Abstract
Salmonella enterica serotype Newport is an important cause of salmonellosis, with strains increasingly being resistant to multiple antimicrobial agents. The increase is associated with the acquisition of multiple resistance genes. This study characterizes the genetic basis of resistance of serotype Newport isolates collected from veterinary sources by PCR and DNA sequencing analysis.
Salmonellosis is a significant public health concern in the United States. From 1997 to 2003, the number of laboratory-confirmed Salmonella enterica serovar Newport infections reported to CDC increased from 1,584 (4.6% of all reported Salmonella infections) to 4,000 (10.3%) (5). Over the same period, the percentage of multidrug-resistant serovar Newport isolates increased nearly fivefold (6). Therefore, the increasing number of serovar Newport infections appears to be associated with the emergence and rapid dissemination of multidrug-resistant (MDR) strains of serovar Newport (18). Multidrug resistance is often associated with mobile genetic elements (i.e., plasmids and transposons) that encode multiple specific resistance genes (1, 12, 13, 17, 19).
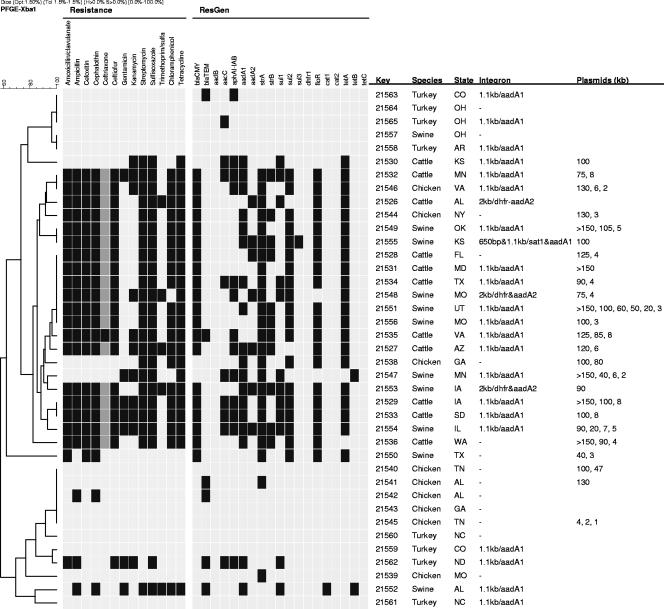
The objective of this study was to further characterize the genetic basis of multiantimicrobial resistance in Salmonella serovar Newport isolates collected from food animals in the United States. These isolates were previously characterized by pulsed-field gel electrophoresis (PFGE), by antimicrobial susceptibility testing, and for their ability to transfer resistance-conferring plasmids from MDR strains to susceptible ones (19). The subset of isolates included in the present study represents strains isolated from chicken, swine, turkey, and cattle from 23 states in the United States (Fig. 1). The susceptibilities of the isolates to the following agents were determined: amikacin, amoxicillin-clavulanic acid, ampicillin, cefoxitin, ceftiofur, ceftriaxone, cephalothin, chloramphenicol, ciprofloxacin, gentamicin, kanamycin, nalidixic acid, streptomycin, sulfisoxazole, tetracycline, and trimethoprim-sulfamethoxazole. Isolates were screened for the presence of 19 genes associated with resistance to 12 of the antibiotics in which resistance was detected previously (no resistance to amikacin, ciprofloxacin, or nalidixic acid was detected) (19). Resistance genes were detected by PCR with the primers shown in Table 1. The reactions were repeated to confirm the initial results, and representative amplification products were sequenced to verify the identities of the PCR products (7). Additionally, plasmids were isolated (16) and analyzed to determine whether there was commonality between particular plasmids and the resistance observed.
FIG. 1.
Antimicrobial susceptibility testing and antimicrobial resistance gene detection results for the Salmonella serovar Newport isolates characterized in the study. The isolates are arranged by a PFGE profile similarity dendrogram (calculated in reference 19) and are described by culture number (Key), animal of origin (Species), state of origin (State), the sizes and resistance gene inserts in the class 1 integrons (Integron), and the sizes of plasmids isolated from each strain (Plasmids [kb]). For the susceptibility testing results (Resistance), a black box indicates resistance, a light gray box susceptibility, and a darker gray box reduced susceptibility to ceftriaxone. For resistance gene detection (ResGen), a black box indicates that the gene was detected by PCR, and a light gray box indicates the absence of the gene.
TABLE 1.
PCR primers and gene targets for antimicrobial resistance
| Gene | Primera | Nucleotide sequence (5′ to 3′) | Annealing temp (°C)b | Resistance mechanism | Resistancec | Reference or source |
|---|---|---|---|---|---|---|
| aadA1 | F | TATCAGAGGTAGTTGGCGTCAT | 54 | Aminoglycoside adenyltransferase | STR | 13 |
| R | GTTCCATAGCGTTAAGGTTTCATT | |||||
| aadA2 | F | TGTTGGTTACTGTGGCCGTA | 62 | Aminoglycoside adenyltransferase | STR | 13 |
| R | GATCTCGCCTTTCACAAAGC | |||||
| aadB | F | GAGCGAAATCTGCCGCTCTGG | 61 | Aminoglycoside adenyltransferase | GEN | 13 |
| R | CTGTTACAACGGACTGGCCGC | |||||
| aacC | F | GGCGCGATCAACGAATTTATCCGA | 58 | Aminoglycoside acetyltransferase | GEN | This study |
| R | CCATTCGATGCCGAAGGAAACGAT | |||||
| aphAI-IAB | F | AAACGTCTTGCTCGAGGC | 55 | Aminoglycoside phosphoryltranferase | KAN | 13 |
| R | CAAACCGTTATTCATTCGTGA | |||||
| blaCMY | F | GACAGCCTCTCTTTCTCCACA | 50 | β-Lactamase | AMP | 13 |
| R | TGGAACGAAGGCTACGTA | |||||
| blaTEM | F | CATTTCCGTGTCGCCCTTAT | 55 | β-Lactamase | AMP | 13 |
| R | TCCATAGTTGCCTGACTCCC | |||||
| cat1 | F | CCTATAACCAGACCGTTCAG | 56 | Chlorampenicol acetyltransferase | CHL | 13 |
| R | TCACAGACGGCATGATGAAC | |||||
| cat2 | F | CCGGATTGACCTGAATACCT | 56 | Chlorampenicol acetyltransferase | CHL | 13 |
| R | TCACATACTGCATGATGAAC | |||||
| dfrI | F | GTGAAACTATCACTAATGGTAGCT | 54 | Dihydrofloate reductase inhibitor | TMP | 13 |
| R | ACCCTTTTGCCAGATTTGGTAACT | |||||
| floR | F | AACCCGCCCTCTGGATCAAGTCAA | 60 | Efflux | CHL | 13 |
| R | CAAATCACGGGCCACGCTGTATC | |||||
| strA | F | AGCAGAGCGCGCCTTCGCTC | 59 | Aminoglycoside phosphoryltranferase | STR | 13 |
| R | CCAAAGCCCACTTCACCGAC | |||||
| strB | F | ATCGTCAAGGGATTGAAACC | 49 | Aminoglycoside phosphoryltranferase | STR | 3 |
| R | GGATCGTAGAACATATTGGC | |||||
| sul1 | F | TCACCGAGGACTCCTTCTTC | 60 | Dihydropteroate synthase inhibitor | SUL | 13 |
| R | AATATCGGGATAGAGCGCAG | |||||
| sul2 | F | CGGTCCGGCATCCAGCAATCC | 64 | Dihydropteroate synthase inhibitor | SUL | 13 |
| R | CGAGAGCCACGACCGCGCC | |||||
| sul3 | F | GAGCAAGATTTTTGGAATCG | 51 | Dihydropteroate synthase inhibitor | SUL | 3 |
| R | CATCTGCAGCTAACCTAGGGCTTGGA | |||||
| tetA | F | GCTACATCCTGCTTGCCTTC | 55 | Efflux | TET | 8 |
| R | CATAGATCGCCGTGAAGAGG | |||||
| tetB | F | TTGGTTAGGGGCAAGTTTTG | 53 | Efflux | TET | 8 |
| R | GTAATGGGCCAATAACACCG | |||||
| tetC | F | CTTGAGAGCCTTCAACCCAG | 56 | Efflux | TET | 8 |
| R | ATGGTCGTCATCTACCTGCC | |||||
| intA | F | GGCATCCAAGCAGCAAGC | 50 | Class 1 integron | 13 | |
| R | AAGCAGACTTGACCTGAT | |||||
| intB | F | ATCGCAATAGTTGGCGAGT | 53 | qacEΔ-sul1 of class 1 integron | 13 | |
| R | GCAAGGCGGAAACCCGCGCC |
F, forward; R, reverse.
Annealing temperature for each PCR.
The gene encodes resistance to ampicillin (AMP), chloramphenicol (CHL), gentamicin (GEN), kanamycin (KAN), streptomycin (STR), sulfisoxazole (SUL), tetracycline (TET), and trimethoprim (TMP).
Overall, when resistance was seen, a corresponding resistance gene was detected 96.6% of the time (Fig. 1). Likewise, nearly all of the MDR strains contained large plasmids (≥75 kb), while the pansusceptible strains did not (Fig. 1). Nineteen isolates shared resistance to amoxicillin-clavulanic acid, ampicillin, cephalothin, cefoxitin, and ceftiofur and reduced susceptibility (MIC of 16 or 32 μg/ml) or resistance to ceftriaxone. Each of these isolates was positive for blaCMY, which is most commonly associated with ceftiofur and ceftriaxone resistance in Salmonella strains. A single isolate was resistant to ceftriaxone and was positive for both blaCMY and blaTEM. Five additional isolates were positive for blaTEM. Two of these five isolates were resistant to ampicillin and cephalothin; one was resistant to ampicillin, amoxicillin-clavulanic acid, and ceftiofur; and two were susceptible to all agents tested. Eleven isolates were resistant to kanamycin, and each isolate contained aphAI-IAB. Twenty-three isolates demonstrated resistance to streptomycin, and of these isolates, 21 were positive for strA, 20 were positive for aadA1, 11 were positive for strB, and 7 were positive for aadA2. Five of the seven gentamicin-resistant isolates carried aacC, while none contained aadB. Both genes have been associated with gentamicin resistance in Salmonella serovar Newport isolates (13, 17). Three isolates contained aacC but were not resistant to gentamicin. Even though they did not meet the threshold for resistance, two had decreased susceptibility (MIC of 1 and 8 μg/ml) compared to the level of susceptibility of the majority of susceptible isolates (MIC ≤ 0.25 μg/ml), likely indicating that the enzymes displayed variable levels of activity in these strains. Twenty-four isolates were resistant to sulfisoxazole; all but one contained sul1, sul2, and/or sul3. Five isolates were resistant to trimethoprim-sulfamethoxazole, and three of these isolates carried the dfrXII resistance gene in a class 1 integron (19). The remaining two isolates contained class 1 integrons that lacked dfr genes. Salmonella strains containing dfrXII have predominantly been reported in Europe and Asia, with few reports of such strains in the United States (2, 4, 9, 12, 15). Conversely, there have been reports of dfrXII-associated resistance in Escherichia coli isolates from the United States (14), indicating that the genes are present in microbial populations. Twenty isolates were resistant to chloramphenicol; 19 of these isolates were positive for floR, while the other isolate contained cat1. Additionally, 23 isolates were resistant to tetracycline. Twenty isolates contained tetA, two had tetB, and one isolate lacked the tet genes that we screened for. In cases in which an associated resistance gene was not identified, resistance was likely due to another member of the resistance gene class.
In most cases, our findings were similar to those reported previously (11, 13); however, the detection of aacC-associated gentamicin resistance is in contrast to the findings from other countries, where aadB was the predominant factor associated with gentamicin resistance in Salmonella serovar Newport (16, 19). Thus, our results, along with those of Welch et al. (17), indicate that aacC may play a larger role than aadB in gentamicin resistance in serovar Newport isolates from the United States. Additionally, the only isolate resistant to ceftriaxone contained both blaTEM and blaCMY, which likely indicates synergism among the β-lactamases. Our results also indicated that some isolates with integrons containing aadA1 were susceptible to streptomycin. Previous reports have shown that silent integron-borne aadA genes in Salmonella strains may be expressed when they are transferred to a new host by conjugation (20). All of our streptomycin-susceptible isolates that contained class 1 integrons with aadA1 were isolated from turkeys from multiple states and were spread among divergent PFGE clusters (19), which may indicate that these integrons are disseminated among serovar Newport isolates in turkey flocks. There were some additional differences among the Salmonella isolates from different animal sources, including the fact that tetB was detected only in our swine isolates and that one of these isolates was also the only strain with cat1-associated chloramphenicol resistance.
Overall, cattle and swine isolates demonstrated resistance to the greatest number of antimicrobial agents, which paralleled the results from NARMS from 2001 and 2002 (6). When the PFGE profiles of the isolates were compared, almost all MDR isolates were clustered together (19). These related strains may share a higher capacity to acquire resistance plasmids, thus contributing to the rapid rise of MDR Salmonella serovar Newport isolates over the last decade as important causes of human salmonellosis. The results of this study provide further information on the contribution of specific resistance genes to MDR in serovar Newport strains.
Acknowledgments
We thank Patrick McDermott of the U.S. Food and Drug Administration for assistance with the review of the manuscript.
We thank the Marshfield Clinic Research Foundation for their financial support for the project.
Footnotes
Published ahead of print on 29 October 2007.
REFERENCES
- 1.Aarts, H. J., K. S. Boumedine, X. Nesme, and A. Cloeckaert. 2001. Molecular tools for the characterisation of antibiotic-resistant bacteria. Vet. Res. 32:363-380. [DOI] [PubMed] [Google Scholar]
- 2.Antunes, P., J. Machado, and L. Peixe. 2007. Dissemination of sul3-containing elements linked to class 1 integrons with an unusual 3′ conserved sequence region among Salmonella isolates. Antimicrob. Agents Chemother. 51:1545-1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boerlin, P., R. Travis, C. L. Gyles, R. Reid-Smith, N. Janecko, H. Lim, V. Nicholson, S. A. McEwen, R. Friendship, and M. Archambault. 2005. Antimicrobial resistance and virulence genes of Escherichia coli isolates from swine in Ontario. Appl. Environ. Microbiol. 71:6753-6761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cabrera, R., J. Ruiz, F. Marco, I. Oliveira, M. Arroyo, A. Aladuena, M. A. Usera, M. T. Jimenez De Anta, J. Gascon, and J. Vila. 2004. Mechanism of resistance to several antimicrobial agents in Salmonella clinical isolates causing traveler's diarrhea. Antimicrob. Agents Chemother. 48:3934-3939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control and Prevention. 2005. Salmonella surveillance: annual summary, 2004. Centers for Disease Control and Prevention, Atlanta, GA.
- 6.FDA. 2006. National antimicrobial resistance monitoring system—enteric bacteria (NARMS): 2003 executive report. FDA, U.S. Department of Health and Human Services, Washington, DC.
- 7.Foley, S. L., D. G. White, P. F. McDermott, R. D. Walker, B. Rhodes, P. J. Fedorka-Cray, S. Simjee, and S. Zhao. 2006. Comparison of subtyping methods for differentiating Salmonella enterica serovar Typhimurium isolates obtained from food animal sources. J. Clin. Microbiol. 44:3569-3577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fonseca, E. L., O. L. Mykytczuk, M. D. Asensi, E. M. Reis, L. R. Ferraz, F. L. Paula, L. K. Ng, and D. P. Rodrigues. 2006. Clonality and antimicrobial resistance gene profiles of multidrug-resistant Salmonella enterica serovar Infantis isolates from four public hospitals in Rio de Janeiro, Brazil. J. Clin. Microbiol. 44:2767-2772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hsu, S. C., T. H. Chiu, J. C. Pang, C. H. Hsuan-Yuan, G. N. Chang, and H. Y. Tsen. 2006. Characterisation of antimicrobial resistance patterns and class 1 integrons among Escherichia coli and Salmonella enterica serovar Choleraesuis strains isolated from humans and swine in Taiwan. Int. J. Antimicrob. Agents. 27:383-391. [DOI] [PubMed] [Google Scholar]
- 10.Reference deleted.
- 11.Poppe, C., L. Martin, A. Muckle, M. Archambault, S. McEwen, and E. Weir. 2006. Characterization of antimicrobial resistance of Salmonella Newport isolated from animals, the environment, and animal food products in Canada. Can. J. Vet. Res. 70:105-114. [PMC free article] [PubMed] [Google Scholar]
- 12.Poppe, C., L. C. Martin, C. L. Gyles, R. Reid-Smith, P. Boerlin, S. A. McEwen, J. F. Prescott, and K. R. Forward. 2005. Acquisition of resistance to extended-spectrum cephalosporins by Salmonella enterica subsp. enterica serovar Newport and Escherichia coli in the turkey poult intestinal tract. Appl. Environ Microbiol. 71:1184-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Randall, L. P., S. W. Cooles, M. K. Osborn, L. J. Piddock, and M. J. Woodward. 2004. Antibiotic resistance genes, integrons and multiple antibiotic resistance in thirty-five serotypes of Salmonella enterica isolated from humans and animals in the UK. J. Antimicrob. Chemother. 53:208-216. [DOI] [PubMed] [Google Scholar]
- 14.Singh, R., C. M. Schroeder, J. Meng, D. G. White, P. F. McDermott, D. D. Wagner, H. Yang, S. Simjee, C. Debroy, R. D. Walker, and S. Zhao. 2005. Identification of antimicrobial resistance and class 1 integrons in Shiga toxin-producing Escherichia coli recovered from humans and food animals. J. Antimicrob. Chemother. 56:216-219. [DOI] [PubMed] [Google Scholar]
- 15.Vo, A. T. T., E. van Duijkeren, A. C. Fluit, and W. Gaastra. 2 April 2007. Antimicrobial resistance, class 1 integrons and a novel variant of genomic island 1 in Salmonella isolates from Vietnam. Antimicrob. Agents Chemother. doi: 10.1128/AAC.01093-06. [DOI] [PubMed]
- 16.Wang, Z., and T. G. Rossman. 1994. Large-scale supercoiled plasmid preparation by acidic phenol extraction. BioTechniques 16:460-463. [PubMed] [Google Scholar]
- 17.Welch, T. J., W. F. Fricke, P. F. McDermott, D. G. White, M. L. Rosso, D. A. Rasko, M. K. Mammel, M. Eppinger, M. J. Rosovitz, D. Wagner, L. Rahalison, J. E. Leclerc, J. M. Hinshaw, L. E. Lindler, T. A. Cebula, E. Carniel, and J. Ravel. 2007. Multiple antimicrobial resistance in plague: an emerging public health risk. PLoS ONE 2:e309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Zansky, S., B. Wallace, D. Schoonmaker-Bopp, P. Smith, F. Ramsey, J. Painter, A. Gupta, P. Kalluri, and S. Noviello. 2002. From the Centers for Disease Control and Prevention. Outbreak of multi-drug resistant Salmonella Newport—United States, January-April 2002. JAMA 288:951-953. [PubMed] [Google Scholar]
- 19.Zhao, S., S. Qaiyumi, S. Friedman, R. Singh, S. L. Foley, D. G. White, P. F. McDermott, T. Donkar, C. Bolin, S. Munro, E. J. Baron, and R. D. Walker. 2003. Characterization of Salmonella enterica serotype Newport isolated from humans and food animals. J. Clin. Microbiol. 41:5366-5371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhao, S., D. G. White, B. Ge, S. Ayers, S. Friedman, L. English, D. Wagner, S. Gaines, and J. Meng. 2001. Identification and characterization of integron-mediated antibiotic resistance among Shiga toxin-producing Escherichia coli isolates. Appl. Environ. Microbiol. 67:1558-1564. [DOI] [PMC free article] [PubMed] [Google Scholar]