Abstract
In recent years, the increasing number of donors from different regions of the world is providing a new challenge for the management and selection of suitable donors. This is a worldwide problem in most countries with transplantation programs, especially due to the increase in immigration and international travel. This paper elaborates recommendations regarding the selection criteria for donors from foreign countries who could potentially transmit tropical or geographically restricted infections to solid-organ transplant recipients. For this purpose, an extensive review of the medical literature focusing on viral, fungal, and parasitic infections that could be transmitted during transplantation from donors who have lived or traveled in countries where these infections are endemic has been performed, with special emphasis on tropical and imported infections. The review also includes cases described in the literature as well as risks of transmission during transplantation, microbiological tests available, and recommendations for each infection. A table listing different infectious agents with their geographic distributions and specific recommendations is included.
INTRODUCTION
We are living in an increasingly globalized world in which people have a greater capacity for travel than at any previous time in history. Massive tourist movements, international migration, and increases in world commercial exchanges act as important underlying factors for the emergence and reemergence of specific infectious diseases. The American Centers for Disease Control and Prevention (CDC) have targeted diseases affecting travelers, immigrants, and refugees for the prevention of emerging infectious diseases in the near future (62).
According to the United Nations World Tourism Organization, during 2005, international tourist arrivals worldwide beat all expectations, exceeding 800 million and achieving an all-time record, representing an increase of 42 million compared with previous years. Current predictions for the year 2020 suggest that these figures will reach 1.56 billion. At present, the increase in tourism is most marked in East Asia, the Pacific, South Asia, the Middle East, and Africa, with rates of increase of over 5% per year, compared to the world average of 4.1%. Among the 40 countries in the world that receive the most travelers per year, there are at least 10 countries in tropical and subtropical areas, where the risk of contracting a tropical infection is high (374).
Migration is considered to be one of the defining global issues of the early 21st century. The International Organization for Migration (189) estimated the migrant population worldwide to be 191 million in the year 2005, representing around 3% of the world's population. Between 1965 and 1990, the number of international migrants increased by 45 million, an annual growth rate of about 2.1%. The current annual growth rate is about 2.9%. There are 56.1 million immigrants in Europe (including Russia), 49.9 million in Asia, and 40.8 million in North America; the three countries hosting the largest numbers of international migrants in 2000 were the United States (35.0 million), the Russian Federation (13.0 million), and Germany (7.3 million). There are countries that traditionally have taken in large numbers of immigrants, such as Canada, the United States, and Australia, but nowadays, there are other new countries of destination such as Ireland, Italy, Norway, Portugal, and Spain. The developed world has already entered an era of labor shortage: in Europe alone, the workforce is expected to decline by another 20 million by the year 2030, and there are similar forecasts for other developed regions including countries like Japan, South Korea, and the Russian Federation. The future global work force will be drawn largely from developing countries where tropical infections may be present.
Tropical and Geographically Restricted Infectious Diseases and Organ Transplantation
Even though immigrants and travelers may import a wide variety of tropical pathogens, the possibility of dissemination in the Western community is small, as environmental conditions, intermediate hosts, and the specific vectors required are absent. The majority of imported parasitic tropical infections tend to disappear after 3 to 5 years, but some, such as strongyloidiasis and Chagas’ disease, may persist for decades. Nonparasitic diseases may also manifest many years after infection, as is the case for histoplasmosis and human T-cell lymphotropic virus type 1 (HTLV-1) infection.
As a consequence of immunosuppression, microorganisms may become opportunistic, commensals may become pathogens, poorly pathogenic organisms may behave aggressively or in an aberrant fashion, and patients may respond poorly to treatment. As well as possible transmission via blood products, organ transplant recipients may acquire significant tropical diseases in four ways: transmission with the graft (e.g., HTLV-1), de novo infection (e.g., visceral leishmaniasis), reactivation of dormant infection (e.g., histoplasmosis), and reinfection/reactivation in a healthy graft (e.g., Chagas’ disease).
The current situation in Spain may illustrate what may occur in other countries in the near future. In recent years, Spain has received a large unexpected influx of immigrants. Of the 44 million inhabitants in Spain, approximately 4 million are of foreign origin (around 9%), and these figures increase to up to 12% in main cities such as Madrid and Barcelona. Out of approximately 1,500 transplants performed in Spain during the year 2006, 10% were from foreign donors (up to 19% in the main cities), and the percentage of foreign recipients was 3% (up to 9% in the main cities). Nearly 40% of foreign donors and recipients were of Latin American origin, originating from countries where the transmission of Chagas’ disease, among others, may occur. This led to changes in the criteria for donor selection regarding possible transmission of infections (set by the Spanish National Organization for Transplantation). Screening of blood and organ donors with epidemiological risk factors for Chagas’ disease is now mandatory according to Spanish law.
Commercial transplantation is another emerging phenomenon. In Western countries, economic compensation for donation is prohibited. However, patients with end-stage organ disease and without a suitable donor may choose to acquire organs such as kidneys from live donors or even livers from executed prisoners from other countries. Once again, the issue of imported/tropical infections complicating the transplantation process may be raised.
Several guidelines for pretransplant screening have been published recently, including a consensus conference on the immunocompromised patient, the American Society for Transplantation clinical practice guidelines on the evaluation of renal transplant candidates, and the American Society of Transplant Physicians clinical practice guidelines on the evaluation of living renal transplant donors (6, 201). In addition, the CDC, the Infectious Disease Society of America, and the American Society for Blood and Marrow Transplantation have published guidelines for the prevention of infection in hematopoietic transplant recipients (63). A concise review of parasitic infections in transplant patients has also been published (20). All these guidelines include a wide range of the most important infectious agents related to transplantation and the implications for transmission and reactivation. However, these recommendations could be insufficient with respect to specific geographic/endemic agents. In recent years, the role of these microorganisms has increased as a consequence of travel and migration of populations, and these factors should also be considered when both donors and recipients are assessed.
Health professionals working in the field of transplantation will become increasingly involved in the management of donors and recipients from tropical and other geographic areas where certain infections are endemic. Protocols that include screening for these pathogens in the donor may prevent transmission during transplantation. Early identification of infection in the recipient and prompt notification of the other transplant centers involved could prevent complications for other recipients in the case of multiorgan donation.
VIRAL INFECTIONS
Infections Caused by HTLV-1/2
HTLV-1 is a double-stranded, enveloped RNA virus (family Retroviridae, subfamily Oncovirus), which belongs to a group of retroviruses known as the leukemia/lymphoma T-cell viruses of primates. HTLV-1 has a global homology of 65% with HTLV-2. It is a virus that exhibits T-cell tropism, causes the proliferation of T cells, and has a tendency to produce persistent infection. HTLV-1 and -2 infections are lifelong infections (232).
HTLV-1 has been implicated in the pathogenesis of adult T-cell lymphoma/leukemia (ATL) and a progressive neurological disease known as tropical spastic paraparesis (TSP) or HTLV-1-associated myelopathy (HAM). In the general population, the time from infection to the appearance of disease may be prolonged, an estimated mean of 20 years, and the risks for patients of developing one of these two illnesses at some point during their lives are 2 to 5% for ATL (263) and 1 to 2% for TSP (239, 299, 304).
Illnesses.
(i) ATL.
ATL is a non-Hodgkin's mature T-cell lymphoma that has an initial leukemic phase. The disease develops after a long incubation period. ATL occurs mostly in adults at least 20 to 30 years after infection with HTLV-1. The acute form of ATL comprises 55 to 75% of all ATL cases (155, 408, 409). The distribution of the various subtypes varies geographically. The median survival for patients with the acute subtype is less than a year.
(ii) TSP.
TSP, designated HAM/TSP by a WHO working group, is characterized by a slowly progressive spastic paraparesis due to white matter degeneration and fibrosis of the thoracic spinal cord (191, 192). HAM/TSP typically develops in up to 4% of HTLV-1-infected patients (273). The majority of individuals are diagnosed in the fourth or fifth decade of life.
In contrast with HTLV-1, there is no definite association between HTLV-2 and any human disease. Isolated cases of TSP-like illness, mycosis fungoides, and lymphocytic leukemia have been reported in patients with HTLV-2 infection (315-317, 422).
Geographic distribution.
Although the exact number of HTLV-1-seropositive individuals in the world is not known, it is estimated that up to 15 to 20 million people may be infected (102). The seroprevalence rates differ according to the geographic area, the sociodemographic characteristics of the population studied, and individual risk behaviors (Table 1 and Fig. 1).
TABLE 1.
Geographic distribution of infectious agents
| Geographic area | Countries affected | Infectious agents/diseases |
|---|---|---|
| North Africa | Algeria, Egypt, Libya, Morocco, Tunisia | WNV, rabies virus, malaria (very low risk), Leishmania spp., Entamoeba histolytica, Schistosoma spp. (Nile delta), Echinococcus granulosus, lymphatic filariasis (Nile delta), Taenia solium (cysticercosis) |
| West, Central, and East Africa | Angola, Benin, Burkina Faso, Burundi, Cameroon, Cape Verde Islands, Central African Republic, Chad, Congo, Democratic Republic of Congo (Zaire), Djibouti, Equatorial Guinea, Eritrea, Ethiopia, Gabon, Gambia, Ghana, Guinea, Guinea-Bissau, Ivory Coast, Kenya, Liberia, Madagascar, Malawi, Mali, Mauritania, Mozambique Niger, Nigeria, Reunion Islands (France), Rwanda, Senegal, Seychelles, Sierra Leone, Somalia, Sudan Togo, Sao Tome and Principe, Tanzania, Uganda, Western Sahara, Zambia | HTLV-1 (in certain countries), WNV, rabies virus, Histoplasma spp., malaria, Trypanosoma brucei, filariasis, Leishmania spp., Entamoeba histolytica, Echinococcus granulosus, Schistosoma spp., Strongyloides spp., Taenia solium (cysticercosis) |
| South Africa | Botswana, Lesotho, Namibia, South Africa, Swaziland, Zimbabwe | WNV, rabies virus, Histoplasma spp., malaria, Trypanosoma brucei, Entamoeba histolytica, Schistosoma spp. |
| North America | Canada, United States (including Hawaii) | WNV, rabies virus, Coccidioides immitis, Histoplasma spp., Blastomyces spp., Strongyloides spp., Echinococcus multilocularis, Babesia spp. |
| Central America and Mexico | Belize, Costa Rica, El Salvador, Guatemala, Honduras, Mexico, Nicaragua, Panama | WNV, rabies virus Coccidioides immitis, Histoplasma spp. Paracoccidioides spp., malaria (mainly P. vivax but risk of P. falciparum in Panama), Leishmania spp., Entamoeba histolytica, Trypanosoma cruzi, Strongyloides spp., Taenia solium (cysticercosis) |
| Caribbean | Antigua and Barbuda, Anguilla (United Kingdom), Aruba, Bahamas, Barbados, Bermuda (United Kingdom), Cayman Islands (United Kingdom), Cuba, Dominica, Dominican Republic, Grenada, Guadeloupe (including St. Barthelemy and St. Martin), Haiti, Jamaica, Martinique (France), Montserrat (United Kingdom), The Netherlands Antilles (Bonaire, Curaçao, Saba, St. Eustatius, St. Maarten), Puerto Rico (United States), St. Vincent and the Grenadines, St. Kitts and Nevis, St. Lucia, Trinidad and Tobago, Virgin Islands (United Kingdom), Virgin Islands (United States) | HTLV-1, Histoplasma spp., malaria (Plasmodium falciparum in Haiti and Dominican Republic, isolated cases in Jamaica), lymphatic filariasis (Haiti and Dominican Republic), cutaneous leishmaniasis (Dominican Republic), Schistosoma spp. |
| South America | Argentina, Bolivia, Brazil, Chile, Colombia, Ecuador, Guyana, French Guiana, Paraguay, Peru, Suriname, Uruguay, Venezuela | HTLV-1, rabies virus, Histoplasma spp., Coccidioides immitis, Paracoccidioides spp., malaria (in certain countries), visceral and mucocutaneous leishmaniasis, Trypanosoma cruzi, Entamoeba histolytica, lymphatic filariasis (in certain countries), Strongyloides spp., Taenia solium (cysticercosis), Echinococcus granulosus/Echinococcus multilocularis, Schistosoma spp. |
| Western Europe | Andorra, Austria, Belgium, Denmark, Finland, France, Germany, Greece, Iceland, Ireland, Italy, Liechtenstein, Luxembourg, Malta, Monaco, The Netherlands, Norway, Portugal, San Marino, Spain, Sweden, Switzerland, United Kingdom | Rabies virus, Histoplasma spp. (Mediterranean basin), Blastomyces spp. (Mediterranean basin), visceral and cutaneous leishmaniasis (Mediterranean basin), Echinococcus granulosus, Babesia spp. |
| Eastern Europe and Russia | Albania, Armenia, Azerbaijan, Belarus, Bosnia-Herzegovina, Bulgaria, Croatia, Czech Republic, Estonia, Georgia, Hungary, Kazakhstan, Kyrgyzstan, Latvia, Lithuania, Moldova, Montenegro, Poland, Slovakia, Slovenia, Rumania, Russia, Serbia, Tajikistan, Turkmenistan, Ukraine, Uzbekistan | WNV, rabies virus, malaria (in certain countries) Leishmania spp., Echinococcus granulosus/Echinococcus multilocularis |
| Middle East | Bahrain, Cyprus, Iraq, Iran, Israel, Jordan, Kuwait, Lebanon, Oman, Qatar, Saudi Arabia, Syria, Turkey, United Arab Emirates, Yemen | HTLV (in localized areas of Iran), WNV, rabies virus, malaria (in certain countries), visceral and cutaneous leishmaniasis, filariasis (Yemen), Echinococcus granulosus, Schistosoma spp. (in certain countries) |
| East Asia | China (including Hong Kong and Macau), Japan, Mongolia, North Korea, South Korea, Taiwan | HTLV-1, WNV, rabies virus, Penicillium marneffei, malaria (in certain countries), visceral and cutaneous leishmaniasis, Echinococcus granulosus/Echinococcus multilocularis, Schistosoma spp., Strongyloides spp. |
| Indian subcontinent | Afghanistan, Bangladesh, Bhutan, India, Maldives, Nepal, Pakistan, Sri Lanka | Rabies virus, malaria, visceral and cutaneous leishmaniasis, lymphatic filariasis, Entamoeba histolytica, Taenia solium (cysticercosis), Echinococcus granulosus, Schistosoma spp. |
| Southeast Asia | Brunei, Burma (Myanmar), Cambodia, East Timor, Indonesia, Laos, Malaysia, Philippines, Singapore, Thailand, Vietnam | Rabies virus, Penicillium marneffei, malaria, lymphatic filariasis, Entamoeba histolytica, Taenia solium (cysticercosis), Schistosoma spp., Strongyloides spp. |
| Oceania (Pacific area) | Australia, Fiji, French Polynesia, Kiribati, Marshall Islands, Micronesia (including Guam [United States] and Northern Mariana Islands), Nauru, Niue (New Zealand), New Caledonia (France), New Zealand, Palau, Papua New Guinea, Samoa, Solomon Islands, Tokelau (New Zealand), Tonga, Tuvalu, Vanuatu, Wallis | HTLV-1, malaria (in certain countries), lymphatic filariasis, Entamoeba histolytica, Strongyloides spp., Echinococcus granulosus |
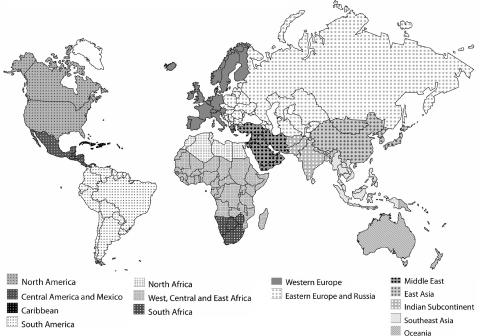
FIG. 1.
World map with geographic distribution (used for Table 1). Note that this map shows a geographic distribution of pathogens as used in Table 1 and does not represent a political distribution.
Relatively high HTLV-1 seroprevalence rates in the general population and in specific groups of individuals such as pregnant women and/or blood donor candidates are found in southwestern Japan (up to 10%) (262, 407), in several countries in the Caribbean area including Jamaica and Trinidad (up to 6%) (155), in several sub-Saharan Africa countries (up to 5%) (8, 110, 133, 324), and in localized areas of Iran and Melanesia (less than 5%) (239, 261, 299).
The seroprevalence rate for low-risk patients in Europe and the United States is <1%. In areas where the disease is not endemic, such as Europe and North America, HTLV-1 infection is found mainly in immigrants, their offspring and sexual contacts, sex workers, and intravenous drug users (IVDU). Among blood donors in North America and Europe, the seroprevalence is very low, ranging from 0.01 to 0.03% in the United States and Canada (80, 264, 399) to 0.002% in Norway (350) and 0.0056% in Greece (370).
HTLV-2 has been described mainly in IVDU and their sexual contacts as well as in populations of native Amerindians. The infection has been found to be endemic in IVDU populations of the United States, Europe, South America (Brazil), and Southeast Asia (Vietnam) (115, 163, 298, 299).
Diagnostic methods.
Following HTLV-1 infection, there is an incubation period of 30 to 90 days prior to seroconversion. HTLV antibody detection is mainly used for diagnosis. Following seroconversion, antibodies persist for life. The serological responses to HTLV-1 and -2 are similar, and specialized tests are needed to differentiate between the two viruses.
The most commonly used serological tests are the enzymatic immunoassays (EIA) prepared with the lysed antigens of the intact HTLV-1 virus. The sensitivities of these methods vary, so samples that test positive initially are retested in order to decrease technical errors. Samples that test positive on two occasions are considered to be reactive. If the sample is reactive using one test only, it is deemed nonreactive. Methods based on immunofluorescent antibodies tests (IFATs) do not distinguish between specific HTLV-1 and -2 antibodies and gene products.
There are additional tests based on Western blot (WB) or radioimmunoprecipitation techniques that facilitate the correct interpretation of reactive samples. These tests can identify antibodies against core (gag) and envelope (env) proteins of HTLV-1 and -2. In order to consider a result a true positive, specimens that are repeatedly reactive using enzyme-linked immunosorbent assay (ELISA) must show immunoreactivity for the gag gene products (p24) and envelope products (gp46 and/or gp61/gp68). WB is the most sensitive confirmatory assay for the detection of antibodies against the gag gene proteins p19, p24, and p28, whereas radioimmunoprecipitation assay-based techniques are more sensitive for the detection of antibodies against glycoproteins gp46 and gp61/gp68. Serum samples that do not meet these criteria but that have immunoreactivity towards at least one of the HTLV gene products (only p19, p19 and p28, or p19 and Env) should be considered to be indeterminate. Serum samples with no immunoreactivity towards HTLV-1 gene products should be considered to be negative (77).
False-positive HTLV-1 EIA results (with negative confirmatory WB results) may be caused by many factors such as the prior use of influenza virus vaccine, some bacterial infections, autoimmune disorders, and multiple pregnancies (61, 74, 235). The majority of nonspecific EIA reactions (59%) are caused by reactivity to HTLV envelope glycoprotein gp21 (230).
PCR nucleic acid sequence-based amplification testing (NAT) or transcription-mediated amplification-based studies could potentially be more specific in identifying false-positive donors. However, currently, there is no commercially available NAT with a turnaround time that would be short enough to solve the problem of donors who are HTLV reactive by EIA. A potential solution would be the development of a commercial NAT multiplex assay that could simultaneously detect hepatitis B and C viruses, human immunodeficiency virus (HIV), and HTLV (421).
Routes of transmission.
HTLV-1 can be transmitted through sexual contact and infected blood products, vertically from mother to child, and during transplantation.
Intravenous exposure to blood seems to be the most efficient mode of HTLV-1 transmission. High risk is associated with the transfusion of infected products containing various types of blood cells (packed red cells, whole blood, and platelets) compared to plasma products (240). Cold storage of blood lowers the risk of transmission, presumably due to the death of HTLV-1-infected lymphocytes (106). The risk of seroconversion after transfusion of HTLV-1-contaminated blood products ranges from 40 to 60%, with a time interval before seroconversion of 51 to 65 days after transfusion (240, 271).
Sharing of contaminated needles and syringes by IVDU is another important mode of transmission of HTLV-1 and -2 (115, 205).
Several cases of transmission through organ and bone marrow transplantation have also been described (121, 140, 194, 252, 307, 366). Most cases have occurred in renal transplant patients. In certain cases, the exact route of transmission was difficult to establish, as patients had undergone hemodialysis and lived in areas of endemicity in which seroprevalence was high. In Japan, the proportion of renal transplant patients who are HTLV-1 carriers has been estimated to be around 12%, compared with only 1.2% of the general population (188, 406, 409). The transmission in some of the cases may have been through an infected blood transfusion, as screening of blood was not compulsory in Japan before 1989.
Transplant-related cases.
Factors that determine risk of infection with HTLV-1/2 in transplant recipients are as follows (413).
(i) Seroprevalence.
In U.S. blood donors, the seroprevalence of HTLV-1 has been determined to be between 0.035 to 0.046%. Surveys of HTLV seroprevalence among blood and tissue donors may not, however, be representative of the seroprevalence among organ donors. Based on the United Network for Organ Sharing data from 1988 to 2000, Shames et al. (335a) reported that the prevalence of HTLV-1 infection in organ donors was 0.027% and that the prevalence of HTLV-2 was 0.064%. However, in another report, Nowicki et al. (269) presented data accumulated during testing of all prospective 1,408 cadaveric organ donors between 2002 and 2003: there were 1.56% donors that were repeatedly reactive by HTLV-1/2 EIA (40% were African American, 20% were Hispanic, and 40% were Caucasian). Approximately 29% of EIA-reactive samples from donors were not confirmed by WB, and another 35% had indeterminate results. Most of the confirmed anti-HTLV-positive donors were positive for HTLV-2-specific antibodies.
Many studies suggest that cases of HTLV in countries with a low seroprevalence are restricted to patients originating from areas of endemicity (HTLV-1), IVDU, and commercial sex workers (HTLV-2). In Spain, a national survey in which 1,298 organ transplant donors and 493 potential recipients were tested for anti-HTLV antibodies was conducted. Of these individuals, none were found to be seropositive for HTLV-1. Only one recipient, a former IVDU, was found to be infected with HTLV-2. In a different survey, HTLV screening of 1,079 immigrants was conducted, and 0.5% were found to be asymptomatic HTLV-1 carriers. All carriers came from areas where HTLV-1 is endemic. No cases of HTLV-2 infection were found among immigrants (365).
(ii) Type of organ transplanted, exposure to blood transfusions, and viral characteristics.
Transmission occurs through infected cell products: the risk increases in correlation with the number of leukocytes that are present and decreases with prolonged preservation time.
The mechanisms by which the virus causes disease remain unclear, but a combination of environmental, host, and viral factors may all play a role. Morbidity has been linked to the presence of proviral DNA load and may vary depending on different strains of the virus. The duration of the latency period remains unknown but may be decreased in transplant patients, possibly due to the greater inoculum of the virus transmitted by this method (366).
(iii) Influence of immunosuppression.
The possible influence of immunosuppression on disease development remains unclear. Immune suppression in transplanted patients may favor the rapid increase of HTLV-1 proviral DNA and is believed to alter the course of HTLV-1 infection in asymptomatic carriers following transplantation. Several cases of ATL in HTLV-1-positive recipients following transplantation have been reported (371, 415). However, two prospective studies conducted among 31 HTLV-1-positive Japanese recipients of kidney allografts have not recorded any cases of HTLV-1-related diseases after an average follow-up of 8 to 10 years (266, 357). Those studies concluded that immune suppression does not seem to favor the development of ATL or TSP.
Several transplant-related cases of HTLV infection have been reported, especially in countries with high seroprevalence rates. In certain cases, transmission was more closely linked to procedures associated with transplantation, such as the need for blood transfusion, than actual infection via the graft (143, 186, 194). In renal transplant patients who developed HTLV-1-associated lymphoproliferative disorders, another possible route of acquisition could have been during hemodialysis (177).
In a report by Gout et al. (143), a 41-year-old male who underwent a heart transplant and received several blood transfusions later developed subacute myelopathy. It was discovered that he had been infected with HTLV-1 from one of the blood transfusions. Remesar et al., who described the transmission of HTLV-1 from a 35-year-old mother to her daughter, reported the first incident of HTLV-1 transmission by organ transplantation (307). The patient was originally from Argentina (a low-seroprevalence area) and had received a kidney graft from her mother. Seroconversion for HTLV-1 was documented 83 days posttransplantation. The infected recipient remained asymptomatic after 4 years of follow-up (307).
In another case reported by Nakatsuji et al. (267), a cadaveric renal transplant recipient developed TSP 4 years after transplantation. At diagnosis, the recipient's serological studies (ELISA and WB) showed antibodies against HTLV-1. There was no history of blood transfusion before or after transplantation. Serology had been negative prior to transplantation, and donor screening was not performed (267). Transmission was believed to have occurred via renal graft transplantation.
Toro et al. (366) reported the transmission of HTLV-1 to three organ transplant recipients from a single donor (two kidneys and one liver) in 2003. Less than 2 years after transplantation, all three recipients developed subacute myelopathy. The donor had been infected by vertical transmission from his mother, who was originally from Venezuela, where seroprevalence is 0.39%. The rapid development of the disease was linked to the high viral inoculum transmitted during the transplantation procedure, the particular virulence of the strain, and the situation of immune suppression of the patients (366). Following this, another report described the development of ATL in another recipient from the same donor (140).
Recommendations.
The majority of organ procurement organizations have a policy of rejecting organs from HTLV-1/2-positive donors. The risk of HTLV-1 transmission during solid-organ transplantation (SOT) has been documented (99).
Policies regarding screening recommendations with respect to HTLV-1/2 are different in every country. During the donor suitability evaluation, the determination of donor HTLV-1/2 status is based primarily on the results obtained from EIA. Confirmatory HTLV testing is not always readily available and requires additional time. The timely performance of a confirmatory assay for HTLV may save organ donations from being rejected because of a false-positive screening test. However, long delays in confirmatory testing performed by commercial laboratories may also lead to the loss of grafts. In a survey performed in 1996 by the Organ Procurement Organization in the United States, only 65% of laboratories had routinely performed confirmatory testing for HTLV (105).
Current United Network for Organ Sharing regulations state that members shall not knowingly participate in the transplantation or sharing of organs from donors who are confirmed to be positive for HTLV-1 antibody by an FDA-licensed screening test unless subsequent confirmation testing unequivocally indicates that the original test results were falsely positive (204).
The decision to reject organs from seropositive patients has greater relevance in countries where these diseases are endemic. The criteria outlined by the Japanese Transplant Organization, for example, lead to the rejection of organs from HTLV-1-seropositive patients even if the recipient is seropositive. Based on these criteria, 3 to 5% of potential donors are excluded.
In other countries with low seroprevalence of HTLV-1 and -2, like Spain, the current policy of mandatory testing of anti-HTLV antibodies is applied only to organ donors coming from areas where HTLV-1 is endemic or with a high suspicion of HTLV-1 infection (364).
Taking the changes in migration trends that are occurring into account, there has been a consequent increase in potential donors from areas of endemicity residing in countries where transplant programs exist. Foreign donors with a risk of infection may be difficult to identify, especially if HTLV has been transmitted vertically or sexually. Seroprevalence studies should be performed in order to evaluate possible changes in HTLV-1/2 screening policies, especially if these tests are restricted to donors deemed to be at high risk.
Screening of blood donor candidates has been shown to be an effective strategy in preventing HTLV-1 transmission. Many countries in areas of endemicity have implemented systematic and permanent screening of all blood donors. In nonendemic areas, reports have shown that the risk of HTLV-1 infection might be enhanced in some selected donor populations, and the implementation of policies for selective donor recruitment has been recommended (297).
Infections Caused by West Nile Virus
West Nile virus (WNV) is an arthropod-borne virus that belongs to the Japanese encephalitis complex of Flaviviridae. It is a lipid-enveloped, single-stranded RNA virus. WNV infection is associated with human encephalitis and meningitis. It is transmitted primarily in birds through mosquito bites, while humans are incidental hosts. Incidental mosquito-borne infection may also occur in other mammals including horses, cats, and other domestic animals.
The preclinical incubation period ranges from 2 to 14 days following the bite of an infected mosquito. Although most individuals with WNV remain asymptomatic, approximately 20% of those infected will develop mild symptoms, often indistinguishable from other viral infections, which may last between 3 and 6 days. A transient WNV viremia occurs within 1 to 3 days after infection and lasts 1 to 11 days (with a mean of 6 days). Longer periods of viremia have been noted in some patients with advanced malignancies or taking immunosuppressive drugs (292). Recently, viremia in asymptomatic donors has been shown to persist for longer periods of time (up to 104 days). There is a greater incidence of encephalitis than meningitis, which develops in around 1 in 150 infected patients (294, 333, 334). Elderly patients have been shown to be at greater risk of developing severe neurological disease.
Geographic distribution.
WNV was first isolated and identified from a patient infected in the West Nile district of Uganda in 1937 (293). The virus has a widespread distribution in Africa, Asia, the Middle East, and Europe. Human and equine WNV outbreaks in Romania (369), Russia, Israel (387), Italy, and Tunisia (181, 418) from 1996 to 2000 have also been reported.
WNV was first detected in the Western Hemisphere in 1999 during an epizootic outbreak among birds and horses and a meningitis and encephalitis epidemic in humans in the New York City area (70, 292, 323). Over the next 5 years, the virus spread across states of the continental United States, north into Canada, and southward into the Caribbean Islands and Latin America (212).
In the United States, the 2002 epidemic of WNV neuroinvasive disease was the largest ever reported. Between 1999 and 2004, more than 16,000 cases of WNV infection were reported in the United States, with more than 7,000 cases of neuroinvasive disease (161). During 2006, 3,830 infections were identified: 35% had neuroinvasive manifestations, and 3% resulted in death (68).
The incidence of WNV disease is seasonal in the temperate zones of North America, Europe, and the Mediterranean Basin, with peak activity from July through October. In the United States, the transmission season has lengthened as the virus has moved south; in 2003, the onset of human illness began as late as December, and in 2004, it began as early as April (CDC, unpublished data). WNV activity in birds and mosquitoes has been documented year round in states with warm winter climates. Human infection in these areas is therefore a theoretical risk at all times of the year. Transmission of WNV in southern Africa and transmission of Kunjin virus in Australia increase in the early months of the year after heavy spring and summer rainfalls (160).
Diagnostic methods.
The most effective method for detecting the infection is the measurement of immunoglobulin M (IgM) antibodies in serum or cerebrospinal fluid (CSF). In documented outbreaks, over 90% of the cases had positive IgM serology, which usually becomes detectable 1 week after infection. The antigenic similarities among viruses of the flavivirus group may cause patients who have been recently vaccinated against yellow fever virus or Japanese encephalitis virus and those who have been recently infected with a related flavivirus to have a positive WNV IgM result (197, 338).
The majority of patients are asymptomatic, and IgM may be detectable for up to 6 months after infection, so an increase in titers between the acute and convalescent phases is needed to confirm acute infection (314).
In order to determine the specificity of antibodies to WNV, serum samples that test positive by ELISA should also be tested by plaque reduction neutralization tests, which are specific for arthropod-borne flaviviruses (388). The detection of viral antigens or nucleic acid in CSF, tissue samples, blood, and other organic fluids is also possible.
Routes of transmission.
Cases of human-to-human transmission have been reported in association with blood transfusions and through organ transplantation.
Recent cases of severe encephalitis due to WNV have been described in patients who have received blood transfusions (159, 348), and the CDC and FDA have investigated cases of possible transmission via blood transfusion or organ transplantation (65, 69). During the WNV outbreak that occurred between 2002 and 2003, the CDC received reports of 61 possible cases of transfusion-transmitted WNV infection. Epidemiological studies and testing of available retained donor blood samples demonstrated that blood transfusion was the confirmed source of WNV infection in 23 of these cases, with 19 cases being inconclusive (285). Forty-three percent occurred in patients who were immunosuppressed due to transplantation or cancer. Of these 23 documented cases, 16 donors who had transmitted the infection were identified. Only nine of these cases recalled symptoms suggestive of WNV infection. Serological studies of serum samples obtained at the time of transmission were negative in all of the 16 donors, showing that serology is not useful in detecting potentially infectious (viremic) patients.
During 2003, an additional 23 suspected cases of transfusion-associated WNV infection were reported to the CDC: 6 cases were classified as being confirmed/probable transfusion-transmitted WNV, 11 were noncases, and 6 were unresolved cases (72). A study containing the latest information on WNV transfusion-associated cases between 2003 and 2005 was reported recently by Montgomery et al. (253).
Transplant-related cases.
Several cases of WNV transmission through SOT have been described (67, 190, 216). Serological and clinical studies indicate that organ transplant recipients have a risk approximately 40 times that of the general population for neuroinvasive disease after WNV infection. Recipients of infected organs and other immunosuppressed patients typically have prolonged WNV incubation periods during which asymptomatic viremia can be detected, and there may also be a delayed antibody response (190).
The first organ-donor-associated WNV transmission was reported in 2002 (190). Four recipients from the same donor developed fever and neurological symptoms in the posttransplant period, and WNV infection was suspected. The donor had no relevant past medical history and had died due to severe trauma after receiving multiple transfusions from 64 different donors. The heart, liver, and both kidneys were transplanted. All four recipients presented fever and neurological symptoms an average of 15 to 18 days posttransplantation. Three of the four recipients had encephalitis, and one died. Three patients had positive serology for WNV, and in the fourth recipient, WNV was detected in cerebral tissue using nucleic acid and antigen detection techniques as well as viral isolation. Serology was found to be negative for the organ donor before and immediately after receiving the blood transfusions, but samples obtained during the transplantation procedure were positive using nucleic acid detection techniques and viral culture. Transmission was attributed to the transfusion of WNV-positive blood received by the donor the day before organ recovery (69, 71, 190).
Following these cases, others have been reported in the context of organ transplantation. In September 2005, the CDC reported that WNV infection was confirmed in three of four recipients of organs transplanted from a common donor (67). Two recipients subsequently developed neuroinvasive disease, one recipient had asymptomatic WNV infection, and the fourth recipient was apparently not infected. Serum and plasma collected from the donor were retrieved. The samples tested positive for WNV IgM antibodies and IgG by EIA but were negative for WNV RNA by PCR. The organ donor was thought to have been infected via a mosquito bite rather than through a blood transfusion, and a serum sample obtained 1 day before the organs were retrieved had WNV IgM and IgG antibodies but was PCR negative. The lung and liver transplant recipients had severe WNV encephalitis and acute flaccid paralysis with respiratory failure. One kidney recipient had a positive PCR test result in serum 22 days after transplantation and remained asymptomatic, and the other kidney recipient had no evidence of WNV infection (67).
Other articles have reported cases of WNV infection occurring in SOT recipients (12, 15, 44, 101, 158, 210, 215, 265, 305, 337, 383). Most of these cases were community-acquired (de novo) infections or had been acquired through infected blood products. The majority of these patients developed severe neurological disease, and the fatality rate was high, especially in those recipients with more intense immunosuppressive regimens.
Recommendations.
The prevention of transfusion-transmitted WNV infection is based on the exclusion of viremic patients. The following factors have raised concerns regarding the safety of the blood supply: (i) most WNV infections are asymptomatic, and thus, viremic donors could not be identified prior to donation; (ii) the estimated risk in epidemic areas could be as high as 2 to 3 cases per 10,000 donors; and (iii) a high incidence of mortality was seen in transfusion recipients. To decrease the risk of transmission, different organizations have elaborated recommendations based on the implementation of more refined donor selection criteria, the quarantine period of blood products, as well as the development and implementation of a test for WNV RNA to screen the blood supply (200, 376).
Screening tests based on specific antibody detection are not useful, as these antibodies appear 1 to 2 weeks after the infection. Screening methods should be based on the detection of nucleic acids (NAT), as antibodies usually appear after the period of viremia. Donor blood could be screened with WNV NAT with a mini-pooled-testing format (52). Routine donor screening using the test kits was implemented in July 2003. Despite the efficacy of this assay, six recipients were infected through blood transfusion in 2003, indicating that the risk of acquiring infection from tainted blood components was not completely eliminated by mini-pooled NAT screening (66).
Organ donors are screened to identify infectious risk on the basis of national organ procurement standards, which are reevaluated continuously. In January 2004, the Health Resources and Services Administration in the United States issued a statement concerning WNV, organ donation, and transplantation. Recognizing that, at this moment, NAT is used only for research and is available from a limited number of laboratories, with turnaround times that may exceed 24 h, the Health Resources and Services Administration did not support the screening of all donors for WNV infection. One study estimated that annual screening could result in the potential loss of 452.4 life years (207).
Based on this, the following recommendations have been made: (i) potential donors with meningoencephalitic or myelitic symptoms of undetermined etiology who reside in specific geographic areas during periods of human WNV activity should be excluded; (ii) if living donors are to be screened with NAT, testing should be performed as close to the time of donation as possible; and (iii) the possibility of WNV infection if an organ recipient develops fever with neurological symptoms should be considered. Appropriate serological tests and early magnetic resonance imaging and lumbar puncture should be performed (101).
In addition, transplant recipients should be educated regarding the risk of WNV infection and the use of preventive measures, especially as a recent study performed in Canada found poor rates of compliance among SOT recipients with regard to WNV protection (214).
Infections Caused by Rabies Virus
Rabies virus, genus Lyssavirus, family Rhabdoviridae, causes acute encephalitis, which is nearly uniformly fatal in unvaccinated hosts. It is a zoonosis that can affect both wild and domesticated animals and is transmitted to other animals and humans through close contact with saliva from infected animals (i.e., bites, scratches, and licks on broken skin and mucous membranes). Although many mammals may become infected, the prevalence of infection varies considerably from continent to continent (37). A large number of mammalian animal species are involved in the persistence and transmission of rabies throughout the world. In most countries of Africa, Asia, Latin America, and the Middle East, dogs continue to be the main hosts and are responsible for most of the human deaths from rabies that occur worldwide. In contrast, in North America, most documented human rabies deaths occurred as a result of infection by the silver-haired bat rabies virus variant (404).
Geographic distribution.
Rabies virus is widely distributed throughout the world and is present in all continents. According to the World Survey of Rabies for 1999, 45 out of 145 countries and territories reported no rabies virus cases during that year. Many rabies virus-free countries and territories are islands of the developed world (e.g., Japan and New Zealand) and the developing world (e.g., Barbados, Fiji, Maldives, and Seychelles). In addition, parts of northern and southern continental Europe (e.g., Greece, Portugal, and the Scandinavian countries) and Latin America (e.g., Uruguay and Chile) are also free of rabies virus. Worldwide, it is estimated that approximately 55,000 people die of rabies each year. Most of the deaths from rabies reported annually around the world occurred in Asia and Africa, and most of the victims were children: 30 to 50% of the reported cases of rabies, and therefore deaths, occurred in children under 15 years of age (404).
Diagnostic methods.
Antigen detection remains the “gold standard” for the diagnosis of rabies virus infection. IFAT is a rapid and sensitive method for diagnosis in animals and humans. Microscopic examination of impressions, smears, or frozen sections of tissue under UV light after they have been treated with antirabies serum or globulin conjugated with fluorescein isothiocyanate is performed. Viral antigen may also be detected by using the IFAT on skin biopsies from patients with clinical rabies virus infection. Test results are independent of the antibody status of the patient.
Rabies virus can be isolated using neuroblastoma cells or following the intracranial inoculation of mice. Virus may be isolated in saliva samples or other biological fluids such as tears and CSF.
Neutralizing antibodies in the serum or CSF of nonvaccinated patients can be measured using a virus neutralization test such as the rapid fluorescent focus inhibition test or the fluorescent antibody virus neutralization test. Virus-neutralizing antibodies in serum tend to appear on average 8 days after clinical symptoms appear. Rabies virus antibodies are infrequently found in CSF. An ELISA has also been used to determine antiglycoprotein antibody levels in the sera of humans and some animal species.
Molecular detection using PCR and nucleic acid sequence-based amplification techniques may be performed, and rabies virus RNA can be detected in several biological fluids and samples (e.g., saliva, CSF, tears, skin biopsy sample, and urine) by these methods (403).
Routes of transmission.
Transmission to humans occurs primarily through the bite of an infected animal but can also occur through the direct contact of mucous membranes or open wounds and skin abrasions with infectious material (e.g., saliva, neural tissue, and CSF).
The virus incubates at the inoculation site for a period ranging from 5 days up to several years, depending on the size of the inoculum and the severity and location of the wound. During the incubation period, the virus replicates locally in muscle cells (classic form) or in the epidermis and dermis (bat variant rabies virus). The virus then attaches to nerve endings and moves centripetally from the periphery to dorsal root ganglia and on to the central nervous system (CNS) by axonal transport. In the CNS, the virus has a predilection for the brain stem, thalamus, basal ganglia, and spinal cord, where it selectively replicates intraneuronally, producing encephalomyelitis, and eventually spreads centrifugally along neural pathways to multiple organ and tissue sites (51).
Transplant-related cases.
Human-to-human transmission of rabies has been described only in rare isolated cases after transplantation. Eight documented cases of rabies transmission through corneal transplants have been reported (7, 13, 18, 60, 134, 178, 193, 313).
Two reports have described transmission through SOT (162, 346). In 2004, transmission of rabies virus from a common organ donor (with unrecognized rabies virus infection) through the transplantation of solid organs and vascular material was reported in the United States. Four patients received organs (two kidneys and the liver) or vascular tissue (iliac vessel conduit used for hepatic artery reconstruction in another liver transplant recipient) from the organ donor, who had been apparently healthy before dying from a subarachnoid hemorrhage. The four recipients developed encephalitis and died within 30 days following transplantation. By the 27th day following transplantation, all three solid-organ recipients had been readmitted to the hospital with complex symptoms and progressive neurological disease that rapidly progressed to coma and death. The artery allograft recipient developed a confusional state with suicidal ideation on day 26 posttransplant. The patients died an average of 13 days after the onset of neurological symptoms. Postmortem examinations led to the diagnosis of transplant-associated rabies virus infection, which was confirmed by multiple methods in several tissue specimens from the recipients (346).
A similar case of transmission of rabies virus to at least three recipients in Germany has been reported. In 2005, the German Foundation for Organ Transplantation declared three cases of suspected rabies virus infection in a group of six patients who received organs from a common donor who died in late December 2004. In this case, the donor had spent time in India and showed no signs of rabies virus infection. While hospitalized, the organ donor had suffered a cardiac arrest, developed rapid neurological deterioration, and died with clinically unsuspected rabies virus infection. Infection of three of the patients who received organs from the donor was confirmed. These patients had received lung, kidney, and kidney/pancreas transplants (162).
Recommendations.
There are no formal recommendations to screen all donors for the presence of rabies virus antibodies, especially as the risk of rabies virus transmission is very low. Burton et al. noted that even if the number of human rabies cases in the United States increased 100-fold, the risk of rabies transmission by organ transplantation would be less than 1 in 1012 (51).
Donor screening could prevent some cases of rabies virus transmission if questions concerning animal bites and donors’ travel history are carefully considered. Questioning the patient and relatives about the possibility of contact with bats anywhere in the world or of any other mammalian bite abroad should identify patients at risk. Also, potential donors with unexplained neurological symptoms should be evaluated for the possibility of CNS infections (217). If there is even a minimal risk of infection, the donor should be tested for rabies virus before transplantation (by skin biopsy, saliva test, and, preferably, a brain biopsy). If there are time restraints or specific diagnostic tests are not available, anyone with a history of possible exposure to rabies virus should not be accepted as a donor.
If organ transplantation from a rabies virus-infected donor occurs, prompt preemptive treatment with rabies virus vaccine and rabies virus immunoglobulin is indicated. Recipients of transplanted organs and the contacts of the infected donor exposed to saliva or other potentially infected secretions or tissues should receive rabies virus immunoglobulin and initiate a course of rabies virus vaccination (217, 403).
FUNGAL INFECTIONS
Infections Caused by Coccidioides immitis
Several species of Coccidioides can cause disease in humans. In addition to Coccidioides immitis, Coccidioides posadasii has been described recently as the likely etiologic agent of coccidioidomycosis originating outside California (30).
Primary coccidioidomycosis is a pulmonary infection in which as many as 60% of subjects may be asymptomatic. The illness begins 1 to 3 weeks after the inhalation of arthroconidia and presents with fever, cough, and pulmonary infiltrates. The usual course of the disease is a tendency to resolution over a period of several weeks. However, in immunosuppressed patients, including transplant recipients, primary coccidioidomycosis may develop into progressive disease with dissemination. In its disseminated form, coccidioidomycosis may involve almost any organ, with the most common sites of involvement being the lungs, skin and soft tissue, bones, joints, and meninges.
Geographic distribution.
Coccidioides spp. have a distribution that encompasses semiarid to arid life zones, principally in the southwestern United States and northern Mexico, where they are endemic (349). Coccidioides is also found in parts of Argentina, Brazil, Colombia, Guatemala, Honduras, Nicaragua, Paraguay, and Venezuela (90). Hyperendemic areas include Kern, Tulare, and Fresno counties in the San Joaquin Valley of California and Pima, Pinal, and Maricopa counties in Arizona. Residence or travel to these areas of endemicity is a risk factor for infection.
Diagnostic methods.
The diagnosis of coccidioidomycosis is based on clinical suspicion supported by microbiological, histopathological, or serological evidence. Approved skin test reagents are no longer commercially available. Direct examination of clinical specimens such as organic fluids, sputum, and tissue in 10% KOH may show spherules with a thick wall and endospores.
Culture provides a definitive diagnosis. Blood cultures may also occasionally yield positive results for patients presenting with overwhelming infection (88). Urine fungal culture could be useful for the diagnosis of disseminated coccidioidomycosis. Histopathological findings of Coccidioides spp. in its host forms include the presence of typical large spherules. Immunological methods using complement fixation (CF) and immunodiffusion (ID) using the complement-fixing antigen have also been used (280), and more recently, EIA for coccidioidal IgG and IgM antibodies has been used (242). Immunodiffusion using the complement-fixing antigen and EIA are the most commonly used tests in clinical practice. False-positive coccidioidal serological results have been documented in candidates for lung transplantation who had underlying cystic fibrosis due to the high circulating levels of nonspecific or cross-reacting serum proteins that interfered with the test (108), and therefore, results must be interpreted with care.
Routes of transmission.
Coccidioides sp. infection is acquired following the inhalation of arthroconidia. Cases of human-to-human transmission have been described in the context of SOT.
Transplant-related cases.
Coccidioidomycoses complicating the postoperative course of renal, heart/heart-lung, liver, or small bowel transplant recipients have been reported (32, 34, 35, 43, 249, 368, 405).
During transplantation, possible routes of transmission include (i) reactivation of latent infection, (ii) posttransplant de novo infection of recipients who live or travel to areas of endemicity, and (iii) transmission secondary to transplantation of organs from an infected donor. Posttransplant reactivation of coccidioidomycosis has been the mechanism most frequently described.
Most of the case series and individual case reports are from areas of endemicity or involved patients who had been former residents in these areas. In a few cases, brief visits to areas of endemicity had been sufficient for the infection to be acquired (35).
The risk of developing symptomatic coccidioidomycosis is increased by a history of prior coccidioidomycosis, positive coccidioidal serological tests at transplantation, or clinical evidence of active infection at transplantation. After transplantation, the main risk factor for developing coccidioidal infection is antirejection therapy (high-dose corticosteroids and mainly the use of polyclonal antilymphocyte or antithymocyte preparations and monoclonal therapies such as muromonab-CD3 [OKT3]). Dissemination is common in transplant recipients, up to 75% in some series, with or without concurrent pulmonary involvement (33, 173).
Coccidioidomycosis after SOT can occur at any time, but the period associated with the highest risk is the first year posttransplantation: 70% of cases develop in this period, with 50% occurring during the first 3 months (35). Overall mortality was 60% to 72% for the first cases described (86), but recent reports indicate that mortality has been lower than in earlier years, ranging from 0 to 33% (33, 154).
The clustering of cases in the first year and the frequency with which these patients have evidence of prior infection indicate that posttransplantation coccidioidomycosis is often a result of reactivation rather than a de novo infection following transplantation. The importance of prophylaxis in these patients has been demonstrated in different studies (35, 126).
The transmission of coccidioidomycosis with grafts has been well documented in certain cases, although this may be difficult to demonstrate in areas of endemicity, where there is significant background seropositivity. This may be illustrated by the results of a prospective serological survey of healthy potential live kidney or liver donors performed in Arizona, which revealed a seroprevalence of 1.9% (31).
Reports of transmission due to infected donor lungs, liver, and kidneys have been published (249, 368, 405). In all these cases, coccidioidal infection developed in the early posttransplant period. In one report, a patient from North Carolina developed fatal coccidioidomycosis soon after bilateral lung transplantation. The donor had previously traveled to Mexico, and the recipient had no history of travel to an area where C. immitis is endemic (249). Another lung transplant recipient developed fulminant pneumonia in the immediate postoperative period after transplantation. The recipient's serological tests had been negative 2 years before the procedure. The donor had been born in Arizona, and a postmortem study confirmed C. immitis in a lymph node (368).
Wright et al. described two cases (in a liver recipient and a kidney recipient) of rapidly fatal, disseminated coccidioidomycosis that occurred in organ transplant recipients who had never visited or lived in an area where C. immitis is endemic (405). Both subjects had received an organ from the same donor, an individual with unrecognized active coccidioidomycosis at the time of death (405). Postmortem examination of liver and kidneys appeared to be normal, and these had been harvested for transplantation. One month later, examination of permanent histopathological specimens of brain and basilar meninges revealed multinucleated giant cells containing fungal organisms consistent with C. immitis. The results of premortem serum CFA tests were positive for C. immitis, at a titer of 1:32. After the deaths of the two other SOT recipients, the recipient of the other kidney received prophylactic itraconazole and continued this regimen for 3 months. The patient remained completely asymptomatic for 2 years after transplantation. The kidney graft had been in cold isotonic solution for 37 h before transplantation, and it is possible that the viability of C. immitis was significantly impaired by the prolonged exposure to cold.
Recommendations.
Serological screening for coccidioidomycosis in transplant donors or recipients coming from or residing in areas of endemicity is recommended. EIA for IgG and IgM, complement fixation for IgG, and immunodiffusion for IgM and IgG are the available serological tests in areas of endemicity. The routine serological screening of donors from areas of endemicity may help identify infections, but the results of such screening would not necessarily make the rejection of the donor organ mandatory, especially after bearing in mind the current donor shortages.
For areas where this organism is not endemic and Coccidioides serology is not routinely performed, it is important to establish the donor's history of travel to areas of endemicity in order to assess the relative risk of coccidioidomycosis. If risk of infection exists (donors with a history of traveling to or living in areas of endemicity), a Coccidioides sp. serological test must be performed at local reference laboratories.
If the donor had a history of remote coccidioidomycosis or radiological changes of prior coccidioidomycosis or had lived in or traveled to areas of endemicity, prophylaxis with oral fluconazole after transplantation could be started until the results of the serological studies become available. If a positive result is obtained and the transplant has already been performed, active illness must be excluded. If no focus is found, prophylaxis with fluconazole or itraconazole should continue for 6 months. After transplantation, all patients should be monitored serologically every 3 to 4 months during the first year and yearly thereafter (36).
Guidelines for the management of coccidioidal infection have been published (127, 128), and recently, posaconazole has been accepted by the American Thoracic Society and European Medicines Agency for coccidioidal therapy. Transplant recipients have received the drug without complications (10).
Infections Caused by Histoplasma capsulatum
Histoplasmosis is an endemic mycosis caused by Histoplasma capsulatum (family Ascomycetes). It is a soil-based fungus acquired by the inhalation of mycelial fragments and microconidia and is most often found in river valleys where specific temperature and humidity conditions favor its growth. High concentrations of the mold phase of H. capsulatum are also found in soil that is rich in nitrogen, as occurs in areas in which large flocks of birds roost (203). Infection is common in areas of endemicity, and most affected people have been infected before adulthood. The extent of disease is determined by the inoculum of conidia inhaled into the lungs and the immune response of the host to the conidia. Almost all those infected with H. capsulatum have asymptomatic hematogenous dissemination, but only rarely does this lead to symptomatic disease.
Geographic distribution.
H. capsulatum is endemic in the Mississippi and Ohio River valleys, Central America, and certain areas of Southeast Asia and the Mediterranean basin.
Diagnostic methods.
Growth of H. capsulatum from tissue or fluid samples is used to establish a definitive diagnosis of histoplasmosis (389), although the organism can take weeks to grow in vitro. Blood cultures, especially those using the lysis-centrifugation system (isolator tube), are more sensitive for patients who have disseminated infection than for those who have pulmonary disease only. Measuring the cell wall polysaccharide antigen of H. capsulatum in urine is a sensitive diagnostic tool for patients who have disseminated infection (394). Antigen is rarely detected in patients who have chronic pulmonary histoplasmosis or granulomatous mediastinitis, but it is positive in approximately 80% of those who have acute pulmonary histoplasmosis. Cross-reactivity can occur with blastomycosis, paracoccidioidomycosis, and penicilliosis, and false-positive results in serum have been observed in 16% of SOT patients who received rabbit antithymocyte globulin (391). Detection of antigen in body fluids (e.g., bronchoalveolar lavage fluid and CSF) offers a valuable approach for rapid diagnosis in patients with progressive disseminated histoplasmosis and diffuse pulmonary histoplasmosis (392, 395).
The development of PCR for detecting H. capsulatum in blood and tissue samples taken from patients who have disseminated histoplasmosis is in progress. Although several assays were reported to be useful, the accuracies of these methods are unclear, and therefore, none are in routine clinical use (29, 42), especially as published studies have not demonstrated superiority compared with standard methods (29, 358).
Serology plays an important role in the diagnosis of certain forms of histoplasmosis (389). The standard assays are CF and ID. The sensitivity of the CF and ID assays is approximately 80%, and the use of both assays increases the diagnostic yield (202). Patients who have chronic cavitating pulmonary histoplasmosis and chronic progressive disseminated histoplasmosis almost always have positive results with both assays. However, in patients who are immunosuppressed and who cannot mount an adequate antibody response, serology is rarely useful and should not be relied upon for the diagnosis of histoplasmosis. In early studies, a specific radioimmunoassay was found to be more sensitive than ID or CF for antibody detection following acute histoplasmosis (390).
For the screening of asymptomatic donors with positive risk factors for histoplasmosis infection (past history of travel to or residence in areas of endemicity), serological methods based on antibody detection (CF or IF assays) would be of use, as fungal burdens in these individuals would be expected to be low. If acute histoplasmosis is suspected in the donor, detection of urinary antigen or culture/histopathological examination of other specimens could be used.
Routes of transmission.
Histoplasma sp. infection results from the inhalation of the microconidia, but isolated cases of human-to-human transmission during transplantation have also been described (227).
Transplant-related cases.
Disease may develop due to the reactivation of latent lesions or from new exposure in zones where Histoplasma is endemic (286, 354, 401), but transmission of histoplasmosis from donor to recipient via graft has also been described (227).
In the cases described in the literature, symptoms started a median of 1 year after organ transplantation, and the majority of cases occurred in the first 18 months. Pulmonary involvement is common, and immunosuppressed patients can develop severe life-threatening pneumonia, although other varied manifestations have been observed in transplant patients (48, 125, 259, 354, 401, 414). In this respect, the presentation and clinical course of histoplasmosis in the SOT population appear to be somewhat less severe than histoplasmosis in the AIDS population (393).
A study performed in Indianapolis, IN, at a medical center located in an area of hyperendemicity demonstrated that histoplasmosis is a rare infection following the immunosuppression of allogeneic bone marrow transplantation (BMT) or SOT (377). In this study, 18% of the recipients had CF titers that were positive for H. capsulatum, and chest X rays showed findings consistent with past histoplasmosis in 4% of the recipients. All allogeneic BMT recipients received prophylaxis with fluconazole, but SOT recipients were not routinely treated with systemic antifungal prophylaxis. During the posttransplant period, no cases of histoplasmosis in BMT or SOT patients were diagnosed. The low incidence of histoplasmosis in immunocompromised patients, in the absence of an outbreak, provides evidence against reactivation as a significant mechanism for histoplasmosis. In areas of endemicity, an increase in the incidence of histoplasmosis in transplant patients during two large outbreaks has been reported (286, 396), but these cases probably represent newly acquired infections.
However, other authors postulated reactivation as a pathological clinical form. Davies et al. reported an estimated incidence of histoplasmosis of 0.4% in renal transplant recipients in Minnesota, an area of low prevalence (94).
Although rare, a third mode of acquisition of histoplasmosis in transplant patients may be transmission through an infected allograft from a patient with unrecognized histoplasmosis. Two cases of disseminated histoplasmosis in residents from nonendemic areas, developing 8 and 9 months following transplantation from a donor who resided in an area of endemicity, have been reported (227). DNA fingerprinting confirmed that the isolates were identical, proving that they were transmitted with the allograft. The donor had been asymptomatic, and tests for anti-Histoplasma antibodies and antigens were negative.
Recommendations.
Serological testing of potential donors and recipients living in areas of endemicity with a history of pulmonary disease within the past 2 years, consistent with histoplasmosis, or radiographic findings suggestive of active or past histoplasmosis should be performed.
In nonendemic areas, it is important to establish the donor's history of travel to areas where this organism is endemic. Serological testing should be recommended in cases where there is a past history of travel to or residence in these areas. Serum could be sent to a reference laboratory, and CF and ID assays (or radioimmunoassay, if available) should be performed. Serology results should not condition the indication for transplantation.
The use of itraconazole prophylaxis in recipients from donors with a past history of histoplasmosis (prior infection, pathological chest X ray, and positive serology) is controversial. Some authors postulated that most of the posttransplant cases of histoplasmosis in areas of endemicity occur de novo during an outbreak and are not due to reactivation, and consequently, routine prophylactic antifungal therapy for the prevention of histoplasmosis following SOT cannot be recommended for these recipients (377). However, other authors believe itraconazole prophylaxis should be offered to recipients of organs from a seropositive donor. In addition, due to possible drug interactions, plasmatic levels of calcineurinic inhibitor drugs should be monitored during itraconazole use. The duration of this prophylaxis is difficult to establish, but a course of at least 3 to 6 months, covering the period of more active immunosuppression, should be offered (127). Early experience with the use of posaconazole in the treatment of histoplasmosis has been favorable, but further studies are necessary to assess its use in prophylaxis (309).
Other Regional Fungal Infections
Infections caused by Paracoccidioides brasiliensis.
Paracoccidioides brasiliensis has a restricted geographic distribution. It has been reported only in Latin America, from Mexico (23°N) to Argentina (34°S), although it is not present in all countries within this area (Chile and some of the Caribbean Islands are not affected). The majority of cases have found in Brazil, where there is an annual incidence rate of 10 to 30 per million inhabitants (88). The disease has two main clinical presentations, a more frequent chronic adult form and the acute/subacute, more severe juvenile form (95). The hallmarks of the chronic form are extensive lung involvement and extrapulmonary lesions, representing endogenous reactivation years after infection as a result of immunosuppression, debilitating disease, chronic alcoholism, malnutrition, or smoking (308). Dry cough and dyspnea are the principal symptoms, and chest X-ray images usually reveal pulmonary infiltrates. Ulcerated mucocutaneous lesions and lymph node chain involvement are frequently observed (more frequently in the juvenile forms).
For diagnosis, wet-mount direct examinations of sputum or exudates reveal P. brasiliensis in >90% of patients, and histological studies reveal typical findings. Serological tests are useful, and IgG, IgM, and IgE are regularly detected, but sensitivity is reduced in patients with disorders that cause immunosuppression (100, 109). The ID test is more specific than CF but is not quantitative. EIA methods are more sensitive but less specific than complement fixation (308). In general, standardized methods are not available for clinical testing (3).
Unusual clinical and radiological manifestations can occur in immunocompromised patients. Only three cases of paracoccidioidomycosis in SOT recipients have been reported, and all occurred in renal transplant patients (339, 353, 417). In all cases, infection developed more than 5 years after transplantation, and clinical presentations were similar to those of other cases of this mycosis in nonimmunosuppressed patients. Exceptionally, one patient was found to have cavitating lung lesions, which is infrequent in immunocompetent patients (417).
There are no reported cases of infection transmission via graft.
The low incidence of paracoccidioidomycosis in SOT recipients may be explained by the routine use of trimethoprim-sulfamethoxazole as primary prophylaxis for Pneumocystis jiroveci pneumonia, which is also effective against Paracoccidioides brasiliensis (135).
Paracoccidioidomycosis is very unusual in transplant patients, and therefore, specific measures to control this organism are unnecessary in this setting. Serological tests are frequently negative for patients with chronic diseases, including transplant candidates, and are therefore not deemed to be useful in these patients. Clinicians and radiologists should be aware of unusual clinical and radiological manifestations of P. brasiliensis infection when evaluating potential donors from Latin America showing lung and skin lesions, particularly when they fail to identify acid-fast bacilli in samples.
Infections caused by Blastomyces dermatitidis.
Blastomyces dermatitidis is endemic in South Central and North Central United States, extending into Wisconsin, Minnesota, and the southern portions of Ontario, Manitoba, Saskatchewan, and Alberta. The organism is also found in the Mediterranean basin and parts of Africa. The natural habitat is thought to be soil and decaying wood (203). Blastomycosis is acquired through the inhalation of the conidia of the mold form and extremely rarely through direct cutaneous inoculation (54, 145). Hematogenous dissemination occurs without clinical manifestations. In immunosuppressed patients, more severe disease is likely to occur, and the mortality rate is higher (281).
Most infections are asymptomatic. The main clinical manifestations are pulmonary and range from atypical, self-limiting pneumonia to chronic pneumonia or even severe infection with adult respiratory distress syndrome (246). Many patients who have blastomycosis present with cutaneous involvement as well as pulmonary disease. Other common manifestations of disseminated blastomycosis are genitourinary tract infections, septic arthritis, CNS infection, and osteomyelitis (321).
The definitive diagnostic test for blastomycosis is the isolation of the organism using specific culture media. Standard antibody assays for blastomycosis are neither sensitive nor specific. A urinary antigen enzyme immunoassay for B. dermatitidis is currently available (112), but significant cross-reactivity with histoplasmosis has been noted. Tissue biopsy with histopathological examination and cytological studies based on the distinctive morphology of the yeast allow early diagnosis. Blastomycosis has been reported infrequently in immunocompromised patients such as solid-organ and bone marrow transplant recipients (335), patients receiving long-term immunosuppressive therapy (283), and patients with AIDS (282).
Studies of blastomycosis infection in SOT recipients performed in Alabama and Wisconsin have shown that it is an uncommon infection in these patients (131, 281). Pneumonia was the most common clinical presentation and was frequently complicated with acute respiratory distress syndrome. Dissemination with skin and CNS involvement occurred frequently. Overall mortality was found to be 29 to 36% and was twice as high in those with acute respiratory distress syndrome. Cases in SOT recipients occurred an average of 26 months after transplantation.
There are no documented cases of blastomycosis transmission from donor to recipient via graft. A case of pulmonary blastomycosis in a renal transplant recipient secondary to dissemination following accidental cutaneous inoculation of B. dermatitidis has been described (54).
Specific precautions in recipients and donors prior to transplantation are probably unnecessary mainly due to the low incidence of the infection reported in transplant patients and the low diagnostic yield of the antigen- and antibody-based techniques available.
Infections caused by Penicillium marneffei.
Penicillium marneffei is a dimorphic fungus that is endemic in Southeast Asia, southern China, Taiwan, and Hong Kong and causes opportunistic infections. Isolated cases have been reported for patients who had traveled to areas of endemicity and returned home to Western countries (22, 312, 378). It has also been reported for patients with deficiencies in cellular immunity and HIV infection and for patients receiving steroids or other forms of immunosuppressive therapy (82, 365, 378, 400).
The initial presenting features of the disease are usually nonspecific, like fever, anemia, and weight loss. A molluscum contagiosum-like skin lesion has been reported in 70% of the patients. Other common clinical features include generalized lymphadenopathy and hepatosplenomegaly (111).
A definitive diagnosis can be made only by direct visualization of the fungi using different staining techniques (355) or after culture from infected material (78).
Recently, serological diagnosis by an indirect immunofluorescent antibody test has been shown to be useful for the early diagnosis of the infection (412). More specific ELISAs have also been developed (56, 57).
P. marneffei infection has seldom been reported in transplant recipients even in areas of endemicity and is only rarely described as being an important cause of invasive fungal infection among transplant patients (79, 180, 386). In the cases described, infection developed several months after transplantation, most probably due to the reactivation of latent infection.
No cases of P. marneffei infection transmitted from donor to recipient have been reported, and therefore, no special screening tests or precautions would be necessary in these patients, as the infection occurs only rarely in transplant patients.
PARASITIC INFECTIONS
Infections Caused by Plasmodium spp.
Malaria is an acute systemic illness caused by infection with Plasmodium falciparum, Plasmodium vivax, Plasmodium malariae, or Plasmodium ovale, all of which are transmitted to humans by female Anopheles species mosquitoes. There are an estimated 300 to 800 million clinical cases of malaria and 1 to 3 million deaths due to malaria annually in the tropics and subtropics (149).
Plasmodium species have two main phases in their life cycle; an asexual replicative phase in humans and a phase of sexual replication in the mosquito. All symptoms, signs, and pathological features of the disease are caused by the asexual erythrocytic stage of the parasite's life cycle. This stage involves the invasion of normal erythrocytes by parasites, replication of the parasites in the erythrocytes over 2 to 3 days, rupture of these cells, and reinvasion of normal erythrocytes. This exponential parasite replication in the bloodstream can increase parasite density by 5- to 30-fold every 2 to 3 days. In the case of P. vivax and P. ovale, a proportion (hypnozoites) remain dormant inside the hepatocytes, and these forms would be responsible for future relapses (149). Without reinfection, and if the patient survives without treatment, the persistence of the parasite in the human is estimated to be 1 year for P. falciparum, 3 to 5 years for P. vivax and P. ovale, and as long as 40 years for P. malariae. During this time, the patient may have few symptoms; this occurs especially in the semi-immune population of countries where the disease is endemic.
Geographic distribution.
Malaria is currently endemic in more than 100 countries worldwide, which in return are visited by more than 125 million travelers annually. P. falciparum is found in sub-Saharan Africa, Southeast Asia, and the Indian subcontinent as well as in South America, Haiti, the Dominican Republic, Jamaica (where isolated cases have been recently reported), and areas of Oceania. P. malariae and P. ovale are present in sub-Saharan Africa. P. vivax is prevalent in areas of Southeast Asia, the Indian Subcontinent, and Central and South America (76).
Diagnostic methods.
The use of thick and thin blood smears stained with Giemsa, Field, or Wright stain is a sensitive technique for the diagnosis of malaria and allows an estimation of the degree of parasitemia as well as the identification of the infecting species of Plasmodium (148, 254). There are other rapid diagnostic techniques based on immunochromatography, which detect the HRP2 (histidine-rich protein 2) antigen, that have a high sensitivity (95%) but that do not quantify parasitemia or identify the species involved. These tests also have a high rate of false-negative results, with parasitemias below 300 parasites/μl or above 18,000 parasites/μl (148, 254).
Techniques based on the amplification of parasitic DNA (PCR) have high sensitivity and specificity (close to 100%) and allow the detection of low levels of circulating parasites (not usually detectable by conventional microscopy) and mixed infections. The main drawback is the time required to perform the test, which, in practical terms, limits its use as a rapid diagnostic method (148, 254).
Serology is not useful in the diagnosis of current infections.
Routes of transmission.
Bearing the life cycles of different species of Plasmodium in mind, malaria may be transmitted in several ways in the context of SOT. Malaria may be transmitted through infected blood products. Malaria may also be directly transmitted via an infected organ. It may be difficult to demonstrate whether the infection is transmitted by an infected organ or by parasitized erythrocytes within the organ. In the case of liver transplantation specifically, transmission may be due to infected hepatocytes (hepatic schizogony) or parasitized erythrocytes within the hepatic sinusoids. In other types of organ transplants (renal and cardiac), if the infection has not been acquired through transfusion, it would be assumed that it must have occurred due to the transmission of parasitized red cells within the organ, even though the washing of organ blood during the transplantation procedure should minimize this risk. The time frame from transplantation to development of symptoms may help clarify the mechanism involved in transmission, taking into account the incubation periods of different Plasmodium species. If the infection is transfusion associated or due to the transmission of parasitized red blood cells, symptoms should develop earlier (1 to 3 days) than if the infection is transmitted through infected cells within the organ (more than 1 week).
Reactivation of infection due to posttransplant immunosuppression has been described in recipients (20).
Exposed organ recipients could have an increased risk of acquiring malaria infection de novo, although this has not been clearly documented to date.
Transplant-related cases.
Several cases of malaria in organ transplant recipients have been described in the literature, with the majority of cases involving renal transplant patients. At least 45 cases have been identified in total: 36 in renal transplant patients (24, 55, 92, 147, 174, 183, 198, 223, 224, 270, 372, 410), 6 in liver transplant patients (89, 243, 356), and 3 in the context of cardiac transplantation (17). Upon analysis of the data available in the literature, P. falciparum was identified as the infecting species in the majority of cases (21 cases), there were 13 cases due to P. vivax, 1 case due to P. ovale (hepatic transplant), and 1 case of P. malariae in a renal transplant patient. In three renal transplant recipients, a mixed parasitemia with P. falciparum and P. malariae was found.
Although it can be difficult to establish the exact mode of transmission of the infection, in at least 14 of these cases (3 heart, 5 liver, and 6 renal transplants), there was evidence of donor-to-host transmission via the graft.
Included in these data are the data from three publications that identified cases of malaria following multiorgan donation (81, 120, 245). In the cases reported by Fischer et al. in 1999 following organ donation from an immigrant from an endemic zone (120), malaria due to P. vivax was detected in the liver recipient (28 days posttransplantation), heart recipient (suspected due to a rise in specific antibodies against P. vivax 12 months posttransplantation), and kidney recipient (6 weeks posttransplantation). In the recipient of the second kidney, there was no clinical or laboratory evidence of malaria infection (120). Chiche et al. (81) described another case of transmission of P. falciparum from a common donor who had a history of recent travel to an area of endemicity, although the cause of death was not attributed to acute malaria infection. The heart recipient developed symptoms 5 days posttransplantation and died as a direct consequence of the infection. Parasitemia was detected 8 days posttransplantation in the liver recipient, and the kidney recipients received preventive antimalarial therapy (81). All three recipients had favorable outcomes. Menichetti et al. recently reported a case of P. falciparum transmitted from a donor from a country of endemicity to a liver recipient (symptoms commenced 3 days posttransplantation) and to a kidney recipient (no infection was demonstrated in the recipient of the other kidney) (245). In the cases described, diagnosis was made following transplantation, and no prior screening tests had been performed.
The majority of cases occurring in renal transplant patients had favorable outcomes. The majority of deaths were associated with infection by P. falciparum. The prognosis of posttransplant malaria varies depending on a series of factors, including the type of organ transplanted, the species of Plasmodium involved, the type of immunosuppressive therapy, and, most importantly, the delay in diagnosis and initiation of treatment. In general, P. falciparum tends to be more virulent than other species (120, 183, 372). The parasites are capable of survival for more than 24 h in blood at 4°C, and therefore, the time of cold preservation does not prevent the transmission of the parasite. Renal transplants tend to have a better prognosis: cold preservation time for the kidney is longer (24 to 48 h), and therefore, it may be assumed that a decreased parasitic load is transmitted compared to that for liver (<12 h) or heart (3 to 4 h) transplants. Less aggressive immunosuppressive therapy also tends to be used in renal transplantation compared to liver or heart transplantation (81). In spite of this, the majority of cases have occurred in renal transplant recipients, but this must reflect the higher number of these transplants performed. It is also possible that cases of malaria in other types of organ transplants may be underdiagnosed due to the more severe course of the infection and unfavorable outcome before a diagnosis may be established.
Recommendations.
Malaria is an infrequent complication of SOT in countries where the disease is not endemic, but screening of donors from countries of endemicity or if there is a history of recent travel (two or three preceding years) to these areas should be performed. Detection of this infection should not necessarily contraindicate organ donation unless the cause of death is related to the malaria, in which case the organs should be rejected.
The diagnostic tests that should be performed are examinations of thick and thin blood films. Immunochromatography-based techniques are useful but do not detect low levels of parasitemia. The use of PCR, if available, could exclude cases with low parasitemia. If a diagnosis is established, the donor should be treated, but if this is not possible, prompt treatment of recipients should be initiated, bearing in mind the specific species involved and resistance patterns, as early treatment has been demonstrated to prevent complications. It would be necessary to administer primaquine only for radical cure in liver transplantation in the case of infection due to P. vivax and P. ovale, as hypnozoites from hepatic schizogony are not established for other species. Primaquine would not be necessary in cases of transfusion-transmitted malaria, as hepatic hypnozoites would not be established in these cases either.
The possible drug toxicities of antimalarial drugs, especially the possible interactions with other drugs, such as those between quinine and chloroquine with cyclosporine, should be taken into account (20).
Infections Caused by Leishmania spp.
The term leishmaniasis designates the group of diseases produced by protozoa of the genus Leishmania. The parasite is transmitted to humans through the bite of an infected female Phlebotomus fly (or Lutzomyia in America). Various clinical syndromes exist: visceral leishmaniasis (VL) (kala-azar) produced by Leishmania donovani, Leishmania infantum, and others; cutaneous, mucocutaneous, and diffuse cutaneous leishmaniasis; and post-kala-azar dermal leishmaniasis (149). In immunocompetent patients, infection may be subclinical, with no hematological or clinical abnormalities: only 1 in 8 to 10 infected patients tend to develop overt disease. Leishmania spp. have the ability to elude the immune response and remain latent inside macrophages for years. The risk of developing active disease depends on factors such as the size of the inoculum, the virulence of the strain, and the host's ability to control the infection, and for the latter, intact cellular immunity would be most important.
Geographic distribution.
VL is endemic in around 60 countries worldwide, and an estimated 500,000 new cases are diagnosed every year (402). This disease has a high prevalence rate in Southern Europe, India, Kenya, Sudan, Brazil, and tropical areas where various mammals can act as reservoirs (canines and rodents in zoonotic VL and humans in anthroponotic VL).
Diagnostic methods.
Confirmation of the parasite in bone marrow or splenic aspirate via direct microscopy after staining with Giemsa or culture in Novy-MacNeal-Nicholl or other media provides a definitive diagnosis. In the majority of cases of VL in transplant patients, diagnosis has been made by the detection of parasites in bone marrow biopsies (21, 27, 164, 319). The most widely used serological techniques to detect anti-Leishmania antibodies are IFAT, ELISA, and direct agglutination tests. Certain recombinant antigens of Leishmania spp. such as rK39 have been used in ELISAs as well as in rapid immunochromatography tests. A positive reaction would have a correlation with an active episode of VL, although occasionally, antibodies against the rK39 antigen may persist even after cure (91, 419).
In contrast to HIV-positive patients, where seroconversion occurs in only 50% of patients with VL (295), positive IFAT or ELISA serology with accompanying symptoms suggestive of VL in transplant patients has a sensitivity similar to that found in immunocompetent patients according to some series (around 80%) (319). However, cross-reactivity with other infections and the inability of these tests to differentiate between recent or past infection may pose problems (331).
In recent years, this has led to an increasing interest in the development of techniques for the direct detection of Leishmania antigens. In chronic infections such as VL, detection of antigens in serum may prove to be difficult due to the presence of circulating immune complexes and autoantibodies. A new latex agglutination test that detects Leishmania antigen in urine has demonstrated 100% specificity and 68 to 100% sensitivity and a good correlation with parasitic activity, declining rapidly after treatment (16). Molecular diagnosis based on PCR techniques also has a high sensitivity and specificity and allows a differentiation between different species of Leishmania (331).
Routes of transmission.
In transplant patients, Leishmania infection may occur in one of four ways. First, if the donor has undiagnosed VL, the recipient may be infected via the graft, especially as asymptomatic infection is more frequent than symptomatic disease even in areas of endemicity. This mode of transmission would be limited to organs that form part of the reticuloendothelial system, such as the liver. Second, although anecdotal, cases of transfusion-associated VL have been reported in Great Britain, France, Belgium, and India (275). Routine serology testing for Leishmania spp. for blood or organ donors is not performed, even in areas of high endemicity. Third, a previously infected recipient may reactivate latent infection in the posttransplant period; this is believed to be the mechanism responsible for most cases of transplant-related leishmaniasis (27, 164, 319). Leishmania serology is not performed routinely in transplant recipients. Finally, immunosuppressed patients may develop de novo infection with a greater frequency than immunocompetent patients. Based on this, periodic routine serology testing could be recommended for transplant patients living in or traveling to areas of endemicity in order to detect new infections (248).
Transplant-related cases.
Over 60 cases of VL in SOT recipients have been described (14, 27, 136, 164, 176, 184, 251, 274, 319, 342), with the majority occurring in renal transplant patients. This correlates with the increased number of renal transplants performed compared to other organs. As this type of transplantation procedure is technically more straightforward, it is also possible that more renal transplants may be performed in countries of endemicity where the infrastructure to perform the more complicated heart or liver transplantation procedures may not be readily available.
At least 50 cases of VL in renal transplant patients (1, 4, 14, 21, 27, 40, 49, 107, 114, 116, 117, 138, 139, 152, 164, 182, 184, 199, 206, 219, 221, 229, 233, 238, 250, 251, 258, 260, 274, 303, 322, 336, 342, 359), 6 in liver transplant recipients (21, 153, 164, 176), 3 in heart transplant recipients (124, 164, 420), 2 in lung transplant recipients (21, 255), 1 in a BMT recipient (343), and 1 in a combined kidney-pancreas recipient (367) have been documented. According to several authors, the number of cases may well be underestimated. The majority of transplant patients who developed VL were originally from an area of endemicity (one-third of cases have been reported in Spain) or had a history of travel to areas of endemicity (164, 319).
The number of transplant recipients with positive Leishmania serologies who developed VL in the posttransplant period remains unknown, as this test is not routinely performed in these patients. The difficulties in diagnosing these patients who may present with atypical symptoms due to immune suppression and the consequent delay in diagnosis and treatment explain the high resulting mortality in this context (up to 20 to 30%) (27, 164, 319).
The most frequent clinical finding in the cases reported in the literature was fever, followed by splenomegaly and hepatomegaly. Of note, approximately 50% of the patients presented with pancytopenia (21, 27, 164).
Recommendations.
Routine serological screening of organ donors from areas of endemicity would not be advocated due to the lack of definitive evidence of transmission of Leishmania spp. through transplanted grafts. If an available donor serology is known to be positive, strict monitoring of the recipient in the posttransplant period rather than organ rejection would be recommended.
Prior serological data for recipients who developed leishmaniasis in the posttransplant period were not reported in the cases described. It is unclear whether the routine testing of recipients would help identify those individuals with a greater probability of developing leishmaniasis due to the reactivation of a latent infection after immunosuppression.
Infections Caused by Trypanosoma cruzi
American trypanosomiasis (Chagas’ disease) is a zoonosis produced by the protozoon Trypanosoma cruzi. The life cycle of T. cruzi involves mammalian hosts, including humans, and various insect vectors (Triatoma infestans, Rhodnius prolixus, and Panstrongylus megisutus). Vectors become infected when they ingest the blood of an infected mammal. Transmission to humans occurs when the vector's fecal matter containing the infective form of the parasite contaminates a breach in a conjunctival or mucosal surface. Once inside the host, parasites can multiply intracellularly in different tissues, invading adjacent tissues and then disseminating via the bloodstream to distant sites, where new cycles of replication are initiated (149). T. cruzi infection may also be transmitted by blood and vertically. Cases following laboratory accidents and isolated outbreaks of ingestion of contaminated food or drink have been described (83).
In the acute phase, fever is the most frequent symptom, although a proportion of patients may be completely asymptomatic. Immunosuppressed patients and children are more susceptible to developing more severe manifestations, with severe cardiac failure or encephalomyelitis, which may lead to death. The infection then progresses to an asymptomatic latent or indeterminate phase, and after several years, only a proportion of susceptible individuals (approximately 20 to 30%) develop the symptomatic chronic form of the disease, principally with cardiac and gastrointestinal involvement.
Geographic distribution.
The area where T. cruzi is endemic spans from the south of the United States to Argentina and Chile; the WHO estimates 16 to 18 million people are infected worldwide, but it is also believed the these figures may underestimate the magnitude of the problem. Approximately 45,000 of these patients die each year (64). More than 12 million immigrants from Latin America currently reside in the United States (375), and in Europe, the number of immigrants from these areas has increased significantly in recent years. In Spain alone, the immigrant population has practically doubled in the last 5 years and accounts for nearly 8% of the total population (nearly 60% coming from Latin America) (97). Due to this phenomenon, patients with Chagas’ disease are being managed by health care professionals in areas where the disease is not endemic with a greater frequency.
Diagnostic methods.
(i) Parasitological methods.
Parasitological methods are the methods of choice for the diagnosis of the infection in the acute phase, when there is a high circulating parasitemia (137). These methods include the identification of T. cruzi in Giemsa-stained thick and thin blood films or by means of concentration techniques. Among the latter, Strout's method has a sensitivity of 95% in acute Chagas’ infection, and the micromethod also has a high sensitivity and allows rapid diagnosis. A micromethod test may be negative if the parasitemic level is too low in later stages. Xenodiagnosis is available only in research centers and has the added inconvenience of being a time-consuming technique with low sensitivity (326). Blood cultures also have a low sensitivity, and a negative result does not rule out infection (137).
(ii) Serological methods.
Detection of specific antibodies is not useful in the first months of life in the case of congenitally acquired infection or in the first weeks of acute vectorially transmitted infection. These are the methods of choice, however, in the chronic phase and in the indeterminate phase of Chagas’ disease, when parasitemia is low and difficult to detect with parasitological methods. Recommended techniques are IFAT and ELISA, which have sensitivities of 99 and 98% and specificities of 99 and close to 100%, respectively (104, 362). The inconvenience of these methods is the possibility of false-positive results if there is cross-reactivity with other diseases such as Leishmania sp. infection, malaria, and syphilis (208). In immunosuppressed patients posttransplantation, discordant results using different serological techniques have been reported (5, 104, 310), and this has also been noted in patients with viral infections and AIDS. Although not specifically used in immunocompromised patients, new techniques using T. cruzi excreted-secreted antigens are under development (416) Tests based on T. cruzi excreted-secreted antigens (ELISA and WB) have shown high sensitivity and specificity in the diagnosis of acute and chronic infection by T. cruzi (373), without cross-reactivity with other diseases (341). In order to confirm infection with T. cruzi, the WHO recommends a minimum of two positive serological tests using different methods and different antigens.
Finally, there are new rapid serological tests that use recombinant proteins in an immunochromatography cassette test with high sensitivity (99%) and specificity (99%), which may be used in emergency situations such as in the hours preceding a transplant procedure (231, 296).
(iii) Molecular diagnosis.
Based on PCR techniques, molecular diagnosis procedures may have greater sensitivity and specificity than microscopy in the acute phases and allow detection of the parasite in the chronic phase, when the circulating parasitemia is low. In some studies, PCR has been found to be more sensitive than parasitological methods in the detection of reactivation in T. cruzi-infected patients undergoing cardiac transplantation (25, 237, 327). PCR may be useful in the diagnosis of infection transmitted by seropositive organ donors.
Routes of transmission.
Chagas’ disease in organ transplant recipients may occur in one of the following circumstances.
One possible route of transmission may be blood transfusions. Due to asymptomatic parasitemia, which may be maintained for many years, blood transfusions have become an important form of transmission of the disease in some areas of endemicity. The risk of transmission of the infection after transfusion of a contaminated blood unit has been estimated to be around 20% (328). The first report of transmission via an infected blood transfusion was in Brazil in 1952, and since then, there have been at least 200 declared cases in Latin America (269, 329). In 1989, a case of a renal transplant recipient who died due to acute Chagas ’ disease infection was reported. An infected blood transfusion was the suspected method of transmission (361), and a number of other cases have occurred since that report. Seroprevalence rates in blood banks have been found to vary according to different areas. Screening tests for T. cruzi are still not performed in all blood donors in some countries where this disease is endemic (328, 330), although routine screening of organ donors has been established.
In the United States, seroprevalence rates among asymptomatic blood donors vary depending on the area, with an increased rate in areas where there is a significant number of immigrants from countries where the disease is endemic. A recent publication showed seroprevalence versus T. cruzi among blood donors to be 1:7,500 and 1:9,000 in Los Angeles and Miami, respectively (225).
Since 1980, six cases of transfusion-associated Chagas’ disease in North America and Mexico have been described. All cases occurred in immunosuppressed patients, and it is thus possible that the number of cases may be underestimated, as the disease may be asymptomatic or manifest with only mild symptoms in immunocompetent patients (53, 85, 144, 209, 226). The American Red Cross recently conducted a study to evaluate an assay for detecting T. cruzi in blood donations, identifying approximately 1 in 4,650 specimens as being positive. Following that report, the FDA approved the first blood donor screening test for Chagas’ disease in the United States. Although the use of this test is not required by law, the organizations responsible for around 65% of the blood supply in the United States began screening all donations in January 2007, and it is expected that in the near future, this screening will become more widespread (75).
In Europe, only in certain countries are all donors questioned to determine the risk of T. cruzi infection (306), although legislation regarding donor selection criteria is currently changing. In Spain, blood donors with Chagas’ disease are permanently excluded from blood donation. Potential donors born in areas of endemicity or whose mothers were born in such areas as well as patients who have received blood transfusions in at-risk countries are also excluded unless a screening test is found to be negative. In Spain, two cases of infection following a contaminated transfusion have been described (123, 382). Villalba et al. reported the first fatal case of acute Chagas’ disease in Europe, where the donor was identified retrospectively, as the recipient developed a reactivation of Chagas’ disease following a cord blood transplant (382).
Another possibility is reactivation of latent infection. Immunosuppression in the posttransplant period may lead to the reactivation of Chagas’ disease in a previously infected patient. Strictly speaking, this would actually represent acute invasion of a disease-free graft with dissemination in a patient who is already infected, but in the literature and in practical terms, these are defined as cases of reactivation.
A third possible route of transmission is the de novo acquisition of the infection with an increased risk due to the situation of immune suppression.
Transplant-related cases.
The majority of cases of T. cruzi infection in transplant patients have been described in Latin America, where a positive serology in a donor does not necessarily contraindicate donation (except in the case of cardiac transplantation) due to organ shortage and the high prevalence of the disease.
A retrospective study in 2006 in the south of California, an area with a large immigrant population, examined the prevalence of T. cruzi antibodies in a population of organ donors. A male donor was found to be positive, and the authorities were notified, but data regarding the recipients have not been published (269). In a similar study in a different area of the United States, no seropositive donors were found in a period of 6 years (50). Based on these findings, it would seem that serological screening of potential donors could be beneficial, especially in areas where there is a high frequency of donors from countries where the disease is endemic.
(i) Reactivation.
Reactivation does not occur in all Chagas’ disease patients who undergo immunosuppression; it is possible that this may be influenced by the intrinsic characteristics of the particular infecting strain, as has been demonstrated in animal models (289).
(a) Cardiac transplantation. Reactivation is more frequent than transmission, especially in those patients infected with T. cruzi who undergo cardiac transplantation because of chagasic cardiomyopathy. Reactivation of Chagas’ disease following cardiac transplantation has been estimated to occur in up to 20 to 30% of patients (25, 28), although some authors reported much higher rates. Reactivation is higher during the first year after surgery, when immunosuppression is more intense (363). A significant proportion of patients do not have acute myocarditis as a manifestation of reactivation, and therefore, a high index of suspicion is necessary in order to initiate diagnostic tests (28). Some patients will go on to develop severe symptoms (208).
There has been some controversy as to whether patients with chagasic cardiomyopathy should be candidates for heart transplantation due to the possibility of reactivation and the increased incidence and severity of rejection episodes associated with active myocarditis. The higher rates of reactivation and myocarditis reported following heart transplantation may be related to the degree of immunosuppression used (38, 119), and outcomes also vary according to different series (39, 96). There are also conflicting results regarding the influence of pre- and posttransplantation treatment with benznidazole on outcomes in these patients (96, 119).
(b) Renal transplantation. Reactivation has also been described in renal transplant patients in association with the use of immunosuppression, although manifestations are usually less severe. Two descriptive series from transplant centers in Argentina that examined the outcome of renal transplants in seropositive patients found a rate of reactivation of 21.7 and 37% (55, 310). There were no acute manifestations of the disease, and all patients responded well to benznidazole treatment.
(ii) Transmission via graft.
It is difficult to estimate the potential risk of transmission of T. cruzi in transplant patients. According to some authors, the rate of transmission is estimated to be around 35% when infected renal grafts are used in seronegative patients (19). For other types of transplantation, consistent figures are not available due to the decreased number of cases.
(a) Renal transplantation. In patients who receive renal transplants from seropositive donors, the rate of transmission does not appear to be high, and if transmission occurs, patients do not tend to have severe complications as demonstrated in the main publications.
Out of 234 renal transplants performed at a specific unit in Buenos Aires, Argentina, over a period of 7 years (1989 to 1996), 16 were from seropositive donors. In only three cases (18.7%) was infection diagnosed in the recipient by finding asymptomatic parasitemia. All three patients received specific treatment: in one patient, parasitemia was undetectable following treatment, another progressed to the indeterminate phase, and the third patient developed acute Chagas’ disease after immunosuppression was intensified due to an episode of chronic rejection (310).
In a series of 239 renal transplant patients studied in Brazil between 1992 and 1997, 9 seronegative recipients received an organ from a seropositive donor. All recipients received benznidazole for 14 days starting on the first day posttransplantation. After a 10-year follow-up period, none of the patients developed acute illness or seroconverted. The conclusions reached by those authors were that due to organ shortage, donors with serologies positive for Chagas’ disease should not necessarily be rejected (345).
Another series monitored the outcomes of 26 patients who received renal grafts from seropositive patients. Two patients developed asymptomatic parasitemia 15 and 45 days posttransplantation, respectively, and one patient developed acute infection 145 days posttransplant, with fever and hepatosplenomegaly. All three responded to specific treatment (55).
In another report, for nine patients who received grafts from seropositive donors (eight renal graft and one liver graft), parasitemia was detected in only two patients in the posttransplant period without any accompanying symptoms. In one of the cases, results became negative after specific treatment with nifurtimox, and in the other, infection persisted despite therapy first with nifurtimox and then with benznidazole, progressing to an indeterminate phase (380).
(b) Liver transplantation. A recent publication described a case where a liver graft was accepted from a donor infected with T. cruzi in an emergency situation. The patient was strictly monitored, and asymptomatic parasitemia was detected by parasitological (Strout's method) and serological methods 84 days posttransplantation. Treatment was commenced with benznidazole, with rapid elimination of parasitemia. Those authors recommended that T. cruzi-infected grafts should be used only in emergency situations (19). However, another article published in 2007 identified six patients who received a liver graft from donors who were seropositive for Chagas’ disease at a specific unit during the period of 2000 to 2005: all but one of the patients (because of drug intolerance) received prophylactic benznidazole treatment for 60 days following transplantation. Four of the patients had a favorable outcome, maintaining negative serology. Two patients died: one of them due to biliary sepsis 6 months following transplantation and the other from complications secondary to pulmonary tuberculosis. Both had negative serology for Chagas’ disease. Based on the results, those authors maintain that the use of liver grafts from patients who were seropositive for Chagas’ disease followed by prophylactic treatment with benznidazole may be a feasible therapeutic option for patients with severe liver disease (93).
(c) Multiorgan transplantation. The first cases of transplant-associated Chagas’ disease in the United States were reported in 2001. The donor was an immigrant from Central America presumed to be infected with T. cruzi for whom no specific screening tests for Chagas’ disease were performed. Parasitemia was detected in all recipients. The patient who received one of the kidneys and pancreas developed acute infection 10 days after transplantation, dying from chagasic myocarditis in spite of treatment with nifurtimox for 4 months. The recipient of the other kidney was also treated for 4 months with the same drug, achieving a negative parasitemia with no further recurrences. The liver recipient died from sepsis that was unrelated to the infection with T. cruzi (64).
In 2006, two cases of acute Chagas’ disease in heart transplant recipients were communicated to the authorities (73). In the first case, T. cruzi was detected in a blood smear, blood cultures, and endomyocardial biopsy 1 month posttransplantation. Serology was negative, but PCR was positive, as would be expected in an acute infection. After nifurtimox treatment, parasitemia was eliminated, but 3 months posttransplant, the patient died due to acute rejection. The donor's blood tested positive when analyzed retrospectively. In the liver and kidney recipients from the same donor, no transmission was detected. Regarding the second case, parasites were detected 1 month posttransplantation in blood films and blood cultures, and PCR was positive. The patient improved with nifurtimox treatment. Myocardial biopsies and serology were negative. The patient died months later due to cardiac failure. The donors of the transfusions used during the transplantation procedure were found to be negative for T. cruzi, but the organ donor tested positive. The other three recipients from the same donor were not infected. Those two cases represented the fourth and fifth cases of T. cruzi transmission following SOT in the United States. Nifurtimox was used in both cases, as benznidazole is currently not commercially available in the United States (73).
In summary, the transmission of Chagas’ disease during transplantation, especially if the heart is transplanted, has been documented. Early diagnosis and initiation of specific therapy are necessary to prevent complications.
Recommendations.
The cases described highlight the need for screening protocols for potential donors from countries where the disease is endemic. Chagas’ disease is the main protozoal infection that may be transmitted through organ transplantation from Latin Americans and should therefore be ruled out in all donors who have resided in these areas. The use of serological tests for T. cruzi would be mandatory for these donors. Two positive results using different serological techniques are necessary to consider a patient to be infected. Before deciding on transplantation, a comprehensive study of the donor should be performed: if the cause of death is deemed to be acute Chagas’ disease, the donor should be excluded.
In the case of cardiac transplantation, the use of a heart from a patient with chronic infection is an absolute contraindication given the risk of development of chagasic myocarditis during the period of immune suppression.
There is no consensus on the possible use of other organs from infected patients. In Latin America, this is common practice; transmission of the infection via a renal graft does not occur in the majority of patients, and when transmission does occur, the infection can be managed with specific treatment.
If an organ from an infected donor is transplanted, close follow-up with serological and parasitological methods starting in the first week posttransplantation and performed weekly for the first month, fortnightly for the next 3 months, and monthly thereafter are recommended (5, 104, 310). Immediate treatment with benznidazole for 30 to 60 days or nifurtimox for 90 to 120 days should be started upon finding evidence of infection.
Use of prophylactic treatment is indicated for patients with chagasic cardiomyopathy who undergo cardiac transplantation from a healthy donor to prevent disease reactivation, which is more frequent and may be more severe than for other types of transplant (96). In other recipients, early treatment would be recommended if there is evidence of reactivation.
Infections Caused by Strongyloides stercoralis
Strongyloidiasis is caused by the nematode Strongyloides stercoralis. It is the fourth most important intestinal nematode infection in the world. S. stercoralis infection in humans usually produces an asymptomatic chronic disease of the gastrointestinal tract that can remain undetected for several decades. However, in immunocompromised patients, especially those receiving corticosteroids, hyperinfection can develop, with dissemination of larvae to extraintestinal organs and resulting mortality rates as high as 85%.
Geographic distribution.
S. stercoralis has a nonuniform distribution throughout the world in the tropics and other areas with warm and humid climates, mainly in Southeast Asia, sub-Saharan Africa, Brazil (where prevalence rates are close to 60%), and the southern United States (149). There are an estimated 90 million people infected in the world (284).
Diagnostic methods.
Diagnosis is obtained following the visualization of larvae in stool and with larval culture (351). Examination of several samples is recommended, as the diagnostic yield of a single sample is low. The use of special microbiological techniques such as Harada-Mori, Baerman, or larval culture in agar medium with coliforms increases the sensitivity of diagnosis. In cases of hyperinfestation, the yield may be higher due to the increased parasitic load. Other diagnostic methods include the detection of the parasite in other samples. Serological tests have a low sensitivity in posttransplant patients due to immune suppression.
Routes of transmission.
Humans contract S. stercoralis infection when larvae from contaminated soil penetrate skin or mucous membranes. This parasite differs from other intestinal nematodes because of its capacity for replication inside the human host, which allows the perpetuation of autoinfection cycles by the production of larval forms within the infected organism. S. stercoralis infection may persist for decades in this way without any further exposure of the host to exterior infectious larvae (146, 228).
Posttransplant strongyloidiasis may develop after primary infection, by autoinfection, or by transmission via graft.
Transplant-related cases.
Various cases in renal and heart transplant recipients and, more recently, following pancreatic transplantation have been reported. In the majority of cases, symptoms of strongyloidiasis developed in the first 6 months following transplantation (103, 257, 351).
Even though S. stercoralis is an intestinal nematode, there are references in the literature to possible transmission during renal transplantation. Those observations are based on the possibility of transmission of existing latent larval forms in the kidney. Although the adult worm lives in the gastrointestinal tract, larval forms have been observed in urine as well as in inflammatory lesions in the kidneys of patients infected with S. stercoralis (278). Cases that suggest direct transmission via the graft are scarce; to our knowledge, there are two cases related to renal transplantation (179, 278). In 2005, a case of S. stercoralis transmitted through an infected pancreas was described. The patient developed fever and gastrointestinal and respiratory symptoms 5 weeks posttransplantation. Rhabditiform larvae and sections of the adult helminth were observed in a duodenal biopsy. After retrospective analysis of the donor's serum, a positive IgG ELISA result for S. stercoralis was found. Other organ recipients from the same donor were not found to be infected (26).
Another situation that has been well described in transplant patients, not related to transmission via the organ but related to prior infection of the recipient, is hyperinfestation syndrome (113, 187, 247, 257, 284, 325, 379, 381, 398). This is due to an accelerated autoinfection cycle almost always associated with immune suppression (especially suppression of T-lymphocyte activity). In hyperinfestation syndrome, intestinal ulceration favors the development of bacteremia due to gram-negative bacilli or other bacteria from the intestinal flora with a high associated morbidity (2).
Recommendations.
Widespread donor screening is not considered to be necessary, and current recommendations should be applied to organ recipients in areas of endemicity. Diagnostic tests to exclude S. stercoralis should be performed during the pretransplant evaluation in patients who have resided in or traveled to zones of endemicity, and specific treatment should be recommended prior to transplantation (220).
Infections Caused by Filariae
Filariae are a group of tissue-based nematodes that can grow in subcutaneous tissue and lymphatic vessels. There are eight species of filariae that usually infect humans, and of these, four (Wuchereria bancrofti, Brugia malayi, Onchocerca volvulus, and Loa loa) cause the most severe infections (268).
Geographic distribution.
Due to their worldwide distribution, these filariae are known to be an important health problem, especially in tropical and developing countries, affecting an estimated 170 million people (172, 244, 276).
Diagnostic methods.
Lysis-centrifugation of peripheral blood and Giemsa staining as well as identification of filariae in “skin snips” are methods used for diagnosis. Antigen detection techniques, WB, serology, and PCR are also available (149).
Routes of transmission.
Filariae have complex life cycles that include arthropods as vectors. They are transmitted by specific species of Diptera and have a life cycle that includes an infectious larval phase transmitted by insects and an adult worm that remains in the human lymphatic or subcutaneous tissues. Adult forms give rise to microfilariae, which, depending on the species, circulate in the blood or migrate through the skin or subcutaneous tissues. To complete their life cycle, microfilariae need to be ingested by the arthropod vector and develop into new infectious larvae in the space of 1 or 2 weeks. Adult worms live for many years, whereas microfilariae survive between 3 and 36 months.
W. bancrofti microfilariae reside in the lung, renal and heart capillaries, and some of the main arteries during the day, appearing periodically in the bloodstream during the night. Microfilariae in the glomerular capillaries do not tend to produce specific lesions directly; these occur as a result of the inflammatory response to the degenerating parasites.
Transplant-related cases.
Transmission of W. bancrofti via the placenta and through infected blood transfusions has been previously described (9, 340). There is only one documented case of possible transmission of microfilariae of W. bancrofti via a living-donor renal transplant (151), where both donor and recipient were from an area of endemicity. The perioperative biopsy revealed microfilariae and eosinophils in the glomerular and peritubular capillaries. Antifilarial treatment was added to the immunosuppressive regimen for 3 weeks, with a favorable outcome. Microfilariae transmitted in this way would not produce filariasis because the vector stage is absent, and the symptoms of lymphatic filariasis are caused by the adult form in the lymphatic capillaries. Only the microfilariae capable of microfilaremias, which eventually die, but not the larvae capable of developing into the adult form are transplanted.
Recommendations.
There are no special recommendations for donors from countries where the disease is endemic, but if there is a high index of suspicion clinically, peripheral blood smears could be screened, and the donor could be treated prior to transplantation if results are positive.
Infections Caused by Echinococcus spp.
Echinococcosis is the infection caused by the larval stage of Echinococcus spp. There are four main species that may affect humans. In order of frequency, these are Echinococcus granulosus (cystic echinococcosis/hydatid disease), Echinococcus multilocularis (multilocular or alveolar echinococcosis), Echinococcus vogeli, and Echinococcus oligarthrus (polycystic echinococcosis).
Geographic distribution.
E. granulosus has a worldwide distribution, although it is more frequent in rural areas where dogs may eat offal from livestock, which contain cysts in their tissues. The areas of highest prevalence are the coastal areas of the Mediterranean, South America, southern areas of Russia, Central Asia, China, Australia, and some areas of Africa. In the United States, the majority of cases are due to imported infections.
E. multilocularis infection is frequent in the Northern hemisphere, mainly in Central Europe, Russia, Central Asia, North America (especially in hunters in Canada and Alaska), and West China. E. vogeli infection occurs mainly in Central and South America (Colombia, Venezuela, Brazil, and Panama).
Diagnostic methods.
Serology may be useful for confirming a radiological diagnosis but may be problematic since there may be a significant proportion of false-positive and false-negative results. Cysts that are found in liver or bone tend to produce a positive serology with greater frequency than those located in lung, brain, or spleen. Calcified cysts or those with an intact capsule may be associated with negative serology. Serology would not be useful in the follow-up of patients treated medically or surgically, as antibodies may persist for a long time despite treatment.
Indirect hemagglutination assay (IHA), IFAT, and ELISA are the serological tests most commonly used for the detection of E. granulosus. Titers of >1/64 in the IHA tests have a sensitivity greater than 95%, although another immunoblot or ID test would be necessary for the detection of Arc-5. The detection of specific IgG subclasses and, in particular, the detection of IgG1 and IgG4 by ELISA have a sensitivity higher than 80%. Detection of IgG4 is also of value in the follow-up after surgery.
For alveolar echinococcosis, serological tests tend to be positive at elevated titers, and purified antigens are highly specific. Serological tests are not always of value for the diagnosis of E. vogeli (149).
Routes of transmission.
The tenia of E. granulosus remains localized in the small intestine of the definitive host, most frequently the dog, although other canines can be affected. Humans act as an intermediate host, with disease being localized most frequently in liver (65 to 75%), lung (25%), spleen, kidneys, heart, bone, and CNS, among others. If dogs ingest these tissues (offal from infected cattle), the proglottid evaginates and gives rise to the adult form in the small intestine in 30 to 80 days.
E. multilocularis has a life cycle that is similar to that of E. granulosus, with the main difference being that the larvae of E. multilocularis remain in the proliferative phase indefinitely, thus producing a slow and progressive invasion of adjacent tissues and a greater degree of destruction, as a limiting cyst is not formed. The disease affects mainly the liver and occasionally the lung and CNS.
E. vogeli may also affect humans, producing cystic disease in specific tissues.
Transplant-related cases.
(i) Infections caused by E. granulosus (cystic echinococcosis).
Cases of hydatidosis in organ recipients arising from transmission from an infected donor are extremely rare. A case of a transplant patient who received a liver with an isolated calcified cyst that was resected prior to transplantation has been reported. In the recipient, there was no evidence of regrowth of the cyst or positive serology in the posttransplant period (196). Another case, where a liver containing a calcified cyst of E. granulosus was used, has also been reported (23).
A study carried out in Spain examined the outcomes for patients undergoing liver transplantation due to complicated hydatidosis with extensive hepatic involvement and a history of previous surgery. Four patients were still alive after 37 to 65 months of follow-up, five patients had a recurrence of the infection, and another two patients died due to other complications (pulmonary embolus and a cerebrovascular event) (256).
(ii) Infections caused by E. multilocularis (alveolar echinococcosis).
There are no cases described where the organs from a patient infected with alveolar echinococcosis have been used for transplantation.
However, there are a number of studies that documented the outcomes for patients receiving a liver transplant because of advanced alveolar echinococcosis (45-47, 211). A multicenter study performed in Europe showed an overall survival rate of 71% at 5 years, and in 58% of patients, there were no documented recurrences (211).
Recommendations.
(i) Cystic echinococcosis.
The finding of an image suggestive of a hydatid cyst in a patient from an area of endemicity should raise suspicion of the diagnosis and should be confirmed with serology. If a patient has negative serology and a suspicious lesion on imaging, puncture and aspiration of the lesion should be performed in order to obtain a definitive diagnosis.
An organ infected with hydatid cysts should not be used for transplantation unless the cyst is localized, inactive, and calcified, permitting radical excision prior to transplantation (196). If there is isolated hepatic involvement, other organs may be used if a computed tomography (CT) scan rules out extensive disease.
(ii) Alveolar echinococcosis.
In alveolar echinococcosis, the affected organ cannot be used, as it is infiltrated by the disease. There are no reported cases of donors infected with E. multilocularis, but should the situation arise, an infected organ should not be used in transplantation, and a CT scan should be performed to search for disease at other sites (311).
In conclusion, a patient with hydatidosis may donate only organs that are not infected unless the cyst is localized and inactive. A study of disease extension should be performed, and if there is no evidence of disease, the organ may be transplanted. It is extremely rare for a donor to be infected by E. multilocularis, but if this occurs, the infected organ cannot be used for transplantation, and disease at other sites, mainly pulmonary sites and CNS, should be ruled out.
Infections Caused by Trematodes
Clinically relevant trematodes include Schistosoma spp. (S. haematobium, S. mansoni, S. japonicum, S. intercalatum, and S. mekongi), Fasciola spp., Clonorchis spp., Opistorchis spp., and Paragonimus spp.
Geographic distribution.
The distribution of various species of Schistosoma is widespread: S. haematobium, S. intercalatum, and S. mansoni are endemic in sub-Saharan Africa, and the latter is also found in Brazil, Venezuela, and certain areas of the Caribbean. S. japonicum occurs mainly in China, Indonesia, and the Philippines, and S. mekongi is present in Cambodia and Laos. Different organs may be involved: S. mansoni and S. japonicum involve the liver, and S. haematobium involves mainly the urinary tract and the kidney.
Fasciola spp. are endemic in Europe, East Asia, South Africa, North and South America, the Caribbean, and Australia. The infection affects mainly the liver and bile ducts.
Clonorchis sinensis is present in China, Taiwan, Korea, and Japan. Opistorchis spp. are endemic in Eastern Europe, countries of the former Soviet Union, India, and Thailand. Both parasites infect the liver and bile ducts.
More than 40 species of Paragonimus have been described, only 8 of which are important in humans: of these, Paragonimus westermanii is the most well known. It is found in Japan, India, certain islands of the Pacific, West and Central Africa, and South and Central America. Pulmonary involvement is common, with extrapulmonary manifestations occurring only rarely.
Diagnostic methods.
Specific diagnoses of intestinal and hepatic trematodiases (Clonorchis spp. and Opistorchis spp.) and intestinal schistosomiases (S. mansoni, S. japonicum, and S. intercalatum) are made after direct visualization of the parasite's ova in feces. Paragonimiasis is diagnosed after direct visualization of ova in sputum and stool specimens. In the case of genitourinary schistosomiasis (S. haematobium), ova can be visualized in urine specimens.
Existing ELISA and IHA techniques for the detection of antibodies against Schistosoma spp. have low sensitivity and specificity (318, 352). Certain ELISAs may detect specific IgG against Paragonimus spp. and Fasciola spp. in serum as well as pleural fluid in the case of Paragonimus spp. New PCR techniques for the diagnosis of Opistorchis spp., which would have a sensitivity and specificity close to 100% without the risk of false-positive results, are under development. Imaging techniques may also be useful diagnostic tools.
Routes of transmission.
The life cycles of these parasites are complex and include several animals and humans as the definitive hosts, with a variety of intermediate hosts. Ova produced in the adult host are eliminated in urine, feces, or sputum and fall into water. Following a series of transformations including some in the intermediate host, they can invade the definitive host, thus completing the cycle. They are ingested by humans in the form of contaminated freshwater fish (Clonorchis spp. and Opistorchis spp.), raw fish or crustaceans (Paragonimus spp.), or aquatic plants (Fasciola spp.). Schistosomiasis is acquired by penetration of the skin by the parasite during contact with contaminated freshwater.
Transplant-related cases.
(i) Schistosoma spp.
Isolated cases of transmission of Schistosoma through transplantation have been described: four cases where an infected liver was used in transplantation have been identified. In these cases, there was no previous history of hepatic disease or abnormalities in the donor's liver function tests. In the first report, S. mansoni ova and granulomas were detected in the perioperative biopsy of the graft. The recipient was treated with praziquantel with a favorable outcome and with no evidence of infection due to Schistosoma in biopsies performed 6 months posttransplantation (279). In the second publication, three patients who received grafts infected with S. mansoni (detected in the perioperative biopsy) were identified. The donors were originally from Puerto Rico, an area where S. mansoni is endemic. All patients did well with praziquantel treatment (300).
Although only a few cases have been identified, the authors of those studies concluded that schistosomiasis infection in the donor does not seem to condition an adverse clinical outcome in the patient or of the graft when recipients are treated correctly. Broadening the differential diagnosis upon finding granulomas in the perioperative liver biopsies to rule out more unusual infections, which may present subclinically in the donor, would be important.
There are two recent publications that described schistosomiasis infection in the posttransplant period. These patients were originally from areas of endemicity, and the most probable mechanism was reactivation of a prior infection secondary to immune suppression (in particular due to cellular immunity). Those authors recommended the examination of stool specimens for parasites as well as performing serology in the pretransplant work-up of patients from at-risk areas (171).
Various articles analyzed the repercussions of previous infection with Schistosoma spp. on the outcome of transplantation. Infected live donors and renal transplant recipients received antischistosomal therapy prior to transplantation. In spite of an increased number of local complications such as urinary tract infections and ureteral stenoses, infection with Schistosoma spp. was not considered a contraindication for transplantation in these studies. An increase in acute and chronic rejection was not observed either. Infected patients (both live donors and recipients) should be diagnosed and treated correctly with praziquantel before transplantation (236).
(ii) Clonorchis spp.
Six cases where a liver graft infected with Clonorchis spp. has been transplanted have been described (169, 185, 222, 411). In four of the cases, in the donors’ preoperative studies, abnormalities of the bile ducts were found on CT scanning, and ova of Clonorchis spp. were identified in stool samples (185). In one of the cases, the preoperative study was normal, but during the surgery, minimal bile duct inflammation was observed (222). Parasites were identified in the bile ducts in all cases, and intraoperative irrigation of the ducts was performed. Treatment with praziquantel was administered in three of the cases: in two of these cases, it was given to the donor pretransplant (185, 222), and in the other case, it was given to the donor and recipient in the posttransplant period (222).
Of the two patients reported by Yeung et al. who did not receive treatment, one developed early postoperative blockage of the hepaticojejunostomy splint (411). In none of the cases was Clonorchis spp. identified in the samples in subsequent controls, and no abnormalities of liver function were observed. The assumption was made that mechanical irrigation and cold perfusion of the graft must have been sufficient to kill the parasites. However, specific antihelminthic therapy used in the preoperative period may serve to reduce the risk of local complications.
(iii) Other species
No cases in association with Fasciola spp. or Paragonimus spp. have been described.
Recommendations.
The use of diagnostic tests in all donors from areas of endemicity would be recommended, especially in the presence of peripheral blood eosinophilia. Screening tests should include the examination of stool, urine, or sputum for ova depending on the species. A positive finding would not necessarily contraindicate transplantation, but specific treatment should be administered and cases should be closely monitored due to the risk of possible long-term complications. If a recipient is found to be infected, treatment should be given prior to transplantation.
Other Parasitic Infections
Infections caused by Babesia spp.
Human babesiosis is caused by intraerythrocytic infection by parasites from the genus Babesia that are transmitted following the bite of an infected Ixodes tick. Babesia sp. infection may persist as a chronic infection for many years.
The infection has a worldwide distribution, but the majority of cases of babesiosis have been described in the temperate zones of the United States and Europe, even though isolated cases have also been described in China, Taiwan, Egypt, South Africa, Mexico, and, more recently, India (149, 175, 241).
Babesia microti has been found most frequently in human cases from the United States, although recently, other species of Babesia (types WA1, CA1, and MO1) have also been described (142, 165, 290). In Europe, Babesia infections are caused mainly by Babesia divergens (142). The majority of cases described occurred in splenectomized patients (166).
Clinical manifestations of human babesiosis are varied and seem to be directly related to the level of circulating parasites. Complications arise most frequently in immunosuppressed patients, those with advanced age, or those who have undergone splenectomy.
In general, in order to make a diagnosis, a high index of suspicion is needed for patients with specific clinical symptoms who have a history of having stayed in areas of endemicity, have a history of tick bites or exposure to ticks, have received a recent blood transfusion, or have undergone splenectomy. Definitive diagnosis is obtained after the parasites are demonstrated inside red blood cells in a Giemsa-stained peripheral blood film. Serological tests, mainly the measurement of antibodies by indirect immunofluorescence (IFAT), have been demonstrated to be both specific and sensitive for the diagnosis of B. microti infection, especially in chronic infections (84), but the persistence of antibodies does not necessarily reflect active infection, and the possibility of false-positive and false-negative results may occur (290).
PCR techniques for the detection of B. microti and B. divergens are currently in use (272, 291) but tend to be readily available only in specialized centers.
Several cases of transfusion-associated babesiosis have been described, mainly in the United States (to the authors’ knowledge, none were from Europe) (167).
To date, only four cases of B. microti infection have been described in the context of SOT, and in all of those cases, the mechanism of transmission was attributed to a transfusion of infected blood at the time of transplantation (150, 232, 288, 344). Three cases occurred in renal transplant patients, and one occurred following a heart transplant. Two of the renal transplant patients were splenectomized, and the infection presented as a hemophagocytic syndrome.
In the United States, current strategies for the prevention of transfusion-associated babesiosis are limited to the use of questionnaires regarding possible risk factors or exposure and the exclusion of patients with acute illnesses or fever. No tests are used for the routine screening of donors for tick-borne diseases. In Europe, specific serological tests for the screening of asymptomatic blood or organ donors are not performed either (306).
Babesiosis in organ transplant recipients has not been transmitted by infected grafts, and screening for this infection in organ donors is not considered to be necessary.
Infections caused by Entamoeba histolytica (amebiasis).
Entamoeba histolytica produces a protozoal infection known as amebiasis, which is one of the main pathogenic causes of dysentery in the world. Although its distribution is worldwide, it occurs mainly in areas of Central and South America, Africa, and the Indian subcontinent (149). Infection may be asymptomatic but can also cause dysentery and extraintestinal disease, characteristically with the formation of hepatic abscesses (156).
The most widely used method for the diagnosis of intestinal amebiasis, especially in developing countries, is examination of feces by microscopy to search for cysts or trophozoites. However, the sensitivity of the test is low (only 30 to 50%), and there may be false-positive results. Detection of fecal antigen or specific E. histolytica DNA with PCR has improved sensitivity (up to 90%) in symptomatic patients (157). ELISA or IFAT serological tests may aid diagnosis. During the acute phase of the infection, these tests may have a sensitivity of 70% in the case of amebic colitis, between 70 and 80% in the case of hepatic amebic abscesses, and greater than 90% in the convalescent period (156). However, the test may remain positive for years and does not allow discrimination between current and past infections. A seroprevalence of 10 to 30% has been found in asymptomatic residents in developing countries.
Infection with E. histolytica occurs when the cystic forms are ingested through food or water that has been contaminated with fecal matter. Cysts divide in the intestine, giving rise to trophozoites, which have the ability to invade the intestinal mucosa and reach the liver by migration through the portal vein.
Only a few cases have been reported for solid-organ recipients (277). There have been no documented cases of transmission of E. histolytica directly via an infected graft, although this could theoretically occur in liver and intestinal transplants.
Screening tests are not routinely necessary for the prevention of transmission of E. histolytica during transplantation. Serological tests in donors would probably not be adequate, as seroprevalence rates are high in developing countries (149), and this could lead to an increase in organ loss.
Infections caused by free-living amebae.
There are several species of free-living amebae that exist in nature, and of these amebae, Naegleria fowleri, several species of Acanthamoeba, and Balamuthia mandrillaris are known to cause disease in humans. More recently, the first case of human infection due to Sappinia diploidea was identified (132). These organisms are widely distributed in the environment, but they occur mainly where there is freshwater (rivers, streams, lakes, swimming pools, and water treatment systems).
Infection by N. fowleri is produced when the ameba invades the CNS via the olfactory neuroepithelium; Acanthamoeba sp. and B. mandrillaris infections occur after the organism penetrates the olfactory or corneal neuroepithelium (332). Cases peak in the summer months, when more freshwater activities are practiced (149).
N. fowleri produces an acute, fulminant, and frequently lethal disease known as primary amebic meningoencephalitis, which tends to affect patients with recent involvement in water-related sports or activities. Acanthamoeba spp. may cause amebic keratitis in immunocompetent patients, but in addition, Acanthamoeba spp. and Balamuthia mandrillaris may produce an insidious disease of the CNS known as granulomatous amebic encephalitis (GAE), which tends to affect HIV-infected or immunosuppressed patients posttransplantation. This has a worldwide distribution. Cases of extracerebral Acanthamoeba disease produced by dissemination via the bloodstream have been described (234, 347).
Obtaining a diagnosis may prove difficult and requires a high index of suspicion. The majority of cases have been described postmortem. Naegleria trophozoites may be visualized by direct microscopy of a CSF sample, but Acanthamoeba and Balamuthia cannot be detected by this method and require histopathological confirmation in a brain biopsy in the case of encephalitis or in another tissue sample in the case of disseminated infection (149). Currently, there are no serological tests that contribute to the diagnostic procedure. Recently, a new triplex PCR technique that would allow the simultaneous identification of Acanthamoeba spp., B. mandrillaris, and N. fowleri with a high specificity and with a reduced timeframe has been developed (302).
A case where the donor died due to amebic meningoencephalitis secondary to N. fowleri has been described, and the disease was diagnosed postmortem, when organ donation had already occurred (liver and kidneys). The recipients did not receive specific prophylaxis, and there was no evidence of Naegleria infection in any of them, possibly because the donor's infection was limited to the CNS (213). Another unpublished case exists where a kidney donor died before Naegleria infection was diagnosed, but data on the outcome in the recipients are unavailable (CDC, unpublished). The risk of transmission of Naegleria through organ donation is unknown.
There is no evidence of Acanthamoeba transmission through SOT, possibly because patients who die due to encephalitis are generally rejected as potential organ donors. There is a case of B. mandrillaris infection described in a series documenting opportunistic infections in the posttransplant period (287).
Transmission of free-living amebas in the context of organ transplantation is an unusual phenomenon; specific tests to rule out these infections would be unnecessary. Until new PCR techniques become readily available, there will be no fast, reliable, or practical test available to exclude these amebic infections in transplant candidates, and currently, no prophylactic treatment regimens have been established.
Infections caused by Trypanosoma brucei.
Human African trypanosomiasis, or sleeping sickness, is caused by Trypanosoma brucei gambiense (West and Central Africa) or Trypanosoma brucei rhodesiense (East Africa) and is transmitted by the bite of an infected tsetse fly (genus Glossina) (218). There are few reports of cases outside tropical Africa, but it is possible that these reports may increase in the future due to the increase in international travel and migration, as reflected by the recent reports of tourists visiting national parks in Tanzania (41).
In the initial phase, the parasites may be detected in the bloodstream or in lymph nodes, and a patient infected by Trypanosoma brucei gambiense may be asymptomatic and may then progress to a late phase with CNS involvement, when the trypanosomes may be detected in CSF. Based on this cycle, isolated cases of transmission via a transfusion of infected blood have been described (168).
There have been no described cases of transmission of human African trypanosomiasis through solid-organ or bone marrow transplantation. It is possible that this may reflect the reduced number of transplants carried out in countries where the disease is endemic and the limited reporting of the infection (385). Due to the severe prognosis of this disease and the toxicity of the treatment, organs coming from a known infected donor should be rejected. There are no specific recommendations of serological or parasitological screening for donors from areas of endemicity. No specific precautions would be required in organ donors.
Infections caused by Taenia solium (cysticercosis).
Human cysticercosis is a parasitic infection produced by the larval stage of the cestode Taenia solium. The clinical presentation, pathogenesis, management, and prognosis of T. solium infections vary depending on the location and number of cysticerci and the associated host response (149).
The infection has a worldwide distribution, predominating in areas where there is porcine livestock, and because of this, it is rare in Islamic countries. The disease has a greater incidence in developing countries and is endemic in parts of Asia, Africa, and Latin America, where it is a common cause of late-onset seizures. In recent years, an increase in the number of cases has been observed in developed countries especially if there is a large immigrant population and also as a consequence of increasing travel to high-prevalence areas (11, 59, 118, 122, 195, 360, 397).
To establish a diagnosis of cysticercosis, epidemiological and clinical data as well as results of serological and imaging tests should be taken into account. Epidemiological data may be unclear, as affected patients may remain asymptomatic for long periods of time, presenting late with symptoms, as is often the case in neurocysticercosis. A set of revised criteria for the diagnosis of human cysticercosis has been published elsewhere (98).
Serology may be positive in up to 8 to 12% of patients living in areas of endemicity and may reflect exposure rather than infection (58). The most widely accepted serological technique is immunoblot/WB, which utilizes purified antigens from the larval/cysticercal phase (130). Antibody detection by ELISA has lower sensitivity and specificity. The sensitivity of these tests may decrease if cysts are calcified or if they are scarce in number, so a negative serology does not rule out infection. Cross-reactivity with other parasitic infections (mainly Echinococcus spp.) is also possible.
Infection is caused after ova eliminated in the feces of patients who carry the adult helminth in the intestine are ingested and occasionally through a process of autoinfection. After ingestion, dissemination via the bloodstream occurs and may remain localized in its cystic form in skeletal muscle, subcutaneous or ocular tissue, brain, or bone marrow. If the larval form is ingested after eating poorly cooked pork that is infected with the cyst, evagination of the cyst will give rise to adult T. solium, which remains in the small intestine (129).
Only a few transplant-related cases have been described. A case of a cadaveric renal transplant recipient who developed neurocysticercosis in the posttransplant period has been reported (141). More recently, another case of neurocysticercosis developing 1 month after liver transplantation (the first case related to hepatic transplantation) was reported (170). Both cases may have resulted from the reactivation of previously asymptomatic lesions in the context of immune suppression, as both patients had resided in areas of endemicity.
Given that the cysts occur only in the central nervous, ocular, and subcutaneous tissues or skeletal muscle, the transmission to an organ recipient would be extremely rare, as these are nontransplantable organs. Cysts may arise in cardiac muscle and theoretically may be transmitted during a heart transplant procedure (87, 301, 320).
If the donor is from an area of endemicity or has clinical symptoms or signs suggesting cysticercosis, serological screening tests (immunoblot) may be performed, bearing in mind the possibility of false-positive and false-negative results.
An imaging technique of the donor organ in the case of the heart may be performed, which, together with negative serology, should rule out infection of the organ. The use of organs from a patient with neurocysticercosis would not be contraindicated.
CONCLUSIONS
The generosity and altruism of organ donation have no nationality and no frontiers. Due to this, increases in migration and international travel have also led to a rise in the number of donors from foreign countries. Linked to this is an increased risk of infections from specific areas of the world, which may persist in a latent or chronic form in the donor and may be transmitted during transplantation.
Knowledge of the potential pathogens involved, their geographic distribution and transmission, the diagnostic methods used, and recommendations to minimize the risk of transmission during transplantation and of infections in the posttransplant period is essential (Table 2). Infectious diseases in the immunosuppressed transplant patient may run a different course, with a shorter time to development of disease and greater associated morbidity and mortality than in immunocompetent patients.
TABLE 2.
Infectious agents with transplant-related cases, donor screening tests, and recommendations
| Infectious agent | Transplant-related cases | Donor screening recommended | Screening test(s) | Action if positive test result | Comments |
|---|---|---|---|---|---|
| HTLV-1/2 | Yes | Yes; different policies in different countries,a systematic screening in areas of endemicity with high seroprevalence and selective donor screening in nonendemic areas | ELISA-based serology, WB confirmatory test | Rejection of organs from HTLV-1/2-positive donors depending on the time and resources available; if 1st test is positive, a 2nd sample should be processed if time is available, and if no 2nd sample is available for retest, donor should be rejected; if 2nd ELISA is negative, organs can be used, but if both ELISA tests are positive, organs should be rejected | Determination of donor HTLV-1/2 status is based primarily on the results obtained from EIA testing; HTLV confirmatory testing (WB) is not always readily available and requires additional time; timely performance of a confirmatory assay for HTLV may save organ donations from being rejected; long delays in confirmatory testing performed by commercial laboratories may lead to loss of grafts; formal recommendations include performance of a confirmatory test; in the future, NAT may be useful in identifying falsely positive donors |
| WNV | Yes | Consider if high-risk donor is from area of endemicity with a declared epidemic outbreak; consider exclusion of such donors, especially if symptomatic | Screening methods should be based on detection of viral antigens by NAT in CSF, tissue samples, or blood; IgM ELISA-based serology is not useful (antibodies usually appear after the period of viremia) | Viremic donors should be rejected | If living donors are to be screened with NAT, testing should be performed as close to donation as possible; IgM is detectable 1 wk after infection and can persist for 6 mo |
| Rabies virus | Yes | Yes, if history of animal bite; consider also for donors with unexplained mental or neurological symptoms | Antigen detection in tissues (IFAT); serology (neutralizing antibodies), NAT techniques | Donor with recent possible exposure to rabies virus should not be accepted; donor with confirmed rabies virus infection should be rejected | Questioning donor's relatives about the possibility of contact with bats or of any other mammalian bite abroad, should identify patients at risk; if organ transplantation from undiagnosed rabies-infected donor occurs, prompt preemptive treatment is indicated (see the text) |
| Coccidioides immitis (coccidioidomycosis) | Yes | Consider if high-risk donor | Serology (IDCF, EIA) | Positive test does not necessarily contraindicate transplantation; if donor is high risk, antifungal prophylaxis should be started in recipients until serology is available; if test is positive, prophylaxis should be continued, and recipients should be monitored | In nonendemic countries, the donor's travel history should be established |
| Histoplasma capsulatum (histoplasmosis) | Yes | Consider if high-risk donor | Serology (CF and ID) | Transplant not contraindicated; antifungal prophylaxis if donor tests positive is controversial | Most cases are due to primary infection after transplantation, but some authors consider use of antifungal prophylaxis in recipients posttransplant for 3-6 mo |
| Paracoccidioides brasiliensis (paracoccidiomycosis) | No | No | No transmission via graft has been reported | ||
| Blastomyces dermatitidis (blastomycosis) | No | No | Low incidence in transplant patients; most cases are due to primary infection after transplantation | ||
| Penicillium marneffei (penicilliosis) | No | No | Most cases are due to reactivation of latent infection; no transmission via graft has been reported | ||
| Plasmodium spp. (malaria) | Yes | Yes, in immigrants, refugees, and travelers (3 preceding yr) from areas of endemicity | Thick and thin blood films; other techniques include HRP2 (immunochromatography) and PCR | Transplantation is not contraindicated, but organs should be rejected if donor's death is secondary to malaria | Establish donor's travel or residing history in areas of endemicity during the last 3 yr if possible |
| Leishmania spp. (leishmaniasis) | No | No | Most cases are linked to reactivation or primary infection; if donor serology is known to be positive, there should be strict monitoring posttransplant to commence early treatment if necessary | ||
| Trypanosoma cruzi (Chagas’ disease) | Yes | Yes | Two serology-based tests should be performed, including PCR techniques; immunochromatography tests have not yet been validated for donor screening | Use of donors with acute infection is contraindicated; use of heart from donor with chronic infection contraindicated; there is no consensus on use of other organs from donor with chronic infection, but strict follow-up is mandatory if organs are transplanted (see the text) | PCR techniques have higher sensitivity and specificity but are not routinely available in most laboratories; in a heart recipient with chronic chagasic disease, specific pre- and posttransplant therapy may be recommended; no consensus on routine posttransplant treatment if organs other than the heart from a seropositive donor are used in seronegative recipients |
| Strongyloides spp. (strongyloidiasis) | Yes | No | In the recipient, direct search and culture of larvae in stool if recipient is from area of endemicity | Specific treatment is recommended for recipients from areas of endemicity | Cases of direct transmission via graft are scarce; most cases are related to primary infection or autoinfection |
| Taenia solium (cysticercosis) | No | No; may consider serology and imaging for heart transplant if donor is high risk | Organs from a donor with neurocysticercosis may be used | ||
| Echinococcus granulosus (cystic hydatidosis) | Yes (rare) | Yes | Confirmation serology or fine-needle aspiration if imaging suggests hydatid disease | Organ affected by hydatidosis should not be used in transplantation except if cyst is very localized, inactive, or calcified and may be radically excised | Thoracic and abdominal CT scan to ascertain disease extension should be performed |
| Echinococcus multilocularis (alveolar hydatidosis) | No | No | Affected organs may not be used as they are infiltrated by disease | ||
| Filariae (filariasis) | Yes | No | Routine donor screening not recommended | ||
| Clonorchis spp., Opistorchis spp., Schistosoma spp., Paragonimus spp., Fasciola spp. | Cases related to Clonorchis spp. and Schistosoma spp. | Yes | Stool, urine, or sputum examination (depending on spp.) in donors from areas of endemicity or if there is peripheral eosinophilia | Specific treatment; donation is not contraindicated | Strict follow-up is necessary; if recipient is infected, transplantation is not contraindicated, and treatment is recommended pretransplant |
| Babesia spp. (babesiosis) | No | No | Transmission linked to infected blood transfusions in all cases | ||
| Entamoeba histolytica (amebiasis) | No | No | Screening tests are not routinely necessary; serological tests in donors coming from countries of endemicity are not adequate due to high seroprevalence rates | ||
| Free-living amoebae | No | No | |||
| Trypansoma brucei (sleeping sickness) | No | No | There is a potential risk, but there are no documented cases; there have been isolated cases of transmission via blood transfusion |
Some countries with low prevalence also perform universal screening of donors.
Donor selection protocols should be updated to include the latest microbiological diagnostic screening techniques to be used for the detection of potentially transmissible infections from areas of endemicity. The use of screening questionnaires may identify the potential donor's risk factors, and special emphasis should be made on the donor's travel and sexual history, exposure to animal or insect bites, history of prior blood transfusions, as well as the country of birth and residence of both the donor and his or her parents.
Acknowledgments
P.M.-D., J.F., A.M., and T.P. are members of GESITRA (Transplant Infections Study Group belonging to the Spanish Infectious Diseases Society).
F. Norman is the recipient of a research grant (C-45/07) from the Fundación Biomédica para la Investigación del Hospital Ramón y Cajal (Madrid, Spain).
The clinical research team acknowledges the support provided by the Red de Investigacion de Centros de Enfermedades Tropicales.
REFERENCES
- 1.Aguado, J. M., F. Bonet, J. J. Plaza, and A. Escudero. 1986. Visceral leishmaniasis in a renal transplant recipient: a diagnostic and therapeutic challenge. J. Infect. 13:301-303. [DOI] [PubMed] [Google Scholar]
- 2.Aguado, J. M., J. A. Herrero, and C. Lumbreras. 1997. Tuberculosis and protozoan infections in patients undergoing transplantation. Enferm. Infecc. Microbiol. Clin. 15(Suppl. 2):57-68. (In Spanish.) [PubMed] [Google Scholar]
- 3.Albuquerque, C. F., S. H. da Silva, and Z. P. Camargo. 2005. Improvement of the specificity of an enzyme-linked immunosorbent assay for diagnosis of paracoccidioidomycosis. J. Clin. Microbiol. 43:1944-1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alrajhi, A. A., M. Saleem, E. A. Ibrahim, and M. Gramiccia. 1998. Leishmaniasis of the tongue in a renal transplant recipient. Clin. Infect. Dis. 27:1332-1333. [PubMed] [Google Scholar]
- 5.Altclas, J., A. Sinagra, G. Jaimovich, C. Salgueira, C. Luna, A. Requejo, V. Milovic, A. De Rissio, L. Feldman, and A. Riarte. 1999. Reactivation of chronic Chagas’ disease following allogeneic bone marrow transplantation and successful pre-emptive therapy with benznidazole. Transpl. Infect. Dis. 1:135-137. [DOI] [PubMed] [Google Scholar]
- 6.American Journal of Transplantation. 2004. Screening of donor and recipient prior to solid organ transplantation. Am. J. Transplant. 4(Suppl. 10):10-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Medical News. 1978. Patient received cornea: rabies case linked to transplant. Am. Med. News 21:3. [PubMed] [Google Scholar]
- 8.Andersson, S., F. Dias, P. J. Mendez, A. Rodrigues, and G. Biberfeld. 1997. HTLV-I and -II infections in a nationwide survey of pregnant women in Guinea-Bissau, West Africa. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 15:320-322. [DOI] [PubMed] [Google Scholar]
- 9.Anosike, J. C., C. O. Onwuliri, and O. C. Abanobi. 1994. A case of probable transplacental transmission of Wuchereria bancrofti microfilariae. Appl. Parasitol. 35:294-296. [PubMed] [Google Scholar]
- 10.Anstead, G. M., G. Corcoran, J. Lewis, D. Berg, and J. R. Graybill. 2005. Refractory coccidioidomycosis treated with posaconazole. Clin. Infect. Dis. 40:1770-1776. [DOI] [PubMed] [Google Scholar]
- 11.Anton, M. J., B. P. Gonzalez, and S. N. Gutierrez. 2002. The neurocysticercosis is not only an imported illness. Med. Clin. (Barcelona) 118:77. [DOI] [PubMed] [Google Scholar]
- 12.Antony, S. 2004. Severe meningo-encephalitis and death in a renal transplant recipient resulting from West Nile virus infection. J. Natl. Med. Assoc. 96:1646-1647. [PMC free article] [PubMed] [Google Scholar]
- 13.AORN Journal. 1980. Second rabies death attributed to graft [news]. AORN J. 31:818. [PubMed] [Google Scholar]
- 14.Apaydin, S., R. Ataman, K. Serdengect, N. Tuzuner, E. Polat, E. Erek, and U. Ulku. 1997. Visceral leishmaniasis without fever in a kidney transplant recipient. Nephron 75:241-242. [DOI] [PubMed] [Google Scholar]
- 15.Armali, Z., R. Ramadan, A. Chlebowski, and Z. S. Azzam. 2003. West Nile meningo-encephalitis infection in a kidney transplant recipient. Transplant. Proc. 35:2935-2936. [DOI] [PubMed] [Google Scholar]
- 16.Attar, Z. J., M. L. Chance, S. el-Safi, J. Carney, A. Azazy, M. El-Hadi, C. Dourado, and M. Hommel. 2001. Latex agglutination test for the detection of urinary antigens in visceral leishmaniasis. Acta Trop. 78:11-16. [DOI] [PubMed] [Google Scholar]
- 17.Babinet, J., F. Gay, D. Bustos, M. Dubarry, D. Jaulmes, L. Nguyen, and M. Gentilini. 1991. Transmission of Plasmodium falciparum by heart transplant. BMJ 303:1515-1516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Baer, G. M., J. H. Shaddock, S. A. Houff, A. K. Harrison, and J. J. Gardner. 1982. Human rabies transmitted by corneal transplant. Arch. Neurol. 39:103-107. [DOI] [PubMed] [Google Scholar]
- 19.Barcan, L., C. Luna, L. Clara, A. Sinagra, A. Valledor, A. M. De Rissio, A. Gadano, M. M. Garcia, E. de Santibañes, and A. Riarte. 2005. Transmission of T. cruzi infection via liver transplantation to a nonreactive recipient for Chagas’ disease. Liver Transpl. 11:1112-1116. [DOI] [PubMed] [Google Scholar]
- 20.Barsoum, R. S. 2004. Parasitic infections in organ transplantation. Exp. Clin. Transplant. 2:258-267. [PubMed] [Google Scholar]
- 21.Basset, D., F. Faraut, P. Marty, J. Dereure, E. Rosenthal, C. Mary, F. Pratlong, L. Lachaud, P. Bastien, and J. P. Dedet. 2005. Visceral leishmaniasis in organ transplant recipients: 11 new cases and a review of the literature. Microbes Infect. 7:1370-1375. [DOI] [PubMed] [Google Scholar]
- 22.Bateman, A. C., G. R. Jones, S. O'Connell, F. J. Clark, and M. Plummeridge. 2002. Massive hepatosplenomegaly caused by Penicillium marneffei associated with human immunodeficiency virus infection in a Thai patient. J. Clin. Pathol. 55:143-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bein, T., W. Haerty, M. Haller, H. Forst, and E. Pratschke. 1993. Organ selection in intensive care: transplantation of a liver allograft, including calcified cyst of Echinococcus granularis. Intensive Care Med. 19:182. [DOI] [PubMed] [Google Scholar]
- 24.Bemelman, F., K. De Blok, P. De Vries, S. Surachno, and I. Ten Berge. 2004. Falciparum malaria transmitted by a thick blood smear negative kidney donor. Scand. J. Infect. Dis. 36:769-771. [DOI] [PubMed] [Google Scholar]
- 25.Benvenuti, L. A., A. Roggerio, N. V. Sambiase, A. Fiorelli, and M. L. Higuchi. 2005. Polymerase chain reaction in endomyocardial biopsies for monitoring reactivation of Chagas’ disease in heart transplantation: a case report and review of the literature. Cardiovasc. Pathol. 14:265-268. [DOI] [PubMed] [Google Scholar]
- 26.Ben-Youssef, R., P. Baron, F. Edson, R. Raghavan, and O. Okechukwu. 2005. Stronglyoides stercoralis infection from pancreas allograft: case report. Transplantation 80:997-998. [DOI] [PubMed] [Google Scholar]
- 27.Berenguer, J., F. Gomez-Campdera, B. Padilla, M. Rodriguez-Ferrero, F. Anaya, S. Moreno, and F. Valderrabano. 1998. Visceral leishmaniasis (kala-azar) in transplant recipients: case report and review. Transplantation 65:1401-1404. [DOI] [PubMed] [Google Scholar]
- 28.Bestetti, R. B., P. M. Cury, T. A. Theodoropoulos, and D. Villafanha. 2004. Trypanosoma cruzi myocardial infection reactivation presenting as complete atrioventricular block in a Chagas’ heart transplant recipient. Cardiovasc. Pathol. 13:323-326. [DOI] [PubMed] [Google Scholar]
- 29.Bialek, R., A. Feucht, C. Aepinus, G. Just-Nubling, V. J. Robertson, J. Knobloch, and R. Hohle. 2002. Evaluation of two nested PCR assays for detection of Histoplasma capsulatum DNA in human tissue. J. Clin. Microbiol. 40:1644-1647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bialek, R., J. Kern, T. Herrmann, R. Tijerina, L. Cecenas, U. Reischl, and G. M. Gonzalez. 2004. PCR assays for identification of Coccidioides posadasii based on the nucleotide sequence of the antigen 2/proline-rich antigen. J. Clin. Microbiol. 42:778-783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Blair, J. E. 2005. Asymptomatic coccidioidomycosis among healthy persons undergoing evaluation for possible liver or kidney donation, abstr. M-981, Abstr. 45th Intersci. Conf. Antimicrob. Agents Chemother. ASM Press, Washington, DC.
- 32.Blair, J. E. 2004. Coccidioidal pneumonia, arthritis, and soft-tissue infection after kidney transplantation. Transpl. Infect. Dis. 6:74-76. [DOI] [PubMed] [Google Scholar]
- 33.Blair, J. E. 2006. Coccidioidomycosis in liver transplantation. Liver Transpl. 12:31-39. [DOI] [PubMed] [Google Scholar]
- 34.Blair, J. E., and D. D. Douglas. 2004. Coccidioidomycosis in liver transplant recipients relocating to an endemic area. Dig. Dis. Sci. 49:1981-1985. [DOI] [PubMed] [Google Scholar]
- 35.Blair, J. E., and J. L. Logan. 2001. Coccidioidomycosis in solid organ transplantation. Clin. Infect. Dis. 33:1536-1544. [DOI] [PubMed] [Google Scholar]
- 36.Blair, J. E., and D. C. Mulligan. 2007. Coccidioidomycosis in healthy persons evaluated for liver or kidney donation. Transpl. Infect. Dis. 9:78-82. [DOI] [PubMed] [Google Scholar]
- 37.Bleck, T. P., and C. E. Rupprecht. 2005. Rhabdoviruses, p. 2047-2056. In G. E. Mandell, R. G. Douglas, and R. Dolin (ed.), Mandell, Douglas and Bennet's principles and practice of infectious diseases. Elsevier Churchill-Livingstone, Philadelphia, PA.
- 38.Bocchi, E. A., G. Bellotti, D. Uip, J. Kalil, H. M. de Lourdes, A. Fiorelli, N. Stolf, A. Jatene, and F. Pilleggi. 1993. Long-term follow-up after heart transplantation in Chagas’ disease. Transplant. Proc. 25:1329-1330. [PubMed] [Google Scholar]
- 39.Bocchi, E. A., A. Fiorelli, et al. 2001. The paradox of survival results after heart transplantation for cardiomyopathy caused by Trypanosoma cruzi. Ann. Thorac. Surg. 71:1833-1838. [DOI] [PubMed] [Google Scholar]
- 40.Boletis, J. N., A. Pefanis, C. Stathakis, H. Helioti, A. Kostakis, and H. Giamarellou. 1999. Visceral leishmaniasis in renal transplant recipients: successful treatment with liposomal amphotericin B (AmBisome). Clin. Infect. Dis. 28:1308-1309. [DOI] [PubMed] [Google Scholar]
- 41.Boonstra, E. 2002. Trypanosomiasis—a real risk for tourists visiting national parks in Tanzania. Tidsskr. Nor. Laegeforen. 122:35-37. (In Norweigan.) [PubMed] [Google Scholar]
- 42.Bracca, A., M. E. Tosello, J. E. Girardini, S. L. Amigot, C. Gomez, and E. Serra. 2003. Molecular detection of Histoplasma capsulatum var. capsulatum in human clinical samples. J. Clin. Microbiol. 41:1753-1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Braddy, C. M., R. L. Heilman, and J. E. Blair. 2006. Coccidioidomycosis after renal transplantation in an endemic area. Am. J. Transplant. 6:340-345. [DOI] [PubMed] [Google Scholar]
- 44.Bragin-Sanchez, D., and P. P. Chang. 2005. West Nile virus encephalitis infection in a heart transplant recipient: a case report. J. Heart Lung Transplant. 24:621-623. [DOI] [PubMed] [Google Scholar]
- 45.Bresson-Hadni, S., S. Koch, I. Beurton, D. A. Vuitton, B. Bartholomot, S. Hrusovsky, B. Heyd, D. Lenys, A. Minello, M. C. Becker, C. Vanlemmens, G. A. Mantion, and J. P. Miguet. 1999. Primary disease recurrence after liver transplantation for alveolar echinococcosis: long-term evaluation in 15 patients. Hepatology 30:857-864. [DOI] [PubMed] [Google Scholar]
- 46.Bresson-Hadni, S., J. P. Miguet, D. Lenys, D. A. Vuitton, G. Viennet, M. C. Becker, P. Rohmer, G. Mantion, and M. Gillet. 1992. Recurrence of alveolar echinococcosis in the liver graft after liver transplantation. Hepatology 16:279-280. [DOI] [PubMed] [Google Scholar]
- 47.Bresson-Hadni, S., D. A. Vuitton, B. Bartholomot, B. Heyd, D. Godart, J. P. Meyer, S. Hrusovsky, M. C. Becker, G. Mantion, D. Lenys, and J. P. Miguet. 2000. A twenty-year history of alveolar echinococcosis: analysis of a series of 117 patients from eastern France. Eur. J. Gastroenterol. Hepatol. 12:327-336. [DOI] [PubMed] [Google Scholar]
- 48.Brett, M. T., J. T. Kwan, and M. R. Bending. 1988. Caecal perforation in a renal transplant patient with disseminated histoplasmosis. J. Clin. Pathol. 41:992-995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Broeckaert-van Orshoven, A., P. Michielsen, and J. Vandepitte. 1979. Fatal leishmaniasis in renal-transplant patient. Lancet ii:740-741. [DOI] [PubMed] [Google Scholar]
- 50.Bryan, C. F., G. E. Tegtmeier, N. Rafik, L. E. Markham, D. Murillo, P. W. Nelson, C. F. Shield III, B. A. Warady, and M. I. Aeder. 2004. The risk for Chagas’ disease in the Midwestern United States organ donor population is low. Clin. Transplant. 18(Suppl. 12):12-15. [DOI] [PubMed] [Google Scholar]
- 51.Burton, E. C., D. K. Burns, M. J. Opatowsky, W. H. El-Feky, B. Fischbach, L. Melton, E. Sanchez, H. Randall, D. L. Watkins, J. Chang, and G. Klintmalm. 2005. Rabies encephalomyelitis: clinical, neuroradiological, and pathological findings in 4 transplant recipients. Arch. Neurol. 62:873-882. [DOI] [PubMed] [Google Scholar]
- 52.Busch, M. P., S. Caglioti, E. F. Robertson, J. D. McAuley, L. H. Tobler, H. Kamel, J. M. Linnen, V. Shyamala, P. Tomasulo, and S. H. Kleinman. 2005. Screening the blood supply for West Nile virus RNA by nucleic acid amplification testing. N. Engl. J. Med. 353:460-467. [DOI] [PubMed] [Google Scholar]
- 53.Busch, M. P., S. H. Kleinman, and G. J. Nemo. 2003. Current and emerging infectious risks of blood transfusions. JAMA 289:959-962. [DOI] [PubMed] [Google Scholar]
- 54.Butka, B. J., S. R. Bennett, and A. C. Johnson. 1984. Disseminated inoculation blastomycosis in a renal transplant recipient. Am. Rev. Respir. Dis. 130:1180-1183. [DOI] [PubMed] [Google Scholar]
- 55.Cantarovich, F., M. Vazquez, W. D. Garcia, F. M. Abbud, C. Herrera, and H. A. Villegas. 1992. Special infections in organ transplantation in South America. Transplant. Proc. 24:1902-1908. [PubMed] [Google Scholar]
- 56.Cao, L., K. M. Chan, D. Chen, N. Vanittanakom, C. Lee, C. M. Chan, T. Sirisanthana, D. N. Tsang, and K. Y. Yuen. 1999. Detection of cell wall mannoprotein Mp1p in culture supernatants of Penicillium marneffei and in sera of penicilliosis patients. J. Clin. Microbiol. 37:981-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Cao, L., D. L. Chen, C. Lee, C. M. Chan, K. M. Chan, N. Vanittanakom, D. N. Tsang, and K. Y. Yuen. 1998. Detection of specific antibodies to an antigenic mannoprotein for diagnosis of Penicillium marneffei penicilliosis. J. Clin. Microbiol. 36:3028-3031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Carpio, A. 2002. Neurocysticercosis: an update. Lancet Infect. Dis. 2:751-762. [DOI] [PubMed] [Google Scholar]
- 59.Castellanos, F., I. Montes, L. F. Porras, E. Peragallo, J. Ampuero, and R. Rueda. 2000. Giant subarachnoid cysts due to neurocysticercosis: two cases reported fro a rural area in Extremadura. Rev. Neurol. 30:433-435. (In Spanish.) [PubMed] [Google Scholar]
- 60.Centers for Disease Control. 1981. Human-to-human transmission of rabies via corneal transplant—Thailand. MMWR Morb. Mortal. Wkly. Rep. 30:473-474. [PubMed] [Google Scholar]
- 61.Centers for Disease Control and Prevention. 1993. False-positive serologic tests for human T-cell lymphotropic virus type I among blood donors following influenza vaccination, 1992. JAMA 269:2076-2078. [PubMed] [Google Scholar]
- 62.Centers for Disease Control and Prevention. 1998. Preventing emerging infectious diseases: a strategy for the 21st century overview of the updated CDC plan. MMWR Morb. Mortal. Wkly. Rep. 47:1-14. [PubMed] [Google Scholar]
- 63.Centers for Disease Control and Prevention. 2000. Guidelines for preventing opportunistic infections among hematopoietic stem cell transplant recipients: recommendations of CDC, the Infectious Disease Society of America and the American Society of Blood and Marrow Transplantation. Centers for Disease Control and Prevention, Atlanta, GA. http://www.cdc.gov/mmwr/preview/mmwrhtlm/rr4910a1.htm. [DOI] [PMC free article] [PubMed]
- 64.Centers for Disease Control and Prevention. 2002. Chagas disease after organ transplantation—United States, 2001. JAMA 287:1795-1796. [PubMed] [Google Scholar]
- 65.Centers for Disease Control and Prevention. 2002. West Nile virus activity—United States, September 26-October 2, 2002, and investigations of West Nile virus infections in recipients of blood transfusion and organ transplantation. JAMA 288:1975-1976. [PubMed] [Google Scholar]
- 66.Centers for Disease Control and Prevention. 2004. Transfusion-associated transmission of West Nile virus—Arizona, 2004. MMWR Morb. Mortal. Wkly. Rep. 53:842-844. [PubMed] [Google Scholar]
- 67.Centers for Disease Control and Prevention. 2005. West Nile virus infections in organ transplant recipients—New York and Pennsylvania, August-September, 2005. MMWR Morb. Mortal. Wkly. Rep. 54:1021-1023. [PubMed] [Google Scholar]
- 68.Centers for Disease Control and Prevention. 2006. West nile virus activity—United States, January 1-November 7, 2006. MMWR Morb. Mortal. Wkly. Rep. 55:1204-1205. [PubMed] [Google Scholar]
- 69.Centers for Disease Control and Prevention. 2002. West Nile virus infection in organ donor and transplant recipients—Georgia and Florida, 2002. JAMA 288:1465-1466. [PubMed] [Google Scholar]
- 70.Centers for Disease Control and Prevention. 2002. West Nile virus activity—United States, September 26-October 2, 2002, and investigations of West Nile virus infections in recipients of blood transfusion and organ transplantation. MMWR Morb. Mortal. Wkly. Rep. 51:884, 895. [PubMed] [Google Scholar]
- 71.Centers for Disease Control and Prevention. 2002. West Nile virus infection in organ donor and transplant recipients—Georgia and Florida, 2002. MMWR Morb. Mortal. Wkly. Rep. 51:790. [PubMed] [Google Scholar]
- 72.Centers for Disease Control and Prevention. 2004. Update: West Nile virus screening of blood donations and transfusion-associated transmission—United States, 2003. MMWR Morb. Mortal. Wkly. Rep. 53:281-284. [PubMed] [Google Scholar]
- 73.Centers for Disease Control and Prevention. 2006. Chagas disease after organ transplantation—Los Angeles, California, 2006. MMWR Morb. Mortal. Wkly. Rep. 55:798-800. [PubMed] [Google Scholar]
- 74.Centers for Disease Control and Prevention. 1993. False-positive serologic tests for human T-cell lymphotropic virus type I among blood donors following influenza vaccination, 1992. MMWR Morb. Mortal. Wkly. Rep. 42:173-175. [PubMed] [Google Scholar]
- 75.Centers for Disease Control and Prevention. 2007. Blood donor screening for Chagas disease—United States, 2006-2007. MMWR Morb. Mortal. Wkly. Rep. 56:141-143. [PubMed] [Google Scholar]
- 76.Centers of Disease Control and Prevention. 26 April 2007, accession date. Malaria. Centers of Disease Control and Prevention, Atlanta, GA. http://www.cdc.gov/travel/diseases.htm#malaria.
- 77.Centers for Disease Control and Prevention and the USPHS Working Group. 1993. Guidelines for counseling persons infected with human T-lymphotropic virus type I (HTLV-I) and type II (HTLV-II). Ann. Intern. Med. 118:448-454. [DOI] [PubMed] [Google Scholar]
- 78.Chaiwun, B., S. Khunamornpong, C. Sirivanichai, S. Rangdaeng, K. Supparatpinyo, J. Settakorn, C. Ya-in, and P. Thorner. 2002. Lymphadenopathy due to Penicillium marneffei infection: diagnosis by fine needle aspiration cytology. Mod. Pathol. 15:939-943. [DOI] [PubMed] [Google Scholar]
- 79.Chan, Y. H., K. M. Wong, K. C. Lee, P. C. Kwok, W. L. Chak, K. S. Choi, K. F. Chau, and C. S. Li. 2004. Pneumonia and mesenteric lymphadenopathy caused by disseminated Penicillium marneffei infection in a cadaveric renal transplant recipient. Transpl. Infect. Dis. 6:28-32. [DOI] [PubMed] [Google Scholar]
- 80.Chiavetta, J. A., M. Escobar, A. Newman, Y. He, P. Driezen, S. Deeks, D. E. Hone, S. F. O'Brien, and G. Sher. 2003. Incidence and estimated rates of residual risk for HIV, hepatitis C, hepatitis B and human T-cell lymphotropic viruses in blood donors in Canada, 1990-2000. CMAJ 169:767-773. [PMC free article] [PubMed] [Google Scholar]
- 81.Chiche, L., A. Lesage, C. Duhamel, E. Salame, M. Malet, D. Samba, P. Segol, and M. Treilhaud. 2003. Posttransplant malaria: first case of transmission of Plasmodium falciparum from a white multiorgan donor to four recipients. Transplantation 75:166-168. [DOI] [PubMed] [Google Scholar]
- 82.Chim, C. S., C. Y. Fong, S. K. Ma, S. S. Wong, and K. Y. Yuen. 1998. Reactive hemophagocytic syndrome associated with Penicillium marneffei infection. Am. J. Med. 104:196-197. [DOI] [PubMed] [Google Scholar]
- 83.Chimol Barbosa, P. R. 2006. The oral transmission of Chagas’ disease: an acute form of infection responsible for regional outbreaks. Int. J. Cardiol. 112:132-133. [DOI] [PubMed] [Google Scholar]
- 84.Chisholm, E. S., T. K. Ruebush, A. J. Sulzer, and G. R. Healy. 1978. Babesia microti infection in man: evaluation of an indirect immunofluorescent antibody test. Am. J. Trop. Med. Hyg. 27:14-19. [DOI] [PubMed] [Google Scholar]
- 85.Cimo, P. L., W. E. Luper, and M. A. Scouros. 1993. Transfusion-associated Chagas’ disease in Texas: report of a case. Tex. Med. 89:48-50. [PubMed] [Google Scholar]
- 86.Cohen, I. M., J. N. Galgiani, D. Potter, and D. A. Ogden. 1982. Coccidioidomycosis in renal replacement therapy. Arch. Intern. Med. 142:489-494. [PubMed] [Google Scholar]
- 87.Costa-Cruz, J. M., A. Rocha, A. M. Silva, A. T. De Moraes, A. H. Guimaraes, E. C. Salomao, and T. M. Alcantara. 1995. Occurrence of cysticercosis in autopsies performed in Uberlandia, Minas Gerais, Brazil. Arq. Neuropsiquiatr. 53:227-232. (In Portugese.) [DOI] [PubMed] [Google Scholar]
- 88.Coutinho, Z. F., D. Silva, M. Lazera, V. Petri, R. M. Oliveira, P. C. Sabroza, and B. Wanke. 2002. Paracoccidioidomycosis mortality in Brazil (1980-1995). Cad. Saude Publica 18:1441-1454. [DOI] [PubMed] [Google Scholar]
- 89.Crafa, F., J. Gugenheim, P. Fabiani, L. Di Marzo, G. Militerno, L. Iovine, B. Goubaux, and J. Mouiel. 1991. Possible transmission of malaria by liver transplantation. Transplant. Proc. 23:2664. [PubMed] [Google Scholar]
- 90.Crum, N. F., E. R. Lederman, C. M. Stafford, J. S. Parrish, and M. R. Wallace. 2004. Coccidioidomycosis: a descriptive survey of a reemerging disease. Clinical characteristics and current controversies. Medicine (Baltimore) 83:149-175. [DOI] [PubMed] [Google Scholar]
- 91.Cruz, I., C. Chicharro, J. Nieto, B. Bailo, C. Canavate, M. C. Figueras, and J. Alvar. 2006. Comparison of new diagnostic tools for management of pediatric Mediterranean visceral leishmaniasis. J. Clin. Microbiol. 44:2343-2347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cruz, I., V. Mody, C. Callender, and A. Hosten. 1978. Malaria infection in transplant recipient. J. Natl. Med. Assoc. 70:105-107. [PMC free article] [PubMed] [Google Scholar]
- 93.D'Albuquerque, L. A., A. M. Gonzalez, H. L. Filho, J. L. Copstein, F. I. Larrea, J. M. Mansero, G. Peron, Jr., M. A. Ribeiro, Jr., and A. Oliveira e Silva. 2007. Liver transplantation from deceased donors serologically positive for Chagas disease. Am. J. Transplant. 7:680-684. [DOI] [PubMed] [Google Scholar]
- 94.Davies, S. F., G. A. Sarosi, P. K. Peterson, M. Khan, R. J. Howard, R. L. Simmons, and J. S. Najarian. 1979. Disseminated histoplasmosis in renal transplant recipients. Am. J. Surg. 137:686-691. [DOI] [PubMed] [Google Scholar]
- 95.de Camargo, Z. P., and M. F. de Franco. 2000. Current knowledge on pathogenesis and immunodiagnosis of paracoccidioidomycosis. Rev. Iberoam. Micol. 17:41-48. [PubMed] [Google Scholar]
- 96.de Carvalho, V. B., E. F. Sousa, J. H. Vila, J. P. da Silva, M. R. Caiado, S. R. Araujo, R. Macruz, and E. J. Zerbini. 1996. Heart transplantation in Chagas’ disease. 10 years after the initial experience. Circulation 94:1815-1817. [DOI] [PubMed] [Google Scholar]
- 97.de la Torre, J., C. Coll, M. Coloma, J. I. Martin, E. Padron, and N. L. Gonzalez Gonzalez. 2006. Antenatal care in immigrants. An. Sist. Sanit. Navar. 29(Suppl. 1):49-61. (In Spanish.) [PubMed] [Google Scholar]
- 98.del Brutto, O. H., V. Rajshekhar, A. C. White, Jr., V. C. Tsang, T. E. Nash, O. M. Takayanagui, P. M. Schantz, C. A. Evans, A. Flisser, D. Correa, D. Botero, J. C. Allan, E. Sarti, A. E. Gonzalez, R. H. Gilman, and H. H. Garcia. 2001. Proposed diagnostic criteria for neurocysticercosis. Neurology 57:177-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Delmonico, F. L., and D. R. Snydman. 1998. Organ donor screening for infectious diseases: review of practice and implications for transplantation. Transplantation 65:603-610. [DOI] [PubMed] [Google Scholar]
- 100.Del Negro, G. M., C. N. Pereira, H. F. Andrade, S. A. Palacios, M. M. Vidal, C. E. Charbel, and G. Benard. 2000. Evaluation of tests for antibody response in the follow-up of patients with acute and chronic forms of paracoccidioidomycosis. J. Med. Microbiol. 49:37-46. [DOI] [PubMed] [Google Scholar]
- 101.DeSalvo, D., P. Roy-Chaudhury, R. Peddi, T. Merchen, K. Konijetti, M. Gupta, R. Boardman, C. Rogers, J. Buell, M. Hanaway, J. Broderick, R. Smith, and E. S. Woodle. 2004. West Nile virus encephalitis in organ transplant recipients: another high-risk group for meningoencephalitis and death. Transplantation 77:466-469. [DOI] [PubMed] [Google Scholar]
- 102.de Thé, G., and M. Kazanji. 1996. An HTLV-I/II vaccine: from animal models to clinical trials? J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 13(Suppl. 1):S191-S198. [DOI] [PubMed] [Google Scholar]
- 103.DeVault, G. A., Jr., J. W. King, M. S. Rohr, M. D. Landreneau, S. T. Brown III, and J. C. McDonald. 1990. Opportunistic infections with Strongyloides stercoralis in renal transplantation. Rev. Infect. Dis. 12:653-671. [DOI] [PubMed] [Google Scholar]
- 104.Dictar, M., A. Sinagra, M. T. Veron, C. Luna, C. Dengra, A. De Rissio, R. Bayo, D. Ceraso, E. Segura, B. Koziner, and A. Riarte. 1998. Recipients and donors of bone marrow transplants suffering from Chagas’ disease: management and preemptive therapy of parasitemia. Bone Marrow Transplant. 21:391-393. [DOI] [PubMed] [Google Scholar]
- 105.Domen, R. E., and K. A. Nelson. 1997. Results of a survey of infectious disease testing practices by organ procurement organizations in the United States. Transplantation 63:1790-1794. [DOI] [PubMed] [Google Scholar]
- 106.Donegan, E., M. P. Busch, J. A. Galleshaw, G. M. Shaw, J. W. Mosley, et al. 1990. Transfusion of blood components from a donor with human T-lymphotropic virus type II (HTLV-II) infection. Ann. Intern. Med. 113:555-556. [DOI] [PubMed] [Google Scholar]
- 107.Donovan, K. L., A. D. White, D. A. Cooke, and D. J. Fisher. 1990. Pancreatitis and palindromic arthropathy with effusions associated with sodium stibogluconate treatment in a renal transplant recipient. J. Infect. 21:107-110. [DOI] [PubMed] [Google Scholar]
- 108.Dosanjh, A., J. Theodore, and D. Pappagianis. 1998. Probable false positive coccidioidal serologic results in patients with cystic fibrosis. Pediatr. Transplant. 2:313-317. [PubMed] [Google Scholar]
- 109.Do Valle, A. C., R. L. Costa, P. C. Fialho Monteiro, H. J. Von, M. M. Muniz, and R. M. Zancope-Oliveira. 2001. Interpretation and clinical correlation of serological tests in paracoccidioidomycosis. Med. Mycol. 39:373-377. [DOI] [PubMed] [Google Scholar]
- 110.Dumas, M., D. Houinato, M. Verdier, T. Zohoun, R. Josse, J. Bonis, I. Zohoun, A. Massougbodji, and F. Denis. 1991. Seroepidemiology of human T-cell lymphotropic virus type I/II in Benin (West Africa). AIDS Res. Hum. Retrovir. 7:447-451. [DOI] [PubMed] [Google Scholar]
- 111.Duong, T. A. 1996. Infection due to Penicillium marneffei, an emerging pathogen: review of 155 reported cases. Clin. Infect. Dis. 23:125-130. [DOI] [PubMed] [Google Scholar]
- 112.Durkin, M., J. Witt, A. Lemonte, B. Wheat, and P. Connolly. 2004. Antigen assay with the potential to aid in diagnosis of blastomycosis. J. Clin. Microbiol. 42:4873-4875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.El Masry, H. Z., and J. O'Donnell. 2005. Fatal stongyloides hyperinfection in heart transplantation. J. Heart Lung Transplant. 24:1980-1983. [DOI] [PubMed] [Google Scholar]
- 114.Ersoy, A., M. Gullulu, M. Usta, T. Ozcelik, E. Ylmaz, E. K. Uzaslan, H. Vuruskan, M. Yavuz, B. Oktay, K. Dilek, and M. Yurtkuran. 2003. A renal transplant recipient with pulmonary tuberculosis and visceral leishmaniasis: review of superimposed infections and therapy approaches. Clin. Nephrol. 60:289-294. [DOI] [PubMed] [Google Scholar]
- 115.Feigal, E., E. Murphy, K. Vranizan, P. Bacchetti, R. Chaisson, J. E. Drummond, W. Blattner, M. McGrath, J. Greenspan, and A. Moss. 1991. Human T cell lymphotropic virus types I and II in intravenous drug users in San Francisco: risk factors associated with seropositivity. J. Infect. Dis. 164:36-42. [DOI] [PubMed] [Google Scholar]
- 116.Fernandes, I. M., M. A. Baptista, T. R. Barbon, J. F. Oliveira, R. C. Oliveira, N. M. Murai, F. C. Camelo, H. J. Ramalho, and M. Abbud-Filho. 2002. Cutaneous leishmaniasis in kidney transplant recipient. Transplant. Proc. 34:504-505. [DOI] [PubMed] [Google Scholar]
- 117.Fernandez-Guerrero, M. L., J. M. Aguado, L. Buzon, C. Barros, C. Montalban, T. Martin, and E. Bouza. 1987. Visceral leishmaniasis in immunocompromised hosts. Am. J. Med. 83:1098-1102. [DOI] [PubMed] [Google Scholar]
- 118.Fernandez-Rodriguez, R., G. Ozaita, A. Viso, R. Garcia-Mata, A. Gomez, and O. Fernandez. 1991. Active and inactive forms of cerebral cysticercosis. Study of 10 cases. Rev. Clin. Esp. 188:409-411. (In Spanish.) [PubMed] [Google Scholar]
- 119.Fiorelli, A. I., N. A. Stolf, R. Honorato, E. Bocchi, F. Bacal, D. Uip, T. Strabelli, V. Issa, V. A. Amato, L. R. Fiorelli, and S. A. Oliveira. 2005. Later evolution after cardiac transplantation in Chagas’ disease. Transplant. Proc. 37:2793-2798. [DOI] [PubMed] [Google Scholar]
- 120.Fischer, L., M. Sterneck, M. Claus, A. Costard-Jackle, B. Fleischer, H. Herbst, X. Rogiers, and C. E. Broelsch. 1999. Transmission of malaria tertiana by multi-organ donation. Clin. Transplant. 13:491-495. [DOI] [PubMed] [Google Scholar]
- 121.Focosi, D., and M. Petrini. 2006. More on donor-derived T-cell leukemia after bone marrow transplantation. N. Engl. J. Med. 355:212-213. [DOI] [PubMed] [Google Scholar]
- 122.Font, P. C., J. A. Ruiz Postigo, B. C. Munoz, A. F. Pardos, and C. M. Corachan. 1999. Neurocysticercosis in Spain. Apropos 4 cases seen in immigrant patients from endemic countries. An. Med. Interna 16:89-91. (In Spanish.) [PubMed] [Google Scholar]
- 123.Fores, R., I. Sanjuan, F. Portero, E. Ruiz, C. Regidor, R. Lopez-Velez, M. Linares, S. Gil, E. Ojeda, I. Krsnik, G. Bautista, C. Vallejo, J. Garcia-Marco, M. N. Fernandez, and J. R. Cabrera. 2007. Chagas disease in a recipient of cord blood transplantation. Bone Marrow Transplant. 39:127-128. [DOI] [PubMed] [Google Scholar]
- 124.Frapier, J. M., B. Abraham, J. Dereure, and B. Albat. 2001. Fatal visceral leishmaniasis in a heart transplant recipient. J. Heart Lung Transplant. 20:912-913. [DOI] [PubMed] [Google Scholar]
- 125.Freifeld, A. G., P. C. Iwen, B. L. Lesiak, R. K. Gilroy, R. B. Stevens, and A. C. Kalil. 2005. Histoplasmosis in solid organ transplant recipients at a large Midwestern university transplant center. Transpl. Infect. Dis. 7:109-115. [DOI] [PubMed] [Google Scholar]
- 126.Galgiani, J. N. 1997. Coccidioidomycosis. Curr. Clin. Top. Infect. Dis. 17:188-204. [PubMed] [Google Scholar]
- 127.Galgiani, J. N., N. M. Ampel, J. E. Blair, A. Catanzaro, R. H. Johnson, D. A. Stevens, and P. L. Williams. 2005. Coccidioidomycosis. Clin. Infect. Dis. 41:1217-1223. [DOI] [PubMed] [Google Scholar]
- 128.Galgiani, J. N., N. M. Ampel, A. Catanzaro, R. H. Johnson, D. A. Stevens, P. L. Williams, et al. 2000. Practice guideline for the treatment of coccidioidomycosis. Clin. Infect. Dis. 30:658-661. [DOI] [PubMed] [Google Scholar]
- 129.Garcia, H. H., and O. H. del Brutto. 2005. Neurocysticercosis: updated concepts about an old disease. Lancet Neurol. 4:653-661. [DOI] [PubMed] [Google Scholar]
- 130.Garcia, H. H., O. H. del Brutto, T. E. Nash, A. C. White, Jr., V. C. Tsang, and R. H. Gilman. 2005. New concepts in the diagnosis and management of neurocysticercosis (Taenia solium). Am. J. Trop. Med. Hyg. 72:3-9. [PubMed] [Google Scholar]
- 131.Gauthier, G. M., N. Safdar, B. S. Klein, and D. R. Andes. 2007. Blastomycosis in solid organ transplant recipients. Transpl. Infect. Dis. 9:310-317. [DOI] [PubMed] [Google Scholar]
- 132.Gelman, B. B., S. J. Rauf, R. Nader, V. Popov, J. Borkowski, G. Chaljub, H. W. Nauta, and G. S. Visvesvara. 2001. Amoebic encephalitis due to Sappinia diploidea. JAMA 285:2450-2451. [DOI] [PubMed] [Google Scholar]
- 133.Gessain, A., and G. de The. 1996. What is the situation of human T cell lymphotropic virus type II (HTLV-II) in Africa? Origin and dissemination of genomic subtypes. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 13(Suppl. 1):S228-S235. [DOI] [PubMed] [Google Scholar]
- 134.Gode, G. R., and N. K. Bhide. 1988. Two rabies deaths after corneal grafts from one donor. Lancet ii:791. [DOI] [PubMed] [Google Scholar]
- 135.Goldani, L. Z., and A. M. Sugar. 1995. Paracoccidioidomycosis and AIDS: an overview. Clin. Infect. Dis. 21:1275-1281. [DOI] [PubMed] [Google Scholar]
- 136.Golino, A., J. M. Duncan, B. Zeluff, J. DePriest, H. A. McAllister, B. Radovancevic, and O. H. Frazier. 1992. Leishmaniasis in a heart transplant patient. J. Heart Lung Transplant. 11:820-823. [PubMed] [Google Scholar]
- 137.Gomes, M. L., L. M. Galvao, A. M. Macedo, S. D. Pena, and E. Chiari. 1999. Chagas’ disease diagnosis: comparative analysis of parasitologic, molecular, and serologic methods. Am. J. Trop. Med. Hyg. 60:205-210. [DOI] [PubMed] [Google Scholar]
- 138.Gomez, C. F., J. Berenguer, F. Anaya, M. Rodriguez, and F. Valderrabano. 1998. Visceral leishmaniasis in a renal transplant recipient. Short review and therapy alternative. Am. J. Nephrol. 18:171. [DOI] [PubMed] [Google Scholar]
- 139.Gontijo, C. M., R. S. Pacheco, F. Orefice, E. Lasmar, E. S. Silva, and M. N. Melo. 2002. Concurrent cutaneous, visceral and ocular leishmaniasis caused by Leishmania (Viannia) braziliensis in a kidney transplant patient. Mem. Inst. Oswaldo Cruz 97:751-753. [DOI] [PubMed] [Google Scholar]
- 140.Gonzalez-Perez, M. P., L. Munoz-Juarez, F. C. Cardenas, J. J. Zarranz Imirizaldu, J. C. Carranceja, and A. Garcia-Saiz. 2003. Human T-cell leukemia virus type I infection in various recipients of transplants from the same donor. Transplantation 75:1006-1011. [DOI] [PubMed] [Google Scholar]
- 141.Gordillo-Paniagua, G., R. Munoz-Arizpe, and R. Ponsa-Molina. 1987. Unusual complication in a patient with renal transplantation: cerebral cysticercosis. Nephron 45:65-67. [DOI] [PubMed] [Google Scholar]
- 142.Gorenflot, A., K. Moubri, E. Precigout, B. Carcy, and T. P. Schetters. 1998. Human babesiosis. Ann. Trop. Med. Parasitol. 92:489-501. [DOI] [PubMed] [Google Scholar]
- 143.Gout, O., M. Baulac, A. Gessain, F. Semah, F. Saal, J. Peries, C. Cabrol, C. Foucault-Fretz, D. Laplane, F. Sigaux, et al. 1990. Rapid development of myelopathy after HTLV-I infection acquired by transfusion during cardiac transplantation. N. Engl. J. Med. 322:383-388. [DOI] [PubMed] [Google Scholar]
- 144.Grant, I. H., J. W. Gold, M. Wittner, H. B. Tanowitz, C. Nathan, K. Mayer, L. Reich, N. Wollner, L. Steinherz, F. Ghavimi, et al. 1989. Transfusion-associated acute Chagas disease acquired in the United States. Ann. Intern. Med. 111:849-851. [DOI] [PubMed] [Google Scholar]
- 145.Gray, N. A., and L. M. Baddour. 2002. Cutaneous inoculation blastomycosis. Clin. Infect. Dis. 34:E44-E49. [DOI] [PubMed] [Google Scholar]
- 146.Grove, D. I. 1996. Human strongyloidiasis. Adv. Parasitol. 38:251-309. [DOI] [PubMed] [Google Scholar]
- 147.Gueco, I., M. Saniel, M. Mendoza, F. Alano, and E. Ona. 1989. Tropical infections after renal transplantation. Transplant. Proc. 21:2105-2107. [PubMed] [Google Scholar]
- 148.Guerin, P. J., P. Olliaro, F. Nosten, P. Druilhe, R. Laxminarayan, F. Binka, W. L. Kilama, N. Ford, and N. J. White. 2002. Malaria: current status of control, diagnosis, treatment, and a proposed agenda for research and development. Lancet Infect. Dis. 2:564-573. [DOI] [PubMed] [Google Scholar]
- 149.Guerrant, R. L., D. H. Walker, and P. F. Weller. 2006. Tropical infectious diseases: principles, patogens and practice. Elsevier Churchill-Livingstone, Philadelphia, PA.
- 150.Gupta, P., R. W. Hurley, P. H. Helseth, J. L. Goodman, and D. E. Hammerschmidt. 1995. Pancytopenia due to hemophagocytic syndrome as the presenting manifestation of babesiosis. Am. J. Hematol. 50:60-62. [DOI] [PubMed] [Google Scholar]
- 151.Gupta, R. K., and M. Jain. 1998. Renal transplantation: potential source of microfilarial transmission. Transplant. Proc. 30:4320-4321. [DOI] [PubMed] [Google Scholar]
- 152.Halim, M. A., O. Alfurayh, M. E. Kalin, S. Dammas, A. al-Eisa, and G. Damanhouri. 1993. Successful treatment of visceral leishmaniasis with allopurinol plus ketoconazole in a renal transplant recipient after the occurrence of pancreatitis due to stibogluconate. Clin. Infect. Dis. 16:397-399. [DOI] [PubMed] [Google Scholar]
- 153.Halkic, N., R. Ksontini, B. Scholl, C. Blanc, T. Kovacsovics, P. Meylan, C. Muheim, M. Gillet, and F. Mosimann. 2004. Recurrent cytomegalovirus disease, visceral leishmaniosis, and Legionella pneumonia after liver transplantation: a case report. Can. J. Anaesth. 51:84-87. [DOI] [PubMed] [Google Scholar]
- 154.Hall, K. A., G. K. Sethi, L. J. Rosado, J. D. Martinez, C. L. Huston, and J. G. Copeland. 1993. Coccidioidomycosis and heart transplantation. J. Heart Lung Transplant. 12:525-526. [PubMed] [Google Scholar]
- 155.Hanchard, B. 1996. Adult T-cell leukemia/lymphoma in Jamaica: 1986-1995. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 13(Suppl. 1):S20-S25. [DOI] [PubMed] [Google Scholar]
- 156.Haque, R., C. D. Huston, M. Hughes, E. Houpt, and W. A. Petri, Jr. 2003. Amebiasis. N. Engl. J. Med. 348:1565-1573. [DOI] [PubMed] [Google Scholar]
- 157.Haque, R., N. U. Mollah, I. K. Ali, K. Alam, A. Eubanks, D. Lyerly, and W. A. Petri, Jr. 2000. Diagnosis of amebic liver abscess and intestinal infection with the TechLab Entamoeba histolytica II antigen detection and antibody tests. J. Clin. Microbiol. 38:3235-3239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Hardinger, K. L., B. Miller, G. A. Storch, N. M. Desai, and D. C. Brennan. 2003. West Nile virus-associated meningoencephalitis in two chronically immunosuppressed renal transplant recipients. Am. J. Transplant. 3:1312-1315. [DOI] [PubMed] [Google Scholar]
- 159.Harrington, T., M. J. Kuehnert, H. Kamel, R. S. Lanciotti, S. Hand, M. Currier, M. E. Chamberland, L. R. Petersen, and A. A. Marfin. 2003. West Nile virus infection transmitted by blood transfusion. Transfusion 43:1018-1022. [DOI] [PubMed] [Google Scholar]
- 160.Hayes, E. B., N. Komar, R. S. Nasci, S. P. Montgomery, D. R. O'Leary, and G. L. Campbell. 2005. Epidemiology and transmission dynamics of West Nile virus disease. Emerg. Infect. Dis. 11:1167-1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Hayes, E. B., J. J. Sejvar, S. R. Zaki, R. S. Lanciotti, A. V. Bode, and G. L. Campbell. 2005. Virology, pathology, and clinical manifestations of West Nile virus disease. Emerg. Infect. Dis. 11:1174-1179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Hellenbrand, W., C. Meyer, G. Rasch, I. Steffens, and A. Ammon. 2005. Cases of rabies in Germany following organ transplantation. Eur. Surveill. 10:E050224. [DOI] [PubMed] [Google Scholar]
- 163.Henrard, D. R., V. Soriano, E. Robertson, M. Gutierrez, J. Stephens, F. Dronda, F. Miles, E. Pujol, M. Buytendorp, A. Castro, and the HTLV-1 and HTLV-2 Spanish Study Group. 1995. Prevalence of human T-cell lymphotropic virus type 1 (HTLV-1) and HTLV-2 infection among Spanish drug users measured by HTLV-1 assay and HTLV-1 and -2 assay. J. Clin. Microbiol. 33:1735-1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Hernandez-Perez, J., M. Yebra-Bango, E. Jimenez-Martinez, C. Sanz-Moreno, V. Cuervas-Mons, P. L. Alonso, A. Ramos-Martinez, and J. Fernandez-Fernandez. 1999. Visceral leishmaniasis (kala-azar) in solid organ transplantation: report of five cases and review. Clin. Infect. Dis. 29:918-921. [DOI] [PubMed] [Google Scholar]
- 165.Herwaldt, B., D. H. Persing, E. A. Precigout, W. L. Goff, D. A. Mathiesen, P. W. Taylor, M. L. Eberhard, and A. F. Gorenflot. 1996. A fatal case of babesiosis in Missouri: identification of another piroplasm that infects humans. Ann. Intern. Med. 124:643-650. [DOI] [PubMed] [Google Scholar]
- 166.Herwaldt, B. L. 2003. Molecular characterization of a non-Babesia divergens organism causing zoonotic babesiosis in Europe. Emerg. Infect. Dis. 9:942-948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Herwaldt, B. L., A. M. Kjemtrup, P. A. Conrad, R. C. Barnes, M. Wilson, M. G. McCarthy, M. H. Sayers, and M. L. Eberhard. 1997. Transfusion-transmitted babesiosis in Washington State: first reported case caused by a WA1-type parasite. J. Infect. Dis. 175:1259-1262. [DOI] [PubMed] [Google Scholar]
- 168.Hira, P. R., and S. F. Husein. 1979. Some transfusion-induced parasitic infections in Zambia. J. Hyg. Epidemiol. Microbiol. Immunol. 23:436-444. [PubMed] [Google Scholar]
- 169.Ho, J. K., W. Y. Lau, K. Liu, N. Leung, T. Leung, C. T. Liew, and A. K. Li. 1994. Liver infested with Clonorchis sinensis in orthotopic liver transplantation: a case report. Transplant. Proc. 26:2269-2271. [PubMed] [Google Scholar]
- 170.Hoare, M., W. T. Gelson, N. Antoun, and G. J. Alexander. 2006. Early recurrence of neurocysticercosis after orthotopic liver transplant. Liver Transpl. 12:490-491. [DOI] [PubMed] [Google Scholar]
- 171.Hoare, M., W. T. Gelson, S. E. Davies, M. Curran, and G. J. Alexander. 2005. Hepatic and intestinal schistosomiasis after orthotopic liver transplant. Liver Transpl. 11:1603-1607. [DOI] [PubMed] [Google Scholar]
- 172.Hoerauf, A. 2006. New strategies to combat filariasis. Expert Rev. Anti. Infect. Ther. 4:211-222. [DOI] [PubMed] [Google Scholar]
- 173.Holt, C. D., D. J. Winston, B. Kubak, D. K. Imagawa, P. Martin, L. Goldstein, K. Olthoff, J. M. Millis, A. Shaked, C. R. Shackleton, and R. W. Busuttil. 1997. Coccidioidomycosis in liver transplant patients. Clin. Infect. Dis. 24:216-221. [DOI] [PubMed] [Google Scholar]
- 174.Holzer, B. R., Z. Gluck, D. Zambelli, and M. Fey. 1985. Transmission of malaria by renal transplantation. Transplantation 39:315-316. [DOI] [PubMed] [Google Scholar]
- 175.Homer, M. J., I. Guilar-Delfin, S. R. Telford III, P. J. Krause, and D. H. Persing. 2000. Babesiosis. Clin. Microbiol. Rev. 13:451-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Horber, F. F., J. P. Lerut, J. Reichen, A. Zimmermann, P. Jaeger, and R. Malinverni. 1993. Visceral leishmaniasis after orthotopic liver transplantation: impact of persistent splenomegaly. Transpl. Int. 6:55-57. [DOI] [PubMed] [Google Scholar]
- 177.Hoshida, Y., T. Li, Z. Dong, Y. Tomita, A. Yamauchi, J. Hanai, and K. Aozasa. 2001. Lymphoproliferative disorders in renal transplant patients in Japan. Int. J. Cancer 91:869-875. [DOI] [PubMed] [Google Scholar]
- 178.Houff, S. A., R. C. Burton, R. W. Wilson, T. E. Henson, W. T. London, G. M. Baer, L. J. Anderson, W. G. Winkler, D. L. Madden, and J. L. Sever. 1979. Human-to-human transmission of rabies virus by corneal transplant. N. Engl. J. Med. 300:603-604. [DOI] [PubMed] [Google Scholar]
- 179.Hoy, W. E., N. J. Roberts, Jr., M. F. Bryson, C. Bowles, J. C. Lee, A. J. Rivero, and A. L. Ritterson. 1981. Transmission of strongyloidiasis by kidney transplant? Disseminated strongyloidiasis in both recipients of kidney allografts from a single cadaver donor. JAMA 246:1937-1939. [PubMed] [Google Scholar]
- 180.Hsueh, P. R., L. J. Teng, C. C. Hung, J. H. Hsu, P. C. Yang, S. W. Ho, and K. T. Luh. 2000. Molecular evidence for strain dissemination of Penicillium marneffei: an emerging pathogen in Taiwan. J. Infect. Dis. 181:1706-1712. [DOI] [PubMed] [Google Scholar]
- 181.Hubalek, Z., and J. Halouzka. 1999. West Nile fever—a reemerging mosquito-borne viral disease in Europe. Emerg. Infect. Dis. 5:643-650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Hueso, M., J. Bover, D. Seron, S. Gil-Vernet, G. Rufi, J. Alsina, and J. M. Grinyo. 1999. The renal transplant patient with visceral leishmaniasis who could not tolerate meglumine antimoniate-cure with ketoconazole and allopurinol. Nephrol. Dial. Transplant. 14:2941-2943. [DOI] [PubMed] [Google Scholar]
- 183.Hung, C. C., S. C. Chang, Y. C. Chen, T. S. Yen, and W. C. Hsieh. 1994. Plasmodium vivax infection in a renal transplant recipient: report of a case. J. Formos. Med. Assoc. 93:888-889. [PubMed] [Google Scholar]
- 184.Hussein, M. M., J. M. Mooij, H. M. Roujouleh, O. A. Hamour, and H. Felemban. 2001. Non-typhoid Salmonella septicemia and visceral leishmaniasis in a renal transplant patient. Transplantation 71:479-481. [DOI] [PubMed] [Google Scholar]
- 185.Hwang, Y. J., Y. I. Kim, Y. K. Yun, and J. W. Kim. 2000. Use of liver graft infested with Clonorchis sinensis for living related liver transplantation: a case report. Transplant. Proc. 32:2182-2183. [DOI] [PubMed] [Google Scholar]
- 186.Ichikawa, Y., M. Iida, C. Ebisui, C. Fujio, K. Yazawa, T. Hanafusa, T. Kouro, K. Seki, and S. Nagano. 2000. A case study of adult T-cell lymphoma in a kidney transplant patient. Transplant. Proc. 32:1982-1983. [DOI] [PubMed] [Google Scholar]
- 187.Igra-Siegman, Y., R. Kapila, P. Sen, Z. C. Kaminski, and D. B. Louria. 1981. Syndrome of hyperinfection with Strongyloides stercoralis. Rev. Infect. Dis. 3:397-407. [DOI] [PubMed] [Google Scholar]
- 188.Inaba, S., K. Okochi, H. Sato, K. Fukada, N. Kinukawa, H. Nakata, K. Kinjyo, F. Fujii, and Y. Maeda. 1999. Efficacy of donor screening for HTLV-I and the natural history of transfusion-transmitted infection. Transfusion 39:1104-1110. [DOI] [PubMed] [Google Scholar]
- 189.International Organization for Migration. 2007. Migration in the twenty-first century. Facts and figures. Global estimates and trends. International Organization for Migration, Geneva, Switzerland. http://www.iom.int/jahia/page254.html.
- 190.Iwamoto, M., D. B. Jernigan, A. Guasch, M. J. Trepka, C. G. Blackmore, W. C. Hellinger, S. M. Pham, S. Zaki, R. S. Lanciotti, S. E. Lance-Parker, C. A. DiazGranados, A. G. Winquist, C. A. Perlino, S. Wiersma, K. L. Hillyer, J. L. Goodman, A. A. Marfin, M. E. Chamberland, L. R. Petersen, et al. 2003. Transmission of West Nile virus from an organ donor to four transplant recipients. N. Engl. J. Med. 348:2196-2203. [DOI] [PubMed] [Google Scholar]
- 191.Iwasaki, Y. 1990. Pathology of chronic myelopathy associated with HTLV-I infection (HAM/TSP). J. Neurol. Sci. 96:103-123. [DOI] [PubMed] [Google Scholar]
- 192.Iwasaki, Y. 1993. Human T cell leukemia virus type I infection and chronic myelopathy. Brain Pathol. 3:1-10. [DOI] [PubMed] [Google Scholar]
- 193.Javadi, M. A., A. Fayaz, S. A. Mirdehghan, and B. Ainollahi. 1996. Transmission of rabies by corneal graft. Cornea 15:431-433. [DOI] [PubMed] [Google Scholar]
- 194.Jenks, P. J., W. Y. Barrett, M. J. Raftery, S. M. Kelsey, J. D. van der Walt, S. P. Kon, and J. Breuer. 1995. Development of human T-cell lymphotropic virus type I-associated adult T-cell leukemia/lymphoma during immunosuppressive treatment following renal transplantation. Clin. Infect. Dis. 21:992-993. [DOI] [PubMed] [Google Scholar]
- 195.Jimenez Jimenez, F. J., J. A. Molina Arjona, F. Zancada, J. Santos, M. A. Roldan, and B. A. Fernandez. 1990. Etiology of late-onset epilepsy. A prospective study in an area of rural health care. Med. Clin. (Barcelona) 94:521-524. (In Spanish.) [PubMed] [Google Scholar]
- 196.Jiménez Romero, C., E. Moreno Gonzáles, I. García García, C. Loinaz Sequrola, I. González Pinto, R. Gomez Sanz, D. Hernández-Gallardo, and C. Moreno Sanz. 1995. Successful transplantation of a liver graft with a calcified hydatid cyst after back-table resection. Transplantation 60:883-884. [PubMed] [Google Scholar]
- 197.Johnson, A. J., S. Langevin, K. L. Wolff, and N. Komar. 2003. Detection of anti-West Nile virus immunoglobulin M in chicken serum by an enzyme-linked immunosorbent assay. J. Clin. Microbiol. 41:2002-2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Johnston, I. D. 1981. Possible transmission of malaria by renal transplantation. Br. Med. J. 282:780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Jokipii, L., K. Salmela, H. Saha, H. Kyronseppa, B. Eklund, D. Evans, E. von Willebrand, and A. M. Jokipii. 1992. Leishmaniasis diagnosed from bronchoalveolar lavage. Scand. J. Infect. Dis. 24:677-681. [DOI] [PubMed] [Google Scholar]
- 200.Kakaiya, R. 16 August 2007, accession date. Transfusion-transmitted West Nile infection update. Transfusion medicine update. Institute for Transfusion Medicine, Pittsburgh, PA. www.itxm.org.
- 201.Kasiske, B. L., M. Ravenscraft, E. L. Ramos, R. S. Gaston, M. J. Bia, G. M. Danovitch, et al. 1996. The evaluation of living renal transplant donors: clinical practice guidelines. J. Am. Soc. Nephrol. 7:2288-2313. [DOI] [PubMed] [Google Scholar]
- 202.Kauffman, C. A. 2003. Histoplasmosis, p. 285-298. In W. E. Dismukes, P. G. Pappas, and J. D. Sobel (ed.), Clinical mycology. Oxford University Press, New York, NY.
- 203.Kauffman, C. A. 2006. Endemic mycoses: blastomycosis, histoplasmosis, and sporotrichosis. Infect. Dis. Clin. N. Am. 20:645-662. [DOI] [PubMed] [Google Scholar]
- 204.Kauffman, H. M., and S. E. Taranto. 2003. Human T-cell lymphotrophic virus type-1 and organ donors. Transplantation 76:745-746. [DOI] [PubMed] [Google Scholar]
- 205.Khabbaz, R. F., I. M. Onorato, R. O. Cannon, T. M. Hartley, B. Roberts, B. Hosein, and J. E. Kaplan. 1992. Seroprevalence of HTLV-1 and HTLV-2 among intravenous drug users and persons in clinics for sexually transmitted diseases. N. Engl. J. Med. 326:375-380. [DOI] [PubMed] [Google Scholar]
- 206.Kher, V., A. K. Ghosh, A. Gupta, P. Arora, and T. N. Dhole. 1991. Visceral leishmaniasis: an unusual case of fever in a renal transplant recipient. Nephrol. Dial. Transplant. 6:736-738. [DOI] [PubMed] [Google Scholar]
- 207.Kiberd, B. A., and K. Forward. 2004. Screening for West Nile virus in organ transplantation: a medical decision analysis. Am. J. Transplant. 4:1296-1301. [DOI] [PubMed] [Google Scholar]
- 208.Kirchhoff, L. V. 1993. American trypanosomiasis (Chagas’ disease)—a tropical disease now in the United States. N. Engl. J. Med. 329:639-644. [DOI] [PubMed] [Google Scholar]
- 209.Kirchhoff, L. V., P. Paredes, A. Lomeli-Guerrero, M. Paredes-Espinoza, C. S. Ron-Guerrero, M. Gado-Mejia, and J. G. Pena-Munoz. 2006. Transfusion-associated Chagas disease (American trypanosomiasis) in Mexico: implications for transfusion medicine in the United States. Transfusion 46:298-304. [DOI] [PubMed] [Google Scholar]
- 210.Kleinschmidt-DeMasters, B. K., B. A. Marder, M. E. Levi, S. P. Laird, J. T. McNutt, E. J. Escott, G. T. Everson, and K. L. Tyler. 2004. Naturally acquired West Nile virus encephalomyelitis in transplant recipients: clinical, laboratory, diagnostic, and neuropathological features. Arch. Neurol. 61:1210-1220. [DOI] [PubMed] [Google Scholar]
- 211.Koch, S., S. Bresson-Hadni, J. P. Miguet, J. P. Crumbach, M. Gillet, G. A. Mantion, B. Heyd, D. A. Vuitton, A. Minello, and S. Kurtz. 2003. Experience of liver transplantation for incurable alveolar echinococcosis: a 45-case European collaborative report. Transplantation 75:856-863. [DOI] [PubMed] [Google Scholar]
- 212.Komar, N., and G. G. Clark. 2006. West Nile virus activity in Latin America and the Caribbean. Rev. Panam. Salud Publica 19:112-117. [DOI] [PubMed] [Google Scholar]
- 213.Kramer, M. H., C. J. Lerner, and G. S. Visvesvara. 1997. Kidney and liver transplants from a donor infected with Naegleria fowleri. J. Clin. Microbiol. 35:1032-1033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Kumar, D., M. A. Drebot, S. J. Wong, G. Lim, H. Artsob, P. Buck, and A. Humar. 2004. A seroprevalence study of West Nile virus infection in solid organ transplant recipients. Am. J. Transplant. 4:1883-1888. [DOI] [PubMed] [Google Scholar]
- 215.Kumar, D., G. V. Prasad, J. Zaltzman, G. A. Levy, and A. Humar. 2004. Community-acquired West Nile virus infection in solid-organ transplant recipients. Transplantation 77:399-402. [DOI] [PubMed] [Google Scholar]
- 216.Kusne, S., and J. Smilack. 2005. Transmission of West Nile virus by organ transplantation. Liver Transpl. 11:239-241. [DOI] [PubMed] [Google Scholar]
- 217.Kusne, S., and J. Smilack. 2005. Transmission of rabies virus from an organ donor to four transplant recipients. Liver Transpl. 11:1295-1297. [DOI] [PubMed] [Google Scholar]
- 218.Kuzoe, F. A. 1993. Current situation of African trypanosomiasis. Acta Trop. 54:153-162. [DOI] [PubMed] [Google Scholar]
- 219.Lamas, S., L. Orte, F. Parras, L. J. Garcia, R. Matesanz, and J. Ortuno. 1987. Non-fatal leishmaniasis in a renal transplant recipient. Nephron 45:71. [DOI] [PubMed] [Google Scholar]
- 220.Leapman, S. B., J. B. Rosenberg, R. S. Filo, and E. J. Smith. 1980. Strongyloides stercoralis in chronic renal failure: safe therapy with thiabendazole. South. Med. J. 73:1400-1402. [DOI] [PubMed] [Google Scholar]
- 221.Le Cacheux, P., B. H. de Ligny, O. Reman, and J. P. Ryckelynck. 1990. Visceral leishmaniasis of favourable course in a patient with renal transplantation. Rev. Med. Interne 11:250-251. (In French.) [PubMed] [Google Scholar]
- 222.Lee, K. W., J. W. Joh, S. J. Kim, J. H. Park, S. E. Chon, S. H. Choi, J. S. Heo, J. H. Song, S. M. Kim, K. R. Peck, Y. I. Kim, B. B. Lee, and S. K. Lee. 2003. Living donor liver transplantation using graft infested with Clonorchis sinensis: two cases. Transplant. Proc. 35:66-67. [DOI] [PubMed] [Google Scholar]
- 223.Lee, P. C., P. Y. Lee, H. Y. Lei, F. F. Chen, J. Y. Tseng, and Y. T. Ching. 1994. Malaria infection in kidney transplant recipients. Transplant. Proc. 26:2099-2100. [PubMed] [Google Scholar]
- 224.Lefavour, G. S., J. C. Pierce, and J. D. Frame. 1980. Renal transplant-associated malaria. JAMA 244:1820-1821. [DOI] [PubMed] [Google Scholar]
- 225.Leiby, D. A., R. M. Herron, Jr., E. J. Read, B. A. Lenes, and R. J. Stumpf. 2002. Trypanosoma cruzi in Los Angeles and Miami blood donors: impact of evolving donor demographics on seroprevalence and implications for transfusion transmission. Transfusion 42:549-555. [DOI] [PubMed] [Google Scholar]
- 226.Leiby, D. A., B. A. Lenes, M. A. Tibbals, and M. T. Tames-Olmedo. 1999. Prospective evaluation of a patient with Trypanosoma cruzi infection transmitted by transfusion. N. Engl. J. Med. 341:1237-1239. [DOI] [PubMed] [Google Scholar]
- 227.Limaye, A. P., P. A. Connolly, M. Sagar, T. R. Fritsche, B. T. Cookson, L. J. Wheat, and W. E. Stamm. 2000. Transmission of Histoplasma capsulatum by organ transplantation. N. Engl. J. Med. 343:1163-1166. [DOI] [PubMed] [Google Scholar]
- 228.Liu, L. X., and P. F. Weller. 1993. Strongyloidiasis and other intestinal nematode infections. Infect. Dis. Clin. N. Am. 7:655-682. [PubMed] [Google Scholar]
- 229.Llorente, S., L. Gimeno, M. J. Navarro, S. Moreno, and M. Rodriguez-Girones. 2000. Therapy of visceral leishmaniasis in renal transplant recipients intolerant to pentavalent antimonials. Transplantation 70:800-801. [DOI] [PubMed] [Google Scholar]
- 230.Lu, S. C., and B. H. Chen. 2003. Seroindeterminate HTLV-1 prevalence and characteristics in blood donors in Taiwan. Int. J. Hematol. 77:412-413. [DOI] [PubMed] [Google Scholar]
- 231.Luquetti, A. O., C. Ponce, E. Ponce, J. Esfandiari, A. Schijman, S. Revollo, N. Añez, B. Zingales, R. Ramgel-Aldao, A. Gonzalez, M. J. Levin, E. S. Umezawa, and J. Franco da Silveira. 2003. Chagas’ disease diagnosis: a multicentric evaluation of Chagas Stat-Pak, a rapid immunochromatographic assay with recombinant proteins of Trypanosoma cruzi. Diagn. Microbiol. Infect. Dis. 46:265-271. [DOI] [PubMed] [Google Scholar]
- 232.Lux, J. Z., D. Weiss, J. V. Linden, D. Kessler, B. L. Herwaldt, S. J. Wong, J. Keithly, P. Della-Latta, and B. E. Scully. 2003. Transfusion-associated babesiosis after heart transplant. Emerg. Infect. Dis. 9:116-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 233.Ma, D. D., A. J. Concannon, and J. Hayes. 1979. Fatal leishmaniasis in renal-transport patient. Lancet ii:311-312. [DOI] [PubMed] [Google Scholar]
- 234.Ma, P., G. S. Visvesvara, A. J. Martinez, F. H. Theodore, P. M. Daggett, and T. K. Sawyer. 1990. Naegleria and Acanthamoeba infections: review. Rev. Infect. Dis. 12:490-513. [DOI] [PubMed] [Google Scholar]
- 235.MacKenzie, W. R., J. P. Davis, D. E. Peterson, A. J. Hibbard, G. Becker, and B. S. Zarvan. 1992. Multiple false-positive serologic tests for HIV, HTLV-1, and hepatitis C following influenza vaccination, 1991. JAMA 268:1015-1017. [PubMed] [Google Scholar]
- 236.Mahmoud, K. M., M. A. Sobh, A. E. El-Agroudy, F. E. Mostafa, M. E. Baz, A. A. Shokeir, and M. A. Ghoneim. 2001. Impact of schistosomiasis on patient and graft outcome after renal transplantation: 10 years’ follow-up. Nephrol. Dial. Transplant. 16:2214-2221. [DOI] [PubMed] [Google Scholar]
- 237.Maldonado, C., S. Albano, L. Vettorazzi, O. Salomone, J. C. Zlocowski, C. Abiega, M. Amuchastegui, R. Cordoba, and T. Alvarellos. 2004. Using polymerase chain reaction in early diagnosis of re-activated Trypanosoma cruzi infection after heart transplantation. J. Heart Lung Transplant. 23:1345-1348. [DOI] [PubMed] [Google Scholar]
- 238.Malek Hosseini, S. A., R. Javid, H. Salahi, N. Nezakatgoo, E. Ahmad, and N. Ghahramani. 1995. A case report of kala-azar in a kidney transplant patient. Transplant. Proc. 27:2715. [PubMed] [Google Scholar]
- 239.Manns, A., M. Hisada, and L. La Grenade. 1999. Human T-lymphotropic virus type I infection. Lancet 353:1951-1958. [DOI] [PubMed] [Google Scholar]
- 240.Manns, A., R. J. Wilks, E. L. Murphy, G. Haynes, J. P. Figueroa, M. Barnett, B. Hanchard, and W. A. Blattner. 1992. A prospective study of transmission by transfusion of HTLV-I and risk factors associated with seroconversion. Int. J. Cancer 51:886-891. [DOI] [PubMed] [Google Scholar]
- 241.Marathe, A., J. Tripathi, V. Handa, and V. Date. 2005. Human babesiosis—a case report. Ind. J. Med. Microbiol. 23:267-269. [PubMed] [Google Scholar]
- 242.Martins, T. B., T. D. Jaskowski, C. L. Mouritsen, and H. R. Hill. 1995. Comparison of commercially available enzyme immunoassay with traditional serological tests for detection of antibodies to Coccidioides immitis. J. Clin. Microbiol. 33:940-943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.Mejia, G. A., C. A. Alvarez, H. H. Pulido, B. Ramirez, C. Cardozo, Y. Suarez, R. Lobelo, T. Sarquis, and A. M. Uribe. 2006. Malaria in a liver transplant recipient: a case report. Transplant. Proc. 38:3132-3134. [DOI] [PubMed] [Google Scholar]
- 244.Melrose, W. D. 2002. Lymphatic filariasis: new insights into an old disease. Int. J. Parasitol. 32:947-960. [DOI] [PubMed] [Google Scholar]
- 245.Menichetti, F., M. L. Bindi, C. Tascini, L. Urbani, G. Biancofiore, R. Doria, M. Esposito, R. Mozzo, G. Catalano, and F. Filipponi. 2006. Fever, mental impairment, acute anemia, and renal failure in patient undergoing orthotopic liver transplantation: posttransplantation malaria. Liver Transpl. 12:674-676. [DOI] [PubMed] [Google Scholar]
- 246.Meyer, K. C., E. J. McManus, and D. G. Maki. 1993. Overwhelming pulmonary blastomycosis associated with the adult respiratory distress syndrome. N. Engl. J. Med. 329:1231-1236. [DOI] [PubMed] [Google Scholar]
- 247.Meyers, A. M., D. J. Shapiro, F. J. Milne, J. A. Myburgh, and R. Rabkin. 1976. Strongyloides stercoralis hyperinfection in a renal allograft recipient. S. Afr. Med. J. 50:1301-1302. [PubMed] [Google Scholar]
- 248.Mileno, M. D., and F. J. Bia. 1998. The compromised traveler. Infect. Dis. Clin. N. Am. 12:369-412. [DOI] [PubMed] [Google Scholar]
- 249.Miller, M. B., R. Hendren, and P. H. Gilligan. 2004. Posttransplantation disseminated coccidioidomycosis acquired from donor lungs. J. Clin. Microbiol. 42:2347-2349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Mirzabeigi, M., U. Farooq, S. Baraniak, L. Dowdy, G. Ciancio, and V. Vincek. 2006. Reactivation of dormant cutaneous Leishmania infection in a kidney transplant patient. J. Cutan. Pathol. 33:701-704. [DOI] [PubMed] [Google Scholar]
- 251.Mittal, R., S. Saxena, S. Guleria, S. K. Mittal, S. K. Agarwal, S. C. Tiwari, and S. C. Dash. 1995. Visceral leishmaniasis: a rare cause of unexplained pyrexia in a renal allograft recipient. Nephron 70:123-124. [DOI] [PubMed] [Google Scholar]
- 252.Miyoshi, I., N. Murata, H. Machida, and H. Taguchi. 1995. Transmission of human T-lymphotrophic virus type 1 by bone marrow transplantation. Br. J. Haematol. 89:690-691. [DOI] [PubMed] [Google Scholar]
- 253.Montgomery, S. P., J. A. Brown, M. Kuehnert, T. L. Smith, N. Crall, R. S. Lanciotti, A. Macedo de Oliveira, T. Boo, and A. A. Marfin. 2006. Transfusion-associated transmission of West Nile virus, United States 2003 through 2005. Transfusion 46:2038-2046. [DOI] [PubMed] [Google Scholar]
- 254.Moody, A. 2002. Rapid diagnostic tests for malaria parasites. Clin. Microbiol. Rev. 15:66-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Morales, P., J. J. Torres, M. Salavert, J. Peman, J. Lacruz, and A. Sole. 2003. Visceral leishmaniasis in lung transplantation. Transplant. Proc. 35:2001-2003. [DOI] [PubMed] [Google Scholar]
- 256.Moreno-Gonzalez, E., S. C. Loinaz, M. A. Garcia Urena, G. Garcia, I. S. R. Gomez, R. C. Jimenez, P. Gonzalez, I. M. A. Corral Sanchez, and C. F. Palma. 1994. Liver transplantation for Echinococcus granulosus hydatid disease. Transplantation 58:797-800. [PubMed] [Google Scholar]
- 257.Morgan, J. S., W. Schaffner, and W. J. Stone. 1986. Opportunistic strongyloidiasis in renal transplant recipients. Transplantation 42:518-524. [DOI] [PubMed] [Google Scholar]
- 258.Moroni, G., and L. Bossi. 1995. Don't forget visceral leishmaniasis in transplant patients. Nephrol. Dial. Transplant. 10:563-564. [DOI] [PubMed] [Google Scholar]
- 259.Motta, A. C., R. Galo, A. G. Lourenco, M. C. Komesu, D. Arruda, F. G. Velasco, B. C. Garcia, and N. T. Foss. 2006. Unusual orofacial manifestations of histoplasmosis in renal transplanted patient. Mycopathologia 161:161-165. [DOI] [PubMed] [Google Scholar]
- 260.Moulin, B., J. Ollier, D. Bouchouareb, R. Purgus, and M. Olmer. 1992. Leishmaniasis: a rare cause of unexplained fever in a renal graft recipient. Nephron 60:360-362. [DOI] [PubMed] [Google Scholar]
- 261.Mueller, N. 1991. The epidemiology of HTLV-I infection. Cancer Causes Control 2:37-52. [DOI] [PubMed] [Google Scholar]
- 262.Mueller, N., A. Okayama, S. Stuver, and N. Tachibana. 1996. Findings from the Miyazaki Cohort Study. J. Acquir. Immune Defic. Syndr. Hum. Retrovirol. 13(Suppl. 1):S2-S7. [DOI] [PubMed] [Google Scholar]
- 263.Murphy, E. L., B. Hanchard, J. P. Figueroa, W. N. Gibbs, W. S. Lofters, M. Campbell, J. J. Goedert, and W. A. Blattner. 1989. Modelling the risk of adult T-cell leukemia/lymphoma in persons infected with human T-lymphotropic virus type I. Int. J. Cancer 43:250-253. [DOI] [PubMed] [Google Scholar]
- 264.Murphy, E. L., K. Watanabe, C. C. Nass, H. Ownby, A. Williams, and G. Nemo. 1999. Evidence among blood donors for a 30-year-old epidemic of human T lymphotropic virus type II infection in the United States. J. Infect. Dis. 180:1777-1783. [DOI] [PubMed] [Google Scholar]
- 265.Murtagh, B., Y. Wadia, G. Messner, P. Allison, Y. Harati, and R. Delgado. 2005. West Nile virus infection after cardiac transplantation. J. Heart Lung Transplant. 24:774-776. [DOI] [PubMed] [Google Scholar]
- 266.Nakamura, N., Y. Arakaki, H. Sunagawa, Y. Shiohira, H. Uehara, T. Miyasato, Y. Koyama, Y. Ogawa, and T. Kowatari. 1998. Influence of immunosuppression in HTLV-1-positive renal transplant recipients. Transplant. Proc. 30:1324-1326. [DOI] [PubMed] [Google Scholar]
- 267.Nakatsuji, Y., F. Sugai, S. Watanabe, M. Kaido, K. Koguchi, K. Abe, and S. Sakoda. 2000. HTLV-I-associated myelopathy manifested after renal transplantation. J. Neurol. Sci. 177:154-156. [DOI] [PubMed] [Google Scholar]
- 268.Nanduri, J., and J. W. Kazura. 1989. Clinical and laboratory aspects of filariasis. Clin. Microbiol. Rev. 2:39-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 269.Nowicki, M. J., C. Chinchilla, L. Corado, L. Matsuoka, R. Selby, F. Steurer, T. Mone, R. Mendez, and S. Aswad. 2006. Prevalence of antibodies to Trypanosoma cruzi among solid organ donors in Southern California: a population at risk. Transplantation 81:477-479. [DOI] [PubMed] [Google Scholar]
- 270.Nuesch, R., E. Cynke, M. C. Jost, and W. Zimmerli. 2000. Thrombocytopenia after kidney transplantation. Am. J. Kidney Dis. 35:537-538. [DOI] [PubMed] [Google Scholar]
- 271.Okochi, K., H. Sato, and Y. Hinuma. 1984. A retrospective study on transmission of adult T cell leukemia virus by blood transfusion: seroconversion in recipients. Vox Sang. 46:245-253. [DOI] [PubMed] [Google Scholar]
- 272.Olmeda, A. S., P. M. Armstrong, B. M. Rosenthal, B. Valladares, A. del Castillo, F. de Armas, M. Miguelez, A. Gonzalez, J. A. Rodriguez Rodriguez, A. Spielman, and S. R. Telford III. 1997. A subtropical case of human babesiosis. Acta Trop. 67:229-234. [DOI] [PubMed] [Google Scholar]
- 273.Orland, J. R., J. Engstrom, J. Fridey, R. A. Sacher, J. W. Smith, C. Nass, G. Garratty, B. Newman, D. Smith, B. Wang, K. Loughlin, and E. L. Murphy. 2003. Prevalence and clinical features of HTLV neurologic disease in the HTLV Outcomes Study. Neurology 61:1588-1594. [DOI] [PubMed] [Google Scholar]
- 274.Orofino, L., R. Marcen, C. Gamez, L. Orte, R. Lopez-Velez, C. Quereda, and J. Ortuno. 1992. Visceral leishmaniasis in renal transplant patients. Nephrol. Dial. Transplant. 7:651. [DOI] [PubMed] [Google Scholar]
- 275.Otero, A. C., V. O. da Silva, K. G. Luz, M. Palatnik, C. Pirmez, O. Fernandes, and C. B. Palatnik de Sousa. 2000. Occurrence of Leishmania donovani DNA in donated blood from seroreactive Brazilian blood donors. Am. J. Trop. Med. Hyg. 62:128-131. [DOI] [PubMed] [Google Scholar]
- 276.Ottesen, E. A. 2006. Lymphatic filariasis: treatment, control and elimination. Adv. Parasitol. 61:395-441. [DOI] [PubMed] [Google Scholar]
- 277.Palau, L. A., and S. A. Kemmerly. 1997. First report of invasive amebiasis in an organ transplant recipient. Transplantation 64:936-937. [DOI] [PubMed] [Google Scholar]
- 278.Palau, L. A., and G. A. Pankey. 1997. Strongyloides hyperinfection in a renal transplant recipient receiving cyclosporine: possible Strongyloides stercoralis transmission by kidney transplant. Am. J. Trop. Med. Hyg. 57:413-415. [DOI] [PubMed] [Google Scholar]
- 279.Pannegeon, V., J. P. Masini, F. Paye, O. Chazouilleres, and P. M. Girard. 2005. Schistosoma mansoni infection and liver graft. Transplantation 80:287. [DOI] [PubMed] [Google Scholar]
- 280.Pappagianis, D. 2001. Serologic studies in coccidioidomycosis. Semin. Respir. Infect. 16:242-250. [DOI] [PubMed] [Google Scholar]
- 281.Pappas, P. G. 1997. Blastomycosis in the immunocompromised patient. Semin. Respir. Infect. 12:243-251. [PubMed] [Google Scholar]
- 282.Pappas, P. G., J. C. Pottage, W. G. Powderly, V. J. Fraser, C. W. Stratton, S. McKenzie, M. L. Tapper, H. Chmel, F. C. Bonebrake, R. Blum, et al. 1992. Blastomycosis in patients with the acquired immunodeficiency syndrome. Ann. Intern. Med. 116:847-853. [DOI] [PubMed] [Google Scholar]
- 283.Pappas, P. G., M. G. Threlkeld, G. D. Bedsole, K. O. Cleveland, M. S. Gelfand, and W. E. Dismukes. 1993. Blastomycosis in immunocompromised patients. Medicine (Baltimore) 72:311-325. [DOI] [PubMed] [Google Scholar]
- 284.Patel, R., and C. V. Paya. 1997. Infections in solid-organ transplant recipients. Clin. Microbiol. Rev. 10:86-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Pealer, L. N., A. A. Marfin, L. R. Petersen, R. S. Lanciotti, P. L. Page, S. L. Stramer, M. G. Stobierski, K. Signs, B. Newman, H. Kapoor, J. L. Goodman, and M. E. Chamberland. 2003. Transmission of West Nile virus through blood transfusion in the United States in 2002. N. Engl. J. Med. 349:1236-1245. [DOI] [PubMed] [Google Scholar]
- 286.Peddi, V. R., S. Hariharan, and M. R. First. 1996. Disseminated histoplasmosis in renal allograft recipients. Clin. Transplant. 10:160-165. [PubMed] [Google Scholar]
- 287.Peleg, A. Y., S. Husain, E. J. Kwak, F. P. Silveira, M. Ndirangu, J. Tran, K. A. Shutt, R. Shapiro, N. Thai, K. bu-Elmagd, K. R. McCurry, A. Marcos, and D. L. Paterson. 2007. Opportunistic infections in 547 organ transplant recipients receiving alemtuzumab, a humanized monoclonal CD-52 antibody. Clin. Infect. Dis. 44:204-212. [DOI] [PubMed] [Google Scholar]
- 288.Perdrizet, G. A., N. H. Olson, P. J. Krause, G. T. Banever, A. Spielman, and R. G. Cable. 2000. Babesiosis in a renal transplant recipient acquired through blood transfusion. Transplantation 70:205-208. [PubMed] [Google Scholar]
- 289.Pereira, M. E., L. M. Santos, M. S. Araujo, and Z. Brener. 1996. Recrudescence induced by cyclophosphamide of chronic Trypanosoma cruzi infection in mice is influenced by the parasite strain. Mem. Inst. Oswaldo Cruz 91:71-74. [DOI] [PubMed] [Google Scholar]
- 290.Persing, D. H., B. L. Herwaldt, C. Glaser, R. S. Lane, J. W. Thomford, D. Mathiesen, P. J. Krause, D. F. Phillip, and P. A. Conrad. 1995. Infection with a Babesia-like organism in northern California. N. Engl. J. Med. 332:298-303. [DOI] [PubMed] [Google Scholar]
- 291.Persing, D. H., D. Mathiesen, W. F. Marshall, S. R. Telford, A. Spielman, J. W. Thomford, and P. A. Conrad. 1992. Detection of Babesia microti by polymerase chain reaction. J. Clin. Microbiol. 30:2097-2103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Petersen, L. R., and A. A. Marfin. 2002. West Nile virus: a primer for the clinician. Ann. Intern. Med. 137:173-179. [DOI] [PubMed] [Google Scholar]
- 293.Petersen, L. R., A. A. Marfin, and D. J. Gubler. 2003. West Nile virus. JAMA 290:524-528. [DOI] [PubMed] [Google Scholar]
- 294.Petersen, L. R., J. T. Roehrig, and J. M. Hughes. 2002. West Nile virus encephalitis. N. Engl. J. Med. 347:1225-1226. [DOI] [PubMed] [Google Scholar]
- 295.Pintado, V., P. Martin-Rabadan, M. L. Rivera, S. Moreno, and E. Bouza. 2001. Visceral leishmaniasis in human immunodeficiency virus (HIV)-infected and non-HIV-infected patients. A comparative study. Medicine (Baltimore) 80:54-73. [DOI] [PubMed] [Google Scholar]
- 296.Ponce, C., E. Ponce, E. Vinelli, A. Montoya, V. de Aguilar, A. Gonzalez, B. Zingales, R. Rangel-Aldao, M. J. Levin, J. Esfandiari, E. S. Umezawa, A. O. Luquetti, and J. F. da Silveira. 2005. Validation of a rapid and reliable test for diagnosis of Chagas’ disease by detection of Trypanosoma cruzi-specific antibodies in blood of donors and patients in Central America. J. Clin. Microbiol. 43:5065-5068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Price, J., B. A. Cant, J. A. Barbara, and R. S. Tedder. 2001. Human T-cell leukaemia/lymphoma virus risk may be enhanced in some selected donor populations. Vox Sang. 80:148-150. [DOI] [PubMed] [Google Scholar]
- 298.Proietti, F. A., and A. B. Carneiro-Proietti. 2006. HTLV in the Americas. Rev. Panam. Salud Publica 19:7-8. [DOI] [PubMed] [Google Scholar]
- 299.Proietti, F. A., A. B. Carneiro-Proietti, B. C. Catalan-Soares, and E. L. Murphy. 2005. Global epidemiology of HTLV-I infection and associated diseases. Oncogene 24:6058-6068. [DOI] [PubMed] [Google Scholar]
- 300.Pungpapong, S., S. Alvarez, W. C. Hellinger, D. J. Kramer, D. L. Willingham, J. C. Mendez, J. H. Nguyen, W. R. Hewitt, J. Randa-Michel, D. M. Harnois, B. G. Rosser, C. B. Hughes, H. P. Grewal, R. Satyanarayana, R. C. Dickson, J. L. Steers, and A. P. Keaveny. 2006. Peritonitis after liver transplantation: incidence, risk factors, microbiology profiles, and outcome. Liver Transpl. 12:1244-1252. [DOI] [PubMed] [Google Scholar]
- 301.Pushker, N., M. S. Bajaj, and S. M. Betharia. 2002. Orbital and adnexal cysticercosis. Clin. Exp. Ophthalmol. 30:322-333. [DOI] [PubMed] [Google Scholar]
- 302.Qvarnstrom, Y., G. S. Visvesvara, R. Sriram, and A. J. da Silva. 2006. Multiplex real-time PCR assay for simultaneous detection of Acanthamoeba spp., Balamuthia mandrillaris, and Naegleria fowleri. J. Clin. Microbiol. 44:3589-3595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Rajaram, K. G., K. Sud, H. S. Kohli, K. L. Gupta, and V. Sakhuja. 2002. Visceral leishmaniasis: a rare cause of transplant fever and pancytopenia. J. Assoc. Physicians India 50:979-980. [PubMed] [Google Scholar]
- 304.Ratner, L. 2005. Human T cell lymphotropic virus-associated leukemia/lymphoma. Curr. Opin. Oncol. 17:469-473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 305.Ravindra, K. V., A. G. Freifeld, A. C. Kalil, D. F. Mercer, W. J. Grant, J. F. Botha, L. E. Wrenshall, and R. B. Stevens. 2004. West Nile virus-associated encephalitis in recipients of renal and pancreas transplants: case series and literature review. Clin. Infect. Dis. 38:1257-1260. [DOI] [PubMed] [Google Scholar]
- 306.Reesink, H. W. 2005. European strategies against the parasite transfusion risk. Transfus. Clin. Biol. 12:1-4. [DOI] [PubMed] [Google Scholar]
- 307.Remesar, M. C., A. E. del Pozo, M. G. Pittis, A. M. Mangano, L. Sen, and L. Briones. 2000. Transmission of HTLV-I by kidney transplant. Transfusion 40:1421-1422. [DOI] [PubMed] [Google Scholar]
- 308.Restrepo, A., and A. Tobon. 2005. Paracoccidioides brasiliensis, p. 3062-3068. In G. L. Mandell, J. E. Bennett, and R. Dolin (ed.), Principles and practice of infectious diseases. Elsevier Churchill-Livingstone, Philadelphia, PA.
- 309.Restrepo, A., A. Tobon, B. Clark, D. R. Graham, G. Corcoran, R. W. Bradsher, M. Goldman, G. Pankey, T. Moore, R. Negroni, and J. R. Graybill. 2007. Salvage treatment of histoplasmosis with posaconazole. J. Infect. 54:319-327. [DOI] [PubMed] [Google Scholar]
- 310.Riarte, A., C. Luna, R. Sabatiello, A. Sinagra, R. Schiavelli, A. De Rissio, E. Maiolo, M. M. Garcia, N. Jacob, M. Pattin, M. Lauricella, E. L. Segura, and M. Vazquez. 1999. Chagas’ disease in patients with kidney transplants: 7 years of experience 1989-1996. Clin. Infect. Dis. 29:561-567. [DOI] [PubMed] [Google Scholar]
- 311.Rigano, R., S. Ioppolo, E. Ortona, P. Margutti, E. Profumo, M. D. Ali, B. Di Vico, A. Teggi, and A. Siracusano. 2002. Long-term serological evaluation of patients with cystic echinococcosis treated with benzimidazole carbamates. Clin. Exp. Immunol. 129:485-492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 312.Rimek, D., T. Zimmermann, M. Hartmann, C. Prariyachatigul, and R. Kappe. 1999. Disseminated Penicillium marneffei infection in an HIV-positive female from Thailand in Germany. Mycoses 42(Suppl. 2):25-28. [PubMed] [Google Scholar]
- 313.Robertson, I. 1979. Corneal transplants and rabies. Med. J. Aust. 2:697. [PubMed] [Google Scholar]
- 314.Roehrig, J. T., D. Nash, B. Maldin, A. Labowitz, D. A. Martin, R. S. Lanciotti, and G. L. Campbell. 2003. Persistence of virus-reactive serum immunoglobulin M antibody in confirmed West Nile virus encephalitis cases. Emerg. Infect. Dis. 9:376-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 315.Rosenblatt, J. D., J. C. Gasson, J. Glaspy, S. Bhuta, M. Aboud, I. S. Chen, and D. W. Golde. 1987. Relationship between human T cell leukemia virus-II and atypical hairy cell leukemia: a serologic study of hairy cell leukemia patients. Leukemia 1:397-401. [PubMed] [Google Scholar]
- 316.Rosenblatt, J. D., D. W. Golde, W. Wachsman, J. V. Giorgi, A. Jacobs, G. M. Schmidt, S. Quan, J. C. Gasson, and I. S. Chen. 1986. A second isolate of HTLV-II associated with atypical hairy-cell leukemia. N. Engl. J. Med. 315:372-377. [DOI] [PubMed] [Google Scholar]
- 317.Rosenblatt, J. D., S. Plaeger-Marshall, J. V. Giorgi, P. Swanson, I. S. Chen, E. Chin, H. J. Wang, M. Canavaggio, M. A. Hausner, and A. C. Black. 1990. A clinical, hematologic, and immunologic analysis of 21 HTLV-II-infected intravenous drug users. Blood 76:409-417. [PubMed] [Google Scholar]
- 318.Ross, A. G., P. B. Bartley, A. C. Sleigh, G. R. Olds, Y. Li, G. M. Williams, and D. P. McManus. 2002. Schistosomiasis. N. Engl. J. Med. 346:1212-1220. [DOI] [PubMed] [Google Scholar]
- 319.Sabbatini, M., A. Pisani, A. Ragosta, R. Gallo, F. Borrelli, and B. Cianciaruso. 2002. Visceral leishmaniasis in renal transplant recipients: is it still a challenge to the nephrologist? Transplantation 73:299-301. [DOI] [PubMed] [Google Scholar]
- 320.Sabrosa, N. A., and M. Zajdenweber. 2002. Nematode infections of the eye: toxocariasis, onchocerciasis, diffuse unilateral subacute neuroretinitis, and cysticercosis. Ophthalmol. Clin. N. Am. 15:351-356. [DOI] [PubMed] [Google Scholar]
- 321.Saccente, M., R. S. Abernathy, P. G. Pappas, H. R. Shah, and R. W. Bradsher. 1998. Vertebral blastomycosis with paravertebral abscess: report of eight cases and review of the literature. Clin. Infect. Dis. 26:413-418. [DOI] [PubMed] [Google Scholar]
- 322.Salva, M., J. Fernandez Fernandez, F. Berisa, R. Enriquez, M. C. Sanz, G. D. Sanz, J. L. Gallego, J. Hernandez, and J. Botella. 1986. Visceral leishmaniasis in kidney transplantation: report of one case. Clin. Transpl. 1986:134. [PubMed] [Google Scholar]
- 323.Sampathkumar, P. 2003. West Nile virus: epidemiology, clinical presentation, diagnosis, and prevention. Mayo Clin. Proc. 78:1137-1143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Sarkodie, F., M. Adarkwa, Y. du-Sarkodie, D. Candotti, J. W. Acheampong, and J. P. Allain. 2001. Screening for viral markers in volunteer and replacement blood donors in West Africa. Vox Sang. 80:142-147. [DOI] [PubMed] [Google Scholar]
- 325.Schaeffer, M. W., J. F. Buell, M. Gupta, G. D. Conway, S. A. Akhter, and L. E. Wagoner. 2004. Strongyloides hyperinfection syndrome after heart transplantation: case report and review of the literature. J. Heart Lung Transplant. 23:905-911. [DOI] [PubMed] [Google Scholar]
- 326.Schenone, H. 1999. Xenodiagnosis. Mem. Inst. Oswaldo Cruz 94(Suppl. 1):289-294. [DOI] [PubMed] [Google Scholar]
- 327.Schijman, A. G., C. Vigliano, J. Burgos, R. Favaloro, S. Perrone, R. Laguens, and M. J. Levin. 2000. Early diagnosis of recurrence of Trypanosoma cruzi infection by polymerase chain reaction after heart transplantation of a chronic Chagas’ heart disease patient. J. Heart Lung Transplant. 19:1114-1117. [DOI] [PubMed] [Google Scholar]
- 328.Schmunis, G. A., and J. R. Cruz. 2005. Safety of the blood supply in Latin America. Clin. Microbiol. Rev. 18:12-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 329.Schmunis, G. A., F. Zicker, F. Pinheiro, and D. Brandlind-Bennett. 1998. Risk for transfusion-transmitted infectious diseases in Central and South America. Emerg. Infect. Dis. 4:5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 330.Schmunis, G. A., F. Zicker, E. L. Segura, and A. E. del Pozo. 2000. Transfusion-transmitted infectious diseases in Argentina, 1995 through 1997. Transfusion 40:1048-1053. [DOI] [PubMed] [Google Scholar]
- 331.Schulz, A., K. Mellenthin, G. Schonian, B. Fleischer, and C. Drosten. 2003. Detection, differentiation, and quantitation of pathogenic leishmania organisms by a fluorescence resonance energy transfer-based real-time PCR assay. J. Clin. Microbiol. 41:1529-1535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Schuster, F. L., and G. S. Visvesvara. 2004. Free-living amoebae as opportunistic and non-opportunistic pathogens of humans and animals. Int. J. Parasitol. 34:1001-1027. [DOI] [PubMed] [Google Scholar]
- 333.Sejvar, J. J., M. B. Haddad, B. C. Tierney, G. L. Campbell, A. A. Marfin, J. A. Van Gerpen, A. Fleischauer, A. A. Leis, D. S. Stokic, and L. R. Petersen. 2003. Neurologic manifestations and outcome of West Nile virus infection. JAMA 290:511-515. [DOI] [PubMed] [Google Scholar]
- 334.Sejvar, J. J., A. A. Leis, D. S. Stokic, J. A. Van Gerpen, A. A. Marfin, R. Webb, M. B. Haddad, B. C. Tierney, S. A. Slavinski, J. L. Polk, V. Dostrow, M. Winkelmann, and L. R. Petersen. 2003. Acute flaccid paralysis and West Nile virus infection. Emerg. Infect. Dis. 9:788-793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Serody, J. S., M. R. Mill, F. C. Detterbeck, D. T. Harris, and M. S. Cohen. 1993. Blastomycosis in transplant recipients: report of a case and review. Clin. Infect. Dis. 16:54-58. [DOI] [PubMed] [Google Scholar]
- 335a.Shames, B. D., A. M. D'Alessandro, and H. W. Sollinger. 2002. Human T-cell lymphotrophic virus infection in organ donors: a need to reassess policy? Am. J. Transplant. 2:658-663. [DOI] [PubMed] [Google Scholar]
- 336.Sharma, R. K., R. Jha, P. Kumar, V. Kher, A. Gupta, A. Kumar, S. Gulati, P. Arora, M. Murari, and M. Bhandari. 1996. Visceral leishmaniasis in a renal transplant recipient: diagnostic and therapeutic problems. Am. J. Nephrol. 16:358-360. [DOI] [PubMed] [Google Scholar]
- 337.Shepherd, J. C., A. Subramanian, R. A. Montgomery, M. D. Samaniego, G. Gong, A. Bergmann, D. Blythe, and L. Dropulic. 2004. West Nile virus encephalitis in a kidney transplant recipient. Am. J. Transplant. 4:830-833. [DOI] [PubMed] [Google Scholar]
- 338.Shi, P. Y., and S. J. Wong. 2003. Serologic diagnosis of West Nile virus infection. Expert Rev. Mol. Diagn. 3:733-741. [DOI] [PubMed] [Google Scholar]
- 339.Shikanai-Yasuda, M. A., M. I. Duarte, D. F. Nunes, C. S. Lacaz, E. Sabagga, E. Abdala, A. J. Duarte, and M. H. Lopes. 1995. Paracoccidioidomycosis in a renal transplant recipient. J. Med. Vet. Mycol. 33:411-414. [DOI] [PubMed] [Google Scholar]
- 340.Shulman, I. A., and M. D. Appleman. 1991. Transmission of parasitic and bacterial infections through blood transfusion within the U.S. Crit. Rev. Clin. Lab. Sci. 28:447-459. [DOI] [PubMed] [Google Scholar]
- 341.Silveira-Lacerda, E. P., A. G. Silva, S. F. Junior, M. A. Souza, N. Kesper, A. Botelho-Filho, and E. S. Umezawa. 2004. Chagas’ disease: application of TESA-blot in inconclusive sera from a Brazilian blood bank. Vox Sang. 87:204-207. [DOI] [PubMed] [Google Scholar]
- 342.Sipsas, N. V., and J. Boletis. 2003. Fever, hepatosplenomegaly, and pancytopenia in a renal transplant recipient. Transpl. Infect. Dis. 5:47-52. [DOI] [PubMed] [Google Scholar]
- 343.Sirvent-von Bueltzingsloewen, A., P. Marty, E. Rosenthal, P. Delaunay, A. Allieri-Rosenthal, N. Gratecos, and J. P. Cassuto. 2004. Visceral leishmaniasis: a new opportunistic infection in hematopoietic stem-cell-transplanted patients. Bone Marrow Transplant. 33:667-668. [DOI] [PubMed] [Google Scholar]
- 344.Slovut, D. P., E. Benedetti, and A. J. Matas. 1996. Babesiosis and hemophagocytic syndrome in an asplenic renal transplant recipient. Transplantation 62:537-539. [DOI] [PubMed] [Google Scholar]
- 345.Sousa, A. A., M. C. Lobo, R. A. Barbosa, and V. Bello. 2004. Chagas seropositive donors in kidney transplantation. Transplant. Proc. 36:868-869. [DOI] [PubMed] [Google Scholar]
- 346.Srinivasan, A., E. C. Burton, M. J. Kuehnert, C. Rupprecht, W. L. Sutker, T. G. Ksiazek, C. D. Paddock, J. Guarner, W. J. Shieh, C. Goldsmith, C. A. Hanlon, J. Zoretic, B. Fischbach, M. Niezgoda, W. H. El-Feky, L. Orciari, E. Q. Sanchez, A. Likos, G. B. Klintmalm, D. Cardo, J. LeDuc, M. E. Chamberland, D. B. Jernigan, and S. R. Zaki. 2005. Transmission of rabies virus from an organ donor to four transplant recipients. N. Engl. J. Med. 352:1103-1111. [DOI] [PubMed] [Google Scholar]
- 347.Steinberg, J. P., R. L. Galindo, E. S. Kraus, and K. G. Ghanem. 2002. Disseminated acanthamebiasis in a renal transplant recipient with osteomyelitis and cutaneous lesions: case report and literature review. Clin. Infect. Dis. 35:e43-e49. [DOI] [PubMed] [Google Scholar]
- 348.Stephenson, J. 2002. Investigation probes risk of contracting West Nile virus via blood transfusions. JAMA 288:1573-1574. [DOI] [PubMed] [Google Scholar]
- 349.Stevens, D. A. 1995. Coccidioidomycosis. N. Engl. J. Med. 332:1077-1082. [DOI] [PubMed] [Google Scholar]
- 350.Stigum, H., P. Magnus, H. H. Samdal, and E. Nord. 2000. Human T-cell lymphotropic virus testing of blood donors in Norway: a cost-effect model. Int. J. Epidemiol. 29:1076-1084. [DOI] [PubMed] [Google Scholar]
- 351.Stone, W. J., and W. Schaffner. 1990. Strongyloides infections in transplant recipients. Semin. Respir. Infect. 5:58-64. [PubMed] [Google Scholar]
- 352.Sturrock, R. F. 2001. Schistosomiasis epidemiology and control: how did we get here and where should we go? Mem. Inst. Oswaldo Cruz 96(Suppl.):17-27. [DOI] [PubMed] [Google Scholar]
- 353.Sugar, A. M., A. Restrepo, and D. A. Stevens. 1984. Paracoccidioidomycosis in the immunosuppressed host: report of a case and review of the literature. Am. Rev. Respir. Dis. 129:340-342. [PubMed] [Google Scholar]
- 354.Superdock, K. R., J. S. Dummer, M. O. Koch, D. M. Gilliam, D. H. Van Buren, W. A. Nylander, R. E. Richie, R. C. MacDonell, Jr., H. K. Johnson, and J. H. Helderman. 1994. Disseminated histoplasmosis presenting as urinary tract obstruction in a renal transplant recipient. Am. J. Kidney Dis. 23:600-604. [DOI] [PubMed] [Google Scholar]
- 355.Supparatpinyo, K., C. Khamwan, V. Baosoung, K. E. Nelson, and T. Sirisanthana. 1994. Disseminated Penicillium marneffei infection in southeast Asia. Lancet 344:110-113. [DOI] [PubMed] [Google Scholar]
- 356.Talabiska, D. G., M. J. Komar, D. H. Wytock, and R. A. Rubin. 1996. Post-transfusion acquired malaria complicating orthotopic liver transplantation. Am. J. Gastroenterol. 91:376-379. [PubMed] [Google Scholar]
- 357.Tanabe, K., R. Kitani, K. Takahashi, T. Tokumoto, N. Ishikawa, T. Oshima, A. Kanematsu, S. Fuchinoue, T. Yagisawa, K. Ota, and H. Toma. 1998. Long-term results in human T-cell leukemia virus type 1-positive renal transplant recipients. Transplant. Proc. 30:3168-3170. [DOI] [PubMed] [Google Scholar]
- 358.Tang, Y. W., H. Li, M. M. Durkin, S. E. Sefers, S. Meng, P. A. Connolly, C. W. Stratton, and L. J. Wheat. 2006. Urine polymerase chain reaction is not as sensitive as urine antigen for the diagnosis of disseminated histoplasmosis. Diagn. Microbiol. Infect. Dis. 54:283-287. [DOI] [PubMed] [Google Scholar]
- 359.Tavora, E. R., E. P. Lasmar, J. Orefice, C. M. Gontijo, and J. S. Andrade Filho. 2002. Unusual manifestations of leishmaniasis in renal transplant. Transplant. Proc. 34:502-503. [DOI] [PubMed] [Google Scholar]
- 360.Terraza, S., T. Pujol, J. Gascon, and M. Corachan. 2001. Neurocysticercosis: an imported disease? Med. Clin. (Barcelona) 116:261-263. (In Spanish.) [DOI] [PubMed] [Google Scholar]
- 361.Thambo, S., W. Passalacqua, C. R. Van, and F. Lazcano. 1989. Chagas’ disease in patients with renal transplantation. Rev. Med. Chil. 117:18-22. (In Spanish.) [PubMed] [Google Scholar]
- 362.Tobler, L. H., P. Contestable, L. Pitina, H. Groth, S. Shaffer, G. R. Blackburn, H. Warren, S. R. Lee, and M. P. Busch. 2007. Evaluation of a new enzyme-linked immunosorbent assay for detection of Chagas antibody in US blood donors. Transfusion 47:90-96. [DOI] [PubMed] [Google Scholar]
- 363.Tomimori-Yamashita, J., P. D. Deps, D. R. Almeida, M. M. Enokihara, M. T. De Seixas, and E. Freymuller. 1997. Cutaneous manifestation of Chagas’ disease after heart transplantation: successful treatment with allopurinol. Br. J. Dermatol. 137:626-630. [DOI] [PubMed] [Google Scholar]
- 364.Toro, C., R. Benito, A. Aguilera, S. Bassani, C. Rodriguez, E. Calderon, E. Caballero, P. Alvarez, J. Garcia, M. Rodriguez-Iglesias, A. Guelar, J. del Romero, and V. Soriano. 2005. Infection with human T lymphotropic virus type I in organ transplant donors and recipients in Spain. J. Med. Virol. 76:268-270. [DOI] [PubMed] [Google Scholar]
- 365.Toro, C., B. Rodes, A. Aguilera, E. Caballero, R. Benito, C. Tuset, J. Garcia, R. O. De Lejarazu, J. M. Eiros, E. Calderon, C. Rodriguez, and V. Soriano. 2002. Clinical impact of HTLV-1 infection in Spain: implications for public health and mandatory screening. J. Acquir. Immune Defic. Syndr. 30:366-368. [DOI] [PubMed] [Google Scholar]
- 366.Toro, C., B. Rodes, E. Poveda, and V. Soriano. 2003. Rapid development of subacute myelopathy in three organ transplant recipients after transmission of human T-cell lymphotropic virus type I from a single donor. Transplantation 75:102-104. [DOI] [PubMed] [Google Scholar]
- 367.Torregrosa, J. V., M. J. Ricart, M. Montesinos, J. M. Campistol, A. Moreno, X. Claramonte, J. Andreu, and P. Carretero. 1993. Visceral leishmaniasis-like cause of unexplained fever in a reno-pancreatic graft recipient. Nephron 65:318-319. [DOI] [PubMed] [Google Scholar]
- 368.Tripathy, U., G. L. Yung, J. M. Kriett, P. A. Thistlethwaite, D. P. Kapelanski, and S. W. Jamieson. 2002. Donor transfer of pulmonary coccidioidomycosis in lung transplantation. Ann. Thorac. Surg. 73:306-308. [DOI] [PubMed] [Google Scholar]
- 369.Tsai, T. F., F. Popovici, C. Cernescu, G. L. Campbell, and N. I. Nedelcu. 1998. West Nile encephalitis epidemic in southeastern Romania. Lancet 352:767-771. [DOI] [PubMed] [Google Scholar]
- 370.Tseliou, P. M., N. Spanakis, A. Spiliotakara, C. Politis, N. J. Legakis, and A. Tsakris. 2003. HTLV-I and -II in southwestern Greece. Transfusion 43:1641-1642. [DOI] [PubMed] [Google Scholar]
- 371.Tsurumi, H., K. Tani, T. Tsuruta, R. Shirato, T. Matsudaira, A. Tojo, C. Wada, H. Uchida, K. Ozawa, and S. Asano. 1992. Adult T-cell leukemia developing during immunosuppressive treatment in a renal transplant recipient. Am. J. Hematol. 41:292-294. [DOI] [PubMed] [Google Scholar]
- 372.Turkmen, A., M. S. Sever, T. Ecder, A. Yildiz, A. E. Aydin, R. Erkoc, H. Eraksoy, U. Eldegez, and E. Ark. 1996. Posttransplant malaria. Transplantation 62:1521-1523. [DOI] [PubMed] [Google Scholar]
- 373.Umezawa, E. S., M. S. Nascimento, and A. M. Stolf. 2001. Enzyme-linked immunosorbent assay with Trypanosoma cruzi excreted-secreted antigens (TESA-ELISA) for serodiagnosis of acute and chronic Chagas’ disease. Diagn. Microbiol. Infect. Dis. 39:169-176. [DOI] [PubMed] [Google Scholar]
- 374.United Nations World Toursim Organization. 2006. Tourism highlights, edition 2006. United Nations World Tourism Organization, Madrid, Spain. http://www.unwto.org/facts/eng/highlights.htm.
- 375.U.S. Census Bureau. 26 April 2007, accession date. Latin America population. U.S. Census Bureau 2000. U.S. Census Bureau, Washington, DC. http://www.census.gov/population/cen2000/stp159.latin_america.pdf.
- 376.U.S. Department of Health and Human Services and Food and Drug Administration Center for Biologics Evaluation and Research. 29 April 2007, accession date. Guidance for industry: assessing donor suitability and blood and blood product safety in cases of known or suspected West Nile virus infection. U.S. Department of Health and Human Services, Washington, DC. http://www.fda.gov/cber/gdlns/wnvguid.htm.
- 377.Vail, G. M., R. S. Young, L. J. Wheat, R. S. Filo, K. Cornetta, and M. Goldman. 2002. Incidence of histoplasmosis following allogeneic bone marrow transplant or solid organ transplant in a hyperendemic area. Transpl. Infect. Dis. 4:148-151. [DOI] [PubMed] [Google Scholar]
- 378.Valeyrie, L., F. Botterel, C. Minozzi, P. Roger, P. Bourree, and D. Vittecoq. 1999. Prolonged fever revealing disseminated infection due to Penicillium marneffei in a French HIV-seropositive patient. AIDS 13:731-732. [DOI] [PubMed] [Google Scholar]
- 379.van der Woude, F. J., P. A. Kager, J. Weits, E. J. van der Jagt, W. J. Van Son, M. J. Sloof, and A. M. Tegzess. 1985. Strongyloides stercoralis hyperinfection as a consequence of immunosuppressive treatment. Neth. J. Med. 28:315-317. [PubMed] [Google Scholar]
- 380.Vazquez, M. C., A. Riarte, M. Pattin, and M. Lauricella. 1993. Chagas’ disease can be transmitted through kidney transplantation. Transplant. Proc. 25:3259-3260. [PubMed] [Google Scholar]
- 381.Venizelos, P. C., M. Lopata, W. A. Bardawil, and J. T. Sharp. 1980. Respiratory failure due to Strongyloides stercoralis in a patient with a renal transplant. Chest 78:104-106. [DOI] [PubMed] [Google Scholar]
- 382.Villalba, R., G. Fornes, M. A. Alvarez, J. Roman, V. Rubio, M. Fernandez, J. M. Garcia, M. Vinals, and A. Torres. 1992. Acute Chagas’ disease in a recipient of a bone marrow transplant in Spain: case report. Clin. Infect. Dis. 14:594-595. [DOI] [PubMed] [Google Scholar]
- 383.Wadei, H., G. J. Alangaden, D. H. Sillix, J. M. El Amm, S. A. Gruber, M. S. West, D. K. Granger, J. Garnick, P. Chandrasekar, S. D. Migdal, and A. Haririan. 2004. West Nile virus encephalitis: an emerging disease in renal transplant recipients. Clin. Transplant. 18:753-758. [DOI] [PubMed] [Google Scholar]
- 384.Reference deleted.
- 385.Walker, M., J. G. Kublin, and J. R. Zunt. 2006. Parasitic central nervous system infections in immunocompromised hosts: malaria, microsporidiosis, leishmaniasis, and African trypanosomiasis. Clin. Infect. Dis. 42:115-125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Wang, J. L., C. C. Hung, S. C. Chang, S. C. Chueh, and M. K. La. 2003. Disseminated Penicillium marneffei infection in a renal-transplant recipient successfully treated with liposomal amphotericin B. Transplantation 76:1136-1137. [DOI] [PubMed] [Google Scholar]
- 387.Weinberger, M., S. D. Pitlik, D. Gandacu, R. Lang, F. Nassar, D. D. Ben, E. Rubinstein, A. Izthaki, J. Mishal, R. Kitzes, Y. Siegman-Igra, M. Giladi, N. Pick, E. Mendelson, H. Bin, and T. Shohat. 2001. West Nile fever outbreak, Israel, 2000: epidemiologic aspects. Emerg. Infect. Dis. 7:686-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Weingartl, H. M., M. A. Drebot, Z. Hubalek, J. Halouzka, M. Andonova, A. Dibernardo, C. Cottam-Birt, J. Larence, and P. Marszal. 2003. Comparison of assays for the detection of West Nile virus antibodies in chicken serum. Can. J. Vet. Res. 67:128-132. [PMC free article] [PubMed] [Google Scholar]
- 389.Wheat, L. J. 2001. Laboratory diagnosis of histoplasmosis: update 2000. Semin. Respir. Infect. 16:131-140. [DOI] [PubMed] [Google Scholar]
- 390.Wheat, L. J. 1992. Histoplasmosis in Indianapolis. Clin. Infect. Dis. 14(Suppl. 1):S91-S99. [DOI] [PubMed] [Google Scholar]
- 391.Wheat, L. J., P. Connolly, M. Durkin, B. K. Book, A. J. Tector, J. Fridell, and M. D. Pescovitz. 2004. False-positive Histoplasma antigenemia caused by antithymocyte globulin antibodies. Transpl. Infect. Dis. 6:23-27. [DOI] [PubMed] [Google Scholar]
- 392.Wheat, L. J., P. Connolly-Stringfield, B. Williams, K. Connolly, R. Blair, M. Bartlett, and M. Durkin. 1992. Diagnosis of histoplasmosis in patients with the acquired immunodeficiency syndrome by detection of Histoplasma capsulatum polysaccharide antigen in bronchoalveolar lavage fluid. Am. Rev. Respir. Dis. 145:1421-1424. [DOI] [PubMed] [Google Scholar]
- 393.Wheat, L. J., P. A. Connolly-Stringfield, R. L. Baker, M. F. Curfman, M. E. Eads, K. S. Israel, S. A. Norris, D. H. Webb, and M. L. Zeckel. 1990. Disseminated histoplasmosis in the acquired immune deficiency syndrome: clinical findings, diagnosis and treatment, and review of the literature. Medicine (Baltimore) 69:361-374. [DOI] [PubMed] [Google Scholar]
- 394.Wheat, L. J., T. Garringer, E. Brizendine, and P. Connolly. 2002. Diagnosis of histoplasmosis by antigen detection based upon experience at the histoplasmosis reference laboratory. Diagn. Microbiol. Infect. Dis. 43:29-37. [DOI] [PubMed] [Google Scholar]
- 395.Wheat, L. J., C. E. Musial, and E. Jenny-Avital. 2005. Diagnosis and management of central nervous system histoplasmosis. Clin. Infect. Dis. 40:844-852. [DOI] [PubMed] [Google Scholar]
- 396.Wheat, L. J., E. J. Smith, B. Sathapatayavongs, B. Batteiger, R. S. Filo, S. B. Leapman, and M. V. French. 1983. Histoplasmosis in renal allograft recipients. Two large urban outbreaks. Arch. Intern. Med. 143:703-707. [PubMed] [Google Scholar]
- 397.White, A. C., Jr. 1997. Neurocysticercosis: a major cause of neurological disease worldwide. Clin. Infect. Dis. 24:101-113. [DOI] [PubMed] [Google Scholar]
- 398.White, J. V., G. Garvey, and M. A. Hardy. 1982. Fatal strongyloidiasis after renal transplantation: a complication of immunosuppression. Am. Surg. 48:39-41. [PubMed] [Google Scholar]
- 399.Williams, A. E., C. T. Fang, D. J. Slamon, B. J. Poiesz, S. G. Sandler, W. F. Darr, G. Shulman, E. I. McGowan, D. K. Douglas, R. J. Bowman, and. 1988. Seroprevalence and epidemiological correlates of HTLV-I infection in U.S. blood donors. Science 240:643-646. [DOI] [PubMed] [Google Scholar]
- 400.Wong, S. S., K. H. Wong, W. T. Hui, S. S. Lee, J. Y. Lo, L. Cao, and K. Y. Yuen. 2001. Differences in clinical and laboratory diagnostic characteristics of penicilliosis marneffei in human immunodeficiency virus (HIV)- and non-HIV-infected patients. J. Clin. Microbiol. 39:4535-4540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.Wong, S. Y., and D. M. Allen. 1992. Transmission of disseminated histoplasmosis via cadaveric renal transplantation: case report. Clin. Infect. Dis. 14:232-234. [DOI] [PubMed] [Google Scholar]
- 402.World Health Organization. 16 August 2007, accession date. Leishmaniasis. Magnitude of the problem. World Health Organization, Geneva, Switzerland. http:/www.who.int/leishmaniasis/burden/magnitude/burden_magnitude/en/index.html.
- 403.World Health Organization. 27 July 2007, accession date. Report from WHO Expert Consultation on Rabies, Geneva, Switzerland, 5-8 October, 2004. World Health Organization, Geneva, Switzerland. http://www.who.int/mediacentre/factsheets/fs099/en/index.html.
- 404.World Health Organization. 2006. Rabies. Fact sheet no. 99. World Health Organization, Geneva, Switzerland. http://www.who.int/mediacentre/factsheets/fs099/en/print.html.
- 405.Wright, P. W., D. Pappagianis, M. Wilson, A. Louro, S. A. Moser, K. Komatsu, and P. G. Pappas. 2003. Donor-related coccidioidomycosis in organ transplant recipients. Clin. Infect. Dis. 37:1265-1269. [DOI] [PubMed] [Google Scholar]
- 406.Yamaguchi, K. 2001. Declining trends in HTLV-I prevalence among blood donors in Japan. Intern. Med. 40:1-2. [DOI] [PubMed] [Google Scholar]
- 407.Yamaguchi, K. 1994. Human T-lymphotropic virus type I in Japan. Lancet 343:213-216. [DOI] [PubMed] [Google Scholar]
- 408.Yamaguchi, K., and K. Takatsuki. 1993. Adult T cell leukaemia-lymphoma. Baillieres Clin. Haematol. 6:899-915. [DOI] [PubMed] [Google Scholar]
- 409.Yamaguchi, K., and T. Watanabe. 2002. Human T lymphotropic virus type-I and adult T-cell leukemia in Japan. Int. J. Hematol. 76(Suppl. 2):240-245. [DOI] [PubMed] [Google Scholar]
- 410.Yenen, O. S., K. Keskin, S. Cavuslu, N. Kocak, and M. Y. Tuybek. 1994. A case of Plasmodium vivax infection transmitted by renal allograft. Nephrol. Dial. Transplant. 9:1805-1806. [PubMed] [Google Scholar]
- 411.Yeung, C. K., J. K. Ho, W. Y. Lau, K. H. Lee, and A. K. Li. 1996. The use of liver grafts infested with Clonorchis sinensis for orthotopic liver transplantation. Postgrad. Med. J. 72:427-428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Yuen, K. Y., S. S. Wong, D. N. Tsang, and P. Y. Chau. 1994. Serodiagnosis of Penicillium marneffei infection. Lancet 344:444-445. [DOI] [PubMed] [Google Scholar]
- 413.Zaaijer, H. 1996. Human T-lymphotropic virus infection: is it a threat? Transplant. Proc. 28:2940. [PubMed] [Google Scholar]
- 414.Zainudin, B. M., F. Kassim, N. M. Annuar, C. S. Lim, A. K. Ghazali, and Z. Murad. 1992. Disseminated histoplasmosis presenting with ileal perforation in a renal transplant recipient. J. Trop. Med. Hyg. 95:276-279. [PubMed] [Google Scholar]
- 415.Zanke, B. W., D. N. Rush, J. R. Jeffery, and L. G. Israels. 1989. HTLV-1 T cell lymphoma in a cyclosporine-treated renal transplant patient. Transplantation 48:695-697. [PubMed] [Google Scholar]
- 416.Zarate-Blades, C. R., N. Blades, M. S. Nascimento, J. F. da Silveira, and E. S. Umezawa. 2007. Diagnostic performance of tests based on Trypanosoma cruzi excreted-secreted antigens in an endemic area for Chagas’ disease in Bolivia. Diagn. Microbiol. Infect. Dis. 57:229-232. [DOI] [PubMed] [Google Scholar]
- 417.Zavascki, A. P., J. C. Bienardt, and L. C. Severo. 2004. Paracoccidioidomycosis in organ transplant recipient: case report. Rev. Inst. Med. Trop. Sao Paulo 46:279-281. [DOI] [PubMed] [Google Scholar]
- 418.Zeller, H. G., and I. Schuffenecker. 2004. West Nile virus: an overview of its spread in Europe and the Mediterranean basin in contrast to its spread in the Americas. Eur. J. Clin. Microbiol. Infect. Dis. 23:147-156. [DOI] [PubMed] [Google Scholar]
- 419.Zijlstra, E. E., N. S. Daifalla, P. A. Kager, E. A. Khalil, A. M. El-Hassan, S. G. Reed, and H. W. Ghalib. 1998. rK39 enzyme-linked immunosorbent assay for diagnosis of Leishmania donovani infection. Clin. Diagn. Lab. Immunol. 5:717-720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Zorio, G. E., J. M. Blanes, L. Martinez de Ortiz de Urbina, B. L. Almenar, and G. J. Peman. 2003. Persistent fever, pancytopenia and spleen enlargement in a heart transplant carrier as presentation of visceral leishmaniasis. Rev. Clin. Esp. 203:164-165. (In Spanish.) [DOI] [PubMed] [Google Scholar]
- 421.Zou, S., R. Y. Dodd, S. L. Stramer, and D. M. Strong. 2004. Probability of viremia with HBV, HCV, HIV, and HTLV among tissue donors in the United States. N. Engl. J. Med. 351:751-759. [DOI] [PubMed] [Google Scholar]
- 422.Zucker-Franklin, D., W. C. Hooper, and B. L. Evatt. 1992. Human lymphotropic retroviruses associated with mycosis fungoides: evidence that human T-cell lymphotropic virus type II (HTLV-II) as well as HTLV-I may play a role in the disease. Blood 80:1537-1545. [PubMed] [Google Scholar]