. L. Laporte, W. H. Tepp, M. Bradshaw, E. A. Johnson, L. A. Smith, and J. D. Marks. 2005. Sequence variation within botulinum neurotoxin serotypes impacts antibody binding and neutralization. Infect. Immun. 735450-5457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang, W., M. A. Bevins, B. A. Plantz, L. A. Smith, and M. M. Meagher. 2000. Modeling Pichia pastoris growth on methanol and optimizing the production of a recombinant protein, the heavy-chain fragment C of botulinum neurotoxin, serotype A. Biotechnol. Bioeng. 701-8. [DOI] [PubMed] [Google Scholar]