Abstract
The aim of this study was to develop a highly sensitive human papillomavirus type 31 (HPV31) neutralization assay based on the production of pseudovirions carrying luciferase. Neutralizing antibodies against HPV31 were investigated in a set of HPV31 monoclonal antibodies and in women with evidence of HPV31 infection. Neutralizing antibodies were detected in 78% of subjects with a positive enzyme-linked immunosorbent assay.
Serologic studies have demonstrated that infection with genital human papillomaviruses (HPVs) is followed by a humoral immune response to viral capsid proteins and that anti-virus-like-particle (anti-VLP) antibodies can be an indicator of past as well as current infection (4, 7) and can persist for many years (1, 4, 23). Among subjects who had had an incident of infection with HPV type 16 (HPV16), seroconversion was a very slow process that required sufficient exposure (high viral load or persistence of infection), and fewer than two-thirds of infected women became seropositive (11). Whether this anti-VLP response elicited by natural HPV infection confers protection against reinfection with the same or related types remains a matter of discussion. Studies on neutralizing antibodies against HPVs have been hampered by the lack of a convenient cell culture system for the production of HPV virions and for monitoring HPV infections. Various methods have been developed to overcome this problem, based on neutralization of authentic virions (5, 16), pseudotyped virions (15), VLPs that have encapsidated reporter genes in cellular or cell-free systems (17, 18, 21), or VLPs expressing a reporter gene on their surfaces (2). Due to low production of pseudovirions, most of these assays lack sensitivity and are not reliable for detecting serum-neutralizing antibodies following natural infection, with the exception of the system recently described by Buck et al. (3) for the generation of high levels of pseudovirions and applied to the production of HPV pseudovirions for types 6, 16, 18, 31, 45, 52, and 58 (3, 9, 12, 14).
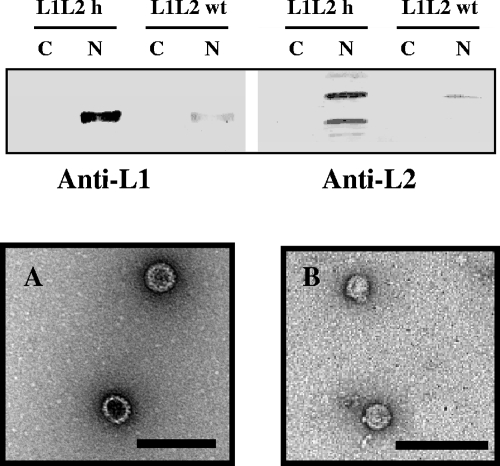
We report here a technique based on the production of pseudovirions obtained by cellular encapsidation of a plasmid coding for luciferase as a reporter for the development of a papillomavirus neutralization assay for HPV31. Validation of this assay was achieved by analyzing the neutralizing activity of HPV31 monoclonal antibodies (MAbs) and sera from women naturally infected with HPV31. Two systems were used for the generation of pseudovirions. One was an acellular system of production, based on the direct interaction between HPV31 L1- and L2-expressing VLPs produced in Sf21 insect cells and DNA coding for luciferase (2). The second method was based on the production of HPV31 pseudovirions in 293FT cells, using codon-modified HPV31 L1 and L2 genes. To increase the expression level of the HPV31 capsid proteins in mammalian cells, Homo sapiens codon-optimized HPV31 L1 (L1h) and HPV31 L2 (L2h) genes (GenBank database entries EU127831 and EU127832, respectively), with deletion of the internal polyadenylation signals and the addition of a Kozak sequence, were synthesized (Geneart, Regensburg, Germany) and cloned into the bicistronic expression vector pIRES, which contains the simian virus 40 ori (BD Biosciences, Clontech, France). Wild-type HPV31 L1 and L2 genes were cloned into the same vector as controls. Both constructs (pIRES31L1L2h and pIRES31L1L2wt; 9.0 kb) were transfected into 293FT cells by using Fugene6 according to the manufacturer's instructions, and nuclear fractions were analyzed by Western blotting, using H31.D24 MAb (8) and an L2 polyclonal antibody for L1 and L2 detection, respectively. The levels of expression of the L1 and L2 proteins were estimated by integration (Molecular Analyst software; Bio-Rad, Marnes-la-Coquette, France) of the Western blotting signals, and the amounts of L1 and L2 proteins produced with the optimized genes were 17 times higher than those produced with the wild-type genes (Fig. 1). HPV31 pseudovirions were produced by cotransfecting 293FT cells with pIRES31L1L2h and the pGL3 luciferase reporter plasmid (a 5.3-kbp plasmid containing the simian virus 40 ori). Cells were transfected with DNA and Fugene6 (Roche) and harvested at 2 days posttransfection for this purpose. Nuclear fractions, obtained as previously described (19), were loaded on a CsCl gradient and ultracentrifuged in a Beckman SW28 rotor (22 h at 27,000 rpm and 4°C). L1-positive gradient fractions were detected by Western blotting at densities of 1.35 to 1.36, corresponding to the density of virions, whereas the L1-positive fractions from 293FT cells transfected with pIRES31L1L2h in the absence of the pGL3 luciferase reporter plasmid were detected only at densities of 1.26 to 1.27, corresponding to VLPs (data not shown). L1-reactive fractions were observed by electron microscopy on a JEOL 1010 electron microscope after being negatively stained (19), and the presence of pseudovirions and VLPs was confirmed (Fig. 1). The total amounts of VLPs present in the two pseudovirion preparations were estimated by enzyme-linked immunosorbent assay (ELISA) and Western blotting using anti-L1 antibody. The results indicated 20 to 25 times higher levels of L1 in the preparation obtained by the direct interaction method than those in the preparation obtained with 293FT cells. This suggests that the proportion of effective pseudovirions among the total VLPs produced using the direct interaction method is low, in accordance with the detection of L1 reactivity in CsCl gradients mainly at densities of 1.26 to 1.28 (corresponding to VLPs) and in contrast to the L1 reactivity detected mainly at densities of 1.35 to 1.36 (corresponding to the density of pseudovirions) with pseudovirions produced in 293FT cells (data not shown).
FIG. 1.
Expression of wild-type (wt) and codon-optimized (h) HPV31 capsid protein level in human 293FT cells transfected with 10 μg wild-type L1L2 (pIRES31L1L2wt) and codon-optimized L1L2 (pIRES31L1L2h) plasmids. L1 proteins were detected using H31.D24 MAb, and L2 proteins were detected by HPV18 L2 polyclonal rabbit serum. HPV31 L1L2h VLPs (A) and HPV31 L1L2h/pGL3 pseudovirions (B) were observed by transmission electron microscopy. Bars, 100 nm. Lanes C, cytoplasmic fraction; lanes N, nuclear fraction.
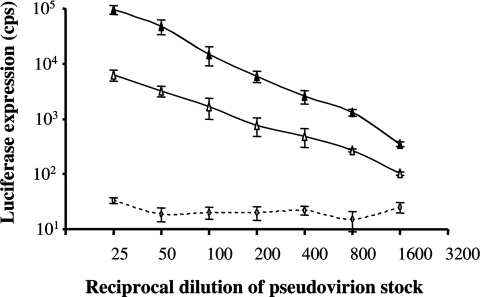
The ability of HPV31 L1L2h/pGL3 pseudovirions to transfer genes was investigated with COS-7 cells and compared to gene transfer with pseudovirions obtained by the direct interaction method. The two pseudovirion preparations were derived from the same number of producing cells. Luciferase expression of about 105 cps was observed at a 1:25 dilution of the crude HPV31 L1L2h pseudovirion stock, and >103 cps was observed at a dilution of 1:800 (Fig. 2). This was eight times higher than the gene transfer level observed with pseudovirions produced by the direct interaction method. To investigate whether the HPV31 L1L2h pseudovirion assay represented a substantial improvement over our previous neutralization assay, we investigated 18 HPV31 MAbs (8) for neutralizing activity and compared the findings using a neutralization assay with pseudovirions obtained by the direct interaction method (Table 1). In these assays, the HPV31 pseudovirions were preincubated with antibodies, and then the inhibition in gene transfer expression was measured in COS-7 cells. The cutoff value used for these assays was inhibition of gene transfer of >80%, a value previously determined using sera (diluted 1/20) from 20 infants and 10 nonimmunized mice that demonstrated <80% inhibition of luciferase expression. The results indicated that the same MAbs were neutralizing in both assays. However, the neutralizing titers were 3 to 27 times higher (mean, 15 times) with the neutralization assay using the L1L2h pseudovirions produced in 293FT cells than with the assay using pseudovirions obtained by the direct interaction method. The greater sensitivity of the test using pseudovirions generated in 293FT cells using optimized L1 and L2 genes may have been related to a greater ratio between pseudovirions and VLPs, since empty VLPs (noninfectious particles) can compete with pseudovirions for binding to neutralizing antibodies. In addition, it should be noted that in comparing the neutralizing titers and the ELISA titers, some MAbs were highly neutralizing, since their ELISA and neutralizing titers were similar (B18, E17, F16, H12, and H17), in contrast with others, such as A19, D7, B1, and F7, that evidenced low neutralizing capacities.
FIG. 2.
Luciferase expression in COS-7 cells after infection with pseudovirions obtained by direct interaction between plasmid and VLPs or with pseudovirions obtained by intracellular encapsidation of the reporter gene in a capsid expressing humanized L1 and L2 genes. ▴, L1L2h pseudovirions; ▵, L1L2 pseudovirions; ⋄, pLuc alone.
TABLE 1.
Neutralizing titers of HPV31 MAbsa
| MAb | ELISA titer (mean ± SD) | Neutralizing titer (mean ± SD)
|
|
|---|---|---|---|
| Method A | Method B | ||
| CamVir-1 | >7,290 | 0 ± 0 | 0 ± 0 |
| H31.B5 | 30 ± 0 | 0 ± 0 | 0 ± 0 |
| H31.E22 | 25 ± 7 | 0 ± 0 | 0 ± 0 |
| H31.D24 | 7,290 ± 0 | 0 ± 0 | 0 ± 0 |
| H31.C19 | 2,430 ± 0 | 0 ± 0 | 0 ± 0 |
| H31.E17 | 25 ± 3 | 10 ± 0 | 30 ± 0 |
| H31.B18 | 75 ± 22 | 30 ± 0 | 90 ± 0 |
| H31.D7 | 810 ± 0 | 3 ± 0 | 30 ± 0 |
| H31.F16 | 810 ± 0 | 90 ± 0 | 675 ± 202 |
| H31.C24 | 2,430 ± 0 | 15 ± 7 | 270 ± 0 |
| H31.E16 | 2,025 ± 608 | 45 ± 22 | 810 ± 0 |
| H31.H9 | 2,430 ± 0 | 90 ± 0 | 810 ± 0 |
| H31.H17 | 2,430 ± 0 | 90 ± 0 | 2,430 ± 0 |
| H31.F7 | 7,290 ± 0 | 10 ± 0 | 30 ± 0 |
| H31.A19 | 7,290 ± 0 | 15 ± 7 | 270 ± 0 |
| H31.B1 | 7,290 ± 0 | 90 ± 0 | 810 ± 0 |
| H31.G5 | 7,290 ± 0 | 135 ± 67 | 2,430 ± 0 |
| H31.D14 | 7,290 ± 0 | 90 ± 0 | 3,645 ± 1822 |
| H31.H12 | 7,290 ± 0 | 810 ± 0 | 7,290 ± 0 |
Titers were obtained by inhibition of luciferase gene transfer, using pseudovirions obtained by direct interaction of wild-type L1 and L2 VLPs with plasmid DNA and by encapsidation of the same plasmid within 293FT cells in which humanized L1 and L2 were expressed. The first 3 MAbs recognize linear epitopes, and the 15 others recognize conformational epitopes (8). Method A, pseudovirions obtained by direct interaction of wild-type L1 and L2 VLPs; method B, pseudovirions obtained by encapsidation with humanized L1 and L2 in 293FT cells. The ELISA end-point titer was determined as the reciprocal of the highest serum dilution giving an absorbance value greater than the average absorbance for sera from 30 infants plus three times the standard deviation (value of 0.200). The neutralizing end-point titer was determined as the reciprocal of the highest serum dilution giving >80% inhibition of luciferase expression. Data are means of four determinations for samples serially diluted threefold from 1/3 to 1/7,290.
Sera from 68 anti-HPV31-negative and 55 anti-HPV31-positive women were also investigated for neutralizing antibodies (Table 2). These subjects were extracted from a larger study including practicing prostitutes and women from the general population recruited in Oviedo and Barcelona, Spain. Serum samples from 38 practicing prostitutes and 85 women from the general population (22 virgins and 63 sexually active women) were selected for this study on the basis of previous results of HPV DNA and anti-HPV31 VLP antibody detection (20). HPV31 DNA was detected in four women, two of whom were anti-HPV31 positive by ELISA. None of the anti-HPV31-negative samples in ELISA were found to be positive for anti-HPV31 by the neutralization assay. Data concerning neutralizing antibodies were log transformed, resulting in a normal distribution of the data, and analyzed as continuous variables by using geometric means. The chi-square test was used to evaluate associations between categorical variables and neutralizing antibody status. Differences in continuous variables were evaluated by the t test, using the log-transformed values for neutralizing antibody titers. All analyses were conducted using STATA (STATA statistical software release 9.0). Of the 55 anti-HPV31-positive samples in ELISA, 43 (78%) revealed evidence of neutralizing activity. The ELISA antibody titers ranged from 25 to 1,600, whereas the neutralizing titers ranged from 25 to 6,400. The mean neutralizing titer was 496.5 for the ELISA-positive samples, 305.2 for sexually active women, and 822.1 for prostitutes (P = 0.18). The geometric mean titer of neutralizing antibodies was 112.2 for sexually active women and 208.3 for prostitutes (P = 0.18). It should be noted that the neutralizing titers were higher than the ELISA titers for 21 subjects, the same for 20 subjects, and lower for 3 subjects. Neutralizing antibodies (titer, 25) were detected in 2 of the 22 virgins investigated. These two women were also anti-HPV31 positive by ELISA. The fact that 2 of 22 women reporting as virgins had HPV31 antibodies detected by ELISA is in agreement with reports that HPV infection can occur following nonpenetrative sexual contact (24). The ELISA and neutralizing titers were low after natural infection (25 to 6,400), and the ELISA and neutralizing titers were slightly higher in prostitutes than in the other women. This could be related to a much higher rate of reinfection for prostitutes, which could boost the immune response. Our results indicate that 22% of anti-HPV31 ELISA-positive sera were not found to be neutralizing. This may indicate the existence of false-positive ELISA results, that ELISA is more sensitive than the neutralization assay in detecting anti-HPV antibodies, or that the neutralizing titers are lower than the ELISA titers (i.e., that some antibodies are not directed at neutralizing epitopes). This is in agreement with findings reported by Buck et al. (3) and Pastrana et al. (13) and could be related to differences in antibody-VLP avidity or the types of antibodies involved in the neutralization and ELISA tests. In addition, it is clear that individual HPV31 MAbs are not equal in neutralizing capacity, since several MAbs showed strong reactivity to HPV31 VLPs but only minimal binding to infectious pseudovirions, a finding recently reported for HPV16 by Culp et al. (6). They suggested that this could be related to the fact that surface epitopes on L1L2 pseudovirions produced in 293FT cells are closer to epitopes of authentic virions than are epitopes present on L1-only VLPs.
TABLE 2.
Detection of HPV31 neutralizing antibodies after natural infection (n = 123 subjects)
| ELISA result | Population group (no. of patients) | ELISA antibodies
|
No. (%) of patient samples with neutralizing activity | Neutralizing antibodies
|
|||
|---|---|---|---|---|---|---|---|
| Median titer (95% CI) | Geometric mean titer (95% CI)c | Median titer (95% CI) | Geometric mean titerb (95% CI)d | ||||
| Anti-HPV31 negative | All (68) | 0 (0) | |||||
| Virgins (20) | 0 (0) | ||||||
| Sexually active women (29) | 0 (0) | ||||||
| Prostitutes (19) | 0 (0) | ||||||
| Anti-HPV31 positive | All (55) | 50 (42.8-64.4) | 66.0 (49.6-87.8) | 43 (78) | 100 (50-200) | 133.7 (85.7-208.5) | |
| Virgins (2) | 25 (25-25) | 25 (25-25) | 2 (100) | 25 (25-25) | 25 (25-25) | ||
| Sexually active women (34) | 50 (25-50) | 61.3 (42.6-88.3) | 24 (71) | 100 (50-200) | 112.2 (66.6-189.3) | ||
| Prostitutes (19) | 100 (25-200) | 83.3 (49.5-140.2) | 17 (89) | 100 (50-400) | 208.3 (89.9-482.7) | ||
aELISA and neutralization end-point titers are means of two to four determinations for serum samples serially diluted twofold from 1/25 to 1/3,200.
Calculated for neutralizing antibody-positive subjects.
The P value, based on log-transformed antibody titers, for subjects, excluding virgins, was 0.31.
The P value for subjects, excluding virgins, was 0.18.
Investigation of the protective role of anti-HPV16 antibodies after natural infection indicated that ELISA titers of >400 to 800 at more than two consultations are associated with a reduced risk of subsequent infection (10). Assuming that anti-HPV16 and anti-HPV31 antibody titers are at similar levels after natural infection, this would suggest that fewer than 10% of anti-HPV31-positive subjects had protective levels of antibodies. However, Viscidi et al. (22) showed in a large prospective study conducted in Costa Rica that seropositive women had the same risk of subsequent HPV infection as seronegative women, with the most likely explanation being that the low level of antibodies elicited after natural HPV infection is not protective against viral reinfection or reactivation.
Acknowledgments
We thank Richard Roden (John Hopkins Hospital, Baltimore, MD) for the kind gift of the anti-HPV18 L2 antibody, Rebecca Font (Institut Catala d'Oncologia) for statistical analysis, and the women interviewed and medical personnel at the Dermatology Clinic of Monte Naranco Hospital in Oviedo, Spain, and Costa Ponent, Hospitalet de Llobregat, Spain.
This research was supported by funding from the Institut National de la Santé et de la Recherche Médicale (INSERM) and by a special grant from the Association Vaincre la Mucoviscidose. Maxime Fleury was supported by a fellowship from the Ministère de l'Enseignement Supérieur et de la Recherche.
Footnotes
Published ahead of print on 7 November 2007.
REFERENCES
- 1.Af Geijersstam, V., M. Kibur, Z. Wang, P. Koskela, E. Pukkala, J. Schiller, M. Lehtinen, and J. Dillner. 1998. Stability over time of serum antibody levels to human papillomavirus type 16. J. Infect. Dis. 177:1710-1714. [DOI] [PubMed] [Google Scholar]
- 2.Bousarghin, L., A.-L. Combita-Rojas, A. Touzé, S. El Mehdaoui, P.-Y. Sizaret, M. M. Bravo, and P. Coursaget. 2002. Detection of neutralizing antibodies against human papillomaviruses (HPV) by inhibition of gene transfer mediated by HPV pseudovirions. J. Clin. Microbiol. 40:926-932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Buck, C. B., D. V. Pastrana, D. R. Lowy, and J. T. Schiller. 2005. Generation of HPV pseudovirions using transfection and their use in neutralization assays. Methods Mol. Med. 119:445-462. [DOI] [PubMed] [Google Scholar]
- 4.Carter, J. L., L. A. Koutsky, G. C. Wipf, N. D. Christensen, S. Lee, J. Kuypers, N. Kiviat, and D. A. Galloway. 1996. The natural history of human papillomavirus type 16 capsid antibodies among a cohort of university women. J. Infect. Dis. 174:927-936. [DOI] [PubMed] [Google Scholar]
- 5.Christensen, N. D., J. W. Kreider, K. V. Shah, and R. F. Rando. 1992. Detection of human serum antibodies that neutralize infectious human papillomavirus type 11 virions. J. Gen. Virol. 73:1261-1267. [DOI] [PubMed] [Google Scholar]
- 6.Culp, T. D., C. M. Spatz, C. A. Reed, and N. D. Christensen. 2007. Binding and neutralization efficiencies of monoclonal antibodies, Fab fragments, and scFv specific for L1 epitopes on the capsid of infectious HPV particles. Virology 361:435-446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Gruijl, T. D., H. J. Bontkes, J. M. M. Walboomers, P. Coursaget, M. J. Stukart, C. Dupuy, E. Kueter, R. H. Verheijen, T. J. Helmerhorst, M. F. Duggan-Keen, P. L. Stern, C. J. Meijer, and R. J. Scheper. 1999. Immune responses against human papillomavirus (HPV) type 16 virus-like particles in a cohort study of women with cervical intraepithelial neoplasia. I. Differential T-helper and IgG responses in relation to HPV infection and disease outcome. J. Gen. Virol. 80:399-408. [DOI] [PubMed] [Google Scholar]
- 8.Fleury, M. J. J., A. Touzé, E. Alvarez, G. Carpentier, C. Clavel, J. F. Vautherot, and P. Coursaget. 2006. Identification of type-specific and cross-reactive neutralizing conformational epitopes on the major capsid protein of human papillomavirus type 31. Arch. Virol. 151:1511-1523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gambhira, R., B. Karanam, S. Jagu, J. N. Roberts, C. B. Buck, I. Bossis, H. Alphs, T. Culp, N. D. Christensen, and R. B. Roden. 10 October 2007. A protective and broadly cross-neutralizing epitope of human papillomavirus L2. J. Virol. doi: 10.1128/JVI.00936-07. [DOI] [PMC free article] [PubMed]
- 10.Ho, G. Y., Y. Studentsov, C. B. Hall, R. Bierman, L. Beardsley, M. Lempa, and R. D. Burk. 2002. Risk factors for subsequent cervicovaginal human papillomavirus (HPV) infection and the protective role of antibodies to HPV-16 virus-like particles. J. Infect. Dis. 186:737-742. [DOI] [PubMed] [Google Scholar]
- 11.Ho, G. Y., Y. Y. Studentsov, R. Bierman, and R. D. Burk. 2004. Natural history of human papillomavirus type 16 virus-like particle antibodies in young women. Cancer Epidemiol. Biomarkers Prev. 13:110-116. [DOI] [PubMed] [Google Scholar]
- 12.Kondo, K., Y. Ishii, H. Ochi, T. Matsumoto, H. Yoshikawa, and T. Kanda. 2007. Neutralization of HPV16, 18, 31, and 58 pseudovirions with antisera induced by immunizing rabbits with synthetic peptides representing segments of the HPV16 minor capsid protein L2 surface region. Virology 358:266-272. [DOI] [PubMed] [Google Scholar]
- 13.Pastrana, D. V., C. B. Buck, Y. Y. Pang, C. D. Thompson, P. E. Castle, P. C. Fitzgerald, S. Kruger Kjaer, D. R. Lowy, and J. T. Schiller. 2004. Reactivity of human sera in a sensitive, high-throughput pseudovirus-based papillomavirus neutralization assay for HPV16 and HPV18. Virology 321:205-216. [DOI] [PubMed] [Google Scholar]
- 14.Pastrana, D. V., R. Gambhira, C. B. Buck, Y. Y. Pang, C. D. Thompson, T. D. Culp, N. D. Christensen, D. R. Lowy, J. T. Schiller, and R. B. Roden. 2005. Cross-neutralization of cutaneous and mucosal papillomavirus types with anti-sera to the amino terminus of L2. Virology 337:365-372. [DOI] [PubMed] [Google Scholar]
- 15.Roden, R. B., E. M. Weissinger, D. W. Henderson, F. Booy, R. Kirnbauer, J. F. Mushinski, D. R. Lowy, and J. T. Schiller. 1994. Neutralization of bovine papillomavirus by antibodies to L1 and L2 capsid proteins. J. Virol. 68:7570-7574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rose, R. C., R. C. Reichman, and W. Bonnez. 1994. Human papillomavirus (HPV) type 11 recombinant virus-like particles induce the formation of neutralizing antibodies and detect HPV-specific antibodies in human sera. J. Gen. Virol. 75:2075-2079. [DOI] [PubMed] [Google Scholar]
- 17.Stauffer, Y., K. Raj, K. Masternak, and P. Beard. 1998. Infectious human papillomavirus type 18 pseudovirions. J. Mol. Biol. 283:529-536. [DOI] [PubMed] [Google Scholar]
- 18.Touzé, A., and P. Coursaget. 1998. In vitro gene transfer using human papillomavirus-like particles. Nucleic Acids Res. 26:1317-1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Touzé, A., S. El Mehdaoui, P. Y. Sizaret, C. Mougin, N. Munoz, and P. Coursaget. 1998. The L1 major capsid protein of human papillomavirus type 16 variants affects yield of virus-like particles produced in an insect cell expression system. J. Clin. Microbiol. 36:2046-2051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Touzé, A., S. de Sanjose, P. Coursaget, M. R. Almirall, V. Palacio, C. J. Meijer, J. Kornegay, and F. X. Bosch. 2001. Prevalence of anti-human papillomavirus type 16, 18, 31, and 58 virus-like particles in women in the general population and in prostitutes. J. Clin. Microbiol. 39:4344-4348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Unckell, F., R. E. Streeck, and M. Sapp. 1997. Generation and neutralization of pseudovirions of human papillomavirus type 33. J. Virol. 71:2934-2939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Viscidi, R. P., M. Schiffman, A. Hildesheim, R. Herrero, P. E. Castle, M. C. Bratti, A. C. Rodriguez, M. E. Sherman, S. Wan, B. Clayman, and R. D. Burk. 2004. Seroreactivity to human papillomavirus (HPV) types 16, 18, or 31 and risk of subsequent HPV infection: results from a population-based study in Costa Rica. Cancer Epidemiol. Biomarkers Prev. 13:324-327. [DOI] [PubMed] [Google Scholar]
- 23.Wang, S. S., M. Schiffman, R. Herrero, J. Carreon, A. Hildesheim, A. C. Rodriguez, M. C. Bratti, M. E. Sherman, J. Morales, D. Guillen, M. Alfaro, B. Clayman, R. D. Burk, and R. P. Viscidi. 2004. Determinants of human papillomavirus 16 serological conversion and persistence in a population-based cohort of 10,000 women in Costa Rica. Br. J. Cancer 91:1269-1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Winer, R. L., S. K. Lee, J. P. Hughes, D. E. Adam, N. B. Kiviat, and L. A. Koutsky. 2003. Genital human papillomavirus infection: incidence and risk factors in a cohort of female university students. Am. J. Epidemiol. 157:218-226. [DOI] [PubMed] [Google Scholar]